Abstract
Purpose
To evaluate the accuracy of magnetic resonance imaging (MRI) for jawbone assessment compared to reference-standard measurements in the literature.
Materials and methods
An electronic database search was conducted in PubMed, EMBASE, Scopus, Web of Science, and the Cochrane Library in June 2022, and updated in August 2023. Studies evaluating the accuracy of MRI for jawbone assessment compared with reference-standard measurements (histology, physical measurements, or computed tomography) were included. The outcome measures included bone histomorphometry and linear measurements. The risk of bias was assessed by the Quality Assessment Tool for Diagnostic Accuracy Studies (QUADAS-2). The review was registered in the PROSPERO database (CRD42022342697).
Results
From 63 studies selected for full-text analysis, nine manuscripts were considered eligible for this review. The studies included assessments of 54 participants, 35 cadavers, and one phantom. A linear measurement error ranging from 0.03 to 3.11 mm was shown. The accuracy of bone histomorphometry varies among studies. Limitations of the evidence included heterogeneity of MRI protocols and the methodology of the included studies.
Conclusion
Few studies have suggested the feasibility of MRI for jawbone assessment, as MRI provides comparable results to those of standard reference tests. However, further advancements and optimizations are needed to increase the applicability, validate the efficacy, and establish clinical utility of these methods.
Similar content being viewed by others
Introduction
Imaging exams are an essential complement for diagnosing and treating diseases and conditions affecting the maxillofacial region. Despite the exposure to ionizing radiation and limitations in displaying and differentiating soft tissues, intraoral radiography, extraoral radiography and cone beam computed tomography (CBCT) are commonly used to evaluate maxillofacial structures [1].
CBCT is still considered the standard imaging technique for assessing maxillofacial bones, but magnetic resonance imaging (MRI) has emerged as a potential alternative due to its superior soft tissue contrast and lack of ionizing radiation. MRI is a noninvasive diagnostic tool that generates images based on the interaction between magnetic fields and radio waves with hydrogen atoms present in the human body [2].
Advancements in MRI, primarily known for its application in soft tissue evaluation, have extended to include quantitative bone imaging and microstructural analysis [3]. For instance, the ability of MRI to detect interactions between water, fat, and blood within marrow tissues has enabled the assessment of different trabecular and cortical characteristics [4, 5]. Additionally, indirect assessment of bone mineral density (BMD) by quantifying bone mineral fat (BMF) can offer an alternative approach to the conventional X-ray imaging techniques commonly used for osteoporosis diagnosis, fracture risk prediction, and treatment planning [6]. Moreover, the application of standard pulse sequences combined with commercially available coils and MRI scanners can allow for detailed bone microarchitecture assessment [7].
A recent pilot study evaluated different trabecular bone parameters via MRI in comparison to those via microcomputed tomography (µCT). While MRI has been shown to slightly overestimate bone parameters, indicating increased density, it also exhibited statistically significant fixed linear deviations [8]. Other studies reported similar bone results using MRI and other imaging techniques, including CT [9] and CBCT [10,11,12].
Therefore, MRI has been suggested as a potential alternative for assessing bone quality in various dental scenarios, including dental and periodontal anatomical analysis [13], cephalometry [14] and panoramic imaging [15], preoperative diagnosis in third molar surgery [16], caries detection [17], and dental implant planning [18,19,20]. However, despite recent improvements, the literature on the use of MRI for jawbone assessment is scarce, and different methods for obtaining MR images are available. Therefore, the aim of this study was to evaluate the accuracy of MRI for jawbone assessment compared to reference-standard measurements in the literature.
Materials and methods
Protocol registration
This systematic review was performed according to the Preferred Reporting Items of Systematic Reviews and Meta-analysis (PRISMA) [21] and registered in the International Prospective Register of Systematic Reviews (PROSPERO) [22] according to the CRD42022342697 protocol [23]. The proposed focused question was “What is the accuracy of magnetic resonance imaging for jawbone assessment compared to reference-standard measurements?”.
