Abstract
Background
Paid parental leave policies may promote breastfeeding, which can have short- and long-term health benefits for both members of the birthing person-infant dyad. In the United States, where 56% of the workforce qualifies for unpaid federal medical leave, certain states have recently enacted paid parental and family leave policies. We aimed to assess the extent to which living in states with versus without paid family leave was associated with feeding regimens that included breastfeeding.
Methods
In this cross-sectional analysis of the 2021 National Immunization Survey-Child, we assessed feeding outcomes: (1) exclusively breastfed (only fed breastmilk—never infant formula—both before and after six months of age), (2) late mixed breastfeeding (formula after six months), (3) early mixed breastfeeding (breastfed, formula before six months), and (4) never breastfed. We conducted Pearson χ2 to compare social-demographic characteristics and multivariable nominal regression to assess extent to paid family leave was associated with breastfeeding regimens, compared with never breastfeeding.
Results
Of the 35,995 respondents, 5,806 (25% of weighted respondents) were from states with paid family leave policies. Compared with never breastfeeding, all feeding that incorporated breastfeeding—exclusive breastfeeding, late mixed feeding (breastfed, formula introduced after six months), and early mixed feeding (breastfed, formula introduced before six months)—were more prevalent in states with paid family leave policies. The adjusted prevalence ratio (aPR) and differences in adjusted prevalence compared with never breastfeeding in states with versus without paid family leave policies were: aPR 1.41 (95% CI 1.15, 1.73), 5.36% difference for exclusive breastfeeding; aPR 1.25 (95% CI 1.01, 1.53), 3.19% difference for late mixed feeding, aPR 1.32 (95% CI 1.32, 1.97), 5.42% difference for early mixed feeding.
Conclusion
States with paid family leave policies have higher rates of any breastfeeding and of exclusive breastfeeding than states without such policies. Because all feeding types that incorporate breastfeeding were higher in states with paid family leave policies, expansion of paid family leave may improve breastfeeding rates.
Similar content being viewed by others
Background
The short- and long-term benefits of breastfeeding for both members of the birthing person-infant dyad have been well-established. The American Academy of Pediatrics, the American College of Obstetrics and Gynecology, and the World Health Organization promote exclusive breastfeeding for six months followed by continued breastfeeding until one to two years of age [1,2,3]. For newborns, sustained breastfeeding is associated with decreased adverse health consequences including lower rates of infant mortality and lower incidence of sudden infant death syndrome; respiratory, ear, and gastrointestinal infections; asthma; eczema; autoimmune conditions; and diabetes [2]. While exclusive breastfeeding without infant formula introduction is recommended to maximize benefits, data suggest protective effects of any breastfeeding against gastrointestinal illnesses, ear infections, asthma, and obesity [4,5,6]. For birthing people, breastfeeding is associated with decreased rates of hypertension, diabetes, and certain types of cancer [1, 2]. In addition to the individual benefits, breastfeeding promotes dyadic health with opportunities for bonding and benefits for mental and physical health [7]. According to the Centers for Disease Control and Prevention (CDC) breastfeeding report card, in 2019, only 25% of infants born in the United States (US) exclusively breastfed until six months of age and about 36% were breastfeeding at one year [8], falling short of the US Healthy People 2030 targets of 42.4% and 54.1%, respectively [9].
A major barrier to sustained breastfeeding can be caregivers returning to work. Globally, longer maternity leave is associated with higher rates of breastfeeding [10]. In the US, exclusive breastfeeding decreases by approximately 25% within the first week of life, nearly 50% by three months, and 70% by six months, correlating with return to work for many parents [8].
With nearly two-thirds of females participating in the US workforce having a child under three years of age [11], the need to establish and evaluate policies that protect breastfeeding for working lactating persons has been underscored in formal recommendations, including through the Surgeon General’s Calls to Action to Support Breastfeeding and to Improve Maternal Health and the 2022 White House National Strategy on Hunger, Nutrition and Health [12,13,14]. Despite these recommendations, the US is the only country in the Organization for Economic Cooperation and Development (OECD) to not offer a paid federal family leave policy [15, 16].
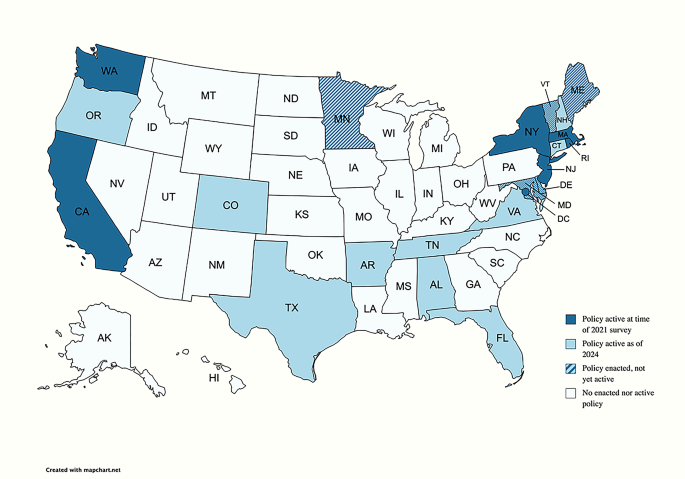
Federal US Legislation supporting unpaid leave and lactation includes the 1993 Family Medical Leave Act (FMLA), the 2010 Patient Protection and Affordable Care Act, and the 2021 Providing Urgent Maternal Protections for Nursing Mothers (PUMP) Act [17]. Federal FMLA stipulates 12 weeks of unpaid, job-protective leave for care of a child [18]. A growing number of states and regions have enacted paid family leave policies. As of 2024, 17 US states and Washington, DC have active paid family leave policies, with five states’ legislation to be enacted in future years (Fig. 1) [19].
