Abstract
Background
Nonalcoholic fatty liver disease (NAFLD) is the most prevalent chronic liver ailment worldwide, in which nonpharmacological strategies have a considerable role in the treatment. Probiotic supplementation as well as physical exercise can improve cardiometabolic parameters, but further research is needed to determine the effects of combined treatment versus exercise alone in managing NAFLD-associated biomarkers, primarily liver enzymes, lipid markers, and insulin resistance.
Objectives
This systematic review and meta-analysis aimed to evaluate the effects of probiotic supplementation, combined with exercise versus exercise alone, on liver enzymes and cardiometabolic markers in patients with NAFLD.
Methods
A systematic review and meta-analysis of randomized clinical trials was performed by searching PubMed, Scopus, and Web of Science databases up to April 2024. The search was restricted to articles published in the English language and human studies. Random effects models were used to calculate weighted mean differences (WMD).
Results
Pooled estimates (9 studies, 615 patients, intervention durations ranging from 8 to 48 weeks) revealed that probiotics plus exercise decreased aspartate transaminase (AST) [WMD=-5.64 U/L, p = 0.02], gamma-glutamyl transferase (GGT) [WMD=-7.09 U/L, p = 0.004], low-density lipoprotein (LDL) [WMD=-8.98 mg/dL, p = 0.03], total cholesterol (TC) [WMD=-16.97 mg/dL, p = 0.01], and homeostatic model assessment for insulin resistance (HOMA-IR) [WMD=-0.94, p = 0.005] significantly more than exercise only. However, probiotics plus exercise did not significantly change high-density lipoprotein (HDL) [WMD = 0.07 mg/dL, p = 0.9], fasting insulin [WMD=-1.47 µIU/mL, p = 0.4] or fasting blood glucose (FBG) [WMD=-1.57 mg/dL, p = 0.3] compared with exercise only. While not statistically significant, there were clinically relevant reductions in alanine aminotransferase (ALT) [WMD=-6.78 U/L, p = 0.1], triglycerides (TG) [WMD=-21.84 mg/dL, p = 0.1], and body weight (BW) [WMD=-1.45 kg, p = 0.5] for probiotics plus exercise compared with exercise only. The included studies exhibited significant heterogeneity for AST (I2 = 78.99%, p = 0.001), GGT (I2 = 73.87%, p = 0.004), LDL (I2 = 62.78%, p = 0.02), TC (I2 = 72.41%, p = 0.003), HOMA-IR (I2 = 93.86%, p = 0.001), HDL (I2 = 0.00%, p = 0.9), FBG (I2 = 66.30%, p = 0.01), ALT (I2 = 88.08%, p = 0.001), and TG (I2 = 85.46%, p = 0.001). There was no significant heterogeneity among the included studies for BW (I2 = 0.00%, p = 0.9).
Conclusion
Probiotic supplementation combined with exercise training elicited better results compared to exercise alone on liver enzymes, lipid profile, and insulin resistance in patients with NAFLD.
Systematic Review Registration
PROSPERO registration number CRD42023424290.
Similar content being viewed by others
Introduction
Nonalcoholic fatty liver disease (NAFLD) is the most common long-term liver condition globally [1, 2]. NAFLD is identified when individuals without a history of liver-damaging diseases or conditions, such as excessive alcohol consumption, medication use, hepatitis C virus infection, or starvation, exhibit an excess buildup of fat in the liver [1, 2]. The more advanced subtype implies progressive liver injury resulting in liver cirrhosis and hepatocellular carcinoma [1, 2]. The prevalence of NAFLD is increasing and currently affects about 32% of the world’s population [3]. Obesity is a risk factor for NAFLD, and obesity is now considered to be a pandemic, with obesity nearly tripling between 1975 and 2016 [4,5,6]. Thus, the necessity of effective interventions for the treatment of NAFLD is prominent in any healthcare system.
Lifestyle modifications such as dietary amelioration or engaging in more physical activity are regarded as the primary and most effective methods for preventing and treating NAFLD [2]. In addition, there is a major scientific effort proposing new dietary strategies against NAFLD [7,8,9,10,11]. In light of this, gut microbiota modulation has been deemed as a potential therapeutic option in the management of NAFLD and its related metabolic complications [4, 12].
Probiotics are living microorganisms that have been shown to play an important role in gut microbiota composition [13]. Specifically, several meta-analyses have demonstrated that probiotics have a notable role in decreasing the occurrence of NAFLD [14,15,16], as well as reducing fasting blood glucose (FBG), body weight (BW), insulin, total cholesterol (TC), low-density lipoprotein (LDL), triglycerides (TG), tumor necrosis factor-alpha, high-sensitivity C-reactive protein, alanine aminotransferase (ALT), and aspartate transaminase (AST) levels among patients with NAFLD [4]. In addition, umbrella meta-analyses have shown that probiotic supplementation can be considered a tool for improving obesity and glycemic parameters [17,18,19,20]. Nevertheless, existing evidence is inconsistent regarding the possible effects of probiotic supplementation in combination with exercise training on NAFLD-associated enzymes and cardiometabolic markers [21,22,23,24,25,26,27].
Taking into account the importance of drawing an overall conclusion for health professionals dealing with NAFLD (e.g., gastroenterologists, general practitioners, dietitians, and exercise physiologists), this current systematic review and meta-analysis was performed to evaluate the general effects of probiotic supplementation combined with exercise training, compared with exercise alone, on liver enzymes (ALT, AST, and gamma-glutamyl transferase (GGT) and cardiometabolic markers (lipid profile and insulin resistance) in individuals diagnosed with NAFLD.
Materials and methods
Trial registration
Systematic review and meta-analysis were carried out in accordance with the guidelines provided by the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) and followed the methodology outlined in the Cochrane Handbook of Systematic Reviews of Interventions. The project was registered in advance in the International Prospective Register of Systematic Reviews (PROSPERO; ID: CRD42023424290).
