Abstract
Background
Routine data are increasingly used in randomised controlled trials evaluating healthcare interventions. They can aid participant identification, outcome assessment, and intervention delivery. Randomised implementation trials evaluate the effect of implementation strategies on implementation outcomes. Implementation strategies, such as reminders, are used to increase the uptake of evidence-based interventions into practice, while implementation outcomes, such as adoption, are key measures of the implementation process. The use of routine data in effectiveness trials has been explored; however, there are no reviews on implementation trials. We therefore aimed to describe how routine data have been used in randomised implementation trials and the design characteristics of these trials.
Methods
We searched MEDLINE (Ovid) and Cochrane Central Register of Controlled Trials from Jan 2000 to Dec 2021 and manually searched protocols from trial registers. We included implementation trials and type II and type III hybrid effectiveness-implementation trials conducted using routine data. We extracted quantitative and qualitative data and narratively synthesised findings.
Results
From 4206 titles, we included 80 trials, of which 22.5% targeted implementation of evidence-based clinical guidelines. Multicomponent implementation strategies were more commonly evaluated (70.0%) than single strategies. Most trials assessed adoption as the primary outcome (65.0%). The majority of trials extracted data from electronic health records (EHRs) (62.5%), and 91.3% used routine data for outcome ascertainment. Reported reasons for using routine data were increasing efficiency, assessing outcomes, reducing research burden, improving quality of care, identifying study samples, confirming findings, and assessing representativeness. Data quality, the EHR system, research governance, and external factors such as government policy could act either as facilitators or barriers.
Conclusions
Adherence to guidance on designing and reporting implementation studies, and specifically to harmonise the language used in describing implementation strategies and implementation outcomes, would aid identification of studies and data extraction. Routine healthcare data are widely used for participant identification, outcome assessment and intervention delivery. Researchers should familiarise themselves with the barriers and facilitators to using routine data, and efforts could be made to improve data quality to overcome some of the barriers.
Registration
PROSPERO CRD42022292321.
Similar content being viewed by others
Introduction
The randomised implementation trial (hereafter implementation trial) evaluates the effect of implementation strategies on implementation outcomes [1], in distinction to the effectiveness randomised controlled trial (RCT) which evaluates the impact of healthcare interventions on health-related outcomes. Implementation trials aim to promote the uptake of evidence-based interventions into practice by employing various strategies. For example, text messaging increases the adoption of influenza vaccination [2]. The Expert Recommendations for Implementing Change (ERIC) study [3] identified 73 commonly used implementation strategies, such as audit and feedback, financial incentives, and educational and training sessions. These were then mapped into categories relating to infrastructure change, implementation context, and stakeholders’ support and management [4]. Implementation outcomes are key indicators of the implementation process; they are also intermediate outcomes in relation to health outcomes (e.g. biomarkers, quality of life) [5]. Common implementation outcomes include the adoption of evidence-based interventions [2], the quality of programme delivery (fidelity) [6], the feasibility and acceptability of implementing interventions in a given context [7]. Proctor and colleagues conceptualised implementation outcomes into eight categories, including acceptability, adoption, feasibility, fidelity, appropriateness, penetration, sustainability, and costs [5]. Implementation trials may also report the effect on health-related outcomes. These types of trials have been described as effectiveness-implementation hybrid trial designs [8].
Routine healthcare data (hereafter routine data), obtained from electronic health records (EHR), administrative databases, and registries [9], are not collected for research purposes but are increasingly used for research, for example in the execution of RCTs [10]. The use of routine data in RCTs is deemed a novel trial design to improve the efficiency and effectiveness of RCT delivery, and the value of routine data potentially manifests in various ways [11, 12]. For example, Reeves and colleagues evaluated a weight loss intervention for women following treatment for breast cancer, for which 90 obese participants were recruited from a state-based cancer registry [13]; Sandner and colleagues assessed the effects of a targeted home visiting programme, in which they used administrative data from the German public health insurance system to measure the maternal mental health outcomes [14]; and Downing and colleagues evaluated an EHR-based clinical decision support alert for improving severe sepsis treatments [15].
To address the growing interest in employing routine data in RCTs and to improve the reporting quality, the Consolidated Standards of Reporting Trials extension for randomised controlled trials conducted using cohorts and routinely collected data (CONSORT-ROUTINE) has been developed [10]. The CONSORT-ROUTINE team reviewed published effectiveness RCTs using data from EHRs, registries, and administrative datasets and assessed those trials’ reporting transparency and completeness against the guideline [16,17,18,19]. There is, however, no review focused on how routine data are used in implementation trials. Therefore, the objectives of this review are to (1) describe the characteristics of implementation trial designs conducted using routine data, (2) investigate how routine data were used and reported in these implementation trials, and (3) explore the reported rationales, facilitators, and barriers of using routine data in implementation trials.
