Abstract
High-grade gliomas are the most common intracranial malignancies, and their current prognosis remains poor despite standard aggressive therapy. Charged particle beams have unique physical and biological properties, especially high relative biological effectiveness (RBE) of carbon ion beam might improve the clinical treatment outcomes of malignant gliomas. We systematically reviewed the safety, efficacy, and dosimetry of carbon-ion or proton radiotherapy to treat high-grade gliomas. The protocol is detailed in the online PROSPERO database, registration No. CRD42021258495. PubMed, EMBASE, Web of Science, and The Cochrane Library databases were collected for data analysis on charged particle radiotherapy for high-grade gliomas. Until July 2022, two independent reviewers extracted data based on inclusion and exclusion criteria. Eleven articles were eligible for further analysis. Overall survival rates were marginally higher in patients with the current standard of care than those receiving concurrent intensity-modulated radiotherapy plus temozolomide. The most common side effects of carbon-ion-related therapy were grade 1–2 (such as dermatitis, headache, and alopecia). Long-term toxicities (more than three to six months) usually present as radiation necrosis; however, toxicities higher than grade 3 were not observed. Similarly, dermatitis, headache, and alopecia are among the most common acute side effects of proton therapy treatment. Despite improvement in survival rates, the method of dose-escalation using proton boost is associated with severe brain necrosis which should not be clinically underestimated. Regarding dosimetry, two studies compared proton therapy and intensity‐modulated radiation therapy plans. Proton therapy plans aimed to minimize dose exposure to non-target tissues while maintaining target coverage. The use of charged-particle radiotherapy seems to be effective with acceptable adverse effects when used either alone or as a boost. The tendency of survival outcome shows that carbon ion boost is seemingly superior to proton boost. The proton beam could provide good target coverage, and it seems to reduce dose exposure to contralateral organs at risk significantly. This can potentially reduce the treatment-related dose- and volume-related side effects in long-term survivors, such as neurocognitive impairment. High-quality randomized control trials should be conducted in the future. Moreover, Systemic therapeutic options that can be paired with charged particles are necessary.
Similar content being viewed by others
Background
High-grade gliomas (HGGs) are the most common primary intracranial malignancies, accounting for approximately 47.1% of malignant brain tumors [1, 2]. According to the World Health Organization (WHO) classification, HGGs mainly consist of glioblastoma multiforme (GBM), anaplastic astrocytoma (AA), or oligodendroglioma [3]. The poor prognosis of aggressive treatment, including gross total resection, photon radiotherapy, chemotherapy, and(or) tumor treatment fields makes treatment challenging worldwide. Considering the features of highly infiltrative tumors and rapid progression, new treatment techniques need to be explored. Compared with X-rays, a high linear energy transfer beam has significant physical characteristics. The apparent decrease in the integral dosage is affected by a Bragg peak [4, 5]. Carbon ion beam has stronger biological effects than normal X-rays, and cell death caused by DNA double-strand breaks is far more difficult to repair. Some in vitro studies calculated the relative biological effectiveness of carbon ions in glioblastoma range between 3 and 5 [6, 7]. It is generally reported that the relative biological effectiveness of proton beams is 1.1 equivalent to that of photon [8]. Charged particles have been used to treat HGGs in the USA, Japan, Germany, and China. It is important to closely assess whether charged particles are effective and safe over current standard therapeutic options for treating HGGs. Therefore, we systematically reviewed the currently available data to thoroughly examine the clinical efficacy and safety of carbon ions and protons for treating HGGs and compare the results with those of conventional techniques.
Materials and methods
Search strategy
This systematic review was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses statement. All literature searches were conducted until July 2022, using the search tools of Embase, Cochrane Library, Web of Science, and PubMed databases with the search terms, “particle”, “charged particle”, “heavy-ion*”, OR “carbon ion”, OR “proton” AND “high-grade glioma” OR “glioblastoma” OR “anaplastic astrocytoma”. “particle”, “charged particle”, “heavy-ion*”, OR “carbon ion”, OR “proton” AND “Dosimetry” OR “Dosimetry study”. Only publications written in English were included. Additional studies were identified from the citation counts of conference abstracts, review articles, and reference lists. All references were screened to ensure that relevant studies were included.
Inclusion and exclusion criteria
Studies were included if they met the following criteria: (a) clinical or retrospective studies reporting efficacy, adverse reaction, and/or dosimetry comparison in patients with newly diagnosed HGG with charged particle beam; (b) Trials enrolling adults; and (c) studies reporting tumors that had been pathologically diagnosed. Publications were excluded if they were (a) case reports on one or two patients; (b) letters, editorials, protocols, reviews, or meta-analyses; (c) duplicate publications; (d) cell and animal experimental studies; (e) lacking detailed data; (f) recurrent glioma; (g)prior brain radiation.
Data extraction
The necessary data were extracted independently by two researchers, and the results were discussed with senior investigators if there was no discrepancy. Overall survival (OS), progression-free survival (PFS), treatment-related toxicity, target volume dose, and organ at risk dose were among the outcomes studied. For each article, the following data were obtained: first author, publication year, study period, the number of patients, institution, tumor site, tumor status, total treatment dose, and the median follow-up time.
Quality assessment
Case series reports were evaluated using the case series report bias evaluation tool as shown in Table 1 with the answer yes, no, or ambiguous. The evaluation indicators were as follows: (a) inclusion and exclusion criteria; (b) clinical heterogeneity of patients, including disease severity, classification, duration, and onset time; (c) whether the main intervention measures (dose, administration, and course of treatment, etc.) were clearly described; (d) whether the measurement method of relevant outcome measures was reasonable; (e) whether the outcome measures were measured before and after the intervention; (f) whether the loss to follow-up and follow-up time were recorded; (g) whether adverse events related to clinical treatment were documented; and (h) whether the outcome measurer was blinded. The literature quality evaluation was independently completed by two members, respectively.
Results
Study characteristics
During the duplication removal and abstract screening process, 1357 of the original 2845 studies classified by four databases were removed (refer to Fig. 1). According to the applicable exclusion criterion, 33 full texts were screened further, leaving 11 relevant studies for data extraction. Eight clinical trials and three dosimetry comparability studies were conducted. Eight clinical studies were chosen (one retrospective study, seven prospective studies) including two carbon-ion-related treatments, and six protons and/or photon-based combinations. A total of 350 patients were drawn from eight cohorts, with case numbers ranging from 13 to 67, and the median follow-up times ranging from 14.3 to 48.7 months. All 350 patients were diagnosed with HGG (WHO grade III–IV), and the pathological types, including glioblastoma and AA. Two prospective studies associated with carbon-ion therapy were undertaken in Japan and China, while the rest of the research was conducted in two countries (USA, Germany). The general characteristics are shown in detail in Table 2. Despite some inconsistencies in the definitions of both regions of interest (for example, the healthy brain tissue) and relevant dosimetry indices (for example, inhomogeneity coefficients and conformity indices), which hindered data pooling, most dosimetry studies reported a statistical analysis providing quantitative support for the results. The ongoing clinical trials are reported in a Table 5.