Search strategy
A thorough search of electronic databases including Web of Science, Scopus, and PubMed was conducted to identify relevant articles. Two reviewers (KH.M and B.K) independently screened and selected published articles up to April 2024. A comprehensive search was conducted using keywords such as “non-alcoholic fatty liver disease,” “nonalcoholic fatty liver disease,” “non-alcoholic fatty liver,” “nonalcoholic fatty liver,” “fatty liver disease,” “non-alcoholic steatohepatitis,” “NAFLD,” “fatty liver nonalcoholic,” “liver nonalcoholic fatty,” “nonalcoholic fatty liver,” “nonalcoholic fatty livers,” and “steatohepatitis,“. Additionally, specific terms related to probiotics such as “probiotics,” “synbiotics,” “lactobacillus,” “bifidobacterium,” and “streptococcus” were used to identify relevant studies. Similarly, terms related to exercise training including “exercise,” “training,” “exercise training,” and “physical activity” were employed in the search strategy. The search encompassed articles published up until April 2024. To identify any additional references that may have been overlooked in the initial electronic search, reference lists of all studies that met inclusion criteria were searched. The search was restricted to articles published in the English language and studies of human participants. There was no limit on the publication dates of the articles. The search strategies for the included databases are reported in Supplementary Table 1.
Eligibility criteria
Studies were eligible for inclusion if they met the following PICO (population, intervention, comparison, and outcome) criteria: (1) for population, studies that included human participants who were diagnosed with NAFLD; (2) for intervention, studies using probiotic supplements plus exercise; (3) for comparison, studies examining the effects of probiotic supplements plus exercise versus an exercise-only group; and (4) for outcomes, studies that reported liver enzymes (ALT, AST, and GGT), lipid profiles (LDL, HDL, TG, and TC), glycemic indices (fasting insulin, FBG, and homeostatic model assessment for insulin resistance (HOMA-IR)), and BW measured using a fully validated method.
Study selection
After eliminating duplicate records, the titles and abstracts of the remaining articles were evaluated independently by two reviewers (KH.M and B.K) to assess their relevance. Subsequently, the full texts of potentially eligible studies were thoroughly examined by the same reviewers to determine their eligibility for inclusion in the systematic review. In the event of any disagreements, resolutions were determined through discussions involving another author (F.K). The process of selecting studies was carried out independently by two reviewers (KH.M and B.K). The extracted study characteristics included the following: (A) participant details such as biological sex, age, body mass index (BMI), health status, and sample size; (B) exercise-related factors including training duration and frequency of sessions per week; (C) information regarding the type of probiotic used and the duration of the interventions in weeks; and (D) reported energy intake (kcal/day). The data extraction process was carried out by two authors (KH.M and B.K) with guidance from F.K. regarding the selection criteria. To analyze each outcome (ALT, AST, GGT, LDL, high-density lipoprotein (HDL), TG, TC, fasting insulin, FBG, HOMA-IR, and BW), the pre- and post-intervention means and standard deviations, or mean differences and their corresponding standard deviations, were extracted. These data were then utilized in the meta-analyses to generate forest plots. In cases where the means and standard deviations (SDs) were not explicitly provided, the SDs were calculated using alternative quantitative measures such as standard errors of means (SEM), medians and interquartile ranges (IQRs), or means and IQRs [28,29,30].
Quality evaluation and sensitivity analyses
The risk of bias was evaluated using the Physiotherapy Evidence Database (PEDro) scale to evaluate the quality of the included studies [31]. This scale consists of eleven items: (1) clear eligibility criteria, (2) randomized participant allocation, (3) concealed allocation, (4) baseline group similarity, (5) blinding of all participants, (6) blinding of all therapists, (7) blinding of all assessors, (8) evaluation of outcomes in at least 85% of participants, (9) intention-to-treat (ITT) analysis, (10) reporting of statistical comparisons between groups, inclusion of point measures and statistics of variability. These items are detailed in supplementary Table 1. Additionally, sensitivity analyses were conducted by excluding each study one by one to assess their individual impact on the overall results [32].
Statistical analyses
Meta-analyses were conducted using the Comprehensive Meta-analysis (CMA) software (version 2.0, Biostat Inc., NJ, USA). Weighted mean differences (WMD), and 95% confidence intervals (CIs) were calculated for variables that had the same measurement unit. Effect sizes were calculated to compare the effects of probiotic supplementation plus exercise training vs. exercise training only on liver enzymes (ALT, AST, and GGT), and metabolic outcomes (LDL, HDL, TG, TC, FBG, fasting insulin, HOMA-IR, and BW). Heterogeneity was evaluated by using the I2 statistic. Significance was set at p < 0.05. According to Cochrane guidelines, I2 statistics were interpreted as follows: 25% indicated low heterogeneity, 50% indicated moderate heterogeneity, and 75% indicated high heterogeneity. The results were combined using random-effects models due to the likelihood of heterogeneity arising from clinical or methodological factors that could potentially impact the outcomes [33]. Publication bias was evaluated using funnel plot interpretation with the Begg-Mazumdar Kendall’s tau, and Egger’s tests conducted as secondary tests when publication bias was detected. A p-value of less than 0.1 was considered indicative of significant publication bias [34]. Subgroup analyses were performed as follows: duration of the interventions included: low ≤ 12 h intervention, or high > 12 h intervention.
Results
Included studies
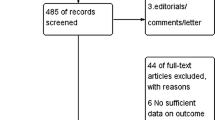
The initial search strategy identified 73 records from Web of Science, 73 records from Scopus, and 54 records from PubMed. Following the removal of duplicate records and screening of titles and abstracts, a total of 11 studies were identified for a more comprehensive evaluation of the full texts. Two animal model studies were excluded after reviewing full texts since we focused on human studies. Consequently, a total of 9 studies were included in the current systematic review and meta-analysis. Figure 1 displays the flow diagram illustrating the systematic literature search process.