Method
We conducted a methodology systematic review [20] to investigate the characteristics of randomised implementation trials using routine healthcare data. The review protocol was previously registered on PROSPERO CRD42022292321, and we report the results according to the PRISMA 2020 checklist [21] (see Additional file 1).
Systematic searches
The literature search was conducted initially in two main databases: MEDLINE via Ovid and Cochrane Library. We originally planned to search Cochrane Methodology Registry, but it has not been updated since 2012 and does not support an advanced search function. We therefore searched Cochrane Central Register of Controlled Trials (CENTRAL) instead to capture all relevant implementation trials. The databases were searched from Jan 2000, due to the growing recognition of electronic health records and implementation science in the last two decades [22], to Dec 2021 (see Additional file 2 for search strategy). A manual search of citations was performed for unpublished and in-progress studies, and trial protocols were tracked in ClinicalTrials.gov, BMC ISRCTN registry, WHO International Clinical Trials Registry Platform, and Australian New Zealand Clinical Trials Registry.
Definitions, inclusion, and exclusion criteria
Eligible RCTs had to be randomised implementation trials evaluating the effectiveness of implementation strategies to promote the uptake of evidence-based interventions/practices/programmes/treatments/services. Three types of implementation trials were considered: (1) implementation trials, where the goal was to assess the impact of implementation strategies only on implementation outcomes; (2) type II hybrid effectiveness-implementation trials, where the co-primary aims were to determine the impact of the implementation strategies on implementation outcomes as well as the effectiveness of the intervention on health outcomes [8]; and (3) type III effectiveness-implementation hybrid trials where the primary focus was on implementation outcomes with the secondary focus on the intervention outcomes [8].
The trials had to use any type of routine data (EHR, administrative dataset, registry) in either (1) trial participants identification and recruitment, (2) outcome ascertainment, (3) intervention delivery, or (4) any combination of these uses. The included trials had to be peer-reviewed articles written in English. Nested economic and process evaluations were excluded. Studies that exclusively focused on health economic outcomes or only reported long-term follow-up outcomes were also excluded. Conference abstracts and study protocols were not included, but we performed a citation search for full publications reporting trial outcomes. A detailed description of inclusion criteria is outlined in Table 1.
Data screening
CX screened titles and abstracts of all searched records; LS independently screened a random sample of 10% of all titles and abstract. Due to poor reporting of implementation trials [16,17,18, 30], we included all publications with potential eligibility at this stage, even if the trials did not specify they were implementation trials or if the trials did not explicitly describe the use of routine data in the abstract. Any disagreements were resolved by discussion and consensus.
Full texts screening was undertaken by two reviewers (C. X. and L. S.). Again, C. X. assessed all full texts, with a random sample of 10% independently screened by L. S. Discrepancies between two reviewers were resolved through consultation with a third reviewer (E. I.). Further disagreements were resolved in consensus meetings with four senior researchers in the review team (C. R., S. E., H. P., A. S.).
Data extraction and analysis
Data extracted from all relevant papers addressed the following: (1) general study characteristics: authors, year of publication, country, setting, health condition, and type of randomisation (individual, cluster); (2) characteristics of trials: type of trials (implementation, hybrid type II, hybrid type III), implementation strategies, comparators, implementation outcomes, and evidence-based interventions; (3) characteristics of routine data: types (EHR, administrative datasets, registries), usage (participant identification, outcome assessment, intervention delivery or combinations), and data linkage; and (4) reported rationales, barriers, and facilitators of using routine data in those trials. Two reviewers (C. X. and E. I.) independently extracted data from four trials (5%, 4/80), compared findings, and agreed on the initial data extraction. C. X. then completed the remaining data extraction. Any uncertainties were discussed with other authors.
Data were extracted into an Excel spreadsheet for analysis by CX. Descriptive statistics were performed using Stata SE v17 to summarise the study characteristics, implementation strategies and outcomes, and the type and usage of routine data. Thematic analysis was conducted to synthesise the reported rationale, barriers, and facilitators.
Results
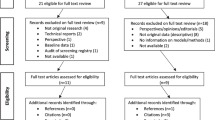
Overall, 4459 citations were retrieved from database searches. After the removal of duplicates, 4206 titles and abstracts were reviewed. Of those unique records, 3885 were excluded after the title and abstract review, and 254 were excluded after the full-text review. Sixty-seven eligible studies met inclusion criteria from database searches. We additionally found 13 trials via study protocols and citation tracking. Eighty studies were therefore included for data extraction. Figure 1 is the PRISMA flow diagram, and references for all eligible studies are provided in Additional file 4.
