Abstract
Background
The risk of cardiovascular diseases has rapidly increased among middle-aged and elderly. However, little is known about the relationship of body composition changes with the risk of cardiovascular events among this population in China. We explored the associations of 2-year changes in fat percentage (fat%) and fat-free mass percentage (FFM%) with subsequent cardiovascular events in a middle-aged and elderly community-based cohort.
Methods
This study included 1048 participants (456 men [43.51%], aged 50–80 years) without overt cardiovascular disease, who underwent two examinations during 2013–2014 and 2015–2016. All participants were followed up until 2022 for cardiovascular events. A bioelectrical impedance analyzer was used to calculate fat% and FFM% change.
Results
At baseline, the median body mass index (BMI), fat%, and FFM% were 23.9 (22.1–25.9) kg/m2, 27.2 (20.8–33.6)%, and 72.8 (66.4–79.2)%, respectively. Two-year changes in fat% and FFM% were 0.31 (− 5.53 to 6.87)% and − 0.12 (− 2.36 to 2.06)%. During an average follow-up of 5.5 years, 86 cardiovascular events (8.21%) occurred. Cox regression models showed that hazard ratios (HRs) of every 2% change in fat% and FFM% for cardiovascular events were 1.04 (95% confidence interval [CI] 1.01–1.07) and 0.84 (95% CI 0.74–0.95), respectively. Compared with participants with stable fat% (–2% ≤ ⊿fat% < 2%), those with fat% gain ≥ 2% had an increased risk of cardiovascular events (HR 2.07, 95% CI 1.08–3.97). FFM% loss > 8% was associated with a higher risk of cardiovascular events (HR 3.83, 95% CI 1.29–11.4).
Conclusions
In a middle-aged and elderly community-based Chinese population, fat% gain or FFM% loss was associated with an increased risk of cardiovascular events.
Similar content being viewed by others
Background
Obesity is a major global public health concern. According to data from the World Health Organization (2021), the global prevalence of obesity has nearly tripled since 1975 [1]. As the prevalence of obesity continues to rise, the burden of obesity-related comorbidities, especially cardiovascular diseases (CVD), also increases [2, 3]. Body mass index (BMI) is the most widely used index to assess adiposity; however, recent studies have found that individuals with a normal BMI may still be at a high risk for CVD [4]. One possible reason for this may be due to its limited ability to distinguish between fat mass (FM) and fat-free mass (FFM) (mainly skeletal muscle). Thus, the association between body composition and cardiovascular events has attracted considerable attention. Medina-Inojosa et al. reported that among 717 patients with coronary artery disease, the risk of cardiovascular events for those in the highest quartile of fat percentage (fat%) was nearly twice compared with that of the patients in the lowest quartile after a median follow-up of 3.9 years. Conversely, the risk for those in the highest quartile of FFM was 47% lower than that of the patients in the lowest quartile. No association was observed between BMI and cardiovascular events [5]. Another cohort study involving 10,251 diabetic patients demonstrated that after a mean follow-up of 8.8 years, participants in the fourth quartile of the FM index were associated with a 53% increased risk of cardiovascular events compared with those in the first quartile, whereas no significant association was observed between the FFM index and cardiovascular events [6]. Therefore, assessing the role of FM and FFM in the development of CVD may yield new insights into clinical practice. However, most existing studies were somehow limited by single baseline assessment or nonconcurrent measurement at follow-up.
Recent studies have focused on the association between body composition changes and incident CVD. A study involving 5103 patients with type 2 diabetes demonstrated that the decline in FM, but not FFM, was associated with a lower risk of heart failure [7]. However, another type 2 diabetes cohort did not show any significant association of changes in FM and FFM with cardiovascular events [8]. Evidence from participants aged 20–39 years in Korea supported the association of FM and FFM change with cardiovascular events [9]. Nevertheless, there is still a lack of community-based studies in China.
As the risk of high CVD accelerated to increase at the age of 50 years in China [10], studies focusing on middle-aged and elderly population are important. Thus, we aimed to evaluate the relationship of fat% and FFM percentage (FFM%) changes with cardiovascular events in a middle-aged and elderly community-based Chinese cohort.
