Abstract
Objectives
The SWORD trial is the first multicenter, single arm, phase II study assessing the safety and efficacy of a PD-1 inhibitor (Sintilimab), stereotactic body radiotherapy (SBRT) and granulocyte–macrophage colony stimulating factor (GM-CSF) in advanced non-small cell lung cancer (NSCLC) without sensitizing driver mutations. A safety run-in phase was conducted to determine the tolerability of the experimental treatment.
Materials and methods
Twenty metastatic NSCLC patients who failed first-line chemotherapy were enrolled, and they received SBRT (8 Gy × 3) to one lesion, followed by Sintilimab (200 mg d1, every 3 weeks, until disease progression, unacceptable toxicity, or up to 35 cycles) and GM-CSF (125 μg/m2 d1-d14, cycle 1) within 2 weeks after SBRT. In addition, blood and tissue samples were serially collected for translational research.
Results
Median age of the patients was 61 and all of them had more than 5 lesions at baseline. The sites of SBRT included lung (n = 11), mediastinal lymph node (n = 5), liver (n = 1), abdominal lymph node (n = 1), pleural nodule (n = 1) and vertebra (n = 1). No patients had dose-limiting toxicities (DLTs) and 18 patients experienced treatment-related adverse event (TRAE). The most common TRAEs were fatigue (50%), fever (30%), and ostealgia (20%), and they all were grade 1. Only 2 grade 3 TRAEs were observed, including elevation of liver enzymes in one and transient acute heart failure in another. No grade 4 or 5 AE was observed.
Conclusion
Sintilimab, SBRT and GM-CSF for advanced NSCLC is safe with manageable TRAEs and the trial continues to recruit participants.
Trial registration ClinicalTrials.gov, NCT04106180. Registered 26 September 2019, SBRT in Combination With Sintilimab and GM-CSF for the Treatment of Advanced NSCLC-Tabular View-ClinicalTrials.gov.
Similar content being viewed by others
Introduction
Over the last decade, immune checkpoint inhibitors, particularly inhibitors of the programmed cell death-1(PD-1)/programmed cell death ligand-1(PD-L1) axis, have transformed the therapeutic landscape in advanced non-small cell lung cancer (NSCLC) without driver mutations. Several PD-1/PD-L1 inhibitors have been demonstrated to provide significant overall survival (OS) benefit than docetaxel as second-line therapy [1,2,3,4,5,6]. However, the treatment efficacy of single-agent PD-1/PD-L1 inhibitors, which have an overall response rate (ORR) of around 15%–20% in all comers, is unsatisfactory [7].
Radiotherapy, especially stereotactic body radiotherapy (SBRT), is repeatedly found to enhance anti-tumor immunity and has the potential to synergize with immunotherapy in NSCLC [8, 9]. The underlying molecular mechanisms include the induction of immunogenic cell death [10], release of tumour associated antigen (TAA) and cytokines [11,12,13], and enhance the homing of immune cells to tumours [14, 15], thus converting immunologically “cold” tumours into “hot” tumours [16]. In addition, the upregulation of PD-L1 expression on tumour cells induced by radiotherapy makes patients more susceptible to subsequent PD-1/PD-L1 inhibitors, contributing to a higher response rate and longer survival [17]. Given that the radiation-induced antitumour immunity is dose-dependent, SBRT, which delivers a high radiation dose in generally 3–5 fractions to single-tumour sites with high accuracy, potentially has more potent immune activation effects than conventional radiotherapy [18, 19]. This superiority makes SBRT favorably combine with PD-1/PD-L1 inhibitors. In the phase II randomised clinical trial PEMBRO-RT, the combination of SBRT (8 Gy \(\times\) 3 fractions) and Pembrolizumab revealed enhanced antitumour immunity with numerically improved ORR (36% vs. 18%), progression-free survival (PFS, 6.6 months vs. 1.9 months) and OS (15.9 months vs. 7.6 months) compared with Pembrolizumab alone [20]. Moreover, an individual patient-level meta-analysis of the Pembro-RT trial and MDACC study [21], demonstrated that adding radiotherapy, especially SBRT, to Pembrolizumab, significantly improved out-of-field (abscopal) response rate (ASR, 41.7% vs 19.7%, p = 0.0039), PFS (9.0 months vs 4.4 months, p = 0.0450) and OS (19.2 months vs 8.7 months, p = 0.0004) in patients with pretreated metastatic NSCLC [22]. However, these results need to be verified in further clinical trials enrolling patients from different races and genetic backgrounds. The reported efficacy of combining SBRT and PD-1/PD-L1 inhibitor remains unsatisfactory, and novel partners with non-redundant molecular mechanisms are demanded.
