Abstract
Background
Factors influencing antidepressant treatment discontinuation are poorly understood. In the present study, we aimed to estimate the prevalence of antidepressant treatment discontinuation and identify demographic characteristics, psychiatric comorbidities, and specific side effects associated with treatment discontinuation.
Methods
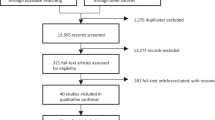
We leveraged data from the Australian Genetics of Depression Study (AGDS; N = 20,941) to perform a retrospective cohort study on antidepressant treatment discontinuation. Participants were eligible if they were over 18 years of age, had taken antidepressants in the past 4 years, and provided informed consent.
Results
Among the ten antidepressants studied, the highest discontinuation rates were observed for Mirtazapine (57.3%) and Amitriptyline (51.6%). Discontinuation rates were comparable across sexes except for Mirtazapine, for which women were more likely to discontinue. The two most common side effects, reduced sexual function and weight gain, were not associated with increased odds of treatment discontinuation. Anxiety, agitation, suicidal thoughts, vomiting, and rashes were associated with higher odds for treatment discontinuation, as were lifetime diagnoses of PTSD, ADHD, and a higher neuroticism score. Educational attainment showed a negative (protective) association with discontinuation across medications.
Conclusions
Our study suggests that not all side effects contribute equally to discontinuation. Common side effects such as reduced sexual function and weight gain may not necessarily increase the risk of treatment discontinuation. Side effects linked to discontinuation can be divided into two groups, psychopathology related and allergy/intolerance.
Similar content being viewed by others
Background
Depression is among the most common psychiatric disorders. It has a detrimental impact on the quality of life and functioning of individuals. It is estimated to become the leading global cause of disability by 2030 [1], and 70 to 80% of diagnosed patients will experience relapses and recurrences that often require long-term treatment [2].
Pharmacological interventions, which are commonly used as the first line of treatment for depression, are broadly classified as first- or second-generation antidepressants according to their mechanism of action. Although treatment response rates have been estimated around 50% [3], a significant number of individuals will still experience severe residual symptoms of depression, even when undergoing treatment. A lack of treatment response without appropriate medical guidance can lead to treatment discontinuation, which in turn results in relapse, a diminished quality of life, and symptoms such as insomnia, imbalance, nausea, and sensory disturbances [4].
Treatment discontinuation also occurs due to adverse side effects. In a previous study, we described the prevalence, risk factors, and genetic basis of antidepressant side effects in a cohort of 20,941 Australian adults. We discovered that regardless of the antidepressant taken, 60–75% of participants reported at least one side effect. In particular, we identified reduced sexual function and weight gain as the most frequently reported side effects [5]. These findings were reiterated by various long-term studies in which reduced sexual function and weight gain affected up to 70% of individuals who were prescribed antidepressants [6, 7].
Previous research has primarily focused on discontinuation rates from the larger subset of antidepressant drug classes [8, 9], and several studies have observed the highest discontinuation rates in patients who were taking tricyclic antidepressants (TCAs) [8, 10]. In addition, some evidence suggests males are almost twice more likely to discontinue treatment [11]. Previous literature suggests that specific side effects such as skin rash, attempted suicide, headache, and mania are associated with an increased discontinuation from clinical trials of depression treatment in adolescents [12]. Nonetheless, a study seeking to identify potential risk factors for treatment discontinuation, as opposed to discontinuation from clinical trials, is currently lacking. Therefore, in the present study, we explore participant-reported treatment discontinuation due to adverse side effects for ten commonly prescribed antidepressants using a sample of 20,941 participants. We estimate discontinuation rates for each antidepressant and test for association between discontinuation and specific side effects, demographic variables, and psychiatric comorbidities.
Methods
AGDS cohort sample
The Australian Genetics of Depression Study (AGDS) recruited 22,424 Australian participants through two streams: a targeted assisted mailout campaign (14%) and an open media campaign (86%). Potential participants were directed to the AGDS website. Ninety-five percent of participants in the AGDS reported being given a diagnosis of depression by a medical practitioner [13]. Informed consent was gathered prior to data collection through online questionnaires after participants received a complete description of the study. The AGDS inclusion criteria included (i) having been prescribed and taken antidepressants and (ii) providing consent to donate a saliva sample for genotyping. A full and detailed description of AGDS recruitment is reported elsewhere [13]. For this study, participants who did not report having a diagnosis of depression were excluded from the analyses (N = 1483), yielding a total sample size of 20,941 participants. This study was approved by the QIMR Berghofer Human and Research Ethics Committee under project number P1218.