Methods
Study population
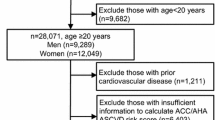
The participants in this prospective cohort study were recruited from Shanghai communities in 2013–2014. All participants underwent a physical examination, laboratory testing, and body composition measurements at baseline. Information on the history of current and past diseases, medication use, smoking habits, menopausal status, family history, and personal habits was collected using standardized questionnaires at baseline [11]. Those with a validated history of malignant tumors, thyroid dysfunction or hyperthyroidism or hypothyroidism, cardiovascular or cerebrovascular diseases, severe liver or kidney dysfunction, treatment with steroids or thyroxine, age < 50 years, or premenopausal women at enrollment were excluded. In 2015–2016, these participants were invited for a second examination which was similar to the previous. Afterward, participants were followed up during 2021–2022 via telephone or electronic medical records (Fig. 1). From the second examination to the last follow-up, the mean follow-up period was 5.5 ± 0.6 years.
For this study, 1048 participants undergoing two examinations during 2013–2014 and 2015–2016, non-CVD at baseline and during health examination periods, with complete data, were finally included. When compared with non-respondents (including those with missing covariate data or lost to follow-up), respondents had similar BMI, blood pressure, glucose levels, and lifestyle habits. There were fewer men than women in the current study. All participants provided written informed consent. The study was approved by the Ethics Committee of the Shanghai Sixth People’s Hospital affiliated to Shanghai Jiao Tong University School of Medicine.
Anthropometric and laboratory measurements
Height, weight, waist circumference, and blood pressure were measured using standardized methods. BMI was calculated as the weight in kilograms divided by the squared height in meters. The total FM, fat%, FFM, and FFM% were measured using an automatic bioelectrical impedance analyzer (BIA; TBF-418B; Tanita Corp., Tokyo, Japan). Changes in each body composition compartment (fat% and FFM%) between the first and second examinations were calculated as percentage change [(value2 – value1)/value1 × 100%]. According to previous literature, age-associated muscle loss begins at around 50 years, with mass loss at a rate of 0.5–1.2% per year [12]. Participants were then categorized into four groups:⊿FFM% < – 8%, – 8% ≤ ⊿FFM% < – 2%, – 2% ≤ ⊿FFM% < 2% (reference group: stable), and ⊿FFM% ≥ 2%. In addition, adults who maintain their weight, lose their FFM and gain a similar amount of fat% [13]. Thus, the same classification method was used for fat% change.
Venous blood samples for the measurement of blood routine, glucose, and lipid levels were drawn after a 10-h overnight fast. Participants without a validated history of diabetes underwent a 75-g oral glucose tolerance test, whereas those with diabetes performed a standard bread meal instead. Homeostasis model assessment of insulin resistance (HOMA-IR) was evaluated using the following formula: HOMA-IR = fasting insulin (FINS) (mU/L) × fasting plasma glucose (FPG) (mmol/L)/22.5 [14].
Outcome
The primary endpoint was a composite of cardiovascular events, including nonfatal myocardial infarction, unstable angina pectoris, hospitalization for heart failure, coronary revascularization, ischemic stroke, and cardiovascular death [15]. The first occurrence of cardiovascular event was recorded via phone calls or electronic medical records in 2021–2022. Subsequently, two well-trained physicians evaluated the outcome data and used the International Classification of Diseases-Tenth Revision (ICD-10) to identify cardiovascular events (I00–I99).
Diagnostic criteria
Current smokers were defined as participants who smoked at least one cigarette per day for more than six months at baseline [16]. According to the International Physical Activity Questionnaire 2010, physical activity levels were classified as light, moderate, and high [17]. Participants were categorized into two groups: BMI < 25 kg/m2 and BMI ≥ 25 kg/m2, based on the World Health Organization 2000 criteria [18]. On the basis of the 2020 guidelines of the International Society of Hypertension [19], hypertension was defined as systolic blood pressure (SBP) ≥ 140 mmHg, diastolic blood pressure (DBP) ≥ 90 mmHg, and/or the use of antihypertensive drugs. Diabetes was diagnosed according to the following criteria: (1) FPG ≥ 7 mmol/L, (2) 2 h-plasma glucose (2hPG) ≥ 11.1 mmol/L, (3) glycated hemoglobin A1c (HbA1c) ≥ 6.5%, or (4) a previous diagnosis of diabetes, according to the guidelines of the 2021 American Diabetes Association [20]. Participants with total cholesterol (TC) ≥ 5.2 mmol/L (200 mg/dL), triglyceride (TG) ≥ 1.7 mmol/L (150 mg/dL), low-density lipoprotein cholesterol (LDL-C) ≥ 3.4 mmol/L (130 mg/dL), high-density lipoprotein cholesterol (HDL-C) < 1.0 mmol/L (40 mg/dL), or using lipid-lowering drugs were identified as having dyslipidemia [21].