In this cross-sectional study, we aimed to assess the relationship of paid family leave with a spectrum of breastfeeding outcomes, including metrics of breastfeeding duration and exclusivity, at the population level. We hypothesized that residence in US states with paid family leave policies is associated with higher rates of both exclusive and any breastfeeding.
Methods
Data source
This cross-sectional, secondary dataset analysis was conducted using data from the 2021 National Immunization Survey-Child (NIS-C), which included the fifty US states and Washington, DC. The National Immunization Surveys (NIS), which includes NIS-C, are telephone surveys administered via random digit dialing to a stratified representative US sample, conducted by the CDC’s National Center for Immunization and Respiratory Disease. The NIS-C incorporates data from parent/guardian interviews and from questionnaires sent to medical providers to evaluate multiple domains of health, including immunization, breastfeeding, and usage of the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) program. The 2021 NIS-C target population included US families of children who were 19–35 months old during calendar year 2021. The survey was translated into English and Spanish, and other languages were queried using telephonic interpretation [20, 21].
The NIS-C is a publicly available, de-identified dataset. Its use is not considered Human Subjects Research, and we did not obtain a determination of this status from the Institutional Review Board. We followed the STrengthening the Reporting of OBservational studies in Epidemiology (STROBE) guidelines for cross-sectional observational data (Additional File 1) [22].
Study variable terminology
When analyzing and presenting data, we used terminology as reported in the NIS-C dataset, which includes terms such as breastfeeding and mother, rather than gender-inclusive terms such as chest feeding and birthing person [23, 24].
States with and without paid family leave policies
The locations with paid family leave policies at the time of the 2021 NIS-C included California, Massachusetts, New Jersey, New York, Rhode Island, Washington, and Washington, DC (Fig. 1). All other states without active paid family leave policies were grouped together, and Puerto Rico was excluded. Three locations—Washington DC, Massachusetts, and Washington—had aspects of their policies enacted in 2020, so some of the surveyed families may have given birth before full enactment. Thus, post-hoc sensitivity analyses were also conducted with these locations removed from analyses.
Primary outcome
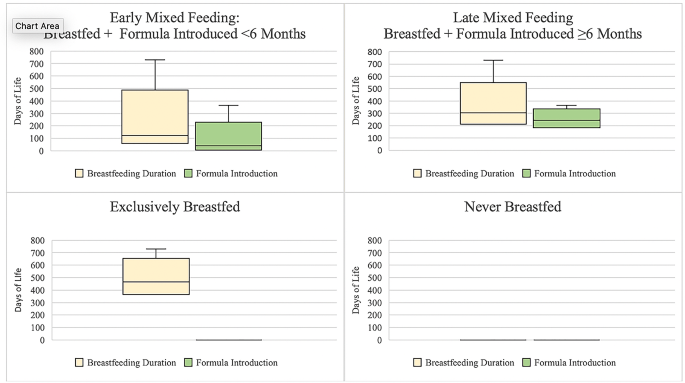
The primary outcome was a composite variable reflecting breastmilk and infant formula feeding. To construct this variable, we accounted for three NIS-C variables that assessed if the child ever was fed breastmilk, duration of breastfeeding, and the date of first formula introduction. The finalized infant feeding primary outcome is summarized in Fig. 2 and includes four categories: (1) exclusively breastfed for the duration captured by data (without formula introduction), (2) late mixed breastfeeding (breastfed exclusively until six months, introduced formula after 6 months), and (3) early mixed breastfeeding (breastfed, introduced formula either before six months of age or at unknown time), and (4) never breastfed. “Exclusively breastfed” refers to receiving breastmilk and never infant formula as source of nutrition but may include supplementary, non-infant formula foods. Because the primary outcome centered around breastfeeding, the 141 respondents with unknown breastfeeding data were excluded from the analysis (see Additional File 2 for characteristics of excluded respondents, who could be considered as non-respondents generally due to high rates of missingness for other variables).
Total days of breastfeeding duration and first day of formula by primary outcome of infant feeding category. Legend: “Exclusively breastfed” refers to receiving breastmilk and never infant formula as source of nutrition but may include supplementary, non-infant formula foods. Figure includes maximum (upper whisker) but not minimum values, as some respondents who reported exclusive breastfeeding had very few days of breastfeeding reported, which we assumed to be errors in reporting. Box indicates upper and lower quartiles. Line indicates median. Adjusted n’s: Exclusively Breastfed n = 6,579.82, Late Mixed Feeding n = 5,899.27, Early Mixed Feeding n = 16,312.40, Never Breastfed n = 5,9343.9
Covariate selection
Based on prior studies of breastfeeding outcomes and available data in the NIS-C, selected covariates included: maternal age, infant age, infant sex, infant race and ethnicity (as reported by the NIS-C dataset), household size, children in the home, maternal education, marital status, language of interviews, poverty level, and WIC enrollment [2]. In order to control for policies that may affect breastfeeding outcomes at the state level, we also developed a covariate to account for workplace lactation protection policies; thirty states and the District of Columbia have such protections in place [25].
