Abstract
Enhanced perioperative care protocols become the standard of care in elective surgery with a significant improvement in patients’ outcome. The key element of the enhanced perioperative care protocol is the multimodal and interdisciplinary approach targeted to the patient, focused on a holistic approach to reduce surgical stress and improve perioperative recovery. Enhanced perioperative care in emergency general surgery is still a debated topic with little evidence available. The present position paper illustrates the existing evidence about perioperative care in emergency surgery patients with a focus on each perioperative intervention in the preoperative, intraoperative and postoperative phase. For each item was proposed and approved a statement by the WSES collaborative group.
Similar content being viewed by others
Introduction
Enhanced recovery after surgery (ERAS®) protocol refers to a standardized multimodal approach based on the application of structured protocols in perioperative patients' management. The main goal of these interventions is patient management optimization during the perioperative period under all aspects of perioperative care, not only about the surgical technique, by reducing surgical stress, minimizing the physiological response to surgery, and improving postoperative recovery. The key element of the ERAS protocol is the multimodal and interdisciplinary approach targeted to the patient, focused on a holistic approach [1].
Perioperative care protocols are structured as a bundle of interventions to be applied during the preoperative, intraoperative and postoperative periods. Each intervention is linked to the others and shares the common goal of reducing the burden of perioperative patient stress (Fig. 1). For this reason, it is very difficult to evaluate the efficacy of a single item without considering the effect of all the others, applied as a bundle. Designing studies to evaluate and demonstrate the effect of every single intervention is therefore a major challenge, markedly limiting the available scientific evidence.
The effectiveness and safety of ERAS protocols in elective surgery are now widely established. Several meta-analyses comparing standard care and fast-track approach show that ERAS protocols in elective surgery lead to a reduction in length of stay and in the rate of postoperative non-surgical complications [2,3,4,5]. Most of the available studies focused on the postoperative phase, considering the main “surgical” items as study outcomes, with relatively small attention being devoted to preoperative and intraoperative interventions. However, main postoperative items such as oral feeding, urinary drain removal and mobilization should also be considered as compliance indicators rather than only interventions to be implemented [6]. From a methodological standpoint, there is a clear difference between adherence and compliance to an enhanced recovery protocol. Adherence should identify the percentage of items applied throughout the perioperative care process, while postoperative compliance also reflects how the patient follows the enhanced recovery process. For example, patients’ compliance to a postoperative pathway including early oral feeding and mobilization can be obtained easier if there is good adherence to a preoperative and an intraoperative enhanced pathway (and not only for a medical decision).
Based on the beneficial effect of enhanced perioperative care protocols in elective surgery, the implementation of structured protocols for emergency general surgery patients has also been advocated after the promising results of some studies [7, 8]. However, enhanced perioperative care in emergency general surgery remains a “grey area” with little evidence available and great debate.
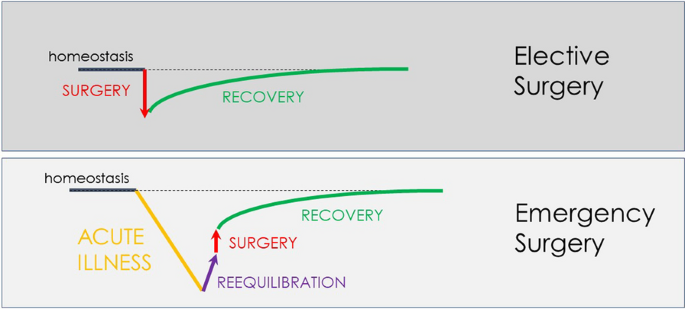
Patients undergoing elective surgery should be normothermic, euvolemic, clean, and “healthy”, and surgery per se represents their main stressful factor. Emergency surgery represents a more complex scenario where surgery is at the same time a stressful factor but also the key-intervention to solve the pre-existing physiologic imbalance secondary to the acute underlying disease (Fig. 2).
The diagram (Fig. 2) shows the impact of the pre-existing acute disorder causing a marked decline of the physiological reserve. The importance of the preoperative phase (re-equilibration) seems intuitive. Despite emergency surgery by definition does not allow schedulable interventions, some preoperative optimization is still possible in the emergency setting, though with much reduced time. The time available between patient presentation and surgery should be optimized to improve the patient’s physiological status to promote post-surgical recovery. In this complex scenario, also the timing of surgery should be carefully evaluated. One of the most intriguing and difficult challenges is to identify the right balance between hastening surgery to directly "face" the acute disease and delaying surgery in trying to improve the patient's condition.
Evidence supporting enhanced perioperative care in emergency general surgery.
Currently, available studies about enhanced perioperative care in emergency general surgery are few, sparse and very heterogeneous. In addition, the perioperative care protocol derived from the elective ERAS protocol but with several and substantial differences [9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28]. Tables 1 and 2 show in detail the protocols adopted in the evaluated studies. A single perioperative care protocol cannot be identified through the existing literature, and each study applied different interventions.
Huddart et al. demonstrated that the introduction of a bundle evidence care protocol decreased mortality among patients undergoing emergency laparotomy, with a reduction in delayed diagnosis, increased implementation of goal-directed fluid therapy, and improved restoration of biochemical homeostasis [29]. The bundle protocol consisted in an accurate preoperative assessment with early warning score, early broad-spectrum antibiotics, prompt resuscitation using goal-directed techniques and postoperative ICU admission for all high-risk patients.
Tandberg and colleagues introduced a standardized perioperative care protocol in patients undergoing high-risk emergency abdominal surgery [9]. The study protocol included consultant-led attention and care, early resuscitation and high-dose antibiotics, surgery within 6 h, perioperative stroke volume-guided volume status optimization, standardized analgesic treatment, early mobilization and early oral feeding. Compared with a historical cohort from the same department, the introduction of the protocol lead to a significant reduction in mortality from 21.8 to 15.5%.
An Italian observational multicentric study demonstrated that adherence to the intraoperative protocol items was low. Major determinants of postoperative compliance were minimally invasive surgery and low intraoperative fluid infusions [22].
Several other studies investigated the introduction of enhanced perioperative care protocols in emergency general surgery [10, 12, 14,15,16,17,18,19,20, 22, 23, 27]. Each study applied a different protocol in different subsets of patients with contrasting results. Some studies adopted a modified ERAS protocol in patients with obstructive colorectal cancer [13, 14, 16, 19], others on patients with perforated peptic ulcer [10, 15, 17], others on major emergency laparotomy and trauma [12, 18, 20, 22]. Most of the published enhanced recovery programs in emergency surgery focus on the intra- and postoperative phases of the program, reporting no substantial differences in the preoperative care of patients enrolled in ERAS protocols versus standard “not-ERAS” patients. The majority of the existing studies did not report results on adherence to the protocol items; moreover, also data on compliance to the postoperative pathway were lacking.
The results of some of these studies were included in a meta-analysis published by Hajibandeh et al. published in 2020 [30]. Despite the great heterogeneity and the poor quality of the evidence, the results showed a reduction in length of stay, pulmonary complications, postoperative ileus and wound infections. No differences were observed in 30-day rehospitalization and 30-day mortality rates.
Despite the promising results, the implementation of an enhanced perioperative care protocol in emergency general surgery may encounter several obstacles. Patients receiving urgent care typically present to medical teams with a complex situation: their conditions at the time of admission are not optimal and they have extremely heterogeneous characteristics [31, 32]. The acute illness often leads to several physiological derangements secondary to fasting, vomiting, dehydration, augmented capillary permeability, and metabolic imbalance.
Columbus et al. [33] have identified two main critical issues concerning the urgent care field: the diversification of patients and the wide range of possible settings and operative contexts (including the hospital organization and the medical team management). Therefore, efforts should focus on improving the structural and organizational aspects. Dedicated medical personnel training and a widespread standardization of the diagnostic and therapeutic process may improve medical performance and, ultimately, the clinical outcome. A recent study demonstrated that the familiarity between surgeon and anesthetist used to work together improve patients’ outcome [34]. Unfortunately, emergency general surgery is rarely managed by a dedicated staff. Emergency care requires a higher number of specialists and personnel turnover and, therefore, it would lead to wider cross-collaborations and variability in staff composition. In addition, patients undergoing emergency surgery are rarely managed by enhanced recovery-trained anesthetists, surgeons and nurses (working in abdominal surgery), making the development of new treatment protocols very difficult.