Phenotype ascertainment
From the participants that had been diagnosed with depression, they first confirmed they had taken any of the ten most commonly prescribed antidepressants in Australia, listed as Sertraline, Escitalopram, Venlafaxine, Fluoxetine, Citalopram, Desvenlafaxine, Duloxetine, Mirtazapine, Amitriptyline, and Paroxetine. For each antidepressant taken, participants were asked whether they had experienced side effects and, if so, to select which from a checklist of 23 commonly reported antidepressant side effects.
Participants were further asked explicitly whether they stopped taking a specific medication due to adverse side effects. Data on demographics, clinical history, as well as psychiatric traits (such as neuroticism and extraversion) were also gathered. The full list and details of instruments used for AGDS phenotyping are available at https://bit.ly/3y72lyg.
Statistical analyses
The present study investigated the relationship between participant-reported antidepressant treatment discontinuation and other variables, including demographic factors, side effects, psychiatric comorbidities, and other factors in the Eysenck Personality Questionnaire neuroticism, extraversion scores, and chronotype measures. We assessed these relationships using four multiple logistic regression models, including demographic factors, side effects, psychiatric comorbidities, and Eysenck Personality Questionnaire. This enabled us to quantify associations with antidepressant treatment discontinuation while adjusting for covariate effects, such as the age of treatment initiation and sex. Briefly, logistic regressions are considered extensions of linear models. Therefore, a logistic regression is used to model a linear relationship between predictor variables and the natural logarithm of the odds of a dependent variable [14] . A predominant advantage of logistic regression models is that they enable the estimation of an odds ratio, which in turn indicates the odds of observing a given outcome (i.e., the dependent variable) given a particular exposure (i.e., the predictor variables).
We estimated odds ratios from the effect sizes on the logistic scale and calculated p-values using Wald tests. For every antidepressant, discontinuation was modeled as a binary variable in which cases included participants who stopped antidepressant treatment due to side effects, and controls included participants who did not stop antidepressant treatment due to side effects. All statistical analyses were performed in Python 3.0 using the following modules: pandas, numpy, statsmodels, scipy, seaborn, and matplotlib. Statistical significance was defined using Bonferroni multiple testing correction for each group of variables was performed based on the total number of variables in each group (i.e., 7 demographic factors, 23 side effects, 18 psychiatric comorbidities, and 9 items of the Eysenck Personality Questionnaire; Additional file 1: Tables S1). Nominal associations refer to those with a p-value < 0.05.
Results
Demographics
Table 1 shows the discontinuation rates and key demographics across medications. The present study included a total of 20,941 participants from the AGDS cohort. Of those, 15,830 were women (76%), and 5111 were men (24%). A total of 7723 participants (36·9%) had stopped taking at least one medication due to adverse side effects. We observed the highest discontinuation rate for Mirtazapine (57·3%) and the lowest discontinuation rates for Escitalopram (38.9%) and Desvenlafaxine (38.4%; Fig. 1a).
Prevalence and factors associated with treatment discontinuation a Estimated discontinuation rates and 95% confidence intervals are shown across medications. The graph is color coded according to medication class (from left to right): SSRIs, SNRIs, and others. Purple dashed lines show the estimates for males, whereas the green solid lines show the results for females. b Heatmap depicting the odds ratio between treatment discontinuation and side effects, comorbidities, chronotype, and demographic variables. The color scale represents the odds ratios of associations between these variables and treatment discontinuation. Blue color indicates an increased risk, whereas red color indicates a decreased risk (protective effect). *Nominally significant (p-value < 0·05) odds ratio. **Significant odds ratio after Bonferroni multiple testing correction.
Women showed higher odds of Mirtazapine discontinuation but not for other antidepressants (Fig. 1a). Divorced participants were more likely to discontinue SSRIs, including Sertraline, Escitalopram, and Citalopram. Further, participants who were never married were more likely to discontinue Citalopram and Duloxetine (Fig. 1b). Higher educational attainment was associated with lower discontinuation of SSRIs such as Citalopram, Escitalopram, Fluoxetine, and Sertraline. We observed a similar effect of high educational attainment on the discontinuation of SNRIs (Fig. 1b).
