Abstract
Objectives
To assess the ability of procalcitonin (PCT)—a promising marker for coinfections—to predict coinfections in patients with COVID-19.
Methods
In this systematic review and meta-analysis, PubMed, Embase, Web of Science, Cochrane, the China National Knowledge Infrastructure (CNKI), and Wanfang were searched to identify eligible studies (up to August 30, 2021). Articles that reported the predictive value of PCT for coinfections in patients with COVID-19 were included. Individual and pooled sensitivities and specificities were reported, and I2 was used to test heterogeneity. This study was prospectively registered on the International Prospective Register of Systematic Reviews (PROSPERO) database (registration number: CRD42021283344).
Results
Five studies involving a total of 2775 patients reported the predictive value of PCT for coinfections in patients with COVID-19. The sensitivity, specificity, and area under the curve of PCT in predicting coinfections in the pooled studies were 0.60 (95% CI 0.35–0.81, I2 = 88.85), 0.71 (95% CI 0.58–0.81, I2 = 87.82), and 0.72(95% CI 0.68–0.76) respectively.
Conclusions
Although PCT has limited predictive value for coinfections in patients with COVID-19, lower PCT levels seem to indicate a decreased probability of having a coinfection.
Similar content being viewed by others
Introduction
The prevalence of bacterial coinfections in hospitalized patients with coronavirus disease 2019 (COVID-19), a novel human-to-human infectious disease [1], is less than 10% [2,3,4]. The rate of bacterial respiratory infection in critically ill patients with COVID-19 has been estimated to be between 14 and 28% [5,6,7], and the prevalence of coinfections in patients in intensive care units (ICUs) ranges from 14 to 50% [3, 8]. However, another study found that 81.7% of patients who died from COVID-19 had bacterial coinfections [9]. Additionally, Martins-Filho et al. showed that sepsis was associated with a 2.4-fold increased risk of death in these patients [10]. These findings indicate that the overall rate of confirmed coinfections is low, but the mortality rate of coinfections is high.
The vast majority (57–86%) of patients with COVID-19 receive empiric antibiotic therapy [2, 4, 11], which may not be required in most cases. Antimicrobial prescriptions have increased since the pandemic began, posing the threat of increasing antimicrobial resistance worldwide [12]. Therefore, identifying an indicator that can predict COVID-19 coinfections is of important clinical significance.
Serum procalcitonin (PCT) may help identify coinfections in patients with COVID-19 [13], facilitating decisions about antibiotic therapy for lower respiratory tract infections [14,15,16]. However, previous studies demonstrated that in isolated COVID-19 patients, as in other viral infections, PCT levels generally remain normal (≤ 0.5 µg/L); this may be because the virus stimulates macrophages to produce interferon-γ, thereby suppressing TNF-α during the immune response [16]. Other research found that a PCT level of < 0.25 µg/L had a negative predictive value of 81%, and a PCT level of > 1 µg/L had a positive predictive value of 93% for coinfections [8].
To more rigorously assess the predictive value of PCT for coinfections in patients with COVID-19, we performed a systematic review and meta-analysis.
Materials and methods
This meta-analysis was performed following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA statement) guidelines [17] and was prospectively registered on the International Prospective Register of Systematic Reviews (PROSPERO) database (registration number: CRD42021283344).
Search strategy and selection criteria
The PubMed, Embase, Web of Science, Cochrane, China National Knowledge Infrastructure (CNKI), and Wanfang databases (up to August 30, 2021) were searched with the following terms: ((((((((((co-infection) OR (coinfection)) OR (super-infection)) OR (superinfection)) OR (secondary infection)) OR (bacterial infection)) OR (bacterial culture)) OR (other pathogens NOT SARS Cov-2)) OR (other organisms NOT SARS Cov-2)) AND ((procalcitonin) OR (PCT))) AND (((((Coronavirus disease 2019) OR (2019 Novel Coronavirus)) OR (SARS-CoV-2)) OR (2019-nCoV)) OR (COVID-19)).
The full search strategies are shown in Additional file 1. No language restrictions were applied. To identify additional literature, the reference lists of eligible studies and previous evidence summaries were also reviewed by two reviewers (SCW and LNW) independently. Disagreements were resolved by consensus, and in cases of persistent disagreement, the third reviewer (XML) was consulted.
The inclusion criteria of studies were as follows: (1) the predictive value of PCT for coinfections in patients with COVID-19 was evaluated; (2) a 2 × 2 table of results was able to be constructed (i.e., sufficient information was included to calculate the true positive [TP], false positive [FP], false negative [FN], and true negative [TN]). The following study types were excluded: case reports, reviews, editorials, conference abstracts, comments, letters, and animal studies.