Statistical analyses
Since the data were collected using stratified random sampling, survey responses have been weighted by the weights provided by the NIS-C, to reflect strata and non-response. Simple descriptive statistics (count, percent) and Pearson χ2 tests were used to describe and compare the social and demographic characteristics of children and mothers from states that did and did not have active paid family leave policies in 2021 (Table 1).
We used multivariable nominal regression to examine the extent to which the primary exposure variable of residence in states with and without paid family leave policies in 2021 was associated with the primary outcome of any infant feeding regimen that included breastfeeding, compared with never breastfeeding. In this multivariable regression, we controlled for a priori chosen covariates, all of which were retained in the adjusted model and are displayed in Tables 1 and 2. Results are reported as adjusted estimates of prevalence of each feeding regimen (as percentages within each outcome level); differences between adjusted prevalence of breastfeeding outcomes (exclusive, late mixed, early mixed) and adjusted prevalence of never breastfeed; and unadjusted and adjusted prevalence ratios (PR, aPR) with 95% confidence intervals (CI), which were obtained postestimation via linear combinations of relevant parameters and use of marginal mean statement [26]. As noted in the description of the independent variable (states with and without family leave policies), we also conducted post-hoc sensitivity analyses without states where implementation of policies occurred during the study period. Because we were interested in the effect of paid family leave on a spectrum of breastfeeding outcomes that corresponded to independent hypotheses, we did not adjust for multiple comparisons [27, 28].
Given the predetermined sample size by the NIS-C, our conclusions are based on the magnitude of the PR and surrounding 95% CI, rather than the p-values [29, 30]. We further defined a meaningful magnitude of difference in the prevalence of breastfeeding at the 1% point, which reflects the change noted in the prior three years of exclusive breastfeeding in the United States, per Healthy People 2030 [9].
We completed analyses in Stata Version 15 (StataCorp College Station, Texas).
Results
Sociodemographic characteristics by state paid family leave policy
As shown in Table 1, of the 34,722 NIS-C unweighted survey respondents from 2021, 5,806 were from states with paid family leave policies, and they accounted for 25% of weighted survey respondents. We did not observe a meaningful difference between states with and without paid family leave policies in terms of infant sex, infant age, or household size. Differences were noted when assessing breastfeeding workplace policies, maternal age, number of children in the home, parental education, marital status, language of the interview, poverty level, and WIC enrollment (Table 1). Families in states with paid parental leave policies were more likely to reside in states that had workplace breastfeeding protections, report that the mother was over 29 years old, the infant was of Hispanic/Latino ethnicity, there were fewer children in the home, the mother graduated college, the mother was married, and that the income was above poverty and above $75,000. They were less likely to report being enrolled in WIC (Table 1).
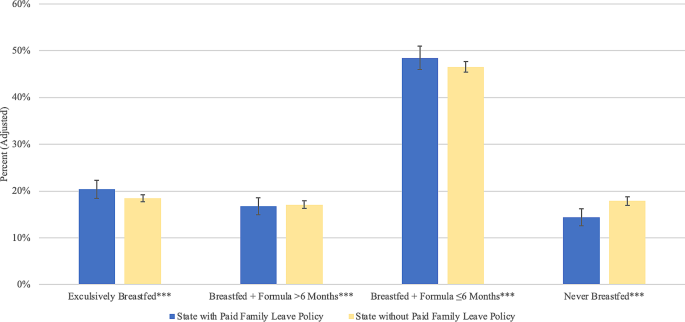
Infant feeding patterns by state paid family leave policy
Exclusive breastfeeding was more prevalent in states with paid family leave policies than in states without such policies: 20.36% (95% CI 18.46%, 22.26%) in states with policies vs. 18.48% (95% CI 17.74%, 19.22%) in states without policies. Late mixed breastfeeding was similar in states with vs. without paid family leave: 16.78% (95% CI 14.97%, 18.60%) vs. 17.09% (95% CI 16.30%, 17.88%). Early mixed breastfeeding was more prevalent in states with vs. without paid family leave: 48.48% (95% CI 46.00%, 50.97%) vs. 46.55% (95% CI 45.47%, 47.64%). Fewer reported never breastfeeding in states with paid family leave: 14.38% (95% CI 12.52%, 16.23%) vs. 17.87% (95% CI 16.98%, 18.76%) (Fig. 3).