Eligibility criteria
The diagnostic studies (e.g., experimental, observational, clinical, animal, in vitro and ex vivo) with no language or time restriction were included following the eligibility criteria established according to the PIRD method (population, index test, reference test and diagnostic of interest) and are described as follows: population - healthy maxilla and mandible sites; index test - magnetic resonance imaging; reference test - reference-standard measurements (e.g., histology, physical measurements, or computed tomography); and diagnosis of interest - quantitative and/or bone histomorphometry measurements. The exclusion criteria for studies were as follows: evaluating maxillary and mandibular sites under deformities; traumatic, pathological, or healing conditions (these conditions can alter tissue fluid levels, potentially distorting bone assessments in MRI); not performing quantitative and/or qualitative bone histomorphometry measurements by means of MRI and reference standards; reviews, letters, abstracts, posters, research protocols, personal opinions, case reports, or technique articles; and studies in which the full-text was unavailable.
Information sources
Five electronic databases (Medline via PubMed, EMBASE, Scopus, Web of Science, and CENTRAL [the Cochrane Central Register of Controlled Trials Cochrane Library]) were used to identify studies by two reviewers. The searches were conducted up to June 22nd, 2022, and updated on August 18th, 2023. No time or language restrictions were applied. Additionally, the reference lists of the studies included in the full-text analyses and of relevant review articles on the topic [6, 12, 16, 24,25,26,27] were manually searched.
Search strategy
The primary search strategy was obtained and applied to the PubMed database. Later, the primary search was adapted for other databases to meet their requirements (additional file 1).
Selection process
Duplicates were removed, and two reviewers (H.P. and S.S.) independently examined the studies by title and abstract for full-text reading. Afterwards, the eligibility criteria were applied to the studies remaining, resulting in the inclusion of studies in this review. Conflicts were settled by consensus or, if they persisted, by the judgment of a third independent review author (L. B.). All articles that did not meet the eligibility criteria were excluded and are presented in additional file 2.
Data collection process and items
The data from the included studies were extracted in duplicate by two reviewers and cross-checked. Quantitative bone histomorphometry was regarded as the primary outcome. The definitions from the American Society for Bone and Mineral Research were adopted for bone tissue (cortical or cancellous), and the histomorphometry outcomes included linear measurements (distance between points) and structural indices (e.g., trabecular bone density, trabecular separation, and trabecular width) [28]. When needed, the authors of the included studies were contacted to obtain additional information.
Study risk of bias assessment
The risk of bias was assessed using the Quality Assessment Tool for Diagnostic Accuracy Studies-2 (QUADAS-2) by two independent reviewers. The tool is divided into four categories: patient selection, index test, reference standard, and flow and timing. The questions were answered as “Yes”, “Unclear” or “No” according to the potential risk of bias [29].
Certainty assessment
The certainty of evidence was assessed according to the Grading of Recommendation Assessment, Development, and Evaluation (GRADE) criteria [30] by two independent reviewers.
Results
Study selection
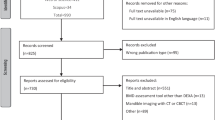
The electronic search identified 1681 articles, which were reduced to 825 after duplicate removal. Sixty-three articles were selected for full-text analysis after the title and abstract were screened. The full texts of two studies were not found; thus, they were excluded. Finally, 54 articles were excluded during this stage (reasons for exclusion are reported in additional file 2), leaving nine articles suitable for this review (Fig. 1). Cohen’s kappa coefficient for interrater reliability was 0.868.
Study characteristics
The study characteristics are described in Table 1. In total, four in vivo [9, 31,32,33], three in vitro [11, 12, 34], and two ex vivo/in vitro [10, 35] studies were assessed, including a total of 54 patients, 35 cadavers and one phantom. Most of those studies evaluated the mandible [9,10,11,12, 32,33,34,35], and three studies evaluated the maxilla [10, 12, 33], mostly at posterior sites [9,10,11,12, 35]. In terms of diagnostic purposes, most studies have evaluated MRI for dental implant planning [9, 12, 31,32,33,34], two studies have focused on maxillofacial surgery planning [11, 35], and one has applied MRI for routine maxillofacial diagnosis [10]. For outcomes, most studies have evaluated bone geometric accuracy through linear measurements [9,10,11,12, 33,34,35] and angular measurements. Two studies assessed the trabecular structure through bone density/volume [31, 32]. The most common reference test was CT [9, 11, 34, 35], followed by digital calipers [11, 34, 35], CBCT [10, 12, 31, 33], µ-CT [31, 32] and histology [10]. Additionally, the studies differed according to the MRI device, magnetic field strength, sequence parameters, and radiofrequency coil employed.
