Abstract
Background
Minimally invasive surgical approaches are widely used for total hip arthroplasty (THA). However, potential problems related to a reduced visual field during surgery, such as implant malposition, neurovascular injury, and poor implant fixation, have been reported. In these situations, a shorter stem is easier to insert in the femoral canal. To evaluate the accuracy of shorter stem orientation, we focused on the accuracy of stem orientation especially in short tapered wedge stems and evaluated the contribution factors of stem malalignment during mini-invasive total hip arthroplasty.
Methods
One hundred ten hips that underwent THA with a Summit stem (58 hips) (DePuy, Warsaw, IN) as straight stem and TriLock stem (52 hips) (DePuy) as tapered wedge stem were enrolled in this study. For preoperative and postoperative evaluation, a CT scan of the pelvis and knee joint was obtained and was transferred to 3D template software. We compared the alignment of preoperative plan for stem anteversion/valgus/anterior tilt angles and postoperative stem alignment, and the absolute error was defined as the surgical error. To clarify the factors contributing to the malalignment or surgical error, we evaluated postoperative stem alignment and several associated factors.
Further, we compared the clinical parameters between two types of stems for analysis of the influence of stem type differences.
Results
The mean absolute value of the alignment error (postoperative stem alignment-preoperative planning alignment) was not changed in the short tapered wedge and straight stems. Sex, age at operation, or original canal anteversion did not affect the accuracy of stem alignment. However, high body mass index (BMI) affected the accuracy of stem alignment. Clinical outcomes were not changed by the difference of stem types.
Conclusion
The postoperative alignment of short tapered wedge stem was accurate, same as the straight stem during mini-invasive THA, but we need to pay attention when using this in obese patients.
Similar content being viewed by others
Background
Socket and stem orientation during total hip arthroplasty (THA) are critical factors for achieving an optimal range of motion and joint stability [1-3]. Although stem orientation can be estimated by the surgeon during the operation, the intraoperative estimation of stem alignment was found to have limited accuracy, even when an anatomically shaped cementless stem was used [4].
Classically, templating is performed using a plain anteroposterior (AP) radiograph of the pelvis [5]. However, because of the differences in individual patient anatomy and variations in magnification and projection, important radiographic parameters are not always reliable on plain radiographs. Sariali et al. reported on the high accuracy of hip anatomy restoration performed using a novel 3-dimensional (3D) CT scan-based technique for preoperative planning, and the results were comparable with those of navigation for stem alignment [6]. Even for the postoperative evaluation of implant orientation, the evaluation of stem orientation using CT data is very valuable. We recently showed that the accuracy of stem orientation based on CT-based fluoro-matched navigation can be assessed using postoperative CT data, and the clinical accuracy of CT-based fluoro-matched navigation is adequate for stem alignment orientation [7]. Thus, computer-assisted navigation is an effective tool to obtain precise information about stem orientation. However, the navigation system for THA is not popular worldwide because of its cost. Therefore, the factors contributing to stem alignment should be evaluated.
Minimally invasive surgical approaches are currently used for THA. Mini-incision THA reduced postoperative pain and blood loss, speed recovery, and reduce the hospital stay compared with THA using a standard approach [8]. However, some researchers are concerned that mini-incision THA may introduce new potential problems related to a reduced visual field during surgery, such as implant malposition, neurovascular injury, and poor implant fixation [9,10].
Actually, a shorter and thinner stem is easier to insert into the femoral canal when minimally invasive surgical approaches are used for THA. Therefore, surgical error should be used to evaluate the accuracy of intraoperative estimations especially in the case of shorter stems. In this study, we determined the absolute difference between the stem alignment estimated by surgeons intraoperatively and that measured using postoperative CT and evaluated the contribution factors of stem malalignment during total hip arthroplasty.
