Abstract
Background
Vaccination is one of the most effective ways to manage infectious disease epidemics such as Covid-19. However, the low rates of vaccination in populations at risk including people using illicit substances, hinders the effectiveness of preventive vaccines in reducing transmission. The aim of this study was to investigate the rate of Covid-19 vaccination and its related factors among people who use substances in Tehran, Iran.
Methods
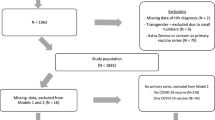
Between July and December 2022, 386 people who use substances aged ≥ 18 years old were recruited by convenience street-based sampling in Tehran. The outcome variable in this study was self-reported completion of at least two doses of the Covid-19 vaccine. Logistic regression was used to investigate the factors related to Covid-19 vaccination. Data were analyzed using SPSS software version 20 at the 0.05 level of significance. As a measure of risk, 95% Confidence interval (CI) was used. The level of significance was considered at 0.05.
Results
Almost three-quarters (n = 286) of the participants reported receiving at least two doses of the Covid-19 vaccine (95% CI, 70.2–79.3). Those participants with high school diplomas were 1.17 times more likely than less educated participants to report having had 2 vaccinations (OR of 1.17, CI 95%: 1.03–1.81). Participants with a higher mean score of having a positive attitude towards Covid-19 vaccination were more likely to have received a vaccination (OR of 1.12, CI 95%: 1.08–1.17). Ethnicity was also an influential variable, people with non-Fars ethnicity were less likely to be vaccinated than those of Fars ethnicity (OR of 0.33, CI 95%: 0.13–0.81). People with higher-than-average monthly income were more likely to report vaccination than those with low monthly incomes (OR of 1.27, CI 95%: 1.09–1.8). Also, participants reporting less access to vaccination centers had a lower chance of reporting having been vaccinated than those who reported high access to vaccination centers (OR of .17, CI 95%: .08-.36).
Conclusions
Covid-19 vaccine uptake was found to be relatively high among people using illicit substances in this study. Higher levels of education, Fars ethnicity, higher income levels, having a positive attitude towards vaccination and access to vaccination centers were the most important predictors of Covid-19 vaccination in this study.
Similar content being viewed by others
Background
The Covid-19 pandemic is a modern global crisis endangering the life, health and well-being with particularly negative effects on the lives of people living with chronic health issues including people who use illicit substances [1]. Previous research has shown that the Covid-19 pandemic led to the increased use of alcohol and other substances in a range of settings globally [2,3,4,5]. It has also been well established that substance use has negative effects on health with devastating social harms [6,7,8,9,10]. So, effective, practical, and sustainable policies and practices is necessary to prevent substance use and all the problems and risk factors that increase substance use and its consequences [11, 12]. Preventive vaccination is a vital strategy in managing the challenges of Covid-19 among people who use substances. Vaccination is well known to be an effective tool in the control of Covid-19 transmission, hospitalization and mortality [13]. Previous research has highlighted low vaccination rates are one of the major factors contributing to the transmission of Covid-19 [14].
Increasing the uptake of the Covid-19 vaccination is one way to slow the spread of associated illness and to reduce the most negative consequences of infection. The acceptance and uptake of some vaccines such as influenza have been found to be less than optimal in different population groups, with vulnerable populations showing high rates of mistrust [15]. Concerns about non-compliance with prevention and treatment for people who use illicit substances have been noted amongst health care workers [16]. There are a range of factors affecting vaccine uptake. These include age, race, physicians’ profession, seasonal influenza vaccine compliance, Covid-19 patient care involvement, confidence in Covid-19 vaccine safety and effectiveness, previous Covid‑19 infection, negative economic impacts of the pandemic, reporting a negative opinion about Covid‑19 vaccine safety, trust in Covid‑19 vaccine information when delivered by the doctor, trust in the government’s actions, having health insurance, knowing more vaccinated people and having a history of imprisonment that have been found to be associated with Covid-19 vaccine compliance in the previous studies [4, 17,18,19,20,21,22]. Available literature has shown that, in general, people using illicit substances have lower hepatitis B and influenza vaccination rates than the general population [23, 24]. People who use illicit substances are among the most marginalized social groups and may live with compromised immune systems and hence have greater vulnerability to pathogens [25]. They often have extensive experiences of homelessness, due to living in shelters or crowded centers and other poor social conditions. They may also live with chronic and communicable diseases and together with their living circumstances these increase the opportunities for Covid-19 exposure and infection [20, 26]. Combine this with lower health literacy than the general population and higher levels of mistrust of health services, experiences of stigma, and limited access to mass media and information, all impact the acceptance of vaccines across this population [25, 27].