Synthesis of results
A summary of the comparisons between MRI and the reference tests is presented in Table 2. The geometric accuracy of MRI has varied among studies. The deviation in linear measurements ranged from lower values, such as 0.03 mm [34] and 0.04 mm [10], to higher values, reaching 1.67 mm [34] and 3.11 mm [12]. However, MRI measurements showed strong correlations and/or no significant differences compared to histology [10], digital calipers [34, 35] micrometer [35], CT [9, 11, 34], or CBCT [10,11,12, 33].
Bone structural assessments were performed by two studies that measured bone density/volume. Both studies applied high-strength magnetic fields (14T [31] and 15T [32]) and reported a positive correlation between MRI and µCT measurements. However, one study found a weak correlation between MRI and CBCT values [31].
Risk of bias
The QUADAS-2 assessment is shown in Fig. 2. Most studies [9,10,11,12, 34, 35] presented a high risk of bias for patient selection due to the lack of clear inclusion and exclusion criteria, whereas three studies [31,32,33] reported detailed eligibility criteria. The index test, reference standard test, time, and flow were regarded as having a low risk of bias for all included studies. Additionally, all the included studies presented low applicability concerns for patient selection, index tests, and reference standard tests.
Assessment of the quality of evidence
GRADE assessed certainty as very low due to the high risk of bias for patient selection and heterogeneity across the included studies (Table 3).
Discussion
This systematic review evaluated whether MRI can be considered a viable method for assessing the jawbone in the maxillofacial region and demonstrated similar results to those of standard reference tests. These findings support the potential of MRI as a valuable tool in the evaluation and diagnosis of jawbone tissues [36] However, the limited number of studies and methodological heterogeneity require careful interpretation, and further studies are needed to establish the comprehensive scope and reliability of MRI in the assessment of maxillofacial bones.
MRI requires a wide range of parameters to assess bone tissues [27], resulting in variability in image quality [37, 38]. These parameters include magnetic field strength and MRI sequences. Therefore, the variations in diagnostic questions among the included studies resulted in variations in the MRI protocols and analysis methods, tailored to the specific objectives of each investigation [39]. One challenging factor in MRI is the rapid signal decay of bone tissue. This factor can be overcome by faster MRI sequences with high signal-to-noise ratios and contrast-to-noise ratios to improve the visualization and segmentation of bone tissue [27] (e.g., 3D VIBE [35], gradient-echo fast low flip angle shots (FLASH) [10], and zero echo time (ZTE)) [12].
In general, MRI reveals image quality, the ability to visualize bone structures [10, 33,34,35] and consistent quality in defining bone boundaries, as confirmed by high intraobserver and interobserver agreement [34]. For the jawbone, several different MRI sequences were tested to determine the optimal parameters for imaging, focusing on both the examination time and image quality. As a result, the 3D volumetric interpolated breath-hold examination (VIBE) sequence presented the clearest visibility of cortical bone structures [35]. Additionally, other methods for improving jawbone visibility, including the use of dedicated inductively coupled radiofrequency coils attached to oral tissues, which are capable of identifying several maxillofacial structures, including the individual branches of the inferior alveolar nerve, were tested [10].
While the majority of the included studies evaluated dental implant planning, maxillofacial surgery, and diagnosis, a wide range of MRI findings for evaluating the maxillofacial region has also been recently reported [36, 40]. Most included in vitro designs, which exclude clinical factors and lack the complexity of living biological systems. Consequently, the lack of these clinical factors may limit the external validity and generalizability of the findings to real clinical situations, where patient-specific variations are integral to diagnostic and therapeutic decision-making processes.
Variations in study design can introduce inconsistencies in bone measurements and affect the comparability of results across studies. Therefore, the high heterogeneity in imaging protocols and study methodologies restricted quantitative analysis of the findings and resulted in a high risk of bias and very low certainty of evidence. This heterogeneity also limited comparisons between studies and analyses of the reliability, accuracy, and efficacy of MRI for bone assessment in the maxillofacial region. For instance, MRI was compared to different index tests and varied on the outcomes evaluated across studies, potentially leading to different conclusions, or over- and underestimation results.
Like other medical imaging methods, MRI is susceptible to artifacts induced by the presence of various materials within patients [41]. This susceptibility can lead to inadequate visualization or inaccurate assessment of bone structures within regions affected by these artifacts, potentially reducing the accuracy of MRI. However, the impact of these artifacts on accuracy was not explored in most of the included studies. In addition, the exclusion of patients with metallic materials from studies further adds to this limitation, thereby restricting the scope of clinical investigations and their applicability. To address this limitation, improved imaging techniques and postprocessing techniques can be used to mitigate the impact of metallic artifacts and increase the diagnostic value of MRI in this context.