Data extraction and quality assessment
Relevant information was extracted from individual studies with a standardized form; specifically, the first author, publication year, number of patients (male/female), mean age, cut-off value, area under the curve (AUC), TP, TN, FP, FN, sensitivity (SEN), and specificity (SPE) were recorded. Data extraction was assessed by two reviewers (SCW and LNW), and disagreements were resolved by consensus. The Quality Assessment of Diagnostic Accuracy Studies 2 (QUADAS-2) criteria was used to evaluate each of the included studies (Additional file 2).
Statistical analysis
StataMP (version 16.0) with the MIDAS module was used to conduct the statistical analyses. The pooled SEN, SPE, likelihood ratio (LR), and diagnostic odds ratio (DOR) with corresponding 95% confidence intervals (CIs) were calculated by a bivariate random effects meta-analysis model [18]. The extent of heterogeneity among the studies was quantified by calculating the I2 statistic, and I2 values above 50% indicate substantial heterogeneity. The overall diagnostic accuracy was assessed by a summary receiver operating characteristic (SROC) curve. A Fagan nomograph was used to explore the relationship between the pretest probability, likelihood ratio, and post-test probability.
Results
Selection and characteristics of studies
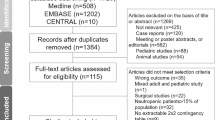
The literature search identified 947 studies, including 151 from PubMed, 284 from Embase, 410 from Web of Science, 6 from Cochrane, 53 from the CNKI, and 43 from the Wanfang database. Figure 1 shows the study selection process. A total of 209 duplicate publications were excluded, and 618 studies were excluded after the title and abstract assessment according to the inclusion and exclusion criteria. The remaining 120 studies were reviewed by reading the full text. Of these, five studies were finally included in the meta-analysis.
The characteristics of the included studies and the predictive value of PCT for coinfections in each study are listed in Table 1. The number of participants ranged from 66 to 2443. Notably, the SEN, SPE, and AUC varied widely among the included studies. All studies were retrospective except for one [19]. All but two studies [19, 20] diagnosed coinfections with positive blood and/or lower respiratory tract cultures. One study did not specify which specimens were cultured and defined colonization as a positive culture without clinical manifestations [19]. The other study included urine cultures in addition to blood and lower respiratory tract specimens [20].
Predictive value of PCT for coinfections
Five studies involving a total of 2775 participants reported the predictive value of PCT for coinfections in patients with COVID-19. The combined SEN and SPE were 0.60 (95% CI 0.35–0.81, I2 = 88.85) and 0.71 (95% CI 0.58–0.81, I2 = 87.82), respectively (Fig. 2). The positive likelihood ratio was 2.1 (95% CI 1.2–3.5), and the negative likelihood ratio was 0.56 (95% CI 0.31–1.04). The DOR was 13 (95% CI 9–18). The SROC curve is shown in Fig. 3; the AUC of PCT for predicting coinfections with COVID-19 was 0.72 (95% CI 0.68–0.76), indicating limited diagnostic value of PCT. The Fagan nomogram (Fig. 4) indicated that if the pretest probability was set to 50%, the post-test probability of PCT for predicting coinfections was 67% when PCT was above the cut-off value. Conversely, when PCT was below the cut-off value, the post-test probability was 36%.
Fagan nomogram of PCT for predicting coinfection in patients with COVID-19. The pre-test probability was set to 50%. The post-test probability of PCT for the detection of coinfection was 67% when the PCT was above the cut-off value. The post-test probability was 36% when the PCT was below the cut-off value
Study quality
The methodological quality of the included studies is summarized in Additional file 2. One study only selected patients admitted to the ICU [21], and another included only critically ill patients with COVID-19 [19]. Therefore, these two studies were considered to have a high risk of patient selection bias.
Discussion
The concentration of procalcitonin (PCT) in the circulation is low (≤ 0.1 µg/L), and an increase in PCT concentration is positively associated with the severity of bacterial infections; notably, PCT is the most sensitive indicator for the early clinical identification of bacterial and viral infections [22]. The presence of PCT had a high negative predictive value (94%) for bacterial coinfections in patients with influenza in ICUs [23]. However, the PCT concentration does not increase (≤ 0 5 µg/L) in most patients with COVID-19, but it increases frequently in severe cases and those that result in death [24]. A previous meta-analysis of four studies showed that elevated PCT was associated with a nearly five-fold increase in the risk of severe COVID-19(OR 4.76, 95% CI 2.74–8.29) [25]. Thus, it is of great significance to validate whether PCT is a reliable predictor of coinfections.