The availability of resources is another central tenant to the safe and optimal delivery of surgical care in the emergency setting. For example, laparoscopic facilities or advanced hemodynamic monitoring systems are not universally available, and reported unavailable by some authors, due to logistical issues, timing of surgical interventions (e.g., in office hours vs. after hours), and higher costs [18, 35].
Methods
The WSES panel promoted the development of this position paper. The work process consisted of two different phases. The first phase was a review of the existing literature about enhanced recovery protocol in emergency general surgery. The second phase was the identification of enhanced recovery protocol items and the development of position statements for each perioperative intervention. This position paper was written according to the WSES methodology [36]. All the statements contained the level of evidence (LoE) available about the topic, graded according to the GRADE methodology. The consensus on the position paper statements was assessed through a web survey (by Google Form) open to all the members of the steering committee and the experts’ panel, as well as the board of governor members of the WSES. The consensus was reached if a statement was associated with ≥ 70% of the agreement. Otherwise, the statement was re-discussed by email or videoconference, modified, and resubmitted to the experts’ vote until consensus was reached. Table 3 summarizes approved statements.
Preoperative interventions
Education and counseling
Patient counseling and education should be encouraged and implemented to explain perioperative risks and post-operative pathway (LoE D)
Relieving patient anxiety through preoperative counseling is of utmost importance, especially in an emergent situation. Full preoperative counseling, which is known to reduce post-operative stress, pain and anxiety, may not be possible in the emergency setting. Nevertheless, information such as details of the procedure, possible perioperative complications, the need for the creation of a stoma and length of hospitalization should be communicated with patients and their families before the procedure [30, 37]. A recent meta-analysis focusing on the implementation of enhanced recovery protocols in emergency abdominal surgery reported that adapted preoperative counseling was carried out in all of the six included studies. No data about adherence to this counseling were reported [30]. Depending on the urgency of surgery, preoperative education/counseling may not be possible. However, a recently published multidisciplinary experience reported very high compliance (more than 90% 1 year after implementation) with items such as standardized preoperative patient information and bilateral ostomy marking in patients undergoing emergency general surgery [11, 38]. In the case of stoma creation, the implementation of patient education reduced stoma complications and improved postoperative quality of life, reducing the average hospital stay [39]. However, although it seems feasible and of some utility to appropriately counsel patients before emergency procedures, evidence in support of this hypothesis has not been produced yet and the degree of benefit in terms of postoperative recovery has not been measured.
Fluid balance and volemic status
Volemic status should be evaluated and corrected with goal-directed fluid therapy as soon as possible in the pre-operative phase (LoE B)
The majority of emergency general surgery patients present with fluid derangements, mostly related to acute illness, underlying sepsis, prolonged fasting and vomiting. In this setting, preoperative evaluation of the patient should focus on the volemic assessment to rapidly correct alterations in patients' homeostasis, including stress response, gut dysfunction, insulin resistance, electrolyte imbalances, fluid shifts, SIRS and sepsis with varying degrees of organ dysfunction. Although complete optimization of medical conditions cannot be fully achieved in the emergency setting, adequate intravenous fluid resuscitation in emergency general surgery is crucial and feasible, and it should be attempted in all patients. A prospective randomized trial demonstrated better postoperative outcomes when patients were preoperatively managed with a fixed protocol to reach homeostasis [40]. The adopted protocol defined three targets for the goal-directed crystalloid resuscitation: central venous pressure of 8–12 cmH2O, mean arterial pressure > 65 mmHg and urinary output > 0.5 mL/Kg/h. The initial resuscitation should be titrated to the clinical response, such as fluid responsiveness, and not solely guided by a predetermined protocol, with particular attention to the underlying disease. Despite restoring homeostasis should be considered a goal, surgical treatment should not be delayed. According to the indications from the 2016 Surviving Sepsis Guidelines, resuscitation from sepsis-induced hypoperfusion should require at least 30 ml/kg of intravenous crystalloid fluids within the first 3 h [41]. However, in the updated 2021 version of the Guidelines, the strength of this recommendation was downgraded from “strong” to “weak” (quality of evidence: low) and the recommendation was modified in a suggestion [42]. Massive fluid therapy has been challenged in the enhanced recovery approach [9]. Fluid overload should be avoided since it is associated with higher rates of respiratory complications (i.e., pneumonia, pleural effusion, and respiratory failure) and secondary anastomotic leaks. Early, i.e., preoperative, goal-directed fluid therapy in sepsis was the treatment of the experimental arm in a randomized clinical trial enrolling septic patients published in 2001 [43]. Excluding patients who needed immediate surgery from the trial, in-hospital mortality was 30.5% in the group assigned to early goal-directed therapy, as compared with 46.5% in the group assigned to standard therapy (P = 0.009). Tendberg et al. developed a perioperative protocol for emergency high-risk abdominal surgery in which stroke volume-guided hemodynamic optimization before surgery was a key element. The study has shown a significant reduction in mortality as well as postoperative length of ICU stay after the introduction of the standardized protocol [9]. Therefore, patients should be carefully evaluated and goal-directed fluid resuscitation should be implemented as soon as possible.
Metabolic balance
Glycemic control should be implemented in all emergency surgery patients to prevent both hypo- and hyperglycemia (LoE C)
Perioperative hyperglycemia has been demonstrated to be associated with adverse clinical outcomes [44]. The correction of hyperglycemia with insulin administration and the management of glycemia with the implementation of glycaemic control protocols have been shown to reduce hospital complications and decreases mortality in elective general surgery patients [45]. Pre-existing diabetes mellitus, acute illness and physiologic changes accompanying a surgical procedure contribute to the worsening of glycemic control. The resulting hyperglycemia due to an abnormal glucose balance is a risk factor for postoperative complications that include poor wound healing and postoperative infections as well as an increase in morbidity, mortality, intensive care unit admission, and hospital length of stay [46]. Preoperative hyperglycemia has been demonstrated to have a role in postoperative compliance to an enhanced recovery pathway also in emergency surgery patients [22]. However, in emergency general surgery and in critically ill patients the role of hyperglycemia is more debated and less certain. Hyperglycemia could be considered a marker of organ failure and disease severity. A recent network meta-analysis comparing four different target blood glucose concentrations (< 110, 110–144, 144–180, and > 180 mg/dL) in terms of the benefit and risk of insulin therapy found no significant difference in the risk of mortality and infection among four target blood glucose ranges in critically ill patients, but indicated that target blood glucose levels of below 144 mg/dL were associated with a higher risk of hypoglycemia [47]. Although a proactive approach to avoid both hyper- and hypoglycemia should be suggested in emergency patients, close glycemic control is advisable and Institutions should develop their own protocols to treat both hyper and hypoglycemia in critically ill patients.
Intraoperative interventions
Postoperative nausea and vomiting (PONV) prevention
PONV prevention with a multimodal approach in an emergency setting should be implemented (LoE D)
Prevention of PONV in elective general surgery has become a key element of enhanced recovery protocols [48]. PONV is very common after general anesthesia and it may negatively impact recovery and short-term outcomes [49]. Several factors are linked to the occurrence of PONV; however, its exact pathophysiology is still unclear [50]. Some risk factors are patient-related such as advanced age, female gender, non-smoking status, pain, and anxiety. Other risk factors are related to the type of operative gastro-intestinal manipulation and vagal stimulation, anesthetics, and opioids [50,51,52]. Few data are available on emergency patients who frequently complain of nausea and vomiting before surgery in association with anxiety and pain. Several studies investigated the role of different drugs to prevent PONV. The commonest antiemetic drugs are dopamine and serotonin antagonists (e.g., ondansetron) and corticosteroids (e.g., dexamethasone) [53,54,55,56]. Pre-emptive anesthesia was associated with better pain control and reduction in PONV [57, 58].