Participant characteristics
The current meta-analysis included a total of 615 patients diagnosed with NAFLD, with sample sizes ranging from 39 [24] to 140 [23]. The mean ages ranged from 11.28 [26] to 57.38 [25] years, and the mean BMIs ranged from 26.00 [24] to 33.19 [25] kg/m², respectively. The majority of studies [21,22,23,24,25,26, 35, 36] included both males and females as participants. However, one study did not report the biological sex of the participants [37]. Participants in the included studies had varying health statuses, including NAFLD [21,22,23,24, 35], NAFLD with obesity [26, 27, 37], and NAFLD with type 2 diabetes mellitus (T2DM) [25]. The detailed participant characteristics are shown in Table 1.
Intervention characteristics
The majority of included studies used a probiotic capsule containing one or two different types of probiotic cultures [21,22,23,24,25,26,27, 37]. For all studies, the exercise-only control group used a placebo capsule. Intervention durations ranged from 8 [25] to 48 [24] weeks. The energy intakes ranged from 2117 ± 624 to 2388.8 ± 542.5 kcal/day in the probiotic plus exercise group, and from 2083 ± 539 to 2417.1 ± 706.5 kcal/day in the exercise group. The intervention characteristics are more fully described in Table 1.
The bacterial strains and doses in the probiotic supplements included 108 CFUs Bifidobacterium animalis [35]; Lactobacillus casei, Lactobacillus rhamnosus, Lactobacillus acidophilus, Bifidobacterium longum, and Bifidobacterium breve (16 g/d) [21, 22]; live combined Bifidobacterium, Lactobacillus, and Enterococcus powder (2 g/d) [23]; 109 CFUs of Lactobacillus salivarius, 109 CFUs Lactobacillus rhamnosus, and 8 × 109 CFU Bifidobacterium animalis [37]; Lactobacillus paracasei, Lactobacillus plantarum, Lactobacillus acidophilus, and Lactobacillus delbrueckii subsp [24]; 1 × 1010 CFU/g Bifidobacterium, 6 × 1010 CFU/g Lactobacillus + Lactococcus, 1 × 106 CFU/g Acetobacter, and 3 × 1010 CFU/g short-chain fatty acids producing Propionibacterium [25]; and Lactobacillus acidophilus (4.3 × 108 CFU/sachet), Lacticaseibacillus rhamnosus (4.3 × 108 CFU/sachet), Bifidobacterium bifidum (4.3 × 108 CFU/sachet), B. longum (4.3 × 108 CFU/ sachet), and Enterococcus faecium (8.2 × 108 CFU/sachet), total 2.5 × 109 CFU per sachet. [36].
The exercise protocols included aerobic exercises such as brisk walking, jogging, running, swimming, cycling, etc., with ≥ 30 min/session for 3–5 days/week [21, 23,24,25,26,27]. In other studies, exercise protocol details were not mentioned [22, 35, 37].
Meta-analysis
ALT
Based on 7 intervention arms, probiotics plus exercise did not decrease ALT significantly more than exercise training only [WMD = -6.78 U/L (95% CI -16.84 to 3.26), p = 0.1] (Fig. 2). Significant heterogeneity was observed among the included studies (I2 = 88.08%, p = 0.001). Visual examination of the funnel plots and the results of the Egger’s test (p = 0.9), and Begg-Mazumdar Kendall’s Tau (p = 1.0) did not indicate the presence of publication bias. Sensitivity analysis, conducted by excluding each study individually, revealed that removing the Rodrigo et al. [26] study resulted in an increase in the effect size and a statistically significant effect (WMD = -10.97 U/L, p = 0.01), while the direction of the results remained consistent.
Considering subgroup analyses for the duration of intervention, there was no significant change in ALT for > 12 h interventions [WMD= -5.07 U/L (95% CI -36.10 to 25.94, p = 0.7, 3 interventions] or for ≤ 12 h interventions [WMD=-8.02 U/L (95% CI -17.52 to 1.47), p = 0.09, 4 interventions], when compared with exercise only.
AST
Based on 7 intervention arms, probiotics plus exercise decreased AST significantly more than exercise training only [WMD = -5.64 U/L (95% CI -10.41 to -0.88), p = 0.02] (Fig. 3). There was significant heterogeneity among the included studies (I2 = 78.99%, p = 0.001). Visual interpretation of funnel plots and results of the Egger’s test (p = 0.6), and Begg-Mazumdar Kendall’s Tau (p = 1.0) did not show publication bias. The sensitivity analysis was conducted by excluding each study individually. When the Cai et al. [23] study was removed, there were small changes in the effect size and significance (WMD = -5.72 U/L, p = 0.05), but the overall direction of the results remained the same. Furthermore, when the Bakhshimoghaddam et al. [35] study was excluded, there was a decrease in the effect size and the result became non statistically significant (WMD=-4.57 U/L, p = 0.09), but the overall direction of the results remained unchanged. Also, when the Behrouz et al. [21] study was excluded, there were again decreases in the effect size that was now non-statistically significant (WMD = -3.86 U/L, p = 0.09), but the overall direction of the results remained the same.
Regarding subgroup analyses by the duration of intervention, probiotics plus exercise decreased AST significantly for ≤ 12 h interventions [WMD=-6.34 U/L (95% CI -12.65 to -0.04), p = 0.04, 4 interventions], but not for > 12 h interventions [WMD= -3.96 U/L (95% CI -14.48 to 6.55, p = 0.4, 3 interventions], when compared with exercise only.
GGT
Based on 5 intervention arms, probiotics plus exercise decreased GGT significantly more than exercise only [WMD= -7.09 U/L (95% CI -11.92 to -2.27), p = 0.004] (Fig. 4). The included studies exhibited significant heterogeneity (I2 = 73.87%, p = 0.004). Visual examination of funnel plots and the results of the Egger’s test (p = 0.3), and Begg-Mazumdar Kendall’s Tau (p = 0.4) indicated no evidence of publication bias.
Subgroup analyses according to the duration of the interventions, indicated thatprobiotics plus exercise decreased GGT significantly for ≤ 12 h interventions [WMD=-7.73 U/L (95% CI -14.21 to -1.25), p = 0.01, 3 interventions], but not for > 12 h interventions [WMD= -6.56 U/L (95% CI -17.57 to 4.41, p = 0.2, 2 interventions], when compared with exercise only.