Statistical analysis
For continuous variables, normally distributed variables were presented as means ± standard deviations, while skewed variables were described as median and interquartile range. Frequency (proportion) was used for categorical variables. One-way ANOVA, Kruskal–Wallis H test, and chi-square test were used to compare baseline characteristics between fat% change categories for normally distributed, skewed, and categorical variables, respectively. Cox proportional hazards regression analysis was performed to obtain hazard ratios (HRs) and 95% confidence intervals (CIs) of cardiovascular events based on fat% and FFM% changes. Three models were applied: model 1 was adjusted for age and sex; model 2 was further adjusted for lifestyle factors (baseline smoking status, education attainment, family history of CVD, and physical activity); model 3 was further adjusted for metabolic factors (hypertension, diabetes, dyslipidemia, C-reactive protein (CRP), fat%, FFM%, and BMI). The restricted cubic splines with four knots (5th, 35th, 65th, 95th knots) were used to graphically assess the dose–response association between body composition changes and cardiovascular events, because it could better balance both the smoothness of the curve and the accuracy of the model. Interactions of body composition changes with age group (< 65 vs. ≥ 65 years), sex (men vs. women), and overweight/obesity status (BMI < 25 vs. ≥ 25 kg/m2) were examined in the fully adjusted model, and HRs with 95% CIs were calculated for each subgroup. All analyses were conducted using R version 4.0.3 (R Foundation for Statistical Computing, Vienna, Austria), and a two-tailed P < 0.05 was considered statistically significant.
Results
Baseline characteristics of the study population
A total of 1048 participants aged 50–80 years (median, 60; range, 56–63) were analyzed. Of these, 456 were men and 592 were women. The median baseline BMI, fat%, and FFM% for the entire study population were 23.9 (22.1–25.9) kg/m2, 27.2 (20.8–33.6)%, and 72.8 (66.4–79.2)%, respectively. The baseline characteristics of the study participants grouped by fat% change categories during the first examination in 2013–2014 are detailed in Table 1. Compared with those with stable fat%, individuals with fat% gain were more likely to be men and current smokers, but with a lower BMI and a lower incidence of hypertension at baseline. Moreover, individuals with fat% gain showed worse metabolic profile changes between first and second examinations (elevated blood pressure, glucose, CRP levels, and poor lipid profiles).
Fat% or FFM% change and cardiovascular events
During a mean follow-up of 5.5 years after two examinations, 86 (8.21%) cardiovascular events occurred. The median fat% change and FFM% change for the total population were 0.31 (− 5.53–6.87)% and − 0.12 (2.36–2.06)%, respectively. The restricted cubic spline model (Fig. 2) showed that an increase in fat% change was positively associated with a higher risk of cardiovascular events, whereas a decrease in FFM% change was associated with an increased risk of cardiovascular events.
Restricted cubic splines curves for the association of changes in fat% (A) and FFM% (B) with incident cardiovascular disease. Solid lines represent hazard ratio and dotted regions represent 95% confidence interval. Hazard ratios (95% confidence interval) were calculated by multivariate Cox proportional hazards regression models. The models were adjusted for age, sex, baseline smoking status, education, family history of cardiovascular disease, physical activity, hypertension, diabetes, dyslipidemia, C-reactive protein, fat%, FFM%, and body mass index
After controlling for the potential confounding factors in the Cox regression model (Table 2), a 2-year change in fat% was significantly and positively associated with the risk of cardiovascular events (HR 1.04, 95%CI 1.01–1.07). Participants with fat% gain ≥ 2% had a significantly increased risk (HR 2.07, 95%CI 1.08–3.97) compared with those with stable fat% (− 2 to 2%).
With regard to FFM%, a 2-year change in FFM% was significantly and inversely associated with the risk of cardiovascular events (HR 0.84, 95%CI 0.74–0.95). Participants with FFM% loss > 8% had a higher risk of cardiovascular events than those with stable FFM% (HR 3.83, 95%CI 1.29–11.4).
