Abstract
Background
There is a lack of data on the biologically effective dose and the efficacy of stereotactic body radiotherapy in hepatocellular carcinoma patients, and this study was conducted to explore the relation between BED and efficacy.
Methods
This study is designed as a mono-center study. The participants are randomized into three group, and received the following recommended schedule: 49Gy/7f, 54Gy/6f and 55Gy/5f with BED10 in correspondence to 83.3Gy, 102.6Gy and 115.5Gy. The primary outcome measures are to calculate local control rates (LC), overall survival rates (OS) and progression-free survival rates (PFS). The secondary outcome measures are to observe radiation-induced liver injury (RILD) rates, Child-Pugh score and indocyanine green retention rate at 15 min (ICG-R15) value before and after CK-SBRT. Moreover, gastrointestinal toxicities are also observed.
Discussion
There is no uniform standard for CK-SBRT dose schedule of hepatocellular carcinoma. We propose to conduct a study determining the optimal CK-SBRT schedule of hepatocellular carcinoma patients (≤5 cm). The trial protocol has been approved by the Institutional Review Board of 302 Hospital of PLA (People’s Liberation Army). The Ethics number is 2017111D.
Trail registration
Clinical trails number: NCT03295500. Date of registration: November, 2017.
Similar content being viewed by others
Background
There were 841,080 new liver carcinoma cases and 781,631 deaths worldwide in 2018 [1]. Stereotactic body radiotherapy (SBRT) was an option for hepatocellular carcinoma patients who are not suitable for radical surgery, such as liver transplantation, resection, radio-frequency ablation (RFA) [2]. CyberKnife SBRT (CK-SBRT) is a new type of stereotactic radiosurgery, which can be guided by respiratory synchronous tracking and fiducial markers tracking. With two tracking ways above, CK-SBRT has certain advantages in treating liver lesions that move constantly.
The overall survival rates of lung cancer and cervical cancer patients increased with the delivery of increasing biologically effective doses (BED) to lesions [3, 4]. However, there is a lack of data on the BEDs and the efficacy of SBRT in hepatocellular carcinoma patients. Moreover, it is also worth studying whether BED escalation can cause an increase in the incidence of radiation injury.
Method and design
Study design
This is a mono-center study to explore the efficacy and adverse reaction for hepatocellular carcinoma patients with BED10 escalation of CyberKnife SBRT (CK-SBRT).
Primary outcome measures
-
1.
Local control rate: LC is calculated starting from the date of CK-SBRT to progress (the lesion diameter is more than original tumor in contrast-enhanced CT or contrast enhanced MRI).
-
2.
Overall survival rate: OS is defined starting from the date of CK-SBRT to the date of final follow-up or demise of patients.
-
3.
Progression-free survival: PFS was estimated starting from the date of CK-SBRT to the date of disease progression or demise of patients.
Secondary outcome measures
-
1.
Radiation-induced liver injury (RILD) rate:
RILD included classic RILD and non-classic RILD. Classic RILD manifests as symptoms of fatigue, hepatomegaly, and anicteric ascites, etc. Additionally, the serum alkaline phosphatase level in these patients increases to more than twice the normal level, but the serum transaminase and bilirubin levels in remain normal [5, 6]. Non-classic RILD usually occurred in patients with hepatitis and cirrhosis who are also with markedly elevated serum transaminases (> 5 times the upper limit of normal) rather than elevated alkaline phosphatase or a decline in liver function (measured by a worsening of Child-Pugh score by 2 or more) [7].
RILD was evaluated every 3 days during CK-SBRT, every month for initial 3 months and every 3 months thereafter until 8 months after CK-SBRT.
- 2.
Child-Pugh score was calculated every 3 days during CK-SBRT, every month for initial 3 months and every 3 months thereafter until 8 months after SBRT.
- 3.
Indocyanine green retention rate at 15 min (ICG-R15) value was estimated every 3 days during CK-SBRT, every month for initial 3 months and every 3 months thereafter until 8 months after SBRT.
- 4.
To observe acute and late gastrointestinal toxicities following CK-SBRT [8].
Inclusion criteria
The hepatocellular carcinoma patients were diagnosed by image examination and laboratory test or pathology.
- 1.
The diameter of lesion ≤5 cm.
- 2.
Age of 30–80 years old.
- 3.
Child-pugh classification A or B.
- 4.
ECOG PS score 0 or 1.
- 5.
Leukocyte count≥2*109/L, platelets count≥60*109/L.
- 6.
Kidney function is normal: Urea:2.9–8.2 mmol/L, Cr: 62-115umol/L.
- 7.
Unsuitable to or rejecting other therapies, such as resection, liver transplantation, etc.
- 8.
A life expectancy of ≥6 months.
- 9.
All participants understand the research subject and sign a written informed consent document.
Exclusion criteria
-
1.
With previous therapies, such as resection, liver transplantation, radiofrequency ablation, transarterial chemoembolization, etc.
-
2.
The outline of lesion is not confirmed by image examination.
-
3.
