Abstract
Background
The Default Mode Network (DMN) is a central neural network, with recent evidence indicating that it is composed of functionally distinct sub-networks. Methylphenidate (MPH) administration has been shown before to modulate impulsive behavior, though it is not yet clear whether these effects relate to MPH-induced changes in DMN connectivity. To address this gap, we assessed the impact of MPH administration on functional connectivity patterns within and between distinct DMN sub-networks and tested putative relations to variability in sub-scales of impulsivity.
Methods
Fifty-five right-handed healthy adults underwent two resting-state functional MRI (rs-fMRI) scans, following acute administration of either MPH (20 mg) or placebo, via a randomized double-blind placebo-controlled design. Graph modularity analysis was implemented to fractionate the DMN into distinct sub-networks based on the impact of MPH (vs. placebo) on DMN connectivity patterns with other neural networks.
Results
MPH administration led to an overall decreased DMN connectivity, particularly with the auditory, cinguloopercular, and somatomotor networks, and increased connectivity with the parietomedial network. Graph analysis revealed that the DMN could be fractionated into two distinct sub-networks, with one exhibiting MPH-induced increased connectivity and the other decreased connectivity. Decreased connectivity of the DMN sub-network with the cinguloopercular network following MPH administration was associated with elevated impulsivity and non-planning impulsiveness.
Conclusion
Current findings highlight the intricate effects of MPH administration on DMN rs-fMRI connectivity, uncovering its opposing impact on distinct DMN sub-divisions. MPH-induced dynamics in DMN connectivity patterns with other neural networks may account for some of the effects of MPH administration on impulsive behavior.
Similar content being viewed by others
Introduction
The human brain is functionally organized into distinct regions that collaboratively form extensive, interconnected neural networks [1]. Resting-state functional MRI (rs-fMRI) has emerged as a pivotal tool for delineating these large-scale networks, both in their typical function and in response to various externally induced conditions. This technique capitalizes on the observation that functionally related yet spatially separated brain regions exhibit synchronized low-frequency fluctuations in their blood oxygen level-dependent (BOLD) signals, revealing intrinsic connectivity networks (ICNs) [2]. Central to these ICNs is the Default Mode Network (DMN), that is consistently identified as a key network in rs-fMRI studies [3]. Interestingly, recent evidence suggests that the DMN is not monolithic but rather encompasses multiple intertwined sub-networks, challenging the traditional view of the DMN as a singular entity. Indeed, studies have pointed on functional heterogeneity within the DMN, proposing that the DMN can be fractionated into at least two distinct sub-networks [4,5,6,7,8,9,10].
The importance of studying DMN rs-fMRI connectivity patterns, as well as all other ICNs, is indicated by the notion that these networks are associated with distinct neurocognitive functions [11]. In fact, the majority of established ICNs are labeled according to their assigned neurocognitive roles, such as for example the attention, visual, auditory and somatomotor networks [12, 13]. Furthermore, connectivity patterns within and between specific ICNs were found to be differentially affected by acute pharmacological manipulations [14], as well as to predict antidepressant treatment response [15]. Abnormal connectivity patterns in specific ICNs, including the DMN, have also been linked to psychiatric conditions [16,17,18]. Given this background, understanding the distributed effects of acute drug administration on DMN rs-fMRI connectivity patterns becomes crucial, as it may account for the differential behavioral effects of the drug across individuals.
Methylphenidate (MPH) is an indirect dopaminergic and noradrenergic agonist and is the first line treatment for attention deficit hyperactivity disorder (ADHD) [19]. Among ADHD patients, MPH administration has been shown to modulate rs-fMRI functional connectivity patterns in the DMN [20,21,22], as well as in additional neural networks [21, 23,24,25,26]. Interestingly however, the few studies that directly assessed the impact of acute MPH administration on rs-fMRI connectivity patterns among healthy cohorts yielded somewhat inconclusive results [27, 28], possibly because DMN fractionation into functionally distinct sub-networks was overlooked.
One of the pathways through which MPH may improve clinical status in ADHD is via its impact on impulsivity, yielding reduced impulsive behavior [29, 30]. We recently demonstrated that a similar effect is also observed in healthy adults following acute MPH administration [31]. Notably, multiple sub-scales of impulsivity are considered to rely on DMN and dorsolateral prefrontal cortex functionality and connectivity [31,32,33,34,35]. In support of that, previous studies associated variability in impulsive behavior with connectivity patterns of sub-regions within the DMN network, including the medial prefrontal cortex (mPFC), posterior cingulate cortex (PCC) and anterior cingulate cortex (ACC) [36,37,38,39,40,41,42]. Recently, impulsivity was also linked with age-dependent alterations of functional brain networks during resting-state [43]. Taken together, these findings raise the notion that MPH-induced dynamics in DMN connectivity patterns may account for the effects of MPH administration on impulsivity.
As far as we know, the effects of MPH administration on DMN functional connectivity have yet to be defined, particularly with respect to distinct DMN sub-networks. Nor has it been explored whether these effects relate to variability in impulsivity sub-scales. In order to address this gap, fifty-five healthy young adults completed two rs-fMRI scans, following acute administration of either MPH (20 mg) or placebo, in a randomized double-blind placebo-controlled design. Analysis focused on the impact of MPH (vs. placebo) on DMN functional connectivity with all other ICNs. Graph analysis was used to fractionate the DMN into distinct sub-networks. Analyses further assessed the potential association between the impact of MPH on DMN connectivity patterns and participants’ impulsivity scores. Following previous findings, we hypothesized that acute MPH administration would yield decreased functional connectivity of the DMN with other ICNs. We further hypothesized that MPH may have a differential effect on distinct sub-networks within the DMN, and that these patterns could potentially relate to variability in impulsivity scores.
Methods and materials
Participants
Fifty-seven right-handed young healthy adults (32 females) were recruited to the study using online and posted ads. Inclusion criteria included age between 18 and 40, normal or corrected to normal visual acuity and right-handedness. Exclusion criteria included past or present neurological, psychiatric, or developmental disorder, head injury, substance use, chronic medication (excluding contraceptives), pregnancy or nursing and MRI contraindications. Eligible participants provided written informed consent to a protocol approved by the ethics committees of the University of Haifa (approval #368/17) and Rambam Health Care Campus (approval #0539 − 16) and received monetary compensation for their participation. Two participants were excluded due to poor MRI data quality caused by excessive head motion, yielding a final sample size of 55 participants (32 F, mean age 26.58 ± 3.91).