Other suggested interventions are opioid-sparing anesthesia and avoidance of volatile anesthetics. Unfortunately, the vast majority of evidence is based on elective surgery and very few data are available on emergency general surgery. The emergency setting is associated with more fear, anxiety, pain and, probably, nausea even before surgery. Nevertheless, prevention of PONV should be implemented also in emergency general surgery. Among the interventions suggested, there are opioid-sparing anesthesia, avoidance of volatile anesthetics and a multimodal approach to pharmacological prevention.
Anesthesia and analgesia
General anesthesia warrants proper analgesia, amnesia and muscle relaxation. The ideal general anesthesia protocol should target all these goals, but it should also reduce the need for intraoperative fluids, reduce post-operative residual effects, such as PONV and delirium and it should permit rapid awakening. Several interventions have been implemented to optimize the intraoperative management of the patient. Whether anesthesia should be maintained by a totally intravenous approach or with inhalation drugs still remains uncertain and no recommendations can be made [59]
Benzodiazepines
Benzodiazepines should be avoided in the emergency anesthetic protocol, in particular in older patients, to reduce delirium risk in the postoperative period (LoE C)
The incidence of delirium in the postoperative period has an important impact on clinical outcomes including higher mortality, functional decline, prolonged hospitalizations and risk for institutionalization [60]. Upon the several risk factors for development, that include acute illness and pain management, medications adopted also for general anesthesia play an important role [61]. For these reasons, anesthetic protocols should focus on reducing the use of these medications. Benzodiazepines have been linked with the development of delirium in the postoperative period, with a marked effect in elderly and frail patients [62, 63]. Despite the potential beneficial effects in treating preoperative anxiety, these drugs should be avoided.
Opioids
Opioid use should be limited to short-acting drugs in the perioperative period (LoE D)
Opioids are related to several adverse effects such as nausea, vomiting, respiratory depression, sedation and postoperative ileus. Despite their important role in pain management, the undesired effects may impact negatively on patients' recovery. Some experiences exist about opioid-free anesthesia, with the claim of more patient safety [64]. For this reason, opioids use should be limited to short-acting drugs avoiding morphine to minimize residual effects and to warrant rapid recovery [65].
Anesthesia depth monitoring
Anesthesia depth monitoring should be implemented in the emergency setting, to minimize anesthesia side effects such intra-operative hypotension, increased need for fluids and postoperative delirium (LoE C)
To reduce all the detrimental effects of general anesthetics, such as cognitive effects and vasoactive depressing activity, titrating the minimal needed drug dose guided by the depth of anesthesia monitoring has been recommended. Monitoring of anesthesia depth could be guided by the bispectral index (BIS) or other techniques based on electrical brain activity (EEG). Anesthesia depth monitoring has been demonstrated to be associated with a lower incidence of postoperative delirium and with decreased morbidity [66,67,68]. Moreover, depth monitoring has been demonstrated to be associated also with a higher intraoperative mean arterial pressure, possibly reducing the need for fluid administration to maintain adequate systemic perfusion [69].
Neuromuscular blockade monitoring
Neuromuscular blockade monitoring should be implemented to reduce post-operative morbidity (LoE C)
Neuromuscular blockade is needed during abdominal surgery to improve surgical exposure. A post-operative residual neuromuscular block is a risk factor for morbidity and mortality, conditioning weakness of airway muscles, airway obstruction and aspiration with consequent increased postoperative pulmonary complications [70]. Residual neuromuscular block has been reported in up to 40% of patients treated with neuromuscular blocking agents [71]. Adopting strategies such as the qualitative monitoring of the peripheral muscular blockade as the train of four (TOF) has been demonstrated to significantly reduce the residual blockade at the end of anesthesia [72]. Monitoring of the neuromuscular blockade is therefore recommended to avoid potential side effects.
Multimodal pain control
Multimodal analgesia, with a combination of systemic and loco-regional approaches, should be encouraged in the emergency setting to improve pain control and reduce the need for analgesics and opioids (LoE C)
Pain is one of the limitations to patient recovery after surgery. Standard general anesthesia warrants analgesia during surgery, but has no effect on pain control after surgery, requiring drug administration with possible detrimental effects such as opioids. Multimodal analgesia has been proposed to manage pain with several different treatments reducing the need for systemic opioids and avoiding their potential side effects [73]. The association of general and locoregional analgesia has been demonstrated also to reduce the incidence of postoperative delirium [74].
Thoracic epidural analgesia (TEA) has been demonstrated to be superior to systemic opioids in pain management in open elective abdominal surgery [75]. A recent Scandinavian population study reported that epidural analgesia was adopted in emergency general surgery in less than one third of patients; epidural analgesia was associated with lower 90-day mortality probably due to a reduction in paralytic ileus and pain that most likely allowed an early mobilization and coughing [76]. TEA was included in an emergency general surgery enhanced recovery protocol that demonstrated a significant reduction in mortality, despite the adherence to this specific item was not reported [9]. Spinal analgesia has been proposed as an alternative to epidural analgesia in patients treated with minimally invasive colorectal surgery: the administration of long-acting local anesthetics and opioids warrant pain control in the first postoperative hours allowing early mobilization. Moreover, it has been associated with a lower risk of hypotension and fluid overload [77]. However, spinal and epidural anesthesia should be considered with caution in septic patients.
Surgical incision is one of the main responsible of postoperative pain. To manage this pain, abdominal wall blockade such as the Transversus abdominis plane (TAP) block has been proposed. The adjunct of abdominal wall blocks to general anesthesia has been demonstrated to have beneficial effects on pain control during the first 24 h and to allow faster recovery and better hemodynamic control in elective abdominal surgery [78,79,80,81]. Of note, the TAP block can be performed both ultrasound-guided and laparoscopy-guided [82]. Currently, no studies focus on the performance of the TAP block in emergency general surgery. However, abdominal wall blocks should be considered in a multimodal analgesic approach.
Active warming
Active warming and body temperature monitoring should be encouraged in the emergency setting to reduce postoperative morbidity (LoE C)
Body temperature plays an important role in several pathophysiologic mechanisms Hypothermia typically occurs during general and locoregional anesthesia due to vasodilatation and a rapid redistribution of heat from the core to peripheral districts. Moreover, several anesthetic drugs impair thermoregulatory control, further contributing to the maintenance of hypothermia. Finally, the development of hypothermia is facilitated by direct heat loss deriving from the surgical exposure of the abdominal cavity and by the low operating theater temperature. Importantly, perioperative hypothermia implicates an increased risk of surgical site infection, morbidity and mortality. Moreover, hypothermia may alter drug metabolism and it is also associated with an increased risk for coagulopathy and a consequent increased blood loss [83]. Body temperature monitoring is therefore mandatory and allows temperature correction with active warming. Active warming, ideally starting before the entrance to the operating room, has been recognized as one of the core items of the enhanced recovery pathway and its implementation significantly reduced postoperative morbidity [84, 85].
Fluid management
Fluids should be managed within a goal-directed fluid therapy strategy to target the amount of given fluids on patient needs (LoE C)
General anesthetics lead to dose-depend myocardial depression and systemic vasodilatation. The associated increased venous capacitance leads to a relative hypovolemia that, along with myocardial depression, might lead to hypotension, and organ hypoperfusion with the related consequences. Therefore, during surgery, fluids are frequently administered to maintain an adequate intravascular volume status and systemic perfusion. However, both hypovolemia and hypervolemia are associated with postoperative morbidity and several studies demonstrated the J-shaped relation between intraoperative fluids administered and postoperative morbidity [86,87,88]. Intraoperative fluid management should therefore be balanced, giving the needed amounts of fluids to warrant euvolemia and systemic perfusion, but avoiding fluid overload [89, 90]. Fluid overload is associated with several detrimental effects related to tissue edema. Increased interstitial fluids might impair gas exchange with consequent respiratory failure and foster the development of pneumonia. Moreover, fluid overload is associated with bowel edema and postoperative ileus, conditioning a delayed recovery of GI function [91]. For these reasons in elective surgery, a restrictive fluid strategy has been proposed, with the target of a near-zero fluid balance during surgery and a limited amount of fluids given (generally around 3 mL/Kg/h) [92]. This approach is valid under the condition that patients arrive at the surgery in perfect homeostasis without fluid derangements.