Treatment and clinical survival results
As shown in Tables 2 and 3, the eight selected articles included one retrospective study, six prospective phases I/II mono-institutional studies, and one multi-institutional collaborative registry. Overall, 350 patients with newly diagnosed HGGs were treated. The median follow-up ranged between 14.3 and 48.7 months. Two clinical studies regarding the treatment center of Japan and China conducted carbon-ion-related therapy. These two trials were both prospective and single-center trials, evaluating the outcome of carbon ion or mixed with proton or photon therapy after some surgical procedure. In the National Institute of Radiological Sciences, patients were treated using photon therapy and chemotherapy followed by carbon ion therapy. Photon therapy (1.8 to 2.0 Gy per fraction) was administered five days a week with a total of 50.0 Gy. Nimustine hydrochloride (ACNU) was administrated at a dose of 100 mg/m2 on the first and fourth or fifth weeks of photon therapy. After radio-chemotherapy for each patient, carbon ion radiation was administered four days per week for over two weeks. In a dose-escalation study from 16.8 Gray equivalent (GyE) to 24.8 GyE in every 10% increase, the median OS of AA patients was 35 months while those with GBM was 17 months. The median PFS and OS of patients with GBM were 4 and 7 months for the low-dose group (16.8GyE), 7 and 19 months for the middle-dose group (18.4–22.4GyE), and 14 and 26 months for the high-dose group (24.8GyE), respectively. In a clinical trial by Kong et al., 50 patients were treated with a proton or proton plus carbon ion boost. The proton therapy protocol was 60.0GyE in 30 fractions, with three dose-escalation schemes employing carbon ions in addition to chemotherapy (refer to Table 3). The 12-month and 18-month OS rates were 87.8% and 72.8%, respectively. The 12-month and 18-month OS rates of GBM were 77.4% and 61%, respectively, and those of AA were 100%. The efficacy of these two carbon-ion-related radiations had an advantage over current standardized protocols from Stupp et al. [9, 10].
The remaining six studies were associated with proton and/or photon therapy. In the study by Vora et al. [11], using prospective, multi-institutional clinical trials among HGGs were conducted using therapeutic surgery and temozolomide-based chemotherapy followed by proton radiation alone. The median total dose delivered was 59.4 GyE (range 40 to 66 GyE), which was administered over 15–33 fractions. The median OS for all patients was 18.3 months with 2 years OS of 39.0%, and the median OS for GBM was 17 months. The next study contributed to this systematic review from Brown et al. [12]; the enrolled patients were randomized to proton therapy or intensity-modulated radiation (IMRT) groups. Similarly, surgery and chemotherapy were performed in preparation for subsequent radiotherapy. The simultaneous integrated boost technique treated both PTV50 and PTV60 to 50 Gy and 60 Gy in 30 fractions. There was no difference between the proton therapy and IMRT in median PFS (6.6 months vs.8.9 months) or OS (24.5 months vs.21.2 months).
At different Japanese, German, and USA institutes, the University of Tsukuba explored novel approaches for photon and proton boost therapies. In the study by Tsujii et al. [13], five patients were treated with proton therapy alone with a median 66.8 Gy, while eight patients were treated with photon therapy followed by proton boosts for a total mean 86.8 Gy. The median OS for AA, GBM, and AA + GBM were 25, 13, and 20 months, respectively. Mizumoto et al. [14] reported that patients who underwent photon therapy (total dose 50.4 Gy in 28 fractions) followed by hyper-fractionated boost proton therapy (total dose 46.2GyE in 28 fractions) plus nimustine hydrochloride (80 mg/m2 in the first and fourth weeks) or temozolomide(75 mg/m2, daily) had 1- and 2-year OS rates of 78% and 43%, respectively and median OS of 21.0 months. The treatment plan of studies by Adeberg et al. [14] also included treating the patients with photons (range 50 to 50.4 Gy) and proton boost (total dose 10GyE); the median OS for photon alone and photon plus proton boost was 20.9 and 19.1 months, respectively. Fitzek et al. [15] reported that 23 GBM patients underwent surgery followed by accelerated fractionated photon therapy (total dose 55–65 Gy) and proton therapy applied as a boost (dose escalation to 90 cobalt gray equivalent, CGE) in the United States. The prescription doses for the three target volumes in this prospective phase II trial are, respectively, volume 1, 90 CGE; volume 2, 64.8 CGE; and volume 3, 50.4 CGE (proton doses plus x-ray irradiation doses). The median total dose was 93.5 CGE with 92.05 to 94.2 CGE. The OS rates at one, two, and three years were 78%, 34%, and 18%, respectively. The median survival time was 20 months.
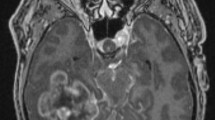
Patterns of failure
The patterns of failure (mainly tumor recurrence) are reported by Fitzek et al. and Mizumoto et al. [15, 16]. Pathological samples were available in 15 (65%) of 23 patients from the dose-escalation plan. On the contrary, nine patients were found to have recurrent tumors and radiation necrosis. Further analysis on three patients by autopsy demonstrated that recurrent tumors were outside the high-dose volume (90CGE). The Kaplan–Meier analysis showed that the median OS of the patients with necrosis was 29 months compared with 16 months in the recurrent patients (p = 0.01). Another study reported that MRI examined all 23 patients treated by hyper-fractionated proton boost. In another study of 23 patients who received hyper-fractionated proton boost, changes in control MRI occurred in 20 cases. Six (75%) of 8 patients within who received 96.6GyE had brain necrosis without tumor recurrence within CTV1.
Toxicity
Almost all patients completed the treatment without interruption or discontinuation. The study examined acute toxicities within 3–6 months of treatment completion. Two studies have reported adverse reactions in patients with HGGs treated with carbon ion boost. No Grade 3 or severe toxicities were reported. These cases reported some acute symptoms following carbon ion boost, such as dermatitis, alopecia, headaches, and late side effects relating to brain necrosis in patients with Grade 1–2 (according to CTCAE or RTOG/EORTC). All of the data are shown in Table 4. The side effects of the photon with proton boost from Adeberg et al. [14] showed that toxicity of Grade 1–2 was observed in 6 patients receiving bimodality radiotherapy and no Grade 3 or higher-grade acute reactions. And late side effects were not reported. Dose escalation using protons as boost to the photon therapy offers a high total dose. The common acute adverse effects (Grade1-2) were alopecia/dermatitis, nausea, or headache, and one patient had a severe acute reaction. Still, brain necrosis was a very common late toxicity (23% of patients with radiation necrosis by Mizumoto et al. [17] and all patients in the study of Fitzek et al. [15]). Similarly, the most common acute adverse effects during treatment with proton therapy were dermatitis, headaches, and alopecia, while radiation necrosis has not yet occurred [11]. Brown et al. [12] reported that proton therapy significantly reduced the dose of normal tissues. When adverse event occurrences are compared for each patient, the average number of Grade 2 or higher toxicities is considerably higher in patients who received IMRT than in those who underwent proton therapy.
Comparison of dosimetry plans
Three available papers were related to dosimetry studies, comparing 3D-CRT, intensity‐modulated radiation therapy (IMRT), and proton therapy, as well as different IMRT techniques, such as volumetric modulated arc therapy (VMAT) versus intensity-modulated proton therapy. The standard photon therapy radiation plan was prescribed at 60 Gy in 30 fractions, while the patients received intensity-modulated proton therapy (IMPT) with 60GyE in 2.0GyE fractions. Holm et al. explored the dose-escalation plan for all three techniques (refer to Table 6).