Procedure
Screening procedures were employed using a combination of online questionnaires and two laboratory sessions held at the University of Haifa. The initial laboratory session involved obtaining informed consent from participants, followed by completion of the Hebrew version of the Edinburgh Handedness Inventory [44], a demographic questionnaire, and an MRI contraindication inventory. To exclude individuals with undiagnosed ADHD symptoms, participants also completed the Hebrew version of the Conners’ Adult ADHD Rating Scale [CAARS; [45]], a self-report questionnaire specifically designed to assess ADHD symptoms in adults. Consistent with established norms, participants scoring 65 or higher on the CAARS ADHD Index subscale were excluded from the study. Additionally, participants underwent clinical evaluation using the Hebrew version of the Mini-International Neuropsychiatric Interview [MINI; [46]], a brief structured interview used to diagnose Axis I psychiatric disorders. This evaluation aimed to exclude individuals with psychiatric or neurological disorders, including prior exposure to stimulant drugs or head injuries. The second session, occurring approximately 1–2 weeks later, involved the completion of the Barratt Impulsiveness Scale [BIS-11; [47]] questionnaire. Subsequently, participants were invited to take part in two neuroimaging sessions, conducted at the MRI institute of Rambam Health Care Campus. The average time interval between the two MRI sessions was 8 days (SD: 2 days). At the commencement of each session, the study’s neurologist conducted an electrocardiogram (ECG) and a pregnancy test. Afterward, participants received, via a double-blind, counterbalanced, within-subject design, a capsule containing either 20 mg of methylphenidate (MPH) or an indistinguishable placebo (PL) capsule. Heart rate and blood pressure were measured by the neurologist prior to drug administration, and ongoing monitoring of side effects was conducted throughout the sessions. Pharmacokinetic data suggest that plasma concentration of MPH reaches its peak approximately one hour after administration [48]. Accordingly, the MRI session began 45 min after drug administration to ensure peak drug blood concentration during the scan. The neuroimaging sessions involved an anatomical scan, completion of a delay discounting task [31] and a spatial attention task [49], and a resting state scan. During the resting-state scan participants were presented with a fixation cross and were instructed to lie with their eyes open.
Measures
Barratt impulsiveness scale (BIS-11) questionnaire
The BIS-11 is a 30-item self-report questionnaire that assesses impulsivity across three subscales: attentional or cognitive impulsivity, non-planning impulsiveness, and motor impulsiveness [47]. Participants rate each statement, reflecting behavioral and cognitive tendencies in various situations, on a scale ranging from 1 (“never/rarely”) to 4 (“always/almost always”). Higher scores indicate a greater propensity for impulsivity. Participants completed the Hebrew version of the BIS-11 [50].
MRI data acquisition
MRI data was acquired using a 3T GE scanner with an eight-channel high-resolution head coil, located at the MRI institute at Rambam Health Care Campus, Haifa, Israel. Functional MRI (fMRI) during the resting-state scan was carried out with a gradient echo-planar imaging (EPI) sequence of functional T2*-weighted images (TR/TE/flip angle: 2000/30/77; FOV: 240 mm; matrix size: 64 × 64) divided into 43 axial slices (voxel-size: 3mm3; gap: 0 mm) covering the whole cerebrum. The scan included 234 repetitions for a total duration of 7 min and 48 s. In addition, anatomical three-dimensional (3D) sequence spoiled gradient (SPGR) echo sequence was obtained at high-resolution 0.9-mm slice thickness (matrix: 256 × 256; flip angle: 12; FOV: 231 mm).
MRI data analyses
MRI data analyses were conducted using SPM12 software (http://www.fil.ion.ucl.ac.uk/spm/software/). Data pre-processing was conducted using the CONN toolbox [version 21.A; [51]], and involved co-registration of functional and anatomical images, segmentation using SPM tissue probability maps, nonlinear volume-based spatial normalization (based on forward deformations obtained during segmentation utilizing Montreal Neurological Institute [MNI] space), and spatial smoothing with a Gaussian filter (full width at half maximum: 6 mm). The Artifact Detection Tool (ART; http://web.mit.edu/swg/software.htm) was used in order to identify and exclude outlier time points in the global mean image time series (threshold: 3 standard deviations from the mean) and movement (threshold: 0.7 mm; measured as scan-to-scan movement, separately for translation and rotation) parameters. Following pre-processing, denoising procedures included regressing out signals from the segmented CSF, white matter, the six motion parameters and their first-order derivatives, and ART volumes. Finally, data were linearly detrended and band-pass-filtered (0.008–0.09 Hz).
Network reconstruction and analysis
To assess DMN connectivity with other ICN’s, connectivity matrices were reconstructed using the CONN toolbox. First, a whole-brain functional network was constructed for each subject, with nodes defined based on a parcellation atlas containing 300 regions of interest [11] (Figure S1). This parcellation atlas was selected because it is based on rs-fMRI data, it has a comprehensive representation of cortical and subcortical areas, and it includes a predefined set of 14 networks, including the DMN. Of this set of networks, the “unassigned” network was omitted from current analyses due to the anatomical locations of its 12 nodes, carrying high susceptibility to motion and magnetic-field artifacts. Next, edges were calculated by computing the Fisher Z-transformed Pearson correlation between the BOLD time series extracted for every two nodes, resulting in a pairwise functional connectivity matrix of 288*288 for each subject for each condition (PL and MPH). Then, a difference matrix was computed by performing paired t-test across subjects for the MPH condition vs. the PL condition for all the edges between the 65 nodes that are included in the DMN according to the atlas, and the nodes in all other 12 predefined networks. This resulted in a single matrix of 65*223. FDR correction was applied to threshold the correlation matrix and correct for the number of comparisons to control the expected proportion of falsely rejected hypotheses while maintaining higher sensitivity to detect true effects across the DMN-networks edges, yielding a Fisher Z correlation matrix of edges at p < 0.05 FDR corrected (range: 0.00002 < q < 0.0499). From this matrix, DMN connectivity with the other 12 predefined networks was examined by performing network-wise t-tests for all the edges per network, applying Bonferroni correction for the number of comparisons (i.e., 12 comparisons). Relations between individual differences in the impact of MPH on resting state connectivity and variability in impulsivity scores (BIS-11) were assessed using Pearson correlations.