Several factors may worsen and make fluid management in emergency surgery patients more difficult. Increased vascular permeability related to acute illness, preoperative fasting, preoperative dehydration and blood loss may dramatically increase the need for intraoperative fluids compared to elective surgical patients. In this complex scenario, goal-directed fluid therapy has been proposed to titrate and balance the amount of fluids. Fluid therapy should be guided by hemodynamic monitoring systems, ideally capable of monitoring dynamic parameters, such as cardiac output, stroke volume variation, pulse pressure variation and stroke volume variation [93, 94]. The implementation of an intraoperative goal-directed fluid strategy, associated with restrictive fluid regimens and the early adoption of vasopressors to maintain adequate circulating volumes has been demonstrated to significantly reduce perioperative morbidity [94]. While only few studies exist on fluid management during general emergency surgery, available evidence derived from elective surgery and current pathophysiological understanding strongly underlines the importance of reasoned fluid management during emergency surgery. In the emergency setting, a recent study highlighted the importance of fluid therapy, with a negative correlation between increasing intraoperative fluids given and patients' recovery [22].
Minimally invasive surgery
Minimally invasive surgery approach in emergency surgery should be encouraged whenever possible and needed skills are available (LoE C)
Reducing surgical stress is the cornerstone of an enhanced perioperative care protocol. The use of minimally invasive surgery in elective major surgery has been demonstrated to reduce inflammation, improve pulmonary function, and facilitate GI function with a consequent reduction in morbidity and length of stay [95,96,97]. Minimally invasive surgery, even within an enhanced recovery pathway, has been associated with a faster recovery when compared with open surgery [98]. In emergency major abdominal surgery, such as repair for perforated peptic ulcer and colorectal surgery invasive minimally techniques have been associated with better clinical outcomes with a lower mortality and length of stay [99,100,101]. A population study on the commonest abdominal surgical emergencies in the USA demonstrated an increasing trend of a laparoscopic approach. Minimally invasive surgery was associated with lower mortality, surgical site infection rate and length of stay. However, minimally invasive surgery in major interventions such as peptic ulcer repair and small bowel obstruction was adopted in less than 40% and 10%, respectively [102]. Data from the national emergency laparotomy audit (NELA) from the U.K. demonstrated that laparoscopy is adopted in less than 20% of major surgeries [99]. Existing data demonstrated the beneficial effect of minimally invasive surgery but also its poor diffusion among surgeons with several difficulties [103]. A recent prospective study identified minimally invasive surgery as the major determinant of postoperative compliance to an enhanced recovery protocol [22]. Efforts should be made to implement laparoscopy in emergency general surgery daily practice.
Drains
Abdominal drains should be placed for limited indications, including in the presence of gross bacterial contamination and inadequate source control (LoE D)
The routine positioning of a peritoneal drain after elective major colorectal surgery has been demonstrated to be ineffective in preventing surgical complications and is not recommended [104]. Moreover, the presence of a drain has been identified as one of the main failure predictors of an enhanced recovery pathway, both in elective and emergency surgery [22, 105]. Drain in emergency general surgery is justified by a clear rationale, in case of contaminated surgical field and intra-abdominal infections. Few experiences exist about avoiding drains in emergency general surgery: some studies focused on the introduction of enhanced perioperative care protocol on colorectal emergencies (obstructions) demonstrated better results avoiding the drain (along with other interventions) [13, 14, 16]; other studies demonstrated the safety of an early removal in perforated peptic ulcer and trauma [15, 20]. Evidence quality is very low to recommend avoiding abdominal drains, but we believe drains should be placed only in case of gross abdominal contamination and high risk for collection and abdominal abscess.
Postoperative care
Analgesia
Multimodal analgesia, using different classes of analgesics and avoiding long-acting opioids, should be recommended in the postoperative phase (LoE C)
Proper analgesia and pain control are key elements of a patient’s recovery after surgery. The control of pain in the postoperative period is the result of many several factors related to patients' characteristics, invasiveness of surgical intervention, the underlying diagnosis and adopted intra- and post-operative analgesia techniques. Perioperative management should be focused on maximizing the effect of pain control and avoiding the side effects of drugs. The use of long-acting opioids, such as morphine, should be ideally avoided also in the postoperative period. Indeed, avoiding opioids has been demonstrated to facilitate mobilization and to fasten GI function recovery [65]. The treatment of pain should be multimodal and tailored to patients’ conditions, according to available skills [106].
Early nasogastric tube removal
The nasogastric tube should be removed as soon as possible, even at the end of surgery (LoE D)
According to a reactive policy, the nasogastric tube (NGT) was traditionally removed after GI function recovery to prevent PONV and inhalation. Enhanced recovery protocols recommend the removal of NGT at the end of elective surgery. This practice reduced pulmonary complications and promoted GI function recovery [107]. Preliminary studies carried out in patients with obstructive colorectal cancer or perforated peptic ulcer reported a high patient compliance to NGT removal at the end of surgery [17, 19, 108]. Other studies suggested removing the NGT when the output was less than 300 ml [15, 18]. When patients are managed according to enhanced recovery protocols, the early removal of NGT is safe and should be implemented in clinical practice.
Early mobilization
Early mobilization should be encouraged and stimulated as soon as possible to reduce post-operative morbidity (LoE C)
Prolonged immobilization is associated with insulin resistance, thromboembolic events and respiratory complications [109]. Several studies reported that early mobilization after surgery reduced overall morbidity and shortened the length of hospital stay [110,111,112,113]. Several factors can negatively impact on patient’s mobilization such as abdominal drain, urinary catheter, suboptimal pain control, prolonged i.v fluids, and patient's motivation. In emergency surgery, different protocols have been proposed targeting mobilization the same day of surgery [15, 18] or on postoperative day 1 [14, 16, 19]. According to existing evidence, patient mobilization should be encouraged as early as possible, along with all the interventions that could facilitate it, such as proper pain control, and the early removal of urinary catheter and drains.
Nutrition and early oral feeding
Early oral feeding should be encouraged and promoted as soon as tolerated by patients (LoE C)
The close relationship between preoperative nutritional status and surgical outcomes has been extensively reported in elective surgery, where tailored nutritional and prehabilitation programs can be planned before the operation [114]. Postoperative fasting has been demonstrated to be harmful in elective surgery with delayed recovery and increased complications[2, 115, 116]. Oral feeding can be resumed early after surgery regardless of bowel canalization, whether removal of the nasogastric tube, PONV prophylaxis, near zero fluid balance, early mobilization, and pain control have been carried out according to enhanced recovery protocol. Patients undergoing emergency surgery often have an altered metabolic status, with dehydration and several derangements such as prolonged fasting, vomiting, impairment of GI function, and fluid loss related to the acute illness. The great condition's heterogeneity in emergency surgery patients makes quite impossible to standardize the timing of oral feeding recovery. However, studies carried out in patients with perforated peptic ulcer or obstructive colorectal cancer demonstrated both feasibility and safety of early oral feeding [19, 20, 117]. Perioperative nutritional intervention should be therefore tailored to the patient's conditions adopting as the target the earliest possible recovery.
Urinary catheter removal
Urinary catheter should be removed as soon as possible when urinary output no longer needs to be monitored (LoE C)
Urinary output monitoring is a key element to assess patients' volemic status and to guide goal-directed fluid therapy. In emergency surgery patients, the urine output target should be 0.5 ml/Kg/h. Different policies about the timing of catheter removal have been proposed: immediately after surgery in a randomized study on perforated peptic ulcer patients [17], on postoperative day 1 [19, 20] or according to urinary output (> 1 ml/Kg/h) [15, 18]. Regardless, the urinary catheter should be removed as early as possible after reaching the minimum urinary output target to facilitate mobilization and reduce infections.