Study characteristics
Table 2 presents the design and context of the 80 included implementation trials using routine data. Forty-three (53.8%) were cluster RCT designs, and 37 (46.3%) were individual designs. The implementation trials were predominantly conducted in North America (63.8%, n = 51) and in primary care settings (90.0%, n = 72). The most frequently researched medical areas were cardiovascular disease (15.0%, n = 12), general health (13.8%, n = 11), and cancer (13.8%, n = 11).
Characteristics of implementation trials
Of the 80 included studies, 55 (68.8%) were implementation trials, 15 (18.8%) were hybrid type II effectiveness-implementation trials, and 10 (12.5%) were type III hybrid trials. A total of 70.0% (n = 56) of included implementation trials tested multicomponent implementation strategies, while 30.0% (n = 24) used a single strategy to implement evidence-based interventions. Of those using single implementation strategies, manual or computerised reminders were the most commonly used strategies (66.7%, n = 16). Additional file 5 summarises the characteristics of single implementation strategies. Most implementation strategies were compared against usual care or no intervention (75.0%, n = 60), but 25.0% were compared with active components such as letters, education, and training. In general, clinical guidelines (22.5%, n = 18) were the most frequently implemented evidence-based practice among included trials, followed by disease screening programmes (15.0%, n = 12). Seven implementation outcomes (adoption, implementation cost, feasibility, fidelity, penetration, sustainability, acceptability) were mentioned in the included trials, among which adoption/uptake was the most examined (65.0%, n = 52), and 12 implementation trials (15.0%) assessed fidelity. See Table 3 for further details.
Characteristics of the use of routine data
As shown in Table 4, more than half of implementation trials employed EHR/EMR in the trial execution (62.5%, n = 50), while 9 (11.3%) used registry, and 11 (13.8%) used administrative datasets. A total of 61.3% of implementation trials specified the routine healthcare databases used, 16.3% of implementation trials linked data within a single source or across three sources, but fewer than half (n = 5, 38.5%) reported methods for data linkage. Figure 2 depicts the use of routine data, solely used for identifying trial participants in 4 (5.0%) studies, for delivering interventions in 3 (3.8%) studies, and for assessing outcomes in 26 (32.5%) studies. The majority of implementation trials (58.8%, n = 47) used routine data for multiple purposes. Of the 47 trials, the combination of all three approaches received the most attention (n = 21, 44.7%), followed by the combination of participant identification and outcome assessment (n = 18, 38.3%). In Fig. 3, among the three types, administrative datasets were mainly used for assessing outcomes, while registries and EHRs were predominantly used in the combination of participant identification, intervention delivery, and/or outcome ascertainment.
Reported rationales, barriers, and facilitators of using routine data in implementation trials
The thematic synthesis used data extracted from 50 studies. Figures 4 and 5 depict all the themes and subthemes identified that capture the reported rationales, facilitators, and barriers, with purposively selected examples. Seven themes capturing the reported rationales were improving quality of care, assessing outcomes, identifying study samples, assessing representativeness, increasing efficiency, confirming findings from other data sources, and reducing the research burden (Fig. 4). Four themes of reported facilitators and barriers of using routine data in implementation trials were data quality (including accuracy, timeliness, availability, interoperability, specificity, completeness), EHR systems (e.g. the choice of EHR vendors), research governance (e.g. informed consent), and external factors such as government policy (Fig. 5). Additional file 6 (themes of rationales) and Additional file 7 (themes of facilitators and barriers) summarise each theme with full examples extracted from included studies. While the theme of EHR systems in Fig. 5 appears to relate directly to the EHR data type, other themes seem not to be associated with particular routine data or implementation trials.
Discussion
Summary of findings
This review provides an overview of implementation trials conducted using routine data. We identified 80 trials that evaluated the effect of various implementation strategies designed to implement evidence-based interventions. More than half of implementation trials made use of EHRs in the trial delivery for a combination of participant identification, intervention delivery, and/or outcome ascertainment. Routine data were favoured in assessing implementation outcomes in almost all trials. In addition, we identified rationales for using routine data including improving quality of care, assessing outcomes, identifying study samples, assessing representativeness, increasing efficiency, confirming findings, and reducing the research burden. Data quality, the EHR system, research governance, and external factors such as government policy could act either as facilitators or barriers. Among those 80 trials, the most frequently used implementation strategy was reminders, either manual or computerised. Strategies primarily focused on the adoption/uptake of evidence-based interventions, followed by implementation fidelity.
