Abstract
Background
Patients who do not respond to conservative treatment of the isthmus are often treated with surgery. We used direct repair plus intersegment pedicle screw fixation for the treatment of lumbar spondylolysis. The aim of this observational study was to assess the effects of this technique and evaluate various risk factors potentially predicting the probability of disc and facet joint degeneration after instrumentation.
Methods
The study included 54 male L5 spondylolysis patients who underwent pars repair and intersegment fixation using pedicle screws. Bony union was evaluated using reconstruction images of computed tomography. Radiographic changes, including disc height, vertebral slip, facet joint and disc degeneration in the grade of adjacent and fixed segments, were determined from before to final follow-up. Logistic regression analysis was performed to identify factors associated with the incidence of disc and facet joint degeneration.
Results
Bony union was achieved in all cases. Logistic regression analysis revealed that instrumentation durations of greater than 15.5 months and 21.0 months were significant risk factors for the incidence of L4/5 and L5S1 facet degeneration, respectively.
Conclusions
Intersegmental pedicle screw fixation provides good surgical outcomes and good isthmic bony union rates in patients with lumbar spondylolysis. The duration of fixation was confirmed as a risk factor for facet joint degeneration. Once bony union is achieved, instrument removal should be recommended.
Similar content being viewed by others
Background
Lumbar spondylolysis refers to a defect of the vertebral pars interarticularis caused by stress fracture and occurs in approximately 6% of the general population, and the incidence of symptomatic spondylolysis is reported to be higher in athletes [1]. The lesion is mainly located at L5 (85–95%) and L4 (5–15%) but can occur at any level [2].
Generally, patients with low back pain due to spondylolysis are often managed conservatively with medication, physical therapy, and injection treatment [3, 4]. Surgery is indicated when in patients who experience no response to comprehensive conservative treatment for more than 6 months as well as those with persistent back pain and pars nonunion. Increasing pain, worsening of preexisting neurological impairment and progressive olisthesis are also indications for surgical treatment [3, 5].
In this study, we used direct repair plus intersegment pedicle screw fixation for the treatment of lumbar spondylolysis. This method fixes an active segment, which may limit the flexibility of the spine, increase the load on the adjacent segments of the fixed segment and cause adjacent segment degeneration (ASD) [6, 7]. However, pedicle screws can be removed when bony union is achieved, and whether it accelerates the degeneration of adjacent segments is unclear. To our knowledge, postoperative instability between adjacent segments, facet joint and disc degeneration have not been examined in a single-center study of cases in which lumbar intersegmental pedicle screw fixation was performed.
The purpose of this study was to reveal the effect of intersegmental pedicle screw fixation in the treatment of lumbar disc herniation and to evaluate various risk factors that may predict the possibility of degeneration of the intervertebral disc and facet joints.
Materials and methods
Patients
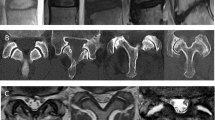
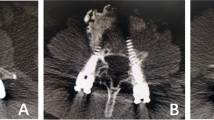
We retrospectively evaluated consecutive spondylolysis patients who underwent pars repair and segmental fixation using pedicle screws at our institution between January 2016 and January 2018. All 54 patients were male, and the lesion was located at L5. Patients with symptomatic spondylolysis were treated with direct iliac bone graft repair combined with intersegmental pedicle screw fixation. Plain radiographs, computed tomography (CT) and magnetic resonance imaging (MRI) were evaluated at 6, 12, 18 and 24 months postoperatively. Instrumentation was removed after bony union was achieved (illustrative cases, Figs. 1 and 2). Local ethical committee and Institutional Research Board approval were obtained for the study.
