Abstract
Background
Knee osteoarthritis (KOA) is an irreversible degenerative disease that characterized by pain and abnormal gait. Radiography is typically used to detect KOA but has limitations. This study aimed to identify changes in plantar pressure that are associated with radiological knee osteoarthritis (ROA) and to validate them using machine learning algorithms.
Methods
This study included 92 participants with variable degrees of KOA. A modified Kellgren–Lawrence scale was used to classify participants into non-ROA and ROA groups. The total feature set included 210 dynamic plantar pressure features captured by a wearable in-shoe system as well as age, gender, height, weight, and body mass index. Filter and wrapper methods identified the optimal features, which were used to train five types of machine learning classification models for further validation: k-nearest neighbors (KNN), support vector machine (SVM), random forest (RF), AdaBoost, and eXtreme gradient boosting (XGBoost).
Results
Age, the standard deviation (SD) of the peak plantar pressure under the left lateral heel (f_L8PPP_std), the SD of the right second peak pressure (f_Rpeak2_std), and the SD of the variation in the anteroposterior displacement of center of pressure (COP) in the right foot (f_RYcopstd_std) were most associated with ROA. The RF model with an accuracy of 82.61% and F1 score of 0.8000 had the best generalization ability.
Conclusion
Changes in dynamic plantar pressure are promising mechanical biomarkers that distinguish between non-ROA and ROA. Combining a wearable in-shoe system with machine learning enables dynamic monitoring of KOA, which could help guide treatment plans.
Similar content being viewed by others
Background
Osteoarthritis (OA) is a chronic, irreversible disease characterized by degeneration of the hyaline articular cartilage, subchondral bone, ligaments, capsule, synovium, and periarticular muscles [1, 2]. Over 300 million people worldwide suffer from OA [3], and knee osteoarthritis (KOA) accounts for approximately 85% of the burden [4]. However, most cases of OA are not appropriately managed [1]. KOA can result in substantial economic losses [5]. In addition, individuals with KOA may be debilitated by pain, stiffness, decreased range of motion, and gait dysfunction [6, 7]. As an age-related disease, KOA is a leading cause of pain and disability among the elderly [6]. Dynamic function tests such as the 40-m (4 × 10 m) fast-paced walking test and timed up and go test are recommended by the Osteoarthritis Research Society International [8]. The incidence of KOA cases is on the rise due to the global population aging and the increasing prevalence of obesity [6], thereby exacerbating the socioeconomic burden associated with this disease. Thus, examinations in different dimensions are essential for effective treatment of KOA.
Imaging examinations like radiography can be used to diagnose OA, grade OA severity, assess OA progression, and monitor treatment responses [9]. Radiography is the first choice in the clinical setting [10]. Radiological OA (ROA) is defined as a case whose Kellgren–Lawrence (K–L) grade is ≥ 2 and indicates that there are definite changes in joint structure. Although the semi-quantitative K–L grading system is widely used in clinical settings [11], it only reflects the static joint structure and requires large equipment and specialized professionals. Exploring additional dynamic features related to radiodiagnosis, such as plantar pressure during walking can enhance assessment tools and offer a new perspective for treatment management.
Gait function, an important indicator of rehabilitation, declines with the progression of KOA. Compared with the Western Ontario and McMaster University Osteoarthritis Index (WOMAC) and the Knee Injury and Osteoarthritis Outcome Score, quantified gait parameters are more objective for functional assessment of KOA patients [12]. Normal individuals and KOA patients can be distinguished by assessing gait parameters such as center of pressure (COP) [13,14,15], regional pressures [13, 16], contact area [16], and peak pressure [15, 16]. Plantar pressure can be measured using a force platform or an in-shoe system (e.g. pedar-X system). Force platforms are typically limited to controlled settings like hospitals and laboratories, whereas in-shoe systems, which comprise pressure sensors and Bluetooth transmission devices, provide a clear advantage in terms of flexibility, efficiency, and portability [17, 18]. Moreover, optimal shoes for patients with KOA remain unknown [19,20,21]. Changes in plantar pressure for patients with KOA are one of the important factors to consider when designing modified footwear. Thus, how dynamic plantar pressure changes in patients with KOA should be further investigated, which may provide guidance for the optimal modified footwear.