With hepatic or any other abdomen radiotherapy history before.
-
4.
With severe internal medicine diseases.
-
5.
Intractable ascites.
-
6.
Distance between lesion and organs at risk (OARs: esophagus, stomach, intestine) is less than 5 mm.
-
7.
The normal liver volume less than 700 cc.
-
8.
With extrahepatic metastasis.
-
9.
Pregnant women.
-
10.
Participants who are in another trial while on study.
Radiation treatment planning
All participants are implanted with 4 to 6 fiducial markers 1 week prior to CT localization. The distance between markers and lesion is less than 6 cm. Before CT localization, a vacuum-bag is used for fixing the body, the arms and the legs (both arms are along the body, and both hands are on thighs). The acquired parameters of CT images are as follows: tilted angel of 0°; slice thickness of 1 mm; voltage of 120 KV tube current of 400 mA; pixel size of 512 × 512. When the patients received simulation, they need hold their breath with smooth breathing. We adopt contrast-enhanced CT or contrast-enhanced MRI as an auxiliary image for fusion. The radiation oncologists contour gross tumor volume (GTV), planning target volume (PTV) and organs at risk. GTV is defined as the visible lesion based on image examination. PTV expands 3-5 mm of GTV. The participants are randomized into three group, and received the following recommended schedule: 49Gy/7f, 54Gy/6f and 55Gy/5f with BED10 in correspondence to 83.3Gy, 102.6Gy and 115.5Gy.
All CK-SBRT plans are calculated by G4 CyberKnife MultiPlan (Version 4.0.2) and VSI CyberKnife MultiPlan (Version 4.6.1). The plans enclosed PTV with 75–90% isodose line of maximum dose equated to the prescribed dose. Normal tissues tolerance doses comply with AAPM TG-101 report [9].
Evaluation and follow-up
The CK-SBRT plan is delivered every day including on weekend. During CK-SBRT, the adverse reaction is evaluated every day. Physical examination and laboratory test are assessed every 3 days. In case patients present nausea and/or vomiting, they will receive corresponding drug treatment. The treatment schedule will be delayed when patients with uncontrollable vomiting and/or abnormal liver function. After CK-SBRT, the patients are followed up, which includes physical examination, laboratory test and image examination. The follow up period defines as every month for initial 3 months, and every 3 months thereafter until 2 years. Follow-up include The trail was planned to begin on September 2017.
A quality assurance
Three radiation oncologists and two physicists formed CyberKnife QA group.
Statistical analysis
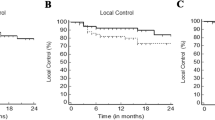
LC, OS and PFS are estimated using the Kaplan-Meier method. LC, OS and PFS related group analyses of BED10 are performed using the log rank test. Univariate and multivariable hazard ratios are calculated using the Cox proportion hazard model. For comparisons between the baseline variables, the χ2 test and Fisher’s exact test were performed. P values< 0.05 are considered statistically significant.
Discussion
There is no uniform standard for CK-SBRT dose schedule of hepatocellular carcinoma. We intend to conduct this study exploring the relation between BED10, efficacy and adverse reaction.
Our previous retrospective study [10] showed that the 1-, 2- and 3-year PFS, OS and distant metastasis- free survival (DMFS) rates were significantly higher in the BED10 ≥ 100Gy group than in the BED10 < 100Gy group (OS: p = 0.020; PFS: p = 0.017; DMFS: p = 0.012). However, LC in two groups were not of statistically significance. We speculated the result was relative to immune microenvironment. Previous studies [11, 12] reported the results of animal experiments of other types of carcinoma, which showed antitumor immunity significantly contributes to the superior response induced by higher single dose when the total dose remained the same. On the one hand, we conduct an animal experiment to explore antitumor immunity of hepatocellular carcinoma, and further experiments are in progress. On the other hand, our previous study was retrospective study, which may be biased. The result of this prospective study will be more credible.
Adverse reactions of hepatocellular carcinoma CK-SBRT are not ignored. Child-Pugh score and ICG R15 are all parameters to evaluate liver function, which are predicting factor of RILD in previous studies [13, 14]. It is worth mentioning that Child-Pugh score progression (increasing by two or more scores) is also a clinical metric for RILD [15]. As the BED10 of prescribed doses increase, so do the doses of the normal liver. Therefore, the study also focuses on predictors of RILD.
Conclusion
Combining BED10 with radiation injury, the optimal CK-SBRT schedule of hepatocellular carcinoma is worth to explore.
Availability of data and materials
Materials and methods are available in the clinicaltrail.gov.
Abbreviations
- BED:
-
Biologically effective dose
- CK:
-
CyberKnife
- CP:
-
Child-Pugh
- CT:
-
Computed tomography
- ECOG:
-
Eastern cooperative oncology group
- GTV:
-
Gross target volume
- LC:
-
Local control
- MRI:
-
Magnetic resonance imaging
- OS:
-
Overall survival
- PD:
-
Progressive disease
- PTV:
-
Planning target volume
- RFA:
-
Radiofrequency ablation
- RILD:
-
Radiation-induced liver disease
- SBRT:
-
Stereotactic body radiotherapy
References
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394–424.