Preoperative and postoperative images obtained in a 21-year-old man with L5 spondylolysis. a–c Preoperative radiographs, CT scan and MRI. d One-week postoperative radiographs. e 12-Month follow-up CT scan showed bilateral bony union of the pars defect. f 15-Month postoperative MRI. g 15-Month postoperative radiographs showed that the lumbar instrumentations had been removed. h–i 15-Month postoperative CT scan and MRI
Preoperative and postoperative images obtained in a 19-year-old man with L5 spondylolysis. a–c Preoperative radiographs, CT scan and MRI. d One-week postoperative radiographs. e 9-Month follow-up CT scan. f 15-Month radiographs showed that the lumbar instrumentations had been removed. g–h 15-Month postoperative CT scan and MRI
Spondylolysis of the lumbar spine was diagnosed by five spine surgeons (HM, ZCZ, GMZ TSS and FL) as follows. All patients with low back pain had simple radiographs of the lumbar spine (anteroposterior, lateral and oblique views). If needed, a CT scan was performed to confirm the presence or absence of spondylolysis. In addition, patients with definite spondylosis on lumbar spine radiographs and CT scans underwent MRI of the lumbar spine to detect other spinal problems, such as disc degeneration and herniation. Surgical treatment was recommended for the following conditions: a patient with low back pain diagnosed with lumbar disc herniation, no response to conservative treatment at least 6 months, and MRI scans revealed no or mild degeneration of the intervertebral disc at the level of the pars defect. The exclusion criteria were radiological signs of spondylolisthesis or instability, previous spinal surgery, significant radicular pain, and improvement after conservative treatment.
Operative procedures
The operation was performed under general anesthesia. The patient was placed in a prone position, and fluoroscopy was used to localize the surgical level. A 10-cm posterior midline incision was made. After incision of the lumbosacral fascia at 2 cm paraspinous process, the multifidus and longissimus muscles were identified and dissected away. The pars defects were exposed using curette and burr, carefully leaving facet joints intact. The lysis was prepared by removing fibrous tissue in and around the gap. The bony elements on both sides of the lysis were decorticated to assure bony healing of the lysis after pars repair. Cancellous bone grafts were harvested unilaterally from the iliac wing and implanted into the pars. Four pedicle screws were implanted to fix the isthmic vertebra and the adjacent distal vertebra. Instrumentation was removed after bony fusion was achieved.
Radiological outcomes
Bony union was evaluated using CT reconstruction images at each follow-up. Reconstructions were made in both the axial and sagittal planes, allowing us to determine the degree of union.
From preoperative to final follow-up, imaging changes, such as disc height, vertebral slippage, facet joints and disc degeneration at adjacent and fixed levels, were determined. The relationship between CT and MRI findings and the progression of degeneration based on preoperative grading were also evaluated.
Disc height and vertebral slip at the L4/5 and L5/S1 levels were measured on lateral plain radiographs. The disc height was measured using Miyakoshi's procedures [8]. On the lateral radiograph, the following points to be marked were identified: the corners of the vertebral bodies, the midpoints of the endplates, and the midpoints of the walls of the vertebral bodies. The points were determined strictly according to the criteria of Quint et al. [9]. Using these easily defined points, the heights of the L4/5 and L5S1 discs were measured. The disc height (DH) was calculated as the mean of the anterior, middle and posterior disc heights. The sagittal diameter of the vertebral body from the anterior to posterior margin was measured at the mid-vertebral level, and the disc height index (DHI) was calculated as the disc height/sagittal diameter of the vertebral body [10].
Disc degeneration of the adjacent and fixed segments was reviewed using MRI during the follow-up. Disc degenerative grading was measured using the Pfirrmann 5-grade classification, which ranges from grades 1 to 5 [11]. Facet joint degeneration was measured using the classification for osteoarthritis of the Japanese Orthpaedic Association (JOA), which includes grades 0 to 4. Grade 0 indicates severe degeneration, whereas Grade 4 indicates a normal joint without degeneration [12].