Graph analysis
Modular organization of neural networks was assessed using the Brain Connectivity Toolbox (BCT; available at https://sites.google.com/site/bctnet/), based on the Newman optimization method [52]. Modularity, a salient characteristic of whole-brain functional networks, refers to the extent to which a network can be partitioned into distinct, non-overlapping communities. Modularity is assessed by optimizing the configuration where intra-community connections are maximized, while inter-community connections are minimized. Within this context, a community is defined as a subset of nodes in the network (i.e., sub-network) that exhibit denser internal connectivity compared to their connectivity with external nodes in the network [52]. Here, modularity analysis was implemented to fractionate the 65 nodes of the DMN into distinct sub-networks. Fractionation was based on the impact of MPH on rs-fMRI connectivity of each DMN node with the other 12 predefined networks. Testing across levels of gamma values (γ) showed consistent results (gamma values starting from 0 and up to 10 in steps of 0.1). Hence, the resolution parameter was set to unity (γ = 1). To assess the reliability of this modular organization, the modularity detection procedure was repeated for 1000 iterations. In each iteration, the algorithm maximized the modularity Q, a metric that quantifies the strength of division of a network into modules, such that connections within modules are denser than connections between modules. Then, normalized mutual information (NMI) values were computed between each pair of the 1000 parcellations [53]. Results showed that the NMI was constantly one, indicating the same module assignment across different parcellations. Consequently, the initial partition was utilized as the modular organization.
Results
Impact of MPH on resting state functional connectivity of the DMN
Paired sample t-tests for the MPH vs. PL conditions for all the edges between nodes within the DMN and all other nodes yielded a difference matrix. This matrix depicts significant changes in DMN resting state functional connectivity following MPH administration compared to placebo, corrected for the number of comparisons. Interestingly, some nodes within the DMN showed MPH-induced increased functional connectivity, while other DMN nodes showed decreased functional connectivity. These opposite effects of MPH on DMN functional connectivity patterns were found with relation to DMN connectivity with all the 12 other networks that were tested (Fig. 1). One sample t-test on all these edges revealed an overall decreased functional connectivity between nodes in the DMN and all other nodes across networks (t[901] = −6.17, p < 0.001). One sample t-test for the connectivity of the DMN separately with nodes within each of the other 12 predefined network, corrected for the number of comparisons, revealed significantly decreased functional connectivity of the DMN following MPH administration with three specific networks (somatomotordorsal: t[216] = −6.11, pBonf. corr.< 0.001; cinguloopercular: t[119] = −7.35, pBonf. corr.< 0.001; auditory: t [71] = −3.31, pBonf. corr.= 0.018). In contrast, a single network increased its functional connectivity with the DMN following MPH (parietomedial: t[38] = 4.56, pBonf. corr.< 0.001) (Fig. 2). Supplementary Fig. 2S depicts the results of analyses assessing sex-specific differences in the impact of MPH on DMN resting state functional connectivity with all other networks.
Impact of MPH on DMN resting-state functional connectivity with all other predefined networks. Nodes within the DMN with significantly increased (A) or decreased (B) functional connectivity with all other nodes following MPH compared to PL administration. All nodes are color-coded by predefined network classification. The size of the nodes, the width of the lines and their opacity depict the strength of individual connections. DMN - Default Mode Network; Methylphenidate – MPH; PL – Placebo
Impact of MPH on resting state functional connectivity of DMN sub-networks
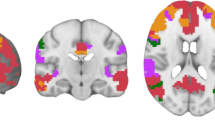
Modularity analysis revealed that the impact of MPH administration on DMN resting-state functional connectivity is best accounted for by dividing the DMN into two distinct communities of nodes (i.e., sub-networks). Of a total of 65 nodes within the DMN, the first community here included 28 nodes and the second community included 37 nodes. Interestingly, both sub-networks exhibited a similar anatomical distribution, with both sub-networks including DMN nodes in parietal, frontal and temporal lobes (Fig. 3, Supplementary Table 1). In order to uncover what drives this differentiation, one sample t-tests were performed separately for MPH-induced changes in connectivity of each DMN sub-network with all other networks, corrected for the number of comparisons. Interestingly, these analyses yielded opposite effects of MPH on functional connectivity of DMN sub-networks. For the DMN nodes included in the 1st DMN sub-network, three networks decreased their functional connectivity (somatomotordorsal: t[93] = −8.16, pBonf. corr. < 0.001; cinguloopercular: t[56] = −12.95, pBonf. corr.< 0.001; auditory: t[41] = −9.84, pBonf. corr. < 0.001). For the 2nd DMN sub-network, one network increased its functional connectivity (parietomedial: t[22] = 3.96, pBonf. corr.= 0.015) (Fig. 4).
DMN sub-networks. Visualization of the two sub-networks of the DMN that emerged from the graph modularity analysis and differ in the impact of MPH on their resting-state functional connectivity. The two sub-networks share similar anatomical distribution (see Supplementary Table 1 for a specific list of coordinates)
MPH-induced change in DMN functional connectivity and impulsivity
While group results revealed robust effects of MPH administration on DMN connectivity with the other predefined networks, high variability was also observed across subjects. Correlation analyses were focused on the four networks that depicted significant group effects of MPH-induced change in DMN connectivity (parietomedial, somatomotordorsal, cinguloopercular and auditory), assessing the relation between individuals’ impulsivity scores and the impact of MPH (vs. PL) on their sub-network connectivity. These analyses revealed that total impulsivity score and non-planning impulsiveness were both negatively associated with the impact of MPH on DMN functional connectivity with the cinguloopercular network (r = − 0.315, p = 0.019; r = − 0.371, p = 0.005; respectively) (Fig. 5A&B). Non-planning impulsiveness was also marginally negatively associated with MPH-induced change in resting-state functional connectivity of the cinguloopercular network with the 1st DMN sub-network as derived from the modularity analysis (r = − 0.250, p = 0.068) (Fig. 5C). These results did not survive correction for multiple comparisons.
The impact of MPH on DMN and impulsivity. Negative associations between MPH-induced change in DMN resting-state functional connectivity with the cinguloopercular network and (A) BIS-11 total impulsivity score and (B) non-planning impulsiveness; as well as between MPH-induced change in resting-state functional connectivity of the first DMN sub-network, as derived from the modularity graph analysis, with the cinguloopercular network and non-planning impulsiveness (C). DMN - Default Mode Network; Methylphenidate - MPH
Discussion
The aim of the current study was to examine the effects of acute MPH administration, an indirect dopaminergic and noradrenergic agonist, on resting-state functional connectivity patterns among healthy adults. We particularly focused on the connectivity of the DMN as a whole with other networks, as well as on connectivity of distinct DMN sub-networks as derived from graph modularity analysis. An additional focus was on the association between these connectivity patterns and participants’ impulsivity scores. Results revealed that, compared to placebo, MPH administration was associated with overall reduced DMN connectivity with other networks during resting-state. This is in accordance with Sripada (2013) showing decreased DMN between-network connectivity in healthy adults, and Cary (2017) showing increased segregation in multiple networks including DMN in ADHD, following MPH administration [21, 28]. Along these lines, MPH administration was also shown to increase internal DMN functional connectivity [20,21,22]. Considering that the DMN is highly involved in internal forms of mentalization and spontaneous cognition and is antagonistic to networks that are engaged by active attention to the external sensory environment, these findings further support the notion that MPH-induced alterations in DMN connectivity may underlie its attention-enhancing effects [54, 55]. Reduced DMN connectivity with other externally-oriented brain networks may therfore represent a neural mechanism for the cognitive enhancement properties of MPH in healthy individuals, as well as for some of its therapeutic effects in ADHD [19, 56, 57].