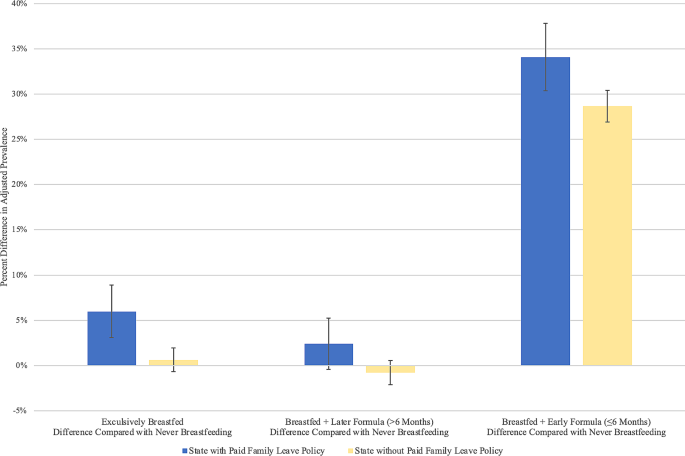
As shown in Table 2; Fig. 4, compared with never breastfeeding, the adjusted prevalence of exclusive breastfeeding was higher by 5.36% (aPR = 1.41) in states with paid family leave vs. in states without paid family leave. Similarly, the adjusted prevalence of late mixed breastfeeding was higher by 3.19% (aPR = 1.25), and early mixed breastfeeding was higher by 5.42% (aPR = 1.32).
Difference in adjusted prevalence of breastfeeding outcomes and prevalence of never breastfeeding by US state paid family leave policies, National Immunization Survey-Child, 2021. Legend: Reported values are estimated differences in adjusted prevalence of each feeding type. Error bars correspond to 95% confidence intervals
A sensitivity analysis which excluded states that enacted family leave policies during the study period (Washington DC, Washington, and Massachusetts) found similar results across all feeding types (Additional File 3).
Covariates associated with breastfeeding
As shown in Table 2, several covariates remained associated with breastfeeding outcomes in the adjusted model.
Workplace breastfeeding policies were positively associated with all types of breastfeeding.
Women with income below poverty had lower aPR of late mixed breastfeeding. Women who were married had greater aPR of all breastfeeding outcomes. Respondents who reported the race/ethnicity of their child as non-Hispanic/Latino Black had lower aPR of exclusively breastfeeding compared with non-Hispanic/Latino White children. Respondents who identified their children as Hispanic/Latino had higher aPR of late mixed feeding compared with non-Hispanic/Latino White children. Compared with English-speaking respondents, Spanish-speaking respondents had higher aPR of all breastfeeding types. Respondents with lower education levels had lower aPR of all breastfeeding outcomes. WIC enrollees also had lower aPR of all types of breastfeeding.
Discussion
In this secondary dataset analysis using a US representative sample, we found that, after adjusting for covariates, all feeding types that incorporate breastfeeding (exclusive breastfeeding, late mixed feeding, and/or early mixed feeding) were higher in states with paid family leave compared with states without paid family leave policies. These findings offer novel insight into various feeding approaches indicative of real-world infant feeding practices among breastfeeding persons in the labor force. Even after controlling for state-level workplace breastfeeding policies, paid family leave policies are associated with exclusive breastfeeding and with a spectrum of feeding types that incorporate breastfeeding. These results demonstrate that the paid family leave policies are positively associated with breastfeeding, and thus may reflect health benefits for the parent/baby dyad that accompany any degree of breastfeeding [2, 4,5,6].
Paid family leave policies have previously been associated with improvements in breastfeeding duration and with health and economic benefits [31,32,33,34,35,36]. After California was the first US state to provide eight weeks of partial paid family leave in 2004, Huang et al. utilized the CDC Infant Feeding Practices Study and found contemporaneous increases in the rates of breastfeeding in California compared with other US states, with difference-in-differences of 15.8%, 17.4%, and 18.4% in the rates of any breastfeeding at three, six, and nine months, respectively [37, 38]. Globally, parental leave after childbirth has been associated with reduced maternal and infant morbidity and mortality [15, 39,40,41,42]. In high-income countries, paid parental leave has been associated with increases in exclusive breastfeeding, downstream earning potential, workforce retention, and infant vaccination rates and with reductions in maternal medical and mental health morbidity [16, 43]. Data suggest higher degrees of benefit with increasingly generous leave, including longer breastfeeding duration and higher maternal pay [44].
Just over half (56%) of the US workforce qualifies for federal FMLA, which is unpaid [45]. There are also limited opportunities for paid leave in the United States, which results in suboptimal breastfeeding initiation and duration [41]. Cross-sectional US studies have found that 59% of women did not receive paid leave, and, even when it was received, paid leave averaged about three weeks, with reduced salary [46]. Current FMLA policies and qualifications tend to support families who can afford unpaid time off work and have stable employment from large employers [18]. Women facing social and structural barriers to breastfeeding, such as low income, lower educational attainment, and membership in minority racial and ethnic groups, disproportionately do not benefit from federal FMLA policies. In this multivariable analysis, we found disparities in breastfeeding was associated with multiple factors that are also related to disparities in medical leave policies.
When evaluating income, we found that, in the adjusted model, women below the poverty level were less likely to exclusively breastfeed for the first six months before introducing infant formula. Families with lower incomes have previously been shown to have less paid and unpaid leave. One 2014 cross-sectional study found that only 20% of families making under $35,000 per year received paid leave, averaging 1.5 weeks in duration, compared with a respective 55% and 4.5 weeks for families making over $75,000 per year [46]. The 2018 US Department of Labor FMLA surveys demonstrated that low-wage workers making $15 per hour or less were least likely to take needed medical leave, citing the inability to afford unpaid time off from work and fear of job loss [45].