All surgeries were performed using the same procedures by four spine surgeons (HM, ZCZ, GMZ and FL) at our institution, and the incidence of complications was compared between the two groups. Potential risk factors for disc and facet joint degeneration, such as age, obesity (body mass index, BMI), duration of fixation, vertebral slip and facet joint degeneration before primary surgery, were identified by reviewing medical records. Imaging assessment was assessed by two spine surgeons (ZCZ and GMZ). The inter-observer reliability was assessed by weighted kappa statistic. The degree of inter-observer reliability for qualitative measures was almost perfect for preoperative and end of follow-up measurements of facet degeneration grade on CT (pre: 0.795, end of follow-up: 0.854) and disc degeneration grade on MRI (pre: 0.821, end of follow-up: 0.833).
The demographic and clinical data of patients are in accordance with the normal distribution (Kolmogorov–Smirnov one-sample test, all p > 0.05). Student’s t test or analysis of variance was used for continuous variables, and Fisher’s exact test was used for categorical variables. SPSS software, version 23.0 (SPSS, Chicago, IL, USA), was used for all analyses, and a two-sided p value < 0.05 was considered statistically significant. Logistic regression analysis was performed to identify factors independently associated with the incidence of disc and facet joint degeneration.
Results
At the time of the primary surgery, the mean age was 22.76 years (18 to 34). The mean BMI was 22.81 kg/m2 (19.23 to 24.77). Bony union was achieved in all cases as confirmed by CT reconstruction, and the mean fixed time was 17.04 months (8 to 39). No complications were observed during the follow-up.
Patient characteristics of disc and facet joint degeneration detected on plain radiographs are shown in Table 1. Decreased disc height in the upper adjacent segment L4/5 of ≥ 20% occurred in one patient, whereas decreased disc height in the fixed segment L5/S1 of ≥ 20% was observed in one patient. The disc height of the upper adjacent segment L4/5 was reduced by 20% to 10% in 7 patients, and 8 patients were observed in the fixed segment L5/S1. CT indicated facet joint degeneration at L4/5 and L5/S1 in 7 and 9 patients, respectively. MRI showed disc degeneration at L4/5 and L5/S1 in 5 patients, separately.
The mean disc height in the upper adjacent segment L4/5 was 14.17 ± 1.74 before surgery and 14.01 ± 2.23 after removal of instruments. The mean DHI in L4/5 was 0.381 ± 0.03 before surgery and 0.370 ± 0.04 after removal of instruments. The mean disc height in the fixed segment L5/S1 was 14.13 ± 1.90 before surgery and 13.82 ± 2.03 after removal of instruments. The mean DHI in L5S1 was 0.389 ± 0.05 before surgery and 0.380 ± 0.05 after removal of internal fixation. No significant differences were observed (Table 2). There were 15 patients with a DHI decrease ≥ 10% and 39 patients with a DHI decrease ≤ 10%. Regarding the L5S1 level, the number of preoperative facet joint degeneration patients with a DHI reduction of ≥ 10% was 9 cases, and the number of patients with a DHI reduction of < 10% was 34 cases. The difference is significant (p < 0.05). The difference was significant (p < 0.05). Preoperative DHI decreased by ≥ 10% in 12 cases, and DHI decreased by less than 10% in 29 cases, but the difference was not significant (Table 3). Regarding the L4/5 level, no significant differences were observed between the DHI changes and preoperative facet joint and disc degeneration (Table 3).
In the analysis of L4/5 and L5S1 disc degeneration, no significant differences in demographic data (age, BMI, duration of instrument fixation, vertebral slip, and preoperative facet and disc degeneration change) were noted between the two groups (degeneration group and no degeneration group) (Table 4). In the analysis of L4/5 facet degeneration, no significant differences in demographic data (BMI, vertebral slip, and preoperative facet and disc degeneration change) were noted between the two groups (degeneration group and no degeneration group); however, the facet degeneration group showed a significantly older age and longer duration of instrument fixation than the no degeneration group (Table 5). In the analysis of L5S1 facet degeneration, no significant differences in demographic data (age, vertebral slip, and preoperative facet and disc degeneration change) were noted between the two groups (degeneration group and no degeneration group). The facet degeneration group showed a significantly higher BMI and longer duration of instrument fixation than the no degeneration group (Table 5).