Machine learning uses algorithms that learn from data and make decisions with minimal human intervention [22]. Implementing machine learning in wearable devices will allow long-term and dynamic monitoring, which has already been used to detect plantar fasciitis [23], assess fall risk [24, 25] and stroke rehabilitation [26], and monitor freezing of gait in patients with Parkinson’s disease [27]. Although Wang et al. [28] used wearable insoles and machine learning to detect KOA, the progression of KOA could not be characterized in the study population, which included patients scheduled for surgery due to ineffectively conservative treatment as well as healthy subjects without symptoms of KOA. Other studies developed machine learning models to classify patients based on K-L grades [29] and WOMAC scores [30] using other gait parameters (e.g. spatial–temporal parameters) captured by force plates and three-dimensional optical motion capture systems. However, wearable devices and machine learning are seldom used to classify the severity of KOA based on plantar pressure distributions.
This study aimed to identify changes in dynamic plantar pressure associated with non-ROA and ROA using wearable devices and machine learning models. We hypothesized that dynamic plantar pressure measurements would significantly change following structural alterations of knee (i.e. ROA). This study offers insights into the dynamic monitoring of KOA and also guides the rational design of modified footwear to improve treatment outcomes for patients with KOA.
Methods
Participants
All participants were enrolled between January 2022 and February 2023 from the Pearl River Osteoarthritis Cohort (PROC) study at the Zhujiang Hospital of Southern Medical University, Guangzhou. This study was approved by an Institutional Review Board (IRB No. 2019-KY-016-02), and informed consent was obtained from all participants. The PROC includes people aged 45–79 years old from OA outpatient clinics and the communities nearby, who have never had knee surgery but reported having experienced knee pain most of the time in the past month. Exclusion criteria in this study were as follows: (1) with a history of spine surgery and severe spine disease (e.g. radicular pain to the lower extremity); (2) hip, ankle, or foot arthritis; (3) foot deformity (foot varus/valgus, flatfoot, etc.); (4) inability to walk at least 100 m without assistance; (5) acute knee injury in the past year. The calculated methods of the total sample size were as follows: (1) the sample size of the training set should be at least ten times of the included features; (2) the sample size ratio of training set to testing set was 3:1.
Data collection
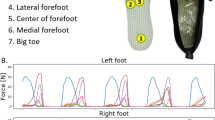
A wireless footwear system (Fig. 1) with a sampling frequency of 20 Hz was provided by the South China University of Technology and used to acquire plantar pressure signals. An insole with a pressure sensor array and data acquisition unit was embedded in the footwear. Sensors were distributed across eight regions: the great toe (sensor 1), the first metatarsal head (sensor 2), the second and third metatarsal head (sensor 3), the fourth and fifth metatarsal head (sensor 4), the medial midfoot (sensor 5), the lateral midfoot (sensor 6), the medial heel (sensor 7), and the lateral heel (sensor 8). The sensor positions mentioned above were determined based on previous research [15]. The stability and effectiveness of the footwear system have been validated by previous studies [24, 31, 32]. The participants were asked to wear socks and appropriate shoes. To reduce deviations from their natural gait, participants walked freely for three minutes before the measurements began. In the formal walking stage, the participants were asked to walk 60 m (three times back and forth on a 20-m straight level walkway). Real-time data were transmitted wirelessly via Bluetooth and displayed on a smartphone.
