Abstract
Background
Systemic response to local anticancer treatment is a phenomenon called ‘abscopal effect’. The immune system is thought to play a pivotal role in its occurrence. To date, several cases have been reported, particularly in patients receiving combined local treatment and immune checkpoint inhibitors. In such cases, it is impossible to discriminate between the effects of local and systemic treatment. Only a few cases of abscopal effect have been described with radiotherapy alone.
Case presentation
Here, we report on the case of an 81-year-old woman with recurrent metastatic squamous cell carcinoma of the lung with mediastinal tumor bulk, lymph node and bone metastases. The patient refused to undergo systemic treatment, and palliative stereotactic radiotherapy of the mediastinal tumor was performed. At restaging with FDG-PET/CT, the patient presented with a decrease in size and FDG-avidity both of the irradiated site and of the lymph node and bone metastases (which did not receive radiotherapy). At 25 months after radiotherapy, the patient is still in remission at all sites.
Conclusions
This is a rare case of an abscopal effect after radiotherapy as monotherapy. It is one of the few hitherto reported for lung cancer. Several ongoing studies with a combination of radiotherapy and immunotherapy are seeking to exploit a potential synergy to induce abscopal effects.
Similar content being viewed by others
Background
The term ‘abscopal effect’ refers to the observation of a systemic effect on metastases after local intervention to one of the lesions [1]. Although radiotherapy is a local treatment, it is capable of inducing abscopal effect, as demonstrated by a limited number of cases [2,3,4]. Evidence from studies on the effect of radiotherapy on cancer immune response suggests the following mechanism for the abscopal effect: tumor cell destruction by irradiation promotes tumor antigen release and their presentation by antigen presenting cells; this in turn leads to an activation and expansion of antitumor lymphocytes that recognize and eliminate tumor cells even in distant metastases [5]. The elaborate work by Demaria and colleagues provided preclinical evidence. They treated mice bearing syngeneic bilateral mamma carcinoma with Flt3-Ligand to enhance dendritic cell expansion and unilateral irradiation, which lead to abscopal effect in wild-type animals but not in T-cell-deficient mice [6].
Given the role of the immune system in abscopal effects and the stimulation of antitumor immune response during immunotherapy, the recent increase of reported cases of abscopal effects is not surprising [3, 7, 8]. Yet, in many cases with immune checkpoint inhibition, no clear distinction between abscopal effect versus sole effect of immunotherapy and concurrent irradiation can be made. Even if immunotherapy had been halted before initiation of radiotherapy, delayed response to immunotherapy after pseudoprogression [9] may also be a possible explanation.
Cases of abscopal effects occurring after sole radiotherapy remain extremely rare [2,3,4, 7]. Here, we describe a seldom case of abscopal effect without concurrent or past systemic cancer treatment, which represents, to the best of our knowledge, the 5th case in patients with lung cancer ever reported [10,11,12,13].
Case presentation
We report on an 81-year-old woman with no relevant comorbidities and a smoking history of 5 pack years. In 2006 she was diagnosed with a pT2a, pN0 (0/5), cM0, UICC stage IB squamous cell carcinoma of the left upper lung lobe, for which she underwent a double-sleeve lobectomy with lymphadenectomy. During 5 years of follow-up, no relapse occurred. In April 2019, the patient presented with a post-stenotic pneumonia. Computed tomography of the chest showed a mass in the left lung. Radiological staging with whole-body 18F-FDG-PET/CT and brain MRI showed metastatic disease with a strongly metabolically active primary tumor (SUVmax 16.7), pleural carcinomatosis on the left side (SUVmax 9.4), periclavicular lymph node metastases on the left side (SUVmax 9.9), and bone metastases in the 12th thoracic and 4th lumbar vertebra (SUVmax 5.0 and 4.6, respectively) (Fig. 1). Histology of bronchoscopic biopsy specimens revealed squamous cell carcinoma, which could be interpreted as recurrence or as a second lung cancer, taking into consideration the 13-year-long disease-free interval. The immunohistochemistry for programmed cell death ligand 1 (PD-L1) revealed an expression in 20% of tumor cells and in < 10% of immune cells. In order to complete our internal lung cancer diagnostic algorithm (Treichler G, manuscript in preparation), we performed next-generation sequencing using the FDA-approved FoundationOne®CDx assay. We found a structural aberration on the long arm of chromosome 3 (3q) with amplifications of the genes PIK3CA, SOX2, and FGF12; mutations of TP53, ATRX1, RB1, and, subclonally, PIK3CA; a stable microsatellite state (MSS), and a low tumor mutational burden (5 Muts/Mb).