Our meta-analysis included five studies involving a total of 2775 patients, and the results showed that the ability of PCT to predict coinfections in patients with COVID-19 was limited (AUC = 0.72, SEN = 0.60, and SPE = 0.71). The results of three of the included studies suggested that PCT was a useful tool to rule out bacterial coinfections (its negative predictive value was over 93%) when its concentration was < 0.50 μg/L [13, 20, 21]. Notably, another study involving 2443 patients showed that PCT had a high negative predictive value of 95% [20] (Table 1).
This meta-analysis has several limitations. First, all included studies were retrospective except one, so the data were prone to confounding factors. Second, the included studies had a considerable level of heterogeneity. The number of included articles and the total number of patients were limited, so publication bias, subgroup, and sensitivity analyses could not be performed. More high-quality studies may be needed to elucidate the role of PCT in coinfections with COVID-19 and identify optimal cut-offs.
In summary, although PCT has a limited ability to diagnose coinfections in patients with COVID-19, low levels of PCT seem to be a good indicator for excluding coinfections. We remain skeptical about the ability of PCT to help clinicians detect coinfections early; more research is needed to validate the usefulness of PCT so that clinicians can initiate effective management quickly and reduce the overall mortality of COVID-19. Further research is needed to develop accurate predictive models and diagnostics for coinfections in patients with COVID-19.
Availability of data and materials
The raw data of this study are available from the corresponding author upon reasonable request.
Abbreviations
- PCT:
-
Procalcitonin
- COVID-19:
-
Coronavirus disease 2019
- CNKI:
-
China National Knowledge Infrastructure
- QUADAS-2:
-
Quality Assessment of Diagnostic Accuracy Studies-2
- SEN:
-
Sensitivity
- SPE:
-
Specificity
- AUC:
-
Area under the curve
- LRs:
-
Likelihood ratios
- DOR:
-
Diagnostic odds ratio
- SROC:
-
Summary receiver operating characteristic
References
Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: s the Chinese Center for Disease Control and Prevention. JAMA. 2020;323(13):1239–42.
Rawson TM, Moore L, Zhu N, Ranganathan N, Skolimowska K, Gilchrist M, et al. Bacterial and fungal coinfection in individuals with coronavirus: a rapid review to support COVID-19 antimicrobial prescribing. Clin Infect Dis. 2020;71(9):2459–68.
Lansbury L, Lim B, Baskaran V, Lim WS. Co-infections in people with COVID-19: a systematic review and meta-analysis. J Infect. 2020;81(2):266–75.
Vaughn VM, Gandhi TN, Petty LA, Patel PK, Prescott HC, Malani AN, et al. Empiric antibacterial therapy and community-onset bacterial coinfection in patients hospitalized with coronavirus disease 2019 (COVID-19): a multi-hospital cohort study. Clin Infect Dis. 2021;72(10):e533–41.
Langford BJ, So M, Raybardhan S, Leung V, Westwood D, MacFadden DR, et al. Bacterial co-infection and secondary infection in patients with COVID-19: a living rapid review and meta-analysis. Clin Microbiol Infect. 2020;26(12):1622–9.
Bassetti M, Kollef MH, Timsit JF. Bacterial and fungal superinfections in critically ill patients with COVID-19. Intensive Care Med. 2020;46(11):2071–4.
Contou D, Claudinon A, Pajot O, Micaelo M, Longuet FP, Dubert M, et al. Bacterial and viral co-infections in patients with severe SARS-CoV-2 pneumonia admitted to a French ICU. Ann Intensive Care. 2020;10(1):119.
van Berkel M, Kox M, Frenzel T, Pickkers P, Schouten J. Biomarkers for antimicrobial stewardship: a reappraisal in COVID-19 times? Crit Care. 2020;24(1):600.
Wang L, He W, Yu X, Hu D, Bao M, Liu H, et al. Coronavirus disease 2019 in elderly patients: characteristics and prognostic factors based on 4-week follow-up. J Infect. 2020;80(6):639–45.
Martins-Filho PR, Tavares C, Santos VS. Factors associated with mortality in patients with COVID-19. A quantitative evidence synthesis of clinical and laboratory data. Eur J Intern Med. 2020;76:97–9.
