Abstract
Background
The length of hospital stay after lower limb arthroplasty has rapidly decreased in the last decade, largely in part due to the rise of improved perioperative protocols, but also as a response to the increased economic demand associated with the rapid growth in hip and knee arthroplasty procedures. In line with this, the development of a new pathway after lower limb arthroplasty that allows for the surgery to be performed in an outpatient setting and permits for same-day discharge after the procedure is increasingly being offered. Although costs and complications between the inpatient and outpatient models have been compared, there appears to be little known about the effects on a patient’s physical function after undergoing hip or knee outpatient arthroplasty. Therefore, this systematic review aims to explore the available evidence for the effect on functional outcomes following inpatient versus outpatient hip or knee arthroplasty.
Methods
This systematic review adhered to the PRISMA guidelines and was prospectively registered (https://osf.io/8bfae/). An electronic search of three online databases (PubMed, CINAHL and EMBASE) was conducted to identify eligible studies. All studies investigating inpatient and outpatient comparator groups, for a population of patients undergoing hip or knee arthroplasty, that assessed one or more functional outcomes, were included. A methodological quality appraisal was undertaken for the final studies contained in this review. A narrative synthesis of results is described along with quantitative outcomes presented in tables and figures.
Results
A total of seven studies containing 1,876 participants were included in this review. Four studies assessed a THA population, two assessed TKA and one assessed both. Functional outcomes varied, with 20 different functional outcomes utilised, of which 18 were patient-reported tools. Results of functional outcomes offered mixed support for both inpatient and outpatient pathways.
Conclusions
The results of this review suggest that outpatient or inpatient pathway selection for hip or knee arthroplasty should not be based on the superiority of functional outcomes alone. However, given there is growing evidence in support of an outpatient pathway in select patients with respect to cost savings and without any increase in complications, it could be proposed that an equivalency of post-operative function between the two settings makes same-day discharge favourable.
Publicly registered with Open Science Framework (https://osf.io/8bfae/).
Similar content being viewed by others
Background
The prevalence of hip and knee osteoarthritis is climbing in line with increases in global lifespan and higher levels of obesity [1,2,3]. A rise in youth sporting injuries is also responsible for increased rates of posttraumatic osteoarthritis in younger adults [4, 5]. With osteoarthritis being the most commonly reported reason for undergoing lower limb arthroplasty it is not surprising that a subsequent surge in hip and knee arthroplasty procedures is predicted [6,7,8,9,10]. As the economic burden associated with the increase in these procedures grows, optimisation of health care resources and the development of sustainable perioperative delivery models are of critical consideration [6, 11,12,13].
One strategy for improving cost containment is by reducing the length of hospital stay after a hip or knee arthroplasty procedure. The financial incentive along with surgical advances and rapid recovery protocols has led to the number of average days a patient stays after arthroplasty surgery decline [10, 14,15,16]. In line with this trend for reducing the length of stay, an outpatient or same-day discharge surgery service, that can be managed in a hospital or ambulatory surgery facility, is being offered to select lower limb arthroplasty patients with increasing frequency [17,18,19,20,21,22].
Existing research suggests that along with decreased costs, there is also no increased risk of complications associated with same-day discharge after lower limb arthroplasty in appropriately selected patients [23,24,25,26,27,28]. For these reasons, utilisation of hip and knee arthroplasty in an outpatient setting has increased and is predicted to continue to do so [29,30,31]. However, typically there are select patient criteria that need to be met before undergoing lower limb arthroplasty in an outpatient setting. The recommended eligibility for outpatient surgery tends to include younger, more active patients with a lower number of comorbidities and who have social support on discharge, as such, an outpatient pathway may not be appropriate for individuals who do not meet these criteria [10, 17, 24, 30, 32]. Patients requiring an inpatient stay are more likely to require access to hygiene assistance, are at a greater risk for falls or need closer monitoring due to an increased risk of post-operative complications [33,34,35]. A risk assessment tool to help predict which patients may safely undergo same-day discharge has been developed, The Outpatient Arthroplasty Risk Assessment (OARA) score stratifies patients by nine medical categories to generate a risk category [36].