Discussion in relation to published literature
The use of routine data
We found that most implementation trials chose EHRs as their data sources, which is consistent with the findings from CONSORT-ROUTINE reviews of 263 effectiveness RCTs using registries, administrative databases, and EHR [16,17,18,19], in which 70% (n = 183) of RCTs used EHRs. Of those 183 trials, 44% used EHR to perform all three functions (i.e. participant identification, intervention delivery, and outcome assessment) [16], which is in line with our findings. EHR contains longitudinal patient medical history which provides rich clinical information such as disease treatment patterns and standards of care [31] and is therefore useful for studying population health. In the context of clinical trials, it is not novel that EHR databases are used for searching patient eligibility; however, this is often done on-site by GPs which is labour intensive [32]. A centralised approach, such as UK Biobank and the Scottish Health Research Register and Biobank, provides in-depth biological and medical data for screening and locating potentially eligible trial participants, which can reduce the research burden for study personnel and facilitate involvement of patients [33]. The use of EHR data to enhance recruitment has previously been endorsed by the PRINCIPLE trial [34], a UK-wide clinical study investigating potential treatments for COVID-19 in the community. The participants joined the trial online, and their eligibility was checked centrally via data received from GP records. This centralised approach was associated with increased recruitment of people with positive COVID-19 test results, demonstrating the value of routine data in reaching out to a wider population.
The capability of routine data in providing outcome assessment with potentially readily available data is also appealing. A search of NIHR HTA-funded trials registered in 2019 found that 47% of the trials planned to use routine data as a source of outcome data [35]. In our review of implementation trials, nearly all of the trials (91.3%) used routine data for outcome ascertainment. This allows outcomes in the whole eligible population to be measured (as opposed to outcomes in trial participants) and is practical because outcomes in implementation trials are typically adoption rates or service utility, which are routinely recorded for whole populations. In contrast, in the context of effectiveness RCTs, some common outcomes of interest such as biomarkers and patient-reported outcomes are not routinely collected in the databases [11]; thus, other data collection methods may be needed.
Rationales, facilitators, and barriers
EHRs, administrative databases, and registries have been promoted for over a decade as offering opportunities for supporting the design and execution of clinical trials [29, 36]. In 2018, a UK National Workshop was held by the National Institute of Health Research (NIHR), Health Data Research UK, and Clinical Practice Research Datalink, to promote the agenda for data-enabled clinical trials [34]. The COVID-19 pandemic has further accelerated the potential of this innovative trial design. For example, RECOVERY, the world’s largest clinical trial evaluating the potential treatments for COVID-19, has endorsed the vital role of routine data in its success in finding effective treatments [37].
Our findings on the challenges and facilitators of using routine data resonate with the findings in studies of effectiveness RCTs [11, 38,39,40]. In addition to the rationales identified in our review, the ability to provide more generalisable outcomes and conduct long-term follow-up seems to attract the most attention [11, 39, 40]. For example, a 9-year follow-up of the ASCEND trial evaluating the effect of aspirin on cardiovascular events in patients with diabetes is supported by linking electronic hospital episode data [41]. This is also of direct relevance to implementation trials, where the ultimate goal is to implement, scale up, and sustain evidence-based innovations in routine practices, which requires substantial time and resource commitment. With the help of routine data, long-term benefits and harms can be monitored among general populations for extended periods after the trial termination [12].
Nevertheless, obstacles exist that may prevent routine data from achieving its full potential. Data quality is the main concern and has been extensively discussed in healthcare data research. In this review, one trial criticised the EHR data extracted for the research team because they were not in real time [s59], which largely impeded data analysis. Timeliness is a key measurement of data quality; in implementation trials, it is also an enabler of seamlessly translating research findings into daily practice. While some routine data such as EHRs are updated regularly, others such as hospital episode statistics are periodically updated which may not support real-time trial delivery.
Since a single data source may not contain all the information required by the trial, trialists may use and link multiple data sources to evaluate all outcomes [32]. The use of data linkage offers opportunities to address the representativeness of the samples and assess the generalisability of the results, as endorsed by the included studies [s31, s61]. No barriers to data interoperability were noted in the trials collated in this review, though only 13 trials (16.3%) performed and reported data linkage. Nonetheless, the concerns with linking routine data have been widely acknowledged in the literature, for example errors in data linkage (e.g. missed matches or false matches) leading to inaccurate results [42], and technical challenges (e.g. handling changing data), the sheer volume of datasets and different linkage scenarios, increase the complexity and the costs [43]. Data quality needs to be reasonably assured in the trial context especially when it relates to outcome measurement, since poor data quality may undermine trial findings. Aside from data quality issues, common barriers such as costs and training associated with obtaining and managing data [11], complex and time-consuming research governance, and regulatory approvals [11, 38, 40] have been identified in previous studies. Addressing these barriers is of utmost importance to improve trial quality and efficiency.