Target dosimetry evaluation
Adeberg et al. [18] showed that clinical target volume(CTV)coverage was comparable among three distinct techniques; V90% and V95% were observed with no difference. The homogeneity index (HI = D5 − D95/Dp) was higher in the proton and VMAT plans than in the 3D-CRT plans. The minimum dose to the CTV (Dmin) in the proton plans was significantly higher than in the photon plans (p-value < 0.05). The PTV coverage, absorbed dose standard deviation for PTV, was the only target parameter illustrated by Rosenschöld et al. [19] research. The PTV coverage was significantly higher for IMPT (p < 0.0001) than VMAT. Holm et al. [20] explored dose escalation of three modalities using two parameters (R30 and ODV refer to Table 5 annotation) to evaluate dose homogeneity. The median ODV was reduced by 4 percentage points (p < 0.05) and 48 percentage points (p < 0.05) for the VMAT and IMPT, respectively. The IMPT significantly reduced the median R30 (45% vs. 35%, p < 0.05).
Dosimetry assessment of OARs
Three papers provide specific figures on OARs: Adeberg et al. [18] reported a significant reduction in the Dmean to the contralateral optic nerve (ON) and brainstem in IMPT compared with VMAT (− 66.8 and − 28.1%, respectively) or 3D-CRT (− 67.6 and − 67.7%, respectively). As described above, the integral dose was reduced when observed on the contralateral optic nerve and brainstem. IMPT reduced the Dmean and integral dosage to the pituitary gland by 52.5% and 65.0%, respectively, along the hypothalamic-pituitary axis. The Dmean and ID to the infratentorial brain could be reduced by 77.0% and 81.7%, respectively, when using IMPT over VMAT and by 91.6 and 81.7%, using 3D-CRT. Adeberg et al. [18] also demonstrated that sparing of the contralateral subventricular zone (SVZ) and hippocampus was significant for Dmean and integral dose when using proton therapy. According to Rosenschöld et al. [19] the Dmean to the whole brain was significantly lower for IMPT than VMAT (p < 0.0001), while the Dmax to the chiasm and brainstem were comparable for all techniques. Holm et al. [20] compared dose-escalation plans and the standard plan in the Dmean to the OAR. For IMPT, the sparing of all the organs at risk was much better than the standard plan when noticed. IMPT significantly reduced the danger of radio-necrosis by estimating the ratio of the dose-volume histograms of the brain.
Discussion
This systematic review aimed to determine the efficacy and safety of charged-particle therapy in adult patients with HGGs. However, few articles are available that are relevant to the aim of this research. The application of charged-particle therapy for treating HGG was now basically in clinical trials. Moreover, these accessible researches, in general, contain inadequacies, such as small sample sizes, a heterogeneous body of research, and obsolete diagnosis or treatment measures. Over the past decade, there has been a consensus on the management of gliomas. For newly diagnosed HGGs, the standard treatment approach includes maximally safe surgery, concurrent TMZ-based radio-chemotherapy (75 mg/m2 for 42 days), adjuvant chemotherapy (150–200 mg/m2 in a 5/28 schedule) for 6–12 cycles, further combined with tumor treatment fields (TTF) for GBM but also for AA in some countries. The radiation dose prescription is up to 60.0 Gy in 2.0 Gy fractions that include the contrast-enhancing area [9, 10, 21]. Even though the median OS and median PFS for radiation plus temozolomide for GBM were 14.6 and 6.9 months, the outcome of survival is still unfavorable [22]. Strategies regarding dose-escalated radiotherapy, hypo-fractionated or hyper-fractioned trial, and stereotactic radiosurgery boost were conducted [23, 24]. However, these active attempts do not seem to fundamentally solve the problem of tumor control.
Up till now, the carbon-ion beams have been applied in clinical practice as boosting technique after proton or photon therapy. Kong et al. [25] reported that the modality of particle therapy plus concurrent temozolomide was carried out to manage HGG for the first time. The 18 months OS and PFS rates with charged particle therapy plus temozolomide were 72.8% and 59.8%, respectively, and 29.4% and 18.4% (18 months) with photon-based chemo-radiotherapy by Stupp et al. [10]. The above results indicate that charged particle therapy (proton plus carbon ion boost) appears to be more effective than traditional photon therapy. However, the median follow-up of 14.3 months is too short to be accurate, and the subsequent results should be considered constantly. The pattern of treatment failure in HGGs is mainly local recurrence, even if maximal surgery and high-dose radiotherapy are completed. The majority of recurrence sites are related to photon therapy CTV [26]. Dose escalation may solve the problem if the brain tissue is spared from high-dose radiation. In the Shanghai Proton and Heavy Ion Center (SPHIC) study, most patients who had residual disease after surgery were treated with high-dose proton therapy followed by a carbon-ion boost; this strategy seems effective in the short term. In another Phase I/II carbon ion dose-escalation trial, Mizoe et al. [27] observed the median OS of AA patients was 35 months, and that of GBM patients was 17 months (p = 0.0035). The median PFS of GBM was 4 months for the low-dose group and 7 and 14 months for the middle-dose and high-dose groups, respectively. The univariate and multivariate analyses of prognostic factors of GBM patients showed that high-dose carbon ion groups had significantly better OS than middle or low-dose groups. Although the number of cases in this series was limited, the median overall survival of patients with WHO grade III and IV gliomas were 35 and 17 months, respectively, which appears to be favorable. To avoid severe and unacceptable radiation toxicity to normal brain tissue, the T2 high-signal area of MRI was treated with photons rather than carbon ions, whose effect was unknown. (Because there had been no research with a clinical application of carbon ions for the treatment of human brain tumors before this study).
With the two main advantages of the heavy particle beam, the adverse effects simultaneously become concerning. Even with high-dose carbon-ion irradiation, triple modalities paired with photon, ACNU, and Carbon ion boost are safe for normal brain tissue. Nonhematologic side effects were uncommon, and there were no Grade III or IV reactions in the brain (the ACNU chemotherapy regime probably caused hematologic toxicities). Because of severe hematological toxicity in patients, ACNU has not been recommended as a chemotherapy guideline. Furthermore, the ineffectiveness of ACNU is most likely due to dosage limitations and the blood–brain barrier [27, 28]. The observation, in particular, was that brain necrosis in the target region using magnetic resonance imaging was only restricted to perilesional necrosis. The symptoms of headache and fatigue in this study are prevalent side effects [29, 30]. According to this Phase I/II trial, carbon ion radiation is safe for normal brain tissues. It would provide a basis for treating gliomas with carbon ion beams. The next phase clinical trial consisting of a carbon ion beam will continue to be conducted. However, a slightly different result from Kong et al. [25] showed 11 patients experienced grade I–II late side effects of radiation-induced brain necrosis after the completion of particle therapy. The late effect of CIRT on brain tissue is unknown due to the short follow-up period. It is difficult to distinguish between brain necrosis and pseudoprogression after radiation in the short term [31,32,33]. The issue of CIRT-induced brain necrosis cannot be overlooked. Hasegawa et al. [34] reported that severe late toxicities in the normal brain occurred after irradiation with CIRT alone (55.2 GyE in 24 fractions). High biological effectiveness results in significant cell-killing outcomes, however, such properties might cause severe irreversible organ dysfunction. Alopecia, along with other acute toxicities such as dermatitis, is a common and reversible symptom. The lack of severe acute side-effects has shown the potential safety of the carbon ion beam. These findings are significantly important for carbon ion beam to corroborate the physical advantages, which could reduce side effects compared to conventional radiation. The neurocognitive function should also be better preserved, in particular in patients without MRI changes like brain necrosis and cerebral edema. But these main complications of intracranial irradiation are not reported after using carbon ion therapy. Bevacizumab, steroid agents, or mannitol could alleviate brain edema generated by radiotherapy [35]. Evaluating neurocognitive function and quality of life (QoL) with ion-radiotherapy might be a direction of research. Still, the poor prognosis of HGGs seemingly impedes long-term follow-up.
