Abstract
Background
In Indonesia, nearly half of all children aged less than six months were not exclusively breastfed in 2017. This study aimed to compare the cost of providing direct or indirect exclusive breastfeeding 0–6 months, partial exclusive breastfeeding and commercial milk formula only. This study also assessed the maternal socioeconomic and mental health factors to providing exclusive breastfeeding.
Methods
Data were collected in 2018 via a cross-sectional survey of 456 mothers in Bandung City and Purwakarta District, West Java Province, Indonesia, who had children aged less than six months. We used micro-costing to calculate the cost of productivity, equipment, supplies, and training of mothers when providing direct exclusive breastfeeding, indirect exclusive breastfeeding, partial exclusive breastfeeding (a mix of breastfeed and commercial milk formula), and infant formula/commercial milk formula only. Logistic regression was used to determine the impact of several independent variables, including mother’s level of depression, on exclusive breastfeeding.
Results
To provide direct exclusive breastfeeding, the cost per mother in the first six months is US$81.08, which is less expensive than indirect exclusive breastfeeding (US$171.15), partial exclusive breastfeeding (US$487.8) and commercial milk formula (US$494.9). We also found that education and age are associated with the decision to provide direct exclusive breastfeeding. Mothers who work will most likely provide indirect exclusive breastfeeding, commercial milk formula, or partial breastfeeding as opposed to direct exclusive breastfeeding. Finally, although severe depression symptoms have a positive relationship with the decision to provide commercial milk formula over direct exclusive breastfeeding, the evidence here is not strong.
Conclusions
The total cost of providing only commercial milk formula is 6-times higher than the cost of direct exclusive breastfeeding. The presence of severe depression symptoms is positively related to mothers opting for other feeding methods aside of direct exclusive breastfeeding and indirect exclusive breastfeeding. This study shows that direct exclusive breastfeeding is economically preferable to other methods, supports policies to reduce the time cost of exclusive breastfeeding (e.g., paid maternity leave and maternal cash transfers), and addresses the importance of mother’s mental health to ensure successful breastfeeding.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Background
Indonesia has the potential to increase its productivity by 2045 due to the low dependency ratio and high productive labor force (age 15–64 years), better known as a demographic bonus [1, 2]. In order to achieve this, issues such as children’s health should be addressed, as children are crucial in realizing the demographic bonus. However, as of 2018, Indonesia still had prevalent issues concerning children’s health, such as underweight, wasting, and particularly stunting, which affected 30.8% of hildren aged 0–59 months [3]. Stunting is associated with a reduction in schooling years, risk of grade failing, more unsatisfactory cognitive performance, and lower school achievement [4, 5]. Thomas and Strauss [6] found that an increase in height of 1% is associated wth a 2.4% increase in wags in Brazil. According to UNICEF conceptual framework on maternal and child nutrition, breastfeeding has a crucial role as an underlying determinant of the short- and long-term outcomes for childhood, adolescence, adulthood, and societies (e.g., improved survival, health, physical growth, productivity, cognitive development, wages in adults) [7]. Breastfeeding newborn babies is crucial for the physical and mental health of both the mother and baby [8], and it can reduce the mother’s depressive symptoms [9]. Subsequently, support from the government would have considerable benefits [10].
Unfortunately, only half of children under six months of age in Indonesia were exclusively breastfed in 2017 [11]. Although this has surpassed the national strategy target of 50% o children under 6 months being breastfed exclusively, this still does not reach the global breastfeeding target of 70% b 2030 [12, 13]. Factors such as mental health and socioeconomic factors may hinder the success of exclusive breastfeeding [14, 15].
Several studies have found that approximately 10% of pregnant women and 13% of women who recently became mothers experience a mental disorder, primarily depression and anxiety [16, 17], which influences the success of exclusive breastfeeding [18, 19]. Social norms, body image, convenience, perception of commercial milk formula (CMF), difficulty breastfeeding, and lack of confidence hinder the provision of breastmilk and may lead to the use of CMF [20]. Moreover, massive marketing of CMF could affect the decision of the mothers to breastfeed [21].