Randomised implementation trials
In this review, identifying randomised implementation trials was a challenge, despite guidelines on planning and reporting implementation studies [1, 30]. Issues, such as lacking implementation trial labels in trial papers, not indicating implementation research in titles and abstracts, not explicitly naming implementation strategies and implementation outcomes, and confusing terminologies occurring in different publications, led to poor reporting of implementation trials. Similar results have been found in other reviews of implementation studies [44, 45].
Standardising and harmonising the reporting of implementation trials will ease the replication of effective strategies for improving implementation outcomes, thus enhancing the integration of implementation science discoveries into routine practice [46]. Furthermore, it will increase the visibility of literature, thereby improving the quality of evidence synthesis in systematic reviews of implementation trials. Informed by guidelines for designing [1] and reporting [30] implementation studies, we have summarised some key considerations in reporting implementation trials in Table 5. Additionally, the current definition of an implementation trial seems insufficient to capture the full characteristics, given the wide variation in designing and reporting, as well as the introduction of hybrid designs. Therefore, we clarified the definition of an implementation trial as a “research design assessing the effects of implementation strategy(ies) on promoting the evidence-based practice into the daily practice, with the primary focus on the implementation outcome that is distinct from service and patient outcomes”.
Implication: realising the potential of routine data in implementation trials
The use of routine data in RCTs has been widely advocated, but this is particularly pertinent in implementation trials. Unlike the evaluation of healthcare interventions on individual health outcomes, implementation research concerns outcome improvements at the whole population level [5]. While routinely collected data capture information in large populations, it provides more comprehensive indicators for evaluating interventions that are directed to the whole population compared to sample-based data sets [47]. They are therefore crucial in implementation research to facilitate translation of research findings into practice.
Implementation science acts proactively to bridge the gap between research evidence and routine healthcare, an implementation trial tests strategies to implement evidence-based clinical innovations into wider practice [48]. Data derived from routine healthcare is an essential connector that can be fed into implementation trials to close the loop of research-practice translation to achieve a continuous optimisation of healthcare interventions and their integration into the real world. This is also an illustration of the learning healthcare system, where knowledge generation is embedded in daily practice for continuous improvement and innovation [49]. Chambers and colleagues [50] addressed the value of implementation science in learning systems and summarised one of the potential synergies between the two domains as “support for implementation of effective practices”. Indeed, by harnessing the power of routine data, implementation science could maximise the capability of closing the known gap, thereby bringing mutual benefit to both scientific research and healthcare routine practice and improving the impact on whole population health.
Strengths and limitations
A key strength of this review is the novelty of the topic, in that no such review has been done in this emerging field. Although we employed a systematic approach to identifying and summarising implementation trials, several limitations require consideration.
Firstly, although the original review protocol focused on the use of routine data in implementation trials, the final review also reported the characteristics of implementation trial designs. We believe this provides valuable context and adds breadth to our research and will be of use to readers. Secondly, our tailored search strategy may have restricted the number of trials identified and led to the underrepresentation of relevant studies not explicit in their reporting of routine data use, possibly affecting the breadth of our findings. This may also introduce a bias towards trials with more meticulous reporting, or in which routine data had a prominent role (e.g. as a primary outcome measure), and potentially overlooking trials where the routine data usage was not featured in the abstract (e.g. for identifying suitable sites). Thirdly, our study did not specifically seek out process evaluations published as separate papers, so we will have overlooked trials in which the routine data contributed exclusively to process outcomes. Future research should include process evaluations to obtain insights on the barriers and facilitators related to the use of routine data, providing a more comprehensive understanding. A further limitation is that we have not summarised all the methodological characteristics of implementation trials using routine data, so may have neglected other potential key characteristics. For example, items listed in CONSORT-ROUTINE checklist [10], such as “information on how to access the list of codes and algorithms used to define or derive the outcomes from the cohort or routinely collected database(s) used to conduct the trial, information on accuracy and completeness of outcome variables, and methods used to validate accuracy and completeness”, are important factors to consider in trials conducted using routine data. In addition, we excluded non-English studies and long-term trial follow-up reports, which could have contributed to the findings. Finally, this review is constrained by the absence of a list of all excluded reports due to a system crash, no complete duplicate study selection and extraction and the lack of quality assessment for the included trials, potentially affecting the results’ reliability and generalisability.
Conclusion
There is a need to enhance adherence to guidance on designing and reporting implementation studies and specifically to harmonise the language used in describing implementation strategies and implementation outcomes. Routine healthcare data offer promise in supporting the implementation of evidence-based interventions and are frequently employed in assessing implementation outcomes. EHRs are widely used in terms of participant identification, outcome ascertainment and intervention delivery. In the meantime, researchers should familiarise themselves with the barriers and facilitators to using routine data, and efforts could be made to improve data quality to overcome some barriers.
