Abstract
Background
Although the importance of context in implementation science is not disputed, knowledge about the actual impact of external context variables on implementation processes remains rather fragmented. Current frameworks, models, and studies merely describe macro-level barriers and facilitators, without acknowledging their dynamic character and how they impact and steer implementation. Including organizational theories in implementation frameworks could be a way of tackling this problem. In this study, we therefore investigate how organizational theories can contribute to our understanding of the ways in which external context variables shape implementation processes. We use the implementation process of goal-oriented primary care in Belgium as a case.
Methods
A qualitative study using in-depth semi-structured interviews was conducted with actors from a variety of primary care organizations. Data was collected and analyzed with an iterative approach. We assessed the potential of four organizational theories to enrich our understanding of the impact of external context variables on implementation processes. The organizational theories assessed are as follows: institutional theory, resource dependency theory, network theory, and contingency theory. Data analysis was based on a combination of inductive and deductive thematic analysis techniques using NVivo 12.
Results
Institutional theory helps to understand mechanisms that steer and facilitate the implementation of goal-oriented care through regulatory and policy measures. For example, the Flemish government issued policy for facilitating more integrated, person-centered care by means of newly created institutions, incentives, expectations, and other regulatory factors. The three other organizational theories describe both counteracting or reinforcing mechanisms. The financial system hampers interprofessional collaboration, which is key for GOC. Networks between primary care providers and health and/or social care organizations on the one hand facilitate GOC, while on the other hand, technology to support interprofessional collaboration is lacking. Contingent variables such as the aging population and increasing workload and complexity within primary care create circumstances in which GOC is presented as a possible answer.
Conclusions
Insights and propositions that derive from organizational theories can be utilized to expand our knowledge on how external context variables affect implementation processes. These insights can be combined with or integrated into existing implementation frameworks and models to increase their explanatory power.
Similar content being viewed by others
Background
In this study, we integrate organizational theories to provide a profound analysis on how external context influences the implementation of complex interventions. There is a growing recognition that the context in which an intervention takes place highly influences implementation outcomes [1, 2]. Despite its importance, researchers are challenged by the lack of a clear definition of context. Most implementation frameworks and models do not define context as such, but describe categories or elements of context, without capturing it as a whole [2, 3]. Studies often distinguish between internal and external context: micro- and meso-level internal context variables are specific to a person, team, or organization. Macro-level external context variables consist of variables on a broader, socio-economic and policy level that are beyond one’s control [4].
Overall, literature provides a rather fragmented and limited perspective on how external context influences the implementation process of a complex intervention. Attempts are made to define, categorize, and conceptualize external context [5, 6]. Certain implementation frameworks and models specifically mention external context, such as the conceptual model of evidence-based practice implementation in public service sectors [7], the Consolidated Framework for Implementation Research [8], or the i-PARiHS framework [9]. However, they remain limited to identifying and describing external context variables. Few studies are conducted that specifically point towards the actual impact of macro-level barriers and facilitators [10,11,12] but only provide limited insights in how these shape an implementation process. Nonetheless, external contextual variables can be highly disruptive for an organization’s implementation efforts, for example, when fluctuations in funding occur or when new legislation or technology is introduced [13]. In order to build a more comprehensive view on external context influences, we need an elaborative theoretical perspective.
Organizational theories as a frame of reference
To better understand how the external context affects the implementation process of a primary care intervention, we build upon research of Birken et al. [13] who demonstrate the explanatory power of organizational theories. Organizational theories can help explain the complex interactions between organizations and their environments [13], providing understanding on the impact of external context on the mechanism of change in an implementation process. We focus on three of the theories Birken et al. [8] put forward: institutional theory, resource dependency theory, and contingency theory. We also include network theory in recognition of the importance of interorganizational context and social ties between various actors, especially in primary care settings which are characterized by a multitude of diverse actors (meaning: participants of a process).
These four organizational theories demonstrate the ways in which organizations interact with their external environment in order to sustain and fulfill their core activities. All four of them do this with a different lens. Institutional theory states that an organization will aim to fulfil the expectations, values, or norms that are posed upon them in order to achieve a fit with their environment [14]. This theory helps to understand the relationships between organizations and actors and the institutional context in which they operate. Institutions can broadly be defined as a set of expectations for social or organizational behavior that can take the form formal structures such as regulatory entities, legislation, or procedures [15]. Resource dependency theory explains actions and decisions of organizations in terms of their dependence on critical and important resources. It postulates that organizations will respond to their external environment to secure the resources they need to operate [16, 17]. This theory helps to gain insight in how fiscal variables can shape the adoption of an innovation. Contingency theory presupposes that an organizations’ effectiveness depends on the congruence between situational factors and organizational characteristics [18]. External context variables such as social and economic change and pressure can impact the way in which an innovation will be integrated. Lastly, network theory in its broader sense underlines the strength of networks: collaborating in networks can establish an effectiveness in which outcomes are achieved that could not be realized by individual organizations acting independently. Networks are about connecting or sharing information, resources, activities, and competences of three or more organizations aiming to achieve a shared goal or outcome [19, 20]. Investigating networks helps to gain understanding of the importance of the interorganizational context and how social ties between organizations affect the implementation process of a complex intervention.