MRI-based assessments of bone morphology are limited by partial volume effects caused by the disparity between MRI resolution and trabecular size, which typically measures 0.1 mm [25]. In cases where the voxel size exceeds this size, trabecular broadening may occur, potentially resulting in the loss or merging of fine trabeculae and thus leading to over- or underestimation [25]. Comparisons with CBCT can also be challenging because of the difference in spatial resolution and image contrast, which consequently impacts the ability to detect fine details of bone morphology and trabecular structure.
During MRI scan planning, balancing the field of view, resolution, signal-to-noise ratio, and acquisition time is essential [42]. However, sequences optimized for bone visualization present unique constraints influenced by factors such as the imaged region’s size and tissue-specific properties like magnetic susceptibility, potentially limiting their utility in certain contexts [42]. Another limitation of the included studies was the scan time, which varied from a few minutes to several hours. Therefore, clinical applications should consider the possibility of motion artifacts. Despite the recent improvements, accessibility, cost, and patient discomfort also should be considered for further clinical application.
Future perspectives on jawbone assessment with MRI include optimizing magnetic fields to improve image quality and resolution; optimizing gradient strength and linearity for faster and more accurate imaging; developing dedicated radiofrequency coils to improve the signal-to-noise ratio and contrast, reduce unwanted signals, and improve patient comfort; refining pulse sequences, especially those dedicated to tissues with fast decaying signals; and improving scanner hardware and software for providing cost-effective image reconstruction and processing [10, 31, 36, 43]. Additionally, the literature still lacks a sensitivity and specificity evaluation of MRI for jawbone assessment [10].
Conclusions
Limited studies suggest the feasibility of MRI for assessing the jawbone, as MRI provides comparable results to those of standard reference tests. However, further advancements and optimizations are required to increase the applicability, validate the efficacy, and establish the utility of these methods in clinical settings.
Data availability
Data described in the manuscript, code book, and analytic code will be made available upon request pending application and approval from the corresponding author.
References
White SC, Pharoah MJ. The evolution and application of Dental Maxillofacial Imaging modalities. Dent Clin North Am. 2008;52:689–705.
Weishaupt D, Köchli VD, Marincek B, Froehlich JM, Nanz D, Pruessmann KP. How does MRI work? An introduction to the physics and function of magnetic resonance imaging. Volume 2. Springer; 2006.
Jerban S, Chang DG, Ma Y, Jang H, Chang EY, Du J. An update in qualitative imaging of bone using Ultrashort Echo Time magnetic resonance. Front Endocrinol (Lausanne). 2020;11:1–12.
Rao AD. Novel techniques for assessment of bone tissue material properties. Curr Opin Endocrinol Diabetes Obes. 2023;30:213–6.
Burdiles A, Babyn PS. Pediatric Bone Marrow MR Imaging. Radiol Clin North Am. 2009;47(6):879–97.
Nishimura DA, Choi IGG, Arita ES, Cortes ARG. Estimating bone mineral density using MRI in medicine and dentistry: a literature review. Oral Radiol. 2021;37:366–75.
West SL, Rajapakse CS, Rayner T, Miller R, Slinger MA, Wells GD. The reproducibility of measuring trabecular bone parameters using a commercially available high-resolution magnetic resonance imaging approach: a pilot study. Bone Rep. 2018;8:180–6.
Bohner L, Tortamano P, Meier N, Gremse F, Kleinheinz J, Hanisch M. Trabecular bone assessment using magnetic-resonance imaging: a pilot study. Int J Environ Res Public Health. 2020;17:1–7.
Imamura H, Sato H, Matsuura T, Ishikawa M, Zeze R. A comparative study of computed tomography and magnetic resonance imaging for the detection of mandibular canals and cross-sectional areas in diagnosis prior to dental implant treatment. Clin Implant Dent Relat Res. 2004;6(2):75–81.
Flügge T, Hövener JB, Ludwig U, Eisenbeiss AK, Spittau B, Hennig J, et al. Magnetic resonance imaging of intraoral hard and soft tissues using an intraoral coil and FLASH sequences. Eur Radiol. 2016;2:4616–23.
Deng W, Huang D, ying, Chen S ling, Chen J, xin. Liao T an. Geometric accuracy of magnetic resonance imaging displaying the inferior alveolar nerve. Chinese J Tissue Eng Res. 2014;18:3840.