To date, most studies have focused on the comparison between inpatient and outpatient settings assessing the safety and success of the surgery as defined by costs and feasibility, or complications and readmissions [25, 37,38,39,40,41] Research investigating outcomes of function and physical performance appears to be far more limited. A recent review reported the effects on patient-reported outcome measures (PROMs) for same-day discharge patients following hip arthroplasty, however, only one included study had an inpatient comparator group [42]. Those undergoing arthroplasty in an outpatient setting have the potential to lack access to the included resources of those with a longer length of hospital stay, such as physical therapy and rehabilitative services or nursing care. Outpatient arthroplasty also relies on extensive preoperative patient education and advanced perioperative protocols for the success of the procedure. It could be suggested then that there is potential for a greater likelihood of decreased physical or self-reported functional outcomes in an outpatient population when compared to an inpatient group.
As rates of outpatient lower limb arthroplasty increase, research comparing the effects on functional outcomes to a traditional inpatient pathway could provide health care stakeholders and prospective patients with greater insight into the risks and benefits of each. If patient functional outcomes are equivalent or superior to those associated with an inpatient stay, then this combined with existing evidence to suggest the outpatient setting is both cost-effective and safe, would add further support for the uptake of the outpatient model in selected patients. Therefore, this systematic review aims to explore the available evidence for the effect on functional outcomes following inpatient versus outpatient hip or knee arthroplasty.
Methods
This systematic review has been conducted in accordance with the Preferred Reporting Items of Systematic Reviews and Meta-Analyses (PRISMA) guidelines (Additional file 1) and the review protocol has been prospectively and publicly registered with Open Science Framework (https://osf.io/8bfae/) [43, 44].
Study eligibility
Inclusion criteria were defined based on Population, Intervention, Comparison, and Outcome (PICO) method.
-
1.
Population: Adults ≥ 18 years of age who have undergone joint arthroplasty, including Total Knee Arthroplasty, Unicompartmental Knee Arthroplasty, or Total Hip Arthroplasty of any surgical approach.
-
2.
Type of Intervention: Arthroplasty surgery is performed as an outpatient procedure, either in an ambulatory surgery centre or hospital, as long as the patient discharges on the day of surgery.
-
3.
Type of Comparison: Arthroplasty surgery performed in a hospital that includes an overnight stay as an inpatient.
-
4.
Outcomes: At least one functional outcome was required, either a measure of physical performance or a patient-reported functional outcome measure could be utilised.
Exclusion criteria: (1) Articles not available in the English language and (2) Articles only available as an abstract or conference proceeding.
Search strategy
Three databases were searched up to November 4th, 2021 (PubMed, CINAHL, EMBASE). Using the advanced search strategy acquired on PubMed, the Polyglot Search Translator was then used to convert these search terms into the polyglot strings necessary for CINAHL and EMBASE [45]. Keywords used for our search included inpatient, outpatient hip arthroplasty, knee arthroplasty and uni-compartmental knee arthroplasty. Associated synonyms were also acquired using mesh terms. The full search strategies utilised across the three databases are reported in full in Appendix Table 9.
Study selection
Using the predetermined eligibility criteria, an initial search of titles and abstracts was conducted. Articles were imported to the Endnote referencing software and the Systematic Review Accelerator tool, Screenatron [46]. Prior to title and abstract screening, all duplicated studies were removed using the De-duplicator tool [47]. The screening of titles and abstracts was divided evenly and completed by three researchers (RP, LK, TC). Following this process, screening of full-text articles was performed independently by two researchers (RP, LK) who were blinded to each other’s decisions, to acquire the final studies included in this review. Any disagreement on final study inclusion was resolved by discussion with a third researcher (TC).
Data extraction
An individual researcher (TC) initially extracted the data, with two researchers (RP, LK) reviewing it upon completion to minimise the chance of error. Information extracted from studies was recorded and saved in separate tables adapted from the Cochrane Collaboration Data Collection Form, identified from the Cochrane Handbook for Systematic Reviews of interventions [48]. The data collected included items that related to study population characteristics, outcomes assessed, and results of functional outcomes measures.
