Abstract
Background
Secretory breast carcinoma (SBC) is a rare malignant breast neoplasm with distinct histological features, including solid, microcystic, tubular, and rarely papillary structures, traditionally characterized by a t (12;15) (p13:q25) translocation, which usually leads to ETV6-NTRK3 fusion, suggesting an early event in tumorigenesis. Due to the rarity of this disease, very few genome sequencing studies have been performed on a series of cases, especially progressive cases.
Methods
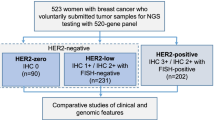
Seven lesions from 5 patients diagnosed at the Third Affiliated Hospital of Soochow University from 2007 to 2021 were included. Clinicopathological features and prognosis/survival data were collected. Next-generation DNA sequencing was performed on six of the seven lesions.
Results
In total, 3/7 (42.9%) lesions demonstrated estrogen receptor (ER) expression, including weak, moderate to strong staining, and no lesion demonstrated progesterone receptor (PR) expression. There were no cases of human epidermal growth factor (HER2) overexpression, and the Ki-67 index was low. S-100 and pan-TRK protein were diffusely positively expressed in all cases. All lesions were characterized by a t(12;15) (p13:q25) translocation, leading to ETV6-NTRK3 fusion confirmed by fluorescence in situ hybridization (FISH). The sequencing results showed that ETV6-NTRK3 fusion was the main driver of early tumorigenesis, while SBC with invasive biological behavior had more complex genomic variation in which TERT promoter mutation was detected.
Conclusions
Immunohistochemical staining of a biomarker panel, including ER, PR, HER2, Ki-67, S-100 and pan-TRK, can be used as an auxiliary diagnostic tool, and FISH detection can be used as a diagnostic tool. ETV6-NTRK3 gene fusion involving multiple sites may drive tumorigenesis, while mutations in the TERT promoter region may be a factor driving tumor progression.
Similar content being viewed by others
Introduction
Secretory breast carcinoma (SBC) is a rare breast cancer accounting for <0.05% of all invasive mammary carcinomas and was initially designated “juvenile carcinoma” by McDiwitt and Stewart in 1966 [1]. Although first described in children, SBCs affect more adults than children, with a median age of 53 years (ranging from 3 to 91 years) [1,2,3].
SBCs are traditionally characterized by a t(12;15) (p13:q25) translocation, leading to ETV6-NTRK3 fusion that presents both in the in situ and invasive components, suggesting that it is an early event in tumorigenesis [4,5,6,7,8,9]. ETV6-NTRK3, originally identified in congenital fibrosarcoma and cellular mesoblastic nephroma, encodes a constitutively activated chimeric tyrosine kinase that drives cellular transformation and oncogenesis through the RAS-MAPK and PI3K pathways [5,6,7, 10, 11]. One recent study found that in addition to ETV6-NTRK3 fusion, fusion of NTRK1 and other genes can also drive SBCs [12]. Transfer of ETV6-NTRK3 retrovirus into mouse mammary epithelial cells produced tumor-prone transformed cells in nude mice, but it is not clear whether the gene can drive tumorigenesis on its own or if additional modifications are required [6].
SBCs generally have an indolent clinical course, even in patients with axillary node metastasis [13]. In one population-based study, the 5- and 10-year cancer-specific survival rates were 94% and 91%, respectively [14]. Another study based on data from the National Cancer Database (NCDB) demonstrated that the overall survival of SBC patients was better than that of invasive ductal carcinoma (IDC) patients [15]. Given this indolent behavior, tumors are usually managed conservatively and routinely removed by surgery; there are nonspecific guidelines for radiotherapy and chemotherapy, with varying treatment regimens in the literature [14,15,16]. As more studies are conducted, it seems necessary to predict outcomes beyond the commonly used 5 or 10 years for diseases such as IDC, but longer for SBC. Most recurrence and metastasis events occur after 5 or even 10 years [17,18,19]. However, cases with rapid progression and a poor prognosis also exist [20, 21]. Cases with different biological behaviors show no obvious differences in histology, immunophenotype, etc. in studies thus far. The advent of next-generation sequencing (NGS) technology has provided an opportunity to further understand the genomic characteristics of such tumors, possibly providing clues to different behaviors. Due to the rarity of this disease, very few genome sequencing studies have been performed on a large number of cases [5, 12], and most sequencing studies are usually case reports involving one or two subjects [2, 11, 18, 22].
To gain greater insights into the biological characteristics of SCBs, especially those that showed disease progression. We described the morphology and immunophenotype of seven lesions in five SBC patients and used capture-based next-generation sequencing of 425 cancer-related genes to more comprehensively characterize the genomics of more SBCs based on previous reports.