The antigen presentation by dendritic cells (DCs) and subsequent activation of adaptive immune response are indispensable steps in cancer-immune cycle, and the granulocyte–macrophage colony–stimulating factor (GM-CSF), which plays a pivotal role in the differentiation and maturation of DCs, can serve as potent immune adjuvant or sensitizer [23, 24]. In solid tumors, GM-CSF augments the recruitment and activations of DCs, which helps in eradicating cancer by presenting TAAs to T cells and subsequently initiating the anti-tumor adaptive immune response. This effect is supported by the GM-CSF-induced enhanced antitumour activity, which disappeared when CD4+ or CD8+ T cells were depleted [25]. In a preclinical study that used the B16 melanoma model, irradiated tumour cells alone could not stimulate significant anti-tumour immunity, whereas irradiated cells expressing murine GM-CSF stimulated potent, long-lasting, and specific anti-tumour immunity [25]. A proof-of-concept phase II trial (NCT02474186) enrolling 41 patients with different metastatic solid tumours found that adding GM-CSF to SBRT could induce abscopal response in 11 (26.8%) patients, including 4 patients with advanced NSCLC [26]. The safety and efficacy of combining radiotherapy and GM-CSF was shown in a phase I/II study in untreated stage III/IV squamous cell cancer of head and neck [27]. These data support the synergic cooperation between radiotherapy and GM-CSF in activating the innate immune response against cancer. However, the T cell exhaustion remains an obstacle for long-term anti-tumour immunity, which may be mitigated by PD-1/PD-L1 inhibitors. Hence, the triple combination of SBRT, GM-CSF and a PD-1/PD-L1 inhibitor may potentially enhance the treatment efficacy of advanced NSCLC through the activation of innate and adaptive anti-tumour immune responses. Nevertheless, feasibility and efficacy have not been evaluated.
Given the above preclinical and clinical data, we conducted a prospective, multicentre, single-arm, phase II trial assessing the safety and efficacy of triple combination of Sintilimab, a PD-1 inhibitor which had been proven to be effective in advanced NSCLC [28, 29], SBRT and GM-CSF as second-line therapy in sensitizing the driver mutation negative metastatic NSCLC. A safety run-in phase is conducted to determine the tolerability of this novel triple combination therapy by monitoring dose-limiting toxicities (DLTs) in the first 20 enrolled patients and herein we reported the results.
Methods
Study design
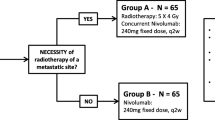
The SWORD trial (NCT04106180) was a single arm, open-label, multicentre, phase II study with a safety run-in phase. Patients with metastatic NSCLC and without driver mutations who failed first-line standard-of-care chemotherapy were treated with SBRT in combination with Sintilimab and GM-CSF. Additionally, blood and tissue samples were serially collected for translational research. The trial was designed to enrol 56 patients. The sample size was calculated for the following hypothesis: H0 (null) with an ORR ≤ 20% in accordance with Checkmate 017 and Checkmate 057 [5], H1 (alternative) with an ORR ≥ 38%. If no less than 17 out of the 56 patients evaluated had objective response (CR or PR), then H0 will be rejected in favour of H1. This design had at least 90% power to reject H0 if the ORR was 30% or more with a one-sided type I error rate of 5%. The study scheme is presented in Fig. 1 and the protocol of this trial is provided as Additional file 1.
The study schema. Description: After baseline screen, eligible patients were treated with SBRT administrated at 24 Gy in 3 fractions (8 Gy/Fx) once-daily. Then, patients received Sintilimab, a PD-1 inhibitor, and rhGM-CSF starting within 2 weeks after SBRT completion. Sintilimab 200 mg was administrated on Day 1 (D1) every 3 weeks until disease progression, intolerable toxicity, up to 35 cycles (2 years), death, or withdrawal of consent. RhGM-CSF 125 μg/m2 would be given daily for 14 consecutive days (D1–D14) on Cycle 1. Treatment visits were performed with a physical examination, laboratory assessments, adverse events collections, and concomitant treatments description on D1 of each treatment cycle. Treatment efficacy was evaluated by radiographic examinations every 9 weeks. Abbreviations: SBRT: stereotactic body radiotherapy, PD-1: programmed cell death-1, rhGM-CSF: recombinant human granulocyte–macrophage colony stimulating factor
Objectives and endpoints
The trial was designed to evaluate the safety and efficacy of Sintilimab in combination with SBRT and GM-CSF in patients with advanced NSCLC previously treated with first-line platinum-based chemotherapy. The primary endpoint was ORR, which was defined as the proportion of participants with partial (PR) or complete (CR) response in evaluable patients in accordance with the Response Evaluation Criteria in Solid Tumors (RECIST) 1.1 [30] determined by investigators.
Secondary objectives were safety profiles according to the Common Terminology Criteria for Adverse Events version 5.0 (CTCAE 5.0), ASR, OS and PFS. ASR was defined as the proportion of patients with at least 30% reduction from baseline in the sum of longest diameter of non-irradiated target lesions defined by the RECIST 1.1 [30]. OS was defined as the time from the date of enrollment until death by any cause. Participants still alive at the time of last follow-up were censored in survival analyses. PFS was measured from the date of enrollment to the date of disease progression (PD) as defined by the RECIST 1.1 [30] or death due to any cause, whichever occurred first. Participants who did not have disease progression by the time of the last radiographic follow-up were censored in survival analyses.
Additionally, this study collected serial peripheral blood and tissue specimens from the enrolled patients who were willing to participate in the translational research. The relationship between biomarkers generated from these serially collected biological samples, treatment efficacy and treatment-related adverse events (TRAEs) were extensively analysed to investigate the molecular mechanisms underlying the synergic effect and primary resistance of this triple combination.