LDL
Based on 6 intervention arms, probiotics plus exercise decreased LDL significantly more than exercise training only [WMD = -8.98 mg/dL (95% CI -17.24 to -0.71), p = 0.03] (Fig. 5). The included studies exhibited significant heterogeneity (I2 = 62.78%, p = 0.02). Visual examination of funnel plots and the results of the Egger’s test (p = 0.8), and Begg-Mazumdar Kendall’s Tau (p = 0.7) indicated no evidence of publication bias. The sensitivity analysis conducted by excluding each individual study revealed that removing the Cai et al. [23] study resulted in an increased effect size and changed the result such that it became non-statistically significant (WMD = -9.61 mg/dL, p = 0.1), but the overall direction of the results remained the same. Also, by removing the Kobyliak et al. [25] study, the effect size was increased slightly and the result became non-statistically significant (WMD = -9.07 mg/dL, p = 0.07), but the direction of the results did not change.
Subgroup analyses according to the duration of intervention, indicated that probiotics plus exercise decreased LDL significantly for ≤ 12 h interventions [WMD=-6.05 mg/dL (95% CI -11.39 to -0.71), p = 0.02, 4 interventions], but not for > 12 h interventions [WMD= -16.08 mg/dL (95% CI -40.87 to 8.71 p = 0.2, 2 interventions], when compared with exercise only.
HDL
Based on 6 intervention arms, probiotics plus exercise did not significantly increase HDL when compared with exercise only [WMD = 0.07 mg/dL (95% CI -1.75 to 1.93), p = 0.9] (Fig. 6). There was no significant heterogeneity found among the included studies (I2 = 0.00%, p = 0.9). The visual examination of funnel plots and the results of the Egger’s test (p = 0.3), and Begg-Mazumdar Kendall’s Tau (p = 0.4) indicated no evidence of publication bias. The sensitivity analysis conducted by excluding each individual study demonstrated that the effect size, significance, and direction of the results remained unchanged.
Subgroup analyses according to the duration of intervention, indicated that there was no significant change in HDL for > 12 h interventions [WMD = 0.12 mg/dL (95% CI -2.98 to 3.22, p = 0.9, 2 interventions] or for ≤ 12 h interventions [WMD = 0.05 mg/dL (95% CI -2.20 to 2.31), p = 0.9, 4 interventions], when compared with exercise only.
TG
Based on 6 intervention arms, probiotics plus exercise did not decrease TG significantly more than exercise only [WMD = -21.84 mg/dL (95% CI -53.05 to 9.36), p = 0.1] (Fig. 7). Considerable heterogeneity was observed among the included studies (I2 = 85.46%, p = 0.001). Based on the visual analysis of funnel plots and the findings from the Egger’s test (p = 0.5), and Begg-Mazumdar Kendall’s Tau (p = 0.4), there was no sign of publication bias. The sensitivity analysis conducted by excluding each individual study demonstrated that the effect size, significance, and direction of the results remained unchanged.
Concerning subgroup analyses by the duration of intervention, there was no significant change in TG for > 12 h interventions [WMD= -33.17 mg/dL (95% CI -125.30 to 58.96, p = 0.4, 2 interventions] or for ≤ 12 h interventions [WMD=-15.96 mg/dL (95% CI -45.23 to 13.30), p = 0.2, 4 interventions], when compared with exercise only.
TC
Based on 6 intervention arms, probiotics plus exercise decreased TC significantly more than exercise training only [WMD=-16.97 mg/dL (95% CI -29.85 to -4.09), p = 0.01] (Fig. 8). A high degree of heterogeneity was observed in the included studies (I2 = 72.41%, p = 0.003). Absence of publication bias was suggested by the visual examination of funnel plots and the outcomes of the Egger’s test (p = 0.7), and Begg-Mazumdar Kendall’s Tau (p = 1.0). When conducting sensitivity analysis by excluding each individual study, removing the Cai et al. 2020 study resulted in minor changes to the effect size and significance (WMD = -15.29 mg/dL, p = 0.06), but the overall direction of the results remained the same.
For subgroup analyses by the duration of intervention, probiotics plus exercise decreased TC significantly for ≤ 12 h interventions [WMD=-12.68 mg/dL (95% CI -24.33 to -1.02), p = 0.03, 4 interventions], but not for > 12 h interventions [WMD= -27.02 mg/dL (95% CI -64.75 to 10.69 p = 0.1, 2 interventions], when compared with exercise only.
Fasting insulin
Based on 4 intervention arms, probiotics plus exercise did not decrease fasting insulin significantly more than exercise training only [WMD = -1.47 µIU/mL (95% CI -5.42 to 2.48), p = 0.4] (Supplementary Fig. 1). The included studies demonstrated marked heterogeneity (I2 = 81.32%, p = 0.001). Visual interpretation of funnel plots and the Egger’s test (p = 0.2), and Begg-Mazumdar Kendall’s Tau (p = 0.7) results also did not show publication bias. By omitting each individual study in a sensitivity analysis, there were no alterations in effect size or significance of results, and the direction of the results did not change.
For subgroup analyses by the duration of intervention, there was no significant change in fasting insulin for > 12 h interventions [WMD= -2.27 µIU/mL (95% CI -7.09 to 2.54, p = 0.3, 2 interventions] or for ≤ 12 h interventions [WMD=-0.46 µIU/mL (95% CI -8.91 to 7.99), p = 0.9, 2 interventions], when compared with exercise only.
FBG
Based on 6 intervention arms, probiotics plus exercise did not decrease FBG more than exercise training only [WMD = -1.57 mg/dL (95% CI -4.86 to 1.71), p = 0.3] (Supplementary Fig. 1). A high degree of heterogeneity was observed in the included studies (I2 = 66.30%, p = 0.01). Visual interpretation of funnel plots and the Egger’s test (p = 0.6), and Begg-Mazumdar Kendall’s Tau (p = 1.0) results also did not show publication bias. Through a sensitivity analysis where each individual study was excluded from consideration, there were no changes in the effect size or significance of results, and the direction of the results did not change.