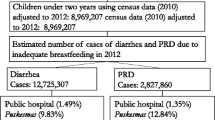
The impact of the decision to not breastfeed also has economic consequences. As the country with the lowest exclusive breastfeeding rate among the Association of Southeast Asian Nations (ASEAN), Thailand has experienced a loss as high as 0.5% of their gross national income (GNI) [22]. The effects of not breastfeeding, such as diarrhea, pneumonia, and cognitive loss, will also lead to considerable economic cost [23,24,25,26,27]. In Indonesia, this cost can reach US$1.5–9.4 billion annually, and the annual number of maternal and infant deaths can reach more than 7000 [10, 22, 28].
West Java is the most populous province in Indonesia, with approximately 48.2 million residents in 2020 [29]. Among children aged 0–59, 25.7% i West Java experience stunting [30], but 63.5% of chldren < 6 months old were exclusively breastfed in 2019 [12]. Though both rates are better than the rates at the national level, the large population in West Java basically results in a higher magnitude of problems in terms of both health and economic impact. For example, the economic impact of not breastfeeding due to respiratory diseases and diarrhea in West Java (US$26.7 million) is more than 5-times higher than that of North Sumatera, the fourth most populous province in Indonesia (~ 15 million people; US$5.9 million) [28].
To the best of our knowledge, the financial need of mothers to provide breastmilk and CMF has rarely been studied, especially in the context of the ASEAN and Indonesia. In this study, we estimated the financial need of mothers who provide breastmilk (either directly or indirectly through feeding expressed breastmilk), commercial milk formula, or a mix of both and explore the factors that may influence this decision, namely socioeconomic factors and mental health. The results will be useful for policy makers to better understand the behavior of mothers in making decisions about breastfeeding and aid in developing proper policies to further promote breastfeeding.
Methods
Study design
We divided our samples into four groups: those who directly exclusively breastfeed (DBF), those who indirectly exclusively breastfeed (IBF), partial exclusive breastfeeding (PEB; a mix of breastfeeding and CMF), and those who provide only commercial milk formula (CMF). We used a micro-costing approach to calculate equipment cost, supplies cost, and productivity loss in the respective groups [31]. We also calculated the cost of training and consultation for mothers who DBF, IBF, or PEB. We calculated our cost within the time frame of six months.
Study setting
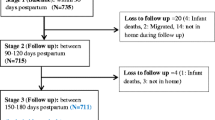
We collected data from Bandung City (the capital of West Java province) and Purwakarta district in 2018. During the study period, Bandung City had the highest rate of six months exclusive breastfeeding in West Java (67.3%), whereas Purwakarta district had the lowest (55.1%) [32]. Based on sample size estimation using the 95% cnfidence level, we needed at least 210 mothers with children under six months old in each region. In the end, we surveyed 456 mothers with children < 6 months old.
Data collection
We provided the respondents with pictures of 25 types of equipment and supplies for breastfeeding and CMF and asked them to choose the relevant pictures of what they used. We estimated the market prices from several websites to obtain the average price. The equipment cost was annualized to obtain yearly cost. Table 1 provides a detailed list of equipment and supplies, as well as their estimated price and the percentage of respondents who own and utilize the goods. We obtained the list of equipment and supplies based on a reference from a previous study [33]. We summed up the total equipment, supplies, and training cost for all respondents from each group and divided it by the number of respondents in the group to obtain the direct cost per mother.
Productivity loss was calculated based on the income per household adjusted for six months divided by the estimated work minutes per six months to find income per minute. The number was multiplied by the time needed to prepare and provide breastmilk and/or CMF. More specifically, for the DBF group, this involves the time needed to breastfeed, while for the IBF group this involves the time needed to express breastmilk (either by hand or by using commercial breast pump), prepare and sterilize equipment, and to feed the breastmilk. For the CMF group, this involves the time needed to prepare and sterilize equipment, prepare the CMF, and to feed the milk, while for the PEB group this involves the combination of the other groups’ use of time. In addition, for mothers in DBF, IBF, and PEB groups, we also calculated the time to receive training and/or obtain consultation regarding breastfeeding and the process to express breastmilk, as well as any relevant preparation. We did not calculate such training/consultation for the CMF group as none of our respondents in this group received such training/consultation. For each group, we totaled the productivity loss of all households and divided it by the number of households per group to obtain the productivity loss per mother for each group.