Fuglsig JM, de Hansen C, Schropp B, Nixdorf L, Wenzel DR, Spin-Neto A. R. Alveolar bone measurements in magnetic resonance imaging compared with cone beam computed tomography: a pilot, ex-vivo study. Acta Odontol Scand. 2022; 0:1– 8.
Mendes S, Rinne CA, Schmidt JC, Dagassan-Berndt D, Walter C. Evaluation of magnetic resonance imaging for diagnostic purposes in operative dentistry—a systematic review. Clin Oral Investig. 2020;24:547–57.
Sennimalai K, Selvaraj M, Kharbanda OP, Kandasamy D, Mohaideen K. MRI-based cephalometrics: a scoping review of current insights and future perspectives. Dentomaxillofacial Radiol. 2023;52:20230024.
Al-Haj Husain A, Schmidt V, Valdec S, Stadlinger B, Winklhofer S, Schönegg D, et al. MR-orthopantomography in operative dentistry and oral and maxillofacial surgery: a proof of concept study. Sci Rep. 2023;13:6228.
Al-Haj Husain A, Stadlinger B, Winklhofer S, Piccirelli M, Valdec S. Magnetic resonance imaging for preoperative diagnosis in third molar surgery: a systematic review. Oral Radiol. 2023;39:1–17.
Bracher AK, Hofmann C, Bornstedt A, Hell E, Janke F, Ulrici J, et al. Ultrashort echo time (UTE) MRI for the assessment of caries lesions. Dentomaxillofacial Radiol. 2013;42(6):20120321.
Flügge T, Ludwig U, Hövener JB, Kohal R, Wismeijer D, Nelson K. Virtual implant planning and fully guided implant surgery using magnetic resonance imaging - proof of principle. Clin Oral Implants Res. 2020;(February):1–9.
Probst FA, Burian E, Malenova Y, Lyutskanova P, Stumbaum MJ, Ritschl LM, et al. Geometric accuracy of magnetic resonance imaging–derived virtual 3-dimensional bone surface models of the mandible in comparison to computed tomography and cone beam computed tomography: a porcine cadaver study. Clin Implant Dent Relat Res. 2021;23:779–88.
Hilgenfeld T, Juerchott A, Jende JME, Rammelsberg P, Heiland S, Bendszus M, et al. Use of dental MRI for radiation-free guided dental implant planning: a prospective, in vivo study of accuracy and reliability. Eur Radiol. 2020;30:6392–401.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Int J Surg. 2021;88:105906.
Booth A, Clarke M, Ghersi D, Moher D, Petticrew M, Stewart L. An international registry of systematic-review protocols. Lancet. 2011;377:108–9.
Parize H, Sadilina S, Kleinheinz J, Dalva Cruz L, Sesma N, Lauren B. Magnetic resonance imaging for maxillofacial bone assessment: a systematic review. PROSPERO Int Prospect Regist Syst Rev. 2022; 1–5.
Wehrli FW. Structural and functional assessment of trabecular and cortical bone by micro magnetic resonance imaging. J Magn Reson Imaging. 2007;25:390–409.
Soldati E, Rossi F, Vicente J, Guenoun D, Pithioux M, Iotti S, et al. Survey of mri usefulness for the clinical assessment of bone microstructure. Int J Mol Sci. 2021;22:1–27.
Wang F, Zheng L, Theopold J, Schleifenbaum S, Heyde CE, Osterhoff G. Methods for bone quality assessment in human bone tissue: a systematic review. J Orthop Surg Res. 2022;17:174.
Florkow MC, Willemsen K, Mascarenhas VV, Oei EHG, van Stralen M, Seevinck PR. Magnetic resonance imaging Versus Computed Tomography for three- dimensional bone imaging of Musculoskeletal pathologies: a review. J Magn Reson Imaging. 2022;56:11–34.
Dempster DW, Compston JE, Drezner MK, Glorieux FH, Kanis JA, Malluche H et al. Standardized nomenclature, symbols, and units for bone histomorphometry: a 2012 update of the report of the ASBMR Histomorphometry Nomenclature Committee. 28, J Bone Miner Res. 2013. 28;2.
Whiting PF, Rutjes AWS, Westwood ME, Mallett S, Deeks JJ, Reitsma JB, et al. QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med. 2011;155:529–36.
Schünemann HJ, Oxman AD, Brozek J, Glasziou P, Jaeschke R, Vist GE, et al. Grading quality of evidence and strength of recommendations for diagnostic tests and strategies. BMJ. 2008;336:1106–10.
