Abstract
Background
Cytomegalovirus (CMV) has been recognized as one of the frequently occurring opportunistic infections (OIs) reported in the patients having human immunodeficiency virus/acquired immunodeficiency syndrome (HIV/AIDS). In addition, it has been identified as the factor leading to gastrointestinal (GI) tract disorder among HIV/AIDS population. CMV exhibits broad cell tropism in different organs. This study evaluated the CMV cell tropism and clinicopathological characteristics of CMV infection in the different GI regions in HIV/AIDS cases.
Methods
Using nucleic acid in situ hybridization (ISH), CMV was detected in the gastrointestinal mucosal biopsy samples. The paraffin-embedded samples were stained with hematoxylin and eosin (HE) and immunohistochemistry (IHC), respectively.
Results
A total of 32 HIV/AIDS patients were enrolled in this study. Fourteen of these patients underwent gastroscopy, while the remaining eighteen received colonoscopy. CMV-infected cells were observed at 46 GI sites. Among them, the colon was the region with the highest susceptibility to GI CMV infection (n = 12, 26.1%). The CMV giant cell inclusion bodies were detected in epithelial cells and mesenchymal cells, including histiocytes, smooth muscle cells, fibroblasts, and endothelial cells. In the duodenum, there were markedly more positive epithelial cells than mesenchymal cells (p = 0.033). In contrast, in the esophagus (p = 0.030), cardia (p = 0.003), rectum (p = 0.019), colon (p < 0.001), and cecum (p < 0.001), there were notably less positive epithelial cells than mesenchymal cells. The expression levels of PDGFRα and Nrp2 in the mesenchymal cells were higher than the epithelial cells in cardia, cecum, colon, sigmoid, and rectum, especially in the areas with ulcers. However, Nrp2 in the epithelial cells was higher than that in the duodenum. Moreover, the positive CMV DNA in peripheral blood was related to the CMV-positive cell count, as well as the ulceration in GI tract (p = 0.035 and 0.036, respectively).
Conclusions
The colon has been identified as the GI site with the highest susceptibility to CMV infection. There are different CMV-infected cells in the different sites of the GI that relate to the expression level of PDGFRα and Nrp2. CMV DNA positive in the blood is related to the positive CMV cell count, as well as ulceration in the GI tract.
Similar content being viewed by others
Background
CMV is among the most common pathogen-induced opportunistic infections detected in patients with infections resulting from the human immunodeficiency virus/acquired immunodeficiency syndrome (HIV/AIDS) [1]. Among such cases, gastrointestinal (GI) tract is among those most susceptible organs to CMV infection. GI manifestations take up about 10% CMV disorders among AIDS cases [2]. CMV infection may be detected in any region of the GI tract, from the mouth to the rectum [3]. Typically, endoscopy, together with mucosal biopsy, is most frequently used for diagnosis, and CMV colitis is confirmed via pathology through identifying the virus-induced cytopathic effects on biopsy tissue. CMV exhibits a broad cell tropism in different organs. The cells, most frequently identified as permissive to CMV, include epithelial cells, smooth muscle cells, endothelial cells, and fibroblasts. Over the years, many different cell surface proteins and molecules have been reported to function as CMV entry receptors, especially platelet-derived growth factor receptor alpha (PDGFRα) and Neuropilin2 (Nrp2), they mediated CMV into fibroblasts and endothelial/epithelial cells, respectively [4]. CMV tropism may be related to the expression of these cell surface receptors. The cell tropism and clinicopathological features for GI CMV infection have been rarely investigated in the literature. Therefore, this work was carried out aiming to assess CMV cell tropism in GI tract, and the pathological features as well as a clinicopathological correlation for CMV disorder were also evaluated.