Data analysis
We also carried out multinomial logistic regression to determine factors that may influence the decision on how to provide breastmilk or CMF. We used the same categories as with the costing analysis for the dependent variable (i.e., DBF, IBF, PEB, and CMF). The socioeconomic variables (e.g., age, marital status), time needed to provide infant formula and/or CMF, cost and time spent to prepare infant formula and/or CMF, and depression symptoms were used as independent variables. Table 2 provides the complete list of variables used for the logistic regression.
Results
Respondent characteristics
Among the 456 respondents, 310 provide DBF, 32 IBF, 87 PEB, and 27 CMF; 32% of the respondents did not provide DBF (Table 3). More than half of the respondents from each group were < 30 years old, but most respondents had completed education up to senior high school. Almost all respondents were married, and most of them were not working and had more than one child.
The financial need of providing milk
The highest average cost of equipment used per mother for the first six months is found within the PEB group (US$ 104.12 per six months), followed by IBF, CMF, and DBF. The lowest average supplies cost per mother is found in the DBF group (US$0.30 per six months), equivalent to only 0.4% of its average total cost. Average CMF cost dominated the supplies cost in the PEB and CMF groups. Table 4 presents the cost breakdown for each group.
Productivity loss
As seen in Table 5, the time spent per day to provide infant formula and/or CMF to infants is the longest in the CMF group (420 min) and the shortest in the DBF group (167 min). Converting these times into the productivity loss over six months showed that IBF cost has the highest productivity loss (US$ 43.58/mother/6 months) due to the highest productivity loss per minute (Table 5).
Multinomial logistic regression
Table 6 presents the multinomial logistic regression results. Mothers who work are most likely to provide breastmilk or milk through IBF, PEB, or CMF. In terms of costs, those who provide IBF, PEB, or CMF are most likely to incur larger costs. Lastly, it seems that mothers who experienced severe depression symptoms may potentially provide DBF, except for mothers in the IBF group, although this relationship is weak.
Discussion
Our results show that mothers in the direct exclusive breastfeeding group bear an approximately 6- times lower cost of providing breastmilk in the first six months than mothers in the partial exclusive breastfeeding and commercial milk formula groups. The cost drivers of direct exclusive breastfeeding and indirect exclusive breastfeeding mothers are productivity loss and equipment, whereas the cost driver of mothers in the PEB and CMF groups is mainly commercial milk formula. Although productivity loss is one of the cost drivers for the DBF and IBF groups, the nominal amount is roughly similar to the productivity loss found in the PEB and CMF groups. As the productivity loss of DBF group consists only of direct breastfeeding, it has the lowest productivity loss (and the average total time spent to breastfeed), as the other groups require additional time to either express breastmilk, prepare and sterilize equipment, and/or prepare CMF, in addition to the time needed to feed the infant formula and/or commercial milk formula. Added by the high cost of CMF, the cost of providing infant formula and/or CMF per mother in the first six months of the PEB and CMF groups is much higher than the DBF and IBF groups. Similarly, a study in England found that, although IBF require purchasing equipment before the babies were born (e.g., this includes breast pumps, breast-milk freezer bags, muslin cloths, nipple shields, breast shells, breast and nipple creams/sprays, breast-milk storage bottles, sterilizers and support pillows), the cost of providing CMF is still 62% more expensive than IBF [33]. Such huge cost difference should be shared with the public more frequently to show the potential savings if a mother decides to DBF or IBF. Unfortunately, such information is rarely available, especially in developing countries, and should be studied more in different settings and socio-economic groups.
Regardless of the type of milk, the opportunity cost of providing infant formula and/or CMF has been recognized as one of the main challenges in breastfeeding, as mothers need to spend time providing, preparing, or expressing the breastmilk and leave their work for a certain amount of time, which is viewed as causing productivity loss [34]. No policies in Indonesia are currently in place that directly address such views and challenges. Considering this finding, a careful assessment of the need of mothers, firms/institutions, and other stakeholders in achieving and supporting optimal breastfeeding conditions should be conducted to design appropriate policies.