Postoperative fluids
Postoperative intravenous fluids should be minimized and maintained until oral fluid intake is adequate (LoE C)
Fluid therapy should be targeted to restore the euvolemic status and to maintain adequate hydration and tissue perfusion until the oral intake can be restarted. As reported for operative management, fluid therapy can be harmful if too many or too few fluids are given [86,87,88]. Following elective colorectal surgery i.v. fluids should be stopped on postoperative day one. Studies performed on emergency surgery patients did not report on timing to stop i.v fluids; however, infusions should be tailored to patient conditions, giving the minimum fluid amount to restore and maintain euvolemia and to obtain adequate perfusion.
Antibiotic therapy
Antibiotic therapy should not be continued in case of non-complicated intra-abdominal infections, while a short course antibiotic therapy is indicated in case of complicated infection (LoE A).
A large part of emergency patients undergo surgery for intra-abdominal infections; therefore, antibiotic therapy is a cornerstone of treatment along with surgical source control. The need for antibiotics during the postoperative period may contribute to delaying patient recovery, as an obstacle to active mobilization and i.v. infusions suspension; moreover, prolonged antibiotic therapies may have a role in delaying home return. Postoperative antibiotic therapy should be reserved for patients with complicated intra-abdominal infections. In these patients, a short therapy (3–5 days) after adequate surgical source control is not inferior when compared to longer therapy [118,119,120]. In non-complicated infections, antibiotic therapy should be stopped at the end of surgery if the source control is adequate.
The majority of patients presenting with a severe infection who initially require IV therapy can be switched to oral therapy after 24–48 h provided that they are improving clinically and can tolerate an oral formulation. The switch from IV to oral route should be encouraged.
Research agenda
The present position paper highlights the great heterogeneity of protocols adopted and the lack of good-quality evidence supporting the implementation of enhanced recovery pathway in emergency general surgery. Further studies on this topic should address:
-
The definition of the safety, feasibility and effectiveness of each perioperative intervention.
-
The definition of a standardized enhanced recovery protocol for emergency general surgery procedures
-
The selection of patients who may benefit from an enhanced recovery pathway and the clinical scenarios in which enhanced recovery pathway could be applied.
Conclusions
Enhanced perioperative care, similar to elective surgery, should be implemented in emergency general surgery. One of the key elements for the success of the enhanced pathways is the multimodal approach involving surgeons, anesthetists, ICU physicians, nurses, patients and patient families. Available evidence suggests future required research on the implementation of enhanced recovery pathways in clinical practice.
Availability of data and materials
Data are available under request to the corresponding author.
Change history
15 October 2023
The CRUE CSIC TA funding note has been removed
References
Ljungqvist O, Scott M, Fearon KC. Enhanced recovery after surgery: a review. JAMA Surg [Internet]. 2017;152:292–8.
Greco M, Capretti G, Beretta L, Gemma M, Pecorelli N, Braga M. Enhanced recovery program in colorectal surgery: a meta-analysis of randomized controlled trials. World J Surg [Internet]. 2014;38:1531–41.
Lee Y, Yu J, Doumouras AG, Li J, Hong D. Enhanced recovery after surgery (ERAS) versus standard recovery for elective gastric cancer surgery: a meta-analysis of randomized controlled trials. Surg Oncol. 2020;32:75–87.
Ni X, Jia D, Chen Y, Wang L, Suo J. Is the enhanced recovery after surgery (ERAS) program effective and safe in laparoscopic colorectal cancer surgery? A meta-analysis of randomized controlled trials. J Gastrointest Surg [Internet]. 2019;23:1502–12.
Ni X, Jia D, Guo Y, Sun X, Suo J. The efficacy and safety of enhanced recovery after surgery (ERAS) program in laparoscopic digestive system surgery: a meta-analysis of randomized controlled trials. Int J Surg. 2019;69:108–15.
Ceresoli M, Braga M. Reply to: Early non compliance to enhanced recovery pathway might be an alert for underlying complications following colon surgery. Eur J Surg Oncol. 2023;49:526.
Quiney N, Aggarwal G, Scott M, Dickinson M. Survival after emergency general surgery: what can we learn from enhanced recovery programmes? World J Surg [Internet]. 2016;40:1283–7. https://doi.org/10.1007/s00268-016-3418-0.
Aggarwal G, Peden CJ, Mohammed MA, Pullyblank A, Williams B, Stephens T, et al. Evaluation of the collaborative use of an evidence-based care bundle in emergency laparotomy. JAMA Surg [Internet]. 2019;154:e190145.
Tengberg LT, Bay-Nielsen M, Bisgaard T, Cihoric M, Lauritsen ML, Foss NB, et al. Multidisciplinary perioperative protocol in patients undergoing acute high-risk abdominal surgery. Br J Surg [Internet]. 2017;104:463–71.
Møller MH, Adamsen S, Thomsen RW, Møller AM. Multicentre trial of a perioperative protocol to reduce mortality in patients with peptic ulcer perforation. Br J Surg. 2011;98:802–10.
Burcharth J, Falkenberg A, Oreskov JO, Ekeloef S, Gögenur I. Patients’ perceptions of barriers to enhanced recovery after emergency abdominal surgery. Langenbecks Arch Surg. 2021;406:405–12.
Wisely JC, Barclay KL. Effects of an Enhanced Recovery After Surgery programme on emergency surgical patients. ANZ J Surg. 2016;86:883–8.
Lohsiriwat V. Enhanced recovery after surgery for emergency colorectal surgery: Are there any differences between intra-abdominal infection and other indications? J Visc Surg [Internet]. 2019;156:489–96.
Lohsiriwat V. Enhanced recovery after surgery vs conventional care in emergency colorectal surgery. World J Gastroenterol [Internet]. 2014;20:13950.
Mohsina S, Shanmugam D, Sureshkumar S, Kundra P, Mahalakshmy T, Kate V. Adapted ERAS pathway vs. standard care in patients with perforated duodenal ulcer—a randomized controlled trial. J Gastrointest Surg [Internet]. 2018;22:107–16. https://doi.org/10.1007/s11605-017-3474-2.
Shang Y, Guo C, Zhang D. Modified enhanced recovery after surgery protocols are beneficial for postoperative recovery for patients undergoing emergency surgery for obstructive colorectal cancer. Medicine [Internet]. 2018;97:e12348. Available from: https://journals.lww.com/00005792-201809280-00034.
Gonenc M, Dural AC, Celik F, Akarsu C, Kocatas A, Kalayci MU, et al. Enhanced postoperative recovery pathways in emergency surgery: a randomised controlled clinical trial. Am J Surg [Internet]. 2014;207:807–14. https://doi.org/10.1016/j.amjsurg.2013.07.025.
Pranavi AR, Sureshkumar S, Mahalakshmy T, Kundra P, Kate V. Adapted ERAS pathway versus standard care in patients undergoing emergency surgery for perforation peritonitis—a randomized controlled trial. J Gastrointest Surg [Internet]. 2022;26:39–49. https://doi.org/10.1007/s11605-021-05184-x.
Roulin D, Blanc C, Muradbegovic M, Hahnloser D, Demartines N, Hübner M. Enhanced recovery pathway for urgent colectomy. World J Surg [Internet]. 2014;38:2153–9. https://doi.org/10.1007/s00268-014-2518-y.
Purushothaman V, Priyadarshini P, Bagaria D, Joshi M, Choudhary N, Kumar A, et al. Enhanced recovery after surgery (ERAS) in patients undergoing emergency laparotomy after trauma: a prospective, randomized controlled trial. Trauma Surg Acute Care Open [Internet]. 2021;6:e000698.
Nechay T, Titkova S, Tyagunov A, Anurov M, Sazhin A. Modified enhanced recovery after surgery protocol in patients with acute cholecystitis: efficacy, safety and feasibility. Multicenter randomized control study. Updates Surg. 2021;73:1407–17.