Methodological quality assessment
A methodological quality appraisal was conducted on included articles in this systematic review, in line with recommended frameworks for conducting systematic reviews [43]. For assessing the quality of the individual articles included, the Joanna Biggs Institute (JBI) critical appraisal tools were utilised [49]. Two researchers (RP, TC) independently assessed the included articles using the relevant JBI appraisal tool that related to the study design and an agreement score was reported. Any disagreement on appraisal scores was resolved by discussion and consensus agreement with a third researcher (LK). The agreement score was converted into a percentage obtaining a quality grade; over 61% were considered of good methodological quality, between 45.4 and 61.0% were considered “fair” and < 45.4% were considered “poor” quality [50]. The Kappa coefficient statistic was used to measure the interrater reliability and agreement between the two researchers (RP, TC). Kappa coefficient agreement values range from near perfect, 0.81–1.00, substantial, 0.61–0.80, moderate, 0.41–0.60, fair, 0.21–0.40, and slight 0.0–0.2 [51].
Results synthesis
Results have been presented for each study and grouped according to outcome measures. A narrative synthesis of the results of all studies is described along with the quantitative outcomes presented in Tables 4, 5, 6, 7 and 8. To aid comparison between studies, where effect measures are reported in an included study, means and standard deviations are recounted in the respective table for each functional outcome, along with the significance level (P value) between the inpatient and outpatient group results.
Results
Literature search and study characteristics
The initial search of the three databases resulted in a combined total of 3422 articles. Of those articles, 1,593 were removed as duplicates leaving 1829 to be reviewed at title and abstract level for eligibility. Following a second full-text screening of 55 articles, a final seven studies were included in this review [52,53,54,55,56,57,58]. The complete search and screening process is outlined in Fig. 1.
Methodological quality assessment results
The articles included in this systematic review underwent a methodological quality appraisal, which was conducted independently by two researchers (RP, TC) and found all studies to be of good methodological quality (> 61%). The agreement between individual scores produced a Cohen’s Kappa result of 0.687, which demonstrated substantial agreement between the two authors (Appendix Table 10). Disagreements were resolved by discussion and consensus with a third researcher (LK) which produced a final Kappa score of 1.00. The full methodological critical appraisal results are reported in Appendix Table 10.
Characteristics of included studies
Of the included studies, four assessed THA, two assessed TKA and one assessed both, however, no included study assessed UKA as part of their population. Study design varied, five provided a cohort study, one a randomised control trial and one a case–control study. A total of 1,876 participants were assessed, with the inpatient group representing a larger sample with 1043 participants. Overall, most participants were aged > 53 years, with a younger age range shown in the outpatient population. Female sex prevalence was greater in the inpatient population (55%) versus the outpatient population (43%). Study characteristics are reported in full in Table 1. Inclusion and exclusion criteria denoting patient eligibility for the outpatient pathway differed between studies, similarities within the criteria pertained to overall patient health relating to co-morbidities that would exclude the patient from an outpatient pathway. However, there was variation on specific eligibility criteria, such as age, with only two studies reporting on inclusion for this [54, 58]. The complete inclusion and exclusion criteria for all studies are reported in Table 2.
Outcomes assessed
A total of 20 functional outcome measures were identified across all studies (Table 3). The majority of these being PROMs with the visual analogue scale (VAS), Harris hip score (HHS) and patient-reported satisfaction score all presenting across three or more studies. The remaining outcomes were present across less than three studies, while only one study assessed measures of physical performance; gait analysis and timed up and go (TUG) [58].
Summary of evidence
The combined results of all studies are reported in Tables 4, 5, 6, and 7 (Table 8).
Pain intensity and function
Concerning decreased pain for the studies investigating a THA population, VAS scores between studies displayed results that were conflicting, with two studies favouring the inpatient group [52, 54] while two studies favoured the outpatient group[57, 58]. Timepoints of these assessments also varied, the results favouring the inpatient group were taken at time points less than three months after surgery, whereas the results favouring the outpatient group were assessed on the day of discharge and at a two-year follow-up. Only one study that included a TKA population reported significantly less pain between the two groups, which was on post-operative day two, and this favoured the inpatient group [55]. Rosinsky, 2020 was the only study to present a significance for outcomes measuring hip function (HHS and modified HHS) in THA patients, which favoured the outpatient group at a two year follow up of participants [57]. No study investigating a TKA population showed a difference in functional outcomes assessed between the two groups.