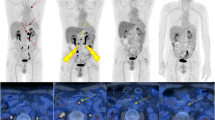
18F-FDG PET/CT images before irradiation and at 1, 3, and 6 months after completion of palliative radiotherapy (RT). a PET MIP image and b fused axial PET/CT images showing the initial stenotic pulmonary tumor bulk (red circle), the periclavicular lymph node (LN) metastases, the bone metastases in vertebrae Th12 and L4 (red arrows), and their regression over time. Further follow-up at 9, 12, and 19 months after radiotherapy showed persistent remission
Based on the recommendation by our multidisciplinary tumor board, a therapy regimen consisting of pembrolizumab, carboplatin and paclitaxel in analogy to the KEYNOTE-407 study [14] was suggested. The patient declined systemic treatment. She was thus referred for radiotherapy in order to achieve local control, due to the central localization of the tumor with associated risk of post-stenotic pneumonia and bleeding. The patient underwent conventionally fractionated radiotherapy of the principal pulmonary tumor bulk with palliative intention with 3 Gy in 12 fractions, resulting in a total dose of 36 Gy, using Volumetric Modulated Arc Therapy (VMAT, RapidArc™). Radiotherapy was well tolerated, with esophagitis grade 2 according to the Common Terminology Criteria for Adverse Events (CTCAE) version 5.0. Four weeks after the last day of radiotherapy, restaging was performed with 18F-FDG-PET/CT. A partial remission of the tumor bulk, the nodal metastases and, surprisingly, also of the vertebral lesions was shown (Fig. 1). Of note, the supraclavicular lymph nodes and the two bone metastases in the spinal column had not been included in the irradiation field with scatter doses of 0.201 Gy, 0.093 Gy, and 0.021 Gy on the lymph nodes, vertebra Th12, and L4, respectively (Fig. 2). Furthermore, no antiresorptive medication had been administered. Due to the remission and the lack of tumor-related symptoms, systemic treatment—although no longer refused by the patient—was withheld. The patient underwent radiological follow-up, during which further decrease in tumor size and complete metabolic remission of the bone, pleural and lymph node metastases was seen (Fig. 1). Currently, 25 months after radiotherapy, the patient is still free of symptoms and has an Eastern Cooperative Oncology Group (ECOG) Performance Status of 0.
Discussion and conclusions
We describe a rare case of an elderly woman with metastatic non-small cell lung cancer, whose distant metastases regressed after radiotherapy of the mediastinal tumor bulk, in the absence of systemic treatment. Recognizing the abscopal effect was crucial to prevent unnecessary systemic treatment in an asymptomatic patient with limited tumor burden, and thus avoid toxicities. In the few previously published cases of “true” abscopal effect in lung cancer [10,11,12,13], with the exception of Hamilton’s report with oligometastatic disease [11], remission was quickly followed by progression. This emphasizes the significance of the persisting long-term remission of 25 months observed in our case.
Multiple variables, such as histological subtype, number of metastases, timing of radiotherapy (concurrent vs. sequential), the volume of irradiation, the number of irradiated sites, the chosen fractionation regimen, and the applied dose are thought to influence the likeliness of an abscopal effect [1, 8]. For instance, based on preclinical data, the type of dose fractionation influences the level of antigen presentation by tumor cells, with the best results obtained with high-dose, low fractionated radiotherapy [15]. In contrast, our case suggests that conventional fractionation might as well efficiently trigger an antitumor immune response, in line with the radiation regimens used in previously reported clinical cases with abscopal effect [2, 3, 16].
Limitations of our observation include the missing histological confirmation of the metastases. However, both the radiological evaluation and the observed simultaneous remission of the lesions make alternative diagnoses unlikely. 18F-FDG PET/CT imaging has an excellent specificity (98%) for the detection of bone metastases of non-small cell lung cancer [17, 18] and our patient had no other potential cause for the initially observed FDG-avidity in the vertebrae, such as a fracture, trauma, inflammation or recent cancer treatment. All metastases were also discernable on native CT images: bone lesions were sclerotic, periclavicular lymph nodes were increased in number and roundish (Fig. 3). Furthermore, the lack of histological confirmation represents a consistent limitation in the literature on abscopal effects [10,11,12,13].