Ceresoli M, Biloslavo A, Bisagni P, Ciuffa C, Fortuna L, La Greca A, et al. Implementing enhanced perioperative care in emergency general surgery: a prospective multicenter observational study. World J Surg [Internet]. 2023. https://doi.org/10.1007/s00268-023-06984-9.
Sharma J, Kumar N, Huda F, Payal YS. Enhanced recovery after surgery protocol in emergency laparotomy: a randomized control study. Surg J. 2021;07:e92–9.
Masood A, Viqar S, Zia N, Ghani M usman. Early oral feeding compared with traditional postoperative care in patients undergoing emergency abdominal surgery for perforated duodenal ulcer. Cureus. 2021.
Chndan MN, Khakholia M, Bhuyan K. Enhanced recovery after surgery (ERAS) versus standard care in patients undergoing emergency surgery for perforated peptic ulcer. Indian J Surg. 2020;82:1044–9.
Ruiz-Tovar J, Llavero C, Perez-Lopez M, Garcia-Marin A. Implementation of an enhanced recovery after surgery (ERAS) protocol for acute complicated and uncomplicated appendicitis. Tech Coloproctol. 2021;25:1073–8.
Saurabh K, Sureshkumar S, Mohsina S, Mahalakshmy T, Kundra P, Kate V. Adapted ERAS pathway versus standard care in patients undergoing emergency small bowel surgery: a randomized controlled trial. J Gastrointest Surg [Internet]. 2020;24:2077–87.
Pathrikar SG, Jadhav GS, Adhikari GR. The application of enhanced recovery after surgery protocols in patients with perforated duodenal ulcer. Cureus. 2023.
Huddart S, Peden CJ, Swart M, McCormick B, Dickinson M, Mohammed MA, et al. Use of a pathway quality improvement care bundle to reduce mortality after emergency laparotomy. Br J Surg [Internet]. 2015;102:57–66.
Hajibandeh S, Hajibandeh S, Bill V, Satyadas T. Meta-analysis of enhanced recovery after surgery (ERAS) protocols in emergency abdominal surgery. World J Surg [Internet]. 2020;44:1336–48. https://doi.org/10.1007/s00268-019-05357-5.
Lee KC, Sturgeon D, Lipsitz S, Weissman JS, Mitchell S, Cooper Z. Mortality and health care utilization among medicare patients undergoing emergency general surgery vs those with acute medical conditions. JAMA Surg. 2020;155:216.
Quiney N, Aggarwal G, Scott M, Dickinson M. Survival after emergency general surgery: what can we learn from enhanced recovery programmes? World J Surg. 2016;40:1283–7.
Columbus AB, Morris MA, Lilley EJ, Harlow AF, Haider AH, Salim A, et al. Critical differences between elective and emergency surgery: identifying domains for quality improvement in emergency general surgery. Surgery [Internet]. 2018;163:832–8.
Hallet J, Sutradhar R, Jerath A, Perez D’empaire P, Carrier F, Turgeon A, et al. Association between familiarity of the surgeon-anesthesiologist dyad and postoperative patient outcomes for complex gastrointestinal cancer surgery. JAMA Surg [Internet]. 2023.
Puccetti F, Elmore U, Rosati R. Application of ERAS protocols in esophagogastric emergency surgery: is it feasible and does it make sense? Updates Surg. 2023;75:383–7.
Bala M, Kashuk J, Moore EE, Catena F, Leppaniemi A, Ansaloni L, et al. Establishing position papers by the WSES. World J Emerg Surg. 2018;13:1.
Shuldham C. A review of the impact of pre-operative education on recovery from surgery. Int J Nurs Stud. 1999;36:171–7.
Burcharth J, Abdulhady L, Danker J, Ekeloef S, Jørgensen T, Lauridsen H, et al. Implementation of a multidisciplinary perioperative protocol in major emergency abdominal surgery. Eur J Trauma Emerg Surg [Internet]. 2021;47:467–77. https://doi.org/10.1007/s00068-019-01238-7.
Ferrara F, Parini D, Bondurri A, Veltri M, Barbierato M, Pata F, et al. Italian guidelines for the surgical management of enteral stomas in adults. Tech Coloproctol. 2019;23:1037–56.
Sethi A, Debbarma M, Narang N, Saxena A, Mahobia M, Tomar GS. Impact of targeted preoperative optimization on clinical outcome in emergency abdominal surgeries: a prospective randomized trial. Anesth Essays Res [Internet]. 2018;12:149.
Rhodes A, Evans LE, Alhazzani W, Levy MM, Antonelli M, Ferrer R, et al. Surviving sepsis campaign. Crit Care Med. 2017;45:486–552.
Evans L, Rhodes A, Alhazzani W, Antonelli M, Coopersmith CM, French C, et al. Surviving sepsis campaign: international guidelines for management of sepsis and septic shock 2021. Crit Care Med. 2021;49:e1063–143.
Rivers E, Nguyen B, Havstad S, Ressler J, Muzzin A, Knoblich B, et al. Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med [Internet]. 2001;345:1368–77. https://doi.org/10.1056/NEJMoa010307.
Duggan EW, Carlson K, Umpierrez GE. Perioperative hyperglycemia management. Anesthesiology. 2017;126:547–60.
Umpierrez GE, Smiley D, Jacobs S, Peng L, Temponi A, Mulligan P, et al. Randomized study of basal-bolus insulin therapy in the inpatient management of patients with type 2 diabetes undergoing general surgery (RABBIT 2 Surgery). Diabetes Care. 2011;34:256–61.
Jehan F, Joseph B. Perioperative glycemic control and postoperative complications in patients undergoing emergency general surgery: what is the role of HbA1c? J Trauma Acute Care Surg. 2019;86:379–379.
Yatabe T, Inoue S, Sakaguchi M, Egi M. The optimal target for acute glycemic control in critically ill patients: a network meta-analysis. Intensive Care Med. 2017;43:16–28.
Gustafsson UO, Scott MJ, Hubner M, Nygren J, Demartines N, Francis N, et al. Guidelines for perioperative care in elective colorectal surgery: enhanced recovery after surgery (ERAS®) society recommendations: 2018. World J Surg [Internet]. 2019;43:659–95.
Koivuranta M, Läärä E, Snåre L, Alahuhta S. A survey of postoperative nausea and vomiting. Anaesthesia [Internet]. 1997;52:443–9.
Horn CC, Wallisch WJ, Homanics GE, Williams JP. Pathophysiological and neurochemical mechanisms of postoperative nausea and vomiting. Eur J Pharmacol [Internet]. 2014;722:55–66.
Veiga-Gil L, Pueyo J, López-Olaondo L. Postoperative nausea and vomiting: physiopathology, risk factors, prophylaxis and treatment. Rev Esp Anestesiol Reanim [Internet]. 2017;64:223–32.
Cozza V, Barberis L, Altieri G, Donatelli M, Sganga G, Greca A la. Prediction of postoperative nausea and vomiting by point-of-care gastric ultrasound: can we improve complications and length of stay in emergency surgery? A cohort study. 2021. https://doi.org/10.1186/s12871-021-01428-0.
de Oliveira GS, Castro-Alves LJS, Ahmad S, Kendall MC, McCarthy RJ. Dexamethasone to prevent postoperative nausea and vomiting: an updated meta-analysis of randomized controlled trials. Anesth Analg [Internet]. 2013;116:58–74.
Eberhart LHJ, Mauch M, Morin AM, Wulf H, Geldner G. Impact of a multimodal anti-emetic prophylaxis on patient satisfaction in high-risk patients for postoperative nausea and vomiting. Anaesthesia [Internet]. 2002;57:1022–7.
Apfel CC, Bacher A, Biedler A, Danner K, Danzeisen O, Eberhart LHJ, et al. A factorial trial of six interventions for the prevention of postoperative nausea and vomiting. Anaesthesist [Internet]. 2005;54:201–9.