Protons have physical features similar to carbon ion beams; however, their biological efficiency is inferior to that of heavy particles, which are roughly 1.1–1.2 equivalent to photons [8, 36, 37]. The role of proton therapy remains controversial due to its efficacy and high cost. Several institutes conducted a series of investigations on clinical trials involving protons, either alone or in combination with photon techniques. Vora et al. reported the outcomes of the high-grade gliomas treated with proton therapy. The treatment was well-tolerated, and the survival rates were comparable to previous photon-based therapy [10]. The short-term toxicities caused by proton therapy were mainly alopecia, headache, or fatigue. These common side-effects following proton therapy were the same as low-grade gliomas or other intracranial tumors [38,39,40]. In a phase II trial by Brown et al. [12], there was no indication of improved survival outcomes with proton therapy compared to IMRT. But adverse reactions have been slightly reduced by proton therapy. According to dosimetry analysis, proton significantly reduced the minimum, average, and maximum dose for organ-at-risks. The physical properties of the proton beam seem to protect normal structures and reduce toxicity. Previous studies have found that intensity-modulated proton therapy (IMPT) can provide more conformal target coverage than IMRT [19, 41]. Similar outcomes with other malignant tumors found less toxicity after proton therapy than IMRT [42,43,44,45]. The different survival outcomes have not been produced by the same radiation dose of the two techniques, so the dose-escalation model for proton therapy will be applied to more prospective research. A promising prospective randomized study (NCT02179086) compared dose-escalated protons to photons for GBM [46] (refer to Table 5).
The current standard of care for high-grade glioma (HGG) patients with photon therapy remains unsatisfactory. The pattern of treatment failure is mainly recurrence in the local region, which is an intractable problem with poor treatment outcomes. Long-term local control for most remains elusive, and local recurrence within 2 cm of the residual cavity is inevitable [26, 47]. McDonald et al. reported that 93% of patients had a central or in-field recurrence after standard care of photon therapy (total dose 60 Gy) plus temozolomide. Novel approaches may increase the target dose intensity while normal brain tissues are spared. Dose-escalation applied for proton boost in previous studies (developed by Fitzek et al. [15]) provided new insights on improving tumor control rates. The escalation of the dose to 90 CGE with a combination of photons and protons boost improved the local control of HGGs. The 2-year OS% and mOS were 34% and 20 months, respectively [15]. The recurrent region is often in the periphery of this 90 CGE volume (frequently observed in regions that received ≤ 60-70CGE). Therefore, the core technical challenge is accompanied by an increase in the target dose, limited by radiation brain necrosis. Although the standard plan was not agreed upon at that time, the innovative dose-escalation referred to some phenomenon in which radiation necrosis survived significantly longer than patients with recurrence (p = 0.01). But the patients endured repeated operations and continuing medical treatment owing to radiation necrosis or recurrence. The use of hyper-fractionation theoretically benefits a large total radiation dose without excessive late toxicity. It has been investigated in many clinical trials involving a wide range of tumor types [48, 49]. Mizumoto et al. [17] evaluated the survival of GBM patients after hyper-fractionated concomitant X-ray and proton boost (more than 6 h after conventional radiation therapy). Total doses of 96.6 GyE in 56 fractions can effectively suppress GBM growth. The area irradiated with > 90 GyE had great local control, while local recurrence was observed in areas which received less than 73.5GyE. Although the physical properties of the proton beam allow dose-escalation radiation on target, brain necrosis is inevitable. In this trial, brain necrosis occurs later than tumor recurrence. The radiation necrosis was observed in 6(26%) of 23 patients; moreover, all the patients (100%) experienced brain necrosis, according to Fitzek et al. [15]. But overall survival in patients with brain necrosis was significantly greater than that of those with tumor recurrence. The same findings that patients with necrosis treated by standard therapy followed by necrotomy had improved overall survival compared to those with tumor recurrence are reported by Rusthoven et al. [50]. Radiation necrosis has often been treated by necrotomy, drugs, hyperbaric oxygen therapy, etc. Recently, some researchers have found that bevacizumab is an effective treatment for radiation necrosis [51, 52]. Two patients treated with bevacizumab in hyper-fractioned proton trial showed favorable responses, relieving the clinical symptoms. Overall, high-dose proton therapy (96.6 GyE) is a potential way to improve local control. Moreover, prolonged hospitalization greatly strains medical resources, perhaps making it difficult to apply into practice.
X-radiation followed by proton radiotherapy as a sequential boost is also a treatment of HGGs. A retrospective study was undertaken at Heidelberg Ion-Beam Therapy Center, comparing sequential proton boost after standard chemoradiation with photon-based concurrent radio-chemotherapy to analyze the feasibility and safety [14]. The median PFS and OS in both treatment groups were comparable, and there were no discrepancies in the historical data [10]. In terms of adverse effects, proton boost was at the very least potentially better than typical standard schemes [10]. Compared with the foregoing carbon ion boost from the SPHIC study, the biological benefits of heavy particles appear to be greater than those of proton boost therapy. A prospective CLEOPATRA trial (NCT01165671) is in progress in patients with glioblastoma to compare the impact of a carbon-ion boost with a proton boost using IMRT [53] (refer to Table 5). Proton or carbon-ion boost is given to macroscopic residuals for patients after surgery. Whether this method could maximize efficacy, we look forward to releasing the results of this study online.
In summary, eight clinical trials regarding charged-particle therapy for high-grade gliomas involved carbon-ion boost combined with proton or photon, proton alone, dose-escalation of proton as boost, and proton boost therapy. All the techniques show favorable treatment-response with controllable toxicity. In comparison with IMRT, proton alone therapy might not have good survival outcomes and local tumor control advantages. Although salvage therapies are effective, dose-escalation of proton as boost produced radiation necrosis. In the future, amino acid positron emission tomography (PET) with 11C-methionine (MET) or 18F-fluoroethyltyrosine (FET) could be more widely used for target delineation to improve the accuracy of radiation areas. Proton therapy as sequential boost is inferior to carbon ion boost in terms of biological effects, but more prospective trials are needed to carry it out.
