Abstract
Age and Gender are vital determinants for the micronutrient demands of normal indviduals. Among these micronutrients are vitamins that are required in small amounts for optimum metabolism, homeostasis, and a healthy lifestyle, acting as coenzymes in several biochemical reactions. The majority of previous studies have examined such issues that relates to a specific vitamin or life stage, with the majority merely reporting the effect of either excess or deficiency. Vitamins are classified into water-soluble and fat-soluble components. The fat-soluble vitamins include vitamins (A, D, E, and K). Fat-soluble vitamins were found to have an indisputable role in an array of physiological processes such as immune regulation, vision, bone and mental health. Nonetheless, the fat-soluble vitamins are now considered a prophylactic measurement for a multitude of diseases such as autism, rickets disease, gestational diabetes, and asthma. Herein, in this review, a deep insight into the orchestration of the four different fat-soluble vitamins requirements is presented for the first time across the human life cycle beginning from fertility, pregnancy, adulthood, and senility with an extensive assessment ofthe interactions among them and their underlying mechanistic actions. The influence of sex for each vitamin is also presented at each life stage to highlight the different daily requirements and effects.
Similar content being viewed by others
Introduction
Despite its tiny molecular size, its physiological functions are indisputable. Vitamins are small organic molecules that are not synthesized endogenously in sufficient amounts which highlights their importance in our diet at all life stages, starting from neonatal to geriatric life [1]. Vitamins are organic essential micronutrients (needed at minute levels) that cannot be synthesized by vertebrates but are required to perform specific biological functions for normal growth and the maintenance of a human’s health [2].
The word “vitamin” was coined from two terms, vital and amine but due to the realization later on that, not all of them are amines the letter “e” was removed. The 13 known vitamins are classified according to their solubility in either water or fat which further affects their pharmacokinetic properties [3]. The fat-soluble vitamins (A, D, E, K) which are the main focus of this review are well-absorbed from the intestine in the presence of fats.
Historically, classical deficiencies of those vitamins were directly correlated with several pathological manifestations such as night blindness (due to Vitamin A deficiency), osteomalacia (due to Vitamin D deficiency), oxidative stress (due to Vitamin E deficiency), and hemorrhage (due to Vitamin K deficiency). However, over the past decade vitamins, A and D, in particular, have been associated with more complex disorders such as cancer and autoimmune diseases [4, 5]. In this review, a detailed description of each fat-soluble vitamin will be presented along with its role at every stage of human life and in the context of different-sex requirements.
Vitamin A
Some vitamins are particularly made of one nutrient; this is not the case in vitamin A as it contains a broad group of related nutrients. The two main forms are retinoids (retinol, retinal, retinoic acid) and carotenes (α, β and γ); the latter refers to a pro-vitamin mainly found in plants, whereas the former is found in animals (non-vegetarian form) [6, 7].
Vitamin A: metabolism, dietary sources, functions, and signaling pathways
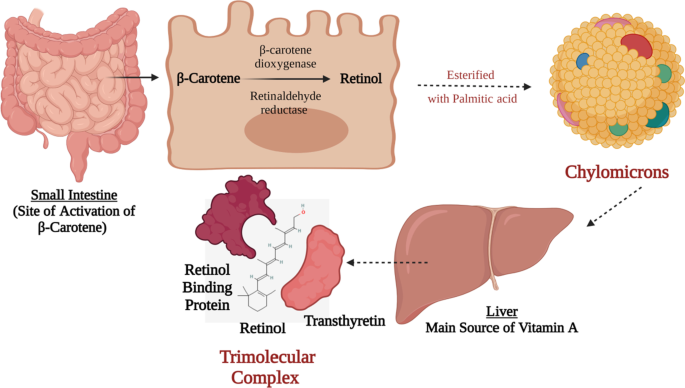
The main pro-vitamin is β-carotene and is transformed to its active form of vitamin A in the intestine where it is cleaved by β-carotene dioxygenase and by retinaldehyde reductase and finally reduced to retinol. Retinol is then esterified with palmitic acid into chylomicrons and with lipids to be delivered to the liver. The liver has around 90% of the vitamin A supply is secreted as retinol bound to retinol-binding protein (RBP), this complex combines with transthyretin (a protein) as presented in Fig. 1. This trimolecular complex acts to avoid vitamin A’s drainage by glomerulus filtration, and to halt the toxicity of retinol [8, 9].
Vitamin A Biosynthesis and Activation. This figure represents a schematic presentation for the activation process of β-carotene to retinol in the small intestine following the absorption of the β-carotene from t;9he apical membrane and then the transportation of the activated retinol via the basolateral membrane directed towards the liver via chylomicrons. In the liver, it is processed in a trimolecular complex that is made up of active retinol, retinol-binding protein, and transthyretin protein. Such trimolecular complex prevents its glomerulus filtration via the kidneys
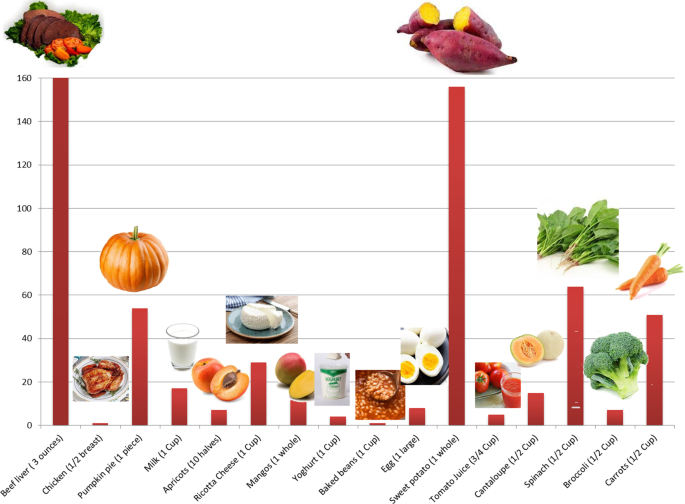
It is also worth noting that vitamin A sources are diverse. It can be found in mammals as retinol and can be found in plants as carotenoids, the figure below (Fig. 2) shows different foods that are rich in vitamin A and their percentage daily value. On the biochemical and molecular levels, it has been reported that in a murine model that was used to investigate the effect of vitamin A on liver regeneration, vitamin A has been found to strongly affect the microbiota profile in treated animals and resulted in an enhancement of bile acid metabolism [10, 11]. On the other hand, gut microbiota (GM) have shown to be able to regulate vitamin A pharmacokinetic profile and immunomodulation functions [10, 12].
Vitamin A sources. A bar chart representing the sources of Vitamin A in daily food and its percentage daily value. Beef liver (3 oz) = 85.05gm; Chicken (½ breast) = 130gm; Pumpkin pie (1 piece) = 323gm; Milk (1 cup) = 240gm; Apricot (10 halves) = 105 gm; Ricotta Cheese (1 cup) = 220gm; Mangos (1 whole) = 336gm; Yoghurt (1cup) = 245gm; Baked beans (1 cup) = 172gm; Egg (1 large) = 50gm; Sweet potato (1 cup) = 133gm; Tomato juice (3/4 cup) = 169gm; Cantaloupe (½ cup) = 27gm; Spinach (½ cup) = 15gm; Broccoli (½ cup) = 35.5gm; Carrots (½ cup) = 64gm
Vitamin A is essential in a wide spectrum of physiological activities such as clear retinal vision [13], skin health [14], immune system [15], reproduction [16], and embryonic development as previously reviewed in [16,17,18,19].
In early development stages throughout embryogenesis, vitamin A (retinol form) stimulates the activation of the transcription factor Hoxa1 which is important for segmentation and patterning of the hindbrain area as shown in Table 1 [20, 21]. During prenatal and postnatal life, it is well-known that either deficiency or excess of vitamin A might lead to birth defects (teratogenic effects). The signals initiated by the retinoids begin after the early phase of embryonic development (gastrulation) where retinoic acid is very important for organ development, including the heart, eyes, ears, lungs, limbs, visceral organs. Moreover, retinoid signaling is essential in the expression of many proteins of the extracellular matrix particularly collagen, laminin, and proteoglycans [22]. Such findings highlight the unquestionable role of Vitamin A in several cellular and molecular functions.
Furthermore, vitamin A contributes to immune system development [23]. Besides being well known as an anti-inflammatory vitamin [24], vitamin A participates in the maturation of immune cells and shows a potent anti-infective effects. It promotes T cells migration by inducing α4β7 expression level [25, 26], and increases B cell immunoglobulin production [27]. In a study performed on rabbits, in which their diet was enriched with carotenoids, serum levels of IgA, IgG, and IgM was elevated showing amelioration in their humoral immunity [27]. Concerning the anti-bacterial action of vitamin A, it has been noticed in a study on tuberculosis-model mice where administration of vitamin A derivatives has remarkably enhanced traditional anti-tuberculosis drugs’ efficacy [28]. Vitamin A exerts its bactericidal activity via inducing NPC2 expression level which in turn hinders cell wall biosynthesis in infective bacteria [29].
Preconception and pregnancy
Pregnancy is an important phase in the life of any woman during which the fate of her fetus is partially defined. During this period, specific nutritional needs are highly demanded to maintain good health for the mother and her fetus. For instance, vitamins demand/intake highly increases with different peaks at different trimesters based on the gradual fetal development [56].
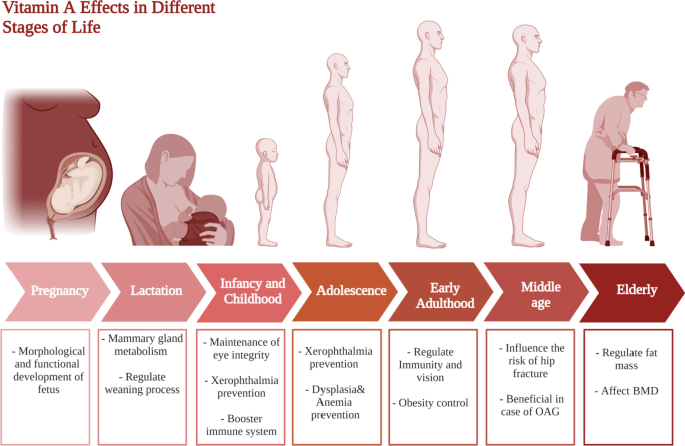
Vitamin A is vital for the growth and maintenance of the fetus to provide a limited reserve in the fetus’s liver and for maternal tissue growth [57]. Vitamin A is not only essential for the morphological and functional development of the fetus, but is also vital for the ocular integrity and it exerts systemic effects on several fetal organs and the fetal skeleton [57]. Vitamin A has an indisputable role in ocular function, as it is involved in cell differentiation, maintenance of eye integrity, and prevention of xerophthalmia [58]. Yet, Vitamin A supplementation during pregnancy is a controversial issue and holds a lot of paradoxical facts.
In several developing countries, vitamin A deficiency is a public health problem being the primary cause of night blindness. On the contrary, in some developed countries, excessive Vitamin A intake during pregnancy has been directly linked with several teratogenic effects especially when administered in the 1st 60 days following conception. However, during the 3rd trimester of pregnancy vitamin A supplementation was found to decrease the incidence of broncho-pulmonary dysplasia in newborns [59].
Consequently, very strict vitamin A supplementation protocols for pregnant women have been conducted by the WHO and other health organizations [57]. In such context, WHO recommends supplementation of 3000 μg RAE/day or 7500 μg RAE/week during pregnancy in areas with the /high popularity of vitamin A deficiency (developing countries) to prevent night blindness in pregnant mothers an infant blindness, but not more than that because of the risk of teratogenicity (birth defects such as fontanelle) [60, 61]. However, the case in the developed countries is slightly different where it is recommended that monitoring of vitamin A intake whether from fortified foods or naturally should take place where it should not exceed 1500 μg RAE of vitamin A/day [60]. This underscores the importance of vitamin A as a vital vitamins for the growth and maintenance of the fetus to provide a limited reserve in the fetus’s liver and for maternal tissue growth [7]. Such discrepancy could be attributed to the different diets of people living in developed versus developing countries.
Lactation
“Mothers should absorb minerals and vitamins from their diets, to replace the amount lost in the milk produced to feed their infants”. This sentence has been widely used in folk medicine highlighting the fact that both the baby and the mother are prone to malnutrition during the lactation period if the intake of the vitamin was not closely monitored [7].
Vitamins are partially transferred to the fetus through placental transfer during the gestation period, but it is mainly transferred through the mother's milk during the neonatal period during lactation. Lactation is characterized by extensive morphological and metabolic changes in different tissues to guarantee a sufficient supply of blood and nutrients to the mammary gland for efficient milk production [56].