Materials and methods
Patients
The study was approved by the Institutional Review Board of the Third Affiliated Hospital of Soochow University. Five SBC patients were identified in the pathology department archives of the Third Affiliated Hospital of Soochow University, spanning from 2007 to 2021. All specimens were fixed in 10% neutral buffered formalin and embedded in paraffin. Clinical information was obtained from the electronic medical records. All of the sections and pathological features were reviewed by two pathologists (T.L., and TB.C.) in the Third Affiliated Hospital of Soochow University. Survival outcomes were evaluated through telephone follow-ups. The disease-free survival (DFS) interval was calculated from the diagnosis of the disease until the first instance of disease progression.
Immunohistochemistry (IHC)
IHC analysis was performed for estrogen receptor (ER) (Ventana, Tucson, Arizona, USA), progesterone receptor (PR) (Ventana, Tucson, Arizona, USA), human epidermal growth factor (HER2/neu) (Ventana, Tucson, Arizona, USA), Ki-67 (Ventana, Tucson, Arizona, USA), S-100 (1:100, MXB Biotechnology, Fujian, China), and pan-TRK (1:100, ZSGB- BIO, Beijing, China). After dewaxing and hydration, 4 µm formalin-fixed paraffin-embedded (FFPE) tissue sections were treated with an immunohistochemical automatic staining machine according to the scheme provided by the Benchmark XT system. For ER, PR, and HER2, positive staining was defined according to American Society of Clinical Oncology/College of American Pathologists (ASCO/CAP) guidelines. For all other markers, positive expression was defined as cytoplasmic (S-100) or nuclear (pan-TRK) staining.
Fluorescence in situ hybridization (FISH)
For ETV6 fluorescence in situ hybridization, 4-μm (FFPE) tumor sections were baked at 60 °C for 1 h, rinsed in 100% ethanol, and then pretreated with 0.2 N HCl (20 min, room temperature), followed by 1 M NaSCN (30 min, 80 °C) before protease digestion with pepsin (2.5 mg/ml pepsin for 27 min at 37 °C). The slides were then fixed in 10% phosphate-buffered saline-buffered formalin, rinsed, dehydrated in an ethanol series, and air dried. The slides were hybridized overnight at 37 °C with a commercial ETV6 break-apart probe (Vysis ETV6 Break Apart FISH Probe Kit, Abbott) according to the manufacturer’s instructions. The slides were washed to remove unbound probes and counterstained with 4,6 diamidino-2-phenylindole. Enumeration of break-apart signals was conducted using a Zeiss fluorescence microscope.
DNA isolation
DNA was extracted from FFPE representative 5-μm tumor tissues using a QIAamp DNA FFPE Tissue Kit (Qiagen, Cat No. 56404) according to the manufacturer’s instructions. The quality of DNA was verified by migration on agarose gel, and the concentration of DNA was quantified by spectrophotometer (Nanodrop 2000, Thermo).
Capture-based next-generation DNA sequencing
Sequencing was performed at a commercial laboratory using an assay that targets the coding regions of 425 cancer-related genes. For the commercial next-generation sequencing (NGS) panel, the mean (n = 41) mapped reads per sample was 463127 (range 111595-646854), the mean depth per base was 3811 (range 983-6145) and the mean reads on the target sequence was 94.57% (range 71.73%-98.71%). Original image data were transferred by base calling analysis into raw sequence data. Single nucleotide variants (SNVs) and short insertions/deletions (indels) were identified by VarScan2 with the minimum variant allele frequency threshold set at 0.01 and a p value threshold for calling variants set at 0.05 to generate Variant Call Format files. All SNVs/indels were annotated with Annotate Variation (ANNOVAR), and each SNV/indel was manually checked on the Integrative Genomics Viewer. Copy number variation analysis was performed using an inhouse developed pipeline. A fold change threshold of 1.6 and 0.6 in DNA copy number was set as the cutoff for amplification and deletion, respectively.
Statistical analysis
Patient clinicopathological characteristics and outcomes are reported as number (%), mean ± SD, or median (95% confidence interval [CI]), as appropriate.
Results
Clinical characteristics and outcomes
The clinicopathologic features, treatment, and follow-up data of SCB patients are summarized in Table 1. All five patients were female, with a median age of 39 years and a mean age of 34.8 ± 3.4 years (range from 33 to 42 years) at first onset. Tumor size ranged from 0.9 to 7.0 cm, with a median size of 2.0 cm and a mean size of 2.7 ± 2.21 cm. Of the five primary cases, three were located in the left mammary gland, and two were located in the right mammary gland, one of which was associated with axillary lymph node metastasis.
