Abstract
Background
The risk factors of postoperative delirium (POD), a serious while preventable complication, developed by patients undergoing knee and replacement surgery are still under investigation. In this systematic review and meta-analysis, we identified risk factors associated with POD in knee and hip replacement.
Methods
PubMed, Ovid MEDLINE, and Ovid EMBASE were used to identify original researches. The studies evaluating the risk factors of POD after knee and hip replacement were reviewed, and the qualities of the included studies were assessed with Newcastle–Ottawa Scale. Data were extracted, pooled, and a meta-analysis was completed
Result
Twenty-two studies were finally included with a total of 11934 patients who underwent knee or hip replacement and 1841 developed POD with an incidence of 17.6% (95% confidential interval (CI) 13.2–22.0%). Eighteen significant risk factors were identified including advanced age (odds ratio (OR) 1.15 95% CI 1.08–1.22), cognitive impairment (OR 6.84, 95% CI 3.27–14.33), history of cerebrovascular events (OR 2.51, 95% CI 1.28–4.91), knee replacement (OR 1.42, 95% CI 1.00–2.02), blood loss (standardized mean difference (SMD) 0.30, 95% CI 0.15–0.44), dementia (OR 3.09, 95% CI 2.10–4.56), neurologic disorders (OR 2.26, 95% CI 1.23–4.15), psychiatric illness (OR 2.74, 95% CI 1.34–5.62), and obstructive sleep apnea (OR 4.17, 95% CI 1.72–10.09) along with several comorbidity evaluation scores and laboratory markers.
Conclusion
We identified risk factors consistently associated with the incidence of POD in knee and hip replacement. Strategies and interventions should be implemented to the patients receiving knee or hip replacement with potential risk factors identified in this meta-analysis.
Similar content being viewed by others
Background
Knee and hip replacement surgeries have been performed for decades and are the most common procedures in the orthopedic department. Annually, there would be 512,000 hip replacement and 700,000 knee replacement in the USA [1, 2], and the demand continues to grow worldwide for the outcomes are satisfying based on pain relief and function improvement. Mainly, these procedures are performed in the age group of those older than 60 years [1, 2]. However, complications may disturb the rehabilitation and outcomes of the procedures, and postoperative delirium (POD) serves as a very common one.
As an acute decline in cognitive function, POD is serious and costly which mainly affects elderly people aged 65 years and older with an incidence rate of 12–51% in orthopedic surgery [3]. It is associated with an increase in mortality and morbidity, prolonged length of hospital stay, and worse surgical outcomes [3, 4]. However, POD is preventable with multi-component and targeted interventions which aim to optimize the mobility, nutrition, orientation, cognitive function, and sleep [5, 6]. Therefore, identifying the patients with the potential risks of developing POD, for whom to receive the specific interventions, is important. Numerous risk factors have been identified in the medical, surgical, and intensive care clinical population, while, to be specific, the risk factors in the knee and hip replacement of POD are still under investigation [3, 7]. In joint replacement surgery, a meta-analysis revealed that 17% of patients who underwent total knee or hip replacement surgery developed POD [8], and a systematic review summarized that general anesthesia, advanced age, history of psychiatric illness, decreased functional status, and specific anesthetic agents would raise the POD rate [9]. However, the existing meta-analysis and systematic reviews have not provided the pooled estimation of risk factors or only summarized the incidence of POD in the knee and hip replacement.
As the elderly population is in the majority of patients undergoing knee or hip replacement which is also at a higher risk of POD, understanding the delirium risk factors may help the surgeons, patients, therapists, and caregivers in providing targeting interventions. The current meta-analysis aims to pool the prevalence and risk factors of POD in patients undergoing knee or hip replacement surgery from existing literature as no formal systematic review or meta-analysis has been performed to date. The result would be helpful and could be used by the clinical team of the joint replacement department in optimizing the perioperative program aiming at lowering the incidence of POD among patients undergoing knee and hip replacement.
Methods
Literature search
The PubMed, Ovid MEDLINE, and Ovid EMBASE were used to identify original research published all through March 2020 with following keywords: “joint replacement,” “joint arthroplasty,” “knee replacement,” “knee arthroplasty,” “hip replacement,” “hip arthroplasty,” “TJR,” “TJA,” “TKR,” “TKA,” “THR,” “THA,” “delirium,” and “confusion.” References in identified articles and systematic reviews were scanned manually for possible inclusion.
Eligibility criteria
The original studies included in this meta-analysis should meet the criteria as follows: (1) only assessing patients who underwent knee or hip replacement, (2) available prevalence or risk factors of POD or data from POD and non-POD patients, (3) used any validated tools (Diagnostic and Statistical Manual of Mental Disorders (DSM) [10], Confusion Assessment Method (CAM) [11], or Delirium Rating Scale (DRS) [12], etc.) for POD assessment; and (4) cohort, case-control, and cross-section studies. Studies assessing delirium after discharge and subsyndromal delirium or any other kind of cognitive impairment were not included.