It is important to note that milk produced by the mother in the first days after birth (colostrum) is higher in proteins, vitamins A, B12, and K, and immunoglobulins and lower in fat content than mature milk 15 days after birth [62]. As previously mentioned retinol is released from the liver and incorporated in breast milk where it provides the infant with the required dosage to sustain visual, immune, and cognitive development. Vitamin A transfer through breast milk during the first 6 months of life is 60 times higher than the transfer occurring through the placenta during the 9 months of pregnancy. If the mother's vitamin A nutritional status is deficient, infants are susceptible to having vitamin A deficiency at the age of 6 months. Consequently, breastfeeding mothers and infants are considered at risk of vitamin A deficiency [63].
The concentration of vitamin A in human milk decreases throughout lactation; it is maximal in the colostrum and reaches a plateau in mature milk. In healthy mothers, vitamin A level varies from 5 to 7 μM in colostrum, 3 to 5 μM in transitional milk, and 1.4 to 2.6 μM in mature milk. The higher levels of retinol in colostrum allow tissue stores in the newborn to be rapidly replenished after limited placental transfer during gestation [56]. It is also noteworthy that low natural antibodies level could be a direct consequence of vitamin A deficiency in infants [64].
Infancy and childhood
Vitamin A supplementation during neonatal life is quite debatable, with one study suggesting that neonatal vitamin A supplementation was correlated with a 14% decrease in mortality by 6 months of age [65]. The WHO conducted three large studies targeting low-income countries in Africa and Asia to examine the accuracy of such hypothesis. This suggestion was disputed as it caused a bulging fontanelle in the newborn babies scoring a 0.1–1.2% and due to having this side effect they would need a long-term follow up to provide healthy development [65].
From 7–12 months, the average daily human milk consumption would be 650 ml and to provide 325 μg of vitamin A. Due to the increased risk of death from 6 months onwards in vitamin A-deficient populations, the requirements and recommendations of safe intake increased to 190 mg for 7 months of age and 400 mg for 12 months of age. It is generally recommended that children 1–3 years should take 300 mcg/day versus 400 mcg/day of vitamin A in 4–8 years, and 600 mcg/day in 9–13 years. Yet, due to the popularity of night blindness (1% or higher) in children at age 24–59 months, a high dosage of vitamin A supplementation is required and this is also applied in populations where infants, children, and mothers are infected with HIV. This has collectively been summarized in Fig. 3.
Adolescence
People between the age of 10 to 19 years old witness the most important physical and mental development which affect their life significantly [66]. Thus, adolescents’ health should be a great concern for health care to avoid future cognitive, developmental, health, and economic problems [67]. In addition, the significant increase in fast food consumption at this age in low- and middle-income countries, along with the unawareness of micronutrients importance, urges the need to pay more attention to applying healthy-diet programs [68, 69].
In a recent study that was performed on adolescent girls, results confirmed that deficiencies in vitamin A and E were common at this age likely attributed to the high growth requirements [70]. Vitamin A deficiency in adolescence is a major problem that exert a remarkable impact on the future life [71].
For vitamin A, it is involved in many critical physiological processes at this age with deficiency that could lead to visual rod cells damage in what is known as nyctalopia or night-blindness as shown in Fig. 3 [72]. Moreover, severe deficiency of vitamin A could lead to xerophthalmia which is irreversible blindness that is common in children and adolescents [72, 73].Furthermore, low vitamin A intake was linked to respiratory diseases recurrence and immune system compromising [74], in addition to dysplasia and anemia as shown in Fig. 3 [72]. Nonetheless, recent studies have revealed that vitamin A intake can reinstate hemoglobin levels if administered along iron supplements [75].
Adulthood
In middle age (between 40 and 60 years old), males and females are susceptible to physiological changes which are reflected in their metabolic profiles [76, 77]. It has been widely known that fat-soluble vitamin supplementation during adulthood serves as prophylactic treatment for numerous adverse health outcomes that could occur during middle age and elderly phases [78, 79].
As mentioned above, vitamin A has been long recognized for its role in immunity and vision warranting the importance of vitamin A supplementation [80]. However, studies highlight further effects of vitamin A in early adulthood. For example, a recent study found that a lower intake of vitamin A is associated with obesity in early adulthood [81]. In contrast, vitamin A might possess some alarming effects including toxicity to the mitochondria, furthermore decreased life quality and increased morbidity rates have been observed among vitamin A supplement users [82].
It is also worth mentioning that vitamin A supplementation has several unrelated roles during middle age. It may serve as a treatment or protective agent to several different ailments. Firstly, it has been shown to influence the risk of hip fractures [83]. It has been also linked to the decreased incidence of open-angle glaucoma (OAG) which is a fairly common health issue that many suffer from during middle age as summarized in Fig. 3 [84].
Elderly
Vitamin A requirements for adults aged 50 years old and higher have very little evidence; but toxicity can occur at lower doses. In addition, the influence of vitamins on senior population health is controversial which necessitates further investigations. A normal real dose of vitamin A (900 μg/day for women and 700 μg/day for men) is obtained by orally multivitamin/mineral labeled as vitamin A acetate that provides 750 μg [85]. A study on 200 women with mean age of 53.0 years old has revealed that normal levels of vitamin A are associated with overweight and obesity [86]. In addition, hypervitaminosis A above 3000 μg could lead to liver and kidney toxicities [85], whereas and unlike the previous studies, a recent study has reported that high vitamin A intake could show favorable outcomes on fracture risk [87].
Sex effect
Although the essentials of a healthy diet appear similar in both males and females. The essential requirements for micronutrients such as vitamins highly differ due to the great differences in their physiological and hormonal statuses. For instance, at the age of 40–60 years old, females experience menopause [88]. Waicek et al. performed a study to investigate changes in vitamin levels in menopausal women revealing that some vitamin levels are altered which necessitate following specific diet and vitamin supplements intake to avoid against future health complications [89].
On the molecular level, intracellular receptors of vitamin A, retinoic acid receptors (RARs) and retinoid X receptors (RXRs) have been found in different testis cell types at different life stages. These receptors affect gene expression by binding promotor regions [90, 91]. In a study on mice in which the gene encoding for RAR was knocked out, remarkable apoptosis of spermatocytes in early meiotic stages was monitored with germ-cell degeneration [33] suggesting that RAR plays a pivotal role in germ-cells survival and spermatogenesis [33].
In case of Vitamin A, recommended dietary allowance is 700 μg RAE/day in females versus 900 μg RAE/day for males for normal gene expression, immune function, and vision as collectively presented in Table 2.
Vitamin D
Vitamin D is a vital micronutrient in all stages of life [92]. Despite being synthesized endogenously, 200–600 IU in different life stages is required daily as shown in Table 2 [93]. Meanwhile, vitamin D is extensively studied in literature owing to its numerous roles in human physiology [94]. Vitamin D is synthesized from cholesterol when the skin is exposed to the sun, it naturally exists in several forms including 7-dehydrocholesterol, vitamin D2, vitamin D3, 25-D, 1.25-D [95, 96].
Vitamin D: metabolism, dietary sources, functions, and signaling pathways
Generally, vitamin D is metabolized through 3 main steps, which are 25-hydroxylation, 1 alpha-hydroxylation, and 24-hydroxylation [97]. These steps are all carried out by cytochrome P450 mixed-function oxidases (CYPs), which are present in the endoplasmic reticulum (ER) and mitochondria [97].
Vitamin D can be found in cod liver and fatty fish like salmon and mackerel [98]. Other fish, eggs, meat, dairy products, wild mushroom, and cultivated mushroom present good sources of vitamin D [98]. It plays a role in the reproduction process [99], bone health [100], prostate cancer [101], breast cancer [102, 103], depression and anxiety [104]. It is also worth noting that vitamin D plays a major role in calcium metabolism, regulation of immune cells functions, as well as hematopoietic cells differentiation and proliferation [105].
At the molecular level, vitamin D exerts its action through binding to vitamin D receptor (VDR) which is a transcription factor that regulates cells epigenetically. Ligand-activated VDR was found to affect the transcription of 1000 genes including genes involved in energy metabolism, calcium and bone homeostasis, as well as innate and adaptive immunity [106]. Moreover, vitamin D was found to downregulate COX-1 and COX-2 expression limiting their role in the inflammatory process as shown in Table 1 [34]. Investigation of cell-cycle controlling system has reported vitamin D participation in cell cycle arrest through controlling expression of different regulatory molecules such as HIF1a, p53, MYC, Ras, MAPK, BRCA1, and GADD45 [34]. Evidence has also revealed the potential role of vitamin D in promoting apoptosis by downregulating the telomerase enzyme [36]. Another antitumor effect for vitamin D was found via angiogenesis inhibition through interfering with HIF-1α/ VEGF axis [37].
Intriguingly, vitamin D was found to affect and get affected by GM, too [10]. Alteration in fecal microflora was reported upon treatment with vitamin D [41, 42]. Yet, GM has been reported to be capable of manipulating vitamin D activity either through upregulating VDR intestinal expression by producing short-chain fatty acid such as butyrate [107], or through competing it for VDR by lithocholic acid, a secondary bile acid [108].
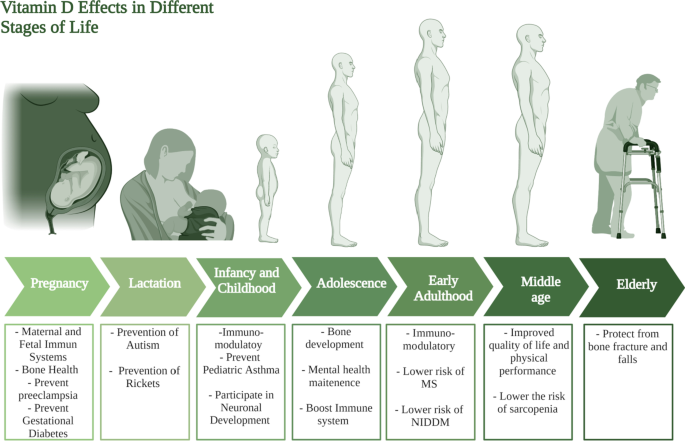
Vitamin D profile at different life stages
Preconception and pregnancy
Vitamin D supplementation during pregnancy has been shown to exert crucial effects on the fetus’s status in terms of skeletal health, immune system, as well as protecting the mother’s health [109, 110]. Furthermore, vitamin D deficiency is common among pregnant women and is associated with several adverse outcomes such as preeclampsia, gestational diabetes, preterm births, and low birth weights [111, 112].
Moreover, vitamin D plays a very significant immunoregulatory role in pregnancy. During pregnancy, the maternal immune system needs to tolerate the fetus. A group of the T lymphocytes, called regulatory T cells (Tregs) of potential immunosuppressive activity responsible for decreasing the destructive effect of the maternal immune system to her fetus [109]. It has been found that vitamin D increases the number of Tregs, in turn decreasing the chance of autoimmune diseases occurrence such as rheumatoid arthritis (RA), systemic lupus erythematosus (SLE), antiphospholipid syndrome (APS), Hashimoto Thyroiditis (HT), and multiple sclerosis (MS) [109].
It has been established that vitamin D alongside calcium plays an important role in skeletal health [113]. Expectedly, several recent reviews have concluded that vitamin D maternal supplementation is essential for healthy fetal bone growth through improving vitamin D and calcium levels in infants [110, 114]. Furthermore, low vitamin D levels in pregnant women are associated with an increased risk of fatal asthma, preeclampsia, gestational diabetes, preterm births, low birth weight wheeze, respiratory tract infections, and eczema [110, 111, 115,116,117].
No agreement has been reached regarding the healthy vitamin D dose per day for pregnant women. For instance, the Institute of Medicine set the healthy dose at 600 IU (international units) per day, while the Endocrine society sets it at 1500- IU per day, others have suggested ranges of 800–1200 IU and 400–800 IU per day for pregnant women [62, 110]. It is also noteworthy to mention that a recent review found conflicting conclusions regarding the main carrier of vitamin D, Vitamin D binding protein (VDBP) [118]. It was found that low levels of maternal serum VDBP are associated with several adverse pregnancy outcomes such as spontaneous miscarriage and pre-eclampsia, nevertheless increased VDBP levels in the cervicovaginal fluid were linked to an unexplained miscarriage [118].
Lactation
The role of vitamin D supplementation for lactating women can be viewed as a continuation of its role during pregnancy, the neonate needs vitamin D for the same reasons they needed for during pregnancy. However, one of the novel roles of vitamin D during lactation lies in the prevention and treatment of autism. Several studies point out the increased incidence of autism in vitamin D deficient children [119]. In such context, it is referred to vitamin D as a neuro-steroid that plays an important role in several process of brain development [119]. It was also found that children who are autistic have lower levels of 25(OH)D levels (the barometer of vitamin D level) at 3 months and age 8 compared to their non-autistic siblings [119]. Collectively, these studies show how vitamin D supplementation during lactation may significantly decrease the incidence of autism. Another important role of vitamin D in lactation is the prevention of rickets in infants [120]. Several reports found that vitamin D deficient neonates suffer from a higher risk of developing several disorders including rickets as summarized in Fig. 4 [120, 121].