We also found that mothers who experience severe depression symptoms are potentially more likely to provide PEB or CMF than DBF. Although this relationship is weak, newer and older studies support the association between breastfeeding difficulties and depression [35,36,37]. This aspect is rarely discussed in developing countries and requires specific procedures and policies. However, this requires further studies as we currently do not have sufficient local evidence to support this argument.
Lastly, in all groups, mothers who work have a slightly higher chance to opt for either IBF, PEB, or CMF, instead of DBF. This can be partly explained by the not optimal or the absence of maternity support at the workplace [38]. Indeed, the existence of workplace interventions to support breastfeeding is crucial to increase the duration of breastfeeding and avoid early introduction of CMF [39]. This is important, as, in the case of urgent need of income, mothers will most likely hurry to get back to work. Although regulations supporting maternal leave are already in place in Indonesia, they only cover the primary salary, and additional income-benefits associated with mothers’ work are not given during maternity leave [40]. This would become an issue, especially in the case of a larger benefit compared to the primary salary. As such, mothers face hard choices between taking the time to DBF or getting back to their office as early as possible without utilizing the full length of their maternity leave [41,42,43]. Moreover, we also should note that although the cost of DBF in the first 6 months is 6 times lower than the CMF group, it is not free. There are still existing opportunity and equipment costs, and such costs may discourage mothers from breastfeeding if informed incorrectly without proper explanation of the costs of other feeding options (i.e., IBF, PEB, CMF). Given these challenges, optimizing maternity protection policies is crucial.
Studies have shown that extending maternal leave in the formal and informal sectors is an economically attractive option, but other supporting policies, such as maintaining income at the appropriate level, flexible working hours, the existence of a lactation room, will also encourage mothers to DBF at the workplace [44,45,46,47]. In addition, reimbursement policies may also provide benefits to the DBF rate. One such example is requiring employers or insurance policies to cover or reimburse the costs of prenatal and postnatal lactation support, counseling, and equipment rental during breastfeeding period [48]. Another form of reimbursement is to share the financial need of paid maternity leave between employers and government, in which the government reimburses a certain % of the financial need already spent by the employers to pay for e.g., salary of mothers during paid maternity leave, thus reducing the burden of employers [44, 49].
Additionally, mothers’ education seemed to be associated with mothers’ decision to provide DBF and/or CMF, and mothers with higher education are most likely to provide DBF instead of CMF. Thus, encouraging women to obtain education may increase the rate of mothers to DBF [50], although it may also lead to a negative effect as there is higher probability of mothers to return to workplaces where support for breastfeeding is limited [51]. This requires similar attention as discussed in the previous paragraph regarding breastfeeding at the workplace.
This study has some limitations. First, our area of study only covers two regions that have completely different rates of mothers who provide direct exclusive breastfeeding. As such, our samples do not represent the whole province. Although more samples may improve the findings, our results could provide a picture of what occurs in two different regions in terms of the cost of providing infant formula and/or CMF and factors that may influence the choice to DBF. Second, we used the CESD-R-10 to measure the mental health variable. This instrument can show depression symptoms but requires further examination to establish a firm diagnosis of depression. In addition, the instrument may have captured depression symptoms at certain periods of time (1 week) but cannot be generalized for a longer period, such as a year. However, we were able to portray the mothers who may experience depression symptoms during the period of exclusive breastfeeding. Recognizing the symptoms early is crucial for further consultation or treatment. Lastly, we did not include training/consultation related to the Baby-Friendly Hospital Initiative (BFHI) or Ten Steps to successful breastfeeding (Ten Steps) in our cost analysis as we have no information regarding the facility where the respondents gave birth. As the number of BFHI hospitals in Indonesia is still limited, it is less likely that the hospitals surrounding the area of our study are BFHI accredited. We found one study in Indonesia that estimate the cost of Ten Steps in a hospital in East Java province [52]. If we include all costs related to training or consultation on breastfeeding or risks of not doing so within the scope of the Ten Steps, this amounts to around US$800,000 (out of US$962,078) annually, using PPP factor in 2019 [52]. We do not, however, have the information of the average cost per person, so we cannot estimate the cost per mother for the purpose of our study. Additionally, the cost of BFHI or Ten Steps is rarely studied, especially in the Indonesian context. As such, more evidence is needed in more settings to have a better picture of how much it really costs per mother.