Study selection
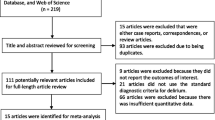
Endnote was used for two levels of screening by two reviewers. Firstly, we screen the titles and abstracts of the articles based on the inclusion criteria for eligible studies. Secondly, the full-text articles were screened. After that, disagreements of the inclusion and exclusion of the articles were discussed to reach the final agreement between the two reviewers. The flow diagram was presented in Fig. 1 and supplement file 1, and the PRISMA checklist was presented in supplement file 2.
Data extraction
Two reviewers independently extracted the data from the included studies. At first, the characteristics including titles, authors, year of publication, study design, sample size, type of surgery, and assessment tools of the included studies would be summarized. Then, the risk factors of POD from the included studies were extracted. Importantly, the definitions of each risk factor from different studies were also extracted to prevent misunderstanding. When multiple studies reported the data from the same source, we would adopt the study with the longest follow-up, the largest sample size, or more valid data. Missing data were sought from the corresponding authors where possible. Finally, the disagreements of the extracted data were resolved through discussion.
Methodological quality assessment
The non-randomized studies included in this meta-analysis were assessed with the Newcastle–Ottawa Scale (NOS) [13] by two independent reviewers. It is a validated and recommended tool for non-randomized studies’ methodological quality describing. The scores of NOS consist of selection criteria, comparability, and outcome (cohort study) or exposure (case-control study). A maximum of 9 scores reveals the highest quality.
Statistical analysis
The odds ratios (ORs) or standardized mean differences (SMDs) with 95% confidential intervals (CIs) were calculated and pooled where a risk factor was examined by two or more included studies to estimate the association between the risk factors and POD. The between-study heterogeneity was tested with I2 which was guided by the Cochrane Handbook for Systematic Reviews of Interventions. The random-effect model was used to calculate the pooled ORs or SMDs when significant heterogeneity was presented (I2 > 50%). And the fixed-effect model was used in the absence of statistical heterogeneity. Incidences of delirium were pooled by the random-effect model which drives an overall effect estimate with 95% CIs. A statistically significant risk factor for POD was considered at a two-tailed p value < 0.05. Forest plots were used to summarize the outcomes of meta-analyses. For a risk factor demonstrated by at least 10 studies, we assessed for the potential publication bias with visual funnel plots for symmetry and Eggar’s test. When a statistically significant bias was demonstrated (p < 0.05), a trim-and-fill method was used to reveal the missing studies and, adjusting for publication bias, provide a combined effect estimate. All statistical analyses were conducted in StataSE 15.0 using metan and associating modules.
Result
Characteristics of studies
One thousand three hundred twenty abstracts and titles were included from the initial electronic search. After deduplication, 928 abstracts were scanned based on eligibility criteria which excluded 746 studies and the remaining 182 were screened with full text (Fig. 1). Finally, 22 studies (Table 1) [14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35] with a total of 11934 patients were included in this meta-analysis and in which 1841 cases were found with POD. Four studies [36,37,38,39] were excluded due to sharing the same cohorts with included ones [15, 17, 27] which derived the longest follow-up. The result of methodological assessment demonstrated a moderate to high quality of the included studies (Table 2) in which four studies scored 9 [15, 24, 28, 29], seven studies scored 8 [14, 18, 19, 22, 23, 25, 27], five studies scored 7 [17, 26, 30,31,32], four studies scored 6 [16, 20, 21, 34], and two studies scored 5 [33, 35]. A total of 28 potential risk factors were initially summarized in this meta-analysis (Table 3).
Incidence of POD
All the included studies reported the incidence of POD which range from 0.6 to 36.6%. A pooled incidence of POD was 17.6% (Fig. 2a, 22 studies, 11934 patients, 95% CI 13.2–22.0%, I2 = 98.6%). Separately, for knee replacement, a pooled incidence was 16.4% (Fig. 2b, 11 studies, 8439 patients, 95% CI 10.1–22.8%, I2 = 99.0%), and for hip replacement, it was 18.8% (Fig. 2b, 11 studies, 2406 patients, 95% CI 15.8–26.2%, I2 = 89.8%).
Risk factors
Advanced age
A total of 15 studies reported the mean age in POD and non-POD groups, and a pooled SMD revealed that POD patients were mildly older (Fig. 3a, SMD 0.43 years, 95% CI 0.24–0.61, p < 0.001, I2 = 73.4%) than the non-POD patients. Further, 11 studies reported advanced age as a prognostic factor for POD with a pooled OR of 1.15 (Fig. 3b, 95% CI 1.08–1.22, p < 0.001, I2 = 63.5%). Funnel plots showed a significant asymmetry (Fig. 3c, Eggar’s p < 0.001). Trim-and-fill revealed that after adjusting for publication bias, the pooled OR remains at 1.12 (95% CI 1.05–1.19, I2 = 64.4% p < 0.001, 5 filled) which sustained the effect estimate was reliable.