Association between fat% and FFM% change and cardiovascular events stratified by different characteristics
Stratified analyses were performed to evaluate the association of fat% and FFM% changes with cardiovascular events, respectively (Fig. 3). The associations were preserved when participants were categorized by age, sex, and overweight/obesity status. We further observed that BMI modified the association between fat% change and cardiovascular events (Pfor interaction = 0.01). A stronger effect of fat% change on cardiovascular events was observed among participants with BMI ≥ 25 kg/m2 (HR 1.07, 95%CI 1.03–1.12) compared with those with BMI < 25 kg/m2 (HR 1.04, 95%CI 1.00–1.08).
Effects of fat% and FFM% changes on cardiovascular events in different subgroups. Hazard ratios were estimated per 2% increase of fat% and FFM% change. A Fat% change and the risk of cardiovascular events. B FFM% change and the risk of cardiovascular events. The models were adjusted for age, sex, baseline smoking status, education, family history of cardiovascular disease, physical activity, hypertension, diabetes, dyslipidemia, C-reactive protein fat%, FFM% and body mass index, except the stratified variable
Discussion
To the best of our knowledge, this is the first study to explore the association of changes in body composition and cardiovascular events by separating fat% and FFM%, instead of using BMI, which is a composite of muscle and FM, in middle-aged and elderly Chinese populations. In this community-based prospective study, we found that 2-year fat% gain or FFM% loss was associated with an elevated risk of cardiovascular events in the next 5.5 years.
CVDs remain the leading cause of premature mortality in the world, accounting for an average of 17.9 million deaths annually [22]. In China, the burden of CVD has rapidly and substantially increased. According to some estimates, the incidence of cardiovascular events is expected to increase by 50% from 2010 to 2030 [23]. Therefore, tackling CVD risk factors remains a key goal in efforts to prevent, control, and reduce the incidence of CVDs worldwide. Obesity, an estimated risk factor for CVD, has been proven to underlie the development of many metabolic disorders, including hypertension, type 2 diabetes, dyslipidemia [24], and even cardiovascular events [3]. As a common index for measuring adiposity, dynamic changes of BMI have received much attention in predicting cardiovascular events. Choi et al. reported that every 1 kg/m2 increase in BMI was associated with a nearly 50% higher risk of acute myocardial infarction or coronary heart disease in the following 9 years [25]. However, BMI alone cannot distinguish body composition. FM plays a detrimental role, whereas FFM is protective [5]. Therefore, it is crucial to accurately evaluate changes in body composition to better understand the association between adiposity and cardiovascular events.
Several prospective studies have explored the association between body composition changes and cardiovascular events. One cohort study recruited over 3 million community-dwelling participants aged 20–39 in Korea [9]. They found that each 1 kg/m2 increase in the 2-year FM index change was associated with an elevated risk of cardiovascular events, whereas each 1 kg/m2 increase in the FFM index change was associated with a reduced risk of cardiovascular events, which was consistent with our study. Inconsistent with our results, Xing et al. [8] observed that changes in FM and FFM conferred no excess risk of cardiovascular events in 9234 type 2 diabetes patients. Patel et al. [7] found that a 10% increase in FM, not FFM, was associated with a 20% higher risk of heart failure in 5145 participants with type 2 diabetes and overweight/obesity in an American population. The discrepancies may be due to the differences in the included participants and the outcome definition. Participants in the two studies mentioned above were patients with type 2 diabetes, whereas the prevalence of diabetes in our cohort was only 20.2%; this may contribute to different association patterns between body composition changes and cardiovascular events. Therefore, the association between body composition changes and cardiovascular events is still inconclusive. Our cohort study in middle-aged and elderly Chinese residents demonstrated that a 2-year fat% gain or FFM% loss was closely associated with an increased risk of cardiovascular events in a 5.5-year of follow-up. Participants with ≥ 2% fat gain had a 1.07-fold higher risk of cardiovascular events than those with a stable fat%. Also, an FFM% loss > 8% was related to a 2.83-fold higher risk of cardiovascular events compared with the stable group.