Zhang T, Sun J, He W, Li H, Piao J, Xu H, Duan X. Stereotactic body radiation therapy as an effective and safe treatment for small hepatocellular carcinoma. BMC Cancer. 2018;18(1):451.
Beskow C, Ågrencronqvist AK, Lewensohn R, Tomadasu I: Biological effective dose evaluation and assessment of rectal and bladder complications for cervical cancer treated with radiotherapy and surgery. J Contemp Brachytherapy 2012;4(4):205–12.
Zhu L, Zhang S, Xu X, Wang B, Wu K, Deng Q, Xia B, Ma S, Yang F. Increased Biological Effective Dose of Radiation Correlates with Prolonged Survival of Patients with Limited-Stage Small Cell Lung Cancer: A Systematic Review. PLOS ONE. 2016;11(5):e0156494.
Lawrence TS, Robertson JM, Anscher MS, Jirtle RL, Ensminger WD, Fajardo LF. Hepatic toxicity resulting from cancer treatment. Int J Radiation Oncol Biol Phys. 1995;31(5):1237.
Liang SX, Huang XB, Zhu XD, Zhang WD, Cai L, Huang HZ, Li YF, Chen L, Liu MZ. Dosimetric predictor identification for radiation-induced liver disease after hypofractionated conformal radiotherapy for primary liver carcinoma patients with child–Pugh grade a cirrhosis. Radiother Oncol. 2011;98(2):265–9.
Pan CC, Kavanagh BD, Dawson LA, Li XA, Das SK, Miften M, Ten Haken RK. Radiation-associated liver injury. Int J Radiat Oncol Biol Phys. 2010;76(3):S94–S100.
Cox JD, Stetz J, Pajak TF. Toxicity criteria of the Radiation Therapy Oncology Group (RTOG) and the European organization for research and treatment of cancer (EORTC). Int J Radiat Oncol Biol Phys. 2015;31(5):1341–6.
Benedict SH, Yenice KM, Followill D, Galvin JM, Hinson W, Kavanagh B, Keall P, Lovelock M, Meeks S, Papiez L. Stereotactic body radiation therapy: the report of AAPM task group 101. Med Phys. 2010;37(8):4078–101.
S J, Z T, W J, L W, Z A, H W, Z D, L D, D J, D X. Biologically effective dose (BED) of stereotactic body radiation therapy (SBRT) was an important factor of therapeutic efficacy in patients with hepatocellular carcinoma (≤5 cm). BMC Cancer. 2019;19(1):846.
Youjin L, Auh SL, Yugang W, Byron B, Yang W, Yuru M, Michael B, Rohit S, Robert C, Tony T. Therapeutic effects of ablative radiation on local tumor require CD8+ T cells: changing strategies for cancer treatment. Blood. 2009;114(3):589.
Schaue D, Ratikan JA, Iwamoto KS, Mcbride WH. Maximizing tumor immunity with fractionated radiation. Int J Radiat Oncol Biol Phys. 2012;83(4):1306–10.
Yoon HI, Koom WS, Lee IJ, Jeong K, Chung Y, Kim JK, Lee KS, Han KH, Seong J. The significance of ICG-R15 in predicting hepatic toxicity in patients receiving radiotherapy for hepatocellular carcinoma. Liver Int. 2012;32(7):1165-1171.
Jun BG, Kim YD, Cheon GJ, Kim ES, Jwa E, Kim SG, Kim YS, Kim BS, Jeong SW, Jang JY, Lee SH, Kim HS. Clinical significance of radiation-induced liver disease after stereotactic body radiation therapy for hepatocellular carcinoma. Korean J Int Med. 2018;33(6):1093-1102.
C TR, B SR, S SK, Y RH, K SW, P JO, Y L, H WP, J GE, L IW, et al. Toward consensus reporting of radiation-induced liver toxicity in the treatment of primary liver malignancies: defining clinically relevant endpoints. Pract Radiat Oncol. 2018;8(3):157–66.
Acknowledgements
We appreciate Ye Lin (University of Chinese Academy of Sciences) for her great help in editing support.
Funding
This study protocol was supported by grants from Beijing Municipal Science and Technology Commission Fund (Z171100001017181).
Author information
Authors and Affiliations
Contributions
XD is the principle investigator and designed the protocol of this study. JS drafted the manuscript. JS, AZ and WL participated in clinical protocol. DL and DZ participated in physical protocol. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Institutional Review Board of 302 Hospital of PLA (People’s Liberation Army). The Ethics number is 2017111D.
Consent for publication
Not Applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Sun, J., Zhang, A., Li, W. et al. Biologically effective dose (BED) escalation of stereotactic body radiotherapy (SBRT) for hepatocellular carcinoma patients (≤5 cm) with CyberKnife: protocol of study. Radiat Oncol 15, 20 (2020). https://doi.org/10.1186/s13014-020-1471-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13014-020-1471-1