Materials and methods
Patients
This study enrolled altogether 32 HIV/AIDS patients with GI CMV infection from Beijing Ditan Hospital from January 2010 to January 2020. All patients enrolled in this study underwent gastroscopy or colonoscopy to evaluate the GI symptoms, including abdominal pain, diarrhea, and hemafecia. Clinical data of all cases were acquired based on patient charts using the electronic medical record system in our center. Those factors extracted included age of patient, gender, serum CD4+ T cells, CD8+ T cells, leukocyte, erythrocyte, hemoglobin, platelet, HIV viral loads, CMV viral loads, and follow-up biopsies. Written informed consent was obtained from the participants by physicians. The study protocol was approved by the Ethics Committee of Beijing Ditan Hospital, Capital Medical University. All procedures performed in studies involving human participants were in accordance with the ethical standards and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Acquisition of mucosal tissue specimens from GI tract
As part of the procedure, mucosal tissues were sampled from inflammatory foci in the esophagus, cardia, gastric antrum, gastric body, duodenum, cecum, colon, sigmoid and rectum, as well as from regions that appeared to be unaffected. The extracted tissues were then fixed in 10% formaldehyde solution. Subsequently, serial sections (4 μm) of tissues fixed in formalin and embedded within paraffin were stained with HE, acid-fast, hexamine silver, periodic acid-Schiff and IHC. Nucleic acid ISH was adopted to prepare samples for detection of CMV.
EnVision two-step method for immunohistochemical staining
Embedded sections were deparaffinized with xylene followed by an alcohol gradient and water rinses and incubated with 0.3% hydrogen peroxide for 10 min at room temperature to eliminate endogenous peroxidase activity. After antigen retrieval under high pressure with a citrate buffer, individual slides were incubated at 4 °C overnight with mouse anti-human PDGFRα (Beijing Zhongshan Biotechnology, Lot:ZA0377, 1:40 dilution), mouse anti-human Nrp2 (Abcam Company, Lot:GR3249327–7, 1:200 dilution), Slides were then washed three times with phosphate-buffered saline (PBS), followed by horseradish peroxidase-labeled secondary antibodies (37 °C for 30 min). Slides were then washed and developed with DAB, hematoxylin counterstained, and mounted. PBS diluent was used in place of individual primary antibodies as negative controls.
Nucleic acid ISH of CMV
Nucleic acid ISH using the digoxigenin-labeled probes was conducted in accordance with the manufacturer protocols. CMV probe was diluted at 1:50–1:100, which generated a strong brown-to-yellow positive signal. The hybridization kit equipped with the digoxigenin probe for detecting CMV, as well as the nitroblue tetrazolium (NBT)/5-bromo-4-chloro-3-indolyl phosphate (BCIP) assay kit, was provided by Leica Biosystems (CMV Probe:REF:PB0614, Lot:62163).
Semi-quantitative evaluation of CMV DNA in mucosal tissues from GI tract
Ten regions of the lamina propria were selected at random for microscopic evaluation. Under high magnification (Nikon 80i, × 400), a grid counter was used to count the CMV-positive cells. The mean positive cell count in each high power field (HPF) was calculated, and then these cases were divided into three groups, including positive cells< 5 /HPF, 5–10/HPF, > 10 /HPF.
Statistical analysis
SPSS 20.0 (IBM statistics, SPSS, Chicago, IL) was adopted for all statistical tests. Fisher’s exact test and Student’s t-test were employed to evaluate the differences. The chi-square test was utilized to analyze those categorical variables. For continuous values, they were expressed in the manner of mean ± standard deviation (SD). A difference of p < 0.05 indicated statistical significance.
Results
Features of patients
29 out of the 32 patients with HIV/AIDS enrolled in this study were males, while 3 were females, with age ranging 25 to 58 years (average, 38.0 ± 10.0 years). In these patients, 14 underwent gastroscopy to check the upper GI tract, whereas the rest 18 received colonoscopy to examine the lower GI tract. CMV infection was confirmed by biopsy and ISH in all patients, but CMV DNA in peripheral blood was detected only in 18 patients, including 7 undergoing gastroscopy and 11 receiving colonoscopy. The difference was not statistically significant between these two groups (p = 0.530). In addition, CD4 cell count of all patients dropped to below 200 cells/μL, and 27 patients had the CD4 cell count of < 50 cells/μL. Patient demographic characteristics and other laboratory measurements, including serum CD4+ T cells, CD8+ T cells, leukocyte, erythrocyte, hemoglobin, platelet, and HIV viral loads, displayed no significant difference between patients receiving gastroscopy and those undergoing colonoscopy. Data are presented in Table 1.