Bilateral anteroposterior radiographs were acquired while the participants were weight-bearing in a double-leg stance (DLS) at a knee flexion angle of 20°–30°. ROA was diagnosed by an experienced radiologist according to the modified K–L (mK–L) grading system [33, 34]. ROA was defined as mK–L grade ≥ 2; all other cases were defined as non-radiological knee OA (non-ROA). Additional file 1: Table S1 describes the mK–L grading system. Radiographs of 20 randomly selected cases were assessed by another experienced radiologist; the intra-observer (κ = 0.814) and inter-observer (κ = 0.827) reliabilities were good.
Data preprocessing
Abnormal and unstable data were discarded according to the midgait method [35] and the bimodal characteristics of plantar pressure. Sixty valid gait cycles were obtained from each participant after segmentation and splicing.
Feature extraction
The extracted multidimensional features of dynamic plantar pressure were as follows: the peak plantar pressure (PPP), the pressure gradient (PG), time-domain features, impulse, the medial–lateral (M/L) plantar pressure ratio, the COP, the symmetry index, and the mean and standard deviation (SD) of the above parameters in 60 valid gait cycles. Methods used to calculate dynamic plantar pressure are described in Additional file 1: Method S1. The total plantar pressure feature set included 210 features (Additional file 1: Table S2). Physiological features related to KOA: age, body mass index (BMI), gender, height, and weight were also included in the feature selection.
Feature selection
Selecting effective feature subsets from the total feature set can reduce overfitting and increase generalizability of the model. The Shapiro–Wilk test was used to assess the normality of the data. The Mann–Whitney U test and independent t-test were used to classify features that did not significantly differ between groups. Statistical significance was defined as a p-value < 0.05. A wrapper method was used to further optimize the selection of features among different groups.
Machine learning model training and evaluation
The optimal features were used to train five types of machine learning algorithms including k-nearest neighbors (KNN), support vector machine (SVM), random forest (RF), AdaBoost, and eXtreme Gradient Boosting (XGBoost). Ten-fold cross-validation was implemented to train and evaluate the models, whose performance was measured based on accuracy and F1 scores obtained from the confusion matrix. Figure 2 outlines the methodology used to build the model. This study used Python 3.10.8 for model training and testing. The Optuna framework was used for hyperparameter tuning, which is an automated hyperparameter tuning software framework specifically designed for machine learning algorithms using Python programming.
Results
Participant characteristics
A total of 92 participants were recruited, of whom 43 were classified as ROA and 49 as non-ROA. Their demographic characteristics are shown in Table 1. The ROA group was older (p = 0.018) and had a larger BMI (p < 0.001) on average.
Sample set division
Four features were input to model building. Thus, at least 54 participants were needed (< 92 recruited in our study). Participants were randomly divided into the training set (75%) and testing set (25%), which included 69 participants (37 non-ROA and 32 ROA) and 23 participants (12 non-ROA and 11 ROA), respectively.
Optimal features
As shown in Table 2 and Fig. 3, 18 features (2 physiological features and 16 dynamic plantar pressure features) significantly differed between groups. These plantar pressure features included the PPP, the MaxPG, the MinPG, COP displacement, SI, the second peak pressure, and the unloading rate.
The accuracy of model was highest (Additional file 1: Fig. S1) when it considered the following four features: age, the SD of PPP in the left lateral heel (f_L8PPP_std), the SD of the right second peak pressure (f_Rpeak2_std), and the SD of variation in the anteroposterior displacement of the COP in the right foot (f_RYcopstd_std).
Performance comparisons across models
Figure 4 shows the accuracy and F1 score of each model in the training set. The accuracy and F1 score were higher than 77% and 0.7000, respectively, for the RF, AdaBoost, and XGBoost models. The testing set was applied to each model; the confusion matrix is shown in Fig. 5. The model with the best generalization ability, RF, had an accuracy of 82.61% and F1 score of 0.8000 (Fig. 6).
Discussion
This study aimed to identify changes in dynamic plantar pressure associated with non-ROA and ROA, which was monitored dynamically using an intelligent footwear system. Machine learning models were developed to distinguish between ROA and non-ROA based on key features and showed good diagnostic performance.