Different sources suggest different amounts and methods of vitamin D supplementation during lactation [122, 123]. For example one study concluded that pregnant and lactating women should take (5000 IU/day) of vitamin D to prevent autism [119]. A randomized controlled trial found that supplying the mother with (6400 IU/day) of vitamin D per day satisfies her infant’s daily intake requirement [124]. Other reports suggest that infant’s supplementation of vitamin D through breastfeeding is not enough and will lead to vitamin D deficiency [123]. It is also noteworthy to mention that in the last 15 years, poison control reports have recorded 15,000 cases of vitamin D overdose, out of which no one died, showing that vitamin D is indeed safe [119].
Infancy and childhood
As an extrapolation of its high demand during the infancy stage, vitamin D is still of vital importance during the whole childhood period. Besides autism, Vitamin D has been found to play several roles in pediatric diseases, one of which is asthma. A recent review concluded that vitamin D supplementation helps in the prevention of the development of asthma [125]. Likewise a randomized, placebo-controlled clinical trial was conducted on school children who suffer from asthma, the trial showed that vitamin D supplementation as an adjunct therapy may help control asthma as summarized Fig. 4 [126].
Respiratory tract infections (RTIs) represent a great burden as they are the most common cause of morbidity among children under 5 years old [127]. Vitamin D level was found to be low in most infants and children who suffer from RTIs [127], and in accordance with other studies confirming that vitamin D supplementation may serve for prophylaxis against some RTIs [128, 129].
Another aspect in which vitamin D plays an important role is bone acquisition and development. Low levels of vitamin D are involved in the development of extra skeletal problems in childhood [130, 131].
Additionally, Vitamin D has been reported to be a vital modulator of neurodevelopment [132], with neurotransmission, oxidative stress, and neural cell proliferation as the most important mechanisms modulated by vitamin D [132]. Subsequently, its deficiency during early childhood negatively affects the developing brain, possibly leading to autism spectrum disorder (ASD) [132]. Furthermore, recent studies shed light onto the relationship between vitamin D deficiency and the development of several mental disorders in children [133]. Collectively, it can be concluded that vitamin D possesses an important preventative/ curative / modulatory role. Yet, regarding its dose, different institutions have opposing opinions about the correct dose of vitamin D that could be due to different geographical characteristics for the participants in each study [134, 135].
Adolescence
During adolescence, vitamin D is vital for bone development being considered as one of the most crucial micronutrient in this phase at which rapid bone development occurs [136]. The recommended dose for adolescents of vitamin D is 600 IU per day, however, the safety margin of vitamin D intake reaches up to 4,000 IU per day [137]. In addition, hypovitaminosis D in early life stages such as in adolescence was linked to mental disorders [133]. Vitamin D was also found to be associated with immune system wellbeing at this stage of life [138].
Adulthood
It has been reported that it is quite essential to keep adequate levels of vitamin D throughout all different stages of life as high serum 25-OHD levels in youth to adulthood [139]. In this stage of life, it has been repeatedly reported the immune-modulatory role of vitamin D, as it decreases excessive inflammation [140]. It is also associated with a decreased risk of developing type 2 diabetes in individuals in their adulthood period as summarized in Fig. 4 [141]. Noteworthy, low vitamin D levels in early life have been directly associated with a risk of multiple sclerosis later in life, however further studies are required to confirm these findings [142].
Vitamin D supplementation serves as a prophylactic treatment for several diseases common for middle-aged individuals. A clinical trial conducted by Manoy et al. [143] revealed that vitamin D2 supplementation (40,000 IU per week) for 6 months decreased oxidative protein damage, improved quality of life and physical performance in osteoarthritis patients. It has been recently reported that vitamin D plays a vital role in alleviating several sleep disorders and chronic pain conditions [144].
Elderly
With the remarkable pace by which life expectancy gains years [145], the demand of micronutrients increases parallel to the decrease in nutrients digestion and food intake from which elderly people suffer from [146]. Consequently, it’s not surprising that in a study investigating the status of different vitamins in elderly population and the effect of vitamin supplements on their health, it was found that 88% of subjects were deficient in vitamin D while 42% were deficient in vitamin K [147], and justifying the importance of regular vitamin intake in this age to avoid many complication that could result from vitamin deficiency or overdoses [147].
Vitamin D deficiency expose senior population to many risks including bone fracture upon falling [92]. A meta-analysis revealed that the risk of falling in senior population is reduced by 19% when vitamin D reaches 17.5–25 μg per day. Consequently, the risk of hip fracture declines [148]. Another clinical trial on institutionalized patients reported that 20 μg of vitamin D combined with 1200 mg calcium per day have resulted in lowering falls and fracture risk. However, lower doses of vitamin D and calcium, 10 μg and 1000 mg per day, respectively, have shown the same outcomes in people older than 65 years [149, 150].
Sex effect
It has been reported that males at younger age are more vulnerable to vitamin D deficiency than females [151]. Vitamin D level has also shown no relevance to all-types of cancer (excluding non-melanoma skin cancers) prevention in senior female population [152]. However, optimum concentration of vitamin D and calcium should be adjusted to avoid the risk of colorectal cancer development among males [153]. Nevertheless, vitamin D is believed to affect males’ fertility by affecting semen quality and sex steroids production [38]. Besides, VDR was found to mediate sperm motility via increasing intracellular calcium concentration [38, 39]. In this context, treatment of vitamin D deficient middle-aged male subjects with vitamin D for 12 month has been found to improve their testosterone levels and erectile function [40].
Vitamin E
Vitamin E is present in different forms such as α-, β-, γ-, δ-, tocopherol and tocotrienols. However, α-tocopherol is considered as the most active form of vitamin E [154], mostly recognized for its antioxidant action. Vitamin E acts mainly as antioxidant to protect the cell from reactive oxygen and nitrogen species (ROS and RNS) along with other antioxidants (e.g., vitamin C, glutathione) and enzymes (e.g., peroxides, catalase) [154]. Vitamin E has also been found to regulate platelets aggregation by the following mechanism; where prostacyclin release is promoted via vitamin E in the endothelial cells, prostacyclin inhibits the aggregation of platelets [154]. Nevertheless, vitamin E was reported to be a suppressor for leukotrienes synthesis exerting an anti-inflammatory effect [85]. In addition, recent studies have shown that different forms of vitamin E have the ability to reduce the risk of cancer development [155].
Vitamin E: metabolism, dietary sources, functions, and signaling pathways
Similar to other fat soluble vitamins, vitamin E is absorbed in chylomicron micelles from the intestines, then, released to the bloodstream by the action of lipoprotein lipase or it goes to the liver and released to the blood stream in form of very-low-density lipoprotein (VLDL) to be eventually stored in the adipose tissue [85]. Vitamin E catabolism usually begins with the rate limiting step in which ω-hydroxylation takes place as mediated via CYP4F2/3A4 enzymes [156]. The metabolites are then conjugated and excreted whether in feces or urine [156, 157].
Similar to other fat-soluble vitamins, vitamin E shows a cross interaction with GM [10]. A study by Choi et al. on mice confirmed differences between GM profiles of high dietary α–tocopherol group and the other which intakes lower dose [158]. Likewise, in a study on male subjects, intake of 400 IU of α–tocopherol form of vitamin E twice daily affected GM by reducing Lactobacillaceae and Bacteroides abundance [50]. Studies further revealed that GM could alter vitamin E lifespan in the intestine by activating its metabolism by CYP450-dependent pathway [159].
Vitamin E can be found in large quantities in legume seeds, almond, butter, tomato, and leafy vegetables (e.g., beet greens, collard greens, spinach) [85]. It also can be found in oils such as sunflower, safflower, soybean oil, and the germ oil of cereal grains [160, 161]. Concerning the daily requirements of vitamin E among both sexes and at different life stages, it has been summarized in Table 2 and explained below.
Anti-oxidant activity of vitamin E has been studied intensively and correlated mainly to CD36 scavenger receptor and Fatty acids translocase (FAT) modulation as shown in Table 1 [43,44,45]. Vitamin E was reported as immunostimulatn by promoting interleukin (IL)-2 production, boostering T cell dividing capability [47]. On the other hand, vitamin E oxidized metabolite α-tocopheryl quinone (α-TQ) has been reported to be an emerging plasma biomarker of lipotoxicity in subjects with fatty liver [48]. In a study on fatty liver patients, α-TQ was positively correlated with liver dysfunction and metabolic failure, which could help in early prediction of non-alcoholic fatty liver disease (NAFLD) and nonalcoholic steatohepatitis (NASH) progression [48, 49].
Vitamin E profile at different stages of life
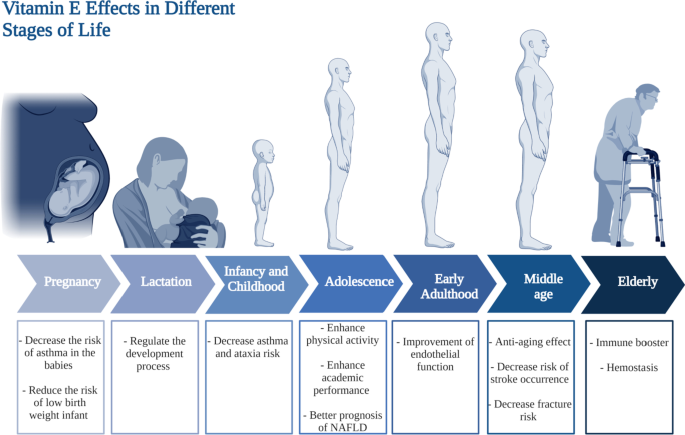
Preconception and pregnancy
Conflicting results have been presented regarding the role of vitamin E in pregnancy. One study suggests that it has antioxidant properties, hence combatting the oxidative stress in the body [162]. An increased level of oxidative stress may lead to pre-eclampsia and premature rupture of membranes (PROM) [162]. Another hypothesizes that vitamin E supplementation during pregnancy does not prevent pre-eclampsia or PROM [163]. Furthermore, a recent review that assessed several trials reached the conclusion that supplementation of any vitamins before or during pregnancy does not prevent the occurrence of miscarriages [164]. On another note, a recent study that included 1924 children found that lower maternal vitamin E supplementation during pregnancy was associated with an increased risk of children being diagnosed with asthma in their first 10 years [165]. To sum up, the role of vitamin E during pregnancy remains controversial, and further clinical investigations are needed to uncover it.
Lactation
In an observational study in which very low birth weights infants’ plasma retinol and alpha-tocopherol levels were measured, at different stages during lactation; vitamin E deficiency has been found to correlate with very low birth weights in new born infants [166]. Physiologically, the level of vitamin E in the milk tends to decrease with the progression of lactation, highlighting the importance of modifying and increasing the recommended dose of vitamin E supplementation [167]. Other factors to influence vitamin E content of the milk include mother’s age, the mother’s vitamin E supplementation, maternal obesity, smoking and the gestational age [167, 168]. Therefore, a customized supplementation of vitamin E should be prescribed to the lactating mother based on her status and medical conditions.
Infancy and childhood
Vitamin E influences several health outcomes during infancy and childhood. Similar to vitamin D, vitamin E plays an important role in the pathogenesis of asthma. In a clinical trial that recruited 1924 children, vitamin E intake was found to be associated with a decreased risk of children being diagnosed with asthma as shown in Fig. 5 [165]. Additionally, several reports recommend vitamin E supplementation as a potential cheap prophylactic for asthma [169]. Ataxia with vitamin E deficiency is an unusual autosomal recessive disorder [170], however all patients who suffer from ataxia since childhood should be tested for vitamin E deficiency, and consequently their treatment protocol should contain high doses of vitamin E [170]. Moreover, higher vitamin E intake during early childhood will decrease the chances of elevated levels of mid-childhood ALT [171].
Adolescence
Vitamin E has shown significant effect on the health of people at the adolescence age [172]. In a study done on 120 school students aged between 15 and 18 years old, high serum levels of α- and γ-tocopherol elicited an enhancement in the academic performance and students’ physical activity [172]. In addition, vitamin E could play a role in the adolescence age that leads to better prognosis in cases of non-alcoholic fatty liver disease (NAFLD) [173]. Studies have revealed that adolescent patients with NAFLD could show moderate improvement in liver biomarkers and histology when treated by tocotrienol form of vitamin E (Fig. 5) [173].
Adulthood
Vitamin E, the antioxidant vitamin, is essential for all age groups. A meta-analysis which included several randomized controlled trials, found a beneficial effect of vitamin E supplementation, specifically in the form of alpha-tocopherol on subclinical levels of inflammation in adults [174]. Another review that revised clinical trials involving adults 18 years of age or older, vitamin E or C supplementation alone, improve endothelial functions [175]. The importance of vitamin E supplementation for middle-aged adults cannot be over-emphasized. It serves as a protective agent against several common and serious adverse health outcomes in that age group. A randomized controlled trials evaluated the effect of a capsulated serum containing a mixture that includes vitamin E exhibiting antiaging and brightening effects of skin [176]. In terms of cardiac health, a recent meta-analysis showed a significant inverse relationship between intake of vitamin E and the risk of stroke occurrence [177]. For skeletal health, fracture risk at any site is significantly decreased when vitamin E intake is increased in men [178]. Collectively, the anti-aging and protecting effects of vitamin E are the main reasons for which vitamin E supplementation during middle age is important.