Population estimates for Iran suggest that there are between 1.2 and 2 million people using illicit drugs [28, 29], about 20–25% of whom are thought to inject [28, 30,31,32,33,34]. As vaccine acceptance in Iran's general population is still not at the optimal level, and because vaccination uptake for people using illicit substances should be a priority of the health system [35, 36], it is important to understand rates of Covid-19 vaccination and its related factors for people using substances in Iran. Thus, the aim of the current study was to investigate the rate of Covid-19 vaccination uptake and related factors among a convenience sample of people using substances.
Methods
Sampling and participants
In this cross-sectional study, street outreach interviews with people who use substances aged over 18 years old took place between July and December 2022. Using street-based sampling potential participants were approached in various locations, such as streets, parks, shelters, motels, river canyons, and vacant lands and asked about their interest in study participation. Data were on all weekdays, in the morning and evening. We used street-based sampling, as responses to sensitive topics are more reliable than phone or home-based survey recruitment for people using substances in Iran [37].
According to the below formula for estimating the sample size, based on the vaccination prevalence (P = 57%) in Iran in March 2021, the sample size with a confidence interval of 95% (Z = 1.96) and an error level of less than 0.05 (D = 0.05) was calculated as 380. As the attrition was considered 10%, the finalized sample size was estimated at 420 people.
Inclusion and exclusion criteria
Participants were eligible if they reported using illicit substances in the past month (at least weekly for the month prior to answering the questionnaire) and must have been living in Tehran for at least a year, and be aged over 18 years. In this study, any type of substances whose consumption is illegal in Iran were considered illicit substances. Substances included the following; (a) opium (locally known as “Teriak,” which has two forms: “Sookhteh” and Shire); (b) heroin and/or crack (H-C); (c) stimulants including methamphetamine, ice, ecstasy (X pill), cocaine or coke, Ritalin or methylphenidate; (e) hallucinogens including lysergic acid diethylamide (LSD), ketamine, and hallucinogenic fungi (ie, mushrooms); and (f) alcohol [37].
Exclusion criteria included unwillingness to participate in the study, lack of verbal communication ability, and lack of cognitive ability to answer survey questions.
Data were collected from the participants through face-to-face interviews after obtaining verbal informed consent. A small gift was provided to the participants as reimbursement for their time and expertise. The study was approved by the Human Research Ethics Committee, from the Iran University of Medical Sciences (IR.IUMS.REC.1401.447).
Variables and measures
The outcome variable of this study was Covid-19 vaccination, which was measured by self-report completion of Covid19 vaccine (at least two doses) using the following question: “Have you received 2 or more doses of the Covid-19 vaccine? Yes/No”.
For independent variables data collection, a checklist and a questionnaire of attitude towards vaccination were used. The independent variables, were selected based on previous published literature and included: age, sex, education level, income level (Tomans per month, although the Rial is the official currency, Iranians use the Toman in everyday life), amount spent on substance consumption per month, living conditions, drug injection history, prison history, mental illness history, heart disease, infectious diseases, self-reported health status (poor, moderate, good), previous Covid-19 infection (asking if they had ever tested for Covid-19), arrest and detoxification camp during Covid-19 pandemic, ethnicity, marital status, access to COVID-19 vaccination center, current living partner. The attitude towards Covid-19 vaccination was measured by using the 5-point Likert Covid -19 vaccination attitude scale for adults (Co-VASA), ranging from completely disagree (score = 1) to completely agree (score = 5) [38].
Questions in this scale measured understanding of Covid-19 disease transmission, trust in the Covid-19 treatment staff and understanding of the advantages of Covid-19 vaccination. Higher scores suggested a better attitude towards Covid-19 vaccination. The validity and reliability of this scale has been confirmed in previous research [38]. Also, in this study, the reliability was rechecked with Cronbach's alpha and 0.9 was obtained, which indicates the good reliability of the questionnaire.