Several changes in plantar pressure parameters were detected in those with ROA. As shown in Fig. 3 and Table 2, differences in regional plantar pressure features were primarily found on the hallux and heel, corresponding to sensor numbers 1 and 7–8, respectively. The absolute values of these features (f_L1PPP, f_L1MAXPG, f_R1MAXPG, f_R1MAXPG_std, f_L1MINPG, f_L1MINPG_std, f_L7MINPG, f_L8PPP_std, f_L8MINPG, f_L8MINPG_std) were lower in patients with ROA than in those without ROA. This finding agrees with Sito et al. [13], who reported that people with KOA had significantly lower plantar pressures on the hallux and heel as a percentage of body weight.
Four features (age, f_L8PPP_std, f_Rpeak2_std, f_RYcopstd_std) mostly associated with ROA were included in the classification models. The optimal plantar pressure features (f_L8PPP_std, f_Rpeak2_std, f_RYcopstd_std) are correlated with the standard deviation, indicating that decreased gait stability is a prominent feature of ROA. As a commonly used variable to express foot load, the PPP represents the maximum load on the foot region [36]. The PPP can be used to determine foot regions of high pressure and provides reference for the formulation of orthopedic shoes [37]. Foot orthotics are a potential simple treatment method for KOA by reducing the knee adduction moment (KAM), a mechanical biomarker of KOA progression [16]. The knee joint of individuals with ROA exhibits distinct structural changes which involve varying degrees of damage to the articular cartilage, surrounding ligaments, bursae, tendons, and muscles. Compensation of the aforementioned changes in the knee joint may occur through ankle–foot complex during walking since the lower limb functions as a kinetic chain. The f_RYcopstd_std indicates the amount of COP variation in the A/P position [38]. ROA was a key factor for unstable postural control [39]. Increased COP variability is an important predictive indicators for falls in older adults [40]. Previous study had reported that the A/P variation of COP was greater in patients with moderate KOA than that in healthy individuals [41]. An important reason of the increased A/P variation of COP in ROA group may due to the impaired knee proprioception [41]. Impaired knee proprioception will affect the motion and position sense of the lower limbs during walking, consequently reducing the balance control ability and gait stability [42]. In addition, quadriceps muscle strength shows a negative correlation with the K–L grade [43], which will in turn impact gait patterns [44]. Aging accelerating the progression of KOA due to biological alterations of knee and the cumulative effects of other risk factors is a consensus view. However, the ROA group was older than non-ROA group in this study. Therefore, findings of this study should be generalized cautiously.
Combining wearable in-shoe plantar pressure measurement devices with machine learning enables continuous and dynamic monitoring of KOA. In this way, dynamic plantar pressure can be more easily measured without being limited to test environmental conditions. Dynamic plantar pressure combined with radiography can be used to determine the KOA severity and therefore guide treatment options.
This study has several limitations that should be addressed. First, our methodology should be externally validated in a larger population to avoid potential overfitting. Moreover, the optimal plantar pressure features may be different in individuals with different affected side, but this study did not conduct a subgroup analysis on the participants based on their affected sides. Lastly, two classification grades (ROA and non-ROA) but not four-level classification (K–L grade = 1–4) were used to reflect the severity of KOA due to insufficient sample sizes.
Conclusions
In summary, this study demonstrates that changes in dynamic plantar pressure can serve as effective mechanical biomarkers that distinguish between non-ROA and ROA employing machine learning in conjunction with an intelligent in-shoe system. Subsequent research endeavors should contemplate broader population cohorts, more classification levels, and encompass diverse functional activities to further explore the clinical potential of plantar pressure as a way to monitor the progression of KOA.
Availability of data and materials
On reasonable request, the datasets are available from the corresponding author.