Importantly, while MPH decreased overall DMN connectivity, the effect was not uniform across all networks, with MPH yielding reduced DMN connectivity specifically with the auditory, cinguloopercular and somatomotor dorsal networks. Inspection of Seitzman et al., (2020) parcellation atlas reveals that nodes that are included in the cinguloopercular and somatomotor networks, as well as those in the DMN, are all part of the cortico-striato-thalamo (CST) circuit [11]. This circuit comprises the supplementary motor area, frontal eye field, lateral orbitofrontal cortex, dorsolateral prefrontal cortex, dorsal anterior cingulate cortex, putamen, caudate, globus pallidus interna, thalamus [58]. The CST circuit is posited to function as a modulatory hub exerting broad influences within and between cortical networks [7]. Previous research has demonstrated that dopamine agonists decrease, and antagonists increase, functional connectivity within this circuit [59]. Therefore, as suggested with other stimulants [26], MPH may facilitate segregation between internally oriented networks, namely DMN, and externally oriented networks, thus enhancing attention allocation towards external stimuli. In line with this suggestion, abnormal functional connectivity within the CST circuit was associated with ADHD [60], and MPH have been shown to “normalize” connectivity within the circuit [61].
MPH administration was also found to increase DMN connectivity with the parietomedial network (PMN), a relatively newly discovered neural network composed of the superior parieto-occipital fissure, posterior cingulate cortex and intraparietal sulcus. The PMN is hypothesized to be involved in memory functions and attention to internal representations [62]. Studies have demonstrate increased connectivity between the DMN and the PMN in tasks that are characterized by evaluation of internal information, suggesting that these large-scale connectivity patterns reflect temporally extended evaluation of self-generated thoughts [63]. Hence, the PMN may be seen as part of an extended DMN and its increased connectivity with the DMN following MPH in here may represent MPH-induced increases in internal DMN functional connectivity, as was demonstrated before [20,21,22]. This again supports the scenario that MPH may reduce the impact of DMN processing on externally oriented networks, thus increasing their potential engagement with external stimuli.
Graph analysis revealed that the DMN can be fractionated into two distinct sub-networks with divergent, even opposing, impacts of MPH administration. This is consistent with prior seed-based analyses that demonstrated MPH’s differentiated impact on DMN sub-networks both in healthy adults [64] and in ADHD [65]. Here, the first DMN sub-network was the one associated with MPH-induced reduced connectivity with the auditory, cinguloopercular and somatomotor networks, while the second DMN sub-network was associated with MPH-induced increased connectivity with the parietomedial network. These distinct component sub-networks are in accordance with previous studies showing a salient feature that includes distributed, parallel nodes within the DMN [7]. Interestingly, here, as in the majority of previous studies, DMN sub-networks did not differ with respect to their anatomical spatial distribution, such that the nodes of one sub-network lie side by side with those of the other sub-network [7, 9, 10]. Buckner and DiNicola (2019) suggested that DMN sub-networks may have originated from a less differentiated proto-organization that specialized over time [7]. Using subject-level clustering, Akiki and Abdalla (2019) suggested that the division of the DMN into two sub-networks is functionally consistent [66]. Evidence from task activation studies indicate that midline DMN structures are functionally specialized for self-relevant decisions and the inference of other people’s mental states, whereas more lateral temporal DMN components are implicated in autobiographical memory and self-oriented mental activity [67]. These findings suggest that the DMN sub-networks uncovered here may carry distinct functionality. The first DMN sub-network may tap into the CST circuit in order to suppress connectivity with external stimuli processing networks, with MPH leading to its reduced connectivity with other neural networks, hence further facilitating this segregation. The second DMN sub-network may promote attention to internal representations, with MPH increasing its connectivity with other associated networks such as the parietomedial network.
Finally, variability in the impact of MPH on DMN connectivity was associated with impulsivity scores. Specifically, MPH administration yielded a reduction in DMN functional connectivity with the cinguloopercular network, and this decreased connectivity was more potent in individuals with elevated impulsivity and non-planning impulsiveness. These results highly resemble the finding of Davis and colleagues demonstrating that differences in whole-brain functional organization are related to impulsivity [68], particularly in brain regions associated with the cinguloopercular network. Specifically, they showed decreased functional coupling between cortical control and subcortical drive modules as a function of increasing impulsivity. Previous studies have also demonstrated an association between reduced DMN- cinguloopercular resting-state functional connectivity and impulsivity, specifically relating to non-planning and disregard for future consequences [69]. In addition, the cingulo-opercular network was found to be associated with failure of response control when faced with anticipating rewards (i.e. non-planning impulsiveness) [70]. This is in accordance with our result showing that more decreased connectivity following MPH is associated with lower non-planning impulsivity. Taken together, individuals with elevated total impulsivity and specifically non-planning impulsiveness may particularly benefit from MPH administration as it leads to greater reduction in their DMN- cinguloopercular resting-state functional connectivity. Further work could examine whether distinct DMN sub-networks and intrinsic (opposed to task-induced) connectivity changes play a role in these associations.
While providing valuable insights, this study does have some limitations worth mentioning. First, we assessed the immediate impact of acute MPH administration hence cannot infer on the impact of chronic administration. Second, given that the current sample was composed of healthy adults we cannot assume that similar patterns will appear among ADHD population nor among other age groups. This is particularly relevant given the demonstrated age-dependent relation between impulsivity and functional brain networks [43], and in light of previous studies reporting on differential impact of MPH administration on resting-state connectivity patterns among healthy compared to ADHD cohorts [71]. Also important in that regard is that by relying solely on fMRI we of course cannot directly link the observed neural changes to dopamine levels. Future research employing hybrid PET/MRI techniques could provide more nuanced insights into the neurotransmitter pathways affected by MPH. It is further important to note that we administered a fixed 20 mg dose of MPH to all participants, without adjusting for individual differences in weight and/or BMI. While this dose is within the range commonly used in both clinical practice and research, future studies could benefit from exploring the effects of varying MPH doses, including weight-adjusted dosing, to fully capture variability in the effects of MPH on resting-state functional connectivity. This variability may also be influenced by plasma levels of the drug, as demonstrated by Müller et al. (2005), who found task-related fMRI signal changes to be plasma-level-dependent, emphasizing the need to consider pharmacokinetic factors in the interpretation of MPH’s neural impacts [72]. Lastly, we did not account for variability in menstrual cycle phase among female participants.