Cognitive impairment
As a recognized risk factor for POD, most studies excluded patients with cognitive impairment for removing confounding factors. Three studies reported the patients with cognitive impairment were at higher risk of POD (Fig. 4a, OR 6.84, 95% CI 3.27–14.33, p < 0.001, I2 = 0.0%) without heterogeneity. The Mini-Mental State Examination (MMSE) test is a 30-point questionnaire which is used to measure the cognitive impairment [40]; any score less than 24 indicates an abnormal cognition. In this meta-analysis, a pooled estimate from eleven studies revealed that the MMSE score in the POD group was significantly lower (Fig. 4b, SMD–0.32, 95% CI (− 0.52, 0.13), p = 0.001, I2 = 57.1%) without publication bias (Eggar’s p = 0.455).
History of cerebrovascular events
Cerebrovascular events, stroke, and transient ischemia, etc., were defined as prognostic factors for POD [3]. Four of the included researches paid attention, and the pooled OR was 2.51 (Fig. 5, 95% CI 1.28–4.91, I2 = 58.4%, p = 0.007) with statistical significance and mild heterogeneity.
Medical comorbidities
Common neuropsychiatric comorbidities were reported in certain studies. Dementia was identified as a prognostic factor for POD [3], and our result demonstrated dementia was a significant risk factor for POD with a pooled OR of 3.09 (Fig. 6a, 95% CI 2.10–4.56, p < 0.001, I2 = 38.6%, 5 studies). Further, neurological disorders (Parkinson’s disease, etc.) were reported in five studies and the result of meta-analysis revealed an OR of 2.26 (Fig. 6b, 95% CI 1.23–4.15, p < 0.001, I2 = 0.0%). Last but not the least, patients with psychiatric illness were evaluated in two studies. The pooling of data derived an OR of 2.74 (Fig. 6c, 95% CI 1.34–5.62, p = 0.006, I2 = 0.0%) which confirmed the prognostic effect of psychosis.
Association has been found between sleep disturbance and POD [41]. The pooling of data from two studies which demonstrated the data between obstructive and POD derived an OR of 4.17 (Fig. 6d, 95% CI 1.72–10.09, p = 0.002, I2 = 0.0%) with statistical significance.
Surgical and anesthesia factors
Performing knee or hip replacement may result in a different rate of POD. Six studies reported the POD incidence in the knee and hip replacement cohort. The meta-analysis result showed that compared with the hip replacement, knee replacement surgery derived an OR of 1.42 (Fig. 7a, 95% CI 1.00–2.02, p = 0.048, I2 = 9.8%) for POD without heterogeneity. Further, the duration of surgery of patients in the POD group was longer (Fig. 7b, SMD 0.29, 95% CI 0.06–0.52, p = 0.013, I2 = 57.4%, 7 studies) and the blood loss was worse (Fig. 7c, SMD 0.30, 95% CI 0.15–0.44, p < 0.001, I2 = 0.0%, 4 studies).
On the other hand, the comparison between anesthesia types was reported by five studies. Patients who underwent spinal anesthesia were less likely to sustain POD when compared with general anesthesia and the combinable OR was 0.62 (Fig. 7d, 95% CI 0.46–0.85, p = 0.003, I2 = 45.7%).
Preoperative evaluation of comorbidities
Multiple preoperative evaluations of the patients’ physical status demonstrated differences existing between the POD group and the non-POD group. Eight studies reported that patients with American Society of Anesthesiologists’ (ASA) score III or above were at a higher risk for developing POD (Fig. 8a, OR 1.59, 95% CI 1.25–2.03, p < 0.001, I2 = 29.3%). Further, the Charlson Comorbidity Index (CCI), reported by five studies, was higher in the POD group compared with that in the non-POD group (Fig. 8b, SMD 0.35, 95% CI 0.04–0.66, p = 0.029, I2 = 56.9%).
Laboratory test
Several preoperative laboratory indicators were presented in certain studies. Patients suffered from POD showed a lower level in total protein (Fig. 9a, 2 studies, SMD − 0.68, 95% CI (− 0.87, − 0.48), p < 0.001, I2 = 0.0%), albumin (Fig. 9b, 2 studies, SMD − 0.77, 95% CI (− 1.36, − 0.19), p = 0.009, I2 = 71.6%), and preoperative hemoglobin (Fig. 9c, 6 studies, SMD − 0.58, 95% CI (− 1.11, − 0.04), p = 0.034, I2 = 94.4%).
Discussion
The current meta-analysis included 22 studies and presented an incidence of 17.6% (Fig. 2) in knee and hip replacement patients. It was consistent with a previous meta-analysis that concluded 17.3% of patients who underwent total joint replacement would develop POD [8]. We identified 28 potential prognostic factors, and 18 revealed statistically significant. Preoperative factors included advanced age, education, ASA and CCI scores, cognitive impairment, neuropsychiatric comorbidities, obstructive sleep apnea, and history of cerebrovascular events. Surgery-related factors were knee replacement, duration of surgery, blood loss, and general anesthesia. Significance difference existed in some laboratory markers including preoperative total protein, albumin, and hemoglobin. Besides, there was a prolonged length of stay of patients who suffered from POD (SMD − 0.53, 95% CI (0.20, 0.87), p = 0.002, I2 = 56.7%).