Logistic regression analysis
To reveal the relative impact of variables on facet and disc degeneration, logistic regression analysis was performed. The variables from the univariate analysis that were associated with the incidence of ASD included age, BMI, duration of instrument fixation, vertebral slip, and preoperative facet and disc degeneration change. Logistic regression analysis revealed that a duration of instrument fixation of greater than 15.5 months was a significant risk factor for the incidence of L4/5 facet degeneration (p = 0.006; odds ratio: 1.337, 95% CI 1.108–1.615). For the duration of fixation, a cutoff value of 15.5 months was determined to discriminate with the highest sensitivity, a receiver operating characteristic (ROC) curve specificity based on receiver operating characteristic (ROC) curve analysis. The area under the curve (AUC) was 0.86 (95% confidence interval 0.74–0.99). A fixation time longer than 21.0 months was a significant risk factor for L5S1 facet joint degeneration (p = 0.001; odds ratio: 1.379, 95% CI 1.133–1.679). The AUC was 0.95 (95% confidence interval 0.88–1.00) (Table 6 and Fig. 3).
Logistic regression and ROC analysis. a L4/5: a cutoff value of 15.5 months at which classification according to fixed time yields a sensitivity of 100% and specificity of 60%. The area under the curve AUC is 0.80. b L5S1: a cutoff value of 21.0 months at which classification according to fixed time yields a sensitivity of 89% and specificity of 89%. The area under the curve AUC is 0.80
Evaluation of aggravation based on preoperative grade suggested that patients with facet joint degeneration at L4/5 pre-operation exhibited no significant difference in greater progression of degeneration compared to patients without preoperative facet joint degeneration. The same results were noted for the L5S1 level. The preoperative grade of facet degeneration was not associated with the postoperative progression of disc degeneration, and preoperative disc degeneration exhibited no relationship with the postoperative progression of facet degeneration.
Discussion
A considerable number of patients, especially young patients, complain of lumbar pain or have bilateral lumbar spondylolysis during physical examination, without or only mild lumbar spondylolisthesis, and usually have no neurological problems in imaging, symptoms and signs [13, 14]. However, consensus or guidelines for the treatment of these patients are not available. The treatment of simple bilateral lumbar spondylolysis can be divided into conservative treatment and surgical treatment [15]. The current clinically accepted view is that active surgical treatment should be adopted for patients who experience no improvement with conservative treatment for 6 months and are in the terminal stage of isthmic fissure on imaging [3, 16].
Previous studies have revealed a great number and variety of surgical techniques for spondylolysis repair, demonstrating the lack of consensus on a satisfactory procedure. Treatment mainly includes intersegmental fusion and intrasegmental isthmus repair [17]. For patients with simple lumbar spondylolisthesis, fusion has an effect on the fixation of the vertebral body, which can effectively prevent the diseased vertebral body from further spondylolisthesis. However, mobility of the fused segment is sacrificed, and the procedure may accelerate the degeneration of adjacent segments. Intrasegment repair is considered to preserve anatomical structure [18]. With the improvement in surgical techniques and the development of materials, surgical methods have gradually developed from early isthmic lag screws [19], transverse process–spinous process wires [20] and screw-hook constructs [21] to shaped rods and combination techniques. However, each of these approaches has limitations. The isthmus is too small to choose a suitable lag screw, and the lack of bone grafting in the isthmus leads to difficulties in bone healing. The wiring technique requires greater surgical exposure with extensive stripping of the muscle to expose the transverse process completely. The uneven force on the bilateral transverse processes can lead to complications, such as transverse process fractures and wire loosening, which may lead to nonunion of the pars defect. Gillet et al. [22] first used “V” rods to connect bilateral pedicle screws instead of laminar hook fixation. Ulibarri et al. [23] used a “U”-shaped titanium rod to connect bilateral pedicle universal screws and achieved a satisfactory fusion rate [24]. Although the hook-screw and shaped rod methods have achieved satisfactory results, a considerable number of spondylolysis patients are associated with laminosis or dysplasia of spinous processes [25], which may affect fixation strength. The use of minimally invasive techniques for the surgical management of spondylolysis has also been reported. Goldstein et al. used cortical screws and a spinous-process modular link in a minimally invasive fashion under intraoperative CT navigation [26]. Ghobrial et al. treated lumbar spondylolysis via a minimally invasive direct pars repair with cannulated screws [27].