The follow-up time ranged from 8 to 170 months. Patient 1 developed contralateral SBC 140 months after the occurrence of left SBC, and Patient 2 developed chest wall recurrence and distant metastasis 84 months after diagnosis. Patient 5 had concurrent primary breast tumors, including SBC and invasive ductal carcinoma (IDC), with no signs of disease progression during an 8-month follow-up. Patient 3 and Patient 4 both had a single lesion, and the follow-up time was short without disease progression. All five (5/5, 100%) patients underwent mastectomy or lumpectomy plus axillary lymph node dissection, in which three of five (3/5, 60%) patients received chemotherapy for the first onset. The patient with moderate to strong ER expression also received radiotherapy and hormonal therapy in addition to chemotherapy (Table 1).
Pathological features and immunohistochemical profiles
All the cases in our study showed a typical SBC morphology composed of polygonal cells with eosinophilic or vacuolated cytoplasm. Round or oval nuclei were arranged in a microcystic, cystic or solid growth pattern in which intracytoplasmic and extracellular amphophilic or eosinophilic secretion existed (Fig. 1). Only one recurrent case showed extensive fibrotic segmented cords and glandular tubular structures. The histological features of every case are shown in Table 2.
SBC (hematoxylin and eosin staining). A Solid area separated by a fibrous septum with intracellular mucinous vacuoles and eosinophilic secretory vacuoles. B, C Solid and microcystic structure with intracellular and extracellular vacuoles. D Tubular area with intracellular and extracellular eosinophilic vacuoles. E Solid structure separated by fibrous septum with extracellular eosinophilic secretion. F Metastatic SBC components in axillary lymph nodes in Patient 2
In all seven lesions, three lesions (3/7, 42.9%) demonstrated ER expression, and no lesion demonstrated PR expression. There were no HER2 overexpression cases. The Ki-67 index ranged from 5% to 35% and was relatively higher in the primary and recurrent lesions of patients with recurrence and distant metastasis. S-100 was diffusely positive in all the cases, and NTRK was diffusely and strongly positively expressed in all nuclei in all cases (Fig. 2).
Immunohistochemistry staining of SBC. A Weak positive ER staining. B Moderate to strong positive ER staining. C Relatively low Ki-67 index/immunoreactivity. D Relatively high Ki-67 index/immunoreactivity. E, F Diffuse and strong S-100 immunoreactivity. G, H Strong positive nuclear staining for Pan-TRK in all cases
Genomics of SBCs
All seven lesions were available for ETV6 break-apart probe detection, in which all the lesions showed break-apart signals (Fig. 3).
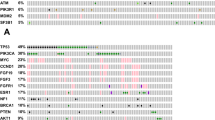
Six of the seven lesions were available for 425 cancer-related gene DNA sequencing detections. All six SBCs revealed ETV6–NTRK3 gene fusions by DNA sequencing, showing a variety of fusion sites, including exon 5 of ETV6 and exon 15 of NTRK3, which were the most frequent alterations; exon 6 of ETV6 and exon 15 of NTRK3; and exon 6 of ETV6 and exon 14 of NTRK3. Patient 1, who developed asynchronous SBCs in the bilateral breast; this patient showed different ETV6–NTRK3 gene fusion sites in the two neoplastic tissues and exhibited no other alterations. In patient 2, except for the same ETV6-NTRK3 gene fusion sites, DOT1L, KDM5A, and LRP1B were also existed in the primary lesion, and TERT and STAT3 mutations were detected in recurrent lesions. Patient 3 had two ETV6-NTRK3 gene fusion sites, exon 5 of ETV6 and exon 15 of NTRK3 and exon 6 of ETV6 and exon 15 of NTRK3. PGR gene variation was also detected. Only the fusion of exon 5 of ETV6 and exon 15 of NTRK3 was detected in patient 4 (Fig. 4). All the lesions showed a low tumor mutation burden (TMB) ranging from 0 mut/Mb to 3.2 mut/Mb, and recurrent lesions had the highest TMB values.
Summary of next-generation sequencing results for 6 lesions in 4 secretory carcinoma patients. All lesions demonstrated ETV6–NTRK3 gene fusion by DNA sequencing. Patient 2 sequencing results showed DOT1L, KDM5A, LRP1B variants in primary lesions and TERT and STAT3 mutation variants in recurrent lesions, except for the same ETV6-NTRK3 gene fusion sites. Patient 3 had two ETV6-NTRK3 gene fusion sites, and PGR gene variation was detected.