Statistical analysis
Descriptive statistics were used as mean and standard deviation (SD) for the quantitative variables, and percentages were used for the qualitative variables. The association between the dependent and independent variables was investigated using chi-square (categorical variables) and Mann–Whitney U tests (continuous variable).
Multivariable logistic regressions with robust standard error estimation via generalized estimating equations were performed to identify factors related to Covid-19 vaccination. Following Hosmer and Lemeshow's "purposeful selection of variables" approach to model building. The dependent variable was Covid-19 vaccine compliance in the model. A p-value of < 0.05 was considered statistically significant in the analysis.
Variables with a significance level of ≤ 0.2 were considered in the multivariable model in the univariate analysis, after checking the co-linearity and variance inflation factors between the variables. Also, based on the importance of variables and the possible associations between them (correlation, confounding and interactions), the forward logistic regression model was performed using SPSS software version 20.
Results
Overall, a total of 386 people who use substances were recruited for the study. The response rate was 91.90%. Among the respondents, 74.1% (n = 286, CI 95%, 70.2–79.3) stated that they had received at least two doses of the COVID-19 vaccination. About 1 in 4 (24.9% n = 96, CI 95%, 28.8–20.7) participants reported receiving fewer than two doses of Covid-19 vaccine (Table 1).
Most (84%) participants were male (n = 304) and about one-third (n = 132, 35.1%) were aged over 50 years. One-third (33%) reported secondary school education with marital status of single (n = 110, 28.8%) and divorced (n = 114, 29.8%). See Tables 2 and 3.
The results of the bivariate analysis showed no association between age, income level, cost of substance consumption per month, living condition, history of drug injection, lifetime prison history, history of mental illness, history of heart disease, history of infectious disease, self-reported health status, history of Covid-19 infection, history of arrest for detoxification camp during Covid-19 pandemic and history of Covid-19 vaccination (p > 0.05) (See Tables 2 and 3).
A significant association was found between sex, current living partner, level of education, ethnicity, marital status, access to COVID-19 vaccination centers, and attitude toward COVID-19 vaccination with receiving COVID-19 vaccination (p < 0.05) (Tables 2 and 3).
The results of Table 4 and multivariable analysis show that the variables of positive attitude towards vaccination, education level, ethnicity, income level, and having access to Covid-19 vaccination centers had a significant association with being vaccinated for Covid-19 (p < 0.05) In other words, these variables are predictors of Covid-19 vaccination. Participants with high school diplomas were 1.17 times more likely to report at least two doses of the Covid-19 vaccine than participants who were illiterate (OR of 1.17, CI 95%: 1.03–1.81). Participants in this study with a higher mean score of positive attitudes towards Covid-19 vaccination were also more likely to report having been vaccinated with two Covid-19 doses (OR of 1.12, CI 95%: 1.08–1.17). Individuals of non-Fars ethnicities (OR of 0.33 CI 95%: 0.13–0.81) had a lower chance of receiving Covid-19 vaccination than people of Fars ethnicity. People with a monthly income of 2–5 million Tomans had a higher chance of receiving Covid-19 vaccination than people with a monthly income of fewer than 2 million Tomans (OR of 1.27, CI 95%: 1.09–1.8). People with low access to vaccination centers had a lower chance of receiving Covid-19 vaccination (OR of 0.17, CI 95%: 0.08–0.36). Also, there was no significant association between other variables and Covid-19 vaccination. The results of the Hosmer–Lemeshow test showed that the model had an appropriate goodness of fit with the data (P = 0.5).
Discussion
Our study is among the first to examine the prevalence of Covid-19 vaccination uptake among people using illicit substances in Iran. We found that 74.1% of the participants have received at least two doses Covid-19 vaccine, which is more than the reported vaccination rate in similar studies in the United States (68%) [39] and Spain (71%) [13]. Explanations for the higher vaccination uptake in the present study may be the different timing of this study (three years after the start of the Covid-19 pandemic, and two years after the approval of the Covid-19 vaccine and the global vaccination campaign). The coverage and availability of Covid-19 vaccinations in Iran was also excellent for the general population. This suggests that efforts to reduce doubt and promote vaccination uptake in people using illicit substances has been somewhat effective for those recruited for this cross-sectional study.