Goal-oriented care in Flanders as a case
In this study, we focus on the implementation of the approach goal-oriented care (GOC) in primary care in Flanders, the Dutch-speaking region in Belgium. Primary care is a highly institutionalized and regulated setting with a high level of professionalism. Healthcare organizations can be viewed as complex adaptive systems that are increasingly interdependent [21]. The primary care landscape in Flanders is characterized by many primary care providers (PCPs) being either self-employed or working in group practices or community health centers. They are organized and financed at different levels (federal, regional, local). In 2015–2019, a primary care reform was initiated in Flanders in which the region was geographically divided into 60 primary care zones that are governed by care councils. The Flemish Institute of Primary Care was created as a supporting institution aiming to strengthen the collaboration between primary care health and welfare actors. The complex and multisectoral nature of primary care in Flanders forms an interesting setting to gain understanding in how macro-level context variables affect implementation processes.
The concept of GOC implies a paradigm shift [22] that shifts away from a disease or problem-oriented focus towards a person-centered focus that departs from “what matters to the patient.” Boeykens et al. [23] state in their concept analysis that GOC could be described as a healthcare approach encompassing a multifaceted, dynamic, and iterative process underpinned by the patient’s context and values. The process is characterized by three stages: goal elicitations, goal setting, and goal evaluation in which patients’ needs and preferences form the common thread. It is an approach in which PCPs and patients collaborate to identify personal life goals and to align care with those goals [23]. An illustration of how this manifests at individual level can be found in Table 1. The concept of GOC was incorporated in Flemish policies and included in the primary care reform in 2015–2019. It has gained interest in research and policy as a potential catalyst for integrated care [24]. As such, the implementation of GOC in Flanders provides an opportunity to investigate the external context of a complex primary care intervention. Our main research question is as follows: what can organizational theories tell us about the influence of external context variables on the implementation process of GOC?
Methods
We assess the potential of four organizational theories to enrich our understanding of the impact of external context variables on implementation processes. The organizational theories assessed are as follows: institutional theory, resource dependency theory, network theory, and contingency theory. Qualitative research methods are most suitable to investigate such complex matters, as they can help answer “how” and “why” questions on implementation [25]. We conducted online, semi-structured in-depth interviews with various primary care actors. These actors all had some level of experience at either meso- or micro-level with GOC implementation efforts.
Sample selection
For our purposive sample, we used the following inclusion criteria: 1) working in a Flemish health/social care context in which initiatives are taken to implement GOC and 2) having at least 6 months of experience. For recruitment, we made an overview of all possible stakeholders that are active in GOC by calling upon the network of the Primary Care Academy (PCA)Footnote 1. Additionally, a snowballing approach was used in which respondents could refer to other relevant stakeholders at the end of each interview. This leads to respondents with different backgrounds (not only medical) and varying roles, such as being a staff member, project coordinator, or policy maker. We aimed at a maximum variation in the type of organizations which were represented by respondents, such as different governmental institutions and a variety of healthcare/social care organizations. In some cases, paired interviews were conducted [26] if the respondents were considered complementary in terms of expertise, background, and experience with the topic. An information letter and a request to participate was send to each stakeholder by e-mail. One reminder was sent in case of nonresponse.
Data collection
Interviews were conducted between January and June 2022 by a sociologist trained in qualitative research methods. Interviewing took place online using the software Microsoft Teams and were audio-recorded and transcribed verbatim. A semi-structured interview guide was used, which included (1) an exploration of the concept of GOC and how the respondent relates to this topic, (2) questions on how GOC became a topic of interest and initiatives within the respondent’s setting, and (3) the perceived barriers and facilitators for implementation. An iterative approach was used between data collection and data analysis, meaning that the interview guide underwent minor adjustments based on proceeding insights from earlier interviews in order to get richer data.
Data analysis
All data were thematically analyzed, both inductively and deductively, supported by the software NVivo 12©. For the inductive part, implicit and explicit ideas within the qualitative data were identified and described [27]. The broader research team, with backgrounds in sociology, medical sciences, and social work, discussed these initial analyses and results. The main researcher then further elaborated this into a broad understanding. This was followed by a deductive part, in which characteristics and perspectives from organizational theories were used as sensitizing concepts, inspired by research from Birken et al. [13]. This provided a frame of reference and direction, adding interpretive value to our analysis [28]. These analyses were subject of peer debriefing with our cooperating research team to validate whether these results aligned with their knowledge of GOC processes. This enhances the trustworthiness and credibility of our results [29, 30]. Data analysis was done in Dutch, but illustrative quotes were translated into English.
Results
In-depth interviews were performed with n = 23 respondents (see Table 2): five interviews were duo interviews, and one interview took place with n = 3 respondents representing one organization. We had n = 6 refusals: n = 3 because of time restraints, n = 1 did not feel sufficiently knowledgeable about the topic, n = 1 changed professional function, and there was n = 1 nonresponse. Respondents had various ways in which they related towards the macro-context: we included actors that formed part of external context (e.g., the Flemish Agency of Care and Health), actors that facilitate and strengthen organizations in the implementation of GOC (e.g., the umbrella organization for community health centers), and actors that actively convey GOC inside and outside their setting (e.g., an autonomous and integral home care service). Interviews lasted between 47 and 72 min. Table 3 gives an overview on the main findings of our deductive analysis with their respective links to the propositions of each of the organizational theories that we applied as a lens.
Institutional theory: laying foundations for a shift towards GOC
For the implementation of GOC in primary care, looking at the data with an institutional theory lens helps us understand the way in which primary care organizations will respond to social structures surrounding them. Institutional theory describes the influence of institutions, which give shape to organizational fields: “organizations that, in the aggregate, constitute a recognized area of institutional life [31], p. 148. Prevailing institutions within primary care in Flanders can affect how organizations within such organizational fields fulfil their activities. Throughout our interviews, we recognized several dynamics that are being described in institutional theory.