Subgroup analyses according to the duration of intervention, indicated that there was no significant change in FBG for > 12 h interventions [WMD= -4.06 mg/dL (95% CI -12.35 to 4.21 p = 0.3, 2 interventions] or for ≤ 12 h interventions [WMD=-0.05 mg/dL (95% CI -2.27 to 2.17), p = 0.9, 4 interventions], when compared with exercise only.
HOMA-IR
Based on 4 intervention arms, probiotics plus exercise decreased HOMA-IR significantly more than exercise training only [WMD=-0.94 (95% CI -1.61 to -0.28), p = 0.005] (Supplementary Fig. 1). There was significant heterogeneity among the included studies (I2 = 93.86%, p = 0.001). Visual interpretation of funnel plots and results of the Egger’s test (p = 0.9), and Begg-Mazumdar Kendall’s Tau (p = 1.0) did not suggest publication bias. By excluding the Behrouz et al. 2017 study during sensitivity analysis, the effect size was reduced and the result became non-statistically significant (WMD = -1.1, p = 0.06), but direction of the overall findings remained consistent. Furthermore, when the Cai et al. 2020 study was excluded, there were similar alterations in the effect size and significance (WMD = -1.2, p = 0.07), with consistent findings overall.
Due to the small number of studies for HOMA-IR, subgroup analyses were not performed.
Body weight
Based on 3 intervention arms, probiotics plus exercise did not decrease body weight significantly more than exercise training only [WMD = -1.45 kg (95% CI -6.36 to 3.46), p = 0.5] (Supplementary Fig. 1). There was a lack of notable heterogeneity among the included studies (I2 = 0.00%, p = 0.9). Visual interpretation of funnel plots and results of the Egger’s test (p = 0.9), and Begg-Mazumdar Kendall’s Tau (p = 1.0) did not suggest publication bias. The sensitivity analysis, where each study was systematically removed, demonstrated that the effect size, significance of results, and direction of the findings remained constant.
Subgroup analyses were not performed due to the small number of studies for BW.
Quality assessment
The PEDro tool was used to assess the methodological quality of each study, with scores ranging from 5 to 11 out of a maximum of 11 points. One study scored 10 [26], one study scored 9 [24], five studies scored 8 [21, 22, 25, 27, 35], one study achieved a score of 7 (28), and one study scored 6 (12). Most of the study scores were lowered due to three items (concealed allocation, blinding of all therapists, and intention-to-treat analysis). Additional information regarding the quality of the studies can be found in Supplementary Table 1.
Discussion
Overall, this systematic review and meta-analysis of 9 RCTs involving patients with NAFLD, revealed that probiotic supplementation combined with exercise improved liver enzymes, lipid profiles, and insulin resistance compared with exercise training alone. More specifically, probiotics plus exercise significantly decreased AST [WMD=-5.64 U/L, p = 0.02], GGT [WMD = -7.09 U/L, p = 0.004], LDL [WMD = -8.98 mg/dL, p = 0.03], TC [WMD = -16.97 mg/dL, p = 0.01], and HOMA-IR [WMD = -0.94, p = 0.005], while there were non-statistically significant but potentially clinically relevant reductions in ALT [WMD = -6.78 U/L, p = 0.1], TG [WMD = -21.84, p = 0.1], and body weight [WMD = -1.45 kg, p = 0.5]. In contrast, probiotics plus exercise did not significantly change HDL [WMD = 0.07 mg/dL, p = 0.9], fasting insulin [WMD = -1.47 µIU/mL, p = 0.4], or FBG [WMD = -1.57 mg/dL, p = 0.3] when compared with exercise only, and these values are not likely to be clinically meaningful.
Our findings are in line with a recently published meta-analysis from 2023, involving 21 RCTs, that also demonstrated notable regulatory effects of probiotic supplementation on ALT, AST, GGT, steatosis, FBG, insulin, and blood lipid levels in individuals with NAFLD (7). Moreover, a previous meta-analysis of 28 RCTs reported positive effects of probiotic supplementation on body mass index, ALT, AST, GGT, insulin, HOMA-IR, and TC in patients with NAFLD [38]. Regarding exercise training, a prior meta-analysis comprising 16 studies revealed a favorable impact of exercise alone, without any dietary intervention, on reducing liver fat, ALT, and AST, as well as BW in individuals with NAFLD [39]. Another meta-analysis of 11 RCTs showed that exercise improved intrahepatic lipid and ALT levels in patients with NAFLD, and the effects of exercise were retained for more than 3 months [40]. In a systematic review and meta-analysis of 21 RCTs investigating the efficacy of exercise for improving indices related to NAFLD, 3 studies assessed the effects of exercise combined with probiotic supplementation and observed better efficacy in reducing ALT, AST, TG, and TC levels compared to exercise alone [41]. While this latter meta-analysis included studies through December 2021 and comprised 3 studies, the current meta-analysis was updated through April 2024 including triple (9 studies) the number of studies.
Mechanistically, the development of gut dysbiosis associated with NAFLD represents a cluster of metabolic dysfunctions such as (1) the prevention of fasting-induced adipocyte factor, which normally stimulates the activity of lipoprotein lipase and promotes lipogenesis; (2) an increase in lipopolysaccharides, leading to inflammation and liver damage through the activation of the NF-kB pathway; (3) an increase in polysaccharide absorption, resulting in the production of short-chain fatty acids and hepatic lipogenesis; and (4) the conversion of choline into methylamines, which reduces choline availability and leads to fat accumulation and the production of reactive oxygen species in the liver [4, 42,43,44]. Dysbiosis can also enhance the permeability of the gut wall, enabling the translocation of bacteria and the uptake of endotoxins, and hence contributes to the development of metabolic dysfunction in NAFLD, whereas probiotic supplementation can mitigate these effects [4, 42,43,44]. Interestingly, probiotic supplementation can activate genes involved in fatty acid oxidation, thereby delaying NAFLD progression through the lipopolysaccharides/toll-like receptor 4 signaling pathway [4, 42,43,44].