Not surprisingly, findings suggest that those people who use substances who have a positive attitude towards Covid-19 vaccination were more likely than those with a negative attitude to have had at least two doses of the vaccine. This is in line with data from the USA where it has also been shown that a positive attitude toward Covid-19 vaccination is correlated to higher rates of vaccination completion [13, 39]. Studies have shown that trust in doctors and the healthcare system increases the willingness to be vaccinated [40]. This suggests that the stigma and discrimination experienced in healthcare centers by the population can also impact vaccine uptake and compliance. Therefore, interventions that are framed around utilizing reliable information sources, including harm reduction activists and trusted peers can increase trust in the health care system and in turn promote vaccination compliance. Previous studies have shown that people who have received direct vaccination advice from healthcare staff were the ones who also had greater rates of vaccination compliance [13, 41].
A systematic review study conducted by Shakeel and colleagues showed that low vaccine acceptance is associated with lower levels of education and awareness [42]. In line with this finding, in the present study, people with a high school diploma were more likely to receive Covid-19 vaccinations when compared to people who were classified as illiterate. Other studies have also shown an association between education and vaccination uptake [43, 44], and also between education and vaccine hesitancy [18, 45].
In the present study, non-Fars participants had a lower chance of receiving vaccination than the Fars ethnic population. People who use substances are highly stigmatized in Iranian society and it may be that the non-Fars population as a minority ethnicity in Tehran, experience this even more. It is possible that people with non-Fars ethnicity are less likely to attend vaccination centers because of their different socio-cultural beliefs and difficulty in communication due to the language. In this regard, studies have shown that ethnic minority and racial groups experience higher rates of Covid-19 infection and death [46, 47], which may be partly due to non-compliance with preventive behaviors. In line with this finding, some studies have shown that African American people including those who use illicit substances are more hesitant and less likely to get vaccinated than the general population [14, 40, 48].
The findings of the present study show that the Covid-19 vaccination rates among low-income participants were less than others in the study. In line with this finding, previous research has shown that people from lower social classes less likely to be vaccinated for other health issues [49]. Previous studies have emphasized structural issues including financial incentives as ways to improve Covid-19 vaccination uptake and completion [50]. These also include providing transportation services, provision of syringes and needles, and food for those who currently inject drugs.
The results of the present study showed that people who had less access to vaccination centers had a lower chance of receiving a vaccination, and this finding is consistent across other studies [13, 51]. Previous studies have shown that efforts to improve vaccination coverage can partially remove the barriers to vaccination [40], so the establishment of clinics and temporary vaccination centers near the places where people inject their Substances can increase the opportunities for vaccination [52].
In the current study, no association was observed between age, marital status, history of chronic diseases, and the chance of receiving the vaccination. Contrary to the results of this study, other studies [39] have observed that younger people have less chance of receiving Covid-19 vaccination [53]. Studies have also shown that PWIDs with comorbidities are more hesitant to receive Covid-19 vaccination [18], and the willingness to receive vaccination in the general married population is higher than for others [54]. Finally, in this study no association was found between the type of substance used and vaccination, which is in line with other studies that have shown hesitation in receiving a vaccine is not correlated to the type of substance used [22, 39].
Limitations
Despite the strengths of the present study, including conducting a study on people who use substances and appropriate sampling, study design and analysis the results of the present study should be interpreted with some limitations in mind. There was no gold standard to determine vaccination and diagnosis rates beyond self-report which may expose the study to social desirability bias and inaccuracy. The cross-sectional nature of this study, means that no causal association between variables could be determined. Convenience sampling method and considering only the people who use substances in Tehran in this study, limits the generalizability of the findings to the population of people who use substances in Iran more widely.