The innate and adaptive immune system plays an important role in tumor control, as demonstrated by the increased incidence of cancer in immunocompromised individuals [19]. Besides systemic immunotherapy, irradiation also stimulates the immune system [5, 6]. The combination of the two strategies, i.e., radiotherapy and immunotherapy, to enhance cancer response appears therefore promising [8, 15, 20, 21]. The PEMBRO-RT study was the first major trial to show clinical efficacy in this setting, although only in the PD-L1-negative subgroup [22]. In contrast, another recently published randomized phase 2 trial in metastatic head and neck cancer patients failed to show a benefit of simultaneous stereotactic body radiation therapy [23], but results were limited by a small study population and lack of selection according to the PD-L1 status. Multiple ongoing phase I and II clinical trials are seeking to exploit such a synergistic effect further [1, 3, 8, 24, 25]. Efficacy and safety profiles of pending trials will determine the future of this novel and exciting interdisciplinary field [26].
In conclusion, we observed a rare case of a true abscopal effect after radiotherapy as monotherapy. The approach of triggering abscopal effects should be examined further in prospective clinical trials, primarily in combination with immunotherapy.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- CTCAE:
-
Common Terminology Criteria for Adverse Events
- ECOG:
-
Eastern Cooperative Oncology Group
- FDA:
-
United States Food and Drug Administration
- 18F-FDG:
-
Fluorodeoxyglucose
- L4:
-
4th lumbar vertebra
- MIP:
-
Maximum intensity projection
- MRI:
-
Magnetic resonance imaging
- MSS:
-
Microsatellite stable
- PD-L1:
-
Programmed cell death ligand 1
- PET/CT:
-
Positron emission tomography–computed tomography
- SUVmax :
-
Maximum standardized uptake value
- Th12:
-
12th thoracic vertebra
- UICC:
-
Union for International Cancer Control
- VMAT:
-
Volumetric modulated arc therapy
References
Seiwert TY, Kiess AP. Time to debunk an urban myth? The “abscopal effect” with radiation and anti-pd-1. J Clin Oncol. 2021;39(1):1–3.
D’Andrea MA, Reddy GK. The systemic immunostimulatory effects of radiation therapy producing overall tumor control through the abscopal effect. J Radiat Oncol. 2019;8(2):143–56.
D’Andrea MA, Reddy GK. Systemic effects of radiation therapy-induced abscopal responses in patients with advanced lung cancer. Oncology. 2021;99(1):1–14.
Abuodeh Y, Venkat P, Kim S. Systematic review of case reports on the abscopal effect. Curr Probl Cancer. 2016;40(1):25–37.
Vatner RE, Cooper BT, Vanpouille-Box C, Demaria S, Formenti SC. Combinations of immunotherapy and radiation in cancer therapy. Front Oncol. 2014;4:325.
Demaria S, Ng B, Devitt ML, Babb JS, Kawashima N, Liebes L, et al. Ionizing radiation inhibition of distant untreated tumors (abscopal effect) is immune mediated. Int J Radiat Oncol Biol Phys. 2004;58(3):862–70.
Garelli E, Rittmeyer A, Putora PM, Glatzer M, Dressel R, Andreas S. Abscopal effect in lung cancer: three case reports and a concise review. Immunotherapy. 2019;11(17):1445–61.
Agrawal V, Benjamin KT, Ko EC. Radiotherapy and immunotherapy combinations for lung cancer. Curr Oncol Rep. 2021;23(1):4.
Vrankar M, Unk M. Immune RECIST criteria and symptomatic pseudoprogression in non-small cell lung cancer patients treated with immunotherapy. Radiol Oncol. 2018;52(4):365–9.
Rees GJG, Ross CMD. Abscopal regression following radiotherapy for adenocarcinoma. Br J Radiol. 1983;56(661):63–6.
Hamilton AJ, Seid J, Verdecchia K, Chuba P. Abscopal effect after radiosurgery for solitary brain metastasis from non-small cell lung cancer. Cureus. 2018;10(12):14.
Kuroda A, Tabuchi T, Iwami E, Sasahara K, Matsuzaki T, Nakajima T, et al. Abscopal effect of radiation on multiple lung metastases of lung adenocarcinoma: a case report. BMC Cancer. 2019;19:5.
Katayama K, Tamiya A, Koba T, Fukuda S, Atagi S. An abscopal response to radiation therapy in a patient with metastatic non-small cell lung cancer: a case report. J Cancer Sci Ther. 2017;9(2):365–7.