Pathological findings and CMV cell tropism in mucosal biopsies from HIV/AIDS patients with CMV infection
In these 32 patients, the CMV-infected cells were observed at 46 sites of the GI tract. Colon was the GI site exhibiting the highest susceptibility to CMV disorder (n = 12, 26.1%). Meanwhile, the stomach (n = 10, 21.7%), including the cardia (n = 3, 6.5%), antrum (n = 5, 10.9%) and gastric body (n = 2, 4.3%), was the second most frequently affected site, followed by esophagus (n = 7, 15.2%), cecum (n = 7, 15.2%), duodenum (n = 4, 8.7%), sigmoid (n = 3, 6.5%) and rectum (n = 3, 6.5%) (Table 2).
Characteristics of the biopsied intestinal mucosal samples included edema, congestion, lymphocytosis, and rare lymphoid aggregates. 27 of the 32 enrolled cases (84.4%) developed obvious active (neutrophilic) as well as chronic (lymphoplasmacytic) inflammation; besides, some areas of ulceration were detected in 14 cases. Only 5 cases showed mild inflammation. HE staining and nucleic acid ISH for CMV revealed that giant cell inclusion bodies were observed in epithelial cells and mesenchymal cells, including histiocytes, smooth muscle cells, fibroblasts, and endothelial cells. Those inclusion bodies were round or oval, and were surrounded by a distinct air halo, a characteristic also known as the “owl’s eye.” Other CMV inclusions were characterized by the affluent rough eosinophilic inclusions of cytoplasm inside those enlarged cells in the absence of clear inclusions of nucleus (Fig.1a).
CMV cell tropism in gastrointestinal tract from patients with HIV/AIDS. (A) CMV viral inclusions showed an ‘eagle eye’ appearance in some virus-infected cells, other CMV inclusions were characterized by abundant coarse eosinophilic cytoplasmic inclusions within enlarged cells. HE, original magnification 400×. (B) CMV mostly infected epithelial cells in duodenum. HE, original magnification 200×. (C) CMV mostly infected mesenchymal cells in colon (brown). ISH, original magnification 200×. (D) Epithelial cells and mesenchymal cells can be all infected by CMV in gastric antrum. ISH, original magnification 200 ×
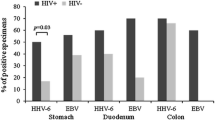
In the duodenum, CMV most frequently infected the epithelial cells, and there were significantly more positive epithelial cells than mesenchymal cells(p = 0.033) (Fig.1b). In the esophagus (p = 0.030), cardia (p = 0.003), rectum (p = 0.019), colon (p<0.001), and cecum (p<0.001), there were markedly less positive epithelial cells than mesenchymal cells (Fig.1c). In the sigmoid, no epithelial cell was positive. In the gastric antrum and gastric body, both epithelial cells and mesenchymal cells were infected by CMV (Fig.1d), and the difference between these two types of cells was not statistically significant (Table 2).
Expression of PDGFRα and Nrp2 in the different sites of the GI tract
Immunoreactive PDGFRα and Nrp2 were detected in the cell membranes and within the cytoplasm of epithelial cells and mesenchymal cells, including histiocytes, fibroblasts, smooth muscle cells, and endothelial cells. However, the immunohistochemical expression intensity and cell type were distinct in the different sites of the GI tract. The expression levels of PDGFRα and Nrp2 in the mesenchymal cells were higher than that in the epithelial cells in cardia, cecum, colon, sigmoid, and rectum, especially in areas with ulcers (Fig.2a and Fig.2b). But Nrp2 in epithelial cells was higher in the duodenum (Fig.2c). In the gastric antrum and gastric body, both epithelial cells and mesenchymal cells expressed PDGFRα and Nrp2 similarly (Fig.2d). These expression characteristics were roughly consistent with the CMV cell tropism in the GI tract.
Expression of PDGFRα and Nrp2 in different sites of the gastrointestinal tract in patients with HIV/AIDS and CMV. (A) Expression level of PDGFRα on mesenchymal cells was higher than epithelial cells in colon. IHC, original magnification 200×. (B) Expression of Nrp2 on hyperplastic mesenchymal cells in areas with ulcers in colon. IHC, original magnification 200×. (C) Expression level of Nrp2 on epithelial cells was higher than mesenchymal cells in duodenum. IHC, original magnification 200×. (D) Expression level of PDGFRα on epithelial cells and mesenchymal cells was similarly in the gastric antrum. IHC, original magnification 200 ×
Clinicopathological correlations of CMV infection in GI tract
According to the mean CMV-positive cell count in every HPF, we divided the 32 enrolled cases into 3 groups: positive cells<5 /HPF, 5–10/HPF, >10 /HPF. Among the 8 cases with CMV positive cells< 5 /HPF, the blood CMV DNA was detectable only within 2 patients, whereas in the 12 cases with positive cells> 10 /HPF, blood CMV DNA was detectable within 10 patients. In the 14 patients with ulceration in GI tract, 11 were CMV DNA positive in blood; by contrast, in the 18 cases with no ulceration, only 7 were CMV DNA positive in blood. Upon Fisher’s exact test, CMV DNA positive in blood was related to the CMV-positive cell count, as well as the ulceration in GI tract (p = 0.035 and 0.036, respectively) (Table 3).