The findings of this study have some important implications for the prevention and control of CVD in China. Unlike weight gain, which is usually due to the increase in FM, weight loss may have two causes: FM loss or FFM loss (mainly muscle mass loss). In our analysis, we observed that > 8% of FFM% loss was related to a higher risk of cardiovascular events, and the risk in participants with decreased FM% was similar to that in participants with stable FM%. Our findings imply that one possible reason for the negative effect of weight loss on CVD in some researches [26, 27] might be due to the loss of muscle mass more than the loss of fat mass. More importantly, it has been demonstrated that total muscle mass peaks at the age of 24 years. Afterward, muscle mass is well maintained as about 10% loss occurred between 24 and 50 years. But between 50 and 80 years, an additional loss of 30% occurs [28]. Although aging is inevitable, body composition can be contained. Hence, for middle aged and elderly population, who commonly experience sarcopenia, more attention should be paid to the causes of weight loss. Our findings emphasize the importance of body composition monitoring for better CVD management. Furthermore, these associations held both for middle-aged and elderly population. Thus, it is never too late to initiate control of body composition changes, even in old age.
For middle-aged and elderly population, a reduction in muscle mass is often accompanied by an increase in fat, and vice versa [29]. Crosstalk between body fat and muscle contributes to negative feedback, which in turn results in the development of CVD. The mechanisms of obesity and muscle function in CVD have been well-reviewed. First, excessive fat accumulation promotes the secretion of pro-inflammatory factors, including TNF-α, IL-6, and IL-1, which upregulate IKK/NF-κB and MAPK pathways to induce cell apoptosis and ultimately contribute to myocardial injury [30, 31]. Second, fat and muscle tissues act as endocrine organs that release diverse cytokines, such as adiponectin and Fstl1. Adiponectin, released from adipocytes, facilitates insulin sensitivity by promoting glucose uptake in skeletal muscle and activating the AMPK pathway [32]. However, serum adiponectin levels decrease with increasing body fat. Likewise, Fstl1 functions as a myokine that modulates endothelial function, adverse cardiac remodeling, and subsequent CVD [33]. The activation of oxidative stress [34] and the sympathetic nervous system [35] are also involved in the progression of CVD.
Our study has several limitations. First, it only included the Shanghai population. Further studies are required to verify these findings in different ethnic groups. Second, dietary information was not included in the analyses and will be supplemented in the future. Third, FM and FFM were measured by BIA, not by dual-energy X-ray absorptiometry. However, validation studies revealed that BIA and dual-energy X-ray absorptiometry had high correlations in both men and women (ICC > 0.8) [36]. In addition, BIA has advantages in that it is easy, low-cost, and non-invasive, and is supported by the Asian Working Group of Sarcopenia in community-dwelling settings [37].
Conclusions
In summary, this longitudinal cohort study revealed that fat% gain or FFM% loss significantly increased the risk of cardiovascular events in middle-aged and elderly, community-based Chinese populations. Thus, changes in body composition should be monitored frequently as an early warning of CVD.
Availability of data and materials
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- CVD:
-
Cardiovascular disease
- BMI:
-
Body mass index
- FM:
-
Fat mass
- FFM%:
-
Fat-free mass percentage
- Fat%:
-
Fat percentage
- BIA:
-
Bioelectrical impedance analyzer
- HR:
-
Hazard ratio
- HOMA-IR:
-
Homeostasis model assessment of insulin resistance
- FINS:
-
Fasting insulin
- FPG:
-
Fasting plasma glucose
- ICD-10:
-
International Classification of Diseases of Tenth Revision
- SBP:
-
Systolic blood pressure
- DBP:
-
Diastolic blood pressure
- 2hPG:
-
2 h-plasma glucose
- HbA1c:
-
Glycated hemoglobin A1c
- TC:
-
Total cholesterol
- TG:
-
Triglyceride
- LDL-C:
-
Low-density lipoprotein cholesterol
- HDL-C:
-
High-density lipoprotein cholesterol
- CRP:
-
C-reactive protein
- CI:
-
Confidence interval
References
Obesity and overweight. World Health Organization. Fact sheet. Updated June 2019. https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight. Accessed 13 May 2020.
Dai H, Alsalhe TA, Chalghaf N, Riccò M, Bragazzi NL, Wu J. The global burden of disease attributable to high body mass index in 195 countries and territories, 1990–2017: an analysis of the Global Burden of Disease Study. PLoS Med. 2020;17(7):e1003198.
Kim MS, Kim WJ, Khera AV, Kim JY, Yon DK, Lee SW, et al. Association between adiposity and cardiovascular outcomes: an umbrella review and meta-analysis of observational and Mendelian randomization studies. Eur Heart J. 2021;42(34):3388–403.