Satisfaction and quality of recovery
Across the included studies there was no significant difference between outpatient and inpatient groups for patient-reported satisfaction in both the THA and TKA populations assessed. Postoperative day one Quality of Recovery scores (QoR-9) presented favourably towards the outpatient group in one TKA study; however, each time point following indicated no significant difference in scores between groups [53]. There were no other outcome measures utilised in the THA or TKA studies that reported a statistical significance between the outpatient and inpatient groups.
Discussion
Perioperative surgical and anaesthetic advancements, increased economic pressures, and the recognised need to maximise patient satisfaction after lower limb arthroplasty, have led to a rise in the number of THA and TKA procedures being performed in an outpatient setting. To the best of our knowledge, this is the first systematic review to explore the evidence for the effects of undergoing knee or hip arthroplasty in either an inpatient or outpatient setting on patient functional outcomes, the results of which demonstrated mixed support for either pathway.
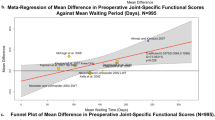
A notable observation was that the majority of studies only utilised PROMs in their assessment and did not measure changes in physical performance outcomes such as gait, strength, endurance, or range of movement parameters. Additionally, the clinical and methodological heterogeneity across studies was considerable, multiple different functional outcomes were utilised and the assessment time points and follow-up periods of these also varied. The lack of randomisation in six out of the seven included trials is likely responsible for selection bias and the diversity of eligibility criteria within the included studies further limits the ability to compare the reported outcomes between groups. For these reasons, a meta-analysis was not feasible. However, despite the described limitations, this review still conjures some support for the outpatient setting as a good option for appropriately selected patients when other benefits of the pathway are considered.
Results for pain intensity across the studies were mixed. Some studies demonstrated a short-term (< 3 months) benefit for reduced pain following an inpatient pathway, however, the differences in pain decreased over time between both settings. The lower reporting of pain in the inpatient group in both THA and TKA study populations could potentially be explained by the outpatient group’s earlier mobilisation and more limited access to analgesia in the domestic environment [59]. In contrast, two THA studies found lower VAS scores in favour of the outpatient groups at short- and long-term assessment points [57, 58], these conflicting results are in line with existing evidence, demonstrating variation in pain scores between the two settings [24, 42].
Interestingly, functional outcomes in one study investigating a THR population (HHS and mHHS) favoured the outpatient pathway at a follow-up of two years, which cannot be explained by between-group differences given the inpatient and outpatient populations were case-matched [57]. Another study, this time investigating a TKA population, reported on improved quality of recovery (QoR-9) for the outpatient group compared to the inpatient group on post-operative day one [53]. This is an important finding as the inpatient setting provides greater access to resources in the acute post-operative period than those who are discharged the same day; however, this did not appear to be a significant factor in patient reporting of their quality of recovery from the TKA procedure.
The clinical implications of these results provide evidence suggesting non-inferior functional outcomes for an outpatient pathway when compared to a traditional inpatient stay after THA or TKA, which further strengthens the support for this option in selected patients. For outcomes assessing pain, self-reported function and quality of life there were no results which solely favoured the inpatient group in the included studies. Additionally, the lack of significance in difference across all other functional outcomes assessed, suggests that outpatient lower limb arthroplasty does not result in poorer self-reported outcomes or outcomes of physical performance when compared to an inpatient setting.
The observations of this review can assist to guide future research comparing inpatient to outpatient settings for TKA or THA. With respect to outcome measures, validated assessments of physical function should be included rather than relying on PROMs alone. As although PROMs capture a person’s perception of their own health and physical function, they lack the objectivity that performance-based physical assessments provide. Further, of the 55 studies assessed for eligibility at full-text, 35 were excluded for not including a functional outcome of any type. An additional recommendation based on the results of this review would be to clearly define and report eligibility criteria for each pathway, and where possible, consider randomisation to mitigate the effects of selection bias within trials.