Discussion
CMV is a double-stranded DNA virus, which is one of the β-herpesvirus family members. The virus is widespread among the general population, and the CMV seroprevalence may be > 60% [5]. CMV infection can be initiated through close contact, intravenous injection, blood transfusion, sexual intercourse, placental transmission, or organ transplantation. CMV disorder is an opportunistic infection that may threaten human life, and it is frequently seen among HIV/AIDS patients. Typically, GI CMV infection is one of the most common clinical manifestations, which represents a severe complication that affects HIV/AIDS patients; besides, it is the primary factor leading to mortality and morbidity [6]. In this article, we discussed the CMV cell tropism in GI tract, pathological features and clinicopathological correlations of GI CMV disorder.
Among cases infected with HIV, the susceptibility to symptomatic disorder is related to the immunosuppression degree, which elevates markedly at the case of number of CD4 cells < 200 cells/μL. According to one study, CMV infection is remarkably prevalent in HIV-infected patients who have the number of CD4 cells < 50 cells/μL, compared with those having the number of CD4 cells> 50 cells/μL [7]. Similar results were obtained in this study, the CD4 cell number in all patients dropped to < 200 cells/μL, among them, 27 cases had that of < 50 cells/μL.
CMV can affect any GI site, among which, colon is the most susceptible site. Among GI CMV patients, colon involvement has been commonly detected, which accounts for 94% patients [8, 9]. Colon was also the most commonly affected site in our results, which accounted for 26.1%. Stomach was most susceptible to CMV infection in upper GI tract, including cardia, antrum and gastric body in 10 patients. Similar results were also noted by Bonetti et al. [10]. But another study finds that, esophagus ranks the second place in terms of its susceptibility to CMV infection in the GI tract, which is only second to colon [11]. CMV-induced esophagitis was found in 7 cases in our study, only second to the stomach. CMV duodenitis is exceedingly rare, which is found in only 1 out of 30 cases with duodenum involvement, as reported in one study [10]. There were 4 cases with CMV duodenitis identified in our study. Patient demographic characteristics and other laboratory measurements, including serum CD4+ T cells, CD8+ T cells, leukocyte, erythrocyte, hemoglobin, platelet, and HIV viral loads, were not significantly different in CMV infection between the upper and lower GI tracts.
Several methods, including viral culture, serological tests, polymerase chain reaction (PCR), and shell viral assay, are proposed to diagnose GI CMV infection. However, virologic and serologic tests may be restricted in diagnosing the GI-restricted CMV disorder [12]. The primary process for diagnosis is endoscopy for identifying mucosal lesion, as well as tissue biopsy to confirm the infection. CMV infection is histopathologically diagnosed according to those virus-infected cells in the biopsied tissues (namely, the viral cytopathic effect). Typically, these virus-infected cells show the characteristic intracellular inclusions, with an ‘owl’s eye’ appearance on slides subjected to routine HE staining, or IHC detection of CMV viral inclusions [13, 14]. Histological findings have been shown with a sensitivity of 93% and a specificity of 100% in confirming the diagnosis [15]. However, it is impossible that all viral inclusions are identified by HE staining alone, because the complex inflammatory background may mask the inclusions, or the “atypical” viral inclusion may be characterized by the affluent rough eosinophilic inclusions of cytoplasm in those enlarged cells with no distinct inclusions of nucleus, as seen in our cases. Furthermore, IHC may yield ambiguous results for various reasons, it is also not the approach with the highest sensitivity in CMV detection. It remains controversial about the necessity of the routine implementation of CMV IHC in biopsy with moderate-severe inflammation [16]. PCR is a sensitive, specific, and rapid molecular tool that may be helpful to aid in early diagnosis of CMV infection on equivocal or clinically highly suspicious small GI biopsies [17], but it cannot show the position of positive cells in situ. Therefore, ISH was applied in this study to detect CMV in GI tract.