Polderman JA, Farhang-Razi V, van Dieren S, Kranke P, DeVries JH, Hollmann MW, et al. Adverse side effects of dexamethasone in surgical patients. Cochrane Database Syst Rev [Internet] 2018;11.
Doleman B, Leonardi-Bee J, Heinink TP, Boyd-Carson H, Carrick L, Mandalia R, et al. Pre-emptive and preventive NSAIDs for postoperative pain in adults undergoing all types of surgery. Cochrane Database Syst Rev [Internet] 2021;6.
Apfel CC, Turan A, Souza K, Pergolizzi J, Hornuss C. Intravenous acetaminophen reduces postoperative nausea and vomiting: a systematic review and meta-analysis. Pain [Internet]. 2013;154:677–89.
Miller D, Lewis SR, Pritchard MW, Schofield-Robinson OJ, Shelton CL, Alderson P, et al. Intravenous versus inhalational maintenance of anaesthesia for postoperative cognitive outcomes in elderly people undergoing non-cardiac surgery. Cochrane Database Syst Rev [Internet] 2018;8.
Saljuqi AT, Hanna K, Asmar S, Tang A, Zeeshan M, Gries L, et al. Prospective evaluation of delirium in geriatric patients undergoing emergency general surgery. J Am Coll Surg [Internet]. 2020;230:758–65.
Moller JT, Cluitmans P, Rasmussen LS, Houx P, Rasmussen H, Canet J, et al. Long-term postoperative cognitive dysfunction in the elderly: ISPOCD1 study. Lancet [Internet]. 1998;351:857–61.
Clegg A, Young JB. Which medications to avoid in people at risk of delirium: a systematic review. Age Ageing [Internet]. 2011;40:23–9.
Duprey MS, Devlin JW, Griffith JL, Travison TG, Briesacher BA, Jones R, et al. Association between perioperative medication use and postoperative delirium and cognition in older adults undergoing elective noncardiac surgery. Anesth Analg [Internet]. 2022;134:1154–63.
McLott J, Stahel PF. Opioid-free anesthesia: the next frontier in surgical patient safety. Patient Saf Surg. BioMed Central Ltd; 2022.
Wick EC, Grant MC, Wu CL. Postoperative multimodal analgesia pain management with nonopioid analgesics and techniques: a review. JAMA Surg [Internet]. 2017;152:691–7.
Chan MTV, Cheng BCP, Lee TMC, Gin T. BIS-guided anesthesia decreases postoperative delirium and cognitive decline. J Neurosurg Anesthesiol [Internet]. 2013;25:33–42.
Zorrilla-Vaca A, Healy RJ, Wu CL, Grant MC. Relation between bispectral index measurements of anesthetic depth and postoperative mortality: a meta-analysis of observational studies. Can J Anaesth [Internet]. 2017;64:597–607.
Evered LA, Chan MTV, Han R, Chu MHM, Cheng BP, Scott DA, et al. Anaesthetic depth and delirium after major surgery: a randomised clinical trial. Br J Anaesth [Internet]. 2021;127:704–12.
Short TG, Campbell D, Frampton C, Chan MTV, Myles PS, Corcoran TB, et al. Anaesthetic depth and complications after major surgery: an international, randomised controlled trial. Lancet [Internet]. 2019;394:1907–14.
Berg H, Viby-Mogensen J, Roed J, Mortensen CR, Engbæk J, Skovgaard LT, et al. Residual neuromuscular block is a risk factor for postoperative pulmonary complications. A prospective, randomised, and blinded study of postoperative pulmonary complications after atracurium, vecuronium and pancuronium. Acta Anaesthesiol Scand [Internet]. 1997;41:1095–103.
Naguib M, Kopman AF, Ensor JE. Neuromuscular monitoring and postoperative residual curarisation: a meta-analysis. Br J Anaesth [Internet]. 2007;98:302–16.
Carvalho H, Verdonck M, Cools W, Geerts L, Forget P, Poelaert J. Forty years of neuromuscular monitoring and postoperative residual curarisation: a meta-analysis and evaluation of confidence in network meta-analysis. Br J Anaesth [Internet]. 2020;125:466–82.
Carli F, Kehlet H, Baldini G, Steel A, McRae K, Slinger P, et al. Evidence basis for regional anesthesia in multidisciplinary fast-track surgical care pathways. Reg Anesth Pain Med [Internet]. 2011;36:63–72.
Li YW, Li HJ, Li HJ, Zhao BJ, Guo XY, Feng Y, et al. Delirium in older patients after combined epidural-general anesthesia or general anesthesia for major surgery: a randomized trial. Anesthesiology [Internet]. 2021;135:218–32.
Werawatganon T, Charuluxananan S. Patient controlled intravenous opioid analgesia versus continuous epidural analgesia for pain after intra-abdominal surgery. Cochrane Database Syst Rev [Internet]. 2013. https://doi.org/10.1002/14651858.CD004088.pub3/full.
Vester-Andersen M, Lundstrøm LH, Møller MH. The association between epidural analgesia and mortality in emergency abdominal surgery: a population-based cohort study. Acta Anaesthesiol Scand [Internet]. 2020;64:104–11.
Hübner M, Blanc C, Roulin D, Winiker M, Gander S, Demartines N. Randomized clinical trial on epidural versus patient-controlled analgesia for laparoscopic colorectal surgery within an enhanced recovery pathway. Ann Surg [Internet]. 2015;261:648–53.
Tsuchiya M, Takahashi R, Furukawa A, Suehiro K, Mizutani K, Nishikawa K. Transversus abdominis plane block in combination with general anesthesia provides better intraoperative hemodynamic control and quicker recovery than general anesthesia alone in high-risk abdominal surgery patients. Minerva Anestesiol [Internet]. 2012;78:1241–7.
McDonnell JG, O’Donnell B, Curley G, Heffernan A, Power C, Laffey JG. The analgesic efficacy of transversus abdominis plane block after abdominal surgery: A prospective randomized controlled trial. Anesth Analg [Internet]. 2007;104:193–7.
Walter CJ, Maxwell-Armstrong C, Pinkney TD, Conaghan PJ, Bedforth N, Gornall CB, et al. A randomised controlled trial of the efficacy of ultrasound-guided transversus abdominis plane (TAP) block in laparoscopic colorectal surgery. Surg Endosc [Internet]. 2013;27:2366–72.
Tikuisis R, Miliauskas P, Lukoseviciene V, Samalavicius N, Dulskas A, Zabuliene L, et al. Transversus abdominis plane block for postoperative pain relief after hand-assisted laparoscopic colon surgery: a randomized, placebo-controlled clinical trial. Tech Coloproctol [Internet]. 2016;20:835–44.
Hamid HK, Emile SH, Saber AA, Ruiz-Tovar J, Minas V, Cataldo TE. Laparoscopic-guided transversus abdominis plane block for postoperative pain management in minimally invasive surgery: systematic review and meta-analysis. J Am Coll Surg [Internet]. 2020;231:376-386.e15.
Billeter AT, Hohmann SF, Druen D, Cannon R, Polk HC. Unintentional perioperative hypothermia is associated with severe complications and high mortality in elective operations. Surgery [Internet]. 2014;156:1245–52.
Braga M, Scatizzi M, Borghi F, Missana G, Radrizzani D, Gemma M, et al. Identification of core items in the enhanced recovery pathway. Clin Nutr ESPEN. 2018;25:139–44.
Balki I, Khan JS, Staibano P, Duceppe E, Bessissow A, Sloan EN, et al. Effect of perioperative active body surface warming systems on analgesic and clinical outcomes: a systematic review and meta-analysis of randomized controlled trials. Anesth Analg. 2020;131:1430–43.
Bellamy MC. Wet, dry or something else? Br J Anaesth [Internet]. 2006;97:755–7.
Shin CH, Long DR, McLean D, Grabitz SD, Ladha K, Timm FP, et al. Effects of intraoperative fluid management on postoperative outcomes: a hospital registry study. Ann Surg [Internet]. 2018;267:1084–92.