Conclusion
Covid-19 vaccine uptake was found to be relatively high among people using drugs in this study. Higher levels of education, Fars ethnicity, higher income levels, having a positive attitude towards vaccination and access to vaccination centers were the most important predictors for people who received at least two doses of the Covid-19 vaccine. Developing such research in other cities in Iran and different diverse populations is proposed to understand more comprehensively the coverage of Covid-19 vaccination. Policymakers should consider the education and income levels of people when designing strategies for increased and better accessibility to the vaccination centers as well as in designing future interventions to improve vaccination rates for among people who use substances across Iran.
Availability of data and materials
No datasets were generated or analysed during the current study.
Abbreviations
- CI:
-
Confidence interval
- Co-VASA:
-
The Covid-19 Vaccination Attitude Scale for Adults
References
Karimi SE, Ahmadi S, SoleimanvandiAzar N. Inequities as a social determinant of health: Responsibility in paying attention to the poor and vulnerable at risk of COVID-19. J Public Health Res. 2021;10(1):jphr. 2021.1904.
McKay D, Asmundson GJ. Substance use and abuse associated with the behavioral immune system during COVID-19: The special case of healthcare workers and essential workers. Addict Behav. 2020;110:106522.
Wu NS, Schairer LC, Dellor E, Grella C. Childhood trauma and health outcomes in adults with comorbid substance abuse and mental health disorders. Addict Behav. 2010;35(1):68–71.
Vallecillo G, Durán X, Canosa I, Roquer A, Martinez MC, Perelló R. COVID-19 vaccination coverage and vaccine hesitancy among people with opioid use disorder in Barcelona Spain. Drug Alcohol Rev. 2022;41(6):1311–8.
Roberts A, Rogers J, Mason R, Siriwardena AN, Hogue T, Whitley GA, Law GR. Alcohol and other substance use during the COVID-19 pandemic: A systematic review. Drug Alcohol Depend. 2021;1(229):109150.
McAlaney J, Dempsey RC, Helmer SM, Van Hal G, Bewick BM, Akvardar Y, Guillén-Grima F, Orosová OG, Kalina O, Stock C, Zeeb H. Negative consequences of substance use in European University students: Results from project SNIPE. Eur Addict Res. 2021;27(1):75–82.
Ahmadi S, Kazemi-Karyani A, Badiee N, Byford S, Mohammadi A, Piroozi B, Rezaei S. The impact of COVID-19 pandemic on hospital admissions for nine diseases in Iran: insight from an interrupted time series analysis. Cost Effectiveness and Resource Allocation. 2022;20(1):58.
Dart RC, Iwanicki JL, Black JC, Olsen HA, Severtson SG. Measuring prescription opioid misuse and its consequences. Br J Clin Pharmacol. 2021;87(4):1647–53.
Lo TW, Yeung JW, Tam CH. Substance abuse and public health: A multilevel perspective and multiple responses. Int J Environ Res Public Health. 2020;17(7):2610.
Ballestar-Tarín ML, Ibáñez-del-Valle V, Cauli O, Navarro-Martínez R. Personal and social consequences of psychotropic substance use: a population-based internet survey. Medicina. 2022;58(1):65.
McLellan AT. Substance misuse and substance use disorders: why do they matter in healthcare? Trans Am Clin Climatol Assoc. 2017;128:112.
Prust ML, Curry L, Callands TA, Drakes J, McLean K, Harris B, Hansen NB. Risk factors for and consequences of substance use in post-conflict Liberia: A qualitative study. Community Ment Health J. 2018;54:438–49.
Vallecillo G, Fonseca F, Oviedo L, Durán X, Martinez I, García-Guix A, Castillo C, Torrens M, Llana S, Roquer A, Martinez MC, Aguelo S, Canosa I; COSG Group (COVID-19 and Opioids Study Group). Similar COVID-19 incidence to the general population in people with opioid use disorder receiving integrated outpatient clinical care. Drug Alcohol Depend Rep. 2022;2:100027. https://doi.org/10.1016/j.dadr.2022.100027.
Scobie HM, Johnson AG, Suthar AB, Severson R, Alden NB, Balter S, et al. Monitoring incidence of COVID-19 cases, hospitalizations, and deaths, by vaccination status—13 US jurisdictions, April 4–July 17, 2021. Morb Mortal Wkly Rep. 2021;70(37):1284.