Conclusion
The results of this systematic review suggest that outpatient or inpatient pathway selection for hip or knee arthroplasty should not be based on the superiority of functional outcomes alone. However, given there is growing evidence in support of an outpatient pathway in select patients with respect to cost savings and without any increase in complications, it could be proposed that an equivalency of post-operative function between the two settings makes same-day discharge favourable.
Availability of data and materials
Not applicable.
Abbreviations
- ADL:
-
Activities of daily living
- ASA:
-
American Society of Anaesthesiologists Physical Status Classification system
- BMI:
-
Body mass index
- DOS:
-
Day of surgery
- F:
-
Female
- HHS:
-
Harris Hip Score
- IP:
-
Inpatient
- JBI:
-
Johanna Briggs Institute
- M:
-
Male
- NHMRC:
-
National Health and Medical Research Council
- NR:
-
Not reported
- nSDD:
-
Not same-day discharge
- OA:
-
Osteoarthritis
- OARA:
-
Outpatient arthroplasty risk assessment
- OP:
-
Outpatient
- POD:
-
Post-operative day
- PRISMA:
-
Preferred reporting items for systematic reviews and meta-analyses
- PROMs:
-
Patient-reported outcome measures
- QoR:
-
Quality of recovery
- SD:
-
Standard deviation
- SDD:
-
Same-day discharge
- SR:
-
Sport and recreation
- THA:
-
Total hip arthroplasty
- TKA:
-
Total knee arthroplasty
- TUG:
-
Timed up and go
- UKA:
-
Unicompartmental knee arthroplasty
- VAS:
-
Visual Analogue Scale
References
Palazzo C, et al. Risk factors and burden of osteoarthritis. Ann Phys Rehabil Med. 2016;59(3):134–8.
Johnson VL, Hunter DJ. The epidemiology of osteoarthritis. Best Pract Res Clin Rheumatol. 2014;28(1):5–15.
Sacitharan PK. Ageing and osteoarthritis. Subcell Biochem. 2019;91:123–59.
Thomas AC, et al. Epidemiology of posttraumatic osteoarthritis. J Athl Train. 2017;52(6):491–6.
Whittaker JL, et al. Association between MRI-defined osteoarthritis, pain, function and strength 3–10 years following knee joint injury in youth sport. Br J Sports Med. 2018;52(14):934–9.
Ackerman IN, et al. The projected burden of primary total knee and hip replacement for osteoarthritis in Australia to the year 2030. BMC Musculoskelet Disord. 2019;20(1):90.
Ackerman IN, et al. Projected burden of osteoarthritis and rheumatoid arthritis in Australia: a population-level analysis. Arthritis Care Res. 2018;70(6):877–83.
Sloan M, Premkumar A, Sheth NP. Projected Volume of Primary Total Joint Arthroplasty in the US, 2014 to 2030. JBJS 2018; 100(17).
Rupp M, et al. Projections of primary TKA and THA in Germany from 2016 through 2040. Clin Orthop Relat Res. 2020;478(7):1622–33.
Price AJ, et al. Knee replacement. Lancet. 2018;392(10158):1672–82.
Masaracchio M, et al. Timing of rehabilitation on length of stay and cost in patients with hip or knee joint arthroplasty: a systematic review with meta-analysis. PLoS ONE. 2017;12(6):e0178295.
Nassar I, Fahey J, Mitchell D. Rapid recovery following hip and knee arthroplasty using local infiltration analgesia: length of stay, rehabilitation protocol and cost savings. ANZ J Surg. 2020;90(3):355–9.
Kee J, et al. Cost analysis and bundled care of hip and knee replacement. J Surg Orthop Adv. 2019;28(4):241–9.
Molloy IB, et al. Effects of the length of stay on the cost of total knee and total hip arthroplasty from 2002 to 2013. JBJS 2017; 99(5).
Guerra ML, Singh PJ, Taylor NF. Early mobilization of patients who have had a hip or knee joint replacement reduces length of stay in hospital: a systematic review. Clin Rehabil. 2014;29(9):844–54.