Abbreviations
- BMI:
-
Body mass index
- COP:
-
Center of pressure
- DLS:
-
Double-leg stance
- KAM:
-
Knee adduction moment
- KNN:
-
K-nearest neighbors
- PG:
-
Pressure gradient
- PPP:
-
Peak plantar pressure
- PROC:
-
Pearl River Osteoarthritis Cohort
- RF:
-
Random Forest
- SD:
-
Standard deviation
- SVM:
-
Support vector machine
- SI:
-
The symmetry index
- WOMAC:
-
The Western Ontario and McMaster Universities Osteoarthritis Index
References
Hunter DJ, Bierma-Zeinstra S. Osteoarthritis. Lancet. 2019;393(10182):1745–59.
van Hoolwerff M, Rodríguez Ruiz A, Bouma M, Suchiman HED, Koning RI, Jost CR, et al. High-impact FN1 mutation decreases chondrogenic potential and affects cartilage deposition via decreased binding to collagen type II. Sci Adv. 2021;7(45):eabg8583.
Disease GBD, Injury I, Prevalence C. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392(10159):1789–858.
Disease GBD, Injury I, Prevalence C. Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388(10053):1545–602.
Al-Saleh JA, Albelooshi AA, Salti AA, Farghaly M, Ghorab AM, Linga S, et al. Burden, treatment patterns and unmet needs of osteoarthritis in Dubai: a retrospective analysis of the dubai real-world claims database. Rheumatol Ther. 2022;9(1):151–74.
Cross M, Smith E, Hoy D, Nolte S, Ackerman I, Fransen M, et al. The global burden of hip and knee osteoarthritis: estimates from the global burden of disease 2010 study. Ann Rheum Dis. 2014;73(7):1323–30.
Kaufman KR, Hughes C, Morrey BF, Morrey M, An KN. Gait characteristics of patients with knee osteoarthritis. J Biomech. 2001;34(7):907–15.
Terwee CB, Mokkink LB, Steultjens MP, Dekker J. Performance-based methods for measuring the physical function of patients with osteoarthritis of the hip or knee: a systematic review of measurement properties. Rheumatology (Oxford). 2006;45(7):890–902.
Oei EHG, Hirvasniemi J, van Zadelhoff TA, van der Heijden RA. Osteoarthritis year in review 2021: imaging. Osteoarthr Cartil. 2022;30(2):226–36.
Hafezi-Nejad N, Demehri S, Guermazi A, Carrino JA. Osteoarthritis year in review 2017: updates on imaging advancements. Osteoarthr Cartil. 2018;26(3):341–9.
Olsson S, Akbarian E, Lind A, Razavian AS, Gordon M. Automating classification of osteoarthritis according to Kellgren-Lawrence in the knee using deep learning in an unfiltered adult population. BMC Musculoskelet Disord. 2021;22(1):844.
Kour N, Gupta S, Arora S. A survey of knee osteoarthritis assessment based on gait. Arch Comput Methods Eng. 2020;28(2):345–85.
Saito I, Okada K, Nishi T, Wakasa M, Saito A, Sugawara K, et al. Foot pressure pattern and its correlation with knee range of motion limitations for individuals with medial knee osteoarthritis. Arch Phys Med Rehabil. 2013;94(12):2502–8.
Sabashi K, Ishida T, Matsumoto H, Mikami K, Chiba T, Yamanaka M, et al. Dynamic postural control correlates with activities of daily living and quality of life in patients with knee osteoarthritis. BMC Musculoskelet Disord. 2021;22(1):287.
Munoz-Organero M, Littlewood C, Parker J, Powell L, Grindell C, Mawson S. Identification of walking strategies of people with osteoarthritis of the knee using insole pressure sensors. IEEE Sens J. 2017;17(12):3909–20.
Zhang Z, Wang L, Hu K, Liu Y. Characteristics of plantar loads during walking in patients with knee osteoarthritis. Med Sci Monit. 2017;23:5714–9.
Racic V, Pavic A, Brownjohn JMW. Modern facilities for experimental measurement of dynamic loads induced by humans: a literature review. Shock Vib. 2013;20(1):53–67.