Availability of data and materials
All data cited in this review derives from published papers and are therefore already available.
Abbreviations
- EHR:
-
Electronic health record
- RCT:
-
Randomised controlled trial
- CONSORT-ROUTINE:
-
Consolidated Standards of Reporting Trials extension for trials conducted using cohorts and routinely collected data
- PI:
-
Participant identification
- ID:
-
Intervention delivery
- OA:
-
Outcome assessment
References
Wolfenden L, Foy R, Presseau J, Grimshaw JM, Ivers NM, Powell BJ, Taljaard M, Wiggers J, Sutherland R, Nathan N, et al. Designing and undertaking randomised implementation trials: guide for researchers. BMJ. 2021;372:m3721.
Herrett E, Williamson E, van Staa T, Ranopa M, Free C, Chadborn T, Goldacre B, Smeeth L. Text messaging reminders for influenza vaccine in primary care: a cluster randomised controlled trial (TXT4FLUJAB). BMJ Open. 2016;6:e010069.
Powell BJ, Waltz TJ, Chinman MJ, Damschroder LJ, Smith JL, Matthieu MM, Proctor EK, Kirchner JE. A refined compilation of implementation strategies: results from the Expert Recommendations for Implementing Change (ERIC) project. Implement Sci. 2015;10:21.
Waltz TJ, Powell BJ, Matthieu MM, Damschroder LJ, Chinman MJ, Smith JL, Proctor EK, Kirchner JE. Use of concept mapping to characterize relationships among implementation strategies and assess their feasibility and importance: results from the Expert Recommendations for Implementing Change (ERIC) study. Implement Sci. 2015;10:109.
Proctor E, Silmere H, Raghavan R, Hovmand P, Aarons G, Bunger A, Griffey R, Hensley M. Outcomes for implementation research: conceptual distinctions, measurement challenges, and research agenda. Adm Policy Ment Health. 2011;38:65–76.
Peremans L, Rethans JJ, Verhoeven V, Coenen S, Debaene L, Meulemans H, Denekens J, Van Royen P. Empowering patients or general practitioners? A randomised clinical trial to improve quality in reproductive health care in Belgium. Eur J Contracept Reprod Health Care. 2010;15:280–9.
Drake C, Meade C, Hull SK, Price A, Snyderman R. Integration of personalized health planning and shared medical appointments for patients with type 2 diabetes mellitus. South Med J. 2018;111:674–82.
Curran GM, Bauer M, Mittman B, Pyne JM, Stetler C. Effectiveness-implementation hybrid designs: combining elements of clinical effectiveness and implementation research to enhance public health impact. Med Care. 2012;50:217–26.
Benchimol EI, Smeeth L, Guttmann A, Harron K, Moher D, Petersen I, Sorensen HT, von Elm E, Langan SM, Committee RW. The REporting of studies Conducted using Observational Routinely-collected health Data (RECORD) statement. PLoS Med. 2015;12:e1001885.
Kwakkenbos L, Imran M, McCall SJ, McCord KA, Frobert O, Hemkens LG, Zwarenstein M, Relton C, Rice DB, Langan SM, et al. CONSORT extension for the reporting of randomised controlled trials conducted using cohorts and routinely collected data (CONSORT-ROUTINE): checklist with explanation and elaboration. BMJ. 2021;373:n857.
Mc Cord KA, Al-Shahi Salman R, Treweek S, Gardner H, Strech D, Whiteley W, Ioannidis JPA, Hemkens LG. Routinely collected data for randomized trials: promises, barriers, and implications. Trials. 2018;19:29.
Fitzpatrick T, Perrier L, Shakik S, Cairncross Z, Tricco AC, Lix L, Zwarenstein M, Rosella L, Henry D. Assessment of long-term follow-up of randomized trial participants by linkage to routinely collected data: a scoping review and analysis. JAMA Netw Open. 2018;1:e186019.
Reeves M, Winkler E, McCarthy N, Lawler S, Terranova C, Hayes S, Janda M, Demark-Wahnefried W, Eakin E. The Living Well after Breast Cancer Pilot Trial: a weight loss intervention for women following treatment for breast cancer. Asia Pac J Clin Oncol. 2017;13:125–36.
Sandner M, Cornelissen T, Jungmann T, Herrmann P. Evaluating the effects of a targeted home visiting program on maternal and child health outcomes. J Health Econ. 2018;58:269–83.
Downing NL, Rolnick J, Poole SF, Hall E, Wessels AJ, Heidenreich P, Shieh L. Electronic health record-based clinical decision support alert for severe sepsis: a randomised evaluation. BMJ Qual Saf. 2019;28:762–8.