Advanced age was a robust prognostic factor. Our study reported that the admission age was 2.7 years older in the POD group with a mild prognostic strength (OR 1.15). The previous researches demonstrated a wide range of OR (1.07–12.95) of advanced age in surgical awards [42,43,44], and the possible reason was the definition of “advanced age” and surgical types differed between studies. Age-related cerebral changes in stress-regulating neurotransmitter and intracellular signal transduction systems were the main reasons for the development of delirium in elderly patients [45]. Further, ASA ≥ III (OR 1.59) or higher CCI (SMD 0.35) were significant indicators that sustain that patients with a deteriorated physical status were susceptible to POD. A previous meta-analysis also indicated older patients with frailty had more chance of developing POD [46]. Indeed, inflammation and sickness may result in aberrant stress response under the surgical circumstance which is vulnerable to POD [47]. Generally, as the gerontic patients are the main population receiving knee or hip replacement, physical status evaluation should be routinely carried out with much attention paid to the advanced age or functional impaired ones.
Pre-existing cognitive impairment is a chronic, long-term status that may manifest as memory impairment, visuospatial disorders, word-finding difficulties, or changes in attention functions [48] while POD is described as an acute confusional state or altered mental status [49]. Consistent with previous meta-analyses [50, 51], we showed patients with pre-existing cognitive impairment are at a higher risk for developing POD (OR 6.84). The age-related cerebral change with the effects of cerebrovascular events, which was also a prognostic factor proved in the study, can result in susceptibility to delirium when biologically stressed, especially when underlying cognitive impairment exists, not to mention surgical stress [47, 52]. Further, patients with neuropsychiatric disorders were more susceptible to POD due to inflammation, chronic stress, neuronal damage, and impaired cholinergic function [53]. We proved that the MMSE score differs between groups significantly. It highlighted that preoperative cognitive assessment would be effective in screening potential delirium-risk patients which was verified by several studies [22, 30, 33]. Therefore, joint replacement surgeons should put the cognitive assessment in the standardized program for elective surgery [54].
Patients who developed delirium were more often those who underwent knee replacement, with longer surgical time, and suffered worse blood loss. It is unclear why knee replacement is a risk factor of POD. We suppose that firstly, the initial diagnoses of patients who underwent knee replacement were more likely inflammatory disease [1], osteoarthritis and rheumatoid arthritis, etc., and as for hip replacement trauma, dysplasia, or necrosis played a part [2]. And an inflammation state may promote the pathophysiology process of delirium [47]. Secondly, patients may suffer greater pain after knee replacement, and it indicates extension analgesic burdens which may be contributory [55]. Finally, in knee replacement, the utilization of a tourniquet was common but it would increase neuroinflammatory burden via the washout of an ischemic limb [17]. Consistently with a previous study, prolonged duration of surgery may contribute to the development of POD [56]. As theory says the possible pathophysiology of delirium is disruptions of cerebral autoregulation, which can occur during surgery [57], a prolonged surgery would result in exacerbated hypercapnia, hypothermia, and worse blood loss, which all contribute to diminished autoregulation and triggers POD. This result draws attention to the complex knee replacement operation including bilateral replacement and revision. For patients with a potential risk of POD receiving this kind of surgery, thorough preoperative planning by experienced surgeons and anesthetists was essential to guarantee the surgery would be completed safely and quickly.
Spinal anesthesia was associated with reduced OR for POD (OR 0.62). This result is consistent with several previous studies [8, 58, 59]. Recently, two high-volume retrospective population-based studies both revealed a 17–45% decrease of odds when compared with general anesthesia. However, the underlying mechanism remains controversial. The spinal anesthesia has the effect of reducing the delirium risk that may be related to the reduction of systemic anesthetic drugs which affect the central nervous system [60]. A study compared epidural with general anesthesia and found a significant mental change after total hip arthroplasty in the general anesthesia group while no change in the epidural group [61]. The explanation was that general anesthesia may lead to potential hyperventilation, reduced cardiac output, reduced cerebral blood flow, postoperative hypoxemia, and cerebral vasoconstriction which all contribute to the development of POD [61]. This result indicates general anesthesia in knee and hip replacement was a risk factor for POD. Preoperative planning of the anesthetic type to certain patients who are under a potential risk of POD would be indispensable, and, when possible, spinal anesthesia should be chosen.
There were several limitations to this study. First, we used both unadjusted ORs and adjusted ORs to pool the final estimates. Some of the studies reported only unadjusted effect measures, which limited their ability to account for possible confounders. Including these data may result in overestimated results. Second, heterogeneity existed in some outcomes. Due to the limited number of studies, the heterogeneity could not always be adequately explored. However, the random-effect model was used when I2 > 50%, and the heterogeneity of results summarized from sufficient studies were explored and the reliability was confirmed. Third, the subtypes of the knee or hip replacement surgery were not evaluated in this study. Some included studies reported data from hemiarthroplasty, revision surgeries, or bilateral surgeries. Due to the lack of sufficient original data, we did not perform subgroup analysis.