Discussion
SBCs are rare malignant neoplasms of the breast with distinct histological features, including solid, microcystic, tubular, and rarely papillary structures [1, 6, 18]. Recent research has revealed that in addition to ETV6-NTRK3 fusion, fusion of NRTK1 with other gene partner genes also drives tumorigenesis [12]. Although an increasing number of studies on SBC have been reported, gene sequencing studies of multiple cases, especially recurrent and metastatic cases, are still limited. In our study, clinicopathological features, treatment modalities, and prognostic information of 7 lesions in 5 patients with SBCs were summarized, and the genomic characteristics of these patients were analyzed using next-generation sequencing technology.
All our cases showed typical morphological features with round or oval nuclei arranged in microcystic or solid growth patterns and intracellular and extracellular eosinophilic or eosinophilic secretions. A panel of IHC markers, including ER, PR, HER2, Ki-67, S-100 and Pan-TRK [2, 23,24,25], may serve as a useful tool to aid the diagnosis of SCB. Initial studies have shown that SBC is usually triple negative or weakly positive for hormone receptors with S-100 positive expression [26,27,28]. With further research, we found that cases with moderate or even strong ER positivity also existed and that S-100 is expression is not specific to SBCs [4, 5, 27]. With the development of molecular detection technology, pan-TRK protein, which recognizes a conserved sequence near the C-terminus of TRK proteins, has been found to have certain sensitivity and specificity in ETV6-NTRK fusion tumors [23, 24, 29]. The literature shows that the unique morphology of the tumor combined with diffuse and at least focal strong nuclear staining can be used for the initial diagnosis in most cases [23, 24, 30]. FISH is still recommended for patients with atypical histomorphology or negative pan-TRK protein expression [23, 24]. Since alternations in both NTRK3 and NTRK1 drive tumorigenesis, it is important to use pan-TRK immunohistochemical staining in the initial screening and to use multiple probes for FISH detection. Our immunohistochemical results showed that pan-TRK protein was localized in the nucleus and diffuse and strongly stained in all cases, and ETV6 break-apart probes were positive for FISH detection.
Further revealing the genomic characteristics of SBC can provide a better understanding of the biological behavior of this disease and provide clues for its prognosis and treatment. To comprehensively describe the gene expression profile of SBC, we summarize the molecular information of SCB detection by NGS in the literature in Table 3 as follows: Krings’ study showed that SBC is mainly driven by fusion of the ETV6-NTRK3 gene, and the DNA breakpoints were mostly in ETV6 intron 5 and NTRK3 intron 14 [5]. In addition, fusion of exon 5 of ETV6 and exon 15 of NTRK3 was detected in two SBCs with distant metastasis, and additional gene variants were present in the two SBCs [18, 22]. Maund et al. detected additional fusion driver genes (LMNA-NTRK1 and TPM3-NTRK1) and some other pathogenic genes, including CCND1, TERT, EMSY, and CDH1 et al [12]. UGT1A1 variants other than ETV6-NTRK3 were found in SBCs with lymph node metastases reported by Chen et al [2]. Compared with the above studies, our study presented more diverse ETV6-NTRK3 gene fusion sites. Although only one case in this study had a mutation in the TERT promoter region, this mutation has been detected in previous studies and in recurrent lesions [12, 18, 22]. The diverse fusion sites of the ETV6 and NTRK3 genes included exon 5 of ETV6 and exon 15 of NTRK3, exon 6 of ETV6 and exon 15 of NTRK3, and exon 6 of ETV6 and exon 14 of NTRK3. The duplication of ETV6-NTRK3 reported in Krings’ Lambros’ and Chen’s study was not detected in our research [2, 5, 11]. It has been shown that the ETV6–NTRK3 fusion gene encodes a chimeric tyrosine kinase that signals through Ras-mitogen-activated protein kinase and phosphatidylinositol-3 kinase pathways to transform cells of multiple lineages, regardless of the molecular type of SBC [5, 6].