Participants who reported discontinuation were more likely to have taken antidepressants for less than three months. The proportion of participants who discontinued SSRIs and SNRIs due to side effects was similar across the time scales studied. For all antidepressants, at least 50% of all participants who did not report discontinuation due to side effects took that antidepressant for one year or more. Nonetheless, a sizable proportion of participants stopped taking treatment within a year (Table 2).
Side effects
We evaluated the influence of 23 participant-reported side effects on antidepressant treatment discontinuation (Additional file 1: Tables S1). Overall, agitation, vomiting, nausea, rashes, and suicidal thoughts were associated with higher discontinuation rates (Fig. 1b). Conversely, sweating was robustly associated with lower odds of Venlafaxine discontinuation, and nominal associations (p-value < 0.05) were observed for Sertraline and Duloxetine discontinuation (Fig. 1b). Weight gain and reduced sexual drive or function, which are the most common side effects in this sample, did not influence discontinuation rates. In addition, rashes were associated with the discontinuation of Venlafaxine or Sertraline. Treatment discontinuation involving other SNRIs showed nominal associations with rashes, as did some SSRIs such as Escitalopram and Fluoxetine (Fig. 1b).
Suicidal thoughts were associated with higher discontinuation rates for all SNRIs studied. For SSRIs, in contrast, only Sertraline, Escitalopram, and Fluoxetine discontinuation were associated with suicidal thoughts after multiple testing correction. Nonetheless, discontinuation for all other SSRIs showed nominally significant associations with suicidal thoughts, as did Mirtazapine. Suicide attempt was nominally associated with higher discontinuation of several SSRIs, namely, Citalopram, Escitalopram, and Sertraline, whereas for SNRIs, only Duloxetine showed a nominal association with suicide attempt (Fig. 1b).
Comorbidities and psychiatric traits
We evaluated whether psychiatric traits, such as participant-reported diagnoses of psychiatric disorders, neuroticism score, or chronotype measures, were associated with antidepressant treatment discontinuation (Additional file 1: Tables S1). Of the 18 mental health conditions assessed, we found that ADHD was nominally associated with higher odds of SSRIs discontinuation, including Citalopram and Sertraline, and the SNRI Venlafaxine (Fig. 1b). Furthermore, reported Post-Traumatic Stress Disorder (PTSD) was associated with higher odds of discontinuing treatment that included the SSRIs Sertraline, Escitalopram, or Fluoxetine, whereas for SNRIs, a strong association with treatment discontinuation was only observed for Venlafaxine (Fig. 1b). Discontinuation for other SSRIs and SNRIs was nominally associated with PTSD (Fig. 1b).
Bipolar disorder was nominally associated with higher odds of discontinuing SSRIs such as Sertraline and Escitalopram, as well as SNRIs such as Venlafaxine and Desvenlafaxine (Fig. 1b). Similarly, panic disorder showed nominal associations with higher odds of discontinuing SSRIs such as Citalopram, Escitalopram, and Fluoxetine, while for SNRIs, panic disorder was only nominally associated with Desvenlafaxine. Duloxetine discontinuation was nominally associated with bulimia, obsessive–compulsive disorder, and seasonal affective disorder (Fig. 1b). In addition, we observed nominal associations between Paroxetine discontinuation and hoarding disorder, premenstrual dysphoric mood disorder, and autism spectrum disorder. Neuroticism was associated with higher discontinuation rates across all antidepressants except Mirtazapine (Fig. 1b).
Discussion
The present study sought to provide an overview of the main variables influencing antidepressant treatment response by investigating which antidepressant side effects, comorbidities, and demographic characteristics were associated with the discontinuation of antidepressant treatment. The most common side effects, weight gain and sexual dysfunction, were not associated with higher discontinuation rates. Although commonly believed to be negative [14], these side effects showed nominal evidence of being protective against discontinuation for some antidepressants. This finding is in contrast to previous studies suggesting that weight gain and sexual dysfunction are often associated with premature discontinuation [15, 16]. The nominal protective effect of the side effects identified here may indicate that antidepressants are working, which in turn may increase the tolerability for undesired side effects. Weight increases may be induced by an improvement in appetite as symptoms ease. Furthermore, sexual dysfunction, particularly in males, may be explained through the known action of antidepressants on testosterone and dopamine regulation [17, 18].