First of all, the changing landscape of primary care in Flanders (see 1.2) was often brought up as a dynamic in which GOC is intertwined with other changes. Respondents mention an overall tendency to reform primary care to becoming more integrated and the ideas of person-centered care becoming more upfront. These expectations in how primary care should be approached seem to affect the organizational field of primary care: “You could tell that in people’s minds they are ready to look into what it actually means to put the patient, the person central. — INT01” Various policy actors are committed to further steer towards these approaches: “the government has called it the direction that we all have to move towards. — INT23” It was part of the foundations for the most recent primary care reform, leading to the creation of demographic primary care zones governed by care councils and the Flemish Institute of Primary Care as supporting institution.
These newly established actors were viewed by our respondents as catalysts of GOC. They pushed towards the aims to depart from local settings and to establish connections between local actors. Overall, respondents emphasized their added value as they are close to the field and they truly connect primary care actors. “They [care councils] have picked up these concepts and have started working on it. At the moment they are truly the incubators and ecosystems, as they would call it in management slang. — INT04” For an innovation such as GOC to be diffused, they are viewed as the ideal actors who can function as a facilitator or conduit. They are uniquely positioned as they are closely in contact with the practice field and can be a top-down conduit for governmental actors but also are able to address the needs from bottom-up. “In this respect, people look at the primary care zones as the ideal partners. […] We can start bringing people together and have that helicopter view: what is it that truly connects you? — INT23” However, some respondents also mentioned their difficult governance structure due to representation of many disciplines and organizations.
Other regulatory factors were mentioned by respondents were other innovations or changes in primary care that were intentionally linked to GOC: e.g., the BelRAIFootnote 2 or Flemish Social ProtectionFootnote 3. “The government also provides incentives. For example, family care services will gradually be obliged to work with the BelRAI screener. This way, you actually force them to start taking up GOC. — INT23” For GOC to be embedded in primary care, links with other regulatory requirements can steer PCPs towards GOC. Furthermore, it was sometimes mentioned that an important step would be for the policy level to acknowledge GOC as quality of care and to include the concept in quality standards. This would further formalize and enforce the institutional expectation to go towards person-centered care.
Currently, a challenge on institutional level as viewed by most respondents is that GOC is not or only to a limited extent incorporated in the basic education of most primary care disciplines. This leads to most of PCPs only having a limited understanding of GOC and different disciplines not having a shared language in this matter. “You have these primary health and welfare actors who each have their own approach, history and culture. To bring them together and to align them is challenging. — INT10” The absence of GOC as a topic in basic education is mentioned by various respondents as a current shortcoming in effectively implementing GOC in the wider primary care landscape.
Overall, GOC is viewed as our respondents as a topic that has recently gained a lot interest, both by individual PCPS, organizations, and governmental actors. The Flemish government has laid some foundations to facilitate this change with newly created institutions and incentives. However, other external context variables can interfere in how the concept of GOC is currently being picked up and what challenges arise.
Resource dependency theory: in search for a financial system that accommodates interprofessional collaboration
Another external context variable that affects how GOC can be introduced is the financial system that is at place. To analyze themes that were raised during the interviews with regard to finances, we utilized a resource dependency perspective. This theory presumes that organizations are dependent on financial resources and are seeking ways to ensure their continued functioning [16, 17]. To a certain extent, this collides with the assumptions of institutional theory that foregrounds organization’s conformity to institutional pressures [32]. Resource dependency theory in contrast highlights differentiation of organizations that seek out competitive advantages [32].
In this context, respondents mention that their interest and willingness to move towards a GOC approach are held back by the current dominant system of pay for performance in the healthcare system. This financial system is experienced as restrictive, as it does not provide any incentive to PCPs for interprofessional collaboration, which is key for GOC. A switch to a flat fee system (in which a fixed fee is charged for each patient) or bundled payment was often mentioned as desirable. PCPs and health/social care organizations working in a context where they are financially rewarded for a trajectory or treatment of a patient in its entirety ensure that there is no tension with their necessity to obtain financial resources, as described in the resource dependency theory. Many of our respondents voice that community health centers are a good example. They cover different healthcare disciplines and operate with a fixed price per enrolled patient, regardless of the number of services for that patient. This promotes setting up preventive and health-promoting actions, which confirms our finding on the relevance of dedicated funding.
At the governmental level, the best way to finance and give incentives is said to be a point of discussion: “For years, we have been arguing about how to finance. Are we going to fund counsel coordination? Or counsel organization? Or care coordination? — INT04” Macro-level respondents do however mention financial incentives that are already in place to stimulate interprofessional collaboration: fees for multidisciplinary consultation being the most prominent. Other examples were given in which certain requirements were set for funding (e.g., ImpulseoFootnote 4, VIPAFootnote 5) that stimulate actors or settings in taking steps towards more interprofessional collaboration.
Nowadays, financial incentives to support organizations to engage in GOC tend to be project grants. However, a structural way to finance GOC approaches is currently lacking, according to our respondents. As a consequence, a long-term perspective for organizations is lacking; there is no stable financing and organizations are obliged to focus on projects instead of normalizing GOC in routine practice. According to a resource dependency perspective, the absence of financial incentives for practicing GOC hinders organizations in engaging with the approach, as they are focused on seeking out resources in order to fulfil their core activities.