Paz-Ares L, Luft A, Vicente D, Tafreshi A, Gumus M, Mazieres J, et al. Pembrolizumab plus chemotherapy for squamous non-small-cell lung cancer. N Engl J Med. 2018;379(21):2040–51.
Herrera FG, Bourhis J, Coukos G. Radiotherapy combination opportunities leveraging immunity for the next oncology practice. Ca-a Cancer J Clin. 2017;67(1):65–85.
Reynders K, Illidge T, Siva S, Chang JY, De Ruysscher D. The abscopal effect of local radiotherapy: using immunotherapy to make a rare event clinically relevant. Cancer Treat Rev. 2015;41(6):503–10.
Liu T, Xu J-Y, Xu W, Bai Y-R, Yan W-L, Yang H-L. Fluorine-18 deoxyglucose positron emission tomography, magnetic resonance imaging and bone scintigraphy for the diagnosis of bone metastases in patients with lung cancer: which one is the best? - a meta-analysis. Clin Oncol. 2011;23(5):350–8.
Wu Y, Li P, Zhang H, Shi Y, Wu H, Zhang J, et al. Diagnostic value of fluorine 18 fluorodeoxyglucose positron emission tomography/computed tomography for the detection of metastases in non-small-cell lung cancer patients. Int J Cancer. 2013;132(2):E37–47.
Lu YC, Robbins PF. Targeting neoantigens for cancer immunotherapy. Int Immunol. 2016;28(7):365–70.
Rodriguez-Ruiz ME, Rodriguez I, Leaman O, Lopez-Campos F, Montero A, Conde AJ, et al. Immune mechanisms mediating abscopal effects in radioimmunotherapy. Pharmacol Ther. 2019;196:195–203.
Ko EC, Raben D, Formenti SC. The integration of radiotherapy with immunotherapy for the treatment of non-small cell lung cancer. Clin Cancer Res. 2018;24(23):5792–806.
Theelen W, Peulen HMU, Lalezari F, van der Noort V, de Vries JF, Aerts J, et al. Effect of pembrolizumab after stereotactic body radiotherapy vs pembrolizumab alone on tumor response in patients with advanced non-small cell lung cancer: results of the PEMBRO-RT phase 2 randomized clinical trial. JAMA Oncol. 2019;5(9):1276–82.
McBride S, Sherman E, Tsai CJ, Baxi S, Aghalar J, Eng J, et al. Randomized phase II trial of nivolumab with stereotactic body radiotherapy versus nivolumab alone in metastatic head and neck squamous cell carcinoma. J Clin Oncol. 2021;39(1):30–7.
Xing D, Siva S, Hanna GG. The abscopal effect of stereotactic radiotherapy and immunotherapy: Fool’s Gold or El Dorado? Clin Oncol. 2019;31(7):432–43.
Spaas M, Lievens Y. Is the Combination of immunotherapy and radiotherapy in non-small cell lung cancer a feasible and effective approach? Front Med. 2019;6:16.
Chicas-Sett R, Zafra-Martin J, Morales-Orue I, Castilla-Martinez J, Berenguer-Frances MA, Gonzalez-Rodriguez E, et al. Immunoradiotherapy as an effective therapeutic strategy in lung cancer: from palliative care to curative intent. Cancers. 2020;12(8):2178.
Acknowledgements
Not applicable.
Funding
This publication was funded by a research grant from Stiftung für angewandte Krebsforschung/Foundation for Applied Cancer Research, Zurich.
Author information
Authors and Affiliations
Contributions
OV wrote the manuscript and evaluated the data. NA evaluated the data. MH wrote the manuscript and evaluated the data. ACF wrote the manuscript and evaluated the data. SGCK wrote the manuscript and evaluated the data. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This report has been performed in accordance with the Declaration of Helsinki.
Consent for publication
The patient consented to publication of the data.
Competing interests
M.H. is a recipient of grants from GE Healthcare, grants for translational and clinical cardiac and oncological research from the Alfred and Annemarie von Sick legacy, and grants from the Clinical Research Priority Program (CRPP) Artificial Intelligence in oncological Imaging Network by the University of Zurich. The other authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Vilinovszki, O., Andratschke, N., Huellner, M. et al. True abscopal effect in a patient with metastatic non-small cell lung cancer. Radiat Oncol 16, 194 (2021). https://doi.org/10.1186/s13014-021-01920-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13014-021-01920-4