In this study, compared with other techniques that require extensive muscle stripping, exposing the transverse process and injuring the interspinous ligament, intersegmental pedicle screws seem to be a technically simple and safe procedure. Easy surgical access through the Wiltse approach allows minimal soft tissue dissection and reduced blood loss. Hyperextension and rotation are the main stresses in the fatigue fracture of the isthmus. Compared with the above-mentioned various methods of intrasegment fixation, intersegment fixation provides stronger stability to resist rotation and extension. In addition, intersegment fixation compresses the isthmus, increases the degree of bone contact and promotes a higher fusion rate. Otherwise, for cases with spondylolisthesis within grade 1 and mild disc degeneration, motion segment fixation can correct and stabilize the spondylolisthesis. Compared with the method of intrasegmental fixation, it has the disadvantage of fixing the moving segment. Therefore, to restore the mobility of this segment, we removed the internal fixation early after CT confirmed complete isthmus healing.
Both facet joints and intervertebral discs are involved in the stability of the lumbar spine structure [28, 29] and are associated with degeneration of adjacent segments [30, 31]. To our knowledge, the incidence and risk factors for fixed and adjacent segment degeneration after intersegment pedicle screw fixation for lumbar spondylolysis have not been previously investigated. In this study, we identified the risk factors for facet joint and disc degeneration to predict and prevent this condition. After the follow-up of 54 patients, 100% bone healing was achieved. Only one patient exhibited a reduction in disc height of ≥ 20% in the upper and fixed segments. When the internal fixation was removed, we found a 9% incidence of grade 1 disc degeneration at the L4/5 and L5S1 levels (based on the Pfirrmann 5-grade classification system). Previous studies reported adjacent biomechanical alterations after lumbar fusion. Umehara et al. [32] reported that the load burden and weight shearing of the posterior column increased significantly at the adjacent segments. Weinhoffer et al. [33] also reported a significant increase in the disc pressure in the levels above the fused segments. In a systematic review, Harrop et al. [34] reported a 9% incidence of ASD after total disc replacement and a 34% incidence after fusion. We also found that 15% of the L4/5 level and 17% of the L5S1 level had a height reduction of greater than 10%, but the difference between pre- and postsurgery was not significant. The incidence of facet joint degeneration was 13% at the L4/5 level and 17% at the L5S1 level. Facet joint degeneration may arise from different mechanisms. First, surgical factors, such as damage to the articular process during screw placement, may lead to an increased risk of facet joint degeneration. Increased loading of the adjacent level after fixation also increases the load on the surrounding facet joints [35, 36]. Biomechanical studies have shown that the facet load can increase at the level of surgery after intervertebral fusion [37]. Although no intervertebral fusion was noted in this study, intersegmental fixation may also increase the load on the facet joint.
The ankylosis of facet joint articulation is a well-known consequence of spinal fusion procedures. Complete ankylosis of the zygapophyseal joints represents the realization of true spinal fusion [38]. In fact, the removal of the means of synthesis seems to slow down this process [39]. The results of this study suggest that fixation time is a risk factor associated with the development of facet degeneration. The nondegeneration cutoff value of fixed time has been hypothesized to be within 15.5 months. In fact, patients in this series with successful pars union presented a mean fixed time of 17.04 months. Therefore, regular postoperative follow-up is required to determine the bony union of the pars defect. Once bony union is achieved, removal of the internal fixation should be recommended. In addition, bone morphogenetic protein 2 (BMP-2) can be used to enhance fusion at an earlier time point [40]. The earlier bony union occurs, the lower the incidence of facet joint degeneration. Second, our results demonstrate that older age and higher BMI are associated with a higher incidence of facet joint degeneration at the L4/5 and L5S1 levels, respectively. In addition, sagittal balance and spinopelvic parameters also probably influence facet joint degeneration development [41]. Further study is needed to analyze spinopelvic parameters.