A network-theory perspective: the importance of connectedness for the diffusion of an innovation
Throughout the interviews, interorganizational contextual elements were often addressed. A network theory lens states that collaborating in networks can lead to outcomes that could not be realized by individual organizations acting independently [19, 20]. Networks consist of a set of actors such as PCPs or health/social care organizations along with a set of ties that link them [33]. These ties can be state-type ties (e.g., role based, cognitive) or event-type ties (e.g., through interactions, transactions). Both type of ties can enable a flow in which information or innovations can pass, as actors interact [33]. To analyze the implementation process of GOC and how this is diffused through various actors, a network theory perspective can help understand the importance of the connection between actors.
A first observation throughout the interviews in which we notice the importance of networks was in the mentioning of local initiatives that already existed before the creation of the primary care zones/care councils. In the area around Ghent, local multidisciplinary networks already organized community meetings, bringing together different PCPs on overarching topics relating to long-term care for patients with chronic conditions. These regions have a tradition of collaboration and connectedness of PCPs, which respondents mention to be highly valuable: “This ensures that we are more decisive, speaking from one voice with regards to what we want to stand for. — INT23” Respondents voice that the existence of such local networks has had a positive effect on the diffusion of ideas such as GOC, as trust between different actors was already established.
Further mentioning of the importance of networks could be found in respondents acknowledging one of the presumptions of network theory: working collaboratively towards a specific objective leads to outcomes that cannot be realized independently. This is especially true for GOC, an approach that in essence requires different disciplines to work together: “When only one GP, nurse or social worker starts working on it, it makes no sense. Everyone who is involved with that person needs to be on board. Actually, you need to finetune teams surrounding a person — INT11.” This is why several policy-level respondents mentioned that emphasis was placed on organizing GOC initiatives in a neighborhood-oriented way, in which accessible, inclusive care is aimed at by strengthening social cohesion. This way, different types of PCPs got to know each other through these sessions an GOC and would start to get aligned on what it means to provide GOC. However, in particular, self-employed PCPs are hard to reach. According to our respondents, occupational groups and care councils are suitable actors to engage these self-employed PCPs, but they are not always much involved in such a network.
To better connect PCPs and health/social care organizations, the absence of connectedness through the technological landscape is also mentioned. Current technological systems and platforms for documenting patient information do not allow for aligning and sharing between disciplines. In Flanders, there is a history of each discipline developing its own software, which lacks centralization or unification: “For years, they have decided to just leave it to the market, in such a way that you ended up with a proliferation of software, each discipline having its own package. — INT06” Most of the respondents mentioning this were aware that Flanders government is currently working on a unified digital care and support platform and were optimistic about its development.
Contingency theory: how environmental pressure can be a trigger for change
Our interviews were conducted during a rather dynamic and unique period of time in which the impact of social change and pressure was clearly visible: the Flemish primary care reform was ongoing which leads to the creation of care councils and VIVEL (see 3.1.1), and the COVID crisis impacted the functioning of these and other primary care actors. These observed effects of societal changes are reminiscent of the assumptions that are made in contingency theory. In essence, contingency theory presupposes that “organizational effectiveness results from fitting characteristics of the organization, such as its structure, to contingencies that reflect the situation of the organization [34], p. 1.” When it comes to the effects of the primary care reform and the COVID crisis, there were several mentions on how primary care actors reorganized their activities to adapt to these circumstances. Representatives of care councils/primary care zones whom we interviewed underlined that they were just at the point where they could again engage with their original action plans, not having to take up so many COVID-related tasks anymore. On the one hand, the COVID crisis had however forced them to immediately become functional and has also contributed that various primary care actors quickly got to know them. On the other hand, the COVID crisis has also kept them from their core activities for a while. On top of that, the crisis has also triggered a change the overall view towards data sharing. Some respondents mention a rather protectionist approach towards data sharing, while data sharing has become more normalized during the COVID crisis. This discussion was also relevant for the creation of a unified shared patient record in terms of documenting and sharing patient goals.
Other societal factors that were mentioned having an impact on the uptake of GOC are the demographic composition of a certain area. It was suggested that areas that are characterized by a patient population with more chronic care needs will be more likely to steer towards GOC as a way of coping with these complex cases. “You always have these GPs who blow it away immediately and question whether this is truly necessary. They will only become receptive to this when they experience needs for which GOC can be a solution — INT11.” On a macro-level, several respondents have mentioned how a driver for change is to have the necessity for change becoming very tangible. As PCPs are confronted with increasing numbers of patients with complex, chronic needs and their work becomes more demanding, the need for change becomes more acute. This finding is in line with what contingency theory underlines: changes in contingency (e.g., the population that is increasingly characterized by aging and multimorbidity) are an impetus for change for health/social care organizations to resolve this by adopting a structure that better fits the current environmental characteristics [34].
Discussion
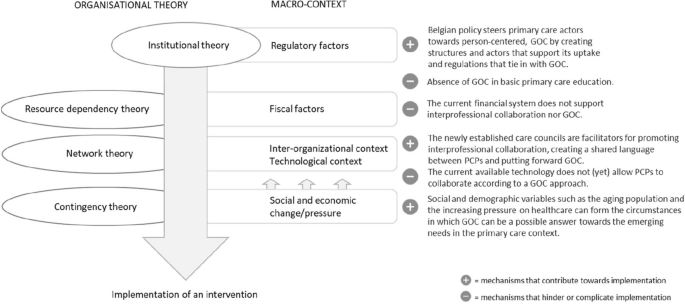
Our research demonstrates the applicability of organizational theories to help explain the impact that macro-level context variables have on an implementation process. These insights can be integrated into existing implementation frameworks and models to add the explanatory power of macro-level context variables, which is to date often neglected. The organizational theories demonstrate the ways in which organizations interact with their external environment in order to sustain and fulfill their core activities. As demonstrated in Fig. 1, institutional theory largely explains how social expectations in the form of institutions lead towards the adoption or implementation of innovation, such as GOC. However, other organizational theories demonstrate how other macro-context elements on different areas can either strengthen or hamper the implementation process.