Methods
Patients and surgery
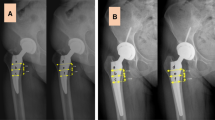
This study analyzed 110 hips in 21 men and 89 women. The patients underwent THA with a Summit stem (58 hips) (DePuy, Warsaw, IN; straight stem) between January 2011 and March 2012 and TriLock stem (52 hips) (DePuy; tapered wedge stem) between April 2012 and December 2013 for osteoarthritis (99 hips, developmental dislocation of the hip (DDH) 71 hips) or idiopathic osteonecrosis of the femoral head (11 hips) (Figure 1a). All surgeries were performed by the anterolateral approach with MIS (OCM approach). Briefly, skin incision was used over the anterior portion of the greater trochanter slightly curved (7 cm). Spread of anterolateral muscular interval without muscle resection, exposure of capsule, and capsular incision were performed. After neck osteotomy, acetabulum preparation and cup implantation were performed. For femoral preparation, leg position was in external rotation, hyperextension, and adduction. Capsular release nearby greater trochanter, stem implantation, repositioning, and wound closure were performed. The mean ages of patients at the time of surgery in the straight and tapered wedge stem groups were 65.2 ± 11.1 and 64.6 ± 9.7 years, respectively. The mean heights of patients in the straight and tapered wedge stem groups were 154.7 ± 8.7 and 154.7 ± 8.1 cm, respectively. The mean weights of patients in the straight and tapered wedge stem groups were 57.4 ± 11.6 and 55.5 ± 11.4 kg, respectively. The mean body mass index (BMIs) of patients in the straight and tapered wedge stem groups were 23.9 ± 3.5 and 23.0 ± 3.1 kg/m2, respectively. There were no significant differences in mean age, height, weight, and BMI between the straight and tapered wedge stem groups (Figure 2a). The proximal femoral shape may be critical for insertion of the stem. Therefore, we classified the cases according to Dorr femoral bone classification. The number of case in each type was similar between the straight and tapered wedge stem groups (Figure 2b).
Materials. (a) Photographs of two different types of stem. Left: Summit stem (straight stem), right: TriLock stem (tapered wedge stem). (b) Postoperative CT data were transferred to the planning module and reconstructed in the axial, frontal, and sagittal planes. The computer-aided design model of the femoral implant was superimposed. The parameters of stem alignment are indicated by red circles.
Preoperative planning and postoperative measurement of stem alignment
For preoperative and postoperative evaluations, a CT scan from the pelvis to the knee joint was performed and transferred to 3D template software (Zed hip, Lexi, Tokyo, Japan). Computer-aided design (CAD) models of the implants were manually adjusted for postoperative multi-planar reconstruction in CT images (Figure 1b). Stem anteversion, valgus, and anterior tilt angles were measured with respect to the mechanical axis of the femur. The mechanical axis was estimated from the center of both epicondyles of the femur and the femoral head. Preoperative planning of the stem alignment for original canal anteversion and zero degree of valgus/anterior tilt was performed preoperatively. Original canal anteversion was defined according to the methods of Sugano et al. [11]. Briefly, the femoral neck axis was calculated as the best-fit line connecting slices drawn through a central segment of the neck. Original canal anteversion was defined as the angle between the axis of the neck and a line connecting the epicondylar line. We compared the preoperative stem anteversion/valgus/anterior tilt angles and postoperative stem alignment, and the absolute error was defined as the surgical error.
Postoperative measurement of clinical results
To analyze the influence of different types of stems on the clinical parameters after THA, we compared the clinical parameters (operation time, blood loss, complications, and Harris hip score at 1 month postoperatively) between the straight stem and tapered wedge stem. The parameter of complications included both intraoperative (fracture and crack) and postoperative (infection, dislocation, and symptmatic embolism) complications.
Statistical analysis
All data are expressed as the mean ± standard deviation (SD) unless otherwise indicated. Statistical analysis was performed by using the Mann-Whitney U test for comparisons of paired samples. Correlations between the postoperative stem alignment error and original canal anteversion, age, height, weight, or BMI were examined by Pearson’s chi-square test. In all cases, p <0.05 was considered significant.
Ethics
The study protocol was approved by the Kobe University Graduate School of Medicine Ethics Committee on 8 September 2011 (No 1220), and all patients provided informed consent.