Specific side effects such as rashes, nausea, vomiting, anxiety, agitation, and suicidality were associated with an increased risk for treatment discontinuation. Our findings are partially consistent with previous observations, which reported that suicidality, mania, rashes, and headaches were associated with discontinuation from clinical trials [12]. These results suggest at least two pathways to discontinuation: an intolerance or allergic component manifested as nausea, vomiting, and rashes, and a psychopathology-related component including anxiety and suicidality. Currently, it is challenging to establish whether the latter is explained by a lack of antidepressant effectiveness as opposed to undesired adverse effects.
Studies reporting the effect of divorce on mental health suggest that married individuals are more likely to respond positively to antidepressant treatment [19]. In addition, we found that individuals with high educational attainment are less likely to discontinue antidepressant treatment, which in turn supports evidence from previous genetic studies [20]. Matching our results, discontinuation is recognized as a concern for individuals diagnosed with ADHD and PTSD [21, 22]. For instance, previous studies report low antidepressant effectiveness among patients with comorbid ADHD [23] or PTSD [24]. It is important to distinguish that these associations are more challenging to interpret due to a lack of information on age at onset. This limitation is less likely to affect associations with ADHD as it is typically an early-onset condition; however, we cannot rule out the possibility of participants starting and stopping an antidepressant regime before developing PTSD or ADHD. In addition, we note that the spectral nature of psychiatric disorders [25, 26] may influence our results. For instance, a higher risk for discontinuation among individuals with ADHD and / or PTSD may be indicative of another psychiatric comorbidity, such as personality disorder. Future studies should aim to delineate further effects and interactions between specific psychiatric disorders and treatment discontinuation.
Some limitations need to be acknowledged. We note that the generalizability of our results must be addressed with caution until confirmed in samples from other populations and ethnicities. Retrospective participant-derived reports of side effects and discontinuation may be subject to recall bias and subjective interpretations of participants. Related to this is the lack of information on comorbidity age of onset. For example, although the association between anxiety as a side effect and discontinuation was stronger compared to anxiety as a previous diagnosis, we do not have sufficient data to assess whether participants who reported anxiety as a side effect had a previous diagnosis of anxiety disorder which could continue through and after treatment. Similarly, due to the nature of the available data, we are not able to know the magnitude of certain side effects such as weight gain. For instance, it may be possible that participants in AGDS experienced weight gain that was insignificant to them and decided to continue their treatment, which is subject to personal interpretations and tolerability. The relationship between discontinuation due to adverse side effects and due to lack of efficacy is complex since these constructs are not independent. A patient could experience severe side effects but high efficacy, potentially increasing the patient’s tolerability to the side effects. However, if a patient experiences low efficacy, it is possible that the patient’s tolerability to side effects will be much lower, increasing the odds of discontinuation. Future studies should aim to further explore the intricate association between tolerability, discontinuation due to adverse side effects, and discontinuation due to lack of efficacy, which was out of the scope of this study.
We note that patients who discontinued more than one drug were considered in analyses for all the drugs they discontinued. Therefore, the effect of individual vulnerabilities predisposing participants to discontinue treatment may be exacerbated. To prevent this, we analyzed discontinuation for each drug separately, avoiding the inclusion of repeated measures in any analysis. In addition, when investigating treatment response for any given antidepressant, we are not able to account for previously taken antidepressants. Due to the nature of our data, we cannot determine if a patient who discontinued treatment was taking any other antidepressants simultaneously. Thus, we cannot account for the potential effects of taking multiple antidepressants or previously taken ones. As an alternative approach to model monotherapy, we conducted our analyses only considering the first prescribed drug for each patient. Although the sample size for this analysis was substantially reduced, which was reflected as lower statistical power, the direction and magnitude of the observed effects is largely consistent with the full results (Additional file 2: Tables S2). Finally, we currently do not have detailed data on treatment regimes such as dosages, which would enable ruling out extremely high or low starting doses as explanations for certain side effects.
In summary, we sought to shed light on which side effects, comorbidities, and demographic factors could influence antidepressant treatment discontinuation. We observed that not all side effects contribute equally to treatment discontinuation. Side effects associated with higher odds of discontinuing treatment included anxiety, agitation, suicidal thoughts, vomiting, and rashes. We showed that participants who also reported comorbid ADHD, PTSD, and a high neuroticism score were at an increased risk for treatment discontinuation. Altogether, our results elucidate which factors could potentially determine antidepressant treatment discontinuation and suggest that discontinuation due to adverse side effects can occur at early and late stages of treatment. We argue that specific drug–factor interactions should be studied in detail to develop new medication recommendations based on demographics and early side effect reports. We suggest that future studies should seek to validate further our results, evaluate discontinuation in monotherapy, estimate the effect of dosages, test for interactions between variables identified here, and investigate the relationship between discontinuation due to side effects, lack of efficacy, and tolerability.