Study population
Patients could be included if they had histologically confirmed stage IV NSCLC without driver mutations, and had failed (documented progression or intolerable toxicity) first-line platinum-based therapy without PD-1/PD-L1 inhibitors. Driver mutations included epidermal growth factor receptor mutations, anaplastic lymphoma kinase or ROS proto-oncogene 1 translocations. Patients should have at least one lesion (size: 1–5 cm) eligible for SBRT (24 Gy/3 Fx) and at least another measurable lesion as defined by the RECIST 1.1 [30]. Patients with brain metastasis were eligible if they were asymptomatic, neurologically stable, and off corticosteroids. Key exclusion criteria included patients who had received any PD-1/PD-L1 inhibitors previously.
Treatment scheme and modalities
Eligible patients were treated with SBRT for one previously unirradiated primary or metastatic lesion (size 1–5 cm), and SBRT was administrated 24 Gy in 3 fractions (8 Gy/Fx) once daily for three consecutive days. Patients then received Sintilimab and GM-CSF intravenously (IV) starting within two weeks after SBRT completion. Sintilimab 200 mg IV was administrated on Day 1 (D1) every three weeks until PD, intolerable toxicity, up to 35 cycles (two years), death, or withdrawal of consent. GM-CSF 125 μg/m2 was given daily for 14 consecutive days (D1–D14) on cycle 1.
Treatment evaluation
For patients who received at least one dose of Sintilimab and GM-CSF, treatment visits were performed with a physical examination, laboratory assessments, adverse event (AE) collections and concomitant treatments description on D1 of each treatment cycle. In addition, weekly phone calls were made to assess patients’ symptoms. Treatment efficacy was evaluated by radiographic examinations every nine weeks.
Safety run-in analysis
Given that the safety profile of SBRT in combination with Sintilimab and GM-CSF has not been evaluated in patients with advanced NSCLC, a safety run-in was adopted to ensure that no excessive severe AE happened in treated patients. Accrual was suspended after the inclusion of 20 patients, and the safety data for each patient were collected within the first 30 days after the first dose of study drugs to detect unexpected non-tolerable toxicities early. DLT was monitored during the DLT observation window, which was defined as 30 days after the first cycle of protocol treatment. DLT was defined as any grade 3 event lasting for more than seven days other than asymptomatic laboratory abnormalities, any grade 4 event or any treatment related grade 5 event.
Grading was made in accordance with CTCAE 5.0. At any time during the safety run-in phase, if excessive numbers (≥ 35%) of DLTs were to be seen, the accrual was to be halted and the Data and Safety Monitoring Board was to be convened to decide on the study continuation. In addition, if excessive numbers (≥ 20%) of death were to be seen within 60 days since the initiation of GM-CSF treatment, the study was to close for safety concerns.
Ethical considerations
Written informed consent was obtained from all patients before performing any study-specific tests or evaluations. The protocol received formal approval by the ethical authorities/committees of all participating academic cemtres.
Statistical analysis
TRAEs and DLTs for the first 20 patients enrolled to the safety run-in phase of the trial were summarised by TRAE type, grade, frequency and proportion. These 20 patients were assessed and included for all outcomes by using the same schedule and criteria as subsequent patients. The demographic variables of these patients were summarised by median and range for continuous variables and by frequency and percentage for categorical variables. Analyses were performed by statisticians through the SPSS 21.0 (SPSS, Chicago, IL, USA) and R version 3.5.1 (The R Foundation for Statistical Computing).
Results
Patient characteristics
From 2019/10/16 to 2020/8/8, 22 patients were screened. Two patients were excluded due to withdrawal of consent in one patient and rapid deterioration of general condition before any treatment initiation in another. Hence, 20 patients were enrolled in the safety run-in phase. The baseline characteristics and SBRT sites of these 20 patients are summarised in Table 1. Most patients were male, smoker and had Eastern Cooperative Oncology Group (ECOG) performance status 1 and non-squamous NSCLC, with a median age of 61 years (range, 32–71 years). Baseline brain, liver and bone metastasis were present in 2, 4 and 8 patients, respectively. The majority of patients had no less than three metastatic organs and all patients had more than five metastatic lesions.
AEs and DLT observation
No DLT was observed during the DLT observation window. Overall, 18 (90.0%) of 20 patients experienced TRAEs. The most common TRAEs were fatigue (50%), fever (30%), and ostealgia (20%), and all were grade 1. Grade 2 TRAEs occurred in four (40.0%) patients, whereas grade 3 TRAEs (ALT/AST elevation and heart failure) were observed in two (10.0%) patients. No patient experienced grade 4 or 5 TRAEs. The detailed information on AEs is summarised in Table 2.
Characteristics of patients experiencing acute heart failure
Two patients experienced acute and transient left heart failure.
Patient 009 was a 62-year-old male, a smoker, and diagnosed with metastatic squamous cell carcinoma of the right lung in July 2019. He denied any previous medical history of cardiovascular diseases. After failing first-line chemotherapy consisting of four cycles of cisplatin and nab-paclitaxel, he was enrolled into the trial. SBRT was performed to one of the metastatic mediastinal lymph nodes uneventfully, followed by Sintilimab and GM-CSF. Four days after Sintilimab and GM-CSF initiation, the patient complained of progressive dyspnoea with moist rales in the lungs. Laboratory tests revealed an elevation in pro-BNP (3970 pg/ml) and echocardiography found mild pulmonary hypertension. Acute left heart failure (grade 2) was diagnosed by an experienced cardiologist and GM-CSF was stopped. The patient recovered three days after administration with diuretics, oxygen therapy and antiasthmatic agents. However, the patient refused to continue the study treatment and was transferred to a local hospital.