This study has some limitations. First, it was a retrospective study and was not performed as a comparative study. Second, the sample size in the present study was limited, which may increase the chances of making a type II error. Third, radiologic evaluations, including sagittal alignment assessment, were not performed.
Conclusions
In this study, intersegmental pedicle screw fixation provided good surgical outcomes and good isthmic bony union rates in patients with lumbar spondylolysis. The duration of fixation was confirmed as a risk factor for facet joint degeneration. Once bony union is achieved, removal of the instruments is recommended.
Abbreviations
- ASD:
-
Adjacent segment degeneration
- CT:
-
Computed tomography
- MRI:
-
Magnetic resonance imaging
- DH:
-
Disc height
- DHI:
-
Disc height index
- JOA:
-
Japanese Orthpaedic Association
- BMI:
-
Body Mass Index
- AUC:
-
Area under the curve
- ROC:
-
Receiver operating characteristic curve
- BMP-2:
-
Bone morphogenetic protein 2
References
Bouras T, Korovessis P. Management of spondylolysis and low-grade spondylolisthesis in fine athletes. A comprehensive review. Eur J Orthop Surg Traumatol. 2015;25(Suppl 1):S167–75.
Standaert CJ, Herring SA. Spondylolysis: a critical review. Br J Sports Med. 2000;34(6):415–22.
Lim MR, Yoon SC, Green DW. Symptomatic spondylolysis: diagnosis and treatment. Curr Opin Pediatr. 2004;16(1):37–46.
Blanda J, Bethem D, Moats W, Lew M. Defects of pars interarticularis in athletes: a protocol for nonoperative treatment. J Spinal Disord. 1993;6(5):406–11.
Radcliff KE, Kalantar SB, Reitman CA. Surgical management of spondylolysis and spondylolisthesis in athletes: indications and return to play. Curr Sports Med Rep. 2009;8(1):35–40.
Park P, Garton HJ, Gala VC, Hoff JT, McGillicuddy JE. Adjacent segment disease after lumbar or lumbosacral fusion: review of the literature. Spine (Phila Pa 1976). 2004;29(17):1938–44.
Cheh G, Bridwell KH, Lenke LG, Buchowski JM, Daubs MD, Kim Y, et al. Adjacent segment disease following lumbar/thoracolumbar fusion with pedicle screw instrumentation: a minimum 5-year follow-up. Spine (Phila Pa 1976). 2007;32(20):2253–7.
Miyakoshi N, Abe E, Shimada Y, Hongo M, Chiba M, Sato K. Anterior decompression with single segmental spinal interbody fusion for lumbar burst fracture. Spine (Phila Pa 1976). 1999;24(1):67–73.
Quint DJ, Tuite GF, Stern JD, Doran SE, Papadopoulos SM, McGillicuddy JE, et al. Computer-assisted measurement of lumbar spine radiographs. Acad Radiol. 1997;4(11):742–52.
Inoue H, Ohmori K, Miyasaka K, Hosoe H. Radiographic evaluation of the lumbosacral disc height. Skeletal Radiol. 1999;28(11):638–43.
Pfirrmann CW, Metzdorf A, Zanetti M, Hodler J, Boos N. Magnetic resonance classification of lumbar intervertebral disc degeneration. Spine (Phila Pa 1976). 2001;26(17):1873–8.
Imagama S, Kawakami N, Matsubara Y, Tsuji T, Ohara T, Katayama Y, et al. Radiographic adjacent segment degeneration at 5 years after L4/5 posterior lumbar interbody fusion with pedicle screw instrumentation: evaluation by computed tomography and annual screening with magnetic resonance imaging. Clin Spine Surg. 2016;29(9):E442–51.
Hu SS, Tribus CB, Diab M, Ghanayem AJ. Spondylolisthesis and spondylolysis. Instr Course Lect. 2008;57:431–45.