Elderly
Vitamin E has long been reported to act as immune booster in senior population [15, 179, 180]. Although the recommended dose for adults is 15 mg, recommended dose for elder population ranges from 400 to 800 mg daily [85]. Among 32 healthy elderlies, the group that received regular administration of 800 mg of vitamin E (α-tocopheryl acetate) has shown improvement in immunity likely mediated by decrease in plasma lipid peroxides and/or PGE2 synthesized by peripheral blood mononuclear cells (PBMCs) [179]. In parallel, recent clinical trial on elderly residents aged above 65 years old assessed the effect of vitamin E daily administration E for a year on respiratory tract infections (RTIs) susceptibility [181]. Daily use of 200 IU vitamin E per day have significantly protected subjects from upper RTIs [181]. Furthermore, risk of pneumonia was found to be remarkably lower in elderly smokers who receive vitamin E supplementation versus placebo group [182]. Additionally, vitamin E exerted haptoglobin genotype-dependent prevention of brain-related problems in type 2 diabetic elderlies [183]. Therefore, vitamin E daily supplementation would be in general highly recommended for senior population [85]. On the other hand, vitamin E deficiency happens rarely in elderlies in cases of fats malabsorption, pancreatic problems, coeliac disease, or enteritis [85]. On the other hand, hypervitaminosis E should be avoided for its accompanied complications. Daily vitamin E overdoses was linked to inhibition of platelet aggregation, diarrhea, nausea, endocrine dysfunction, cardiovascular problems, exhaustion, and muscle weakness [184].
Sex effect
It has been reported that vitamin E requirements among both sexes is the same which is 15 mg/day according to the national institute of health (NIH) as presented in Table 2. Yet, a recent study showed that vitamin E supplementation among males might increase the risk of developing prostate cancer [185].
Vitamin K
Vitamin K is a well-recognized vitamin in terms of its indisputable role in hemostasis through its participation in the post-translational modifications of several coagulation factors [51]. Nevertheless, it’s also involved in connective tissue calcification [186]. Different molecular forms of vitamin K could come from different sources. For instance, vitamin K1 (Phylloquinone) is of plant origin. It is mostly synthesized in photosynthetic organisms such as green plants [186]. For vitamin K2 (Menaquinones), it is mainly synthesized by the anaerobic intestinal flora [51, 85].
Vitamin K: metabolism, dietary sources, functions, and signaling pathways
Vitamin K that comes from diet is absorbed by micelles formation upon mixing with bile salts. The more the fatty content in the meal, the more efficient is its absorption [186]. When taken up by enterocytes, vitamin K and other dietary fats are packed together into the chylomicrons to enter the circulation [51]. While phylloquinone are being transported by the chylomicron, menaquinones is usually transported by the VLDL or low-density lipoprotein (LDL), and both are taken up the liver via lipoprotein receptors [51]. The metabolism of phylloquinone and menaquinone starts with ω-hydroxylation, then β-oxidation of the polyisoprenoic side chain into shorter carboxylic acids takes place in the mitochondria to allow glucuronidation which is followed by urine or bile excretion [187].
Vitamin K bioactive forms could be found in various sources. Menaquinones are present in bovine liver and fermented cheeses. However, menaquinones are rarely found in fish except for eel [186]. On the contrary, phylloquinones are mainly present in green leafy vegetables as previously mentioned such as lettuce, chard, parsley, spinach, cabbage, broccoli, kale, and other green cruciferous vegetables [186, 188]. As previously mentioned, vitamin K content is largely influenced by GM [10, 189, 190]. In this context, any disturbance to the GM would affect vitamin K production levels [191]. However, vitamin K could also affect GM composition [10]. A study on mice groups revealed that treatment with vitamin K could have anti-carcinogenic effect, which in turn decreases the risk of colorectal cancer via affecting GM profile [55].
Vitamin K is important for the synthesis of prothrombin and is considered as key player in posttranslational activation of coagulation factors as mentioned earlier [192]. Intriguingly, not only coagulation factors which are currently known to need vitamin-k-depended γ-carboxylation, but also Gla proteins have been found to undergo posttranslational γ-carboxylation [186]. Gla proteins have been known, so far, to be involved in blood coagulation and connective tissue mineralization [193]. Moreover, four Gla proteins function as transmembrane receptors, one binds the hyaluronic acid, one acts as growth-factor-like signaling molecule, and one is γ-carboxylase [193].
Aside of its role in prothrombin synthesis, vitamin K is also involved in the development of central nervous system (CNS) by participating in sphingolipids biosynthesis which are essential component of the brain cell membranes [53, 54]. Moreover, in the presence of nerve growth factor (NGF), vitamin K can potentiate neurite outgrowth. This action was found to be mediated by protein kinase A (PKA) and mitogen-activated protein kinase (MAPK) in neuronal PC12D cells [53, 194].
Vitamin K profile at different life stages
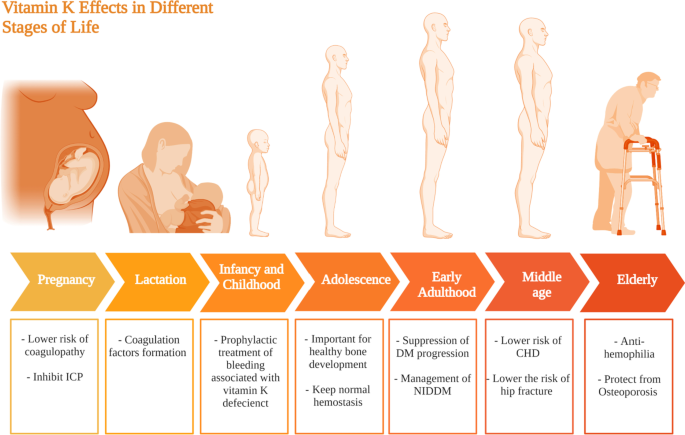
Preconception and pregnancy
A study by Maldonado et al. reported that pregnant women who experience intrahepatic cholestasis of pregnancy (ICP): intense itching in late pregnancy due to liver condition, are considered to be at risk of vitamin K deficiency as shown in Fig. 6 and they need coagulation profile follow-up to avoid coagulopathy complications during labor [195, 196].
Lactation
Vitamin K is naturally present in mother’s milk [197], even though its level has been found to be low in developed countries [198]. Its supplementation to the mother increases its levels in the milk, which subsequently increases its levels in breastfed infants [197]. Nonetheless, maternal vitamin K supplementation cannot substitute vitamin K supplementation to the newly born [197]. The importance of vitamin K to the newborn, stems from its role in the formation of coagulation factors as shown in Fig. 6. Vitamin K deficiency bleeding can be life threatening [199]. It is classified as early; within the first day of birth, classic; within the first week of birth, and late; within the first 2 weeks to 6 months of age [199]. Therefore, it is of importance that all newborns receive vitamin K prophylaxis [199, 200].
Infancy and childhood
Similar to pregnancy, vitamin K supplementation is considered vital it serves as a prophylactic treatment of vitamin K deficiency bleeding (VKDB) [199]. VKDB usually manifests as intra-cranial or mucosal hemorrhages manifested as nodular purpura in an 9 month old infant [201]. Infants with cystic fibrosis suffer from an increased risk of developing vitamin K coagulopathy, therefore adding vitamin K supplementation to their treatment protocol would aid prevent further complications [202, 203]. On the other hand, vitamin K levels were found much higher in children with febrile seizures compared to age-matched healthy controls (33,045,823) suggesting that it has a potential role in the etiopathogenesis of febrile seizures in children. In conclusion, further studies are recommended as vitamin K supplementation’s effect on infants and children is still not that clear compared to other fat soluble vitamins.
Adolescence
Vitamin K is important in the adolescence age for good bone health. Between 155 and 188 μg vitamin K per day is required to maintain healthy bone development [204]. In addition, daily 54–62 μg vitamin K/Kg is needed for normal hemostasis [204]. Yet, evidences showed that during adolescence vitamin K is important for bone health more than hemostasis [204,205,206].
Adulthood
Vitamin K has several beneficial effects regarding diabetes mellitus among adults, with several studies pointing for a beneficial effect on insulin sensitivity and glycemic status of diabetic patients, leading to suppression of the progression of the disease as summarized in Fig. 6 [207, 208]. It is also worth mentioning that Vitamin K2 in particular was found to exert a better effect on type 2 diabetes mellitus patients compared to vitamin K1 [209].
Elderly
Previous studies have shown that vitamin K low levels has been directly associated with poor cognitive functions among senior populations [210]. Likewise, data obtained from the nationwide Cardiovascular disease in Norway suggested that a higher intake of vitamin K2 is associated with a lower risk of coronary heart disease [211]. This conclusion is supported by a study revealing that reduced levels of both vitamin D and K, is associated with adverse cardiac remodeling, and generally all-cause of mortality in men and women [212]. In terms of skeletal health, vitamin K deficiency was found to be prevalent among hip fracture patients [213].
Phylloquinone deficiency in elderly is one of the major causes of hemophilia, in particular, in the gastrointestinal tract, attributed to the absence of coagulation factors that are vitamin-K-dependent. In addition, other studies revealed the involvement of vitamin K deficiency in osteoporosis via alteration of Gla protein osteocalcin activity [92, 214]. Osteocalcin problems are usually linked to bone fractures in senior population. Nevertheless, vitamin K supplements was found to remarkably decrease the probability of hip fractures in individuals older than 75 years old [85].
Sex effect
It has been reported that the daily requirements of vitamin K among both sexes slightly differs as it is recommended for males to have around 120 µg/day while females requirements are fulfilled with only 90 µg/day as summarized in Table 2 [85].
Conclusion
In conclusion, this review article is considered an updated comprehensive overview shedding the light onto the potential role of fat-soluble vitamins at every stage of human's life. During pregnancy, it has been found that vitamin A is essential for normal morphological development for the fetus while vitamin D appears to act as a protective shield against gestational diabetes and preeclampsia. Nonetheless, vitamins E was found to have essential role in decreasing the risk of developing low-birth weight infants whereas vitamin K decreases the risk of coagulopathy among pregnant women. It has been also highlighted that vitamins supplementation during lactation is of potential since some vitamins are of high prophylactic significance such as vitamin D. Vitamin D acts as a preventive measurement from autism, asthma, and rickets diseases in newborn and children. Also, it was highlighted that fat-soluble vitamins when taken in proper quantities, are critical for normal function, growth, and maintenance of tissues as highlighted, though can be toxic warranting for their administration at optimum doses. The study emphasizes on the significant difference between males and females' daily vitamins requirements to aid clinicians decide on best regimen, and as well to highlight for future needed research in that field. The crosstalk between fat-soluble vitamins and GM has also been highlighted. However, the interaction between sex tissues and fat-soluble vitamins was only outlined in case of vitamin A and D highlighting a promising gap that needs to be further studied. Our study warrants for further investigation on the roles of fat soluble vitamins in several pathological conditions such as cancer, autoimmune diseases, infectious diseases and neurodegenerative diseases.
Availability of data and materials
Data sharing is not applicable to this review since no datasets were generated or analyzed during the current article.
References
Nur SM, Rath S, Ahmad V, Ahmad A, Ateeq B, Khan MI. Nutritive vitamins as epidrugs. Crit Rev Food Sci Nutr. 2021;61(1):1–13. https://doi.org/10.1080/10408398.2020.1712674.
Semba RD. The discovery of the vitamins. Int J Vitam Nutr Res. 2012;82(5):310–5. https://doi.org/10.1024/0300-9831/A000124.
Albahrani AA, Greaves RF. Fat-soluble vitamins: clinical indications and current challenges for chromatographic measurement. Clin Biochem Rev. 2016;37(1):27–47.
Yang CY, Leung PSC, Adamopoulos IE, Gershwin ME. The implication of vitamin D and autoimmunity: a comprehensive review. Clin Rev Allergy Immunol. 2013;45(2):217–26. https://doi.org/10.1007/S12016-013-8361-3.
Dankers W, Colin EM, van Hamburg JP, Lubberts E. Vitamin D in autoimmunity: molecular mechanisms and therapeutic potential. Front Immunol. 2017. https://doi.org/10.3389/FIMMU.2016.00697.
Pisetpackdeekul P, et al. Proretinal nanoparticles: stability, release, efficacy, and irritation. Int J Nanomed. 2016;11:3277. https://doi.org/10.2147/IJN.S111748.
Timoneda J, et al. Vitamin A deficiency and the lung. Nutrients. 2018. https://doi.org/10.3390/NU10091132.