This systematic review summarizes the dosimetry advantages of protons over all types of photon techniques to provide precision options. In addition, the analysis of novel charged particle measures can contribute to practical applications. Three articles were used to obtain the parameters of the target dosimetry between protons and photons. When an intensity-modulated proton beam (known as a pencil beam or active scattering) as a novel mode of proton therapy is applied to these three dosimetry studies, it allows for a high-quality target plan that optimizes dose distributions. However, the evaluation criterion could not reach consistency among these plans. It is now generally accepted that the homogeneity index and conformity index are used to compare target dosimetry [54,55,56,57,58]. Overall, homogeneity was significantly improved with protons, regardless of the tumor treatment plan [59,60,61,62,63,64]. Similarly, Adeberg et al. [18] discovered that the HI was high for the proton, and other parameters for evaluating CTV coverage were not different, except that Dmin was shown to be higher in proton plans compared to others. All three modalities were comparable to CTV coverage. Considering that dose coverage and distribution were difficult to distinguish particularly when using the same prescribed dose. Dose escalation may be achieved with protons. Another reason for this might be that the radiation therapist tended to spare important OARs in photons if they were in proximity to the target, as depicted by the high CTV Dmin using protons. For other parameters including PTV coverage, R30, or ODV, it was illustrated that proton techniques produced more conformal target doses than photon techniques. Previous studies drew the same conclusions as well [65,66,67,68].
Dosimetry assessment of OARs for charged particle therapy is important. Adverse reactions related to the quality of life or neurocognitive function in patients need to be considered, not merely survival rates. The physical properties of charged particles seem to decrease the exposed volume of normal tissue [69,70,71,72]. Dose assessment of main intracranial OARs was classified by functions, including sensory (optic nerve, chiasm, lens, etc.), endocrine (hypothalamic-pituitary axis), neurocognition system (hippocampus, SVZ, whole brain). In our analysis of dosimetry data of OARs, the benefits of protons are clear in terms of sparing normal contralateral brain tissues. Proton therapy significantly reduced the contralateral Dmean, Dmax, and integral dose in the optic nerve, brainstem, hippocampus, and other brain regions. Similar studies have also reported that reducing radiation exposure in protons resulted in cerebral OARs, particularly in contralateral non-target normal tissues [70, 73]. Therefore, the decreased risk of radiation-related side effects makes it possible to treat patients with proton beam.
This systematic review has several limitations. First, due to the scarcity of multi-institutional randomized controlled trials (RCTs), all clinical trials involved appear to be of low quality. Furthermore, the small sample size and short-term follow-up period made it difficult to accurately observe the course of treatment outcomes. Second, every concrete charged particle technique applied in clinical studies failed to reach a consistent standard. For example, carbon ion boost used at two different institutes as a treatment measure with various dose fractions or dose intensities is difficult to compare with other techniques. Third, some studies did not adhere to the guidelines for standard treatment, particularly in terms of tumor resection or the administration of chemotherapeutic agents. These factors would an explicit effect on the treatment efficacy. Moreover, more prospective trials regarding dosimetry comparison of charged particles and photon therapy should be taken further into consideration. Finally, the O6methylguanine-DNA methyltransferase status and IDH mutation were not assessed in the majority of research. Alterations to these molecular levels are needed. Three prospective trials (NCT01358058, NCT03180502, NCT02797366, sponsored by NRG Oncology, Sweden and the United States) are conducted regarding proton therapy treating WHO grade 3 glioma with different molecular pathology (IDH1 mutation or 1p/19q codeletion) (see Table 5). This will bring us new ideas to guide different types of patients to benefit from treatment (Table 6).
In conclusion, the use of charged particle radiotherapy seems to be effective with acceptable adverse effects when used either alone or as a boost. To date, no adequate evidence validates which protocol is much more effective. However, survival outcomes show that carbon ion boost is seemingly superior to proton boost concerning biological effects. In terms of toxicity, the side effects of carbon ion and proton therapy could be accepted. Still, the way of dose-escalation as proton boost occurs, brain necrosis should not be overlooked, despite the survival rates improving. The proton beam could provide good target coverage, and it seems to reduce dose exposure to contralateral OARs significantly. This can potentially reduce the dose- and volume-related side effects of treatment, such as neurocognitive impairment, in long-term survivors. Furthermore, high-quality RCTs should be conducted in the future. Moreover, systemic therapy options combined with charged particles are necessary.
Abbreviations
- RBE:
-
Relative biological effectiveness
- PROSPERO:
-
Prospective register of systematic reviews
- HGGs:
-
High-grade gliomas
- GBM:
-
Glioblastoma multiforme
- AA:
-
Anaplastic astrocytoma
- OS:
-
Overall survival
- PFS:
-
Progression-free survival
- ACNU:
-
Nimustine hydrochloride
- GyE:
-
Gray equivalent
- IMRT:
-
Intensity-modulated radiation
- PTV:
-
Plan target volume
- GTV:
-
Gross target volume
- CGE:
-
Cobalt gray equivalent
- VMAT:
-
Volumetric modulated arc therapy
References
Ostrom QT, Gittleman H, Liao P, Vecchione-Koval T, Wolinsky Y, Kruchko C, et al. CBTRUS Statistical Report: primary brain and other central nervous system tumors diagnosed in the United States in 2010–2014. Neuro-oncology (2017) 19(suppl_5):v1-v88. doi: https://doi.org/10.1093/neuonc/nox158.
Ostrom QT, Bauchet L, Davis FG, Deltour I, Fisher JL, Langer CE, et al. The epidemiology of glioma in adults: a “state of the science” review. Neuro Oncol. 2014;16(7):896–913. https://doi.org/10.1093/neuonc/nou087.
Wesseling P, Capper D. WHO 2016 classification of gliomas. Neuropathol Appl Neurobiol. 2018;44(2):139–50. https://doi.org/10.1111/nan.12432.
Schlaich F, Brons S, Haberer T, Debus J, Combs SE, Weber KJ. Comparison of the effects of photon versus carbon ion irradiation when combined with chemotherapy in vitro. Radiat Oncol. 2013;8:260. https://doi.org/10.1186/1748-717x-8-260.
Buglewicz DJ, Banks AB, Hirakawa H, Fujimori A, Kato TA. Monoenergetic 290 MeV/n carbon-ion beam biological lethal dose distribution surrounding the Bragg peak. Sci Rep. 2019;9(1):6157. https://doi.org/10.1038/s41598-019-42600-4.
Tsuboi K, Moritake T, Tsuchida Y, Tokuuye K, Matsumura A, Ando K. Cell cycle checkpoint and apoptosis induction in glioblastoma cells and fibroblasts irradiated with carbon beam. J Radiat Res. 2007;48(4):317–25. https://doi.org/10.1269/jrr.06081.
Combs SE, Bohl J, Elsasser T, Weber KJ, Schulz-Ertner D, Debus J, et al. Radiobiological evaluation and correlation with the local effect model (LEM) of carbon ion radiation therapy and temozolomide in glioblastoma cell lines. Int J Radiat Biol. 2009;85(2):126–37. https://doi.org/10.1080/09553000802641151.
Underwood TS, McMahon SJ. Proton relative biological effectiveness (RBE): a multiscale problem. Br J Radiol. 2019;92(1093):20180004. https://doi.org/10.1259/bjr.20180004.