Gagnet P, Kern K, Andrews K, Elgafy H, Ebraheim N. Spondylolysis and spondylolisthesis: a review of the literature. J Orthop. 2018;15(2):404–7.
Kreiner DS, Baisden J, Mazanec DJ, Patel RD, Bess RS, Burton D, et al. Guideline summary review: an evidence-based clinical guideline for the diagnosis and treatment of adult isthmic spondylolisthesis. Spine J. 2016;16(12):1478–85.
Fujii K, Katoh S, Sairyo K, Ikata T, Yasui N. Union of defects in the pars interarticularis of the lumbar spine in children and adolescents. The radiological outcome after conservative treatment. J Bone Joint Surg Br. 2004;86(2):225–31.
Westacott DJ, Cooke SJ. Functional outcome following direct repair or intervertebral fusion for adolescent spondylolysis: a systematic review. J Pediatr Orthop B. 2012;21(6):596–601.
de Bodman C, Bergerault F, de Courtivron B, Bonnard C. Lumbo-sacral motion conserved after isthmic reconstruction: long-term results. J Child Orthop. 2014;8(1):97–103.
Buck JE. Direct repair of the defect in spondylolisthesis. Preliminary report. J Bone Joint Surg Br. 1970;52(3):432–7.
Johnson GV, Thompson AG. The Scott wiring technique for direct repair of lumbar spondylolysis. J Bone Joint Surg Br. 1992;74(3):426–30.
Morscher E, Gerber B, Fasel J. Surgical treatment of spondylolisthesis by bone grafting and direct stabilization of spondylolysis by means of a hook screw. Arch Orthop Trauma Surg. 1984;103(3):175–8.
Gillet P, Petit M. Direct repair of spondylolysis without spondylolisthesis, using a rod-screw construct and bone grafting of the pars defect. Spine (Phila Pa 1976). 1999;24(12):1252–6.
Ulibarri JA, Anderson PA, Escarcega T, Mann D, Noonan KJ. Biomechanical and clinical evaluation of a novel technique for surgical repair of spondylolysis in adolescents. Spine (Phila Pa 1976). 2006;31(18):2067–72.
Mohammed N, Patra DP, Narayan V, Savardekar AR, Dossani RH, Bollam P, et al. A comparison of the techniques of direct pars interarticularis repairs for spondylolysis and low-grade spondylolisthesis: a meta-analysis. Neurosurg Focus. 2018;44(1):E10.
Seitsalo S, Osterman K, Hyvarinen H, Tallroth K, Schlenzka D, Poussa M. Progression of spondylolisthesis in children and adolescents. A long-term follow-up of 272 patients. Spine (Phila Pa 1976). 1991;16(4):417–21.
Goldstein MJ, Bruffey J, Eastlack RK. New minimally invasive technique for direct pars interarticularis osteosynthesis using cortical screws and spinous-process modular link. Spine (Phila Pa 1976). 2016;41(23):E1421–4.
Ghobrial GM, Crandall KM, Lau A, Williams SK, Levi AD. Minimally invasive direct pars repair with cannulated screws and recombinant human bone morphogenetic protein: case series and review of the literature. Neurosurg Focus. 2017;43(2):E6.
Fujiwara A, Lim TH, An HS, Tanaka N, Jeon CH, Andersson GB, et al. The effect of disc degeneration and facet joint osteoarthritis on the segmental flexibility of the lumbar spine. Spine (Phila Pa 1976). 2000;25(23):3036–44.
Fujiwara A, Tamai K, An HS, Kurihashi T, Lim TH, Yoshida H, et al. The relationship between disc degeneration, facet joint osteoarthritis, and stability of the degenerative lumbar spine. J Spinal Disord. 2000;13(5):444–50.
Liang J, Dong Y, Zhao H. Risk factors for predicting symptomatic adjacent segment degeneration requiring surgery in patients after posterior lumbar fusion. J Orthop Surg Res. 2014;9:97.