It is generally believed that most SBCs have a triple-negative phenotype or weak positive expression of hormone receptors, and the cases of these two phenotypes have similar signaling pathways [5]. Moderate to strong positive cases of hormone receptors also exist, while cases of HER2 overexpression are extremely rare [4, 15, 16]. However, whether there are differences in the genomic characteristics of such cases has not been reported. In our study, 1 lesion was moderately to strongly positive for ER with approximately 30% neoplastic cells, 2 lesions were weakly positive for ER, and the remaining 4 lesions were triple negative. The rate of moderate to strong positive ER staining among our cases was approximately 20% (1/5), which was similar to that of SBCs reported in the literature (range, 5% to 30%) [4]. Several moderately ER-positive cases in Krings' study had no additional variants except for ETV6-NTRK3 gene fusion [5]. Two fusion sites, including 5 of ETV6 and exon 15 of NTRK3 and exon 6 of ETV6 and exon 15 of NTRK3, were detected in cases with moderate to strong positive staining for ER, and PGR mutations were also detected. PGR encodes proteins belonging to the steroid receptor superfamily that mediate the physiological effects of progesterone and play a central role in reproductive events related to the establishment and maintenance of pregnancy [31]. Among its related pathways are “mammary gland development pathway - puberty (stage 2 of 4)” and “signal transduction”. A number of studies have reported associations between PGR gene variants and hormone-related disorders, including breast cancer, where PGR gene mutation more frequently affects ER-positive breast cancer [31, 32].
In one patient, two asynchronous lesions were both weakly positive for ER expression and had different ETV6-NTRK3 fusion sites, and no other alterations were found. The interval for onset of the two lesions was more than 10 years, and no evidence of other site involvement was found. Because of the different gene fusion sites, the two tumors may be double primary tumors, and their similar morphological characteristics and immunophenotypes may be attributed to the unity of the host environment. Similar to common invasive ductal carcinoma, there can be double primary cases of secretory carcinoma. Only Castillo et al reported double primary SBCs in which a patient developed SBC at 14 years old and had a second SBC at 30 years old in the same breast, but the second lesion had a different CGH-array profile [4]. The genomic characteristics of such tumors are not different from those of single tumors but provide clues for the choice of treatment for such tumors.
In this study, the patient who developed distant metastasis and chest wall recurrence had the most aggressive behavior and the most complex genome. The fusion site of ETV6-NTRK3 was the same as that in distant metastatic cases reported in the literature [18]. Hoda et al reported two distant metastases of SBC, one of which had concurrent chest wall recurrent lesions [18]. Sequencing of one chest wall recurrent lesion showed TERT C228-T promotor mutation, while the primary lesion in the other showed no TERT mutation. The incidence of TERT gene promoter mutation in solid tumors is more than 10%, which can generate a new ETS/TCF common binding motif (AAGGCC), promote TERT gene transcription, and enhance telomerase activity. ETS transcription factor binding can promote hTERT transcription factors such as C-MYC and SP1 binding to it in a specific microenvironment [33]. Their respective sites upregulate hTERT transcription and telomerase high expression, activate the MAPK signaling pathway, promote tumor transformation, survival, proliferation and invasion, and participate in the occurrence and development of tumors [34]. TCF transcription factor binding can promote the activation of the Wnt/β-catenin signaling pathway, which is involved in the occurrence and development of tumors and affects prognosis [35, 36]. Targeted gene therapy based on the telomerase hTERT promoter provides a new approach for the treatment of tumors [37, 38]. All the evidence suggests that TERT promoter mutation may be involved in the progression of SBCs, especially those that undergo distant metastasis. In addition to TERT promoter mutation, another mutation is the STAT3 mutation, which has a very low allele frequency (1%) in recurrent lesions, indicating that this gene may not participate in the tumorigenesis and progression of the disease. Comparing the gene expression profiles of the primary and secondary lesions, the lesions had the same ETV6-NTRK3 fusion gene, and the primary lesions also had DOT1L, KDM5A and LRP1B variants. Diseases associated with DOT1L include NUT midline carcinoma and acute promyelocytic leukemia. Among DOT1L related pathways are the PKMT pathway, which involves the methylation of histone lysines, and chromatin organization. Variants of DOT1L have been detected in triple-negative breast cancer [39]. LRP1B, which encodes endocytic LDL-family receptor, is among the top 10 significantly mutated genes in human cancer [40]. It has been demonstrated that LRP1B can bind to multiple extracellular ligands, including fibrinogen and apo E-carrying lipoproteins [40, 41]. Frequent inactivating mutations of LRP1B have been observed in many malignant tumors, including triple-negative breast cancer, whereas its mutation could still have a functional consequence in tumorigenesis and heterogeneity [40, 41]. The KDM5A-encoded protein plays a role in gene regulation through the histone code by specifically demethylating lysine 4 of histone H3 [42]. The encoded protein interacts with many other proteins, including retinoblastoma proteins, and is involved in the transcriptional regulation of Hox genes and cytokines [43]. The gene may play a role in tumor progression, which has been detected to be abnormally expressed in triple-negative breast cancer [44]. Variations in all three of these genes may participate in the progression of the tumor. In addition to the ETV6-NTRK3 gene fusion, PGR, TERT, DOT1L, KDM5A and LRP1B mutations may be passenger mutations that promote tumor progression. To date, the genomic profiles of only three SBC patients with distant metastases have been reported, including that of one patient in our study. Compared with the SBC genomic profile reported without distant metastases, patients with recurrence or metastasis had more complex genomic alterations [2, 11, 13, 18, 22]. This case had axillary lymph node metastasis at the time of initial diagnosis, and the genome of this case was relatively complex compared to that of the cases with axillary lymph node metastasis that had a favorable prognosis reported in the literature [2].