Departing from the mechanisms that are postulated by institutional theory, we observed that the shift towards GOC is part of a larger Flemish primary care reform in which and new institutions have been established and polices have been drawn up to go towards more integrated, person-centered care. To achieve this, governmental actors have placed emphasis on socialization of care, the local context, and establishing ties between organizations in order to become more complementary in providing primary health care [35]. With various initiatives surrounding this aim, the Flemish government is steering towards GOC. This is reminiscent of the mechanisms that are posed within institutional theory: organizations adapt to prevailing norms and expectations and mimic behaviors that are surrounding them [15, 36].
Throughout our data, we came across concrete examples of how institutionalization takes place. DiMaggio and Powell [31] describe the subsequent process of isomorphism: organizations start to resemble each other as they are conforming to their institutional environment. A first mechanism through which this change occurs is coercive isomorphism and is clearly noticeable in our data. This type of isomorphism results from both formal and informal pressure coming from organizations from which a dependency relationship exists and from cultural expectations in the society [31]. Person-centered, GOC care is both formally propagated by governmental institutions and procedures and informally expected by current social tendencies. Care councils within primary care zones explicitly propagate and disseminate ideas and approaches that are desirable on policy level. Another form of isomorphism is professional isomorphism and relates to our finding that incorporation of GOC in basic education is currently lacking. The presumptions of professional isomorphism back up the importance of this: values, norms, and ideas that are developed during education are bound to find entrance within organizations as professionals start operating along these views.
Although many observations in our data back up the assumptions of institutional theory, it should be noticed that new initiatives such as the promotion of person-centered care and GOC can collide with earlier policy trends. Martens et al. [12] have examined the Belgian policy process relating three integrated care projects and concluded that although there is a strong support for a change towards a more patient-centered system, the current provider-driven system and institutional design complicate this objective. Furthermore, institutional theory tends to simplify actors as passive adopters of institutional norms and expectations and overlook the human agency and sensemaking that come with it [37]. For GOC, it is particularly true that PCPs will actively have to seek out their own style and fit the approach in their own way of working. Moreover, GOC was not just addressed as a governmental expectation but for many PCPs something they inherently stood behind.
Resources dependency theory poses that organizations are dependent on critical resources and adapt their way of working in response to those resources [17]. From our findings, it seems that the current financial system does not promote GOC, meaning that the mechanisms that are put forward in resources dependency theory are not set in motion. A macro-level analysis of barriers and facilitators in the implementation of integrated care in Belgium by Danhieux et al. [10] also points towards the financial system and data sharing as two of the main contextual determinants that affect implementation.
Throughout our data, the importance of a network approach was frequently mentioned. Interprofessional collaboration came forward as a prerequisite to make GOC happen, as well as active commitment on different levels. Burns, Nembhard, and Shortell [38] argue that research efforts on implementing person-centered, integrated care should have more focus on the use of social networks to study relational coordination. In terms of interprofessional collaboration, to date, Belgium has a limited tradition of working team-based with different disciplines [35]. However, when it comes to strengthening a cohesive primary care network, the recently established care councils have become an important facilitator. As a network governance structure, they resemble mostly a Network Administrative Organization (NAO): a separate, centralized administrative entity that is externally governed and not another member providing its own services [19]. According to Provan and Kenis [19], this type of governance form is most effective in a rather dense network with many participants, when the goal consensus is moderately high, characteristics that are indeed representative for the Flemish primary care landscape. This strengthens our observation that care councils have favorable characteristics and are well-positioned to facilitate the interorganizational context to implement GOC.
Lastly, the presumptions within contingency theory became apparent as respondents talked about how the need for change needs to become tangible for PCPs and organizations to take action, as they are increasingly faced with a shortage of time and means and more complex patient profiles. Furthermore, De Maeseneer [39] affirms our findings that the COVID-19 crisis could be employed as an opportunity to strengthen primary health care, as health becomes prioritized and its functioning becomes re-evaluated. Overall, contingency theory can help gain insight in how and why certain policy trends or decisions are made. A study of Bruns et al. [40] found that modifiable external context variables such as interagency collaboration were predictive for policy support for intervention adoption, while unmodifiable external context variable such as socio-economic composition of a region was more predictive for fiscal investments that are made.
Strengths and limitations
This study contributes to our overall understanding of implementation processes by looking into real-life implementation efforts for GOC in Flanders. It goes beyond a mere description of external context variables that affect implementation processes but aims to grasp which and how external context variables influence implementation processes. A variety of respondents from different organizations, with different backgrounds and perspectives, were interviewed, and results were analyzed by researchers with backgrounds in sociology, social work, and medical sciences. Results can not only be applied to further develop sustainable implementation plans for GOC but also enhance our understanding of how the external context influences and shapes implementation processes. As most research on contextual variables in implementation processes has until now mainly focused on internal context variables, knowledge on external context variables contributes to gaining a bigger picture of the mechanism of change.