Choi IGG, Pinhata-Baptista OH, Ferraço R, Kim JH, Abdala Júnior R, Arita ES, et al. Correlation among alveolar bone assessments provided by CBCT, micro-CT, and 14 T MRI. Dentomaxillofac Radiol. 2022;51:20210243.
Cortes ARG, Cohen O, Zhao M, Aoki EM, Ribeiro RA, Abu Nada L et al. Assessment of alveolar bone marrow fat content using 15 T MRI. Oral surg oral Med oral pathol oral Radiol.2018; 125:244–9.
Al-Haj Husain A, Stadlinger B, Özcan M, Schönegg D, Winklhofer S, Al-Haj Husain N, et al. Buccal bone thickness assessment for immediate anterior dental implant planning: a pilot study comparing cone-beam computed tomography and 3D double-echo steady-state MRI. Clin Implant Dent Relat Res. 2023;25:35–45.
Aguiar MF, Marques AP, Carvalho ACP, Cavalcanti MGP. Accuracy of magnetic resonance imaging compared with computed tomography for implant planning. Clin Oral Implants Res. 2008;19:362–5.
Goto TK, Nishida S, Nakamura Y, Tokumori K, Nakamura Y, Kobayashi K, et al. The accuracy of 3-dimensional magnetic resonance 3D vibe images of the mandible: an in vitro comparison of magnetic resonance imaging and computed tomography. Oral surgery. Oral Med Oral Pathol Oral Radiol Endodontology. 2007;103:550–9.
Flugge T, Gross C, Ludwig U, Schmitz J, Nahles S, Heiland M, et al. Dental MRIonly a future vision or standard of care? A literature review on current indications and applications of MRI in dentistry. Dentomaxillofacial Radiol. 2023;52:1–13.
National Research Council. Mathematics and Physics of emerging Biomedical Imaging. National Academies; 1996.
Assaf AT, Zrnc TA, Remus CC, Schönfeld M, Habermann CR, Riecke B, et al. Evaluation of four different optimized magnetic-resonance-imaging sequences for visualization of dental and maxillo-mandibular structures at 3 T. J Cranio- Maxillofacial Surg. 2014;42:1356–63.
Maraghelli D, Pietragalla M, Calistri L, Barbato L, Locatello LG, Orlandi M, et al. Techniques, tricks, and stratagems of oral cavity computed tomography and magnetic resonance imaging. Appl Sci. 2022;12:1473.
Johnson M, Sreela LS, Mathew P, Prasad TS. Actual applications of magnetic resonance imaging in dentomaxillofacial region. Oral Radiol. 2022;38:17–28.
Bohner L, Hanisch M, Sesma N, Blanck-Lubarsch M, Kleinheinz J. Artifacts in magnetic resonance imaging caused by dental materials: a systematic review. Dentomaxillofacial Radiol. 2022;51:20210450.
Florkow MC, Willemsen K, Mascarenhas VV, Oei EHG, van Stralen M, Seevinck PR. MRI versus CT for bone imaging: a review. J Magn Reson Imaging. 2022;56(1):11–34.
Özen AC, Ilbey S, Jia F, Idiyatullin D, Garwood M, Nixdorf DR et al. An improved intraoral transverse loop coil design for high-resolution dental MRI. Magn Reson Med. 2023; 1728–37.
Funding
This study was supported by the International Team for Implantology (ITI) through the Grant 2019_1425. Also, HP and SS were ITI Scholars. We acknowledge support from the open access publication fund of the University of Münster.
Author information
Authors and Affiliations
Contributions
Conceptualization, H.P., S.S., J.K., N.S, D.C.L. and L.B.; methodology, H.P., S.S. and L.B.; writing—original draft preparation, H.P.; writing—review and editing, S.S., R.A.C., J.V.C.C., J.K., N.S, D.C.L., and L.B; supervision, R.A.C., J.K., N.S, D.C.L.; project administration, L.B.; funding acquisition, J.K and L.B. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Ethical approval
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
The online version contains supplementary material available at.
Additional file 1:
Search strategies according to the database queried.
Additional file 2:
Articles excluded and the reasons for exclusion.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Parize, H., Sadilina, S., Caldas, R.A. et al. Magnetic resonance imaging for jawbone assessment: a systematic review. Head Face Med 20, 25 (2024). https://doi.org/10.1186/s13005-024-00424-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13005-024-00424-2