Notably, the significant active inflammation, especially with ulceration, stands for a vital clue to suspect GI CMV infection. 27 of our enrolled cases showed significant inflammation, and 14 had ulceration. Nonetheless, CMV infection can not be completely excluded when there is no distinct inflammation. For instance, the inflammation was not significant in 5 of our cases. The less inflammation background may be related to the Highly Active Antiretroviral Therapy (HAART) after CMV infection, or the absence of inflammation may represent a sampling error, specimens were taken from near the lesion [6]. Ulceration was detected in 14 cases in our study, with the deepening of ulcer, vascular erosion might result in substantial bloody diarrhea [18]. The progression of CMV disorder is associated with ulcer formation in the GI tract [13]. We demonstrated that, CMV DNA positive in blood was correlated with ulceration in the GI tract. In addition, if ulcers were observed in the GI tract, the CMV DNA in blood was more likely to be positive.
CMV demonstrates broad tropism in the GI tract. The CMV-infected cell types involve epithelial cells and mesenchymal cells, including histiocytes, endothelial cells fibroblasts and smooth muscle cells. However, we found that, the main types of CMV-infected cells were different at the diverse locations of GI tract. In the duodenum, CMV most frequently infects epithelial cells, whereas mesenchymal cells are the primary target in the esophagus, cardia, cecum, colon and rectum. In the stomach, both epithelial cells and mesenchymal cells can be infected by CMV. The cell tropism may relate to the viral entry machinery. Genetic analysis showed that CMV cell tropism require products of viral genes UL128L, together with gH/gL, forming the gH/gL/pUL128L pentamer complex (PC) that is required for the infection of epithelial or endothelial cells, whereas gH/gL and gO form the gH/gL/gOtrimer complex (TC), required for the infection of both cell types [19]. In 2016, a receptor for the TC that mediates entry into fibroblasts was identified as PDGFRα [20], while in 2018, a receptor for the PC that mediates entry into endothelial/epithelial cells was identified as neuropilin2 (Nrp2) [21]. Therefore, we detected the two receptors in different cell types in GI tract. We found that PDGFRα and Nrp2 all expressed in the epithelial cells and mesenchymal cells, and the expression levels of PDGFRα and Nrp2 in the mesenchymal cells were higher than those in the epithelial cells in cardia, cecum, colon, sigmoid, and rectum, especially in areas with ulcers. These may be the reason for markedly more positive mesenchymal cells than epithelial cells in these sites. The results of some studies were similar to ours. A flow cytometry analysis showed that an Nrp2 receptor was expressed on the cell surface of both epithelial/endothelial cells and fibroblasts. Thus, fibroblasts expressed similar levels of PDGFRα and Nrp2, which made the fibroblasts more susceptible to CMV infection compared to the epithelial cells [4].
Those affected cells become larger, which can comprise the cytoplasmic and nuclear inclusions. The nuclear inclusions are amphophilic, which are encompassed via a rarified chromatin zone, leading to the appearance of “owl’s eye”, while the cytoplasmic inclusions are eosinophilic and granule-like. Because the owl’s eye sign is not often seen in daily clinical practice, ISH serves as the most efficient approach when HE staining is unable to identify the inclusions, particularly when CMV infection is clinically suspected or the endoscopic results of HIV/AIDS cases are abnormal [6].
Peripheral blood CMV DNA test at molecular level is extensively utilized for monitoring those cases susceptible to infection [22]. According to some studies, the viral load of CMV shows poor association with CMV infection burden within GI tissues [23, 24]. Meanwhile, it is indicated in another study that, cell number found in the biopsied GI tissues is related to the systemic CMV viremia [16]. In our study, we also demonstrated that, positive CMV DNA in blood was related to the CMV-positive cell number within the GI tract. Therefore, we speculated that, the lower CMV-infected cell number led to the higher probabilities of negative blood CMV DNA and as a “bystander”; in addition, a higher number of CMV-infected cells resulted in the higher chances of positive blood CMV DNA and a systemic disorder that induces pathological changes, like ulceration or serious inflammation observed in the biopsied tissues. Nonetheless, it’s not uncommon to have isolated GI CMV disease without detectable CMV DNA, as observed among 14 of our cases.