Our study had several strengths. First, we presented 28 potential risk factors among which 18 were statistically significant while the previous meta-analysis only reported pooled incidence of POD in the knee and hip replacement [8], and the risk factors were summarized in a systematic review without an overall estimation of effects [9], which meant this is by far the first study to quantitatively summarize the risk factors for the postoperative delirium after knee replacement or hip replacement. Second, twenty-two studies and over 11,000 patients were included in this meta-analysis which gave us sufficient data to investigate the possible prognostic factors. Third, every included study was carefully screened with methodology assessment resulting in a moderate to high quality, which meant the extracted data was reliable.
Conclusion
In summary, this meta-analysis found POD was common in the knee or hip replacement surgery. And we identified 18 significant risk factors from patient-related and operation-related fields. Future efforts should be made to determine the risk factors in each subtype of joint replacement and which risk factors should be paid more attention to and how to quantify them. This meta-analysis suggested joint replacement surgeons perform cognitive assessment preoperatively and look into the reasons for the prognostic strength of knee replacement.
Availability of data and materials
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
References
Price AJ, Alvand A, Troelsen A, Katz JN, Hooper G, Gray A, Carr A, Beard D. Knee replacement. Lancet. 2018;392(10158):1672–82. https://doi.org/10.1016/S0140-6736(18)32344-4.
Ferguson RJ, Palmer A Jr, Taylor A, Porter ML, Malchau H, Glyn-Jones S. Hip replacement. Lancet. 2018;392(10158):1662–71. https://doi.org/10.1016/S0140-6736(18)31777-X.
Inouye SK, Westendorp RGJ, Saczynski JS. Delirium in elderly people. Lancet. 2014;383(9920):911–22. https://doi.org/10.1016/S0140-6736(13)60688-1.
Inouye SK, Marcantonio ER, Kosar CM, Tommet D, Schmitt EM, Travison TG, Saczynski JS, Ngo LH, Alsop DC, Jones RN. The short-term and long-term relationship between delirium and cognitive trajectory in older surgical patients. Alzheimers Dement. 2016;12(7):766–75. https://doi.org/10.1016/j.jalz.2016.03.005.
Chen CC-H, Li H-C, Liang J-T, Lai IR, Purnomo JDT, Yang Y-T, Lin B-R, Huang J, Yang C-Y, Tien Y-W, Chen C-N, Lin M-T, Huang G-H, Inouye SK. Effect of a modified hospital elder life program on delirium and length of hospital stay in patients undergoing abdominal surgery: a cluster randomized clinical trial. JAMA Surg. 2017;152(9):827–34. https://doi.org/10.1001/jamasurg.2017.1083.
Siddiqi N, Harrison JK, Clegg A, Teale EA, Young J, Taylor J, Simpkins SA. Interventions for preventing delirium in hospitalised non-ICU patients. Cochrane Database Syst Rev. 2016;3:CD005563. https://doi.org/10.1002/14651858.CD005563.pub3.
Sanders RD, Coburn M, Cunningham C, Pandharipande P. Risk factors for postoperative delirium. Lancet Psychiatry. 2014;1(6):404–6. https://doi.org/10.1016/S2215-0366(14)00012-1.
Scott JE, Mathias JL, Kneebone AC. Incidence of delirium following total joint replacement in older adults: a meta-analysis. Gen Hosp Psychiatry. 2015;37(3):223–9. https://doi.org/10.1016/j.genhosppsych.2015.02.004.
Bin Abd Razak HR, Yung WYA. Postoperative delirium in patients undergoing total joint arthroplasty: a systematic review. J Arthroplast. 2015;30(8):1414–7. https://doi.org/10.1016/j.arth.2015.03.012.
Diagnostic and statistical manual of mental disorders: DSM-5. 5th ed. Arlington: American Psychiatric Association; 2013,.
Inouye SK, van Dyck CH, Alessi CA, Balkin S, Siegal AP, Horwitz RI. Clarifying confusion: the confusion assessment method. A new method for detection of delirium. Ann Intern Med. 1990;113(12):941–8. https://doi.org/10.7326/0003-4819-113-12-941.
Trzepacz PT, Mittal D, Torres R, Kanary K, Norton J, Jimerson N. Validation of the Delirium Rating Scale-revised-98: comparison with the delirium rating scale and the cognitive test for delirium. J Neuropsychiatr Clin Neurosci. 2001;13(2):229–42. https://doi.org/10.1176/jnp.13.2.229.
Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25(9):603–5. https://doi.org/10.1007/s10654-010-9491-z.
Peng J, Wu G, Chen J, Chen H. Preoperative C-reactive protein/albumin ratio, a risk factor for postoperative delirium in elderly patients after total joint arthroplasty. J Arthroplast. 2019;34(11):2601–5. https://doi.org/10.1016/j.arth.2019.06.042.
Guo Y, Li Y, Zhang Y, Fang S, Xu X, Zhao A, Zhang J, Li JV, Ma D, Jia W, Jiang W. Post-operative delirium associated with metabolic alterations following hemi-arthroplasty in older patients. Age Ageing. 2019;49(1):88–95. https://doi.org/10.1093/ageing/afz132.
de Jong L, van Rijckevorsel VAJIM, Raats JW, Klem TMAL, Kuijper TM, Roukema GR. Delirium after hip hemiarthroplasty for proximal femoral fractures in elderly patients: risk factors and clinical outcomes. Clin Interv Aging. 2019;14:427–35. https://doi.org/10.2147/CIA.S189760.