Kangas ST, et al. Vitamin A and iron status of children before and after treatment of uncomplicated severe acute malnutrition. Clin Nutr. 2020;39(11):3512–9. https://doi.org/10.1016/J.CLNU.2020.03.016.
Herschel Conaway H, Henning P, Lerner UH. Vitamin a metabolism, action, and role in skeletal homeostasis. Endocr Rev. 2013;34(6):766–97. https://doi.org/10.1210/ER.2012-1071.
Stacchiotti V, Rezzi S, Eggersdorfer M, Galli F. Metabolic and functional interplay between gut microbiota and fat-soluble vitamins. Crit Rev Food Sci Nutr. 2020. https://doi.org/10.1080/10408398.2020.1793728.
Li C, Zhao Z, Zhou J, Liu Y, Wang H, Zhao X. Relationship between the TERT, TNIP1 and OBFC1 genetic polymorphisms and susceptibility to colorectal cancer in Chinese Han population. Oncotarget. 2017;8(34):56932. https://doi.org/10.18632/ONCOTARGET.18378.
Tlaskalová-Hogenová H, et al. The role of gut microbiota (commensal bacteria) and the mucosal barrier in the pathogenesis of inflammatory and autoimmune diseases and cancer: contribution of germ-free and gnotobiotic animal models of human diseases. Cell Mol Immunol. 2011;8(2):110–20. https://doi.org/10.1038/cmi.2010.67.
Faustino JF, et al. Vitamin A and the eye: an old tale for modern times. Arq Bras Oftalmol. 2016;79(1):56–61. https://doi.org/10.5935/0004-2749.20160018.
Lanska DJ Chapter 29 Historical aspects of the major neurological vitamin deficiency disorders. Overview and fat-soluble vitamin A. Handb Clin Neurol. 2009;95:435–444. https://doi.org/10.1016/S0072-9752(08)02129-5
Erkelens MN, Mebius RE. Retinoic acid and immune homeostasis: a balancing act. Trends Immunol. 2017;38(3):168–80. https://doi.org/10.1016/J.IT.2016.12.006.
Clagett-Dame M, Knutson D. Vitamin A in reproduction and development. Nutrients. 2011;3(4):385–428. https://doi.org/10.3390/NU3040385.
Bar-El Dadon S, Reifen R. Vitamin A and the epigenome”. Crit Rev Food Sci Nutr. 2017;57(11):2404–11. https://doi.org/10.1080/10408398.2015.1060940.
Larange A, Cheroutre H. Retinoic acid and retinoic acid receptors as pleiotropic modulators of the immune system. Annu Rev Immunol. 2016;34:369–94. https://doi.org/10.1146/ANNUREV-IMMUNOL-041015-055427.
McLaren DS, Kraemer K. Vitamin A in nature. World Rev Nutr Diet. 2012;103:7–17. https://doi.org/10.1159/000258434.
Lambert B, et al. Protein interactions of the transcription factor Hoxa1. BMC Dev Biol. 2012;12(1):1–17. https://doi.org/10.1186/1471-213X-12-29/FIGURES/4.
Chen Y, Reese DH. A screen for disruptors of the retinol (Vitamin A) signaling pathway. Birth Defects Res Part B Dev Reprod Toxicol. 2013;98(3):276–82. https://doi.org/10.1002/BDRB.21062.
Barber T, Esteban-Pretel G, Marín MP, Timoneda J. Vitamin a deficiency and alterations in the extracellular matrix. Nutrients. 2014;6(11):4984–5017. https://doi.org/10.3390/NU6114984.
Huang Z, Liu Y, Qi G, Brand D, Zheng SG. Role of Vitamin A in the Immune System. J Clin Med. 2018;7(9):258. https://doi.org/10.3390/JCM7090258.
Green HN, Mellanby E. Vitamin A as an anti-infective agent. Br Med J. 1928;2(3537):691. https://doi.org/10.1136/BMJ.2.3537.691.
DeNucci CC, Pagán AJ, Mitchell JS, Shimizu Y. Control of alpha4beta7 integrin expression and CD4 T cell homing by the beta1 integrin subunit. J Immunol. 2010;184(5):2458–67. https://doi.org/10.4049/JIMMUNOL.0902407.
Kang SG, Park J, Cho JY, Ulrich B, Kim CH. Complementary roles of retinoic acid and TGF-β1 in coordinated expression of mucosal integrins by T cells. Mucosal Immunol. 2011;4(1):66–82. https://doi.org/10.1038/MI.2010.42.
Ghodratizadeh S, Kanbak G, Beyramzadeh M, Dikmen ZG, Memarzadeh S, Habibian R. Effect of carotenoid β-cryptoxanthin on cellular and humoral immune response in rabbit. Vet Res Commun. 2014;38(1):59–62. https://doi.org/10.1007/S11259-013-9584-8.
Mourik BC, et al. Immunotherapy added to antibiotic treatment reduces relapse of disease in a mouse model of tuberculosis. Am J Respir Cell Mol Biol. 2017;56(2):233–41. https://doi.org/10.1165/RCMB.2016-0185OC/SUPPL_FILE/DISCLOSURES.PDF.
Wheelwright M, et al. All-trans retinoic acid-triggered antimicrobial activity against mycobacterium tuberculosis is dependent on NPC2. J Immunol. 2014;192(5):2280–90. https://doi.org/10.4049/JIMMUNOL.1301686/-/DCSUPPLEMENTAL.
Zamzami MA, Nasrullah M, Choudhry H, Khan MI. A study on the effect of vitamins A and C to modulate the expression of NKG2D ligands in hepatic and colon cancer cells. Nutr Cancer. 2021;73(11–12):2751–62. https://doi.org/10.1080/01635581.2020.1860240.
Cabezas-Wallscheid N, et al. Vitamin A-retinoic acid signaling regulates hematopoietic stem cell dormancy. Cell. 2017;169(5):807-823.e19. https://doi.org/10.1016/J.CELL.2017.04.018.
Duriancik DM, Lackey DE, Hoag KA. Vitamin A as a regulator of antigen presenting cells. J Nutr. 2010;140(8):1395–9. https://doi.org/10.3945/JN.110.124461.
Doyle TJ, Braun KW, McLean DJ, Wright RW, Griswold MD, Kim KH. Potential functions of retinoic acid receptor A in sertoli cells and germ cells during spermatogenesis. Ann NY Acad Sci. 2007;1120(1):114–30. https://doi.org/10.1196/ANNALS.1411.008.
Guo H, Guo J, Xie W, Yuan L, Sheng X. The role of vitamin D in ovarian cancer: epidemiology, molecular mechanism and prevention. J Ovarian Res. 2018;11(1):1–8. https://doi.org/10.1186/S13048-018-0443-7/FIGURES/1.
Chen L, et al. Inflammatory responses and inflammation-associated diseases in organs. Oncotarget. 2018;9(6):7204. https://doi.org/10.18632/ONCOTARGET.23208.
Jiang F, Bao J, Li P, Nicosia SV, Bai W. Induction of ovarian cancer cell apoptosis by 1,25-dihydroxyvitamin D3 through the down-regulation of telomerase*. J Biol Chem. 2004;279(51):53213–21. https://doi.org/10.1074/JBC.M410395200.
Maj E, Filip-Psurska B, Milczarek M, Psurski M, Kutner A, Wietrzyk J. Vitamin D derivatives potentiate the anticancer and anti-angiogenic activity of tyrosine kinase inhibitors in combination with cytostatic drugs in an A549 non-small cell lung cancer model. Int J Oncol. 2018;52(2):337–66. https://doi.org/10.3892/IJO.2017.4228/HTML.
Boisen IM, Bøllehuus Hansen L, Mortensen LJ, Lanske B, Juul A, Blomberg Jensen M. Possible influence of vitamin D on male reproduction. J Steroid Biochem Mol Biol. 2017;173:215–22. https://doi.org/10.1016/J.JSBMB.2016.09.023.
Jensen MB, et al. Vitamin D is positively associated with sperm motility and increases intracellular calcium in human spermatozoa. Obstet Gynecol Surv. 2011;66(9):556–8. https://doi.org/10.1097/OGX.0B013E31823B65E0.
Canguven O, Talib RA, El Ansari W, Yassin DJ, Al Naimi A. Vitamin D treatment improves levels of sexual hormones, metabolic parameters and erectile function in middle-aged vitamin D deficient men. Aging Male. 2017;20(1):9–16. https://doi.org/10.1080/13685538.2016.1271783.
Sousa GFD, et al. Flavonol triglycosides of leaves from Maytenus robusta with acetylcholinesterase inhibition. Phytochem Lett. 2017;19:34–8. https://doi.org/10.1016/J.PHYTOL.2016.10.024.
Naderpoor N, Mousa A, Arango LFG, Barrett HL, Nitert MD, de Courten B. Effect of Vitamin D supplementation on faecal microbiota: a randomised clinical trial. Nutrients. 2019;11(12):2888. https://doi.org/10.3390/NU11122888.
Munteanu A, Taddei M, Tamburini I, Bergamini E, Azzi A, Zingg JM. Antagonistic effects of oxidized low density lipoprotein and α-tocopherol on CD36 scavenger receptor expression in monocytes: involvement of protein kinase B and peroxisome proliferator-activated receptor-γ *. J Biol Chem. 2006;281(10):6489–97. https://doi.org/10.1074/JBC.M508799200.
Zingg JM, Azzi A, Meydani M. α-tocopheryl phosphate induces VEGF expression via CD36/PI3Kγ in THP-1 monocytes. J Cell Biochem. 2017;118(7):1855–67. https://doi.org/10.1002/JCB.25871.
Zingg JM. Vitamin E: regulatory role on signal transduction. IUBMB Life. 2019;71(4):456–78. https://doi.org/10.1002/IUB.1986.
Silverstein RL, Febbraio M. CD36, a scavenger receptor involved in immunity, metabolism, angiogenesis, and behavior. Sci Signal. 2009. https://doi.org/10.1126/SCISIGNAL.272RE3.
Meydani SN, Han SN, Wu D. Vitamin E and immune response in the aged: molecular mechanisms and clinical implications. Immunol Rev. 2005;205(1):269–84. https://doi.org/10.1111/J.0105-2896.2005.00274.X.
Torquato P, et al. Increased plasma levels of the lipoperoxyl radical-derived vitamin E metabolite α-tocopheryl quinone are an early indicator of lipotoxicity in fatty liver subjects. Free Radic Biol Med. 2019;131:115–25. https://doi.org/10.1016/J.FREERADBIOMED.2018.11.036.
Galli F, et al. Vitamin E: emerging aspects and new directions. Free Radic Biol Med. 2017;102:16–36. https://doi.org/10.1016/J.FREERADBIOMED.2016.09.017.
Kim DJ, et al. Ursodeoxycholic acid improves liver function via phenylalanine/tyrosine pathway and microbiome remodelling in patients with liver dysfunction. Sci Reports. 2018;8(1):1–11. https://doi.org/10.1038/s41598-018-30349-1.
Vermeer C. Vitamin K: the effect on health beyond coagulation–an overview. SNF Swedish Nutr Found. 2012. https://doi.org/10.3402/FNR.V56I0.5329.
Aljafary MA et al. Physiological and cellular functions of vitamin K on cardiovascular function. 2022. https://doi.org/10.5772/INTECHOPEN.99344.
Ferland G. Vitamin K and the nervous system: an overview of its actions. Adv Nutr. 2012;3(2):204–12. https://doi.org/10.3945/AN.111.001784.
Edwards JL, et al. Apparent requirement for vitamin K of rumen strains of fusiformis nigrescens”. Nature. 1958;181(4603):203–4. https://doi.org/10.1038/181203a0.
Zheng X, et al. Bile acid is a significant host factor shaping the gut microbiome of diet-induced obese mice. BMC Biol. 2017;15(1):1–15. https://doi.org/10.1186/S12915-017-0462-7/FIGURES/5.
M. T. Cabezuelo, R. Zaragozá, T. Barber, and J. R. Viña, “Role of Vitamin A in Mammary Gland Development and Lactation,” Nutr. 2020, Vol. 12, Page 80, vol. 12, no. 1, p. 80, Dec. 2019, doi: https://doi.org/10.3390/NU12010080.
Maia SB, et al. Vitamin A and pregnancy: a narrative review. Nutrients. 2019. https://doi.org/10.3390/NU11030681.
D’Ambrosio DN, Clugston RD, Blaner WS. Vitamin A metabolism: an update. Nutrients. 2011;3(1):63–103. https://doi.org/10.3390/NU3010063.
Pacifici GM. Clinical pharmacology of phenobarbital in neonates: effects, metabolism and pharmacokinetics. Curr Pediatr Rev. 2016;12(1):48–54. https://doi.org/10.2174/1573397111666151026223914.
McGuire S. WHO guideline: vitamin A supplementation in pregnant women. Geneva: WHO, 2011; WHO guideline: vitamin A supplementation in postpartum women. Geneva: WHO, 2011. Adv Nutr. 2012;3(2):215–6. https://doi.org/10.3945/AN.111.001701.