Patient 014 was a 71-year-old male, smoker, and diagnosed with metastatic squamous cell carcinoma of the right lung in September 2019. He also denied any past medical history of cardiovascular diseases. Before enrollment, he had been treated with four cycles of Carboplatin and Gemcitabine, as well as salvage thoracic radiotherapy. SBRT was performed to one of the metastatic mediastinal lymph nodes successfully, followed by Sintilimab and GM-CSF. Seven days after Sintilimab and GM-CSF initiation, the patient developed severe shortness of breath, fatigue and facial oedema. On examination, moist rales were observed in the lungs, and the oxygen saturation was 86%. Laboratory tests found a significant elevation in pro-BNP (4820 pg/ml). Acute left heart failure (grade 3) was diagnosed, and GM-CSF was stopped. The patient’s symptoms were alleviated five days after the administration of diuretics and oxygen therapy. This event was considered related to GM-CSF only. Thus, Sintilimab was given for another three cycles, without the recurrence of acute heart failure. The best response to the triple therapy was a stable disease. However, the tumour progressed rapidly after the fourth cycle and eventually led to death.
Discussion
PD-1/PD-L1 inhibitors, alone or in combination with other agents, are now standard of care for advanced NSCLC without driver mutations [31]. However, the response rate of PD-1/PD-L1 inhibitor alone is limited and the treatment toxicities of combinational modalities already available are frequent [32, 33]. Novel treatment strategies with potent efficacy and minimal AEs are highly needed. Here, we report the preliminary results of safety run-in phase of the prospective, multicentre, phase II trial (SWORD) investigating triple combination of Sintilimab, SBRT and GM-CSF as novel second-line therapy for advanced NSCLC without driver mutations. The novel combination is safe with manageable TRAEs.
For the first time, we have found that the triple combination of SBRT, a PD-1 inhibitor and GM-CSF seems to be safe with mild toxicities. The safety of PD-1/PD-L1 inhibitors in combination with SBRT has been demonstrated in several prospective clinical trials [20, 21, 34, 35], with the frequency of grades 3–5 TRAEs ranging from 9.7% to 30.0% and very few patients developed DLTs. The combination of SBRT and GM-CSF has also been tested in a prospective trial with acceptable toxicities [26]. However, the feasibility and safety of combining GM-CSF and PD-1/PD-L1 inhibitors have not been reported. In our study, grade 3 TRAEs occurred in 10.0% of the patients, without DLT or grade 4–5 TRAEs. Most of the TRAEs were mild, and the two grade 3 TRAEs were transient, which could be successfully managed. Taken together, triple combination of Sintilimab, SBRT and GM-CSF in advanced NSCLC was demonstrated to be safe, and the trial has continued to recruit participants.
Nevertheless, acute heart failure was an unexpected AE in our study. Congestive heart failure was previously reported in clinical trials examining the safety and efficacy of combinational regimens involving GM-CSF amongst patients with haematological disorders [36, 37] and solid tumours [38]. The GM-CSF receptor expression and plasma GM-CSF level were also found to be significantly elevated in patients with end-stage heart failure [39, 40]. Mechanically, GM-CSF produced by cardiac fibroblasts could act locally and distally to generate and recruit inflammatory and proteolytic cells, which led to heart failure in mouse models [41]. In our study, two patients experienced transient acute left heart failure and recovered quickly after GM-CSF discontinuation and initiation of diuretics. Hence, GM-CSF-related heart failure was suspected in these two patients. However, we could not totally rule out the possibility that Sintilimab also had a role in the development of acute heart failure in these two patients. The cardiac toxicities of PD-1/PD-L1 inhibitors rarely developed but have detrimental effects [42, 43], and PD-1/PD-L1 inhibitor-related heart failure was anecdotally reported [44,45,46]. However, the two patients recovered rapidly without glucocorticoids, and one of the patients continued to receive further cycles of Sintilimab without the recurrence of heart failure. Hence, acute heart failure should be intensively monitored in patients receiving continuous GM-CSF especially amongst those with concurrent PD-1/PD-L1 inhibitors.
Our study has several strengths. Firstly, this prospective, phase II, multicentre study is the first to assess the safety and efficacy of a triple combination of a PD-1/PD-L1 inhibitor, SBRT and GM-CSF in advanced solid tumors. Although this study is a single-arm study, several clinical trials test the efficacy of PD-1/PD-L1 inhibitor alone as second-line therapy in advanced NSCLC with generally consistent results, which can serve as reliable historical control [1,2,3, 47]. These historical controls and experiences from previous studies are used [20, 21], and the sample size of our study is dedicatedly designed to have a 90% power to detect the difference. Moreover, the data generated from serially collected biological samples can provide valuable information regarding the molecular mechanisms underlying the effective anti-tumor immune response induced by the trial regimen, which can be used to design improved combinational treatment strategies for advanced NSCLC. Notably, the effect of SBRT on the immune microenvironment of tumour lesions outside the radiation field and its relationship between the so-called “abscopal effect” can be examined, which is largely unknown, because tissue samples from the same tumor lesion outside the radiation field both before and after SBRT (but before initiation of Sintilimab and GM-CSF) are collected [48, 49].