Dyer PS, Bamberg SJM. Instrumented insole vs. force plate: a comparison of center of plantar pressure. In: Annual international conference of the IEEE engineering in medicine and biology society IEEE engineering in medicine and biology society annual international conference. 2011;2011:6805–9.
Kolasinski SL, Neogi T, Hochberg MC, Oatis C, Guyatt G, Block J, et al. 2019 American College of Rheumatology/Arthritis foundation guideline for the management of osteoarthritis of the hand, hip, and knee. Arthr Rheumatol. 2020;72(2):220–33.
Haim A, Wolf A, Rubin G, Genis Y, Khoury M, Rozen N. Effect of center of pressure modulation on knee adduction moment in medial compartment knee osteoarthritis. J Orthopaedic Res. 2011;29(11):1668–74.
Duivenvoorden T, Brouwer RW, van Raaij TM, Verhagen AP, Verhaar JA, Bierma-Zeinstra SM. Braces and orthoses for treating osteoarthritis of the knee. Cochrane Database Syst Rev. 2015;2015(3):CD004020.
Giambagli L, Buffoni L, Carletti T, Nocentini W, Fanelli D. Machine learning in spectral domain. Nat Commun. 2021;12(1):1330.
Merry KJ, Macdonald E, MacPherson M, Aziz O, Park E, Ryan M, et al. Classifying sitting, standing, and walking using plantar force data. Med Biol Eng Comput. 2021;59(1):257–70.
Song Z, Ou J, Shu L, Hu G, Wu S, Xu X, et al. Fall risk assessment for the elderly based on weak foot features of wearable plantar pressure. IEEE Trans Neural Syst Rehabil Eng. 2022;30:1060–70.
Antwi-Afari MF, Li H, Seo J, Wong AYL. Automated detection and classification of construction workers’ loss of balance events using wearable insole pressure sensors. Autom Constr. 2018;96:189–99.
Chen X, Hu D, Zhang R, Pan Z, Chen Y, Xie L, et al. Interpretable evaluation for the Brunnstrom recovery stage of the lower limb based on wearable sensors. Front Neuroinform. 2022;16:1006494.
Pardoel S, Nantel J, Kofman J, Lemaire ED. Prediction of freezing of gait in parkinson’s disease using unilateral and bilateral plantar-pressure data. Front Neurol. 2022;13: 831063.
Wang A, Li D, Fan N, Yuan S, Wu Q, Fu Z, et al. Piezoresistive-based gait monitoring technique for the recognition of knee osteoarthritis patients. IEEE Access. 2022;10:123874–84.
Kwon SB, Ro DH, Song MK, Han HS, Lee MC, Kim HC. Identifying key gait features associated with the radiological grade of knee osteoarthritis. Osteoarthr Cartil. 2019;27(12):1755–60.
Kwon SB, Ku Y, Han HS, Lee MC, Kim HC, Ro DH. A machine learning-based diagnostic model associated with knee osteoarthritis severity. Sci Rep. 2020;10(1):15743.
Wang D, Ouyang J, Zhou P, Yan J, Shu L, Xu X. A Novel low-cost wireless footwear system for monitoring diabetic foot patients. IEEE Trans Biomed Circuits Syst. 2021;15(1):43–54.
Yan Y, Ou J, Shi H, Sun C, Shen L, Song Z, et al. Plantar pressure and falling risk in older individuals: a cross-sectional study. J Foot Ankle Res. 2023;16(1):14.
Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957;16(4):494–502.
Felson DT, Niu J, Guermazi A, Sack B, Aliabadi P. Defining radiographic incidence and progression of knee osteoarthritis: suggested modifications of the Kellgren and Lawrence scale. Ann Rheum Dis. 2011;70(11):1884–6. https://doi.org/10.1136/ard.2011.155119.