West KP. Vitamin A deficiency disorders in children and women. Food Nutr Bull. 2003;24(4 SUPPLEMENT):S78–90. https://doi.org/10.1177/15648265030244s104.
Mansur JL. Vitamin D in pediatrics, pregnancy and lactation. Arch Argent Pediatr. 2018;116(4):286–90. https://doi.org/10.5546/AAP.2018.286.
Matamoros N, Visentin S, Ferrari G, Falivene M, Fasano V, González HF. Vitamin A content in mature breast milk and its adequacy to the nutritional recommendations for infants. Arch Argent Pediatr. 2018;116(2):146–9. https://doi.org/10.5546/AAP.2018.ENG.146.
Palmer AC, Schulze KJ, Khatry SK, De Luca LM, West KP. Maternal vitamin A supplementation increases natural antibody concentrations of preadolescent offspring in rural Nepal. Nutrition. 2015;31(6):813–9. https://doi.org/10.1016/J.NUT.2014.11.016.
Haider BA, Bhutta ZA. Neonatal vitamin A supplementation: time to move on. Lancet. 2015;385(9975):1268–71. https://doi.org/10.1016/S0140-6736(14)62342-4.
Viner RM, et al. Life course epidemiology: recognising the importance of adolescence. J Epidemiol Community Heal. 2015;69(8):719–20. https://doi.org/10.1136/JECH-2014-205300.
Campisi SC, Khan A, Zasowski C, Bhutta ZA. Malnutrition. Textb Pediatr Gastroenterol Hepatol Nutr. 2022. https://doi.org/10.1007/978-3-030-80068-0_44.
Li L, et al. Fast food consumption among young adolescents aged 12–15 years in 54 low- and middle-income countries. Glob Health Action. 2020. https://doi.org/10.1080/16549716.2020.1795438/SUPPL_FILE/ZGHA_A_1795438_SM4883.DOCX.
Smith L, et al. Food insecurity (hunger) and fast-food consumption among 180 164 adolescents aged 12–15 years from sixty-eight countries. Br J Nutr. 2020. https://doi.org/10.1017/S0007114521001173.
Fazio-Tirrozzo G, Brabin L, Brabin B, Agbaje O, Harper G, Broadhead R. A community based study of vitamin A and vitamin E status of adolescent girls living in the Shire valley, Southern Malawi. Eur J Clin Nutr. 1998;52(9):637–42. https://doi.org/10.1038/sj.ejcn.1600622.
Harika R, Faber M, Samuel F, Mulugeta A, Kimiywe J, Eilander A. Are low intakes and deficiencies in iron, vitamin A, zinc, and iodine of public health concern in Ethiopian, Kenyan, Nigerian, and South African children and adolescents? Food Nutr Bull. 2017;38(3):405–27. https://doi.org/10.1177/0379572117715818.
Wang R, et al. Serum vitamin A nutritional status of children and adolescents aged 6–17 years—China, 2016–2017. China CDC Wkly. 2021;3(9):189. https://doi.org/10.46234/CCDCW2021.057.
Martini S, et al. Vitamin A deficiency due to selective eating as a cause of blindness in a high-income setting. Pediatrics. 2018. https://doi.org/10.1542/PEDS.2016-2628.
El-Shaheed AA, Fahmy RF, El-Zayat SR, Sibaii H, Mahfouz NN, Moustafa RS. A new insight into the immune regulatory functions of vitamin A in children and adolescents. J Arab Soc Med Res. 2018;13(1):1. https://doi.org/10.4103/JASMR.JASMR_30_17.
Sk P, Chaturvedi A, Bhardwaj A, Chandra S, Naik G, Hb S. Effect of vitamin A supplements with iron therapy among adolescent girls. Int J Physiol. 2019;7(3):45–51.
Lonardo A, et al. Sex differences in nonalcoholic fatty liver disease: state of the art and identification of research gaps. Hepatology. 2019;70(4):1457–69. https://doi.org/10.1002/HEP.30626.
Monteleone P, Mascagni G, Giannini A, Genazzani AR, Simoncini T. Symptoms of menopause—global prevalence, physiology and implications. Nat Rev Endocrinol. 2018;14(4):199–215. https://doi.org/10.1038/nrendo.2017.180.
Blumberg JB, Bailey RL, Sesso HD, Ulrich CM. The Evolving Role of Multivitamin/Multimineral Supplement Use among Adults in the Age of Personalized Nutrition. Nutr. 2018;10(2):248. https://doi.org/10.3390/NU10020248.
Park JA, Lee JH, Lee HJ, Jin BH, Bae KH. Association of some vitamins and minerals with periodontitis in a nationally representative sample of Korean Young Adults. Biol Trace Elem Res. 2017;178(2):171–9. https://doi.org/10.1007/S12011-016-0914-X/TABLES/5.
Iskakova M, Karbyshev M, Piskunov A, Rochette-Egly C. Nuclear and extranuclear effects of vitamin A1. Can J Physiol Pharmacol. 2015;93(12):1065–75. https://doi.org/10.1139/CJPP-2014-0522.
Correa-Rodríguez M, Luis Gómez-Urquiza J, Medina-Martínez I, González-Jiménez E, Schmidt-Riovalle J, Rueda-Medina B. Low intakes of vitamins C and A are associated with obesity in early adulthood. Int J Vitamin Nutr Res. 2022. https://doi.org/10.1024/0300-9831/A000661.
De Oliveira MR. Vitamin A and retinoids as mitochondrial toxicants. Oxid Med Cell Longev. 2015. https://doi.org/10.1155/2015/140267.
Zhang X, et al. The effect of vitamin A on fracture risk: a meta-analysis of cohort studies. Int J Environ Res Public Heal. 2017;14(9):1043. https://doi.org/10.3390/IJERPH14091043.
Ramdas WD, Schouten JSAG, Webers CAB. The effect of vitamins on glaucoma: a systematic review and meta-analysis. Nutrients. 2018;10(3):359. https://doi.org/10.3390/NU10030359.
Csapó J, Albert C, Prokisch J. The role of vitamins in the diet of the elderly I. Fat-soluble vitamins. Acta Univ Sapientiae Aliment. 2017;10(1):127–45. https://doi.org/10.1515/AUSAL-2017-0009.
Bento C, Matos AC, Cordeiro A, Ramalho A. Vitamin A deficiency is associated with body mass index and body adiposity in women with recommended intake of vitamin A. Nutr Hosp. 2018;35(5):1072–8. https://doi.org/10.20960/NH.1630.
De Jonge EAL, et al. Dietary vitamin A intake and bone health in the elderly: the Rotterdam study. Eur J Clin Nutr. 2015;69(12):1360–8. https://doi.org/10.1038/ejcn.2015.154.
Huang T, Lin BM, Redline S, Curhan GC, Hu FB, Tworoger SS. Type of menopause, age at menopause, and risk of developing obstructive sleep apnea in postmenopausal women. Am J Epidemiol. 2018;187(7):1370–9. https://doi.org/10.1093/AJE/KWY011.
Wiacek M, Zubrzycki IZ, Bojke O, Kim HJ. Menopause and age-driven changes in blood level of fat- and water-soluble vitamins. Climacteric. 2013;16(6):689–99. https://doi.org/10.3109/13697137.2012.742504.
Livera G, Rouiller-Fabre V, Pairault C, Levacher C, Habert R. Regulation and perturbation of testicular functions by vitamin A. Reproduction. 2002;124(2):173–80.
Hogarth CA, Griswold MD. The key role of vitamin A in spermatogenesis. J Clin Invest. 2010;120(4):956–62. https://doi.org/10.1172/JCI41303.
Troesch B, Eggersdorfer M, Weber P. 100 Years of vitamins: adequate intake in the elderly is still a matter of concern. J Nutr. 2012;142(6):979–80. https://doi.org/10.3945/JN.112.157826.
Wu F, Juonala M, Pitkänen N, Jula A, Lehtimäki T, Sabin MA, Pahkala K, Hutri-Kähönen N, Kähönen M, Laitinen T, Viikari JSA, Magnussen CG, Raitakari OT. Both youth and long-term vitamin D status is associated with risk of type 2 diabetes mellitus in adulthood: a cohort study. Ann Med. 2018;50(1):74–82. https://doi.org/10.1080/07853890.2017.1399446.
Chang SW, Lee HC. Vitamin D and health - the missing vitamin in humans. Pediatr Neonatol. 2019;60(3):237–44. https://doi.org/10.1016/J.PEDNEO.2019.04.007.
Farach-Carson M, Nemere I. Membrane receptors for vitamin D steroid hormones: potential new drug targets. Curr Drug Targets. 2003;4(1):67–76. https://doi.org/10.2174/1389450033347118.
Nykjaer A, et al. An endocytic pathway essential for renal uptake and activation of the steroid 25-(OH) vitamin D3. Cell. 1999;96(4):507–15. https://doi.org/10.1016/S0092-8674(00)80655-8.
Bikle DD. Vitamin D metabolism, mechanism of action, and clinical applications. Chem Biol. 2014;21(3):319–29. https://doi.org/10.1016/J.CHEMBIOL.2013.12.016.
Giustina A et al. Consensus statement from 2nd International Conference on Controversies in Vitamin D. Rev Endocr Metab Disord. 2020;21(1): 89. https://doi.org/10.1007/S11154-019-09532-W.
Arslan S, Akdevelioğlu Y. The relationship between female reproductive functions and vitamin D. J Am College Nutr. 2018;37(6):546–51. https://doi.org/10.1080/07315724.2018.1431160.
Goltzman D. Functions of vitamin D in bone. Histochem Cell Biol. 2018;149(4):305–12. https://doi.org/10.1007/S00418-018-1648-Y/FIGURES/4.
Trump D, Aragon-Ching J. Vitamin D in prostate cancer. Asian J Androl. 2018;20(3):244. https://doi.org/10.4103/AJA.AJA_14_18.
de La Puente-Yagüe M, Cuadrado-Cenzual MA, Ciudad-Cabañas MJ, Hernández-Cabria M, Collado-Yurrita L. Vitamin D: and its role in breast cancer. Kaohsiung J Med Sci. 2018;34(8):423–7. https://doi.org/10.1016/J.KJMS.2018.03.004.
Jeon SM, Shin EA. Exploring vitamin D metabolism and function in cancer. Exp Mol Med. 2018;50(4):1–14. https://doi.org/10.1038/s12276-018-0038-9.
Casseb GAS, Kaster MP, Rodrigues ALS. Potential role of vitamin D for the management of depression and anxiety. CNS Drugs. 2019;33(7):619–37. https://doi.org/10.1007/S40263-019-00640-4.
Medrano M, Carrillo-Cruz E, Montero I, Perez-Simon JA. Vitamin D: effect on haematopoiesis and immune system and clinical applications. Int J Mol Sci. 2018;19(9):2663. https://doi.org/10.3390/IJMS19092663.
Carlberg C, Muñoz A. An update on vitamin D signaling and cancer. Semin Cancer Biol. 2022;79:217–30. https://doi.org/10.1016/J.SEMCANCER.2020.05.018.
Sun J. VDR/vitamin D receptor regulates autophagic activity through ATG16L1. Autophagy. 2016;12(6):1057–8. https://doi.org/10.1080/15548627.2015.1072670.
Ishizawa M, Akagi D, Makishima M. Lithocholic acid is a vitamin D receptor ligand that acts preferentially in the ileum. Int J Mol Sci. 2018;19(7):1975. https://doi.org/10.3390/IJMS19071975.
Cyprian F, Lefkou E, Varoudi K, Girardi G. Immunomodulatory Effects of Vitamin D in pregnancy and beyond. Front Immunol. 2019;10:2739. https://doi.org/10.3389/FIMMU.2019.02739/BIBTEX.
Pilz S, et al. The role of vitamin D in fertility and during pregnancy and lactation: a review of clinical data. Int J Enviro Res Public Heal. 2018;15(10):2241. https://doi.org/10.3390/IJERPH15102241.
Agarwal S, Kovilam O, Agrawal DK. Vitamin D and its impact on maternal-fetal outcomes in pregnancy: a critical review. Crit Rev Food Sci Nutr. 2017;58(5):755–69. https://doi.org/10.1080/10408398.2016.1220915.
Elsori DH, Hammoud MS. Vitamin D deficiency in mothers, neonates and children. J Steroid Biochem Mol Biol. 2018;175:195–9. https://doi.org/10.1016/J.JSBMB.2017.01.023.
Khazai N, Judd SE, Tangpricha V. Calcium and vitamin D: Skeletal and extraskeletal health. Curr Rheumatol Rep. 2008;10(2):110–7. https://doi.org/10.1007/S11926-008-0020-Y.
Galthen-Sørensen M, Andersen LB, Sperling L, Christesen HT. Maternal 25-hydroxyvitamin D level and fetal bone growth assessed by ultrasound: a systematic review. Ultrasound Obstet Gynecol. 2014;44(6):633–40. https://doi.org/10.1002/UOG.13431.