Williams WW, Lu P-J, O’Halloran A, Bridges CB, Kim DK, Pilishvili T, et al. Vaccination coverage among adults, excluding influenza vaccination—United States, 2013. MMWR Morb Mortal Wkly Rep. 2015;64(4):95.
Van Scoy LJ, Snyder B, Miller EL, Toyobo O, Grewal A, Ha G, et al. ‘Us-Versus-Them’: Othering in COVID-19 public health behavior compliance. PLoS ONE. 2022;17(1):e0261726.
Jung Y-J, Gagneux-Brunon A, Bonneton M, Botelho-Nevers E, Verger P, Ward JK, et al. Factors associated with COVID-19 vaccine uptake among French population aged 65 years and older: results from a national online survey. BMC Geriatr. 2022;22(1):637.
Strathdee SA, Abramovitz D, Harvey-Vera A, Vera CF, Rangel G, Artamonova I, Patterson TL, Mitchell RA, Bazzi AR. Correlates of Coronavirus Disease 2019 (COVID-19) Vaccine Hesitancy Among People Who Inject Drugs in the San Diego-Tijuana Border Region. Clin Infect Dis. 2022;75(1):e726–33. https://doi.org/10.1093/cid/ciab975. PMID:35024825;PMCID:PMC8690110.
Galanis P, Vraka I, Katsiroumpa A, Siskou O, Konstantakopoulou O, Katsoulas T, Mariolis-Sapsakos T, Kaitelidou D. COVID-19 vaccine uptake among healthcare workers: a systematic review and meta-analysis. Vaccines. 2022;10(10):1637.
Wei Y, Shah R. Substance use disorder in the COVID-19 pandemic: a systematic review of vulnerabilities and complications. Pharmaceuticals. 2020;13(7):155.
Kaplan AK, Sahin MK, Parildar H, Adadan GI. The willingness to accept the COVID-19 vaccine and affecting factors among healthcare professionals: a cross-sectional study in turkey. Int J Clin Pract. 2021;75(7):e14226.
Yang Y, Dobalian A, Ward KD. COVID-19 vaccine hesitancy and its determinants among adults with a history of tobacco or marijuana use. J Community Health. 2021;46(6):1090–8.
White B, Dore GJ, Lloyd A, Rawlinson W, Maher L. Ongoing susceptibility to hepatitis B virus infection among people who inject drugs in Sydney. Aust N Z J Public Health. 2012;36(4):351–6.
Price O, Dietze P, Sullivan SG, Salom C, Peacock A. Uptake, barriers and correlates of influenza vaccination among people who inject drugs in Australia. Drug Alcohol Depend. 2021;226:108882. https://doi.org/10.1016/j.drugalcdep.2021.108882.
Farhoudian A, Baldacchino A, Clark N, Gerra G, Ekhtiari H, Dom G, Mokri A, Sadeghi M, Nematollahi P, Demasi M, Schütz CG. COVID-19 and substance use disorders: Recommendations to a comprehensive healthcare response. an international society of addiction medicine practice and policy interest group position paper. Basic Clin Neurosci. 2020;11(2):133.
Ornell F, Moura HF, Scherer JN, Pechansky F, Kessler FH, von Diemen L. The COVID-19 pandemic and its impact on substance use: Implications for prevention and treatment. Psychiatry Res. 2020;1(289):113096.
Knight KR, Duke MR, Carey CA, Pruss G, Garcia CM, Lightfoot M, Imbert E, Kushel M. COVID-19 Testing and vaccine acceptability among homeless-experienced adults: Qualitative data from two samples. J Gen Intern Med. 2022;37(4):823–9. https://doi.org/10.1007/s11606-021-07161-1.
Karimi SE, Zanjari N, SoleimanvandiAzar N, Ahounbar E, Gharehghani MAM, Ahmadi S. Drug injection and associated factors among the elderly living with HIV/AIDS in Tehran. Iran Med J Islamic Republic Iran. 2021;35:55.
Karimi SE, SoleimanvandiAzar N, Zanjari N, Ahmadi S, Mohammadi Gharehghani MA, Faez D. Social determinants of drug use among older people with HIV/AIDS in Tehran. J Subst Use. 2020;25(6):610–4.