In addition to probiotic supplementation, the interaction of the gut microbiota with exercise may exert different effects on NAFLD, since the gut microbiota acts as an endocrine organ and is sensitive to several environmental conditions [45]. A bidirectional relationship between exercise and gut microbiota composition has been highlighted, whereby exercise can enhance the variety of microbiota positively impacting metabolic health, while the composition of gut microbiota can influence adaptation to exercise by modulating factors such as inflammation, oxidative stress, energy balance, intestinal barrier integrity, nutrient absorption, gas production, gastrointestinal motility, and immune modulation [45, 46]. Furthermore, combining probiotics with exercise can serve as an enhanced approach to stimulate the antioxidant defense system and reduce the risk factors associated with certain NAFLD-related cardiovascular diseases [47].
Based on the current meta-analysis, the dosing regimens of probiotic supplementation varied between one strain of Bifidobacterium (Bifidobacterium animalis) and nine strains of Lactobacillus (Lactobacillus salivarius, Lactobacillus rhamnosus, Lactobacillus plantarum, Lactobacillus paracasei, Lactobacillus delbrueckii subsp, Lactobacillus acidophilus, Lactobacillus acidophilus, and Lacticaseibacillus) for 12–48 weeks. However, further research is of pivotal importance in optimizing bacterial strains, doses, and supplementation durations. It is certainly plausible that other combinations of probiotic strains may have differential effects on liver enzymes and cardiometabolic outcomes in patients with NAFLD.
It is worth mentioning that there is a specific caution regarding the use of probiotics in populations at risk, including individuals with compromised immune function, elderly individuals, newborns (especially preterm infants), pregnant women who have mild to morbid obesity, and individuals with certain medical conditions such as life-threatening pneumonia, endocarditis, and sepsis [36]. Furthermore, probiotic supplementation may not be a suitable choice in cases where there are anatomical changes caused by surgical procedures, such as short bowel syndrome, or bariatric surgery [36].
The strengths and limitations of this systematic review and meta-analysis must be discussed. To the best of our knowledge, this is the most comprehensive meta-analysis addressing the effects of probiotic supplementation in concert with exercise in patients with NAFLD. Although meta-analyses of RCTs are at the top of the evidence hierarchy, intrinsic clinical limitations are conceivable due to particular differences between studies that cannot be fully controlled. These differences may be due to differences in (1) probiotic strains, quality of supplements, prior probiotic intake, and study duration [4]; (2) dietary intake and medication control [48,49,50]; (3) lifestyle behaviors and other participant sociodemographic factors [51]; (4) and differences in genetic factors [52], all of which could modify the responses to a specific intervention. The intensity, timing, and type of exercise may also affect the outcomes of an exercise intervention [45, 53]. To further elucidate the potential for additive or synergistic effects when combining probiotic supplementation with exercise, long-term and well-controlled RCTs with sufficient power are needed not only in laboratory markers but also for primary medical outcomes in individuals with NAFLD. Lastly, it is necessary to evaluate the cost-effectiveness of probiotic supplementation in a real-life setting.
Conclusion
Probiotic supplementation combined with exercise training improved liver enzymes, lipid markers, and insulin resistance compared with exercise training alone in patients with NAFLD. More specifically, probiotics plus exercise significantly decreased AST, GGT, LDL, TC, and HOMA-IR when compared with exercise alone. Several of these effects were clinically modest; however, such a combination deserves attention in research and practice as a safe and effective non-pharmacological approach to partially mitigate alterations in liver enzymes and traditional cardiometabolic markers in NAFLD.
Data availability
No datasets were generated or analysed during the current study.
References
Loomba R, Friedman SL, Shulman GI. Mechanisms and disease consequences of nonalcoholic fatty liver disease. Cell. 2021;184:2537–64.
Buzzetti E, Linden A, Best LM, Madden AM, Roberts D, Chase TJG, Freeman SC, Cooper NJ, Sutton AJ, Fritche D, et al. Lifestyle modifications for nonalcohol-related fatty liver disease: a network meta-analysis. Cochrane Database Syst Rev. 2021;6:Cd013156.
Riazi K, Azhari H, Charette JH, Underwood FE, King JA, Afshar EE, Swain MG, Congly SE, Kaplan GG, Shaheen A-A. The prevalence and incidence of NAFLD worldwide: a systematic review and meta-analysis. The lancet gastroenterology & hepatology; 2022.
Hadi A, Mohammadi H, Miraghajani M, Ghaedi E. Efficacy of synbiotic supplementation in patients with nonalcoholic fatty liver disease: a systematic review and meta-analysis of clinical trials: synbiotic supplementation and NAFLD. Crit Rev Food Sci Nutr. 2019;59:2494–505.
Hepatology TLG. Obesity: another ongoing pandemic. vol. 6. pp. 4112021:411.
Luo Y, Lin H. Inflammation initiates a vicious cycle between obesity and nonalcoholic fatty liver disease. Immun Inflamm Dis. 2021;9:59–73.
Kord-Varkaneh H, Salehi-Sahlabadi A, Tinsley GM, Santos HO, Hekmatdoost A. Effects of time-restricted feeding (16/8) combined with a low-sugar diet on the management of non-alcoholic fatty liver disease: a randomized controlled trial. Nutrition. 2023;105:111847.
Khodami B, Hatami B, Yari Z, Alavian SM, Sadeghi A, Varkaneh HK, Santos HO, Hekmatdoost A. Effects of a low free sugar diet on the management of nonalcoholic fatty liver disease: a randomized clinical trial. Eur J Clin Nutr. 2022;76:987–94.
Santos HO, Bueno AA, Mota JF. The effect of artichoke on lipid profile: a review of possible mechanisms of action. Pharmacol Res. 2018;137:170–8.