Lee CS, Hwang CJ, Lee SW, Ahn YJ, Kim YT, Lee DH, et al. Risk factors for adjacent segment disease after lumbar fusion. Eur Spine J. 2009;18(11):1637–43.
Umehara S, Zindrick MR, Patwardhan AG, Havey RM, Vrbos LA, Knight GW, et al. The biomechanical effect of postoperative hypolordosis in instrumented lumbar fusion on instrumented and adjacent spinal segments. Spine (Phila Pa 1976). 2000;25(13):1617–24.
Weinhoffer SL, Guyer RD, Herbert M, Griffith SL. Intradiscal pressure measurements above an instrumented fusion. A cadaveric study. Spine (Phila Pa 1976). 1995;20(5):526–31.
Harrop JS, Youssef JA, Maltenfort M, Vorwald P, Jabbour P, Bono CM, et al. Lumbar adjacent segment degeneration and disease after arthrodesis and total disc arthroplasty. Spine (Phila Pa 1976). 2008;33(15):1701–7.
Dunlop RB, Adams MA, Hutton WC. Disc space narrowing and the lumbar facet joints. J Bone Joint Surg Br. 1984;66(5):706–10.
Adams MA, Dolan P. Recent advances in lumbar spinal mechanics and their clinical significance. Clin Biomech (Bristol, Avon). 1995;10(1):3–19.
Serhan HA, Varnavas G, Dooris AP, Patwadhan A, Tzermiadianos M. Biomechanics of the posterior lumbar articulating elements. Neurosurg Focus. 2007;22(1):E1.
Proietti L, Perna A, Ricciardi L, Fumo C, Santagada DA, Giannelli I, et al. Radiological evaluation of fusion patterns after lateral lumbar interbody fusion: institutional case series. Radiol Med. 2021;126(2):250–7.
Proietti L, Perna A, Schiro GR, Noia G, Fumo C, Tamburrelli FC. Residual mobility after removal of instrumentation in patient, with type a2–a3 vertebral fractures, treated with percutaneous pedicle screw fixation. J Biol Regul Homeost Agents. 2019;33(2 Suppl. 1):133–9 (XIX Congresso Nazionale S I C O O P Societa' Italiana Chirurghi Ortopedici Dell'ospedalita' Privata Accreditata).
Behrbalk E, Uri O, Parks RM, Musson R, Soh RC, Boszczyk BM. Fusion and subsidence rate of stand alone anterior lumbar interbody fusion using PEEK cage with recombinant human bone morphogenetic protein-2. Eur Spine J. 2013;22(12):2869–75.
Kim MW, Lee KY, Lee S. Factors associated with the symptoms of young adults with L5 spondylolysis. Asian Spine J. 2018;12(3):476–83.
Acknowledgements
We thank Xiumei Liu, Junfeng Wang and Simeng Zhang for their assistance with data acquisition.
Funding
The study was supported by the PLA Training Injury Prevention Project, China (no. 20XLS34) and the Capital Health Research and Development of Special Funding (no. 2020-2-5091). The funding bodies had no role in the design of the study or in collection, analysis, interpretation or presentation of data.
Author information
Authors and Affiliations
Contributions
HM was involved in conception and design, drafting the article, analysis and interpretation of data. YG was responsible for analysis and interpretation of data. PL was involved in study data collection and preliminary data analysis. GMZ, ZCZ and TSS were involved in study conception, surgery and patient’s management. FL was involved in study conception, supervision and administrative support. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The clinical retrospective study protocol was established, according to the ethical guidelines of the Helsinki Declaration and was approved by the Human Ethics Committee of the Seventh Medical Center of PLA General Hospital. Written informed consent was obtained from individual or guardian participants.
Consent for publication
The patients consented to the publication of their pictures as well as their anonymous and clustered data.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Meng, H., Gao, Y., Lu, P. et al. Risk factor analysis of disc and facet joint degeneration after intersegmental pedicle screw fixation for lumbar spondylolysis. J Orthop Surg Res 17, 247 (2022). https://doi.org/10.1186/s13018-022-03082-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13018-022-03082-9