Schuh R, Gruber F, Wanivenhaus A, Hartig N, Windhager R, Trnka HJ. Flexor digitorum longus transfer and medial displacement calcaneal osteotomy for the treatment of stage II posterior tibial tendon dysfunction: kinematic and functional results of fifty one feet. Int Orthop. 2013;37(9):1815–20.
Orlin MN, McPoil TG. Plantar pressure assessment. Phys Ther. 2000;80(4):399–409.
Yu X, Yu GR, Chen YX, Liu XC. The characteristics and clinical significance of plantar pressure distribution in patients with diabetic toe deformity: a dynamic plantar pressure analysis. J Int Med Res. 2011;39(6):2352–9.
Haddad JM, Rietdyk S, Ryu JH, Seaman JM, Silver TA, Kalish JA, et al. Postural asymmetries in response to holding evenly and unevenly distributed loads during self-selected stance. J Mot Behav. 2011;43(4):345–55.
Masui T, Hasegawa Y, Yamaguchi J, Kanoh T, Ishiguro N, Suzuki S. Increasing postural sway in rural-community-dwelling elderly persons with knee osteoarthritis. J Orthopaedic Sci. 2006;11(4):353–8.
Lindsay R, Spittle S, Spittle M. Considering the need for movement variability in motor imagery training: implications for sport and rehabilitation. Front Psychol. 2023;14:1178632.
Hosseini I, Najafi Ashtiani MN, Bahrpeyma F. Correlation between the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) scores and the stability metrics in patients with knee osteoarthritis. Int J MusculoskelPain Prev. 2022;7(3):741–9.
Raizah A, Reddy RS, Alshahrani MS, Tedla JS, Dixit S, Gular K, et al. Investigating knee joint proprioception and its impact on limits of stability using dynamic posturography in individuals with bilateral knee osteoarthritis-a cross-sectional study of comparisons and correlations. J Clin Med. 2023;12(8):2764.
Chin C, Sayre EC, Guermazi A, Nicolaou S, Esdaile JM, Kopec J, et al. Quadriceps weakness and risk of knee cartilage loss seen on magnetic resonance imaging in a population-based cohort with knee pain. J Rheumatol. 2019;46(2):198–203.
Spinoso DH, Bellei NC, Marques NR, Navega MT. Quadriceps muscle weakness influences the gait pattern in women with knee osteoarthritis. Adv Rheumatol. 2018;58(1):26.
Acknowledgements
We express our sincere gratitude to all individuals who participated in the Pearl River Osteoarthritis Cohort (PROC) study.
Funding
This research was funded by the by the National Natural Science Foundation of China (Grant Nos.82002380, 82072528), Natural Science Foundation of Guangdong Province (2022A1515012460), Development Center for Medical Science & Technology National Health Commission of China (DCMST-NHC-2019-AHT-01), and Guangdong Medical University-Southern Medical University twinning research team project (No.4SG23033G).
Author information
Authors and Affiliations
Contributions
GH, QZ, SL and GL conceived and designed the study. Data collection was performed by GL, SL and ZZ. GL, SL, GH and QZ drafted and revised the manuscript. JX and LS provided the wearable in-shoe system and analyzed the data. ZZ, JZ, CY and LH produced figures and tables. The final manuscript was approved by all authors.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The Institutional Review Board of Zhujiang Hospital of Southern Medical University, Guangzhou, approved the study (IRB No. 2019-KY-016-02). Participants provided written and informed consent.
Consent for publication
Not applicable.
Competing interests
There are no competing interests between the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Method S1.
Methods to calculate dynamic plantar pressure. Table S1. Description of modified Kellgren–Lawrence grade. Table S2. 210 dynamic plantar pressure features. Fig. S1. Optimal features selection
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Li, G., Li, S., Xie, J. et al. Identifying changes in dynamic plantar pressure associated with radiological knee osteoarthritis based on machine learning and wearable devices. J NeuroEngineering Rehabil 21, 45 (2024). https://doi.org/10.1186/s12984-024-01337-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12984-024-01337-6