Similar to other studies, we found that marital status was positively associated with breastfeeding [47]. The US Department of Labor reports that approximately 95% of fathers with children under three years of age are working, highlighting the potential importance of parental leave for all caregivers in the workforce [11].
Our findings also reflected known racial and ethnic disparities in breastfeeding stemming from complex policies and histories related to structural and ongoing racism [8, 48, 49]. After adjusting for covariates, we found that, compared with respondents who identified their children as non-Hispanic White, non-Hispanic Black respondents were less likely to exclusively breastfeed. Racial and ethnic disparities extend to FMLA eligibility; studies have found that more Black and Hispanic/Latino workforce members (60.2% and 66.9%, respectively) reported being ineligible for or unable to afford unpaid leave than White workers (55.3%) [39]. Because Black women experience higher rates of pregnancy complications and preterm delivery compared to other races, current federal FMLA policies, which count time from pregnancy complications as part of leave, may further exacerbate racial inequities [50,51,52]. We also found that Hispanic/Latino respondents had higher rates of late mixed feeding but lower rates of exclusive breastfeeding compared with non-Hispanic White women. A 2021 study examining feeding goals found that despite Hispanic/Latina women having higher intentions to breastfeeding compared with non-Hispanic/Latina White women, they had lower odds of meeting their goals [53]. Inequitable access to FMLA policies may be contributing to this gap, as Hispanic/Latina women are less likely to qualify for both paid and unpaid leave, which may be related to part-time work status or working for small employers [39, 54, 55].
Employment and education have also previously been associated with breastfeeding outcomes and may be related to access to FMLA [47]. While NIS-C does not include employment data, in the unadjusted and adjusted analyses, we found that women with lower education levels, which are associated with employment opportunities, were less likely to breastfeed. Return to work is among the top reasons for interrupted breastfeeding [33, 56], and women who take six months or more of leave from work have a 30% higher likelihood of any breastfeeding at six months [57].
We also found that women enrolled in WIC were less likely to report breastfeeding across all adjusted and unadjusted analyses. For breastfeeding individuals, WIC distributes breast pumps, offers nutritional support, and supports breastfeeding peer counselor programs [58]. WIC also subsidizes formula purchases, which can result in sales benefits for formula manufactures [59]. Multi-level strategies have been found to enhance breastfeeding for WIC participants, including supporting early WIC enrollment, assessing breastfeeding intentions, and funding peer counseling [60]. However, formula provision may be an incentive for WIC enrollment for some income-eligible individuals, and prior studies have found that some enrollees perceive WIC as a formula provider and appreciate the financial support for formula supplementation [61]. These findings underscore the need to further enrich the lactation-supporting capacity of WIC while considering financial implications and regulations for formula provision.
Limitations of this cross-sectional, secondary dataset analysis included baseline differences between the states with and without paid family leave policies. Respondents in states with paid family leave policies were more likely to report older age, Hispanic/Latina ethnicity, smaller household size, college degree, married status, higher income levels, and lower WIC enrollment. While we adjusted for these characteristics and for workplace breastfeeding policies, there were potentially other unmeasured confounding factors that may have differed between states with and without paid family leave policies, including maternal employment status. Although more generous leave has been found to be associated with greater benefits for breastfeeding-related outcomes, this study did not account for state-by-state variation in leave policies [44]. Several states had policies that went into effect during the survey lookback period, but sensitivity analyses showed similar outcomes regardless of inclusion or exclusion of these states in analyses. Additionally, there were limited data for families who prefer languages other than English or Spanish, and birthing people with varying gender identities may have been excluded.
Despite the limitations of the cross-sectional analysis, it is important to assess differences in breastfeeding outcomes, including mixed breast and formula feeding, as more states enact paid family leave policies. Future prospective studies can evaluate changes in breastfeeding after policy enactment and can assess breastfeeding prevalence in the workforce.
Conclusions
In the United States, all feeding types that incorporate breastfeeding were higher in states with paid family leave compared with states without paid family leave policies. Although multilevel interventions are needed to support breastfeeding, expansion of policies that grant working families and caregivers paid time to raise children can positively affect breastfeeding, which in turn could improve preventative health and economic benefits for individuals and society.
Data availability
The datasets analyzed during the current study are available in the repository which is available from the Centers for Disease Control and Prevention at: https://www.cdc.gov/vaccines/imz-managers/nis/datasets.html.
Abbreviations
- aPR:
-
Adjusted prevalence ratio
- CDC:
-
Centers for Disease Control and Prevention
- CI:
-
Confidence Interval
- FMLA:
-
Family Medical Leave Act
- NIS:
-
National Immunization Surveys
- NIS-C:
-
National Immunization Survey-Child
- OECD:
-
Organization for Economic Cooperation and Development
- PR:
-
Prevalence Ratio
- PUMP:
-
Providing Urgent Maternal Protections for Nursing Mothers Act
- STROBE:
-
STrengthening the Reporting of OBservational studies in Epidemiology
- US:
-
United States
- WIC:
-
Special Supplemental Nutrition Program for Women, Infants, and Children
References
Practice advisory to update the duration of breastfeeding. https://www.acog.org/en/clinical/clinical-guidance/practice-advisory/articles/2023/02/duration-of-breastfeeding-update. Accessed 18 March 2024.