Conclusions
The triple combination of SBRT, GM-CSF and Sintilimab is safe and well tolerated. The SWORD trial continues patient recruitment and the efficacy results are pending.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- PD-1:
-
Programmed cell death-1
- PD-L1:
-
Programmed cell death ligand-1
- NSCLC:
-
Non-small cell lung cancer
- OS:
-
Overall survival
- ORR:
-
Overall response rate
- SBRT:
-
Stereotactic body radiotherapy
- TAA:
-
Tumor associated antigen
- PFS:
-
Progression-free survival
- ASR:
-
Abscopal response rate
- DC:
-
Dendritic cell
- GM-CSF:
-
Granulocyte–macrophage colony stimulating factor
- DLT:
-
Dose-limiting toxicity
- PR:
-
Partial response
- CR:
-
Complete response
- RECIST:
-
Response Evaluation Criteria in Solid Tumors
- CTCAE 5.0:
-
Common Terminology Criteria for Adverse Events version 5.0
- PD:
-
Progression disease
- TRAE:
-
Treatment-related adverse events
- D:
-
Day
- AE:
-
Adverse event
- ECOG:
-
Eastern Cooperative Oncology Group
References
Borghaei H, Paz-Ares L, Horn L, Spigel DR, Steins M, Ready NE, Chow LQ, Vokes EE, Felip E, Holgado E, Barlesi F, Kohlhäufl M, Arrieta O, Burgio MA, Fayette J, Lena H, Poddubskaya E, Gerber DE, Gettinger SN, Rudin CM, Rizvi N, Crinò L, Blumenschein GR Jr, Antonia SJ, Dorange C, Harbison CT, Graf Finckenstein F, Brahmer JR. Nivolumab versus docetaxel in advanced nonsquamous non-small-cell lung cancer. N Engl J Med. 2015;373:1627–39.
Brahmer J, Reckamp KL, Baas P, Crinò L, Eberhardt WE, Poddubskaya E, Antonia S, Pluzanski A, Vokes EE, Holgado E, Waterhouse D, Ready N, Gainor J, Arén Frontera O, Havel L, Steins M, Garassino MC, Aerts JG, Domine M, Paz-Ares L, Reck M, Baudelet C, Harbison CT, Lestini B, Spigel DR. Nivolumab versus docetaxel in advanced squamous-cell non-small-cell lung cancer. N Engl J Med. 2015;373:123–35.
Rittmeyer A, Barlesi F, Waterkamp D, Park K, Ciardiello F, von Pawel J, Gadgeel SM, Hida T, Kowalski DM, Dols MC, Cortinovis DL, Leach J, Polikoff J, Barrios C, Kabbinavar F, Frontera OA, De Marinis F, Turna H, Lee JS, Ballinger M, Kowanetz M, He P, Chen DS, Sandler A, Gandara DR. Atezolizumab versus docetaxel in patients with previously treated non-small-cell lung cancer (OAK): a phase 3, open-label, multicentre randomised controlled trial. Lancet. 2017;389:255–65.
Fehrenbacher L, Spira A, Ballinger M, Kowanetz M, Vansteenkiste J, Mazieres J, Park K, Smith D, Artal-Cortes A, Lewanski C, Braiteh F, Waterkamp D, He P, Zou W, Chen DS, Yi J, Sandler A, Rittmeyer A. Atezolizumab versus docetaxel for patients with previously treated non-small-cell lung cancer (POPLAR): a multicentre, open-label, phase 2 randomised controlled trial. Lancet. 2016;387:1837–46.
Horn L, Spigel DR, Vokes EE, Holgado E, Ready N, Steins M, Poddubskaya E, Borghaei H, Felip E, Paz-Ares L, Pluzanski A, Reckamp KL, Burgio MA, Kohlhäeufl M, Waterhouse D, Barlesi F, Antonia S, Arrieta O, Fayette J, Crinò L, Rizvi N, Reck M, Hellmann MD, Geese WJ, Li A, Blackwood-Chirchir A, Healey D, Brahmer J, Eberhardt WEE. Nivolumab versus docetaxel in previously treated patients with advanced non-small-cell lung cancer: two-year outcomes from two randomized, open-label, phase III trials (CheckMate 017 and CheckMate 057). J Clin Oncol. 2017;35:3924–33.
Herbst RS, Baas P, Kim D-W, Felip E, Pérez-Gracia JL, Han J-Y, Molina J, Kim J-H, Arvis CD, Ahn M-J, Majem M, Fidler MJ, de Castro G, Garrido M, Lubiniecki GM, Shentu Y, Im E, Dolled-Filhart M, Garon EB. Pembrolizumab versus docetaxel for previously treated, PD-L1-positive, advanced non-small-cell lung cancer (KEYNOTE-010): a randomised controlled trial. Lancet (London, England). 2016;387:1540–50.
Doroshow DB, Herbst RS. Treatment of advanced non-small cell lung cancer in 2018. JAMA Oncol. 2018;4:569–70.