Kord Varkaneh H, Găman M-A, Rajabnia M, Sedanur Macit-Çelebi M, Santos HO, Hekmatdoost A. Effects of the 5: 2 intermittent fasting diet on non-alcoholic fatty liver disease: a randomized controlled trial. Front Nutr. 2022;9:948655.
Santos HO, Price JC, Bueno AA. Beyond fish oil supplementation: the effects of alternative plant sources of omega-3 polyunsaturated fatty acids upon lipid indexes and cardiometabolic biomarkers—an overview. Nutrients. 2020;12:3159.
Aron-Wisnewsky J, Vigliotti C, Witjes J, Le P, Holleboom AG, Verheij J, Nieuwdorp M, Clément K. Gut microbiota and human NAFLD: disentangling microbial signatures from metabolic disorders. Nat Reviews Gastroenterol Hepatol. 2020;17:279–97.
Miraghajani M, Zaghian N, Mirlohi M, Ghiasvand R. Probiotic soy milk consumption and renal function among type 2 Diabetic patients with Nephropathy: a Randomized Controlled Clinical Trial. Probiotics Antimicrob Proteins 2017:1–9.
Zhou X, Wang J, Zhou S, Liao J, Ye Z, Mao L. Efficacy of probiotics on nonalcoholic fatty liver disease: a meta-analysis. Med (Baltim). 2023;102:e32734.
Tang Y, Huang J, Zhang WY, Qin S, Yang YX, Ren H, Yang Q-b, Hu H. Effects of probiotics on nonalcoholic fatty liver disease: a systematic review and meta-analysis. Therapeutic Adv Gastroenterol. 2019;12:1756284819878046.
Jin H, Xu X, Pang B, Yang R, Sun H, Jiang C, Shao D, Shi J. Probiotic and prebiotic interventions for non-alcoholic fatty liver disease: a systematic review and network meta-analysis. Beneficial Microbes. 2021;12:517–29.
Musazadeh V, Zarezadeh M, Ghalichi F, Ahrabi SS, Jamilian P, Jamilian P, Ghoreishi Z. Anti-obesity properties of probiotics; a considerable medical nutrition intervention: findings from an umbrella meta-analysis. Eur J Pharmacol. 2022;928:175069.
Zarezadeh M, Musazadeh V, Faghfouri AH, Sarmadi B, Jamilian P, Jamilian P, Tutunchi H, Dehghan P. Probiotic therapy, a novel and efficient adjuvant approach to improve glycemic status: an umbrella meta-analysis. Pharmacol Res. 2022;183:106397.
Musazadeh V, Roshanravan N, Dehghan P, Ahrabi SS. Effect of probiotics on liver enzymes in patients with non-alcoholic fatty liver disease: an umbrella of systematic review and meta-analysis. Front Nutr. 2022;9:844242.
Zarezadeh M, Musazadeh V, Faghfouri AH, Roshanravan N, Dehghan P. Probiotics act as a potent intervention in improving lipid profile: an umbrella systematic review and meta-analysis. Crit Rev Food Sci Nutr. 2022;63:145–58.
Behrouz V, Aryaeian N, Zahedi MJ, Jazayeri S. Effects of probiotic and prebiotic supplementation on metabolic parameters, liver aminotransferases, and systemic inflammation in nonalcoholic fatty liver disease: a randomized clinical trial. J Food Sci. 2020;85:3611–7.
Behrouz V, Jazayeri S, Aryaeian N, Zahedi MJ, Hosseini F. Effects of Probiotic and Prebiotic Supplementation on Leptin, Adiponectin, and glycemic parameters in non-alcoholic fatty liver disease: a Randomized Clinical Trial. Middle East J Dig Dis. 2017;9:151–9.
Cai GS, Su H, Zhang J. Protective effect of probiotics in patients with non-alcoholic fatty liver disease. Medicine 2020, 99.
Duseja A, Acharya SK, Mehta M, Chhabra S, Shalimar, Rana S, Das A, Dattagupta S, Dhiman RK, Chawla YK. High potency multistrain probiotic improves liver histology in non-alcoholic fatty liver disease (NAFLD): a randomised, double-blind, proof of concept study. Bmj Open Gastroenterol 2019, 6.
Kobyliak N, Abenavoli L, Mykhalchyshyn G, Falalyeyeva T, Tsyryuk O, Kononenko L, Kyriienko D, Komisarenko I. Probiotics and smectite absorbent gel formulation reduce liver stiffness, transaminase and cytokine levels in NAFLD associated with type 2 diabetes: a randomized clinical study. Clin Diabetol. 2019;8:205–14.
Rodrigo T, Dulani S, Seneviratne SN, De Silva AP, Fernando J, De Silva HJ, Jayasekera, Wickramasinghe VP. Effects of probiotics combined with dietary and lifestyle modification on clinical, biochemical, and radiological parameters in obese children with nonalcoholic fatty liver disease/nonalcoholic steatohepatitis: a randomized clinical trial. Clin Experimental Pediatr. 2022;65:304–11.
Kilic Yildirim G, Dinleyici M, Vandenplas Y, Dinleyici EC. Effects of multispecies Synbiotic supplementation on anthropometric measurements, glucose and lipid parameters in children with exogenous obesity: a Randomized, double blind, placebo-controlled clinical trial (Probesity-2 trial). Front Nutr 2022, 9.
Wan X, Wang W, Liu J, Tong T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol. 2014;14:1–13.
Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol. 2005;5:1–10.
Higgins JP, Green S. Cochrane handbook for systematic reviews of interventions. 2008.
De Morton NA. The PEDro scale is a valid measure of the methodological quality of clinical trials: a demographic study. Australian J Physiotherapy. 2009;55:129–33.
Copas J, Shi JQ. Meta-analysis, funnel plots and sensitivity analysis. Biostatistics. 2000;1:247–62.
Tufanaru C, Munn Z, Stephenson M, Aromataris E. Fixed or random effects meta-analysis? Common methodological issues in systematic reviews of effectiveness. JBI Evid Implement. 2015;13:196–207.
Egger M, Smith GD, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–34.