Stupp R, Hegi ME, Mason WP, van den Bent MJ, Taphoorn MJ, Janzer RC, et al. Effects of radiotherapy with concomitant and adjuvant temozolomide versus radiotherapy alone on survival in glioblastoma in a randomised phase III study: 5-year analysis of the EORTC-NCIC trial. Lancet Oncol. 2009;10(5):459–66. https://doi.org/10.1016/s1470-2045(09)70025-7.
Stupp R, Mason WP, van den Bent MJ, Weller M, Fisher B, Taphoorn MJ, et al. Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N Engl J Med. 2005;352(10):987–96. https://doi.org/10.1056/NEJMoa043330.
Vora SA, Gondi V, Tseng YD, Vargas CE, Larson GL, Tsai HK, et al. Safety and Efficacy of proton beam therapy for high-grade glioma: initial report from the Proton Collaborative Group (PCG). Int J of Radiat Oncol Biol Phys (2018) 102(3):E362-E. https://doi.org/10.1016/j.ijrobp.2018.07.1089.
Brown PD, Chung C, Liu DD, McAvoy S, Grosshans D, Al Feghali K, et al. A Prospective phase II randomized trial of proton radiotherapy vs. intensity modulated radiotherapy for patients with newly diagnosed glioblastoma. Neuro-Oncol (2021). https://doi.org/10.1093/neuonc/noab040.
Tsujii H, Tsuji H, Inada T, Maruhashi A, Hayakawa Y, Takada Y, et al. Clinical-results of fractionated proton therapy. Int J Radiat Oncol Biol Phys. 1993;25(1):49–60. https://doi.org/10.1016/0360-3016(93)90144-k.
Adeberg S, Bernhardt D, Ben Harrabi S, Uhl M, Paul A, Bougatf N, et al. Sequential proton boost after standard chemoradiation for high-grade glioma. Radiother Oncol. 2017;125(2):266–72. https://doi.org/10.1016/j.radonc.2017.09.040.
Fitzek MM, Thornton AF, Rabinov JD, Lev MH, Pardo FS, Munzenrider JE, et al. Accelerated fractionated proton/photon irradiation to 90 cobalt gray equivalent for glioblastoma multiforme: results of a phase II prospective trial. J Neurosurg. 1999;91(2):251–60. https://doi.org/10.3171/jns.1999.91.2.0251.
Mizumoto M, Yamamoto T, Ishikawa E, Matsuda M, Takano S, Ishikawa H, et al. Proton beam therapy with concurrent chemotherapy for glioblastoma multiforme: comparison of nimustine hydrochloride and temozolomide. J Neurooncol. 2016;130(1):165–70. https://doi.org/10.1007/s11060-016-2228-4.
Mizumoto M, Yamamoto T, Takano S, Ishikawa E, Matsumura A, Ishikawa H, et al. Long-term survival after treatment of glioblastoma multiforme with hyperfractionated concomitant boost proton beam therapy. Pract Radiat Oncol. 2015;5(1):e9-16. https://doi.org/10.1016/j.prro.2014.03.012.
Adeberg S, Harrabil SB, Bougatf N, Bernhardt D, Rieber J, Koerber SA, et al. Intensity-modulated proton therapy, volumetric-modulated arc therapy, and 3D conformal radiotherapy in anaplastic astrocytoma and glioblastoma. Strahlenther Onkol. 2016;192(11):770–9. https://doi.org/10.1007/s00066-016-1007-7.
Rosenschold P, Engelholm S, Ohlhues L, Law I, Vogelius I, Engelholm SA. Photon and proton therapy planning comparison for malignant glioma based on CT, FDG-PET DTI-MRI and fiber tracking. Acta Oncol. 2011;50(6):777–83. https://doi.org/10.3109/0284186x.2011.584555.
Holm AIS, Petersen JBB, Muren LP, Seiersen K, Borghammer P, Lukacova S. Functional image-guided dose escalation in gliomas using of state-of-the-art photon vs. proton therapy. Acta Oncol (Stockholm, Sweden) 2017;56(6):826–31. https://doi.org/10.1080/0284186x.2017.1285498.
Tan AC, Ashley DM, López GY, Malinzak M, Friedman HS, Khasraw M. Management of glioblastoma: state of the art and future directions. CA 2020;70(4):299–312. https://doi.org/10.3322/caac.21613.
Athanassiou H, Synodinou M, Maragoudakis E, Paraskevaidis M, Verigos C, Misailidou D, et al. Randomized phase II study of temozolomide and radiotherapy compared with radiotherapy alone in newly diagnosed glioblastoma multiforme. J Clin Oncol. 2005;23(10):2372–7. https://doi.org/10.1200/jco.2005.00.331.
Kusumawidjaja G, Gan PZH, Ong WS, Teyateeti A, Dankulchai P, Tan DYH, et al. Dose-escalated intensity-modulated radiotherapy and irradiation of subventricular zones in relation to tumor control outcomes of patients with glioblastoma multiforme. Onco Targets Ther. 2016;9:1115–22. https://doi.org/10.2147/ott.S96509.
Shah JL, Li G, Shaffer JL, Azoulay MI, Gibbs IC, Nagpal S, et al. Stereotactic radiosurgery and hypofractionated radiotherapy for glioblastoma. Neurosurgery. 2018;82(1):24–34. https://doi.org/10.1093/neuros/nyx115.
Kong L, Wu JS, Gao J, Qiu XX, Yang J, Hu J, et al. Particle radiation therapy in the management of malignant glioma: early experience at the Shanghai Proton and Heavy Ion Center. Cancer. 2020;126(12):2802–10. https://doi.org/10.1002/cncr.32828.
Mallick S, Benson R, Hakim A, Rath GK. Management of glioblastoma after recurrence: a changing paradigm. J Egypt Natl Cancer Inst. 2016;28(4):199–210. https://doi.org/10.1016/j.jnci.2016.07.001.
Mizoe JE, Tsujii H, Hasegawa A, Yanagi T, Takagi R, Kamada T, et al. Phase I/II clinical trial of carbon ion radiotherapy for malignant gliomas: combined X-ray radiotherapy, chemotherapy, and carbon ion radiotherapy. Int J Radiat Oncol Biol Phys. 2007;69(2):390–6. https://doi.org/10.1016/j.ijrobp.2007.03.003.
Wang Y, Chen X, Zhang Z, Li S, Chen B, Wu C, et al. Comparison of the clinical efficacy of temozolomide (TMZ) versus nimustine (ACNU)-based chemotherapy in newly diagnosed glioblastoma. Neurosurg Rev. 2014;37(1):73–8. https://doi.org/10.1007/s10143-013-0490-x.
Lawrie TA, Gillespie D, Dowswell T, Evans J, Erridge S, Vale L, et al. Long-term neurocognitive and other side effects of radiotherapy, with or without chemotherapy, for glioma. Cochrane Database Syst Rev 2019;8(8):Cd013047. https://doi.org/10.1002/14651858.CD013047.pub2.
Tabrizi S, Yeap BY, Sherman JC, Nachtigall LB, Colvin MK, Dworkin M, et al. Long-term outcomes and late adverse effects of a prospective study on proton radiotherapy for patients with low-grade glioma. Radiother Oncol. 2019;137:95–101. https://doi.org/10.1016/j.radonc.2019.04.027.