In summary, using a randomized double-blind placebo-controlled design in a sample of fifty-five healthy adults, we were able to characterize the impact of acute MPH administration on DMN resting-state functional connectivity patterns. Results revealed MPH-induced reduced DMN connectivity, particularly with the auditory, cinguloopercular, and somatomotor networks, as well as increased DMN connectivity with the parietomedial network. Graph analysis further showed that the DMN could be fractionated into two distinct sub-networks with divergent, even opposing, functionalities, such that one DMN sub-network was associated with MPH-induced reduced connectivity while the other was associated with increased connectivity. Finally, individuals with elevated impulsivity exhibited the strongest MPH-induced reduction in their DMN connectivity with the cinguloopercular network. Taken together, this study provides novel insights into the modulatory effects of MPH on DMN connectivity and its implications for impulsivity.
Data availability
Data available upon request from the authors.
Refrences
Petersen SE, Sporns O. Brain networks and cognitive architectures. Neuron. 2015;88(1):207–19. https://doi.org/10.1016/j.neuron.2015.09.027. PubMed PMID: 26447582; PubMed Central PMCID: PMCPMC4598639.
Fox MD, Raichle ME. Spontaneous fluctuations in brain activity observed with functional magnetic resonance imaging. Nat Rev Neurosci. 2007;8(9):700 – 11. https://doi.org/10.1038/nrn2201. PubMed PMID: 17704812.
Greicius MD, Krasnow B, Reiss AL, Menon V. Functional connectivity in the resting brain: a network analysis of the default mode hypothesis. Proc Natl Acad Sci U S A. 2003;100(1):253–8. https://doi.org/10.1073/pnas.0135058100. PubMed PMID: 12506194; PubMed Central PMCID: PMCPMC140943.
Uddin LQ, Kelly AM, Biswal BB, Castellanos FX, Milham MP. Functional connectivity of default mode network components: correlation, anticorrelation, and causality. Hum Brain Mapp. 2009;30(2):625–37. https://doi.org/10.1002/hbm.20531. PubMed PMID: 18219617; PubMed Central PMCID: PMCPMC3654104.
Seghier ML, Price CJ. Functional heterogeneity within the Default Network during semantic Processing and Speech Production. Front Psychol. 2012;3:281. https://doi.org/10.3389/fpsyg.2012.00281. PubMed PMID: 22905029; PubMed Central PMCID: PMCPMC3417693.
Salomon R, Levy DR, Malach R. Deconstructing the default: cortical subdivision of the default mode/intrinsic system during self-related processing. Hum Brain Mapp. 2014;35(4):1491–502. https://doi.org/10.1002/hbm.22268. PubMed PMID: 23568328; PubMed Central PMCID: PMCPMC6869590.
Buckner RL, DiNicola LM. The brain’s default network: updated anatomy, physiology and evolving insights. Nat Rev Neurosci. 2019;20(10):593–608. https://doi.org/10.1038/s41583-019-0212-7. PubMed PMID: 31492945.
Kim H. A dual-subsystem model of the brain’s default network: self-referential processing, memory retrieval processes, and autobiographical memory retrieval. NeuroImage. 2012;61(4):966–77. https://doi.org/10.1016/j.neuroimage.2012.03.025. PubMed PMID: 22446489.
Braga RM, Buckner RL. Parallel Interdigitated Distributed Networks within the Individual Estimated by Intrinsic Functional Connectivity. Neuron. 2017;95(2):457 – 71 e5. https://doi.org/10.1016/j.neuron.2017.06.038. PubMed PMID: 28728026; PubMed Central PMCID: PMCPMC5519493.
Braga RM, Van Dijk KRA, Polimeni JR, Eldaief MC, Buckner RL. Parallel distributed networks resolved at high resolution reveal close juxtaposition of distinct regions. J Neurophysiol. 2019;121(4):1513–34. https://doi.org/10.1152/jn.00808.2018. PubMed PMID: 30785825; PubMed Central PMCID: PMCPMC6485740.
Seitzman BA, Gratton C, Marek S, Raut RV, Dosenbach NUF, Schlaggar BL, et al. A set of functionally-defined brain regions with improved representation of the subcortex and cerebellum. NeuroImage. 2020;206:116290. https://doi.org/10.1016/j.neuroimage.2019.116290. PubMed PMID: 31634545; PubMed Central PMCID: PMCPMC6981071.
Yeo BT, Krienen FM, Sepulcre J, Sabuncu MR, Lashkari D, Hollinshead M, et al. The organization of the human cerebral cortex estimated by intrinsic functional connectivity. J Neurophysiol. 2011;106(3):1125–65. https://doi.org/10.1152/jn.00338.2011. PubMed PMID: 21653723; PubMed Central PMCID: PMCPMC3174820.
Menon V, Uddin LQ. Saliency, switching, attention and control: a network model of insula function. Brain Struct Funct. 2010;214(5–6):655–67. https://doi.org/10.1007/s00429-010-0262-0. PubMed PMID: 20512370; PubMed Central PMCID: PMCPMC2899886.
Wang KS, Brown K, Frederick BB, Moran LV, Olson D, Pizzagalli DA, et al. Nicotine acutely alters temporal properties of resting brain states. Drug Alcohol Depend. 2021;226:108846. https://doi.org/10.1016/j.drugalcdep.2021.108846. PubMed PMID: 34198131; PubMed Central PMCID: PMCPMC8355138.
Kaiser RH, Chase HW, Phillips ML, Deckersbach T, Parsey RV, Fava M, et al. Dynamic resting-state network biomarkers of antidepressant treatment response. Biol Psychiatry. 2022;92(7):533–42. PubMed PMID: 35680431.
Menon V. Large-scale brain networks and psychopathology: a unifying triple network model. Trends Cogn Sci. 2011;15(10):483–506. 003. PubMed PMID: 21908230.
Kaiser RH, Andrews-Hanna JR, Wager TD, Pizzagalli DA. Large-Scale Network Dysfunction in Major Depressive disorder: a Meta-analysis of resting-state functional connectivity. JAMA Psychiatry. 2015;72(6):603–11. https://doi.org/10.1001/jamapsychiatry.2015.0071. PubMed PMID: 25785575; PubMed Central PMCID: PMCPMC4456260.