Conclusions
In conclusion, this study is carried out mainly to explore the CMV cell tropism and correlations among clinicopathological features of GI CMV infection. The results suggest that different CMV-infected cells in the different sites of the GI relating to the expression level of PDGFRα and Nrp2 as well as the vital part of pathological assessment in diagnosing and managing CMV among HIV/AIDS cases. Endoscopy is recommended to obtain a tissue biopsy for HE staining and ISH among HIV/AIDS patients with GI tract symptoms, so as to confirm the CMV infection.
Availability of data and materials
The datasets used and/or analyzed during the current study available from the corresponding author on reasonable request.
Abbreviations
- CMV:
-
Cytomegalovirus
- HIV:
-
Human Immunodeficiency Virus
- AIDS:
-
Acquired Immunodeficiency Syndrome
- GI:
-
gastrointestinal
- IHC:
-
immunohistochemical
- HE:
-
haematoxylin and eosin
- ISH:
-
in situ hybridization
- PDGFRα:
-
platelet-derived growth factor receptor alpha
- Nrp2:
-
Neuropilin2
References
Christensen-Quick A, Vanpouille C, Lisco A, Gianella S. Cytomegalovirus and HIV persistence: pouring gas on the fire. AIDS Res Hum Retrovir. 2017;33(S1):S23–30. https://doi.org/10.1089/aid.2017.0145.
Springer KL, Weinberg A. Cytomegalovirus infection in the era of HAART: fewer reactivations and more immunity. J Antimicrob Chemother. 2004;54(3):582–6. https://doi.org/10.1093/jac/dkh396.
Kalkan IH, Dağli U. What is the most accurate method for the diagnosis of cytomegalovirus (CMV) enteritis or colitis. Turk J Gastroenterol. 2010;21:83–6.
Gerna G, Kabanova A, Lilleri D. Human cytomegalovirus cell tropism and host cell receptors. Vaccines (Basel). 2019;7(3):E70. https://doi.org/10.3390/vaccines7030070.
Staras SA, Dollard SC, Radford KW, Flanders WD, Pass RF, Cannon MJ. Seroprevalence of cytomegalovirus infection in the United States. Clin Infect Dis. 2006;43(9):1143–51. https://doi.org/10.1086/508173.
Guo L, DeRoche TC, Salih ZT, Qasem SA. Routine hematoxylin and eosin stain is specific for the diagnosis of cytomegalovirus Infectionin gastrointestinal biopsy specimens. Int J Surg Pathol. 2018;26(6):500–6. https://doi.org/10.1177/1066896918761601.
Lucas SB, Hounnou A, Peacock C, Beaumel A, Djomand G, N'Gbichi JM, et al. The mortality and pathology of HIV infection in a west African city. AIDS. 1993;7(12):1569–79. https://doi.org/10.1097/00002030-199312000-00005.
Lee CY, Chen YH, Lu PL. Reactivated cytomegalovirus proctitis in an immunocompetent patient presenting as nosocomial diarrhea: a case report and literature review. BMC Infect Dis. 2017;17(1):113. https://doi.org/10.1186/s12879-017-2218-y.
Fakhreddine AY, Frenette CT, Konijeti GG. A practical review of cytomegalovirus in gastroenterology and hepatology. Gastroenterol Res Pract. 2019;6156581:1–11. https://doi.org/10.1155/2019/6156581.
Reggiani Bonetti L, Losi L, Di Gregorio C, Bertani A, Merighi A, Bettelli S, et al. Cytomegalovirus infection of the upper gastrointestinal tract: a clinical and pathological study of 30 cases. Scand J Gastroenterol. 2011;46(10):1228–35. https://doi.org/10.3109/00365521.2011.594083.
Wang HW, Kuo CJ, Lin WR, Hsu CM, Ho YP, Lin CJ, et al. The clinical characteristics and manifestations of cytomegalovirus esophagitis. Dis Esophagus. 2016;29(4):392–9. https://doi.org/10.1111/dote.12340.
Shen L, Youssef D, Abu-Abed S, Malhotra SK, Atkinson K, Vikis E, et al. Cytomegalovirus duodenitis associated with life-threatening duodenal hemorrhage in an immunocompetent patient: a case report. Int J Surg Case Rep. 2017;33:102–6. https://doi.org/10.1016/j.ijscr.2017.02.029.