Conclusions
The total cost of providing only commercial milk formula is 6-times higher than the cost of direct exclusive breastfeeding. The total cost and presence of severe depression symptoms are related to mother’s decision to not provide direct exclusive breastfeeding. This study shows that DBF is economically preferable to other methods and supports policies to increase the duration and quality of paid maternity leave as well as other maternity protection policies (e.g., lactation room, maternal cash transfer), and address the potential importance of a mother’s mental health to ensure successful direct exclusive breastfeeding.
Data Availability
The datasets generated and analyzed in the current study are not publicly available due to patient confidentiality concerns but are available from the corresponding author upon reasonable request.
Abbreviations
- ASEAN:
-
Association of Southeast Asian Nations.
- CESD-R-10:
-
Center for Epidemiologic Studies Depression Scale - Revised.
- DBF:
-
Direct Exclusive Breastfeeding.
- IBF:
-
Indirect Exclusive Breastfeeding.
- CMF:
-
Commercial Milk Formula.
- GNI:
-
Gross National Income.
- IDR:
-
Indonesia Rupiah.
- PEB:
-
Partial Exclusive Breastfeeding.
- USD:
-
United States Dollar.
References
Wisnumurti AAGO, Darma IK, Suasih NNRS. Government policy of Indonesia to managing demographic bonus and creating Indonesia Gold in 2045. IOSR J Humanit Social Sci. 2018;23:23–34.
Suryahadi A, Raya UR, Marbun D, Yumna A. Accelerating poverty and vulnerability reduction: Trends, Opportunities and Constraints. Indonesia: Jakarta; 2012.
Ministry of Health of the Republic of Indonesia. - Health Research and Development Agency. Basic Health Research 2018.Jakarta, Indonesia; 2019.
Grantham-McGregor S, Cheung YB, Cueto S, Glewwe P, Richter L, Strupp B. Developmental potential in the first 5 years for children in developing countries. Lancet. 2007;369:60–70.
Martorell R, Horta BL, Adair LS, Stein AD, Richter L, Fall CHD, et al. Weight gain in the first two years of life is an important predictor of schooling outcomes in pooled analyses from five birth cohorts from low- and middle-income countries. J Nutr. 2010;140:348–54.
Thomas D, Strauss J. Health and wages: evidence on men and women in urban Brazil. J Econom. 1997;77:159–85.
UNICEF. Nutrition, For Every Child: UNICEF Nutrition Strategy 2020–2030. New York, USA; 2020.
Abekah-Nkrumah G, Antwi MY, Nkrumah J, Gbagbo FY. Examining working mothers’ experience of exclusive breastfeeding in Ghana. Int Breastfeed J. 2020;15:56.
de Mola CL, Horta BL, Gonçalves H, Quevedo LDA, Pinheiro R, Gigante DP, et al. Breastfeeding and mental health in adulthood: a birth cohort study in Brazil. J Affect Disord. 2016;202:115–9.
Walters DD, Phan LTH, Mathisen R. The cost of not breastfeeding: global results from a new tool. Health Policy Plan. 2019;34:407–17.
National Population and Family Planning Board (BKKBN)., Statistics Indonesia (BPS), Ministry of Health of the Republic of Indonesia, ICF. Indonesia Demographic and Health Survey 2017.Jakarta, Indonesia; 2018.
Ministry of Health (MoH). Indonesia. Indonesian Health Profile. 2020.
WHO, UNICEF. Global breastfeeding scorecard 2019, increasing commitment to Breastfeeding through Funding and Improved Policies and Programmes. Geneva; 2019.
Groer MW, Morgan K. Immune, health and endocrine characteristics of depressed postpartum mothers. Psychoneuroendocrinology. 2007;23:133–9.
Radhakrishnan S, Balamuruga SS. Prevalence of exclusive breastfeeding practices among rural women in Tamil Nadu. Int J Health Allied Sci 2012. 2012;1:64–7.
O’Hara MW, Swain AM. Rates and risk of postpartum depression: a meta-analysis. Int Rev Psychiatry. 2009;8:37–54.