Rothe K, Feihl S, Schneider J, Wallnofer F, Wurst M, Lukas M, et al. Rates of bacterial co-infections and antimicrobial use in COVID-19 patients: a retrospective cohort study in light of antibiotic stewardship. Eur J Clin Microbiol Infect Dis. 2021;40(4):859–69.
Hsu J. How covid-19 is accelerating the threat of antimicrobial resistance. BMJ. 2020;369: m1983.
Pink I, Raupach D, Fuge J, Vonberg RP, Hoeper MM, Welte T, et al. C-reactive protein and procalcitonin for antimicrobial stewardship in COVID-19. Infection. 2021;49(5):935–43.
Schuetz P, Wirz Y, Sager R, Christ-Crain M, Stolz D, Tamm M, et al. Procalcitonin to initiate or discontinue antibiotics in acute respiratory tract infections. Cochrane Database Syst Rev. 2017;10:D7498.
Briel M, Schuetz P, Mueller B, Young J, Schild U, Nusbaumer C, et al. Procalcitonin-guided antibiotic use vs a standard approach for acute respiratory tract infections in primary care. Arch Intern Med. 2008;168(18):2000–7, 2007–8.
Burkhardt O, Ewig S, Haagen U, Giersdorf S, Hartmann O, Wegscheider K, et al. Procalcitonin guidance and reduction of antibiotic use in acute respiratory tract infection. Eur Respir J. 2010;36(3):601–7.
Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg. 2010;8(5):336–41.
Burke DL, Bujkiewicz S, Riley RD. Bayesian bivariate meta-analysis of correlated effects: impact of the prior distributions on the between-study correlation, borrowing of strength, and joint inferences. Stat Methods Med Res. 2018;27(2):428–50.
Kooistra EJ, van Berkel M, van Kempen NF, van Latum C, Bruse N, Frenzel T, et al. Dexamethasone and tocilizumab treatment considerably reduces the value of C-reactive protein and procalcitonin to detect secondary bacterial infections in COVID-19 patients. Crit Care. 2021;25(1):281.
May M, Chang M, Dietz D, Shoucri S, Laracy J, Sobieszczyk ME, et al. Limited utility of procalcitonin in identifying community-associated bacterial infections in patients presenting with coronavirus disease 2019. Antimicrob Agents Chemother. 2021;65(4).
Vanhomwegen C, Veliziotis I, Malinverni S, Konopnicki D, Dechamps P, Claus M, et al. Procalcitonin accurately predicts mortality but not bacterial infection in COVID-19 patients admitted to intensive care unit. Ir J Med Sci. 2021;190(4):1649–52.
Governance CB. PCT non-executives to hold clusters “to account.” Health Serv J. 2011;121(6243):4–5.
Rodriguez AH, Aviles-Jurado FX, Diaz E, Schuetz P, Trefler SI, Sole-Violan J, et al. Procalcitonin (PCT) levels for ruling-out bacterial coinfection in ICU patients with influenza: a CHAID decision-tree analysis. J Infect. 2016;72(2):143–51.
Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395(10223):507–13.
Lippi G, Plebani M. Procalcitonin in patients with severe coronavirus disease 2019 (COVID-19): a meta-analysis. Clin Chim Acta. 2020;505:190–1.
Funding
This work was supported by the National Key R&D Program of China (2020YFC2005401), a Xicheng financial, scientific, and technological project (XCSTS-SD2021-02), and a Project funded by the Baidu Fund of Peking University (2020BD045). The sponsor of the study had no role in the study design, data collection, data analysis, data interpretation, or writing of the report. The corresponding author had full access to all the data in the study and final responsibility for the decision to submit for publication. All authors read and approved the final manuscript.
Author information
Authors and Affiliations
Contributions
XL conceived, designed, and supervised the study. SW and LW acquired the data. SW analyzed and interpreted the data. SW wrote the draft, and LL revised it. All authors have read and approved the final version of the manuscript. The corresponding author attests that all listed authors meet the authorship criteria and that no others authors meeting the criteria have been omitted.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Informed consent
Not applicable.
Consent for publication
Not applicable.
Competing interests
All authors declare that they have no Competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1
. Search strategy and results.
Additional file 2
. Summary of the methodological quality of the studies according to the Quality Assessment of Diagnostic Accuracy Studies 2criteria.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Wei, S., Wang, L., Lin, L. et al. Predictive values of procalcitonin for coinfections in patients with COVID-19: a systematic review and meta-analysis. Virol J 20, 92 (2023). https://doi.org/10.1186/s12985-023-02042-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12985-023-02042-x