Herrera FG, Bourhis J, Coukos G. Radiotherapy combination opportunities leveraging immunity for the next oncology practice. CA Cancer J Clin. 2017;67:65–85.
Grassberger C, Ellsworth SG, Wilks MQ, Keane FK, Loeffler JS. Assessing the interactions between radiotherapy and antitumour immunity. Nat Rev Clin Oncol. 2019;16:729–45.
Rapoport BL, Anderson R. Realizing the Clinical Potential of Immunogenic Cell Death in Cancer Chemotherapy and Radiotherapy. Int J Mol Sci 2019;20.
Weichselbaum RR, Liang H, Deng L, Fu Y-X. Radiotherapy and immunotherapy: a beneficial liaison? Nat Rev Clin Oncol. 2017;14:365–79.
Apetoh L, Ghiringhelli F, Tesniere A, Obeid M, Ortiz C, Criollo A, Mignot G, Maiuri MC, Ullrich E, Saulnier P, Yang H, Amigorena S, Ryffel B, Barrat FJ, Saftig P, Levi F, Lidereau R, Nogues C, Mira JP, Chompret A, Joulin V, Clavel-Chapelon F, Bourhis J, André F, Delaloge S, Tursz T, Kroemer G, Zitvogel L. Toll-like receptor 4-dependent contribution of the immune system to anticancer chemotherapy and radiotherapy. Nat Med. 2007;13:1050–9.
Deng L, Liang H, Xu M, Yang X, Burnette B, Arina A, Li XD, Mauceri H, Beckett M, Darga T, Huang X, Gajewski TF, Chen ZJ, Fu YX, Weichselbaum RR. STING-dependent cytosolic DNA sensing promotes radiation-induced type I interferon-dependent antitumor immunity in immunogenic tumors. Immunity. 2014;41:843–52.
Frey B, Rückert M, Deloch L, Rühle PF, Derer A, Fietkau R, Gaipl US. Immunomodulation by ionizing radiation-impact for design of radio-immunotherapies and for treatment of inflammatory diseases. 2017;280: 231–48.
Matsumura S, Wang B, Kawashima N, Braunstein S, Badura M, Cameron TO, Babb JS, Schneider RJ, Formenti SC, Dustin ML, Demaria S. Radiation-induced CXCL16 release by breast cancer cells attracts effector T cells. J Immunol. 2008;181:3099–107.
Bernstein MB, Krishnan S, Hodge JW, Chang JY. Immunotherapy and stereotactic ablative radiotherapy (ISABR): a curative approach? Nat Rev Clin Oncol. 2016;13:516–24.
Gong X, Li X, Jiang T, Xie H, Zhu Z, Zhou F, Zhou C. Combined radiotherapy and anti-PD-L1 antibody synergistically enhances antitumor effect in non-small cell lung cancer. J Thorac Oncol. 2017;12:1085–97.
Schaue D, Ratikan JA, Iwamoto KS, McBride WH. Maximizing tumor immunity with fractionated radiation. Int J Radiat Oncol Biol Phys. 2012;83:1306–10.
Reits EA, Hodge JW, Herberts CA, Groothuis TA, Chakraborty M, Wansley EK, Camphausen K, Luiten RM, de Ru AH, Neijssen J, Griekspoor A, Mesman E, Verreck FA, Spits H, Schlom J, van Veelen P, Neefjes JJ. Radiation modulates the peptide repertoire, enhances MHC class I expression, and induces successful antitumor immunotherapy. J Exp Med. 2006;203:1259–71.
Theelen WSME, Peulen HMU, Lalezari F, van der Noort V, de Vries JF, Aerts JGJV, Dumoulin DW, Bahce I, Niemeijer A-LN, de Langen AJ, Monkhorst K, Baas P. Effect of Pembrolizumab after stereotactic body radiotherapy vs pembrolizumab alone on tumor response in patients with advanced non-small cell lung cancer: results of the PEMBRO-RT phase 2 randomized clinical trial. JAMA Oncol 2019;5(9):1276–1282..
Welsh J, Menon H, Chen D, Verma V, Tang C, Altan M, Hess K, de Groot P, Nguyen QN, Varghese R, Comeaux NI, Simon G, Skoulidis F, Chang JY, Papdimitrakopoulou V, Lin SH, Heymach JV. Pembrolizumab with or without radiation therapy for metastatic non-small cell lung cancer: a randomized phase I/II trial. J Immunother Cancer 2020;8(2):e001001.
Theelen W, Chen D, Verma V, Hobbs BP, Peulen HMU, Aerts J, Bahce I, Niemeijer ALN, Chang JY, de Groot PM, Nguyen QN, Comeaux NI, Simon GR, Skoulidis F, Lin SH, He K, Patel R, Heymach J, Baas P, Welsh JW. Pembrolizumab with or without radiotherapy for metastatic non-small-cell lung cancer: a pooled analysis of two randomised trials. Lancet Respir Med. 2021;9(5):467–75.
Steinman RM, Banchereau J. Taking dendritic cells into medicine. Nature. 2007;449:419–26.
Inaba K, Inaba M, Romani N, Aya H, Deguchi M, Ikehara S, Muramatsu S, Steinman RM. Generation of large numbers of dendritic cells from mouse bone marrow cultures supplemented with granulocyte/macrophage colony-stimulating factor. J Exp Med. 1992;176:1693–702.