McCall SJ, Imran M, Hemkens LG, Mc Cord K, Kwakkenbos L, Sampson M, Jawad S, Zwarenstein M, Relton C, Langan SM, et al. Reporting transparency and completeness in trials: paper 4 - reporting of randomised controlled trials conducted using routinely collected electronic records - room for improvement. J Clin Epidemiol. 2022;141:198–209.
Imran M, Mc Cord K, McCall SJ, Kwakkenbos L, Sampson M, Frobert O, Gale C, Hemkens LG, Langan SM, Moher D, et al. Reporting transparency and completeness in trials: paper 3 - trials conducted using administrative databases do not adequately report elements related to use of databases. J Clin Epidemiol. 2022;141:187–97.
Mc Cord KA, Imran M, Rice DB, McCall SJ, Kwakkenbos L, Sampson M, Frobert O, Gale C, Langan SM, Moher D, et al. Reporting transparency and completeness in trials: paper 2 - reporting of randomised trials using registries was often inadequate and hindered the interpretation of results. J Clin Epidemiol. 2022;141:175–86.
Hemkens LG, Juszczak E, Thombs BD. Reporting transparency and completeness in trials: paper 1: introduction - better reporting for disruptive clinical trials using routinely collected data. J Clin Epidemiol. 2022;141:172–4.
Cochrane methodology reviews [https://methodology.cochrane.org/].
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71.
Gillum RF. From papyrus to the electronic tablet: a brief history of the clinical medical record with lessons for the digital age. Am J Med. 2013;126:853–7.
Liu FF, Lew A, Andes E, McNamara S, Cassidy J, Whitmore S, Plunkett R, Ong T. Implementation strategies for depression and anxiety screening in a pediatric cystic fibrosis center: a quality improvement project. Pediatr Pulmonol. 2020;55:3328–36.
Sales A, Smith J, Curran G, Kochevar L, Models, strategies, and tools. Theory in implementing evidence-based findings into health care practice. J Gen Intern Med. 2006;21(Suppl 2):43–9.
Nilsen P. Making sense of implementation theories, models and frameworks. Implement Sci. 2015;10:53.
Barr JK, Franks AL, Lee NC, Antonucci DM, Rifkind S, Schachter M. A randomized intervention to improve ongoing participation in mammography. Am J Manag Care. 2001;7:887–94.
Cully JA, Armento ME, Mott J, Nadorff MR, Naik AD, Stanley MA, Sorocco KH, Kunik ME, Petersen NJ, Kauth MR. Brief cognitive behavioral therapy in primary care: a hybrid type 2 patient-randomized effectiveness-implementation design. Implement Sci. 2012;7:64.
Spoelstra SL, Schueller M, Sikorskii A. Testing an implementation strategy bundle on adoption and sustainability of evidence to optimize physical function in community-dwelling disabled and older adults in a Medicaid waiver: a multi-site pragmatic hybrid type III protocol. Implement Sci. 2019;14:60.
Rosa C, Marsch LA, Winstanley EL, Brunner M, Campbell ANC. Using digital technologies in clinical trials: Current and future applications. Contemp Clin Trials. 2021;100:106219.
Pinnock H, Barwick M, Carpenter CR, Eldridge S, Grandes G, Griffiths CJ, Rycroft-Malone J, Meissner P, Murray E, Patel A, et al. Standards for Reporting Implementation Studies (StaRI) statement. BMJ. 2017;356:i6795.
Hsu A, Luo J, Rowe J, Dennis J, Smyth S. Towards data-driven clinical trial planning and strategy. Appl Clin Trials. 2022;31(1/2):21–5.
Sydes MR, Barbachano Y, Bowman L, Denwood T, Farmer A, Garfield-Birkbeck S, Gibson M, Gulliford MC, Harrison DA, Hewitt C, et al. Realising the full potential of data-enabled trials in the UK: a call for action. BMJ Open. 2021;11:e043906.
Quint JK, Moore E, Lewis A, Hashmi M, Sultana K, Wright M, Smeeth L, Chatzidiakou L, Jones R, Beevers S, et al. Recruitment of patients with chronic obstructive pulmonary disease (COPD) from the Clinical Practice Research Datalink (CPRD) for research. NPJ Prim Care Respir Med. 2018;28:21.
Cake C, Ogburn E, Pinches H, Coleman G, Seymour D, Woodard F, Manohar S, Monsur M, Landray M, Dalton G, et al. Development and evaluation of rapid data-enabled access to routine clinical information to enhance early recruitment to the national clinical platform trial of COVID-19 community treatments. Trials. 2022;23:62.
McKay AJ, Jones AP, Gamble CL, Farmer AJ, Williamson PR. Use of routinely collected data in a UK cohort of publicly funded randomised clinical trials. F1000Res. 2020;9:323.