Meek JY, Noble L. Technical report: breastfeeding and the use of human milk. Pediatrics. 2022;150:e2022057989. https://doi.org/10.1542/peds.2022-057988.
World Health Organization. Breastfeeding. https://www.who.int/westernpacific/health-topics/breastfeeding. Accessed 18 March 2024.
Frank NM, Lynch KF, Uusitalo U, Yang J, Lönnrot M, Virtanen SM, et al. The relationship between breastfeeding and reported respiratory and gastrointestinal infection rates in young children. BMC Pediatr. 2019;19:339. https://doi.org/10.1186/s12887-019-1693-2.
Güngör D, Nadaud P, Dreibelbis C, LaPergola C, Terry N, Wong YP et al. Shorter versus longer durations of exclusive human milk feeding prior to the introduction of infant formula and food allergies, allergic rhinitis, atopic dermatitis, and asthma: a systematic review. Alexandria (VA): USDA Nutrition Evidence Systematic Review; 2019. http://www.ncbi.nlm.nih.gov/books/NBK580356/. Accessed 10 April 2023.
Dewey K, Bazzano L, Davis T, Donovan S, Taveras E, Kleinman R et al. The duration, frequency, and volume of exclusive human milk and/or infant formula consumption and overweight and obesity: a systematic review. Alexandria (VA): USDA Nutrition Evidence Systematic Review; 2020. http://www.ncbi.nlm.nih.gov/books/NBK578873/. Accessed 10 April 2023.
Glazer KB, Zeitlin J, Howell EA. Intertwined disparities: applying the maternal-infant dyad lens to advance perinatal health equity. Semin Perinatol. 2021;45(4):151410. https://doi.org/10.1016/j.semperi.2021.151410.
CDC. 2022 Breastfeeding report card. Center for Disease Control and Prevention. 2022. https://www.cdc.gov/breastfeeding/data/reportcard.htm. Accessed 23 Feb 2023.
Increase the proportion of infants who. are breastfed exclusively through age 6 months — MICH–15 - Healthy People 2030 | health.gov. https://health.gov/healthypeople/objectives-and-data/browse-objectives/infants/increase-proportion-infants-who-are-breastfed-exclusively-through-age-6-months-mich-15. Accessed 23 Feb 2023.
Steurer LM. Maternity leave length and workplace policies’ impact on the sustainment of breastfeeding: global perspectives. Public Health Nurs. 2017;34:286–94. https://doi.org/10.1111/phn.12321.
Labor force participation rates | U.S. Department of Labor. https://www.dol.gov/agencies/wb/data/latest-annual-data/labor-force-participation-rates#Labor-Force-Participation-Rate-of-Mothers-and-Fathers-by-Age-of-Youngest-Child. Accessed 1 May 2023.
CDC. The Surgeon General’s call to action to support breastfeeding. Centers for Disease Control and Prevention. 2021. https://www.cdc.gov/breastfeeding/resources/calltoaction.htm. Accessed 30 March 2023.
The Surgeon General’. s call to action to improve maternal health - Healthy People 2030 | health.gov. https://health.gov/healthypeople/tools-action/browse-evidence-based-resources/surgeon-generals-call-action-improve-maternal-health. Accessed 10 April 2023.
The White House. Biden-Harris administration national strategy on hunger, nutrition, and health. 2022. https://www.whitehouse.gov/briefing-room/statements-releases/2022/09/27/executive-summary-biden-harris-administration-national-strategy-on-hunger-nutrition-and-health/. Accessed 10 April 2023.
Nandi A, Jahagirdar D, Dimitris MC, Labrecque JA, Strumpf EC, Kaufman JS, et al. The impact of parental and medical leave policies on socioeconomic and health outcomes in OECD countries: a systematic review of the empirical literature. Milbank Q. 2018;96:434–71.
Heymann J, Sprague AR, Nandi A, Earle A, Batra P, Schickedanz A, et al. Paid parental leave and family wellbeing in the sustainable development era. Public Health Rev. 2017;38:21. https://doi.org/10.1111/1468-0009.12340.
Rep, Maloney. CB [D-N-12. H.R.3110–117th Congress (2021–2022): PUMP for Nursing Mothers Act. 2021. http://www.congress.gov/. Accessed 10 April 2023.
Department of Labor. Family and Medical Leave (FMLA). http://www.dol.gov/general/topic/benefits-leave/fmla. Accessed 1 May 2023.
Bipartisan Policy Center. State paid family leave laws across the U.S https://bipartisanpolicy.org/explainer/state-paid-family-leave-laws-across-the-u-s/. Accessed 10 December 2023.
U.S. Department of Health and Human Services (DHHS) National Center for Immunization and Respiratory Diseases. The 2021 National Immunization Survey - Child. Atlanta, GA: Centers for Disease Control and Prevention. 2022. https://www.cdc.gov/vaccines/imz-managers/nis/downloads/NIS-PUF21-DUG.pdf. Accessed 18 March 2024.
Centers for Disease Control and Prevention. NIS-Child data tables for 2015 to present. 2023. https://www.cdc.gov/vaccines/imz-managers/nis/datasets.html. Accessed 23 February 2023.
von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, et al. The strengthening the reporting of Observational studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol. 2008;61:344–9. https://doi.org/10.1016/j.jclinepi.2007.11.008.