Strauss SB, Meng A, Ebani EJ, Chiang GC. Imaging glioblastoma posttreatment: progression, pseudoprogression, pseudoresponse, radiation necrosis. Radiol Clin N Am. 2019;57(6):1199–216. https://doi.org/10.1016/j.rcl.2019.07.003.
Knudsen-Baas KM, Moen G, Fluge Ø, Storstein A. Pseudoprogression in high-grade glioma. Acta Neurol Scand Suppl. 2013;196:31–7. https://doi.org/10.1111/ane.12047.
Zikou A, Sioka C, Alexiou GA, Fotopoulos A, Voulgaris S, Argyropoulou MI. Radiation necrosis, pseudoprogression, pseudoresponse, and tumor recurrence: imaging challenges for the evaluation of treated gliomas. Contrast Media Mol Imaging. 2018;2018:6828396. https://doi.org/10.1155/2018/6828396.
Hasegawa A, Mizoe JE, Tsujii H, Kamada T, Jingu K, Iwadate Y, et al. Experience with carbon ion radiotherapy for WHO Grade 2 diffuse astrocytomas. Int J Radiat Oncol Biol Phys. 2012;83(1):100–6. https://doi.org/10.1016/j.ijrobp.2011.06.1952.
Zhuang H, Shi S, Yuan Z, Chang JY. Bevacizumab treatment for radiation brain necrosis: mechanism, efficacy and issues. Mol Cancer. 2019;18(1):21. https://doi.org/10.1186/s12943-019-0950-1.
Khachonkham S, Mara E, Gruber S, Preuer R, Kuess P, Dörr W, et al. RBE variation in prostate carcinoma cells in active scanning proton beams: In-vitro measurements in comparison with phenomenological models. Physica Med. 2020;77:187–93. https://doi.org/10.1016/j.ejmp.2020.08.012.
Paganetti H. Relative biological effectiveness (RBE) values for proton beam therapy. Variations as a function of biological endpoint, dose, and linear energy transfer. Phys Med Biol 2014;59(22):R419–72. https://doi.org/10.1088/0031-9155/59/22/r419.
Maquilan G, Grover S, Alonso-Basanta M, Lustig RA. Acute toxicity profile of patients with low-grade gliomas and meningiomas receiving proton therapy. Am J Clin Oncol. 2014;37(5):438–43. https://doi.org/10.1097/COC.0b013e31827de86b.
Hauswald H, Rieken S, Ecker S, Kessel KA, Herfarth K, Debus J, et al. First experiences in treatment of low-grade glioma grade I and II with proton therapy. Radiat Oncol (London, England). 2012;7:189. https://doi.org/10.1186/1748-717x-7-189.
Song J, Aljabab S, Abduljabbar L, Tseng YD, Rockhill JK, Fink JR, et al. Radiation-induced brain injury in patients with meningioma treated with proton or photon therapy. J Neurooncol. 2021;153(1):169–80. https://doi.org/10.1007/s11060-021-03758-y.
Adeberg S, Harrabi SB, Bougatf N, Verma V, Windisch P, Bernhardt D, et al. Dosimetric comparison of proton radiation therapy, volumetric modulated arc therapy, and three-dimensional conformal radiotherapy based on intracranial tumor location. Cancers 2018. https://doi.org/10.3390/cancers10110401.
Lin SH, Hobbs BP, Verma V, Tidwell RS, Smith GL, Lei X, et al. Randomized Phase IIB trial of proton beam therapy versus intensity-modulated radiation therapy for locally advanced esophageal cancer. J Clin Oncol. 2020;38(14):1569–79. https://doi.org/10.1200/jco.19.02503.
Milby AB, Both S, Ingram M, Lin LL. Dosimetric comparison of combined intensity-modulated radiotherapy (IMRT) and proton therapy versus IMRT alone for pelvic and para-aortic radiotherapy in gynecologic malignancies. Int J Radiat Oncol Biol Phys. 2012;82(3):e477–84. https://doi.org/10.1016/j.ijrobp.2011.07.012.
Moreno AC, Frank SJ, Garden AS, Rosenthal DI, Fuller CD, Gunn GB, et al. Intensity modulated proton therapy (IMPT)—the future of IMRT for head and neck cancer. Oral Oncol. 2019;88:66–74. https://doi.org/10.1016/j.oraloncology.2018.11.015.
Zou Z, Bowen SR, Thomas HMT, Sasidharan BK, Rengan R, Zeng J. Scanning beam proton therapy versus photon IMRT for stage III lung cancer: comparison of dosimetry, toxicity, and outcomes. Adv Radiat Oncol. 2020;5(3):434–43. https://doi.org/10.1016/j.adro.2020.03.001.
Mizumoto M, Tsuboi K, Igaki H, Yamamoto T, Takano S, Oshiro Y, et al. Phase I/II trial of hyperfractionated concomitant boost proton radiotherapy for supratentorial glioblastoma multiforme. Int J Radiat Oncol Biol Phys. 2010;77(1):98–105. https://doi.org/10.1016/j.ijrobp.2009.04.054.
Dörner L, Mustafa A, Rohr A, Mehdorn HM, Nabavi A. Growth pattern of tumor recurrence following bis-chloroethylnitrosourea (BCNU) wafer implantation in malignant glioma. J Clin Neurosci. 2013;20(3):429–34. https://doi.org/10.1016/j.jocn.2012.01.060.
Withers HR. Biologic basis for altered fractionation schemes. Cancer. 1985;55(9 Suppl):2086–95. https://doi.org/10.1002/1097-0142(19850501)55:9+%3c2086::aid-cncr2820551409%3e3.0.co;2-1.
Ali AN, Zhang P, Yung WKA, Chen Y, Movsas B, Urtasun RC, et al. NRG oncology RTOG 9006: a phase III randomized trial of hyperfractionated radiotherapy (RT) and BCNU versus standard RT and BCNU for malignant glioma patients. J Neurooncol. 2018;137(1):39–47. https://doi.org/10.1007/s11060-017-2558-x.
Rusthoven KE, Olsen C, Franklin W, Kleinschmidt-DeMasters BK, Kavanagh BD, Gaspar LE, et al. Favorable prognosis in patients with high-grade glioma with radiation necrosis: the University of Colorado reoperation series. Int J Radiat Oncol Biol Phys. 2011;81(1):211–7. https://doi.org/10.1016/j.ijrobp.2010.04.069.
Furuse M, Nonoguchi N, Kawabata S, Yoritsune E, Takahashi M, Inomata T, et al. Bevacizumab treatment for symptomatic radiation necrosis diagnosed by amino acid PET. Jpn J Clin Oncol. 2013;43(3):337–41. https://doi.org/10.1093/jjco/hys231.
Zhuang H, Yuan X, Zheng Y, Li X, Chang JY, Wang J, et al. A study on the evaluation method and recent clinical efficacy of bevacizumab on the treatment of radiation cerebral necrosis. Sci Rep. 2016;6:24364. https://doi.org/10.1038/srep24364.