Dranoff G, Jaffee E, Lazenby A, Golumbek P, Levitsky H, Brose K, Jackson V, Hamada H, Pardoll D, Mulligan RC. Vaccination with irradiated tumor cells engineered to secrete murine granulocyte-macrophage colony-stimulating factor stimulates potent, specific, and long-lasting anti-tumor immunity. Proc Natl Acad Sci U S A. 1993;90:3539–43.
Golden EB, Chhabra A, Chachoua A, Adams S, Donach M, Fenton-Kerimian M, Friedman K, Ponzo F, Babb JS, Goldberg J, Demaria S, Formenti SC. Local radiotherapy and granulocyte-macrophage colony-stimulating factor to generate abscopal responses in patients with metastatic solid tumours: a proof-of-principle trial. Lancet Oncol. 2015;16:795–803.
Harrington KJ, Hingorani M, Tanay MA, Hickey J, Bhide SA, Clarke PM, Renouf LC, Thway K, Sibtain A, McNeish IA, Newbold KL, Goldsweig H, Coffin R, Nutting CM. Phase I/II study of oncolytic HSV GM-CSF in combination with radiotherapy and cisplatin in untreated stage III/IV squamous cell cancer of the head and neck. Clin Cancer Res. 2010;16:4005–15.
Yang Y, Wang Z, Fang J, Yu Q, Han B, Cang S, Chen G, Mei X, Yang Z, Ma R, Bi M, Ren X, Zhou J, Li B, Song Y, Feng J, Li J, He Z, Zhou R, Li W, Lu Y, Wang Y, Wang L, Yang N, Zhang Y, Yu Z, Zhao Y, Xie C, Cheng Y, Zhou H, Wang S, Zhu D, Zhang W, Zhang L. Efficacy and safety of sintilimab plus pemetrexed and platinum as first-line treatment for locally advanced or metastatic nonsquamous NSCLC: a randomized, double-blind, phase 3 study (Oncology pRogram by InnovENT anti-PD-1-11). J Thorac Oncol. 2020;15:1636–46.
Caicun Zhou YW, Yun Fan, et al. Sintilimab plus gemcitabine and platinum (GP) as first-line (1L) treatment for locally advanced or metastatic squamous non-small-cell lung cancer (sqNSCLC). Ann Oncol 2020;31: S1186.
Eisenhauer EA, Therasse P, Bogaerts J, Schwartz LH, Sargent D, Ford R, Dancey J, Arbuck S, Gwyther S, Mooney M, Rubinstein L, Shankar L, Dodd L, Kaplan R, Lacombe D, Verweij J. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer 2009;45: 228–247.
Arbour KC, Riely GJ. Systemic therapy for locally advanced and metastatic non-small cell lung cancer: a review. JAMA. 2019;322:764–74.
Horvath L, Thienpont B, Zhao L, Wolf D, Pircher A. Overcoming immunotherapy resistance in non-small cell lung cancer (NSCLC) - novel approaches and future outlook. Mol Cancer. 2020;19:141.
Huang MY, Jiang XM, Wang BL, Sun Y, Lu JJ. Combination therapy with PD-1/PD-L1 blockade in non-small cell lung cancer: strategies and mechanisms. Pharmacol Ther 2021;219: 107694.
McBride S, Sherman E, Tsai CJ, Baxi S, Aghalar J, Eng J, Zhi WI, McFarland D, Michel LS, Young R, Lefkowitz R, Spielsinger D, Zhang Z, Flynn J, Dunn L, Ho A, Riaz N, Pfister D, Lee N. Randomized phase II trial of nivolumab with stereotactic body radiotherapy versus nivolumab alone in metastatic head and neck squamous cell carcinoma. J Clin Oncol. 2021;39:30–7.
Luke JJ, Lemons JM, Karrison TG, Pitroda SP, Melotek JM, Zha Y, Al-Hallaq HA, Arina A, Khodarev NN, Janisch L, Chang P, Patel JD, Fleming GF, Moroney J, Sharma MR, White JR, Ratain MJ, Gajewski TF, Weichselbaum RR, Chmura SJ. Safety and clinical activity of pembrolizumab and multisite stereotactic body radiotherapy in patients with advanced solid tumors. J Clin Oncol. 2018;36:1611–8.
Runde V, Aul C, Ebert A, Grabenhorst U, Schneider W. Sequential administration of recombinant human granulocyte-macrophage colony-stimulating factor and human erythropoietin for treatment of myelodysplastic syndromes. Eur J Haematol. 1995;54:39–45.
Nand S, Sosman J, Godwin JE, Fisher RI. A phase I/II study of sequential interleukin-3 and granulocyte-macrophage colony-stimulating factor in myelodysplastic syndromes. Blood. 1994;83:357–60.
James ND, Atherton PJ, Jones J, Howie AJ, Tchekmedyian S, Curnow RT. A phase II study of the bispecific antibody MDX-H210 (anti-HER2 x CD64) with GM-CSF in HER2+ advanced prostate cancer. Br J Cancer. 2001;85:152–6.