Dinour LM. Speaking out on breastfeeding terminology: recommendations for gender-inclusive language in research and reporting. Breastfeed Med. 2019;14:523–32. https://doi.org/10.1089/bfm.2019.0110.
National Institutes of Health (NIH). Inclusive and gender-neutral language. https://www.nih.gov/nih-style-guide/inclusive-gender-neutral-language. Accessed 1 May 2023.
National Conference of State Legislatures. Breastfeeding state laws. 2021. https://www.ncsl.org/health/breastfeeding-state-laws. Accessed 6 December 2023.
Stata. mlogit — multinomial (polytomous) logistic regression. https://www.stata.com/manuals/rmlogit.pdf. Accessed 27 May 2023.
Rubin M. When to adjust alpha during multiple testing: a consideration of disjunction, conjunction, and individual testing. Synthese. 2021;199:10969–1000. https://doi.org/10.1007/s11229-021-03276-4.
Rubin M. There’s no need to lower the significance threshold when conducting single tests of multiple individual hypotheses. Acadademia Lett. 2021. https://doi.org/10.20935/AL610.
Poole C. Low p-values or narrow confidence intervals: which are more durable? Epidemiology. 2001;12:291–4. https://doi.org/10.1097/00001648-200105000-00005.
Sullivan GM, Feinn R. Using effect size—or why the p value is not enough. J Grad Med Educ. 2012;4:279–82. https://doi.org/10.4300/JGME-D-12-00156.1.
Navarro-Rosenblatt D, Garmendia M-L. Maternity leave and its impact on breastfeeding: a review of the literature. Breastfeed Med. 2018;13:589–97. https://doi.org/10.1089/bfm.2018.0132.
Rollins NC, Bhandari N, Hajeebhoy N, Horton S, Lutter CK, Martines JC, et al. Why invest, and what it will take to improve breastfeeding practices? Lancet. 2016;387:491–504. https://doi.org/10.1016/S0140-6736(15)01044-2.
Baker M, Milligan K. Maternal employment, breastfeeding, and health: evidence from maternity leave mandates. J Health Econ. 2008;27:871–87. https://doi.org/10.1016/j.jhealeco.2008.02.006.
Andres E, Baird S, Bingenheimer JB, Markus AR. Maternity leave access and health: a systematic narrative review and conceptual framework development. Matern Child Health J. 2016;20:1178–92. https://doi.org/10.1007/s10995-015-1905-9.
Hamad R, Modrek S, White JS. Paid family leave effects on breastfeeding: a quasi-experimental study of US policies. Am J Public Health. 2019;109:164–6. https://doi.org/10.2105/AJPH.2018.304693.
Kortsmit K, Li R, Cox S, Shapiro-Mendoza CK, Perrine CG, D’Angelo DV, et al. Workplace leave and breastfeeding duration among postpartum women, 2016–2018. Am J Public Health. 2021;111:2036–45. https://doi.org/10.2105/AJPH.2021.306484.
Huang R, Yang M. Paid maternity leave and breastfeeding practice before and after California’s implementation of the nation’s first paid family leave program. Econ Hum Biol. 2015;16:45–59. https://doi.org/10.1016/j.ehb.2013.12.009.
Centers for Disease Control and Prevention. Why it matters. 2023. https://www.cdc.gov/breastfeeding/about-breastfeeding/why-it-matters.html. Accessed 10 April 2023.
Sprague A, Earle A, Moreno G, Raub A, Waisath W, Heymann J. National policies on parental leave and breastfeeding breaks: racial, ethnic, gender, and age disparities in access and implications for infant and child health. Public Health Rep. 2023;333549231151661. https://doi.org/10.1177/00333549231151661.
Webster JL, Paul D, Purtle J, Locke R, Goldstein ND. State-level social and economic policies and their association with perinatal and infant outcomes. Milbank Q. 2022;100:218–60. https://doi.org/10.1111/1468-0009.12571.
Ruhm CJ. Parental leave and child health. J Health Econ. 2000;19:931–60. https://doi.org/10.1016/s0167-6296(00)00047-3.
Burtle A, Bezruchka S. Population health and paid parental leave: what the United States can learn from two decades of research. Healthcare. 2016;4:30. https://doi.org/10.3390/healthcare4020030.
Raub A, Nandi A, Earle A, de Guzman Chorny N, Wong E, Chung P et al. Paid parental leave: a detailed look at approaches across OECD countries. UCLA WORLD Policy Analysis Center; 2018. https://www.worldpolicycenter.org/sites/default/files/WORLD%20Report%20-%20Parental%20Leave%20OECD%20Country%20Approaches_0.pdf. Accessed 18 March 2024.
Heshmati A, Honkaniemi H, Juárez SP. The effect of parental leave on parents’ mental health: a systematic review. Lancet Public Health. 2023;8:e57–75. https://doi.org/10.1016/S2468-2667(22)00311-5.
Abt Associates. Assessing FMLA: results from 2018 surveys. https://www.abtassociates.com/insights/publications/report/assessing-fmla-results-from-2018-surveys. Accessed 11 May 2023.
Shepherd-Banigan M, Bell JF. Paid leave benefits among a national sample of working mothers with infants in the United States. Matern Child Health J. 2014;18:286–95. https://doi.org/10.1007/s10995-013-1264-3.