Held C, Hadziosmanovic N, Aylward PE, Hagström E, Hochman JS, Stewart RAH, et al. Body Mass Index and association with cardiovascular outcomes in patients with stable coronary heart disease: a stability substudy. J Am Heart Assoc. 2022;11(3):e023667.
Medina-Inojosa JR, Somers VK, Thomas RJ, Jean N, Jenkins SM, Gomez-Ibarra MA, et al. Association between adiposity and lean mass with long-term cardiovascular events in patients with coronary artery disease: no paradox. J Am Heart Assoc. 2018;7(10):e007505.
Xing Z, Tang L, Chen J, Pei J, Chen P, Fang Z, et al. Association of predicted lean body mass and fat mass with cardiovascular events in patients with type 2 diabetes mellitus. CMAJ. 2019;191(38):E1042–8.
Patel KV, Bahnson JL, Gaussoin SA, Johnson KC, Pi-Sunyer X, White U, Look AHEAD Research Group, et al. Association of baseline and longitudinal changes in body composition measures with risk of heart failure and myocardial infarction in type 2 diabetes: findings from the look AHEAD trial. Circulation. 2020;142(25):2420–30.
Xing Z, Chai X. Changes in fat mass and lean body mass and outcomes in type 2 diabetes mellitus. Intern Emerg Med. 2022;17(4):1073–80.
Kim SR, Lee G, Choi S, Oh YH, Son JS, Park M, et al. Changes in predicted lean body mass, appendicular skeletal muscle mass, and body fat mass and cardiovascular disease. J Cachexia Sarcopenia Muscle. 2022;13(2):1113–23.
Lu J, Lu Y, Yang H, Bilige W, Li Y, Schulz W, Masoudi FA, Krumholz HM. Characteristics of high cardiovascular risk in 1.7 million Chinese adults. Ann Intern Med. 2019;170(5):298–308.
Xu Y, Ma X, Pan X, He X, Wang Y, Bao Y. Serum adipocyte fatty acid-binding protein levels: an indicator of non-alcoholic fatty liver disease in Chinese individuals. Liver Int. 2019;39(3):568–74.
Bell KE, von Allmen MT, Devries MC, Phillips SM. Muscle disuse as a pivotal problem in sarcopenia-related muscle loss and dysfunction. J Frailty Aging. 2016;5(1):33–41.
Newman AB, Lee JS, Visser M, Goodpaster BH, Kritchevsky SB, Tylavsky FA, et al. Weight change and the conservation of lean mass in old age: the health, aging and body composition study. Am J Clin Nutr. 2005;82(4):872–8.
Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985;28(7):412–9.
Hu T, Shen Y, Cao W, Xu Y, Wang Y, Ma X, Bao Y. Neck circumference for predicting the occurrence of future cardiovascular events: a 7.6-year longitudinal study. Nutr Metab Cardiovasc Dis. 2022;32(12):2830–8.
Yang G, Fan L, Tan J, Qi G, Zhang Y, Samet JM, et al. Smoking in China: findings of the 1996 National Prevalence Survey. JAMA. 1999;282(13):1247–53.
Tran VD, Do VV, Pham NM, Nguyen CT, Xuong NT, Jancey J, et al. Validity of the international physical activity questionnaire-short form for application in Asian countries: a study in Vietnam. Eval Health Prof. 2020;43(2):105–9.
Obesity: preventing and managing the global epidemic. Report of a WHO consultation. World Health Organization technical report series. 2000;894:i-xii, 1–253.
Unger T, Borghi C, Charchar F, Khan NA, Poulter NR, Prabhakaran D, et al. 2020 international society of hypertension global hypertension practice guidelines. Hypertension. 2020;75(6):1334–57.
Classification and Diagnosis of Diabetes. Standards of medical care in diabetes-2021. Diabetes Care. 2021;44(Suppl 1):S15–33.
Joint Committee for Guideline Revision. 2016 Chinese guidelines for the management of dyslipidemia in adults. J Geriatr Cardiol. 2018;15(1):1–29.
The World Health Organization (WHO). Noncommunicable diseases. Geneva: World Health Organization. Fact sheet. Updated January 2019. http://www.who.int/mediacentre/factsheets/fs355/en/. Access 23 June 2020.