Jain NB, et al. Trends in epidemiology of knee arthroplasty in the United States, 1990–2000. Arthritis Rheum. 2005;52(12):3928–33.
Scully RD, Kappa JE, Melvin JS. “Outpatient”-same-calendar-day discharge hip and knee arthroplasty. J Am Acad Orthop Surg. 2020;28(20):e900–9.
Bertin KC. Minimally invasive outpatient total hip arthroplasty: a financial analysis. Clin Orthop Relat Res. 2005;435:154–63.
Aynardi M, et al. Outpatient surgery as a means of cost reduction in total hip arthroplasty: a case-control study. HSS J. 2014;10(3):252–5.
Lovald ST, et al. Complications, mortality, and costs for outpatient and short-stay total knee arthroplasty patients in comparison to standard-stay patients. J Arthroplasty. 2014;29(3):510–5.
Courtney PM, et al. Can total knee arthroplasty be performed safely as an outpatient in the medicare population? J Arthroplasty. 2018;33(7):S28–31.
Dorr LD, et al. Outpatient total hip arthroplasty. J Arthroplasty. 2010;25(4):501–6.
Courtney PM, Boniello AJ, Berger RA. Complications following outpatient total joint arthroplasty: an analysis of a national database. J Arthroplasty. 2017;32(5):1426–30.
Pollock M, et al. Outpatient total hip arthroplasty, total knee arthroplasty, and unicompartmental knee arthroplasty—a systematic review of the literature. Osteoarthr Cartil. 2016;24:S433.
Lan RH, et al. Contemporary outpatient arthroplasty is safe compared with inpatient surgery: a propensity score-matched analysis of 574,375 procedures. J Bone Joint Surg. 2021;103(7):593–600.
Migliorini F, et al. Outpatient total hip arthroplasty: a meta-analysis. Appl Sci. 2021;11(15):6853.
Huang A, Ryu J-J, Dervin G. Cost savings of outpatient versus standard inpatient total knee arthroplasty. Can J Surg. 2017;60(1):57–62.
Bemelmans YFL, et al. Safety and efficacy of outpatient hip and knee arthroplasty: a systematic review with meta-analysis. Arch Orthop Trauma Surg 2021.
Banerjee, S., et al., Outpatient lower extremity total joint arthroplasty: Where are We Heading? 2017, Slack Incorporated Thorofare, NJ. p. 72–75.
Bert JM, Hooper J, Moen S. Outpatient total joint arthroplasty. Curr Rev Musculoskelet Med. 2017;10(4):567–74.
Arshi A, et al. Outpatient total hip arthroplasty in the united states: a population-based comparative analysis of complication rates. J Am Acad Orthop Surg. 2019;27(2):61–7.
Jaibaji M, et al. Is Outpatient arthroplasty safe? A systematic review. J Arthroplasty. 2020;35(7):1941–9.
Ziemba-Davis M, Caccavallo P, Meneghini RM. Outpatient joint arthroplasty-patient selection: update on the outpatient arthroplasty risk assessment score. J Arthroplasty. 2019;34(7s):S40-s43.
Rodríguez-Merchán EC. Outpatient total knee arthroplasty: Is it worth considering? EFORT Open Rev. 2020;5(3):172–9.
Bodrogi A, Dervin GF, Beaulé PE. Management of patients undergoing same-day discharge primary total hip and knee arthroplasty. CMAJ. 2020;192(2):E34–9.
Meneghini RM, et al. Safe selection of outpatient joint arthroplasty patients with medical risk stratification: the “outpatient arthroplasty risk assessment score.” J Arthroplasty. 2017;32(8):2325–31.
Weiser MC, et al. Outpatient total hip arthroplasty has minimal short-term complications with the use of institutional protocols. J Arthroplasty. 2018;33(11):3502–7.
Bovonratwet P, et al. Comparison of outpatient vs inpatient total knee arthroplasty: an ACS-NSQIP analysis. J Arthroplasty. 2017;32(6):1773–8.