Roth DE, et al. Vitamin D supplementation in pregnancy and lactation and infant growth. Obstet Gynecol Surv. 2019;74(1):1–2. https://doi.org/10.1097/OGX.0000000000000636.
Curtis EM, Moon RJ, Harvey NC, Cooper C. Maternal vitamin D supplementation during pregnancy. Br Med Bull. 2018;126(1):57–77. https://doi.org/10.1093/BMB/LDY010.
Kiely ME, Wagner CL, Roth DE. Vitamin D in pregnancy: Where we are and where we should go. J Steroid Biochem Mol Biol. 2020;201: 105669. https://doi.org/10.1016/J.JSBMB.2020.105669.
Fernando M, Ellery SJ, Marquina C, Lim S, Naderpoor N, Mousa A. Vitamin D-binding protein in pregnancy and reproductive health. Nutrrients. 2020;12(5):1489. https://doi.org/10.3390/NU12051489.
Cannell JJ. Vitamin D and autism, what’s new? Rev Endocr Metab Disord. 2017;18(2):183–93. https://doi.org/10.1007/S11154-017-9409-0/FIGURES/2.
Bae YJ, Kratzsch J. Vitamin D and calcium in the human breast milk. Best Pract Res Clin Endocrinol Metab. 2018;32(1):39–45. https://doi.org/10.1016/J.BEEM.2018.01.007.
Kovacs CS. The role of vitamin D in pregnancy and lactation: insights from animal models and clinical studies. Annu Rev Nutr. 2012;32:97–123. https://doi.org/10.1146/ANNUREV-NUTR-071811-150742.
Dawodu A, Salameh KM, Al-Janahi NS, Bener A, Elkum N. The effect of high-dose postpartum maternal vitamin D supplementation alone compared with maternal plus infant vitamin D supplementation in breastfeeding infants in a high-risk population. A randomized controlled trial. Nutrients. 2019;11(7):1632. https://doi.org/10.3390/NU11071632.
Allen KJ, et al. Vitality trial: protocol for a randomised controlled trial to establish the role of postnatal vitamin D supplementation in infant immune health. BMJ Open. 2015;5(12): e009377. https://doi.org/10.1136/BMJOPEN-2015-009377.
Hollis BW, et al. Maternal versus infant vitamin D supplementation during lactation: a randomized controlled trial. Pediatrics. 2015;136(4):625–34. https://doi.org/10.1542/PEDS.2015-1669.
Litonjua AA. Vitamin D and childhood asthma - causation and contribution to disease activity. Curr Opin Allergy Clin Immunol. 2019;19(2):126. https://doi.org/10.1097/ACI.0000000000000509.
Tachimoto H, Mezawa H, Segawa T, Akiyama N, Ida H, Urashima M. Improved control of childhood asthma with low-dose, short-term vitamin D supplementation: a randomized, double-blind, placebo-controlled trial. Allergy. 2016;71(7):1001–9. https://doi.org/10.1111/ALL.12856.
Zisi D, Challa A, Makis A. The association between vitamin D status and infectious diseases of the respiratory system in infancy and childhood. Hormones. 2019;18(4):353–63. https://doi.org/10.1007/S42000-019-00155-Z.
Esposito S, Lelii M. Vitamin D and respiratory tract infections in childhood. BMC Infect Dis. 2015;15(1):1–10. https://doi.org/10.1186/S12879-015-1196-1.
Pacheco-González RM, García-Marcos L, Morales E. Prenatal vitamin D status and respiratory and allergic outcomes in childhood: a meta-analysis of observational studies. Pediatr Allergy Immunol. 2018;29(3):243–53. https://doi.org/10.1111/PAI.12876.
Antonucci R, Locci C, Clemente MG, Chicconi E, Antonucci L. Vitamin D deficiency in childhood: old lessons and current challenges. J Pediatr Endocrinol Metab. 2018;31(3):247–60. https://doi.org/10.1515/JPEM-2017-0391/PDF.
Winzenberg T, Jones G. Vitamin D and bone health in childhood and adolescence. Calcif Tissue Int. 2013;92(2):140–50. https://doi.org/10.1007/S00223-012-9615-4/TABLES/2.
Siracusano M, Riccioni A, Abate R, Benvenuto A, Curatolo P, Mazzone L. Vitamin D deficiency and autism spectrum disorder. Curr Pharm Des. 2020;26(21):2460–74. https://doi.org/10.2174/1381612826666200415174311.
Föcker M, et al. Vitamin D and mental health in children and adolescents. Eur Child Adolesc Psychiatry. 2017;26(9):1043–66. https://doi.org/10.1007/S00787-017-0949-3.
Karras SN, Anagnostis P, Naughton D, Annweiler C, Petroczi A, Goulis DG. Vitamin D during pregnancy: why observational studies suggest deficiency and interventional studies show no improvement in clinical outcomes? a narrative review. J Endocrinol Invest. 2015;38(12):1265–75. https://doi.org/10.1007/S40618-015-0363-Y/TABLES/2.
Karras SN, Anagnostis P, Paschou SA, Kandaraki E, Goulis DG. Vitamin D status during pregnancy: time for a more unified approach beyond borders? Eur J Clin Nutr. 2015;69(8):874–7. https://doi.org/10.1038/ejcn.2015.33.
Lamberg-Allardt C. Vitamin D in children and adolescents. Scand J Clin Lab Invest. 2012;72(SUPPL. 243):124–8. https://doi.org/10.3109/00365513.2012.682885.
T. Society for Adolescent Health, “Recommended vitamin D intake and management of low vitamin D Status in Adolescents: A Position Statement of the Society for Adolescent Health and Medicine The Society for Adolescent Health and Medicine) 801e803,” 2013. https://doi.org/10.1016/j.jadohealth.2013.03.022.
Saggese G, et al. Vitamin D in childhood and adolescence: an expert position statement. Eur J Pediatr. 2015;174(5):565–76. https://doi.org/10.1007/S00431-015-2524-6.
Cui X, et al. Vitamin D and the brain: key questions for future research. J Steroid Biochem Mol Biol. 2015;148:305–9. https://doi.org/10.1016/J.JSBMB.2014.11.004.
Battersby AJ, Kampmann B, Burl S. Vitamin D in early childhood and the effect on immunity to mycobacterium tuberculosis. Clin Dev Immunol. 2012. https://doi.org/10.1155/2012/430972.
Wu F, et al. Both youth and long-term vitamin D status is associated with risk of type 2 diabetes mellitus in adulthood: a cohort study. Ann Med. 2018;50(1):74–82. https://doi.org/10.1080/07853890.2017.1399446/SUPPL_FILE/IANN_A_1399446_SM2378.DOCX.
Ismailova K, Poudel P, Parlesak A, Frederiksen P, Heitmann BL. Vitamin D in early life and later risk of multiple sclerosis—a systematic review, meta-analysis. PLoS One. 2019;14(8): e0221645. https://doi.org/10.1371/JOURNAL.PONE.0221645.
Manoy P, et al. Vitamin D supplementation improves quality of life and physical performance in osteoarthritis patients. Nutrients. 2017;9(8):799. https://doi.org/10.3390/NU9080799.
de Oliveira DL, Hirotsu C, Tufik S, Andersen ML. The interfaces between vitamin D, sleep and pain. J Endocrinol. 2017;234(1):R23–36. https://doi.org/10.1530/JOE-16-0514.
Aburto JM, Villavicencio F, Basellini U, Kjærgaard S, Vaupel JW. Dynamics of life expectancy and life span equality. Proc Natl Acad Sci USA. 2020;117(10):5250–9. https://doi.org/10.1073/PNAS.1915884117/-/DCSUPPLEMENTAL.
Brownie S. Why are elderly individuals at risk of nutritional deficiency? Int J Nurs Pract. 2006;12(2):110–8. https://doi.org/10.1111/J.1440-172X.2006.00557.X.
Fabian E, Bogner M, Kickinger A, Wagner KH, Elmadfa I. Vitamin status in elderly people in relation to the use of nutritional supplements. J Nutr Heal Aging. 2011;16(3):206–12. https://doi.org/10.1007/S12603-011-0159-5.
Bischoff-Ferrari HA, et al. Fall prevention with supplemental and active forms of vitamin D: a meta-analysis of randomised controlled trials. BMJ. 2009;339(7725):843. https://doi.org/10.1136/BMJ.B3692.
Mosekilde L. Vitamin D and the elderly. Clin Endocrinol. 2005;62(3):265–81. https://doi.org/10.1111/J.1365-2265.2005.02226.X.
Kweder H, Eidi H. Vitamin D deficiency in elderly: risk factors and drugs impact on vitamin D status. Avicenna J Med. 2018;8(4):139. https://doi.org/10.4103/AJM.AJM_20_18.
AlQuaiz AJM, Kazi A, Fouda M, Alyousefi N. Age and gender differences in the prevalence and correlates of vitamin D deficiency. Arch Osteoporos. 2018. https://doi.org/10.1007/S11657-018-0461-5.
Lappe J, et al. Effect of Vitamin D and calcium supplementation on cancer incidence in older women: a randomized clinical trial. JAMA. 2017;317(12):1234–43. https://doi.org/10.1001/JAMA.2017.2115.
Um CY, Prizment A, Hong CP, Lazovich DA, Bostick RM. Associations of calcium, vitamin D, and dairy product intakes with colorectal cancer risk among older women: the Iowa women’s health study. Nutr Cancer. 2018;71(5):739–48. https://doi.org/10.1080/01635581.2018.1539188.
Anghel L, Baroiu L, Beznea A, Topor G, Grigore CA. The Therapeutic Relevance of Vitamin E. REV.CHIM.(Bucharest), vol. 70, no. 10, 2019, Accessed: Dec. 22, 2021. [Online]. Available: http://www.revistadechimie.ro3711.
Yang CS, Luo P, Zeng Z, Wang H, Malafa M, Suh N. Vitamin E and cancer prevention: studies with different forms of tocopherols and tocotrienols. Mol Carcinog. 2020;59(4):365–89. https://doi.org/10.1002/MC.23160.
Torquato P, et al. Vitamin E: metabolism and molecular aspects. Mol Nutr Vitam. 2020. https://doi.org/10.1016/B978-0-12-811907-5.00020-8.
Schubert M, et al. Long-chain metabolites of vitamin E: metabolic activation as a general concept for lipid-soluble vitamins? Antioxidants. 2018;7(1):10. https://doi.org/10.3390/ANTIOX7010010.
Choi Y, et al. Vitamin E (α-tocopherol) consumption influences gut microbiota composition. Int J Food Sci Nutr. 2019;71(2):221–5. https://doi.org/10.1080/09637486.2019.1639637.
Ran L, Liu AB, Lee MJ, Xie P, Lin Y, Yang CS. Effects of antibiotics on degradation and bioavailability of different vitamin E forms in mice. BioFactors. 2019;45(3):450–62. https://doi.org/10.1002/BIOF.1492.
Rickman JC, Bruhn CM, Barrett DM. Nutritional comparison of fresh, frozen, and canned fruits and vegetables II. Vitamin A and carotenoids, vitamin E, minerals and fiber. J Sci Food Agric. 2007;87(7):1185–96. https://doi.org/10.1002/JSFA.2824.
“Vitamin E | The Nutrition Source | Harvard T.H. Chan School of Public Health.” https://www.hsph.harvard.edu/nutritionsource/vitamin-e/ (accessed Dec. 22, 2021).
Van Leer P. Vitamin E in Pregnancy. Am Fam Physician.2017;95(7). Accessed: Jan. 06, 2022. [Online]. Available: www.aafp.org/afpAmericanFamilyPhysician421http://www.aafp.org/afp/mbtn.
Rumbold A, Ota E, Hori H, Miyazaki C, Crowther CA. Vitamin E supplementation in pregnancy. Cochrane Database Syst Rev. 2015. https://doi.org/10.1002/14651858.CD004069.PUB3/MEDIA/CDSR/CD004069/IMAGE_N/NCD004069-CMP-005-06.PNG.
Rumbold A, Middleton P, Pan N, Crowther CA. Vitamin supplementation for preventing miscarriage. Cochrane Database Syst Rev. 2011. https://doi.org/10.1002/14651858.CD004073.PUB3/MEDIA/CDSR/CD004073/REL0003/CD004073/IMAGE_N/NCD004073-CMP-005-18.PNG.
Devereux G, Craig L, Seaton A, Turner S. Maternal vitamin D and E intakes in pregnancy and asthma to age 15 years: a cohort study. Pediatr Pulmonol. 2019;54(1):11–9. https://doi.org/10.1002/PPUL.24184.
S. Kositamongkol, U. Suthutvoravut, N. Chongviriyaphan, B. Feungpean, and P. Nuntnarumit, “Vitamin A and E status in very low birth weight infants,” J. Perinatol. vol. 31, no. 7, pp. 471–476, Jan. 2011, doi: https://doi.org/10.1038/jp.2010.155.
da Silva ALC, et al. Vitamin in Human Milk and its Relation to the nutritional Requirements of the Term Newborn. Rev Paul Pediatr. 2017;35:158–64.