Olson EA, Kaiser RH, Pizzagalli DA, Rauch SL, Rosso IM. Regional Prefrontal resting-state functional connectivity in posttraumatic stress disorder. Biol Psychiatry Cogn Neurosci Neuroimaging. 2019;4(4):390–8. https://doi.org/10.1016/j.bpsc.2018.09.012. PubMed PMID: 30449518; PubMed Central PMCID: PMCPMC6447465.
Berridge CW, Devilbiss DM, Andrzejewski ME, Arnsten AF, Kelley AE, Schmeichel B, et al. Methylphenidate preferentially increases catecholamine neurotransmission within the prefrontal cortex at low doses that enhance cognitive function. Biol Psychiatry. 2006;60(10):1111–20. https://doi.org/10.1016/j.biopsych.2006.04.022. PubMed PMID: 16806100.
Picon FA, Sato JR, Anes M, Vedolin LM, Mazzola AA, Valentini BB, et al. Methylphenidate Alters Functional Connectivity of Default Mode Network in Drug-Naive male adults with ADHD. J Atten Disord. 2020;24(3):447–55. doi: 10.1177/1087054718816822. PubMed PMID: 30526190.
Cary RP, Ray S, Grayson DS, Painter J, Carpenter S, Maron L, et al. Network structure among Brain systems in adult ADHD is uniquely modified by Stimulant Administration. Cereb Cortex. 2017;27(8):3970–9. https://doi.org/10.1093/cercor/bhw209. PubMed PMID: 27422412; PubMed Central PMCID: PMCPMC6248828.
Mizuno Y, Cai W, Supekar K, Makita K, Takiguchi S, Silk TJ, et al. Methylphenidate enhances spontaneous fluctuations in reward and Cognitive Control Networks in Children with Attention-Deficit/Hyperactivity disorder. Biol Psychiatry Cogn Neurosci Neuroimaging. 2023;8(3):271–80. https://doi.org/10.1016/j.bpsc.2022.10.001. PubMed PMID: 36717325.
Henry TR, Fogleman ND, Nugiel T, Cohen JR. Effect of methylphenidate on functional controllability: a preliminary study in medication-naive children with ADHD. Transl Psychiatry. 2022;12(1):518. https://doi.org/10.1038/s41398-022-02283-4. PubMed PMID: 36528602; PubMed Central PMCID: PMCPMC9759578.
Mizuno Y, Cai W, Supekar K, Makita K, Takiguchi S, Tomoda A, et al. Methylphenidate remediates aberrant brain network dynamics in children with attention-deficit/hyperactivity disorder: a randomized controlled trial. NeuroImage. 2022;257:119332. https://doi.org/10.1016/j.neuroimage.2022.119332. PubMed PMID: 35640787; PubMed Central PMCID: PMCPMC9286726.
Silk TJ, Malpas C, Vance A, Bellgrove MA. The effect of single-dose methylphenidate on resting-state network functional connectivity in ADHD. Brain Imaging Behav. 2017;11(5):1422–31. https://doi.org/10.1007/s11682-016-9620-8. PubMed PMID: 27734305.
Yang Z, Kelly C, Castellanos FX, Leon T, Milham MP, Adler LA. Neural correlates of Symptom Improvement following stimulant treatment in adults with Attention-Deficit/Hyperactivity disorder. J Child Adolesc Psychopharmacol. 2016;26(6):527–36. https://doi.org/10.1089/cap.2015.0243. PubMed PMID: 27027541; PubMed Central PMCID: PMCPMC4991601.
Mueller S, Costa A, Keeser D, Pogarell O, Berman A, Coates U, et al. The effects of methylphenidate on whole brain intrinsic functional connectivity. Hum Brain Mapp. 2014;35(11):5379–88. https://doi.org/10.1002/hbm.22557. PubMed PMID: 24862742; PubMed Central PMCID: PMCPMC6869774.
Sripada CS, Kessler D, Welsh R, Angstadt M, Liberzon I, Phan KL, et al. Distributed effects of methylphenidate on the network structure of the resting brain: a connectomic pattern classification analysis. NeuroImage. 2013;81:213–21. https://doi.org/10.1016/j.neuroimage.2013.05.016. PubMed PMID: 23684862; PubMed Central PMCID: PMCPMC3729859.
Campez M, Raiker JS, Little K, Altszuler AR, Merrill BM, Macphee FL, et al. An evaluation of the effect of methylphenidate on working memory, time perception, and choice impulsivity in children with ADHD. Exp Clin Psychopharmacol. 2022;30(2):209–19. https://doi.org/10.1037/pha0000446. PubMed PMID: 33475395; PubMed Central PMCID: PMCPMC8406432.
Fosco WD, Rosch KS, Waxmonsky JG, Pelham WE, Hawk LW. Baseline performance moderates stimulant effects on cognition in youth with ADHD. Exp Clin Psychopharmacol. 2021;29(4):302–7. https://doi.org/10.1037/pha0000374. PubMed PMID: 32297786; PubMed Central PMCID: PMCPMC8388131.
Daood M, Peled-Avron L, Ben-Hayun R, Nevat M, Aharon-Peretz J, Tomer R, et al. Fronto-striatal connectivity patterns account for the impact of methylphenidate on choice impulsivity among healthy adults. Neuropharmacology. 2022;216:109190. https://doi.org/10.1016/j.neuropharm.2022.109190. PubMed PMID: 35835210.
Sharma L, Markon KE, Clark LA. Toward a theory of distinct types of impulsive behaviors: a meta-analysis of self-report and behavioral measures. Psychol Bull. 2014;140(2):374–408. https://doi.org/10.1037/a0034418. PubMed PMID: 24099400.
Zhang L, Cui Z, Huffman LG, Oshri A. Sleep mediates the effect of stressful environments on youth development of impulsivity: the moderating role of within default mode network resting-state functional connectivity. Sleep Health. 2023. https://doi.org/10.1016/j.sleh.2023.03.005. PubMed PMID: 37270396.
Zhu X, Cortes CR, Mathur K, Tomasi D, Momenan R. Model-free functional connectivity and impulsivity correlates of alcohol dependence: a resting-state study. Addict Biol. 2017;22(1):206–17. https://doi.org/10.1111/adb.12272. PubMed PMID: 26040546; PubMed Central PMCID: PMCPMC4669235.
Varma MM, Zhen S, Yu R. Not all discounts are created equal: Regional activity and brain networks in temporal and effort discounting. NeuroImage. 2023;280:120363. https://doi.org/10.1016/j.neuroimage.2023.120363. PubMed PMID: 37673412.