Noroozi M, Ahmadi S, Armoon B, Jorjoran Shushtari Z, Sharhani A, Ahounbar E, et al. Social determinants associated with risky sexual behaviors among men who inject drugs in Kermanshah, Western Iran. Journal of Substance Use. 2018;23(6):591–6.
Noroozi M, Ahounbar E, Ahmadi S, Najafi M, Bazrafshan A, Shushtari ZJ, et al. HIV risk perception and risky behavior among people who inject drugs in Kermanshah, Western Iran. Int J Behav Med. 2017;24(4):613–8.
Noroozi M, Farhadi MH, Armoon B, Farhoudian A, Shushtari ZJ, Sharhani A, Karimi SE, Sayadnasiri M, Rezaei O, Ghiasvand H. Factors associated with time between using a drug and injection initiation among people who inject drugs in Kermanshah, Iran. Int J Adolesc Med Health. 2018;32(5). https://doi.org/10.1515/ijamh-2017-0204.
Noroozi M, Rahimi E, Ghisvand H, Qorbani M, Sharifi H, Noroozi A, et al. Decomposition of economic inequality in needle and syringe programs utilization to its determinants among men who inject drugs in tehran using blinder–oaxaca decomposition method. Subst Use Misuse. 2018;53(7):1170–6.
Armoon B, Noroozi M, Jorjoran Shushtari Z, Sharhani A, Ahounbar E, Karimi S, et al. Factors associated with HIV risk perception among people who inject drugs: Findings from a cross-sectional behavioral survey in Kermanshah. Iran J Subst Use. 2018;23(1):63–6.
Iversen J, Peacock A, Price O, Byrne J, Dunlop A, Maher L. COVID-19 vaccination among people who inject drugs: leaving no one behind. Drug Alcohol Rev. 2021;40(4):517–20. https://doi.org/10.1111/dar.1327.
Iversen J, Sabin K, Chang J, Morgan Thomas R, Prestage G, Strathdee SA, et al. COVID-19, HIV and key populations: cross-cutting issues and the need for population-specific responses. J Int AIDS Soc. 2020;23(10):e25632.
Rastegari A, Baneshi MR, Hajebi A, Noroozi A, Karamouzian M, Shokoohi M, Mirzazadeh A, Khojasteh Bojnourdi T, Nasiri N, Haji Maghsoudi S, Haghdoost AA, Sharifi H. Population size estimation of people who use illicit drugs and alcohol in Iran (2015-2016). Int J Health Policy Manag. 2023;12:6578. https://doi.org/10.34172/ijhpm.2022.6578.
Tavousi M, Sadighi J, Rezaei F, Ardestani MS, Sarbandi F, Soleymanian A, MozafariKermani R, Rostami R, Haeri-Mehrizi AA. Development and validation of a short instrument for measuring attitude towards Covid-19 vaccination: The covid-19 vaccination attitude scale for adults (Co-VASA). Payesh (Health Monitor). 2022;21(1):91–9.
Cepeda JA, Feder KA, Astemborski J, Schluth C, Kirk GD, Mehta SH, et al. COVID-19 Vaccine Hesitancy and Vaccination Status in a Community-Based Cohort of People Who Inject Drugs in Baltimore, Maryland, March–June 2021. Public Health Rep. 2022;137(5):1031–40.
Sullivan MC, Mistler C, Copenhaver MM, Wickersham JA, Ni Z, Kim RS, et al. Race, trust, and COVID-19 vaccine hesitancy in people with opioid use disorder. Health Psychol. 2022;41(2):115.
Figaro MK, Belue R. Prevalence of influenza vaccination in a high-risk population: impact of age and race. J Ambulatory Care Manage. 2005;28(1):24–9.
Shakeel CS, Mujeeb AA, Mirza MS, Chaudhry B, Khan SJ. Global COVID-19 vaccine acceptance: a systematic review of associated social and behavioral factors. Vaccines. 2022;10(1):110.
Robinson E, Jones A, Daly M. International estimates of intended uptake and refusal of COVID-19 vaccines: A rapid systematic review and meta-analysis of large nationally representative samples. Vaccine. 2021;39(15):2024–34.