Bakhshimoghaddam F, Shateri K, Sina M, Hashemian M, Alizadeh M. Daily consumption of synbiotic yogurt decreases liver steatosis in patients with nonalcoholic fatty liver disease: a randomized controlled clinical trial. J Nutr. 2018;148:1276–84.
Kilic Yildirim G, Dinleyici M, Vandenplas Y, Dinleyici EC. Effects of multispecies Synbiotic supplementation on anthropometric measurements, glucose and lipid parameters in children with exogenous obesity: a Randomized, double blind, placebo-controlled clinical trial (Probesity-2 trial). Front Nutr. 2022;9:898037.
Chen AC, Fang TJ, Ho HH, Chen JF, Kuo YW, Huang YY, Tsai SY, Wu SF, Lin HC, Yeh YT. A multi-strain probiotic blend reshaped obesity-related gut dysbiosis and improved lipid metabolism in obese children. Front Nutr 2022, 9.
Xiao M-W, Lin S-X, Shen Z-H, Luo W-W, Wang X-Y. Systematic Review with Meta-Analysis: The Effects of Probiotics in Nonalcoholic Fatty Liver Disease. Gastroenterology Research and Practice 2019, 2019:1484598.
Baker CJ, Martinez-Huenchullan SF, D’Souza M, Xu Y, Li M, Bi Y, Johnson NA, Twigg SM. Effect of exercise on hepatic steatosis: are benefits seen without dietary intervention? A systematic review and meta‐analysis. J Diabetes. 2021;13:63–77.
Nam H, Yoo J-J, Cho Y, Kang SH, Ahn SB, Lee H-W, Jun DW, Choi M. Effect of exercise-based interventions in nonalcoholic fatty liver disease: a systematic review with meta-analysis. Dig Liver Disease 2023.
Yu X, Wang Y, Lai J, Song T, Duan J. Comparative efficacy of exercise training processes in improving nonalcoholic fatty liver disease: a systematic review and meta-analysis. Ir J Med Sci (1971-). 2023;192:131–42.
Woodhouse C, Patel V, Singanayagam A, Shawcross D. The gut microbiome as a therapeutic target in the pathogenesis and treatment of chronic liver disease. Aliment Pharmacol Ther. 2018;47:192–202.
Song Q, Zhang X. The role of gut–liver axis in gut microbiome dysbiosis associated NAFLD and NAFLD-HCC. Biomedicines. 2022;10:524.
Ma J, Zhou Q, Li H. Gut microbiota and nonalcoholic fatty liver disease: insights on mechanisms and therapy. Nutrients. 2017;9:1124.
Donati Zeppa S, Agostini D, Gervasi M, Annibalini G, Amatori S, Ferrini F, Sisti D, Piccoli G, Barbieri E, Sestili P. Mutual interactions among exercise, sport supplements and microbiota. Nutrients. 2019;12:17.
Hughes RL, Holscher HD. Fueling gut microbes: a review of the interaction between diet, exercise, and the gut microbiota in athletes. Adv Nutr. 2021;12:2190–215.
Maherinia H, Peeri M, Azarbayjani M, Delfan M. Aerobic exercise training combined with probiotic supplement improves antioxidant defence of cardiomyocytes by regulating Nrf2 and caspase3 gene expression in type 2 diabetic rats. Comp Exerc Physiol. 2022;18:255–63.
Ávalos Y, Kerr B, Maliqueo M, Dorfman M. Cell and molecular mechanisms behind diet-induced hypothalamic inflammation and obesity. J Neuroendocrinol. 2018;30:e12598.
Goldenberg JZ, Day A, Brinkworth GD, Sato J, Yamada S, Jönsson T, Beardsley J, Johnson JA, Thabane L, Johnston BC. Efficacy and safety of low and very low carbohydrate diets for type 2 diabetes remission: systematic review and meta-analysis of published and unpublished randomized trial data. bmj 2021, 372.
Tosti V, Bertozzi B, Fontana L. Health benefits of the Mediterranean diet: metabolic and molecular mechanisms. Journals Gerontology: Ser A. 2018;73:318–26.
Pirkola J, Vääräsmäki M, Ala-Korpela M, Bloigu A, Canoy D, Hartikainen A-L, Leinonen M, Miettola S, Paldanius M, Tammelin TH. Low-grade, systemic inflammation in adolescents: association with early-life factors, gender, and lifestyle. Am J Epidemiol. 2009;171:72–82.
Stenvinkel P, Pecoits-Filho R, Lindholm B. Gene polymorphism association studies in dialysis: the nutrition-inflammation axis. In Seminars in dialysis. 2005:322–30.
Xiong Y, Peng Q, Cao C, Xu Z, Zhang B. Effect of different exercise methods on non-alcoholic fatty liver disease: a meta-analysis and meta-regression. Int J Environ Res Public Health. 2021;18:3242.
Chen A-C, Fang T-J, Ho H-H, Chen J-F, Kuo Y-W, Huang Y-Y, Tsai S-Y, Wu S-F, Lin H-C, Yeh Y-T. A multi-strain probiotic blend reshaped obesity-related gut dysbiosis and improved lipid metabolism in obese children. Front Nutr. 2022;9:922993.
Funding
No particular grant or external funding was allocated to support this research.
Author information
Authors and Affiliations
Contributions
The study was conceived and designed by FK, MM, S.RK, H.OS. Data extraction was performed by BK and KH.M. The data were analyzed by FK, who also completed the initial draft of the results. The initial manuscript was drafted by FK and MM. The manuscript was revised by S.RK and Heitor Santos. Finally, FK, MM, S.RK, and H.OS reviewed and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it.The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Kazeminasab, F., Miraghajani, M., Mokhtari, K. et al. The effects of probiotic supplementation and exercise training on liver enzymes and cardiometabolic markers in patients with non-alcoholic fatty liver disease: a systematic review and meta-analysis of randomized clinical trials. Nutr Metab (Lond) 21, 59 (2024). https://doi.org/10.1186/s12986-024-00826-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12986-024-00826-8