Results
The postoperative stem alignment of short tapered wedge stem was accurate, same as the straight stem
The mean original canal anteversion values were 28.7 ± 12.1° (straight stem) and 24.4 ± 12.6° (tapered wedge stem) (Figure 3a). The mean stem anteversion values were 26.2 ± 10.1° (straight stem) and 23.5 ± 12.2° (tapered wedge stem) (Figure 3a). There were no significant differences in the anteversion values between the straight and tapered wedge stems (Figure 3a). The mean absolute values of surgical error (postoperative stem anteversion-preoperative planning anteversion) were 6.3 ± 3.3° (straight stem) and 7.5 ± 3.1° (tapered wedge stem) (Figure 3b). The mean absolute values of valgus error were 1.5 ± 1.1° (straight stem) and 1.9 ± 1.5° (tapered wedge stem) (Figure 3c). The mean absolute values of anterior tilt error were 2.6 ± 1.7° (straight stem) and 3.6 ± 1.1° (tapered wedge stem) (Figure 3d). The mean absolute values of anteversion, valgus, or the anterior tilt error (as measured by postoperative stem alignment-preoperative planning alignment) were not significantly changed in the short tapered wedge and straight stems (Figure 3b-d).
Accuracy of stem alignment. (a) Comparisons of the mean values of original canal and stem anteversions in the straight and tapered wedge stem groups. (b-d) Comparisons of absolute mean values of stem orientation errors in the straight and tapered wedge stem groups: (b) anteversion, (c) valgus, and (d) anterior tilt errors.
The accuracy of stem anterior tilt was affected by BMI
To clarify the contributing factors for stem alignment during insertion, we measured the correlation between the surgical alignment error and original canal anteversion, age, height, and BMI. Surgical alignment errors were significantly correlated with the anteversion/valgus error and original canal anteversion in the straight stem, but not in the tapered wedge stem (Figure 4a, b). Age or height was not significantly correlated with surgical error (data not shown). However, there was significant correlation between the anterior tilt error and BMI in both types of stems (Figure 4c, d). These results indicate that obesity affects the accuracy of postoperative stem alignment.
Clinical outcomes were not changed by the difference of stem types
The mean operation times were 92.1 ± 13.5° (straight stem) and 87.8 ± 10.1° (tapered wedge stem). The mean blood loss volumes were 265.3 ± 78.3° (straight stem) and 26.16 ± 102.6° (tapered wedge stem). The mean points of HHS at 1 month post operation were 88.1 ± 10.4° (straight stem) and 90.2 ± 9.0° (tapered wedge stem). There were no significant differences in the clinical results between the straight and tapered wedge stems (Figure 5). We also analyzed about the intraoperative complications (fracture and crack) and postoperative complications (infection, dislocation, and symptomatic embolism). There was no case of infection, dislocation, or symptomatic embolism. However, intraoperative calcar fracture was occurred in one case of tapered wedge stems (Figure 5).
Discussion
The placement of the femoral stem in excessive anteversion or retroversion can result in a significant increase in the incidence of dislocation resulting from an impingement of the neck of the stem by the rim of the acetabular component [12]. Varus-valgus alignment is a critical factor in the use of cementless stems to avoid complications [13,14]. Vresilovic et al. demonstrated that varus alignment correlated with loosening of cementless stems [13], and Gill et al. demonstrated that varus alignment caused periprosthetic femoral insufficiency fractures [14]. Muller et al. showed that stem tilting in the sagittal plane has an influence on the position of the center of the femoral head and thus also on prosthesis anteversion [15]; therefore, the stem alignment of anteversion, varus-valgus, and sagittal tilt should be correctly considered to avoid complications.
Several studies assessing the accuracy of stem orientation during surgery using postoperative CT data have been published [4-16]. Dorr et al. demonstrated an underestimation of 1.5°. Wines and McNicol demonstrated that the difference between the estimated prosthetic and true anteversion was underestimated by 1.1°. Both studies showed that intraoperative estimations were generally accurate with a small difference of 1.0° and 1.5° between intraoperative and postoperative femoral anteversion. However, those series included cases with underestimation and overestimation. The accuracy of stem orientation should be evaluated using absolute values. Hirata et al. demonstrated that the mean absolute value of surgical error was 7.3° [17]. In this study, the mean absolute values of surgical error were 6.3° (straight stem) and 7.5° (tapered wedge stem), which are consistent with the values reported previously [17]. However, the average difference between preoperative planning and postoperative stem anteversion showed 2.5° (straight stem) and 0.9° (tapered wedge stem) underestimation. Hirata et al. demonstrated that the estimated prosthetic anteversion was significantly greater than the original canal anteversion by 5.8° [17]. The discrepancy could be attributed to the surgical approach. Wines et al. demonstrated that the stem anteversion was higher in the posterior approach than in the modified Hardinge approach [4]. The potential risk of posterior dislocation associated with the posterior approach could explain these observations [4]. Therefore, the average difference between the preoperative planning and postoperative stem anteversion was underestimated in both stems.