Pourshahri E, Dastani M, Khoshkhoo M, Sharghi A, Yaghoubi S, Sadeghmoghadam L. Factors affecting acceptance and non-acceptance of covid-19 Vaccination: A systematic review study. J Health Res Commun. 2022;8(1):93–109. http://jhc.mazums.ac.ir/article-1-670-en.html.
Rahimi Kahkashi S, Adeli OA. Knowledge and Attitude of Iranian People Towards COVID-19 Vaccines and Related Factors. J Modern Med Inform Sci. 2022;8(1):36–47.
Magesh S, John D, Li WT, Li Y, Mattingly-App A, Jain S, et al. Disparities in COVID-19 outcomes by race, ethnicity, and socioeconomic status: a systematic-review and meta-analysis. JAMA Network Open. 2021;4(11):e2134147-e.
Ndugga N, Hill L, Artiga S, Haldar S. Latest data on COVID-19 vaccinations by race/ethnicity. Kaiser Family Foundation website. 2022. Available at: https://www.kff.org/coronavirus-covid-19/issue-brief/latest-data-on-covid-19-vaccinations-by-race-ethnicity/.
Andersen JA, Gloster E, Hall S, Rowland B, Willis DE, Kraleti SS, McElfish PA. Associations between COVID- 19 vaccine uptake, race/ethnicity, and political party affiliation. J Behav Med. 2023;46(3):525–31. https://doi.org/10.1007/s10865-022-00379-2.
Salimi Y, Paykani T, Ahmadi S, Shirazikhah M, Almasi A, Biglarian A, et al. Covid-19 vaccine acceptance and its related factors in the general population of Tehran and Kermanshah. Iran J Epidemiol. 2021;16(5):1–9.
Warren N, Kisely S, Siskind D. Maximizing the uptake of a COVID-19 vaccine in people with severe mental illness: a public health priority. JAMA Psychiat. 2021;78(6):589–90.
Cioffi CC, Kosty D, Nachbar S, Capron CG, Mauricio AM, Tavalire HF. COVID-19 vaccine deliberation among people who inject drugs. Drug and Alcohol Dependence Rep. 2022;1(3):100046.
Harvey-Vera A, Munoz S, Artamonova I, Abramovitz D, Mittal ML, Rosales C, Strathdee SA, Rangel MG. COVID-19 vaccine uptake among people who inject drugs in Tijuana Mexico. Front Public Health. 2022;6(10):931306.
Lee CH, Sibley CG. Attitudes toward vaccinations are becoming more polarized in New Zealand: Findings from a longitudinal survey. EClinicalMedicine. 2020;23:100387.
Al-Mohaithef M, Padhi BK. Determinants of COVID-19 Vaccine Acceptance in Saudi Arabia: A web-based national survey. J Multidiscip Healthc. 2020;13:1657–63. https://doi.org/10.2147/JMDH.S276771.
Acknowledgements
The authors would like to thank all the participants for their willingness to participate in the study and their time for it. We are grateful to the Preventive Medicine and Public Health Research Center of the Iran University of Medical Sciences for their financial support.
Funding
This research was supported by the Iran University of Medical Sciences under Grant: (Grant Number 1401–1-90–23238).
Author information
Authors and Affiliations
Contributions
S.K., N.S., and S.A. had equal contributions in designing the study. Data collection was performed by S.K., N.S., and S.A. Data analysis was performed by S.K. and S.A., and all authors contributed to interpretation. The first draft of the manuscript was written by S.K., N.S., S.A., Z.R., and B.T. and all authors commented on previous versions of the manuscript. M.N.,P.H., and A.H. supervised the project and had a critical revision of the manuscript and approval of the article. All authors reviewed and have given approval to the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
We explained the aim of the study to the participants, and only those who verbally agreed to fill in the questionnaires were recruited. The study was approved by the Research Ethics Committee of the Iran University of Medical Sciences, Tehran, Iran (IR.IUMS.REC.1401.447).
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Karimi, S.E., Amadi, S., Rampisheh, Z. et al. Predictors of COVID-19 vaccine uptake among people who use substances: a case study in Tehran. Subst Abuse Treat Prev Policy 19, 15 (2024). https://doi.org/10.1186/s13011-024-00596-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13011-024-00596-9