The treatment regimens in our study included lumpectomy, modified radical mastectomy and modified radical mastectomy with adjuvant radiotherapy, chemotherapy or endocrine therapy. According to the literature, although there are cases of rapid progression, most tumors show an indolent growth process that requires observation and follow-up for more than 10 years. The current study shows that this group of cases lacks a unified treatment regimen, as indicated by clinical trials and literature reports targeting TRKs, which may have therapeutic value in NTRK rearrangement-related malignant tumors, including SBC [45]. The treatment can be done relatively early, rather than waiting for other treatments to work. Current studies suggest that in addition to the fusion of the ETV6-NTRK3 gene, some advanced cases may be co-driven by other mutated genes, so it is necessary to accumulate more evidence and find more therapeutic targets.
In conclusion, our study demonstrates the genomic characteristics of a group of SBCs with differences in immunophenotype and biological behavior. In addition to ETV6-NTRK3 gene fusion, TERT promoter region mutation may be another factor driving tumor progression. This provides insight into the genomic background and clinical treatment of SBCs.
Take home messages
The ETV6-NTRK3 fusion was the main driver of early tumorigenesis in most SBCs.
SBC with invasive biological behavior had more complex genomic variations including TERT promoter mutation.
TRKs may have therapeutic value in NTRK rearrangement SBCs.
Availability of data and materials
Data are available upon reasonable request to the authors.
References
Rakha EA R-FJ, Sasano H, Wu Y; WHO classifcation of tumours editorial board: Breast tumours. WHO classifcation of tumours series, 5th ed.; 2019.
Chen M, Pu T, Wei B, Bu H, Tang P, Zhang Z. Genomic landscape of secretory carcinoma of the breast with axillary lymph node metastasis. Pathol Res Pract. 2022;231:153790.
Din NU, Idrees R, Fatima S, Kayani N. Secretory carcinoma of breast: clinicopathologic study of 8 cases. Ann Diagn Pathol. 2013;17(1):54–7.
Castillo MD, Chibon F, Arnould L, Croce S, Ribeiro A, Perot G, et al. Secretory Breast Carcinoma: A Histopathologic and Genomic Spectrum Characterized by a Joint Specific ETV6-NTRK3 Gene Fusion. Am J Surg Pathol. 2015;39(11):1458–67.
Krings G, Joseph NM, Bean GR, Solomon D, Onodera C, alevich E, et al. Genomic profiling of breast secretory carcinomas reveals distinct genetics from other breast cancers and similarity to mammary analog secretory carcinomas. Mod Pathol. 2017;30(8):1086–99.
Tognon C, Knezevich SR, Huntsman D, Roskelley CD, Melnyk N, Mathers JA, et al. Expression of the ETV6-NTRK3 gene fusion as a primary event in human secretory breast carcinoma. Cancer Cell. 2002;2(5):367–76.
Lae M, Freneaux P, Sastre-Garau X, Chouchane O, Sigal-Zafrani B, Vincent-Salomon A. Secretory breast carcinomas with ETV6-NTRK3 fusion gene belong to the basal-like carcinoma spectrum. Mod Pathol. 2009;22(2):291–8.
Yang Y, Wang Z, Pan G, Li S, Wu Y, Liu L. Pure secretory carcinoma in situ: a case report and literature review. Diagn Pathol. 2019;14(1):95.
Vasudev P, Onuma K. Secretory breast carcinoma: unique, triple-negative carcinoma with a favorable prognosis and characteristic molecular expression. Arch Pathol Lab Med. 2011;135(12):1606–10.
Suurmeijer AJ, Dickson BC, Swanson D, Zhang L, Sung YS, Huang HY, et al. The histologic spectrum of soft tissue spindle cell tumors with NTRK3 gene rearrangements. Genes Chromosomes Cancer. 2019;58(11):739–46.
Lambros MB, Tan DS, Jones RL, Vatcheva R, Savage K, Tamber N, et al. Genomic profile of a secretory breast cancer with an ETV6-NTRK3 duplication. J Clin Pathol. 2015;62(7):604–12.
Maund SL, Sokol ES, Ang Houle A, Ross JS, Wilson TR. NTRK gene fusions are detected in both secretory and non-secretory breast cancers. Pathol Int. 2022;72(3):187–92.