However, this study is limited to the Flemish landscape, and external context variables and their dynamics might differ from other regions or countries. Furthermore, our study has examined and described how macro-level context variables affect the overall implementation processes of GOC. Further research is needed on the link between outer and inner contexts during implementation and sustainment, as explored by Lengninck-Hall et al. [41]. Another important consideration is that our sample only includes the “believers” in GOC and those who are already taking steps towards its implementation. It is possible that PCPs themselves or other relevant actors who are more skeptical about GOC have a different view on the policy and organizational processes that we explored. Furthermore, data triangulations in which this data is complemented with document analysis could have expanded our understanding and verified subjective perceptions of respondents.
Conclusion
Insights and propositions that derive from organizational theories can be utilized to expand our knowledge on how external context variables affect implementation processes. Our research demonstrates that the implementation of GOC in Flanders is steered and facilitated by regulatory and policy variables, which sets in motion mechanisms that are described in institutional theory. However, other external context variables interact with the implementation process and can further facilitate or hinder the overall implementation process. Assumptions and mechanisms explained within resource dependency theory, network theory, and contingency theory contribute to our understanding on how fiscal, technological, socio-economic, and interorganizational context variables affect an implementation process.
Availability of data and materials
The datasets generated and/or analyzed during the current study are not publicly available due to confidentiality guaranteed to participants but are available from the corresponding author on reasonable request.
Notes
The Primary Care Academy (PCA) is a research and teaching network of four Flemish universities, six university colleges, the White and Yellow Cross (an organization for home nursing), and patient representatives that have included GOC as one of their main research domains.
BelRAI, the Belgian implementation of the interRAI assessment tools; these are scientific, internationally validated instruments enabling an assessment of social, psychological, and physical needs and possibilities of individuals in different care settings. The data follows the person and is shared between care professionals and care organizations.
The Flemish Social Protection is a mandatory insurance established by the Flemish government to provide a range of concessions to individuals with long-term care and support needs due to illness or disability.
Impulseo, financial support for general practitioners who start an individual practice or join a group practice
VIPA, grants for the realization of sustainable, accessible, and affordable healthcare infrastructure
Abbreviations
- GOC:
-
Goal-oriented care
- PCP:
-
Primary care provider
- PCA:
-
Primary Care Academy
References
Squires JE, Graham ID, Hutchinson AM, Michie S, Francis JJ, Sales A, et al. Identifying the domains of context important to implementation science: a study protocol. Implement Sci. 2015;10(1):1–9.
Nilsen P, Bernhardsson S. Context matters in implementation science: a scoping review of determinant frameworks that describe contextual determinants for implementation outcomes. BMC Health Serv Res. 2019;19(1):1–21.
Rogers L, De Brún A, McAuliffe E. Defining and assessing context in healthcare implementation studies: a systematic review. BMC Health Serv Res. 2020;20(1):1–24.
Huybrechts I, Declercq A, Verté E, Raeymaeckers P, Anthierens S. The building blocks of implementation frameworks and models in primary care: a narrative review. Front Public Health. 2021;9:675171.
Hamilton AB, Mittman BS, Eccles AM, Hutchinson CS, Wyatt GE. Conceptualizing and measuring external context in implementation science: studying the impacts of regulatory, fiscal, technological and social change. Implement Sci. 2015;10 BioMed Central.
Watson DP, Adams EL, Shue S, Coates H, McGuire A, Chesher J, et al. Defining the external implementation context: an integrative systematic literature review. BMC Health Serv Res. 2018;18(1):1–14.
Aarons GA, Hurlburt M, Horwitz SM. Advancing a conceptual model of evidence-based practice implementation in public service sectors. Adm Policy Ment Health Ment Health Serv Res. 2011;38:4–23.
Damschroder LJ, Aron DC, Keith RE, Kirsh SR, Alexander JA, Lowery JC. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implement Sci. 2009;4(1):1–15.
Harvey G, Kitson A. PARIHS revisited: from heuristic to integrated framework for the successful implementation of knowledge into practice. Implement Sci. 2015;11(1):1–13.
Danhieux K, Martens M, Colman E, Wouters E, Remmen R, Van Olmen J, et al. What makes integration of chronic care so difficult? A macro-level analysis of barriers and facilitators in Belgium. International. J Integr Care. 2021;21(4).
Hamilton AB, Mittman BS, Campbell D, Hutchinson C, Liu H, Moss NJ, Wyatt GE. Understanding the impact of external context on community-based implementation of an evidence-based HIV risk reduction intervention. BMC Health Serv Res. 2018;18(1):1–10.
Martens M, Danhieux K, Van Belle S, Wouters E, Van Damme W, Remmen R, et al. Integration or fragmentation of health care? Examining policies and politics in a Belgian case study. Int J Health Policy Manag. 2022;11(9):1668.
Birken SA, Bunger AC, Powell BJ, Turner K, Clary AS, Klaman SL, et al. Organizational theory for dissemination and implementation research. Implement Sci. 2017;12(1):1–15.
Powell WW, DiMaggio PJ. The new institutionalism in organizational analysis. University of Chicago Press; 2012.
Zucker LG. Institutional theories of organization. Annu Rev Sociol. 1987;13(1):443–64.
Hillman AJ, Withers MC, Collins BJ. Resource dependence theory: a review. J Manag. 2009;35(6):1404–27.
Nienhüser W. Resource dependence theory-how well does it explain behavior of organizations? Management Revue; 2008. p. 9–32.
Lammers CJ, Mijs AA, Noort WJ. Organisaties vergelijkenderwijs: ontwikkeling en relevantie van het sociologisch denken over organisaties. Het Spectrum. 2000;6.
Provan KG, Kenis P. Modes of network governance: structure, management, and effectiveness. J Public Adm Res Theory. 2008;18(2):229–52.