Thacker JKM, Mountford WK, Ernst FR, Krukas MR, Mythen MG. Perioperative fluid utilization variability and association with outcomes: considerations for enhanced recovery efforts in sample US surgical populations. Ann Surg [Internet]. 2016;263:502–10.
Lowell JA, Schifferdecker C, Driscoll DF, Benotti PN, Bistrian BR. Postoperative fluid overload: not a benign problem. Crit Care Med [Internet]. 1990;18:728–33.
Nisanevich V. Effect of intraoperative fluid management on outcome after intraabdominal surgery. Anesthesiology [Internet]. 2005;103:25–32.
Holte K, Sharrock NE, Kehlet H. Pathophysiology and clinical implications of perioperative fluid excess. Br J Anaesth [Internet]. 2002;89:622–32.
Brandstrup B. Fluid therapy for the surgical patient. Best Pract Res Clin Anaesthesiol [Internet]. 2006;20:265–83.
Bundgaard-Nielsen M, Holte K, Secher NH, Kehlet H. Monitoring of peri-operative fluid administration by individualized goal-directed therapy. Acta Anaesthesiol Scand [Internet]. 2007;51:331–40.
Jessen MK, Vallentin MF, Holmberg MJ, Bolther M, Hansen FB, Holst JM, et al. Goal-directed haemodynamic therapy during general anaesthesia for noncardiac surgery: a systematic review and meta-analysis. Br J Anaesth. 2022;128:416–33.
Mamidanna R, Burns EM, Bottle A, Aylin P, Stonell C, Hanna GB, et al. Reduced risk of medical morbidity and mortality in patients selected for laparoscopic colorectal resection in England: a population-based study. Arch Surg [Internet]. 2012;147:219–27.
Kehlet H. Surgical stress response: does endoscopic surgery confer an advantage? World J Surg [Internet]. 1999;23:801–7.
Novitsky YW, Litwin DEM, Callery MP. The net immunologic advantage of laparoscopic surgery. Surg Endosc [Internet]. 2004;18:1411–9.
Braga M, Borghi F, Scatizzi M, Missana G, Guicciardi MA, Bona S, et al. Impact of laparoscopy on adherence to an enhanced recovery pathway and readiness for discharge in elective colorectal surgery: results from the PeriOperative Italian Society registry. Surg Endosc [Internet]. 2017;31:4393–9. https://doi.org/10.1007/s00464-017-5486-0.
Pucher PH, Mackenzie H, Tucker V, Mercer SJ. A national propensity score-matched analysis of emergency laparoscopic versus open abdominal surgery. Br J Surg [Internet]. 2021;108:934–40.
Tan S, Wu G, Zhuang Q, Xi Q, Meng Q, Jiang Y, et al. Laparoscopic versus open repair for perforated peptic ulcer: a meta analysis of randomized controlled trials. Int J Surg. 2016;33:124–32.
Warps A-LK, Zwanenburg ES, Dekker JWT, Tollenaar RAEM, Bemelman WA, Hompes R, et al. Laparoscopic versus open colorectal surgery in the emergency setting. Ann Surg Open. 2021;2:e097.
Arnold M, Elhage S, Schiffern L, Lauren Paton B, Ross SW, Matthews BD, et al. Use of minimally invasive surgery in emergency general surgery procedures. Surg Endosc [Internet]. 2020;34:2258–65. https://doi.org/10.1007/s00464-019-07016-1.
Ceresoli M, Pisano M, Abu-Zidan F, Allievi N, Gurusamy K, Biffl WL, et al. Minimally invasive surgery in emergency surgery: a WSES survey. World J Emerg Surg. 2022;17:18.
Zhang HY, Zhao CL, Xie J, Ye YW, Sun JF, Ding ZH, et al. To drain or not to drain in colorectal anastomosis: a meta-analysis. Int J Colorectal Dis [Internet]. 2016;31:951–60.
Chen JS, da Sun S, Wang ZS, Cai TH, Huang LK, Sun WX, et al. The factors related to failure of Enhanced Recovery after Surgery (ERAS) in colon cancer surgery. Langenbecks Arch Surg [Internet]. 2020;405:1025–30.
Coccolini F, Corradi F, Sartelli M, Coimbra R, Kryvoruchko IA, Leppaniemi A, et al. Postoperative pain management in non-traumatic emergency general surgery: WSES-GAIS-SIAARTI-AAST guidelines. World J Emerg Surg [Internet]. 2022;17:1–15.
Nelson R, Edwards S, Tse B. Prophylactic nasogastric decompression after abdominal surgery. Cochrane Database Syst Rev [Internet]. 2007;10:50. https://doi.org/10.1002/14651858.CD004929.pub3/full.
Shang Y, Guo C, Zhang D. Modified enhanced recovery after surgery protocols are beneficial for postoperative recovery for patients undergoing emergency surgery for obstructive colorectal cancer. Medicine [Internet]. 2018;97:e12348.
Brower RG. Consequences of bed rest. Crit Care Med. 2009;37:S422–8.
Wren SM, Martin M, Yoon JK, Bech F. Postoperative pneumonia-prevention program for the inpatient surgical ward. J Am Coll Surg. 2010;210:491–5.
Haines KJ, Skinner EH, Berney S. Association of postoperative pulmonary complications with delayed mobilisation following major abdominal surgery: an observational cohort study. Physiotherapy. 2013;99:119–25.
Castelino T, Fiore JF, Niculiseanu P, Landry T, Augustin B, Feldman LS. The effect of early mobilization protocols on postoperative outcomes following abdominal and thoracic surgery: a systematic review. Surgery. 2016;159:991–1003.
Rosowicz A, Brody JS, Lazar DJ, Bangla VG, Panahi A, Nobel TB, et al. Early ambulation is associated with improved outcomes following colorectal surgery. Am Surg. 2022. https://doi.org/10.1177/00031348221142.
Gillis C, Carli F. Promoting perioperative metabolic and nutritional care. Anesthesiology. 2015;123:1455–72.
Zhuang C-L, Ye X-Z, Zhang C-J, Dong Q-T, Chen B-C, Yu Z. Early versus traditional postoperative oral feeding in patients undergoing elective colorectal surgery: a meta-analysis of randomized clinical trials. Dig Surg. 2013;30:225–32.
Andersen HK, Lewis SJ, Thomas S. Early enteral nutrition within 24h of colorectal surgery versus later commencement of feeding for postoperative complications. Cochrane Database Syst Rev. 2006.
Gonenc M, Gemici E, Kalayci MU, Karabulut M, Turhan AN, Alis H. Intracorporeal knotting versus metal endoclip application for the closure of the appendiceal stump during laparoscopic appendectomy in uncomplicated appendicitis. J Laparoendosc Adv Surg Tech. 2011;22:231–5.
Sawyer RG, Claridge JA, Nathens AB, Rotstein OD, Duane TM, Evans HL, et al. Trial of short-course antimicrobial therapy for intraabdominal infection. N Engl J Med [Internet]. 2015;372:1996–2005.
Sartelli M, Catena F, Ansaloni L, Coccolini F, di Saverio S, Griffiths EA. Duration of antimicrobial therapy in treating complicated intra-abdominal infections: a comprehensive review. Surg Infect. 2016;17:9–12. https://doi.org/10.1089/sur.2015.130.
Sartelli M, Coccolini F, Kluger Y, Agastra E, Abu-Zidan FM, Abbas AES, et al. WSES/GAIS/SIS-E/WSIS/AAST global clinical pathways for patients with intra-abdominal infections. World J Emerg Surg. 2021;16:1–48. https://doi.org/10.1186/s13017-021-00387-8.
Funding
No fundings were received for this paper.
Author information
Authors and Affiliations
Contributions
All the authors contributed to the conception, writing, discussion and approval of the present manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical approval was not required for this review and position paper.
Competing interests
All the authors have no conflict of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ceresoli, M., Braga, M., Zanini, N. et al. Enhanced perioperative care in emergency general surgery: the WSES position paper. World J Emerg Surg 18, 47 (2023). https://doi.org/10.1186/s13017-023-00519-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13017-023-00519-2