Noda Y, Barr MS, ElSalhy M, Masuda F, Tarumi R, Ogyu K, et al. Neural correlates of delay discount alterations in addiction and psychiatric disorders: a systematic review of magnetic resonance imaging studies. Prog Neuropsychopharmacol Biol Psychiatry. 2020;99:109822. https://doi.org/10.1016/j.pnpbp.2019.109822. PubMed PMID: 31751662.
Schuller CB, Kuhn J, Jessen F, Hu X. Neuronal correlates of delay discounting in healthy subjects and its implication for addiction: an ALE meta-analysis study. Am J Drug Alcohol Abuse. 2019;45(1):51–66. PubMed PMID: 30632802.
Owens MM, Gray JC, Amlung MT, Oshri A, Sweet LH, MacKillop J. Neuroanatomical foundations of delayed reward discounting decision making. NeuroImage. 2017;161:261–70. https://doi.org/10.1016/j.neuroimage.2017.08.045. PubMed PMID: 28843539; PubMed Central PMCID: PMCPMC5895082.
Wang Q, Chen C, Cai Y, Li S, Zhao X, Zheng L, et al. Dissociated neural substrates underlying impulsive choice and impulsive action. NeuroImage. 2016;134:540–9. https://doi.org/10.1016/j.neuroimage.2016.04.010. PubMed PMID: 27083527.
Cai H, Chen J, Liu S, Zhu J, Yu Y. Brain functional connectome-based prediction of individual decision impulsivity. Cortex. 2020;125:288 – 98. https://doi.org/10.1016/j.cortex.2020.01.022. PubMed PMID: 32113043.
Li N, Ma N, Liu Y, He XS, Sun DL, Fu XM, et al. Resting-state functional connectivity predicts impulsivity in economic decision-making. J Neurosci. 2013;33(11):4886–95. https://doi.org/10.1523/JNEUROSCI.1342-12.2013. PubMed PMID: 23486959; PubMed Central PMCID: PMCPMC6618998.
Mehta K, Pines A, Adebimpe A, Larsen B, Bassett DS, Calkins ME, et al. Individual differences in delay discounting are associated with dorsal prefrontal cortex connectivity in children, adolescents, and adults. Dev Cogn Neurosci. 2023;62:101265. https://doi.org/10.1016/j.dcn.2023.101265. PubMed PMID: 37327696; PubMed Central PMCID: PMCPMC10285090.
Fornaro S, Menardi A, Vallesi A. Topological features of functional brain networks and subclinical impulsivity: an investigation in younger and older adults. Brain Struct Funct. 2024. https://doi.org/10.1007/s00429-023-02745-5. PubMed PMID: 38446245.
Oldfield RC. The assessment and analysis of handedness: the Edinburgh inventory. Neuropsychologia. 1971;9(1):97–113. https://doi.org/10.1016/0028-3932(71)90067-4. PubMed PMID: 5146491.
Conners C, Erhardt D, Sparrow E, Staff M. Conners’ adult ADHD rating scales (CAARS). New York: Multi-Health Systems. Inc; 1999.
Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, et al. The mini-international neuropsychiatric interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. 1998;59(Suppl 20):22–33. quiz 4–57. PubMed PMID: 9881538.
Patton JH, Stanford MS, Barratt ES. Factor structure of the Barratt impulsiveness scale. J Clin Psychol. 1995;51(6):768–74. https://doi.org/10.1002/1097-4679(199511)51:6<768::aid-jclp2270510607>3.0.co;2-1. PubMed PMID: 8778124.
Volkow ND, Wang GJ, Fowler JS, Gatley SJ, Logan J, Ding YS, et al. Dopamine transporter occupancies in the human brain induced by therapeutic doses of oral methylphenidate. Am J Psychiatry. 1998;155(10):1325–31. https://doi.org/10.1176/ajp.155.10.1325. PubMed PMID: 9766762.
Peled-Avron L, Gelbard Goren H, Brande-Eilat N, Dorman-Ilan S, Segev A, Feffer K, et al. Methylphenidate reduces orienting bias in healthy individuals. J Psychopharmacol. 2021;35(6):760–7. 10.1177/0269881121996884. PubMed PMID: 33719709.
Glicksohn J, Nahari G. Interacting personality traits? Smoking as a test case. Eur J Pers. 2007;21(2):225–34.
Whitfield-Gabrieli S, Nieto-Castanon A. Conn: a functional connectivity toolbox for correlated and anticorrelated brain networks. Brain Connect. 2012;2(3):125 – 41. https://doi.org/10.1089/brain.2012.0073. PubMed PMID: 22642651.
Leicht EA, Newman ME. Community structure in directed networks. Phys Rev Lett. 2008;100(11):118703. https://doi.org/10.1103/PhysRevLett.100.118703. PubMed PMID: 18517839.
Alexander-Bloch A, Lambiotte R, Roberts B, Giedd J, Gogtay N, Bullmore E. The discovery of population differences in network community structure: new methods and applications to brain functional networks in schizophrenia. NeuroImage. 2012;59(4):3889–900. PubMed PMID: 22119652; PubMed Central PMCID: PMCPMC3478383.
Fox MD, Snyder AZ, Vincent JL, Corbetta M, Van Essen DC, Raichle ME. The human brain is intrinsically organized into dynamic, anticorrelated functional networks. Proc Natl Acad Sci U S A. 2005;102(27):9673–8. https://doi.org/10.1073/pnas.0504136102. PubMed PMID: 15976020; PubMed Central PMCID: PMCPMC1157105.
Fransson P. Spontaneous low-frequency BOLD signal fluctuations: an fMRI investigation of the resting-state default mode of brain function hypothesis. Hum Brain Mapp. 2005;26(1):15–29. PubMed PMID: 15852468.
Busardo FP, Kyriakou C, Cipolloni L, Zaami S, Frati P. From clinical application to cognitive enhancement: the Example of Methylphenidate. Curr Neuropharmacol. 2016;14(1):17–27. https://doi.org/10.2174/1570159x13666150407225902. PubMed PMID: 26813119; PubMed Central PMCID: PMCPMC4787280.
Rosenberg MD, Zhang S, Hsu WT, Scheinost D, Finn ES, Shen X, et al. Methylphenidate Modulates Functional Network Connectivity to enhance attention. J Neurosci. 2016;36(37):9547–57. https://doi.org/10.1523/JNEUROSCI.1746-16.2016. PubMed PMID: 27629707; PubMed Central PMCID: PMCPMC5039242.
Alexander GE, DeLong MR, Strick PL. Parallel organization of functionally segregated circuits linking basal ganglia and cortex. Annu Rev Neurosci. 1986;9:357 – 81. https://doi.org/10.1146/annurev.ne.09.030186.002041. PubMed PMID: 3085570.