Availability of data and materials
Summary data on prevalence and effects described in this manuscript are available in the supplementary data. Individual-level data used for this article are restricted due to ethical considerations. Access to the dataset can be granted only after review and approval by the QIMR Berghofer Human and Research Ethics Committee as well as the studies’ principal investigators. Requests to access the datasets should be directed to Nicholas G. Martin at nick.martin@qimrberghofer.edu.au.
Abbreviations
- AGDS:
-
Australian genetics of depression study
- SNRI:
-
Serotonin and norepinephrine reuptake inhibitor
- SSRI:
-
Selective serotonin reuptake inhibitor
References
Mathers C, World Health Organization. The global burden of disease: 2004 Update. Geneva: World Health Organization; 2008.
Schweitzer I, Maguire K. Stopping antidepressants. Aust Prescr. 2001;24:13–5.
Khan A, Fahl Mar K, Faucett J, et al. Has the rising placebo response impacted antidepressant clinical trial outcome? Data from the US Food and Drug Administration 1987–2013. World Psychiatry. 2017;16:181–92.
Gabriel M, Sharma V. Antidepressant discontinuation syndrome. CMAJ. 2017;189:E747.
Campos AI, Mulcahy A, Thorp JG, et al. Understanding genetic risk factors for common side effects of antidepressant medications. MedRxiv. 2021. https://doi.org/10.1101/2021.07.12.21260397.
Cartwright C, Gibson K, Read J, et al. Long-term antidepressant use: patient perspectives of benefits and adverse effects. Patient Prefer Adherence. 2016;10:1401–7.
Bet PM, Hugtenburg JG, Penninx BWJH, Hoogendijk WJG. Side effects of antidepressants during long-term use in a naturalistic setting. Eur Neuropsychopharmacol. 2013;23:1443–51.
Machado M, Iskedjian M, Ruiz I, Einarson TR. Remission, dropouts, and adverse drug reaction rates in major depressive disorder: a meta-analysis of head-to-head trials. Curr Med Res Opin. 2006;22:1825–37.
Einarson TR, Arikian SR, Casciano J, Doyle JJ. Comparison of extended-release venlafaxine, selective serotonin reuptake inhibitors, and tricyclic antidepressants in the treatment of depression: a meta-analysis of randomized controlled trials. Clin Ther. 1999;21:296–308.
Anderson IM. SSRIS versus tricyclic antidepressants in depressed inpatients: a meta-analysis of efficacy and tolerability. Depress Anxiety. 1998;7(Suppl 1):11–7.
Pradier MF, McCoy TH Jr, Hughes M, et al. Predicting treatment dropout after antidepressant initiation. Transl Psychiatry. 2020;10:60.
Rohden AI, Benchaya MC, Camargo RS, et al. Dropout prevalence and associated factors in randomized clinical trials of adolescents treated for depression: systematic review and meta-analysis. Clin Ther. 2017;39:971-992.e4.
Byrne EM, Kirk KM, Medland SE, et al. Cohort profile: the Australian genetics of depression study. BMJ Open. 2020;10: e032580.
Donald M, Partanen R, Sharman L, et al. Long-term antidepressant use in general practice: a qualitative study of GPs’ views on discontinuation. Br J Gen Pract. 2021. https://doi.org/10.3399/BJGP.2020.0913.
Lee SH, Paz-Filho G, Mastronardi C, et al. Is increased antidepressant exposure a contributory factor to the obesity pandemic? Transl Psychiatry. 2016;6: e759.
Jing E, Straw-Wilson K. Sexual dysfunction in selective serotonin reuptake inhibitors (SSRIs) and potential solutions: a narrative literature review. Ment Health Clin. 2016;6:191–6.
Stahl SM. Mechanism of action of serotonin selective reuptake inhibitors. Serotonin receptors and pathways mediate therapeutic effects and side effects. J Affect Disord. 1998;51:215–35.