Basques BA, Tetreault MW, Della Valle CJ. Same-day discharge compared with inpatient hospitalization following hip and knee arthroplasty. J Bone Joint Surg Am. 2017;99(23):1969–77.
Edwards PK, et al. Inpatient versus outpatient total knee arthroplasty. J Knee Surg. 2019;32(8):730–5.
Bordoni V, et al. Outpatient total hip arthroplasty does not increase complications and readmissions: a meta-analysis. HIP International, 2020.
Shapira J, et al. Outcomes of outpatient total hip arthroplasty: a systematic review. Hip Int. 2021;31(1):4–11.
Page MJ, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71.
Foster ED, Deardorff A. Open science framework (OSF). J Med Libr Assoc. 2017;105(2):203–6.
Clark JM, et al. Improving the translation of search strategies using the Polyglot Search Translator: a randomized controlled trial. J Med Libr Assoc. 2020;108(2):195–207.
Clark J, et al. A full systematic review was completed in 2 weeks using automation tools: a case study. J Clin Epidemiol. 2020;121:81–90.
Rathbone J, et al. Better duplicate detection for systematic reviewers: evaluation of Systematic Review Assistant-Deduplication Module. Syst Rev. 2015;4(1):6.
Higgins JPT, Chandler TJ, Cumpston M, Li T, Page MJ, Welch VA (Editors) Cochrane Handbook for Systematic Reviews of Interventions version 6.2 (updated February 2021). 2019, Cochrane, 2021.
Jordan Z, et al. The updated Joanna Briggs Institute model of evidence-based healthcare. JBI Evid Implement. 2019;17(1):58–71.
Viera AJ, Garrett JM. Understanding interobserver agreement: the kappa statistic. Fam Med. 2005;37(5):360–3.
Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33(1):159–74.
Gabor JA, et al. Similar outcomes after hospital-based same-day discharge vs inpatient total hip arthroplasty. Arthroplasty Today. 2020;6(3):451–6.
Gauthier-Kwan OY, Dobransky JS, Dervin GF. Quality of recovery, postdischarge hospital utilization, and 2-year functional outcomes after an outpatient total Knee Arthroplasty Program. J Arthroplasty. 2018;33(7):2159-2164.e1.
Goyal N, et al. Otto Aufranc Award: a multicenter, randomized study of outpatient versus inpatient total hip arthroplasty. Clin Orthop Rel Res. 2017;475(2):364–72.
Husted CE, et al. Are functional outcomes and early pain affected by discharge on the day of surgery following total hip and knee arthroplasty? Acta Orthop. 2020;92(1):62–6.
Kolisek FR, et al. Comparison of outpatient versus inpatient total knee arthroplasty. Clin Orthop Relat Res. 2009;467(6):1438–42.
Rosinsky PJ, et al. Outpatient vs inpatient hip arthroplasty: a matched case-control study on a 90-day complication rate and 2-year patient-reported outcomes. J Orthop Surg Res. 2020;15(1):367.
Zomar BO, et al. Perioperative gait analysis after total hip arthroplasty: Does outpatient surgery compromise patient outcomes? Can J Surg J. 2021;64(4):E407–13.
Hoofwijk DMN, et al. Prevalence and predictive factors of chronic postsurgical pain and global surgical recovery 1 year after outpatient knee arthroscopy: a prospective cohort study. Medicine. 2015;94(45):e2017.
Acknowledgements
Not applicable.
Funding
The authors have no funding to declare.
Author information
Authors and Affiliations
Contributions
LS contributed to concept and search strategy development, manuscript writing and results reporting and analysis, editing for final manuscript version. LK contributed to search and screening, manuscript writing and results reporting and analysis. RP contributed to search and screening, manuscript writing and results reporting and analysis. TC contributed to search and screening, manuscript writing and results reporting and analysis. WH contributed to manuscript writing and results reporting and analysis, editing for final manuscript version. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
PRISMA 2020 Checklist.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Sattler, L., Kisaloff, L., Cragnolini, T. et al. A comparison of functional outcomes following inpatient versus outpatient hip or knee arthroplasty. J Orthop Surg Res 17, 372 (2022). https://doi.org/10.1186/s13018-022-03270-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13018-022-03270-7