Jin MS, Lee H, Woo J, Choi S, Do MS, Kim K, et al. Integrated Multi-Omic Analyses Support Distinguishing Secretory Carcinoma of the Breast from Basal-Like Triple-Negative Breast Cancer. Proteomics Clin Appl. 2018;12(5):e1700125.
Horowitz DP, Sharma CS, Connolly E, Gidea-Addeo D, Deutsch I. Secretory carcinoma of the breast: results from the survival, epidemiology and end results database. Breast. 2012;21(3):350–3.
Jacob JD, Hodge C, Franko J, Pezzi CM, Goldman CD, Klimberg VS. Rare breast cancer: 246 invasive secretory carcinomas from the National Cancer Data Base. J Surg Oncol. 2016;113(7):721–5.
Gong P, Xia C, Yang Y, Lei W, Yang W, Yu J, et al. Clinicopathologic profiling and oncologic outcomes of secretory carcinoma of the breast. Sci Rep. 2021;11(1):14738.
Herz H, Cooke B, Goldstein D. Metastatic secretory breast cancer. Non-responsiveness to chemotherapy: case report and review of the literature. Ann Oncol. 2000;11(10):1343–7.
Hoda RS, Brogi E, Pareja F, Nanjangud G, Murray MP, Weigelt B, et al. Secretory carcinoma of the breast: clinicopathologic profile of 14 cases emphasising distant metastatic potential. Histopathology. 2019;75(2):213–24.
Lian J, Wang LX, Guo JH, Bu P, Xi YF, Yun KM. Secretory breast carcinoma in a female adult with liver metastsis: a case report and literature review. Diagn Pathol. 2021;16(1):89.
Tang H, Zhong L, Jiang H, Zhang Y, Liang G, Chen G, et al. Secretory carcinoma of the breast with multiple distant metastases in the brain and unfavorable prognosis: a case report and literature review. Diagn Pathol. 2021;16(1):56.
Xu J, Weisman P. Dedifferentiated secretory breast carcinoma with fibrosarcomatous features harboring an ETV6-NTRK3 fusion in both components. Genes, Chromosomes and Cancer. 2020;60(6):447–51.
Shukla N, Roberts SS, Baki MO, Mushtaq Q, Goss PE, Park BH, et al. Successful Targeted Therapy of Refractory Pediatric ETV6-NTRK3 Fusion-Positive Secretory Breast Carcinoma. JCO Precis Oncol. 2017;2017:PO.17.00034.
Bell D, Ferrarotto R, Liang L, Goepfert RP, Li J, Ning J, et al. Pan-Trk immunohistochemistry reliably identifies ETV6-NTRK3 fusion in secretory carcinoma of the salivary gland. Virchows Arch. 2020;476(2):295–305.
Harrison BT, Fowler E, Krings G, Chen YY, Bean GR, Vincent-Salomon A, et al. Pan-TRK Immunohistochemistry: A Useful Diagnostic Adjunct For Secretory Carcinoma of the Breast. Am J Surg Pathol. 2019;2019(43):1693–700.
Forner D, Bullock M, Manders D, Wallace T, Chin CJ, Johnson LB, et al. Secretory carcinoma: the eastern Canadian experience and literature review. J Otolaryngol Head Neck Surg. 2018;47(1):69.
Banerjee N, Banerjee D, Choudhary N. Secretory carcinoma of the breast, commonly exhibits the features of low grade, triple negative breast carcinoma- A Case report with updated review of literature. Autops Case Rep. 2021;11:e2020227.
Osako T, Takeuchi K, Horii R, Iwase T, Akiyama F. Secretory carcinoma of the breast and its histopathological mimics: value of markers for differential diagnosis. Histopathology. 2013;63(4):509–19.
Li D, Xiao X, Yang W, Shui R, Tu X, Lu H, et al. Secretory breast carcinoma: a clinicopathological and immunophenotypic study of 15 cases with a review of the literature. Mod Pathol. 2012;25(4):567–75.
Weiss LM, Funari VA. NTRK fusions and Trk proteins: what are they and how to test for them. Hum Pathol. 2021;112:59–69.
Wu S, Shi X, Ren X, Li K, Pang J, Liang Z. Evaluation of NTRK Gene Fusion by Five Different Platforms in Triple-Negative Breast Carcinoma. Front Mol Biosci. 2021;8:654387.
Ghali RM, Al-Mutawa MA, Ebrahim BH, Jrah HH, Zaied S, Bhiri H, et al. Progesterone Receptor (PGR) Gene Variants Associated with Breast Cancer and Associated Features: a Case-Control Study. Pathol Oncol Res. 2020;26(1):141–7.