Mandal B, Roe BE, Fein SB. The differential effects of full-time and part-time work status on breastfeeding. Health Policy. 2010;97:79–86. https://doi.org/10.1016/j.healthpol.2010.03.006.
Griswold MK, Crawford SL, Perry DJ, Person SD, Rosenberg L, Cozier YC, et al. Experiences of racism and breastfeeding initiation and duration among first-time mothers of the black women’s health study. J Racial Ethn Health Disparities. 2018;5:1180–91. https://doi.org/10.1007/s40615-018-0465-2.
Manuck TA. Racial and ethnic differences in preterm birth: a complex, multifactorial problem. Semin Perinatol. 2017;41:511–8. https://doi.org/10.1053/j.semperi.2017.08.010.
Bornstein E, Eliner Y, Chervenak FA, Grünebaum A. Racial disparity in pregnancy risks and complications in the US: temporal changes during 2007–2018. J Clin Med. 2020;9:1414. https://doi.org/10.3390/jcm9051414.
Martin JA, Hamilton BE, Osterman MJK. Births in the United States, 2019. NCHS Data Brief. 2020;1–8.
KFF. Preterm Births as a Percent of All Births by Race/Ethnicity. 2023. https://www.kff.org/other/state-indicator/preterm-births-by-raceethnicity/. Accessed 11 May 2023.
Hamner HC, Beauregard JL, Li R, Nelson JM, Perrine CG. Meeting breastfeeding intentions differ by race/ethnicity, infant and toddler feeding practices Study-2. Matern Child Nutr. 2020;17:e13093. https://doi.org/10.1111/mcn.13093.
Ann Bartell, Soohyun K, Nam J, Rossin-Slater M, Ruhm C, Waldfogel J. June. Racial and ethnic disparities in access to and use of paid family and medical leave: evidence from four nationally representative datasets: monthly labor review: U.S. Bureau of Labor Statistics. https://www.bls.gov/opub/mlr/2019/article/racial-and-ethnic-disparities-in-access-to-and-use-of-paid-family-and-medical-leave.htm. Accessed 2 2023.
Goodman JM, Richardson DM, Dow WH. Racial and ethnic inequities in paid family and medical leave: United States, 2011 and 2017–2018. Am J Public Health. 2022;112:1050–8. https://doi.org/10.2105/AJPH.2022.306825.
Schwartz K, D’Arcy HJS, Gillespie B, Bobo J, Longeway M, Foxman B. Factors associated with weaning in the first 3 months postpartum. J Fam Pract. 2002;51:439–44.
UNICEF USA. The ost of not breastfeeding. https://www.unicefusa.org/stories/cost-not-breastfeeding. Accessed 11 May 2023.
Food and Nutrition Service. Breastfeeding promotion in WIC: current federal requirements https://www.fns.usda.gov/wic/breastfeeding-promotion-wic-current-federal-requirements. Accessed 12 May 2023.
Choi YY, Ludwig A, Andreyeva T, Harris JL. Effects of United States WIC infant formula contracts on brand sales of infant formula and toddler milks. J Public Health Policy. 2020;41:303–20. https://doi.org/10.1057/s41271-020-00228-z.
Houghtaling B, Shanks CB, Jenkins M. Likelihood of breastfeeding within the USDA’s Food and Nutrition Service Special Supplemental Nutrition Program for women, infants, and children population: a systematic review of the literature. J Hum Lact off J Int Lact Consult Assoc. 2017;33:83–97. https://doi.org/10.1177/0890334416679619.
Almeida R, Alvarez Gutierrez S, Whaley SE, Ventura AK. A qualitative study of breastfeeding and formula-feeding mothers’ perceptions of and experiences in WIC. J Nutr Educ Behav. 2020;52:615–25. https://doi.org/10.1016/j.jneb.2019.12.006.
Acknowledgements
Not applicable.
Funding
Support for Dr. Rosenberg was made possible by CTSA Grant Number KL2 TR001862 from the National Center for Advancing Translational Science (NCATS), components of the National Institutes of Health (NIH), and NIH roadmap for Medical Research. Its contents are solely the responsibility of the authors and do not necessarily represent the official view of NIH.
Support for Dr. Nardella was made possible by the Yale National Clinician Scholars Program and by CTSA Grant Number TL1 TR001864 from the National Center for Advancing Translational Science (NCATS), a component of the National Institutes of Health (NIH). Its contents are solely the responsibility of the authors and do not necessarily represent the official view of NIH.
Author information
Authors and Affiliations
Contributions
JR: conceptualization, methodology, validation, formal analysis, investigation, resources, data curation, writing – original draft, review, editing, visualization, project administration, funding acquisition. DN: validation, investigation, resources, writing – original draft, review, and editing. VS: conceptualization, methodology, validation, formal analysis, writing – review and editing, supervision. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable. The National Immunization Survey is a publicly available, de-identified dataset. Its use is not considered Human Subjects Research, and we did not obtain a determination of this status from the Institutional Review Board.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Rosenberg, J., Nardella, D. & Shabanova, V. State paid family leave policies and breastfeeding duration: cross-sectional analysis of 2021 national immunization survey-child. Int Breastfeed J 19, 37 (2024). https://doi.org/10.1186/s13006-024-00646-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13006-024-00646-9