Safa M, Sadr S, Talischi F, Ghasem Boroujerdi F. Study of effects of selective serotonin reuptake inhibitors on stages of sexual function in Iranian patients with major depressive disorder. Ther Adv Psychopharmacol. 2013;3:306–13.
Gorwood P, Rouillon F, Even C, et al. Treatment response in major depression: effects of personality dysfunction and prior depression. Br J Psychiatry. 2010;196:139–42.
Pain O, Hodgson K, Trubetskoy V, et al. (2020) Antidepressant response in major depressive disorder: a genome-wide association study. MedRxiv. 2020;12(11):20245035.
Imel ZE, Laska K, Jakupcak M, Simpson TL. Meta-analysis of dropout in treatments for posttraumatic stress disorder. J Consult Clin Psychol. 2013;81:394–404.
Schneider BW, Gerdes AC, Haack LM, Lawton KE. Predicting treatment dropout in parent training interventions for families of school-aged children with ADHD. Child Fam Behav Ther. 2013;35:144–69.
Turgay A, Ansari R. Major Depression with ADHD. In Children and Adolescents Psychiatry. 2006;3:20–32.
Aga-Mizrachi S, Cymerblit-Sabba A, Gurman O, et al. Methylphenidate and desipramine combined treatment improves PTSD symptomatology in a rat model. Transl Psychiatry. 2014;4: e447.
García-Marín LM, Campos AI, Cuéllar-Partida G, et al. Large-scale genetic investigation reveals genetic liability to multiple complex traits influencing a higher risk of ADHD. Sci Rep. 2021;11:1–9.
Anttila V, Bulik-Sullivan B, Finucane HK, et al. Analysis of shared heritability in common disorders of the brain. Science. 2018. https://doi.org/10.1126/science.aap8757.
Acknowledgements
The authors thank our colleagues Richard Parker, Simone Cross, Scott Gordon, and Lenore Sullivan for their valuable work coordinating all the administrative and operational aspects of the AGDS project.
Funding
Data collection for AGDS was possible thanks to funding from the Australian National Health & Medical Research Council (NHMRC) to NGM, NRW, SEM, IHB, EMB, PAL (GNT1086683), and Medical Research Future Fund (APP1200644). LMGM and AIC are supported by UQ Research Training Scholarships from The University of Queensland (UQ). SEM is supported by NHMRC grants GNT1200644 and GNT1172917. The views expressed are those of the authors and not necessarily those of the affiliated or funding institutions.
Author information
Authors and Affiliations
Contributions
AIC, MER, and NGM conceived and directed the study. LMGM and AIC performed the statistical and bioinformatics analyses with support and input from NGM and MER. LMGM, AIC, and AM wrote the first draft of the paper and integrated input and feedback from all co-authors. NRW, EMB, SEM, NGM, and IBH designed and directed the AGDS data collection and funding. All the authors contributed to the interpretation of the results and provided feedback on the preliminary versions of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the QIMR Berghofer Human and Research Ethics Committee under project number P1218, and data were collected with the support and approval of the Australian Government Department of Human Services (DHS). Research conducted in the present study was performed in accordance with the Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
Professor Ian Hickie is the Co-Director, Health and Policy at the Brain and Mind Centre (BMC) University of Sydney, Australia. The BMC operates an early-intervention youth services at Camperdown under contract to headspace. Professor Hickie has previously led community-based and pharmaceutical industry-supported (Wyeth, Eli Lily, Servier, Pfizer, AstraZeneca) projects focused on the identification and better management of anxiety and depression. He is the Chief Scientific Advisor to, and a 5% equity shareholder in, InnoWell Pty Ltd. InnoWell was formed by the University of Sydney (45% equity) and PwC (Australia; 45% equity) to deliver the $30 M Australian Government-funded Project Synergy (2017–20) and to lead transformation of mental health services internationally through the use of innovative technologies. Adrian Campos is a current employee of Regeneron pharmaceuticals and may hold stock or stock options.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:
Tables S1. Summary statistics for all associations described in this study.
Additional file 2:
Tables S2. Summary statistics for associations described in this study only considering the first antidepressant taken as an approach to model monotherapy.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Garcia-Marin, L.M., Mulcahy, A., Byrne, E.M. et al. Discontinuation of antidepressant treatment: a retrospective cohort study on more than 20,000 participants. Ann Gen Psychiatry 22, 49 (2023). https://doi.org/10.1186/s12991-023-00480-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12991-023-00480-z