Pooley KA, Healey CS, Smith PL, Pharoah PD, Thompson D, Tee L, et al. Association of the progesterone receptor gene with breast cancer risk: a single-nucleotide polymorphism tagging approach. Cancer Epidemiol Biomarkers Prev. 2006;15(4):675–82.
Silva EM, Selenica P, Vahdatinia M, Pareja F, Paula ADC, Ferrando L, et al. TERT promoter hotspot mutations and gene amplification in metaplastic breast cancer. NPJ Breast Cancer. 2021;7(1):43.
Shimoi T, Yoshida M, Kitamura Y, Yoshino T, Kawachi A, Shimomura A, et al. TERT promoter hotspot mutations in breast cancer. Breast Cancer. 2018;25(3):292–6.
Bojesen SE, Pooley KA, Johnatty SE, Beesley J, Michailidou K, Tyrer JP, et al. Multiple independent variants at the TERT locus are associated with telomere length and risks of breast and ovarian cancer. Nat Genet. 2013;45(4):371–84.
Gay-Bellile M, Véronèse L, Combes P, Eymard-Pierre E, Kwiatkowski F, Dauplat MM,et al. TERT promoter status and gene copy number gains: effect on TERT expression and association with prognosis in breast cancer. Oncotarget. 2017;8(44):77540–51.
Murofushi Y, Nagano S, Kamizono J, Takahashi T, Fujiwara H, Komiya S, et al. Cell cycle-specific changes in hTERT promoter activity in normal and cancerous cells in adenoviral gene therapy: a promising implication of telomerase-dependent targeted cancer gene therapy. Int J Oncol. 2006;29(3):681–8.
Jafri MA, Ansari SA, Alqahtani MH, Shay JW. Roles of telomeres and telomerase in cancer, and advances in telomerase-targeted therapies. Genome Med. 2016;8(1):69.
Razavi P, Chang MT, Xu G, Bandlamudi C, Ross DS, Vasan N, et al. The Genomic Landscape of Endocrine-Resistant Advanced Breast Cancers. Cancer Cell. 2018;34(3):427–38.
Chen H, Chong W, Wu Q, Yao Y, Mao M, Wang X. Association of LRP1B Mutation With Tumor Mutation Burden and Outcomes in Melanoma and Non-small Cell Lung Cancer Patients Treated With Immune Check-Point Blockades. Front Immunol. 2019;10:1113.
Brown LC, Tucker MD, Sedhom R, Schwartz EB, Zhu J, Kao C, et al. LRP1B mutations are associated with favorable outcomes to immune checkpoint inhibitors across multiple cancer types. J Immunother Cancer. 2021;9(3):e001792.
Tu S, Teng YC, Yuan C, Wu YT, Chan MY, Cheng AN, et al. The ARID domain of the H3K4 demethylase RBP2 binds to a DNA CCGCCC motif. Nat Struct Mol Biol. 2008;15(4):419–21.
Wang GG, Song J, Wang Z, Dormann HL, Casadio F, Li H, et al. Haematopoietic malignancies caused by dysregulation of a chromatin-binding PHD finger. Nature. 2009;459(7248):847–51.
Li S, He J, Liao X, He Y, Chen R, Chen J, et al. Fbxo22 inhibits metastasis in triple-negative breast cancer through ubiquitin modification of KDM5A and regulation of H3K4me3 demethylation. Cell Biol Toxicol. 2022.
Lassen U. How I treat NTRK gene fusion-positive cancers. ESMO Open. 2019;4(Suppl 2):e000612.
Funding
Supported by grants from the Changzhou Science and Technology Project (QN202114), a project funded by Changzhou Health Commission.
Author information
Authors and Affiliations
Contributions
TC and TL conceived and designed the study. TL and XD performed analysis and interpretation of the data and wrote the manuscript. YP, HW, YY and TC contributed to breast cancer database administration. All authors were involved in providing study data, and commenting on the manuscript. All authors approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
In accordance with the institutional ethics guidelines, under permission from Ethics Committee of the Third Affiliated Hospital of Soochow University Institutional Review Board (ID: 2020-41).
Consent for publication
Not applicable.
Competing interests
None declared. Patient consent for publication. Not required.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Lei, T., Yang, Y., Shi, Y. et al. Clinicopathological features and genomic profiles of a group of secretory breast carcinomas in which progressive cases have more complex genomic features. Diagn Pathol 17, 101 (2022). https://doi.org/10.1186/s13000-022-01284-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13000-022-01284-7