M. Bethesda, “Vitamin E, in Drugs and lactation database (LactMed),” Natl. Libr. Med., 2006.
Strait RT, Camargo CA. Vitamin E and the risk of childhood asthma. Expert Rev Respir Med. 2016;10(8):881–90. https://doi.org/10.1080/17476348.2016.1184090.
Elkamil A, Johansen KK, Aasly J. Ataxia with vitamin E deficiency in Norway. J Mov Disord. 2015;8(1):33. https://doi.org/10.14802/JMD.14030.
Woo Baidal JA, Cheng ER, Rifas-Shiman SL, Oken E, Gillman MW, Taveras EM. Association of vitamin E intake at early childhood with alanine aminotransferase levels at mid-childhood. Hepatology. 2018;67(4):1339–47. https://doi.org/10.1002/HEP.29629.
Alghadir AH, Gabr SA, Iqbal ZA, Al-Eisa E. Association of physical activity, vitamin E levels, and total antioxidant capacity with academic performance and executive functions of adolescents. BMC Pediatr. 2019;19(1):1–8. https://doi.org/10.1186/S12887-019-1528-1/TABLES/4.
Al-Baiaty FDR, Ismail A, Abdul Latiff Z, Muhammad Nawawi KN, Raja Ali RA, Mokhtar NM. Possible hepatoprotective effect of tocotrienol-rich fraction vitamin E in non-alcoholic fatty liver disease in obese children and adolescents. Front Pediatr. 2021. https://doi.org/10.3389/FPED.2021.667247.
Asbaghi O, et al. The effect of vitamin E supplementation on selected inflammatory biomarkers in adults: a systematic review and meta-analysis of randomized clinical trials. Sci Rep. 2020;10(1):1–17. https://doi.org/10.1038/s41598-020-73741-6.
Ashor AW, Siervo M, Lara J, Oggioni C, Afshar S, Mathers JC. Effect of vitamin C and vitamin E supplementation on endothelial function: a systematic review and meta-analysis of randomised controlled trials. Br J Nutr. 2015;113(8):1182–94. https://doi.org/10.1017/S0007114515000227.
Rattanawiwatpong P, Wanitphakdeedecha R, Bumrungpert A, Maiprasert M. Anti-aging and brightening effects of a topical treatment containing vitamin C, vitamin E, and raspberry leaf cell culture extract: a split-face, randomized controlled trial. J Cosmet Dermatol. 2020;19(3):671–6. https://doi.org/10.1111/JOCD.13305.
Cheng P, et al. Vitamin E intake and risk of stroke: a meta-analysis. Br J Nutr. 2018;120(10):1181–8. https://doi.org/10.1017/S0007114518002647.
Zhou P, Shao R, Wang H, Miao J, Wang X. Dietary vitamin A, C, and E intake and subsequent fracture risk at various sites: A meta-analysis of prospective cohort studies. Medicine (Baltimore). 2020;99(35): e20841. https://doi.org/10.1097/MD.0000000000020841.
Meydani SN, et al. Vitamin E supplementation enhances cell-mediated immunity in healthy elderly subjects. Am J Clin Nutr. 1990;52(3):557–63. https://doi.org/10.1093/AJCN/52.3.557.
Meydani SN, et al. Vitamin E supplementation and in vivo immune response in healthy elderly subjects: a randomized controlled trial. JAMA. 1997;277(17):1380–6. https://doi.org/10.1001/JAMA.1997.03540410058031.
Meydani SN, et al. Vitamin E and respiratory tract infections in elderly nursing home residents: a randomized controlled trial. JAMA. 2004;292(7):828–36. https://doi.org/10.1001/JAMA.292.7.828.
Hemilä H. Vitamin E administration may decrease the incidence of pneumonia in elderly males. Clin Interv Aging. 2016;11:1379–85. https://doi.org/10.2147/CIA.S114515.
Livny A, et al. Vitamin E Intake Is Associated with Lower Brain Volume in Haptoglobin 1–1 Elderly with Type 2 Diabetes. J Alzheimers Dis. 2020;74(2):649–58. https://doi.org/10.3233/JAD-191294.
Roop JK. Hypervitaminosis-an emerging pathological condition, no. 8, p. 280, 2018, [Online]. Available: https://d1wqtxts1xzle7.cloudfront.net/64071062/40-with-cover-page-v2.pdf?Expires=1640189464&Signature=eugZ76Po8JY~G6fTjw-o2JXBD8KCucHCMKYiLEUWYLrtpWvwZVjoe3dyTjsx-YpOS0AhGtaBZm-Rr-36Pr~6XRGIkjqTEUbc557m89yG7Yt8Pc-Xf911cqsSb02YniNOInoHh6PmpRgS-mUSy-BH5aUXE.
Vivarelli F, et al. Co-carcinogenic effects of vitamin E in prostate. Sci Rep. 2019. https://doi.org/10.1038/S41598-019-48213-1.
Mladěnka P, et al. Vitamin K – sources, physiological role, kinetics, deficiency, detection, therapeutic use, and toxicity. Nutr Rev. 2021. https://doi.org/10.1093/NUTRIT/NUAB061.
Shearer MJ, Newman P. Recent trends in the metabolism and cell biology of vitamin K with special reference to vitamin K cycling and MK-4 biosynthesis. J Lipid Res. 2014;55(3):345–62. https://doi.org/10.1194/JLR.R045559.
Shearer MJ, Fu X, Booth SL. Vitamin K nutrition, metabolism, and requirements: current concepts and future research. Adv Nutr. 2012;3(2):182–95. https://doi.org/10.3945/AN.111.001800.
Ellis JL, et al. Dietary vitamin K is remodeled by gut microbiota and influences community composition. Gut Microbes. 2021;13(1):1–16. https://doi.org/10.1080/19490976.2021.1887721/SUPPL_FILE/KGMI_A_1887721_SM5604.PDF.
Ozaki D, Kubota R, Maeno T, Abdelhakim M, Hitosugi N. Association between gut microbiota, bone metabolism, and fracture risk in postmenopausal Japanese women. Osteoporos Int. 2021;32(1):145–56. https://doi.org/10.1007/S00198-020-05728-Y/FIGURES/4.
Aydin S. Can vitamin K synthesis altered by dysbiosis of microbiota be blamed in the etiopathogenesis of venous thrombosis? Biosci Microbiota, Food Heal. 2017;36(3):73–4. https://doi.org/10.12938/BMFH.17-007.
Imbrescia K, Moszczynski Z. Vitamin K. Princ Nutr Nutr Fundam Individ Nutr. 2021. https://doi.org/10.1016/B978-0-12-804572-5.00034-3.
Wen L, Chen J, Duan L, Li S. Vitamin K-dependent proteins involved in bone and cardiovascular health (Review). Mol Med Rep. 2018;18(1):3–15. https://doi.org/10.3892/MMR.2018.8940/HTML.
Tsang CK, Kamei Y. Novel effect of vitamin K1 (phylloquinone) and vitamin K2 (menaquinone) on promoting nerve growth factor-mediated neurite outgrowth from PC12D cells. Neurosci Lett. 2002;323(1):9–12. https://doi.org/10.1016/S0304-3940(01)02550-2.
Maldonado M, et al. Intrahepatic Cholestasis of Pregnancy Leading to Severe Vitamin K Deficiency and Coagulopathy. Case Rep Obstet Gynecol. 2017;2017:1–3. https://doi.org/10.1155/2017/5646247.
S. Shahrook, E. Ota, N. Hanada, K. Sawada, and R. Mori, “Vitamin K supplementation during pregnancy for improving outcomes: a systematic review and meta-analysis,” Sci. Reports 2018 81, vol. 8, no. 1, pp. 1–11, Jul. 2018, doi: https://doi.org/10.1038/s41598-018-29616-y.
M. Bethesda, “Vitamin K, in Drugs and lactation database (LactMed),” Natl. Libr. Med., 2006.
Erick M. Breast milk is conditionally perfect. Med Hypotheses. 2018;111:82–9. https://doi.org/10.1016/J.MEHY.2017.12.020.
Araki S, Shirahata A. Vitamin K deficiency bleeding in infancy. Nutrients. 2020;12(3):780. https://doi.org/10.3390/NU12030780.
AL-Zuhairy SH. Late vitamin K deficiency bleeding in infants: five-year prospective study. J Pediatr. 2021;97(5):514–9. https://doi.org/10.1016/J.JPED.2020.09.003.
Gahalaut P, Chauhan S. Vitamin K deficiency bleeding presenting as nodular purpura in infancy: a rare and life-threatening entity. Indian J Dermatol. 2013;58(5):407. https://doi.org/10.4103/0019-5154.117334.
Cottam ST, Connett GJ. Routine use of daily oral vitamin K to treat infants with cystic fibrosis. Paediatr Respir Rev. 2015;16:22–4. https://doi.org/10.1016/J.PRRV.2015.07.012.
Shneider BL, et al. Efficacy of fat-soluble vitamin supplementation in infants with biliary Atresia. Pediatrics. 2012;130(3):e607–14. https://doi.org/10.1542/PEDS.2011-1423.
Tsugawa N, et al. A novel method based on curvature analysis for estimating the dietary vitamin K requirement in adolescents. Clin Nutr. 2012;31(2):255–60. https://doi.org/10.1016/J.CLNU.2011.10.006.
Kalkwarf HJ, Khoury JC, Bean J, Elliot JG. Vitamin K, bone turnover, and bone mass in girls. Am J Clin Nutr. 2004;80(4):1075–80. https://doi.org/10.1093/AJCN/80.4.1075.
Fusaro M, et al. Vitamin K plasma levels determination in human health. Clin Chem Lab Med. 2017;55(6):789–99. https://doi.org/10.1515/CCLM-2016-0783/ASSET/GRAPHIC/J_CCLM-2016-0783_FIG_002.JPG.
Ho HJ, Komai M, Shirakawa H. Beneficial effects of vitamin K status on glycemic regulation and diabetes mellitus: a mini-review. Nutrients. 2020;12(8):2485. https://doi.org/10.3390/NU12082485.
Cao AL, Lai YW, Chen HG, Sheng LT, Pan A. Research progress of relationship between vitamin K and type 2 diabetes. Zhonghua Yu Fang Yi Xue Za Zhi. 2020;54(5):555–62. https://doi.org/10.3760/CMA.J.CN112150-20190520-00407.
Li Y, Peng-Chen J, Duan L, Li S. Effect of vitamin K2 on type 2 diabetes mellitus: a review. Diabetes Res Clin Pract. 2018;136:39–51. https://doi.org/10.1016/J.DIABRES.2017.11.020.
Kiely A, Ferland G, Ouliass B, O’Toole PW, Purtill H, O’Connor EM. Vitamin K status and inflammation are associated with cognition in older Irish adults. Nutr Neurosci. 2018;23(8):591–9. https://doi.org/10.1080/1028415X.2018.1536411.
Haugsgjerd TR, et al. Association of dietary vitamin K and risk of coronary heart disease in middle-age adults: the Hordaland health study cohort. BMJ Open. 2020;10(5): e035953. https://doi.org/10.1136/BMJOPEN-2019-035953.
Dal Canto E, et al. The association of vitamin D and vitamin K status with subclinical measures of cardiovascular health and all-cause mortality in older adults: the hoorn study. J Nutr. 2020;150(12):3171–9. https://doi.org/10.1093/JN/NXAA293.
Bultynck C, et al. Prevalence of vitamin K deficiency in older people with hip fracture. Acta Clin Belg. 2020;75(2):136–40. https://doi.org/10.1080/17843286.2018.1564174.
Fusaro M, et al. Vitamin K and Osteoporosis. Nutrients. 2020;12(12):3625. https://doi.org/10.3390/NU12123625.
Acknowledgements
Not Available
Funding
Open access funding provided by The Science, Technology & Innovation Funding Authority (STDF) in cooperation with The Egyptian Knowledge Bank (EKB). This research has received no external funding.
Author information
Authors and Affiliations
Contributions
RAY and MAF contributed to conception and design of the review. RAY, AD, OE wrote the first draft of the manuscript. RAY, AD, OE, and MAF wrote sections of the manuscript. All authors contributed to manuscript writing, editing and revision and finally approved the submitted version.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This review article does not need any ethical approvals or informed consent.
Consent for publication
This review article does not need any consent for publication.
Competing interests
The authors declare that there were not any commercial or financial relationships that could be construed as a potential conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Youness, R.A., Dawoud, A., ElTahtawy, O. et al. Fat-soluble vitamins: updated review of their role and orchestration in human nutrition throughout life cycle with sex differences. Nutr Metab (Lond) 19, 60 (2022). https://doi.org/10.1186/s12986-022-00696-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12986-022-00696-y