Schmidutz et al. demonstrated that only 58% of cases of modular short stem were placed in a neutral position (within 3°), whereas 98% of cases of normal length stem were placed in a neutral position [18]. The stem-shaft axis showed a wider range of varus-valgus positions in the short stem group than in the normal length stem group [18]. Kamada et al. reported a similar tendency in the Mayo short stem [19]. In our study, we demonstrated that the mean absolute error was unchanged between the short tapered wedge and straight stems. The width of the frontal plane is designed wider in the short tapered wedge stem than in other types of short stems such as the Mayo short stem. Therefore, the alignment of the short tapered wedge stem was well controlled.
The femoral anteversion of Asians is generally larger than that of Caucasian [20,21]. Dorr et al. reported that the primary indications for THA were primary osteoarthritis in 98 hips (89.9%) and DDH in only 5 hips (4.6%) in their study [16]. In the present study, a higher number of DDH hips (64.5%) were included, and the mean stem anteversion values were 28.7° ± 12.1° (straight stem) and 24.4° ± 12.6° (tapered wedge stem). We demonstrated a significant correlation between the anteversion/valgus error and original canal anteversion in the straight stem, but not in the tapered wedge stem. The length of the straight stem is relatively long, and then, the alignment of stem may be affected by femoral canal shape such as excessive anteversion, whereas the alignment of short tapered stem can be controlled easily by the surgeon during insertion.
Elson et al. demonstrated that the morbidly obesity in patients undergoing THA increases the risk of varus-valgus femoral stem malpositioning [22]. Operating on a patient with a high BMI makes it difficult to identify bony landmarks because of the excess adipose tissue. In the present study, the accuracy of stem anterior tilt during insertion was affected by BMI in the straight and tapered wedge stems. Therefore, BMI might affect stem alignment, although BMI and stem design do not compromise the stem alignment.
Watts et al. demonstrated that the insertion of uniquely exaggerated proximal taper angle stem (ProxiLock) had an increased risk of postoperative periprosthetic femur fracture compared with non-ProxiLock stem group [23]. We also analyzed the influence of different types of stems on the clinical parameters after THA. However, we did not find any differences of clinical outcomes including postoperative periprosthetic femur fracture.
Conclusion
The alignment of the short tapered wedge stem was well controlled. However, high BMI affected the alignment of short tapered wedge stem. We therefore need to pay attention to obese patients when using the short tapered wedge stem during mini-incision THA.
References
Hassan DM, Johnston GH, Dust WN, Watson G, Dolovich AT. Accuracy of intraoperative assessment of acetabular prosthesis placement. J Arthroplasty. 1998;13(1):80–4.
Yoshimine F. The safe-zones for combined cup and neck anteversions that fulfill the essential range of motion and their optimum combination in total hip replacements. J Biomech. 2006;39(7):1315–23.
Barsoum WK, Patterson RW, Higuera C, Klika AK, Krebs VE, Molloy R. A computer model of the position of the combined component in the prevention of impingement in total hip replacement. J Bone Joint Surg (Br). 2007;89(6):839–45.
Wines AP, McNicol D. Computed tomography measurement of the accuracy of component version in total hip arthroplasty. J Arthroplasty. 2006;21(5):696–701.
Chandler RW, Dorr LD, Perry J. The functional cost of dislocation following total hip arthroplasty. Clin Orthop Relat Res. 1982;168:168–72.
Sariali E, Mouttet A, Pasquier G, Durante E, Catone Y. Accuracy of reconstruction of the hip using computerised three-dimensional pre-operative planning and a cementless modular neck. J Bone Joint Surg (Br). 2009;91(3):333–40.