Kenis P, Provan K. Het network-governance-perspectief. Business performance management Sturen op prestatie en resultaat; 2008. p. 296–312.
Begun JW, Zimmerman B, Dooley K. Health care organizations as complex adaptive systems. Adv Health Care Org Theory. 2003;253:288.
Mold JW. Failure of the problem-oriented medical paradigm and a person-centered alternative. Ann Fam Med. 2022;20(2):145–8.
Boeykens D, Boeckxstaens P, De Sutter A, Lahousse L, Pype P, De Vriendt P, et al. Goal-oriented care for patients with chronic conditions or multimorbidity in primary care: a scoping review and concept analysis. PLoS One. 2022;17(2):e0262843.
Gray CS, Grudniewicz A, Armas A, Mold J, Im J, Boeckxstaens P. Goal-oriented care: a catalyst for person-centred system integration. Int J Integr Care. 2020;20(4).
Hamilton AB, Finley EP. Qualitative methods in implementation research: an introduction. Psychiatry Res. 2019;280:112516.
Wilson AD, Onwuegbuzie AJ, Manning LP. Using paired depth interviews to collect qualitative data. Qual Rep. 2016;21(9):1549.
Guest G, MacQueen KM, Namey EE. Applied thematic analysis. Sage Publications; 2011.
Bowen GA. Grounded theory and sensitizing concepts. Int J Qual Methods. 2006;5(3):12–23.
Connelly LM. Trustworthiness in qualitative research. Medsurg Nurs. 2016;25(6):435.
Morse JM, Barrett M, Mayan M, Olson K, Spiers J. Verification strategies for establishing reliability and validity in qualitative research. Int J Qual Methods. 2002;1(2):13–22.
DiMaggio PJ, Powell WW. The iron cage revisited: institutional isomorphism and collective rationality in organizational fields. Am Sociol Rev. 1983;147-60.
de la Luz F-AM, Valle-Cabrera R. Reconciling institutional theory with organizational theories: how neoinstitutionalism resolves five paradoxes. J Organ Chang Manag. 2006;19(4):503–17.
Borgatti SP, Halgin DS. On network theory. Organ Sci. 2011;22(5):1168–81.
Donaldson L. The contingency theory of organizations. Sage; 2001.
De Maeseneer J, Galle A. Belgium’s healthcare system: the way forward to address the challenges of the 21st century: comment on “Integration or Fragmentation of Health Care? Examining Policies and Politics in a Belgian Case Study”. Int J Health Policy Manag. 2023;12.
Dadich A, Doloswala N. What can organisational theory offer knowledge translation in healthcare? A thematic and lexical analysis. BMC Health Serv Res. 2018;18(1):1–20.
Jensen TB, Kjærgaard A, Svejvig P. Using institutional theory with sensemaking theory: a case study of information system implementation in healthcare. J Inf Technol. 2009;24(4):343–53.
Burns LR, Nembhard IM, Shortell SM. Integrating network theory into the study of integrated healthcare. Soc Sci Med. 2022;296:114664.
De Maeseneer J. COVID-19: using the crisis as an opportunity to strengthen primary health care. Prim Health Care Res Dev. 2021;22:e73.
Bruns EJ, Parker EM, Hensley S, Pullmann MD, Benjamin PH, Lyon AR, Hoagwood KE. The role of the outer setting in implementation: associations between state demographic, fiscal, and policy factors and use of evidence-based treatments in mental healthcare. Implement Sci. 2019;14:1–13.
Lengnick-Hall R, Stadnick NA, Dickson KS, Moullin JC, Aarons GA. Forms and functions of bridging factors: specifying the dynamic links between outer and inner contexts during implementation and sustainment. Implement Sci. 2021;16:1–13.
Acknowledgements
We are grateful for the partnership with the Primary Care Academy (academie-eerstelijn.be) and want to thank the King Baudouin Foundation and Fund Daniël De Coninck for the opportunity they offer us for conducting research and have impact on the primary care of Flanders, Belgium. The consortium of the Primary Care Academy consists of the following: lead author: Roy Remmen—roy.remmen@uantwerpen.be—Department of Primary Care and Interdisciplinary Care, Faculty of Medicine and Health Sciences, University of Antwerp, Antwerp, Belgium; Emily Verté—Department of Primary Care and Interdisciplinary Care, Faculty of Medicine and Health Sciences, University of Antwerp, Antwerp, Belgium, and Department of Family Medicine and Chronic Care, Faculty of Medicine and Pharmacy, Vrije Universiteit Brussel, Brussel, Belgium; Muhammed Mustafa Sirimsi—Centre for Research and Innovation in Care, Faculty of Medicine and Health Sciences, University of Antwerp, Antwerp, Belgium; Peter Van Bogaert—Workforce Management and Outcomes Research in Care, Faculty of Medicine and Health Sciences, University of Antwerp, Belgium; Hans De Loof—Laboratory of Physio-Pharmacology, Faculty of Pharmaceutical Biomedical and Veterinary Sciences, University of Antwerp, Belgium; Kris Van den Broeck—Department of Primary Care and Interdisciplinary Care, Faculty of Medicine and Health Sciences, University of Antwerp, Antwerp, Belgium; Sibyl Anthierens—Department of Primary Care and Interdisciplinary Care, Faculty of Medicine and Health Sciences, University of Antwerp, Antwerp, Belgium; Ine Huybrechts—Department of Primary Care and Interdisciplinary Care, Faculty of Medicine and Health Sciences, University of Antwerp, Antwerp, Belgium; Peter Raeymaeckers—Department of Sociology, Faculty of Social Sciences, University of Antwerp, Belgium; Veerle Bufel—Department of Sociology, Centre for Population, Family