Hendrick V, Altshuler L, Cohen L, Stowe Z. Evaluation of mental health and depression during pregnancy: position paper. Psychopharmacol Bull 1998. 1998;34:297–9.
Thome M, Alder EM, Ramel A. A population-based study of exclusive breastfeeding in icelandic women: is there a relationship with depressive symptoms and parenting stress? Int J Nurs Stud. 2006;43:11–20.
Zubaran C, Foresti K. The correlation between breastfeeding self-efficacy and maternal postpartum depression in southern Brazil. Sex Reprod Healthc. 2013;4:9–15.
Brown A, Raynor P, Lee M. Healthcare professionals’ and mothers’ perceptions of factors that influence decisions to breastfeed or formula feed infants: a comparative study. J Adv Nurs. 2011;67:1993–2003.
Witten C, Claasen N, Kruger HS, Coutsoudis A, Grobler H. Psychosocial barriers and enablers of exclusive breastfeeding: lived experiences of mothers in low-income townships, North West Province, South Africa. Int Breastfeed J. 2020;15:76.
Walters D, Horton S, Siregar AYM, Pitriyan P, Hajeebhoy N, Mathisen R, et al. The cost of not breastfeeding in Southeast Asia. Health Policy Plan. 2016;31:1107–16.
Lamberti LM, Fischer Walker CL, Noiman A, Victora C, Black RE. Breastfeeding and the risk for diarrhea morbidity and mortality. BMC Public Health. 2011;11:15.
Lamberti LM, Zakarija-Grković I, Fischer Walker CL, Theodoratou E, Nair H, Campbell H, et al. Breastfeeding for reducing the risk of pneumonia morbidity and mortality in children under two: a systematic literature review and meta-analysis. BMC Public Health. 2013;13:18.
Horta BL, Victora CG. Short-term effects of breastfeeding: a systematic review on the benefits of breastfeeding on diarrhoea and pneumonia mortality. Switzerland: WHO. Geneva; 2013.
Nkemjika SO, Demissie K. Breast feeding initiation time and its impact on diarrheal disease and pneumonia in West Africa. J Public Health Epidemiol. 2015;7:352–9.
Hanieh S, Ha TT, Simpson JA, Thuy TT, Khuong NC, Thoang DD, et al. Exclusive breast feeding in early infancy reduces the risk of inpatient admission for diarrhea and suspected pneumonia in rural Vietnam: a prospective cohort study. BMC Public Health. 2015;15:1166.
Siregar AYM, Pitriyan P, Walters D. The annual cost of not breastfeeding in Indonesia: the economic burden of treating diarrhea and respiratory disease among children (< 24mo) due to not breastfeeding according to recommendation. Int Breastfeed J. 2018;13:10.
Statistics, Indonesia. Ministry of Internal Affair Indonesia. Official News Statistics: Results of the 2020 Population Census. 2021.
Ministry of Health (MoH) Indonesia. (b). Final Report of the Study on the Nutritional Status of Toddlers in Indonesia in 2019. 2019.
Drummond MF, Sculpher MJ, Claxton K, Stoddart GL, Torrance GW. Methods for the Economic Evaluation of Health Care Programmes. 4th edition. Oxford University Press; 2015.
West Java Health Office. West Java Health Profile 2019. 2019.
Berridge K, Hackett A, Abayomi J, Maxwell S. The cost of infant feeding in Liverpool, England. Public Health Nutr. 2004;7:1039–46.
Bai YK, Wunderlich SM, Weinstock M. Employers’ readiness for the mother-friendly workplace: an elicitation study. Matern Child Nutr. 2012;8:483–91.
Stuebe AM, Meltzer-Brody S, Propper C, Pearson B, Beiler P, Elam M, et al. The mood, mother, and infant study: associations between maternal mood in pregnancy and breastfeeding outcome. Breastfeed Med. 2019;14:551–9.
Cooper PJ, Murray L, Stein A. Psychosocial factors associated with the early termination of breast-feeding. J Psychosom Res. 1993;37:171–6.
Hahn-Holbrook J, Haselton MG, Dunkel Schetter C, Glynn LM. Does breastfeeding offer protection against maternal depressive symptomatology? Arch Womens Ment Health. 2013;16:411–22.