Cunningham EL, McGuinness B, McAuley DF, Toombs J, Mawhinney T, O'Brien S, Beverland D, Schott JM, Lunn MP, Zetterberg H, Passmore AP. CSF Beta-amyloid 1-42 concentration predicts delirium following elective arthroplasty surgery in an observational cohort study. Ann Surg. 2019;269(6):1200–5. https://doi.org/10.1097/SLA.0000000000002684.
Oh TK, Park HY, Shin H-J, Jeon Y-T, Do S-H, Hwang J-W. The role of perioperative statin use in the prevention of delirium after total knee replacement under spinal anesthesia. J Arthroplast. 2018;33(12):3666–3671.e3661. https://doi.org/10.1016/j.arth.2018.08.022.
Xin X, Xin F, Chen X, Zhang Q, Li Y, Huo S, Chang C, Wang Q. Hypertonic saline for prevention of delirium in geriatric patients who underwent hip surgery. J Neuroinflammation. 2017;14(1):221. https://doi.org/10.1186/s12974-017-0999-y.
Wang L, Seok S, Kim S, Kim K, Lee S, Lee K. The risk factors of postoperative delirium after total knee arthroplasty. J Knee Surg. 2017;30(6):600–5. https://doi.org/10.1055/s-0036-1593872.
Huang J, Bin Abd Razak HR, Yeo SJ. Incidence of postoperative delirium in patients undergoing total knee arthroplasty-an Asian perspective. Ann Transl Med. 2017;5(16):321. https://doi.org/10.21037/atm.2017.06.40.
Culley DJ, Flaherty D, Fahey MC, Rudolph JL, Javedan H, Huang C-C, Wright J, Bader AM, Hyman BT, Blacker D, Crosby G. Poor performance on a preoperative cognitive screening test predicts postoperative complications in older orthopedic surgical patients. Anesthesiology. 2017;127(5):765–74. https://doi.org/10.1097/ALN.0000000000001859.
Choi Y-H, Kim D-H, Kim T-Y, Lim T-W, Kim S-W, Yoo J-H. Early postoperative delirium after hemiarthroplasty in elderly patients aged over 70 years with displaced femoral neck fracture. Clin Interv Aging. 2017;12:1835–42. https://doi.org/10.2147/CIA.S147585.
Yen TE, Allen JC, Rivelli SK, Patterson SC, Metcalf MR, Flink BJ, Mirrakhimov AE, Lagoo SA, Vail TP, Young CC, Moon RE, Trzepacz PT, Kwatra MM. Association between Serum IGF-I levels and postoperative delirium in elderly subjects undergoing elective knee arthroplasty. Sci Rep. 2016;6:20736. https://doi.org/10.1038/srep20736.
Guo Y, Jia P, Zhang J, Wang X, Jiang H, Jiang W. Prevalence and risk factors of postoperative delirium in elderly hip fracture patients. J Int Med Res. 2016;44(2):317–27. https://doi.org/10.1177/0300060515624936.
Chung KS, Lee JK, Park JS, Choi CH. Risk factors of delirium in patients undergoing total knee arthroplasty. Arch Gerontol Geriatr. 2015;60(3):443–7. https://doi.org/10.1016/j.archger.2015.01.021.
Cerejeira J, Batista P, Nogueira V, Vaz-Serra A, Mukaetova-Ladinska EB. The stress response to surgery and postoperative delirium: evidence of hypothalamic-pituitary-adrenal axis hyperresponsiveness and decreased suppression of the GH/IGF-1 Axis. J Geriatr Psychiatry Neurol. 2013;26(3):185–94. https://doi.org/10.1177/0891988713495449.
Flink BJ, Rivelli SK, Cox EA, White WD, Falcone G, Vail TP, Young CC, Bolognesi MP, Krystal AD, Trzepacz PT, Moon RE, Kwatra MM. Obstructive sleep apnea and incidence of postoperative delirium after elective knee replacement in the nondemented elderly. Anesthesiology. 2012;116(4):788–96. https://doi.org/10.1097/ALN.0b013e31824b94fc.
Jankowski CJ, Trenerry MR, Cook DJ, Buenvenida SL, Stevens SR, Schroeder DR, Warner DO. Cognitive and functional predictors and sequelae of postoperative delirium in elderly patients undergoing elective joint arthroplasty. Anesth Analg. 2011;112(5):1186–93. https://doi.org/10.1213/ANE.0b013e318211501b.
Priner M, Jourdain M, Bouche G, Merlet-Chicoine I, Chaumier J-A, Paccalin M. Usefulness of the short IQCODE for predicting postoperative delirium in elderly patients undergoing hip and knee replacement surgery. Gerontology. 2008;54(2):116–9. https://doi.org/10.1159/000117574.