Hayashi S, Nishiyama T, Fujishiro T, Hashimoto S, Kanzaki N, Nishida K, et al. Evaluation of the accuracy of femoral component orientation by the CT-based fluoro-matched navigation system. Int Orthop. 2013;37(6):1063–8.
Mayr E, Nogler M, Benedetti MG, Kessler O, Reinthaler A, Krismer M, et al. A prospective randomized assessment of earlier functional recovery in THA patients treated by minimally invasive direct anterior approach: a gait analysis study. Clin Biomech. 2009;24(10):812–8.
Woolson ST, Mow CS, Syquia JF, Lannin JV, Schurman DJ. Comparison of primary total hip replacements performed with a standard incision or a mini-incision. J Bone Joint Surg Am. 2004;86-A(7):1353–8.
Teet JS, Skinner HB, Khoury L. The effect of the “mini” incision in total hip arthroplasty on component position. J Arthroplasty. 2006;21(4):503–7.
Sugano N, Noble PC, Kamaric E, Salama JK, Ochi T, Tullos HS. The morphology of the femur in developmental dysplasia of the hip. J Bone Joint Surg (Br). 1998;80(4):711–9.
Herrlin K, Pettersson H, Selvik G, Lidgren L. Femoral anteversion and restricted range of motion in total hip prostheses. Acta Radiol. 1988;29(5):551–3.
Vresilovic EJ, Hozack WJ, Rothman RH. Radiographic assessment of cementless femoral components: correlation with intraoperative mechanical stability. J Arthroplasty. 1994;9(2):137–41.
Gill TJ, Sledge JB, Orler R, Ganz R. Lateral insufficiency fractures of the femur caused by osteopenia and varus angulation: a complication of total hip arthroplasty. J Arthroplasty. 1999;14(8):982–7.
Müller M, Crucius D, Perka C, Tohtz S. The association between the sagittal femoral stem alignment and the resulting femoral head centre in total hip arthroplasty. Int Orthop. 2011;35(7):981–7.
Dorr LD, Wan Z, Malik A, Zhu J, Dastane M, Deshmane P. A comparison of surgeon estimation and computed tomographic measurement of femoral component anteversion in cementless total hip arthroplasty. J Bone Joint Surg Am. 2009;91(11):2598–604.
Hirata M, Nakashima Y, Ohishi M, Hamai S, Hara D, Iwamoto Y. Surgeon error in performing intraoperative estimation of stem anteversion in cementless total hip arthroplasty. J Arthroplasty. 2013;28(9):1648–53.
Schmidutz F, Beirer M, Weber P, Mazoochian F, Fottner A, Jansson V. Biomechanical reconstruction of the hip: comparison between modular short-stem hip arthroplasty and conventional total hip arthroplasty. Int Orthop. 2012;36(7):1341–7.
Kamada S, Naito M, Nakamura Y, Kiyama T. Hip abductor muscle strength after total hip arthroplasty with short stems. Arch Orthop Trauma Surg. 2011;131(12):1723–9.
Sugano N, Noble PC, Kamaric E. A comparison of alternative methods of measuring femoral anteversion. J Comput Assist Tomogr. 1998;22(4):610–4.
Khang G, Choi K, Kim CS, Yang JS, Bae TS. A study of Korean femoral geometry. Clin Orthop Relat Res. 2003;406:116–22.
Elson LC, Barr CJ, Chandran SE, Hansen VJ, Malchau H, Kwon YM. Are morbidly obese patients undergoing total hip arthroplasty at an increased risk for component malpositioning? J Arthroplasty. 2013;28(8 Suppl):41–4.
Watts CD, Abdel MP, Lewallen DG, Berry DJ, Hanssen AD. Increased risk of periprosthetic femur fractures associated with a unique cementless stem design. Clin Orthop Relat Res. 2014
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
SHy created the study design. SH, TF, SHs, and NK participated in the data collection. SH and TF participated in the data interpretation. SH was responsible for the statics and drafting the article. RK made the critical review. MK made the final approval. All authors read and approved the final manuscript.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Hayashi, S., Fujishiro, T., Hashimoto, S. et al. The contributing factors of tapered wedge stem alignment during mini-invasive total hip arthroplasty. J Orthop Surg Res 10, 52 (2015). https://doi.org/10.1186/s13018-015-0192-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13018-015-0192-x