Snyder K, Hansen K, Brown S, Portratz A, White K, Dinkel D. Workplace breastfeeding support varies by employment type: the service workplace disadvantage. Breastfeed Med. 2018;13:23–7.
Vilar-Compte M, Hernández-Cordero S, Ancira-Moreno M, Burrola-Méndez S, Ferre-Eguiluz I, Omaña I, et al. Breastfeeding at the workplace: a systematic review of interventions to improve workplace environments to facilitate breastfeeding among working women. Int J Equity Health. 2021;20:110.
Ministry of Manpower and Transmigration. Manpower Law No. 13/2003. 2003.
Lo Bue MC, Priebe J. Revisiting the socioeconomic determinants of exclusive breastfeeding practices: evidence from Eastern Indonesia. Oxf Dev Stud. 2018;46:398–410.
Chang P-C, Li S-F, Yang H-Y, Wang L-C, Weng C-Y, Chen K-F, et al. Factors associated with cessation of exclusive breastfeeding at 1 and 2 months postpartum in Taiwan. Int Breastfeed J. 2019;14:18.
Villar M, Santa-Marina L, Murcia M, Amiano P, Gimeno S, Ballester F, et al. Social factors associated with non-initiation and cessation of predominant breastfeeding in a mother-child cohort in Spain. Matern Child Health J. 2018;22:725–34.
Siregar AYM, Pitriyan P, Walters D, Brown M, Phan LTH, Mathisen R. The financing need for expanded maternity protection in Indonesia. Int Breastfeed J. 2019;14:27.
Chen J, Xin T, Gaoshan J, Li Q, Zou K, Tan S, et al. The association between work related factors and breastfeeding practices among chinese working mothers: a mixed-method approach. Int Breastfeed J. 2019;14:1–13.
Siregar AYM, Pitriyan P, Hardiawan D, Zambrano P, Vilar-Compte M, Belismelis GMT, et al. The yearly financing need of providing paid maternity leave in the informal sector in Indonesia. Int Breastfeed J. 2021;16:17.
Addati L, Cattaneo U. Care at work. Geneva, Switzerland: International Labour Office; 2022.
Hawkins SS, Dow-Fleisner S, Noble A. Breastfeeding and the Affordable Care Act. Pediatr Clin North Am. 2015;62:1071–91.
Addati Laura C, Naomi GK. Maternity and paternity at work: Law and practice across the World. International Labour Office; 2014.
Laksono AD, Wulandari RD, Ibad M, Kusrini I. The effects of mother’s education on achieving exclusive breastfeeding in Indonesia. BMC Public Health. 2021;21:14.
Neves PAR, Barros AJD, Gatica-Domínguez G, Vaz JS, Baker P, Lutter CK. Maternal education and equity in breastfeeding: trends and patterns in 81 low- and middle-income countries between 2000 and 2019. Int J Equity Health. 2021;20:20.
Pramono AY, Desborough JL, Smith JP, Bourke S. The social value of implementing the ten steps to successful breastfeeding in an indonesian hospital: a case study. Yale J Biol Med. 2021;94:429–58.
Acknowledgements
The authors wish to thank the Bandung City & Purwakarta Regency Health Department for providing regional recommendations for data collection and Mochamad Eldy Nur Maulana as the data collection coordinator.
Funding
Internal funding of Universitas Padjadjaran, Indonesia.
Author information
Authors and Affiliations
Contributions
RR* conceptualized the research, designed the research, analyzed the data, and prepared the manuscript. AA prepared the manuscript. EDS, DF, and AYMS conceptualized and designed the research. All authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare that they have no competing interests.
Ethics approval
The study was approved by the Ethics Committee Faculty of Medicine Universitas Padjadjaran No. 503/UN6.KEP/EC/2019.
Consent for publication
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Relaksana, R., Akbar, A., Sihaloho, E.D. et al. The financial need of feeding infants for the first six months of life in West Java Province of Indonesia and the implications of socioeconomic and mental health factors. Int Breastfeed J 18, 26 (2023). https://doi.org/10.1186/s13006-023-00561-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13006-023-00561-5