Lowery DP, Wesnes K, Brewster N, Ballard C. Quantifying the association between computerised measures of attention and confusion assessment method defined delirium: a prospective study of older orthopaedic surgical patients, free of dementia. Int J Geriatr Psychiatry. 2008;23(12):1253–60. https://doi.org/10.1002/gps.2059.
Wacker P, Nunes PV, Cabrita H, Forlenza OV. Post-operative delirium is associated with poor cognitive outcome and dementia. Dement Geriatr Cogn Disord. 2006;21(4):221–7. https://doi.org/10.1159/000091022.
Freter SH, Dunbar MJ, MacLeod H, Morrison M, MacKnight C, Rockwood K. Predicting post-operative delirium in elective orthopaedic patients: the Delirium Elderly At-Risk (DEAR) instrument. Age Ageing. 2005;34(2):169–71. https://doi.org/10.1093/ageing/afh245.
Fisher BW, Flowerdew G. A simple model for predicting postoperative delirium in older patients undergoing elective orthopedic surgery. J Am Geriatr Soc. 1995;43(2):175–8. https://doi.org/10.1111/j.1532-5415.1995.tb06385.x.
Rogers MP, Liang MH, Daltroy LH, Eaton H, Peteet J, Wright E, Albert M. Delirium after elective orthopedic surgery: risk factors and natural history. Int J Psychiatry Med. 1989;19(2):109–21. https://doi.org/10.2190/2q3v-hyt4-nn49-bpr4.
Cerejeira J, Batista P, Nogueira V, Firmino H, Vaz-Serra A, Mukaetova-Ladinska EB. Low preoperative plasma cholinesterase activity as a risk marker of postoperative delirium in elderly patients. Age Ageing. 2011;40(5):621–6. https://doi.org/10.1093/ageing/afr053.
Cerejeira J, Nogueira V, Luís P, Vaz-Serra A, Mukaetova-Ladinska EB. The cholinergic system and inflammation: common pathways in delirium pathophysiology. J Am Geriatr Soc. 2012;60(4):669–75. https://doi.org/10.1111/j.1532-5415.2011.03883.x.
Cunningham EL, Mawhinney T, Beverland D, O'Brien S, McAuley DF, Cairns R, Passmore P, McGuinness B. Observational cohort study examining apolipoprotein E status and preoperative neuropsychological performance as predictors of post-operative delirium in an older elective arthroplasty population. Age Ageing. 2017;46(5):779–86. https://doi.org/10.1093/ageing/afx042.
Guo Y, Zhang Y, Jia P, Wang W, Zhou Q, Sun L, Zhao A, Zhang X, Wang X, Li Y, Zhang J, Jiang W. Preoperative serum metabolites are associated with postoperative delirium in elderly hip-fracture patients. J Gerontol A Biol Sci Med Sci. 2017;72(12):1689–96. https://doi.org/10.1093/gerona/glx001.
Pangman VC, Sloan J, Guse L. An examination of psychometric properties of the mini-mental state examination and the standardized mini-mental state examination: implications for clinical practice. Appl Nurs Res. 2000;13(4):209–13. https://doi.org/10.1053/apnr.2000.9231.
Fadayomi AB, Ibala R, Bilotta F, Westover MB, Akeju O. A systematic review and meta-analysis examining the impact of sleep disturbance on postoperative delirium. Crit Care Med. 2018;46(12):e1204–12. https://doi.org/10.1097/CCM.0000000000003400.
Zhu C, Wang B, Yin J, Xue Q, Gao S, Xing L, Wang H, Liu W, Liu X. Risk factors for postoperative delirium after spinal surgery: a systematic review and meta-analysis. Aging Clin Exp Res. 2019. https://doi.org/10.1007/s40520-40019-01319-y, https://doi.org/10.1007/s40520-019-01319-y.
Kubota K, Suzuki A, Ohde S, Yamada U, Hosaka T, Okuno F, Fujitani I, Koitabashi A, Shimada G, Kishida A. Age is the most significantly associated risk factor with the development of delirium in patients hospitalized for more than five days in surgical wards: retrospective cohort study. Ann Surg. 2018;267(5):874–7. https://doi.org/10.1097/SLA.0000000000002347.
Watt J, Tricco AC, Talbot-Hamon C, Pham B, Rios P, Grudniewicz A, Wong C, Sinclair D, Straus SE. Identifying older adults at risk of delirium following elective surgery: a systematic review and meta-analysis. J Gen Intern Med. 2018;33(4):500–9. https://doi.org/10.1007/s11606-017-4204-x.
van der Mast RC. Pathophysiology of delirium. J Geriatr Psychiatry Neurol. 1998;11(3):138–45; discussion 157-138. https://doi.org/10.1177/089198879801100304.
Persico I, Cesari M, Morandi A, Haas J, Mazzola P, Zambon A, Annoni G, Bellelli G. Frailty and delirium in older adults: a systematic review and meta-analysis of the literature. J Am Geriatr Soc. 2018;66(10):2022–30. https://doi.org/10.1111/jgs.15503.