Postiglione L, Montagnani S, Ladogana P, Castaldo C, Di Spigna G, Bruno EM, Turano M, De Santo L, Cudemo G, Cocozza S, de Divitiis O, Rossi G. Granulocyte macrophage-colony stimulating factor receptor expression on human cardiomyocytes from end-stage heart failure patients. Eur J Heart Fail. 2006;8:564–70.
Parissis JT, Adamopoulos S, Venetsanou KF, Mentzikof DG, Karas SM, Kremastinos DT. Clinical and neurohormonal correlates of circulating granulocyte-macrophage colony-stimulating factor in severe heart failure secondary to ischemic or idiopathic dilated cardiomyopathy. Am J Cardiol. 2000;86(707–710):A709-710.
Anzai A, Choi JL, He S, Fenn AM, Nairz M, Rattik S, McAlpine CS, Mindur JE, Chan CT, Iwamoto Y, Tricot B, Wojtkiewicz GR, Weissleder R, Libby P, Nahrendorf M, Stone JR, Becher B, Swirski FK. The infarcted myocardium solicits GM-CSF for the detrimental oversupply of inflammatory leukocytes. J Exp Med. 2017;214:3293–310.
Sury K, Perazella MA, Shirali AC. Cardiorenal complications of immune checkpoint inhibitors. Nat Rev Nephrol. 2018;14:571–88.
Salem JE, Manouchehri A, Moey M, Lebrun-Vignes B, Bastarache L, Pariente A, Gobert A, Spano JP, Balko JM, Bonaca MP, Roden DM, Johnson DB, Moslehi JJ. Cardiovascular toxicities associated with immune checkpoint inhibitors: an observational, retrospective, pharmacovigilance study. Lancet Oncol. 2018;19:1579–89.
Laubli H, Balmelli C, Bossard M, Pfister O, Glatz K, Zippelius A. Acute heart failure due to autoimmune myocarditis under pembrolizumab treatment for metastatic melanoma. J Immunother Cancer. 2015;3:11.
Kimura H, Tounai Y, Nagato K, Morimoto JI, Tounai Y. A case of heart failure after treatment with anti-PD-1 antibody followed by adoptive transfer of cytokine-activated killer cells in a recurrent lung cancer patient. J Thorac Oncol. 2017;12:e128–30.
Samejima Y, Iuchi A, Kanai T, Noda Y, Nasu S, Tanaka A, Morishita N, Suzuki H, Okamoto N, Harada H, Ezumi A, Ueda K, Kawahara K, Hirashima T. Development of severe heart failure in a patient with squamous non-small-cell lung cancer during nivolumab treatment. Intern Med. 2020;59:2003–8.
Wu YL, Lu S, Cheng Y, Zhou C, Wang J, Mok T, Zhang L, Tu HY, Wu L, Feng J, Zhang Y, Luft AV, Zhou J, Ma Z, Lu Y, Hu C, Shi Y, Baudelet C, Cai J, Chang J. Nivolumab versus docetaxel in a predominantly Chinese patient population with previously treated advanced NSCLC: CheckMate 078 randomized phase III clinical trial. J Thorac Oncol. 2019;14:867–75.
Ngwa W, Irabor OC, Schoenfeld JD, Hesser J, Demaria S, Formenti SC. Using immunotherapy to boost the abscopal effect. Nat Rev Cancer. 2018;18:313–22.
Rodriguez-Ruiz ME, Rodriguez I, Leaman O, Lopez-Campos F, Montero A, Conde AJ, Aristu JJ, Lara P, Calvo FM, Melero I. Immune mechanisms mediating abscopal effects in radioimmunotherapy. Pharmacol Ther. 2019;196:195–203.
Acknowledgements
Not applicable.
Funding
This work was supported by Clinical Research Plan of SHDC [Grant No. SHDC2020CR4010] and CSCO foundation [Grant No. Y-XD2019-050].
Author information
Authors and Affiliations
Contributions
Conceptualization: Yue Zhou and Jianjiao Ni. Data curation: Yue Zhou, Jianjiao Ni, Lin Wu, Xinghao Ai and Zhengfei Zhu. Formal analysis: Jianjiao Ni, Yue Zhou, Lin Wu and Xinghao Ai. Methodology: Jianjiao Ni, Lin Wu, Xinghao Ai, Xiaorong Dong, Qian Chu, Chengbo Han and Zhengfei Zhu. Funding acquisition: Zhengfei Zhu. Writing—original draft: Yue Zhou and Jianjiao Ni. Writing—review and editing: all of the authors. Study supervision: Zhengfei Zhu. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical approval was obtained from the ethnical Authorities/Committees of all participating academic centers. Written informed consent was obtained from all patients before performing any study-specific tests or evaluations.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1
. A phase II, open-label, single-arm, multi-center study of Sintilimab, stereotactic body radiotherapy and granulocyte-macrophage colony stimulating factor in advanced non-small cell lung cancer (SWORD).
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ni, J., Zhou, Y., Wu, L. et al. Sintilimab, stereotactic body radiotherapy and granulocyte–macrophage colony stimulating factor as second-line therapy for advanced non-small cell lung cancer: safety run-in results of a multicenter, single-arm, phase II trial. Radiat Oncol 16, 177 (2021). https://doi.org/10.1186/s13014-021-01905-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13014-021-01905-3