Honey GD, Suckling J, Zelaya F, Long C, Routledge C, Jackson S, et al. Dopaminergic drug effects on physiological connectivity in a human cortico-striato-thalamic system. Brain. 2003;126(Pt 8):1767–81. https://doi.org/10.1093/brain/awg184. PubMed PMID: 12805106; PubMed Central PMCID: PMCPMC3838939.
Posner J, Park C, Wang Z. Connecting the dots: a review of resting connectivity MRI studies in attention-deficit/hyperactivity disorder. Neuropsychol Rev. 2014;24(1):3–15. https://doi.org/10.1007/s11065-014-9251-z. PubMed PMID: 24496902; PubMed Central PMCID: PMCPMC4119002.
An L, Cao XH, Cao QJ, Sun L, Yang L, Zou QH, et al. Methylphenidate normalizes resting-state brain dysfunction in boys with attention deficit hyperactivity disorder. Neuropsychopharmacology. 2013;38(7):1287–95. https://doi.org/10.1038/npp.2013.27. PubMed PMID: 23340519; PubMed Central PMCID: PMCPMC3656372.
Gilmore AW, Nelson SM, McDermott KB. A parietal memory network revealed by multiple MRI methods. Trends Cogn Sci. 2015;19(9):534–43. PubMed PMID: 26254740.
Andrews-Hanna JR, Smallwood J, Spreng RN. The default network and self-generated thought: component processes, dynamic control, and clinical relevance. Ann N Y Acad Sci. 2014;1316(1):29–52. https://doi.org/10.1111/nyas.12360. PubMed PMID: 24502540; PubMed Central PMCID: PMCPMC4039623.
Becker M, Repantis D, Dresler M, Kuhn S. Cognitive enhancement: effects of methylphenidate, modafinil, and caffeine on latent memory and resting state functional connectivity in healthy adults. Hum Brain Mapp. 2022;43(14):4225–38. https://doi.org/10.1002/hbm.25949. PubMed PMID: 35670369; PubMed Central PMCID: PMCPMC9435011.
Hong SB, Harrison BJ, Fornito A, Sohn CH, Song IC, Kim JW. Functional dysconnectivity of corticostriatal circuitry and differential response to methylphenidate in youth with attention-deficit/hyperactivity disorder. J Psychiatry Neurosci. 2015;40(1):46–57. https://doi.org/10.1503/jpn.130290. PubMed PMID: 25266402; PubMed Central PMCID: PMCPMC4275331.
Akiki TJ, Abdallah CG. Determining the Hierarchical Architecture of the Human Brain Using Subject-Level Clustering of Functional Networks. Sci Rep. 2019;9(1):19290. https://doi.org/10.1038/s41598-019-55738-y. PubMed PMID: 31848397; PubMed Central PMCID: PMCPMC6917755 Lundbeck, and FSV7, serves as editor for the journal Chronic Stress published by SAGE Publications, Inc, and filed a patent for using mTOR inhibitors to augment the effects of antidepressants (filed on Aug 20, 2018).
Andrews-Hanna JR, Reidler JS, Sepulcre J, Poulin R, Buckner RL. Functional-anatomic fractionation of the brain’s default network. Neuron. 2010;65(4):550–62. https://doi.org/10.1016/j.neuron.2010.02.005. PubMed PMID: 20188659; PubMed Central PMCID: PMCPMC2848443.
Davis FC, Knodt AR, Sporns O, Lahey BB, Zald DH, Brigidi BD, et al. Impulsivity and the modular organization of resting-state neural networks. Cereb Cortex. 2013;23(6):1444–52. https://doi.org/10.1093/cercor/bhs126. PubMed PMID: 22645253; PubMed Central PMCID: PMCPMC3643719.
Chen Z, Guo Y, Suo T, Feng T. Coupling and segregation of large-scale brain networks predict individual differences in delay discounting. Biol Psychol. 2018;133:63–71. PubMed PMID: 29382543.
Zhukovsky P, Morein-Zamir S, Meng C, Dalley JW, Ersche KD. Network failures: when incentives trigger impulsive responses. Hum Brain Mapp. 2020;41(8):2216–28. https://doi.org/10.1002/hbm.24941. PubMed PMID: 32150321; PubMed Central PMCID: PMCPMC7267965.
Kaiser A, Broeder C, Cohen JR, Douw L, Reneman L, Schrantee A. Effects of a single-dose methylphenidate challenge on resting-state functional connectivity in stimulant-treatment naive children and adults with ADHD. Hum Brain Mapp. 2022;43(15):4664–75. https://doi.org/10.1002/hbm.25981. PubMed PMID: 35781371; PubMed Central PMCID: PMCPMC9491277.
Muller U, Suckling J, Zelaya F, Honey G, Faessel H, Williams SC, et al. Plasma level-dependent effects of methylphenidate on task-related functional magnetic resonance imaging signal changes. Psychopharmacology. 2005;180(4):624–33. https://doi.org/10.1007/s00213-005-2264-9. PubMed PMID: 15830222.
Funding
This research was supported by research grants from the Israel Anti-Drug Authority and the Israel Authority for Prevention of Violence, Alcohol and Drug Abuse, the Ministry of Public Security, awarded to R.A.; And by the Israel Science Foundation (ISF) (grant No.1806/16) awarded to R.T.
Author information
Authors and Affiliations
Contributions
MD - Acquisition, Analysis and Interpretation of data and Writing original draftNM - Analysis and Interpretation of data and Writing original draft. LPA - Acquisition, Analysis and Interpretation of data. MN - Analysis and Interpretation of data. RBH – Conceptualization and Funding acquisition. JAP – Conceptualization and Funding acquisition. RT - Conceptualization and Funding acquisition and Writing original draft. RA - Conceptualization and Funding acquisition and Writing original draft.
Corresponding author
Ethics declarations
Ethical approval
Eligible participants provided written informed consent to a protocol approved by the ethics committees of the University of Haifa (approval #368/17) and Rambam Health Care Campus (approval #0539 − 16) and received monetary compensation for their participation.
Disclosures
The authors affirm that they have no financial affiliations or involvement with any commercial organization with direct financial interest in the subject or materials discussed in this manuscript. All authors have thoroughly reviewed and discussed the content of this manuscript and declare no potential conflicts of interest regarding the publication of this paper.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Daood, M., Magal, N., Peled-Avron, L. et al. Graph analysis uncovers an opposing impact of methylphenidate on connectivity patterns within default mode network sub-divisions. Behav Brain Funct 20, 15 (2024). https://doi.org/10.1186/s12993-024-00242-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12993-024-00242-1