Maclullich AM, Ferguson KJ, Miller T, de Rooij SE, Cunningham C. Unravelling the pathophysiology of delirium: a focus on the role of aberrant stress responses. J Psychosom Res. 2008;65(3):229–38. https://doi.org/10.1016/j.jpsychores.2008.05.019.
Langa KM, Levine DA. The diagnosis and management of mild cognitive impairment: a clinical review. Jama. 2014;312(23):2551–61. https://doi.org/10.1001/jama.2014.13806.
Marcantonio ER. Delirium in hospitalized older adults. N Engl J Med. 2017;377(15):1456–66. https://doi.org/10.1056/NEJMcp1605501.
Luan Erfe BM, Boehme J, Erfe JM, Brovman EY, Bader AM, Urman RD. Postoperative outcomes in primary total knee arthroplasty patients with preexisting cognitive impairment: a systematic review. Geriatr Orthop Surg Rehabil. 2018;9:2151459318816482. https://doi.org/10.1177/2151459318816482.
Viramontes O, Luan Erfe BM, Erfe JM, Brovman EY, Boehme J, Bader AM, Urman RD. Cognitive impairment and postoperative outcomes in patients undergoing primary total hip arthroplasty: a systematic review. J Clin Anesth. 2019;56:65–76. https://doi.org/10.1016/j.jclinane.2019.01.024.
Cole MG. Delirium in elderly patients. Am J Geriatr Psychiatry. 2004;12(1):7–21.
Fong TG, Davis D, Growdon ME, Albuquerque A, Inouye SK. The interface between delirium and dementia in elderly adults. Lancet Neurol. 2015;14(8):823–32. https://doi.org/10.1016/S1474-4422(15)00101-5.
Hanson MR, Gálvez-Jiménez N. Management of dementia and acute confusional states in the perioperative period. Neurol Clin. 2004;22(2):vii–422. https://doi.org/10.1016/j.ncl.2004.01.001.
Vaurio LE, Sands LP, Wang Y, Mullen EA, Leung JM. Postoperative delirium: the importance of pain and pain management. Anesth Analg. 2006;102(4):1267–73. https://doi.org/10.1213/01.ane.0000199156.59226.af.
Ravi B, Pincus D, Choi S, Jenkinson R, Wasserstein DN, Redelmeier DA. Association of duration of surgery with postoperative delirium among patients receiving hip fracture repair. JAMA Netw Open. 2019;2(2):e190111. https://doi.org/10.1001/jamanetworkopen.2019.0111.
Goettel N, Burkhart CS, Rossi A, Cabella BCT, Berres M, Monsch AU, Czosnyka M, Steiner LA. Associations between impaired cerebral blood flow autoregulation, cerebral oxygenation, and biomarkers of brain injury and postoperative cognitive dysfunction in elderly patients after major noncardiac surgery. Anesth Analg. 2017;124(3):934–42. https://doi.org/10.1213/ANE.0000000000001803.
Weinstein SM, Poultsides L, Baaklini LR, Mörwald EE, Cozowicz C, Saleh JN, Arrington MB, Poeran J, Zubizarreta N, Memtsoudis SG. Postoperative delirium in total knee and hip arthroplasty patients: a study of perioperative modifiable risk factors. Br J Anaesth. 2018;120(5):999–1008. https://doi.org/10.1016/j.bja.2017.12.046.
Memtsoudis S, Cozowicz C, Zubizarreta N, Weinstein SM, Liu J, Kim DH, Poultsides L, Berger MM, Mazumdar M, Poeran J. Risk factors for postoperative delirium in patients undergoing lower extremity joint arthroplasty: a retrospective population-based cohort study. Reg Anesth Pain Med. 2019:rapm-2019-100700. https://doi.org/10.1136/rapm-2019-100700.
Praticò C, Quattrone D, Lucanto T, Amato A, Penna O, Roscitano C, Fodale V. Drugs of anesthesia acting on central cholinergic system may cause post-operative cognitive dysfunction and delirium. Med Hypotheses. 2005;65(5):972–82. https://doi.org/10.1016/j.mehy.2005.05.037.
Hole A, Terjesen T, Breivik H. Epidural versus general anaesthesia for total hip arthroplasty in elderly patients. Acta Anaesthesiol Scand. 1980;24(4):279–87. https://doi.org/10.1111/j.1399-6576.1980.tb01549.x.
Acknowledgements
We are thankful for the support of the data analysts from the Department of Orthopedic Surgery, West China Hospital.
Funding
This research was not funded.
Author information
Authors and Affiliations
Contributions
XR provided the ideas of this study. ZC-D and XR collected the data. XR and SY-Y analyzed the data. ZC-D and HD-Y helped with the interpretation of data. The authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by Institutional Review Board of West China Hospital
Competing interests
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Supplement file 1.
PRISMA flow diagram.
Additional file 2: Supplement file 2.
PRISMA checklist.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Rong, X., Ding, Zc., Yu, Hd. et al. Risk factors of postoperative delirium in the knee and hip replacement patients: a systematic review and meta-analysis. J Orthop Surg Res 16, 76 (2021). https://doi.org/10.1186/s13018-020-02127-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13018-020-02127-1