and Health, Faculty of Social Sciences, University of Antwerp, Belgium; Dirk Devroey—Department of Family Medicine and Chronic Care, Faculty of Medicine and Pharmacy, Vrije Universiteit Brussel, Brussel; Bert Aertgeerts—Academic Centre for General Practice, Faculty of Medicine, KU Leuven, Leuven, and Department of Public Health and Primary Care, Faculty of Medicine, KU Leuven, Leuven; Birgitte Schoenmakers—Department of Public Health and Primary Care, Faculty of Medicine, KU Leuven, Leuven, Belgium; Lotte Timmermans—Department of Public Health and Primary Care, Faculty of Medicine, KU Leuven, Leuven, Belgium; Veerle Foulon—Department of Pharmaceutical and Pharmacological Sciences, Faculty Pharmaceutical Sciences, KU Leuven, Leuven, Belgium; Anja Declercq—LUCAS-Centre for Care Research and Consultancy, Faculty of Social Sciences, KU Leuven, Leuven, Belgium; Dominique Van de Velde, Department of Rehabilitation Sciences, Occupational Therapy, Faculty of Medicine and Health Sciences, University of Ghent, Belgium, and Department of Occupational Therapy, Artevelde University of Applied Sciences, Ghent, Belgium; Pauline Boeckxstaens—Department of Public Health and Primary Care, Faculty of Medicine and Health Sciences, University of Ghent, Belgium; An De Sutter—Department of Public Health and Primary Care, Faculty of Medicine and Health Sciences, University of Ghent, Belgium; Patricia De Vriendt—Department of Rehabilitation Sciences, Occupational Therapy, Faculty of Medicine and Health Sciences, University of Ghent, Belgium, and Frailty in Ageing (FRIA) Research Group, Department of Gerontology and Mental Health and Wellbeing (MENT) Research Group, Faculty of Medicine and Pharmacy, Vrije Universiteit, Brussels, Belgium, and Department of Occupational Therapy, Artevelde University of Applied Sciences, Ghent, Belgium; Lies Lahousse—Department of Bioanalysis, Faculty of Pharmaceutical Sciences, Ghent University, Ghent, Belgium; Peter Pype—Department of Public Health and Primary Care, Faculty of Medicine and Health Sciences, University of Ghent, Belgium, End-of-Life Care Research Group, Faculty of Medicine and Health Sciences, Vrije Universiteit Brussel and Ghent University, Ghent, Belgium; Dagje Boeykens—Department of Rehabilitation Sciences, Occupational Therapy, Faculty of Medicine and Health Sciences, University of Ghent, Belgium, and Department of Public Health and Primary Care, Faculty of Medicine and Health Sciences, University of Ghent, Belgium; Ann Van Hecke—Department of Public Health and Primary Care, Faculty of Medicine and Health Sciences, University of Ghent, Belgium, University Centre of Nursing and Midwifery, Faculty of Medicine and Health Sciences, University of Ghent, Belgium; Peter Decat—Department of Public Health and Primary Care, Faculty of Medicine and Health Sciences, University of Ghent, Belgium; Rudi Roose—Department of Social Work and Social Pedagogy, Faculty of Psychology and Educational Sciences, University Ghent, Belgium; Sandra Martin—Expertise Centre Health Innovation, University College Leuven-Limburg, Leuven, Belgium; Erica Rutten—Expertise Centre Health Innovation, University College Leuven-Limburg, Leuven, Belgium; Sam Pless—Expertise Centre Health Innovation, University College Leuven-Limburg, Leuven, Belgium; Anouk Tuinstra—Expertise Centre Health Innovation, University College Leuven-Limburg, Leuven, Belgium; Vanessa Gauwe—Department of Occupational Therapy, Artevelde University of Applied Sciences, Ghent, Belgium; Didier ReynaertE-QUAL, University College of Applied Sciences Ghent, Ghent, Belgium; Leen Van Landschoot—Department of Nursing, University of Applied Sciences Ghent, Ghent, Belgium; Maja Lopez Hartmann—Department of Welfare and Health, Karel de Grote University of Applied Sciences and Arts, Antwerp, Belgium; Tony Claeys—LiveLab, VIVES University of Applied Sciences, Kortrijk, Belgium; Hilde Vandenhoudt—LiCalab, Thomas University of Applied Sciences, Turnhout, Belgium; Kristel De Vliegher—Department of Nursing–Homecare, White-Yellow Cross, Brussels, Belgium; and Susanne Op de Beeck—Flemish Patient Platform, Heverlee, Belgium.
Funding
This research was funded by fund Daniël De Coninck, King Baudouin Foundation, Belgium. The funder had no involvement in this study. Grant number: 2019-J5170820-211,588.
Author information
Authors and Affiliations
Consortia
Contributions
IH wrote the main manuscript text. AD, EV, PR, and SA contributed to the different steps of the making of this manuscript. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study protocol was approved by the Medical Ethics Committee of the University of Antwerp/Antwerp University Hospital (reference: 2021-1690). All participants received verbal and written information about the purpose and methods of the study and gave written informed consent.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Huybrechts, I., Declercq, A., Verté, E. et al. How does the external context affect an implementation processes? A qualitative study investigating the impact of macro-level variables on the implementation of goal-oriented primary care. Implementation Sci 19, 32 (2024). https://doi.org/10.1186/s13012-024-01360-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13012-024-01360-0