Rosa C, Campbell AN, Miele GM, Brunner M, Winstanley EL. Using e-technologies in clinical trials. Contemp Clin Trials. 2015;45:41–54.
Two years on from RECOVERY: paving the way to a data-enabled future for clinical trials [hdruk.ac.uk/news/two-years-on-from-recovery-paving-the-way-to-a-data-enabled-future-for-clinical-trials/].
Staa TP, Goldacre B, Gulliford M, Cassell J, Pirmohamed M, Taweel A, Delaney B, Smeeth L. Pragmatic randomised trials using routine electronic health records: putting them to the test. BMJ. 2012;344:e55.
McGregor J, Brooks C, Chalasani P, Chukwuma J, Hutchings H, Lyons RA, Lloyd K. The Health Informatics Trial Enhancement Project (HITE): using routinely collected primary care data to identify potential participants for a depression trial. Trials. 2010;11:39.
van Staa TP, Dyson L, McCann G, Padmanabhan S, Belatri R, Goldacre B, Cassell J, Pirmohamed M, Torgerson D, Ronaldson S, et al. The opportunities and challenges of pragmatic point-of-care randomised trials using routinely collected electronic records: evaluations of two exemplar trials. Health Technol Assess. 2014;18:1–146.
Parish S, Mafham M, Offer A, Barton J, Wallendszus K, Stevens W, Buck G, Haynes R, Collins R, Bowman L, Armitage J. Effects of aspirin on dementia and cognitive function in diabetic patients: the ASCEND trial. Eur Heart J. 2022;43:2010–9.
Doidge JC, Harron KL. Reflections on modern methods: linkage error bias. Int J Epidemiol. 2019;48:2050–60.
Boyd JH, Randall SM, Ferrante AM, Bauer JK, Brown AP, Semmens JB. Technical challenges of providing record linkage services for research. BMC Med Inform Decis Mak. 2014;14:23.
Wolfenden L, Reilly K, Kingsland M, Grady A, Williams CM, Nathan N, Sutherland R, Wiggers J, Jones J, Hodder R, et al. Identifying opportunities to develop the science of implementation for community-based non-communicable disease prevention: a review of implementation trials. Prev Med. 2019;118:279–85.
Pinnock H, Epiphaniou E, Pearce G, Parke H, Greenhalgh T, Sheikh A, Griffiths CJ, Taylor SJ. Implementing supported self-management for asthma: a systematic review and suggested hierarchy of evidence of implementation studies. BMC Med. 2015;13:127.
Murrell JE, Pisegna JL, Juckett LA. Implementation strategies and outcomes for occupational therapy in adult stroke rehabilitation: a scoping review. Implement Sci. 2021;16:105.
Kane RW, K. Free, C. Goodrich, J. Uses of routine data sets in the evaluation of health promotion interventions: opportunities and limitations. Health Educ. 2000;100:33–41.
Bauer MS, Kirchner J. Implementation science: what is it and why should I care? Psychiatry Res. 2020;283:112376.
In Digital Infrastructure for the Learning Health System: The Foundation for Continuous Improvement in Health and Health Care: Workshop Series Summary. Edited by Grossmann C, Powers B, McGinnis JM. Washington (DC); 2011.
Chambers DA, Feero WG, Khoury MJ. Convergence of implementation science, precision medicine, and the learning health care system: a new model for biomedical research. JAMA. 2016;315:1941–2.
Acknowledgements
This report is independent research supported by the National Institute for Health Research ARC North Thames. The views expressed in this publication are those of the author(s) and not necessarily those of the National Institute for Health Research or the Department of Health and Social Care.
Funding
C. X. is funded by the Wellcome Trust (224863/Z/21/Z). For the purpose of open access, the author has applied a CC BY public copyright licence to any author-accepted manuscript version arising from this submission.
Author information
Authors and Affiliations
Contributions
CX, supervised by CR, SE, HP, and AS, designed the review and conducted the searches, data extraction, and results synthesis. LS and EI undertook double data screening, extraction, and checking. The authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Additional file 1.
PRISMA 2020 Checklist. Additional file 2. Search Strategy. Additional file 3. Description of implementation outcomes according to Proctor et al., 2010. Additional file 4. References for included trials. Additional file 5. Summary of single implementation strategies used in included trials. Additional file 6. Reported rationale themes with full examples. Additional file 7. Reported facilitators and barriers with full examples.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Xie, C.X., Sun, L., Ingram, E. et al. Use of routine healthcare data in randomised implementation trials: a methodological mixed-methods systematic review. Implementation Sci 18, 47 (2023). https://doi.org/10.1186/s13012-023-01300-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13012-023-01300-4