Combs SE, Kieser M, Rieken S, Habermehl D, Jäkel O, Haberer T, et al. Randomized phase II study evaluating a carbon ion boost applied after combined radiochemotherapy with temozolomide versus a proton boost after radiochemotherapy with temozolomide in patients with primary glioblastoma: the CLEOPATRA trial. BMC Cancer. 2010;10:478. https://doi.org/10.1186/1471-2407-10-478.
Yoon M, Park SY, Shin D, Lee SB, Pyo HR, Kim DY, et al. A new homogeneity index based on statistical analysis of the dose-volume histogram. J Appl Clin Med Phys. 2007;8(2):9–17. https://doi.org/10.1120/jacmp.v8i2.2390.
Kataria T, Sharma K, Subramani V, Karrthick KP, Bisht SS. Homogeneity Index: An objective tool for assessment of conformal radiation treatments. J Med Phys. 2012;37(4):207–13. https://doi.org/10.4103/0971-6203.103606.
Thieme AH, Stromberger C, Ghadjar P, Piper SK, Budach V. A novel voxel based homogeneity index: rationale and clinical implications for whole-brain radiation therapy. Radiother Oncol. 2018;128(2):229–35. https://doi.org/10.1016/j.radonc.2018.04.007.
Paddick I. A simple scoring ratio to index the conformity of radiosurgical treatment plans. Technical note. J Neurosurg. 2000;93(Suppl 3):219–22. https://doi.org/10.3171/jns.2000.93.supplement.
Howell RM, Giebeler A, Koontz-Raisig W, Mahajan A, Etzel CJ, D’Amelio AM Jr, et al. Comparison of therapeutic dosimetric data from passively scattered proton and photon craniospinal irradiations for medulloblastoma. Radiat Oncol (London, England). 2012;7:116. https://doi.org/10.1186/1748-717x-7-116.
Mondlane G, Gubanski M, Lind PA, Henry T, Ureba A, Siegbahn A. Dosimetric comparison of plans for photon- or proton-beam based radiosurgery of liver metastases. Int J Part Ther. 2016;3(2):277–84. https://doi.org/10.14338/ijpt-16-00010.1.
Paudel NR, Narayanasamy G, Han EY, Penagaricano J, Mavroidis P, Zhang X, et al. Dosimetric and radiobiological comparison for quality assurance of IMRT and VMAT plans. J Appl Clin Med Phys. 2017;18(5):237–44. https://doi.org/10.1002/acm2.12145.
Haefner MF, Verma V, Bougatf N, Mielke T, Tonndorf-Martini E, König L, et al. Dosimetric comparison of advanced radiotherapy approaches using photon techniques and particle therapy in the postoperative management of thymoma. Acta Oncol (Stockholm, Sweden). 2018;57(12):1713–20. https://doi.org/10.1080/0284186x.2018.1502467.
Hirano Y, Onozawa M, Hojo H, Motegi A, Zenda S, Hotta K, et al. Dosimetric comparison between proton beam therapy and photon radiation therapy for locally advanced esophageal squamous cell carcinoma. Radiat Oncol (London, England). 2018;13(1):23. https://doi.org/10.1186/s13014-018-0966-5.
Carbonara R, Di Rito A, Monti A, Rubini G, Sardaro A. Proton versus photon radiotherapy for pediatric central nervous system malignancies: a systematic review and meta-analysis of dosimetric comparison studies. J Oncol. 2019;2019:5879723. https://doi.org/10.1155/2019/5879723.
Poel R, Stuessi Lobmaier A, Andratschke N, Unkelbach J, Tanadini-Lang S, Guckenberger M, et al. Dosimetric comparison of protons vs photons in re-irradiation of intracranial meningioma. Br J Radiol. 2019;92(1100):20190113. https://doi.org/10.1259/bjr.20190113.
Hoffmann L, Alber M, Jensen MF, Holt MI, Møller DS. Adaptation is mandatory for intensity modulated proton therapy of advanced lung cancer to ensure target coverage. Radiother Oncol. 2017;122(3):400–5. https://doi.org/10.1016/j.radonc.2016.12.018.
Lens E, Jagt TZ, Hoogeman MS, Schaart DR. Correlations between the shifts in prompt gamma emission profiles and the changes in daily target coverage during simulated pencil beam scanning proton therapy. Phys Med Biol 2019;64(8):085009. https://doi.org/10.1088/1361-6560/ab145e.
Su Z, Slopsema R, Flampouri S, Li Z. Impact of intrafraction prostate motion on clinical target coverage in proton therapy: a simulation study of dosimetric differences in two delivery techniques. J Appl Clin Med Phys. 2019;20(10):67–73. https://doi.org/10.1002/acm2.12714.
Vargas C, Wagner M, Mahajan C, Indelicato D, Fryer A, Falchook A, et al. Proton therapy coverage for prostate cancer treatment. Int J Radiat Oncol Biol Phys. 2008;70(5):1492–501. https://doi.org/10.1016/j.ijrobp.2007.09.001.
Mohan R, Grosshans D. Proton therapy—Present and future. Adv Drug Deliv Rev. 2017;109:26–44. https://doi.org/10.1016/j.addr.2016.11.006.
Dionisi F, Fiorica F, D’Angelo E, Maddalo M, Giacomelli I, Tornari E, et al. Organs at risk’s tolerance and dose limits for head and neck cancer re-irradiation: a literature review. Oral Oncol. 2019;98:35–47. https://doi.org/10.1016/j.oraloncology.2019.08.017.
Raptis A, Ödén J, Ardenfors O, Flejmer AM, Toma-Dasu I, Dasu A. Cancer risk after breast proton therapy considering physiological and radiobiological uncertainties. Physica Med. 2020;76:1–6. https://doi.org/10.1016/j.ejmp.2020.06.012.
Vaios EJ, Wo JY. Proton beam radiotherapy for anal and rectal cancers. J Gastrointest Oncol. 2020;11(1):176–86. https://doi.org/10.21037/jgo.2019.04.03.
Taphoorn MJ, Heimans JJ, van der Veen EA, Karim AB. Endocrine functions in long-term survivors of low-grade supratentorial glioma treated with radiation therapy. J Neurooncol. 1995;25(2):97–102. https://doi.org/10.1007/bf01057753.
Acknowledgements
Not applicable.
Funding
This study was supported by National Key Research and Development Plan Project (No. 2022YFC2401505); Talent innovation and venture project of Lanzhou city (No.2021-RC-125); Key R&D Program of Science and Technology Department of Gansu Province (No.20YF8FA116); The authorized project of Lanzhou KejinTaiji Corporation, Ltd. (No. BMP-B-02-002).
Author information
Authors and Affiliations
Contributions
Conception and design: X-HW, R-FL, K-HY and, Y-HW. Search and collection of data: Y-HW, R-FL M-D, D-DW, J-RC. Data analysis and interpretation: Y-HW, Y-HO, Q-NZ, H-TL Manuscript writing: Y-HW, R-FL, M-D. All authors contributed to the article and approved the submitted version.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential competing interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Wang, Y., Liu, R., Zhang, Q. et al. Charged particle therapy for high-grade gliomas in adults: a systematic review. Radiat Oncol 18, 29 (2023). https://doi.org/10.1186/s13014-022-02187-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13014-022-02187-z