Zhao D, Liu J, Wang M, Zhang X, Zhou M. Epidemiology of cardiovascular disease in China: current features and implications. Nat Rev Cardiol. 2019;16(4):203–12.
Moore KJ, Shah R. Introduction to the obesity, metabolic syndrome, and CVD compendium. Circ Res. 2020;126(11):1475–6.
Choi S, Kim K, Kim SM, Lee G, Jeong SM, Park SY, et al. Association of obesity or weight change with coronary heart disease among young adults in South Korea. JAMA Intern Med. 2018;178(8):1060–8.
Strand BH, Wills AK, Langballe EM, Rosness TA, Engedal K, Bjertness E. Weight change in midlife and risk of mortality from dementia up to 35 years later. J Gerontol A Biol Sci Med Sci. 2017;72(6):855–60.
Okada C, Kubota Y, Eshak ES, Cui R, Tamakoshi A, Iso H, et al. Weight change and mortality from cardiovascular diseases: the Japan collaborative cohort study. J Atheroscler Thromb. 2021;28(1):25–33.
Dennison EM, Sayer AA, Cooper C. Epidemiology of sarcopenia and insight into possible therapeutic targets. Nat Rev Rheumatol. 2017;13(6):340–7.
Zamboni M, Rubele S, Rossi AP. Sarcopenia and obesity. Curr Opin Clin Nutr Metab Care. 2019;22(1):13–9.
Castoldi A, Naffah de Souza C, Câmara NO, Moraes-Vieira PM. The macrophage switch in obesity development. Front Immunol. 2016;6:637.
Di Pino A, DeFronzo RA. Insulin resistance and atherosclerosis: implications for insulin-sensitizing agents. Endocr Rev. 2019;40(6):1447–67.
Yamauchi T, Kamon J, Minokoshi Y, Ito Y, Waki H, Uchida S, et al. Adiponectin stimulates glucose utilization and fatty-acid oxidation by activating AMP-activated protein kinase. Nat Med. 2002;8(11):1288–95.
Ouchi N, Ohashi K, Shibata R, Murohara T. Protective roles of adipocytokines and myokines in cardiovascular disease. Circ J. 2016;80(10):2073–80.
Hong SH, Choi KM. Sarcopenic obesity, insulin resistance, and their implications in cardiovascular and metabolic consequences. Int J Mol Sci. 2020;21(2):494.
Favre GA, Esnault VL, Van Obberghen E. Modulation of glucose metabolism by the renin-angiotensin-aldosterone system. Am J Physiol Endocrinol Metab. 2015;308(6):E435-449.
Lee MM, Jebb SA, Oke J, Piernas C. Reference values for skeletal muscle mass and fat mass measured by bioelectrical impedance in 390 565 UK adults. J Cachexia Sarcopenia Muscle. 2020;11(2):487–96.
Chen LK, Liu LK, Woo J, Assantachai P, Auyeung TW, Bahyah KS, et al. Sarcopenia in Asia: consensus report of the Asian Working Group for Sarcopenia. J Am Med Dir Assoc. 2014;15(2):95–101.
Acknowledgements
Not applicable.
Funding
This work was supported by grant from Shanghai Municipal Science and Technology Commission Medical Guide Project (19411964300), Shanghai Pujiang Program (21PJ1411800) and Shanghai Research Center for Endocrine and Metabolic Diseases (2022ZZ01002).
Author information
Authors and Affiliations
Contributions
HTT and SY analyzed the data and wrote the manuscript. CWJ, XYT, WYF and MXJ collected the data. BYQ and SY obtained fundings. All authors contributed to the conception and design of the work, interpretation of the data, reviewed and provided edits and comments on manuscript, approved the final version of the manuscript, and agreed to be accountable for all aspects of the work. MXJ and BYQ are the guarantors of this work and, as such, have full access to all the data in the study. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The current study was carried out in accordance with the principles of the Declaration of Helsinki and approved by the institutional review board at the Ethics Committee of Sixth People’s Hospital Affiliated to Shanghai Jiao Tong University School of Medicine. Written informed consent was obtained from all study participants.
Consent for publication
No applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Hu, T., Shen, Y., Cao, W. et al. Two-year changes in body composition and future cardiovascular events: a longitudinal community-based study. Nutr Metab (Lond) 20, 4 (2023). https://doi.org/10.1186/s12986-023-00727-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12986-023-00727-2