Case R Jr, Stoner P, Myrick S, Zimmermann E. Solitary ascending colon ulcer diagnosed as gastrointestinal CMV disease. BMJ Case Rep. 2019;12(2):e226355. https://doi.org/10.1136/bcr-2018-226355.
Lee H, Westerhoff M, Shen B, Liu X. Clinical aspects of idiopathic inflammatory bowel disease: a review for pathologists. Arch Pathol Lab Med. 2016;140(5):413–28. https://doi.org/10.5858/arpa.2015-0305-RA.
Kandiel A, Lashner B. Cytomegalovirus colitis complicating inflammatory bowel disease. Am J Gastroenterol. 2006;101(12):2857–65. https://doi.org/10.1111/j.1572-0241.2006.00869.x.
Sager K, Alam S, Bond A, Chinnappan L, Probert CS. Review article: cytomegalovirus and inflammatory bowel disease. Aliment Pharmacol Ther. 2015;41(8):725–33. https://doi.org/10.1111/apt.13124.
McCoy M, Post K, Sen J, Chang H, Zhao Z, Fan R, et al. qPCR increases sensitivity to detect cytomegalovirus in paraffin-embedded, formalin-fixed tissue of gastrointestinal biopsies. Hum Pathol. 2013;44(10):2075–80.
Liao X, Reed SL, Lin GY. Immunostaining detection of cytomegalovirus in gastrointestinal biopsies: Clinicopathological correlation at a large academic health system. Gastroenterology Res. 2016;9(6):92–8. https://doi.org/10.14740/gr725e.
Nguyen CC, Kamil JP. Pathogen at the gates: human cytomegalovirus entry and cell tropism. Viruses. 2018;10(12):E704. https://doi.org/10.3390/v10120704.
Kabanova A, Marcandalli J, Zhou T, Bianchi S, Baxa U, Tsybovsky Y, et al. Platelet-derived growth factor-αreceptor for human cytomegalovirus gHgLgO trimer. Nat Microbiol. 2016;1(8):16082. https://doi.org/10.1038/nmicrobiol.2016.82.
Martinez-Martin N, Marcandalli J, Huang CS, Arthur CP, Perotti M, Foglierini M, et al. An unbiased screen for human cytomegalovirus identifies neuropilin-2 as a central viral receptor. Cell. 2018;174(5):1158–71. https://doi.org/10.1016/j.cell.2018.06.028.
Drouet E, Michelson S, Denoyel G, Colimon C. Polymerase chain reaction detection of human cytomegalovirus in over 2000 blood specimens correlated with virus isolation and related to urinary virus excretion. J Virol Methods. 1993;45(3):259–76. https://doi.org/10.1016/0166-0934(93)90112-5.
Moreira RK, Norton C, Flavia Nunes R, Cohen C, Nolte F. Histopathologically documented gastrointestinal cytomegalovirus infection in immunosuppressed patients: clinicopathologic analysis with serum quantitative PCR correlation. Int J Med Med Sci. 2010;2:49–59.
Yan Z, Wang L, Dennis J, Doern C, Baker J, Park JY. Clinical significance of isolated cytomegalovirus-infected gastrointestinal cells. Int J Surg Pathol. 2014;22(6):492–8. https://doi.org/10.1177/1066896914537681.
Acknowledgements
Not applicable.
Funding
This work was supported by Beijing Municipal Administration of Hospitals’. Ascent Plan (DFL20191802) and Beijing Municipal Administration of Hospitals. Clinical Medicine Development of Special Funding Support (ZYLX202126).
Author information
Authors and Affiliations
Contributions
LS and JC designed the research study and wrote the manuscript. LZ, ZM, XC, ML and LQ performed the lab work and data collection. KY and XZ performed analysis of data. PL,HZ and JX conducted the clinical work. PW edited the manuscript. All the authors have read and approved the final version of this manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The study protocol was approved by Ethics Committee of Beijing Ditan Hospital, Capital Medical University.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Sun, L., Chen, Jm., Yang, K. et al. Cytomegalovirus cell tropism and clinicopathological characteristics in gastrointestinal tract of patients with HIV/AIDS. Diagn Pathol 17, 9 (2022). https://doi.org/10.1186/s13000-022-01193-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13000-022-01193-9