Abstract
Background
Assessment of bimanual movements, which are frequently impaired in children with cerebral palsy, is highly challenging in clinical practice. Instrumented measures have been developed to evaluate and help to understand impaired upper limb movement during bimanual tasks in these children. The aim of this review was to report instrumented measurement tools (3D motion analysis, sensors, etc.) used for bimanual task movement analysis, and the metrological properties of the measures in children with cerebral palsy.
Methods
A systematic review was conducted (Prospero CRD42022308517). PubMed, Web of Science, Cochrane and Scopus databases were searched with relevant keywords and inclusion/exclusion criteria. Article quality and biomechanical methods were evaluated with a customized scale and metrological properties with the COSMIN checklist.
Results
In total, 452 children, mostly with unilateral cerebral palsy, mean age 10.9 (SD 3.2) years, underwent quantitative bimanual assessments in the 31 included studies (mean quality score 22/32 points [SD 4.7]). The tools used were 3D motion analysis (n = 26), accelerometers (n = 2), and other instruments (cube, digitizer, etc.) (n = 3). Children performed 1–5 bimanual tasks in laboratory settings, mostly activities of daily living or game scenarios. Analyses focused mostly on spatiotemporal variables, 6 of which were specifically developed for bilateral measures (task completion time, goal synchronization, movement overlap time, interlimb coupling, continuous relative phase and asynchrony). These instrumented measurements had moderate to good discriminant and convergent validity, but reliability and responsiveness assessments were lacking.
Conclusions
A large number of quantitative bimanual assessments involving different tools, bimanual tasks and specific variables developed to evaluate bimanual function were found. Development of other relevant variables and validation of these tools are needed to further determine their usefulness, both as research outcomes and to guide therapies in clinical practice. Future research, involving younger children and real-life assessments, will improve our understanding of bimanual function in children with cerebral palsy.
Similar content being viewed by others
Background
Most daily activities require both hands (e.g., buttoning a shirt, tying laces and opening a bottle). For children with cerebral palsy (CP), accomplishing these daily activities can be challenging because of the motor deficit, limited range of motion, lack of motor control and spasticity of their impaired upper limb (UL) [1,2,3]. Bimanual movements are defined as both hands working together to achieve a goal. They are more complex than unimanual movements since they involve coordination of both ULs, with coupling of the movement amplitude and direction of both hands (spatial and temporal constraints) [4, 5]. Difficulty executing bimanual tasks is one of the greatest causes of functional impairment for these children because it impacts their participation and quality of life [6,7,8]. Furthermore, since new, innovative therapies focus on developing and training bimanual performance to improve participation in daily life activities [9], validated evaluation of bimanual movements has become crucial.
Instrumented measurements of UL movements are being developed [10]. 3D movement analysis (3DMA), which is now used routinely for gait analysis [11], is becoming increasingly used for UL analysis, and typical measures include spatiotemporal and kinematic variables. However, 3DMA is mostly used to assess unimanual movements that do not reflect real life since most everyday tasks require the cooperative use of both hands [12]. Few protocols have been developed to assess spontaneous use of the impaired UL in bimanual conditions. The main challenge relating to such protocols performed in a laboratory setting is choosing appropriate bimanual movements that capture how children really move in their daily environment and that are representative of the large number of possible UL movements. Other, child-friendly tools are being increasingly developed to evaluate spontaneous and representative UL use. For example, accelerometers have many advantages (low cost, small size, accurate measurement, etc.), in particular, they can be used out with the laboratory setting in the child’s own environment [13].
Bimanual movement assessment with these quantitative tools is promising, increasingly used and required by both the research and clinical communities. However, a review of available tools, protocols, variables and metrological validation is lacking. Such a review would improve the understanding of impaired movements and would help to more accurately tailor interventions in children with CP. Moreover, few measures have been validated, although this is necessary to determine what is really measured.
The purpose of this systematic review was therefore to report instrumented tools (3DMA, sensors, etc.) and the metrological properties of the measures used to evaluate bimanual movements in children with CP. This systematic review aimed to (1) describe the types of instrumented tools used; (2) identify how data were collected and analyzed (protocols and variables); and (3) report the available evidence of validation of these measures (convergent and discriminant validity, within/between reliability and responsiveness) and (4) identify relevant outcomes for research and clinical application. Based on this review, we wished to draft a set of recommendations for the instrumented measurement of bimanual movements for future clinical development and research.
Methods
Reglementary issues
This systematic review is reported according to the PRISMA guidelines. A PRISMA checklist was completed and the review protocol was published in Prospero (CRD42022308517).
Identification and selection of studies
Searches were conducted in English in the following databases: PubMed (1996 to March 2022), Scopus (2004 to March 2022), Cochrane Library (1995 to March 2022) and Web of Science (2004 to March 2022). To ensure the search was exhaustive, the following combinations of keywords were used: (1) keywords relative to children and adolescents: “child”, “adolescent”, “teen”, “infant”, “baby”, “newborn”; (2) “upper limb”, “upper extremities”, “upper body”, “arm”, “hand”, “bimanual”, “interlimb”; (3) “movement”,”motion”, “motor”, “biomechanical”, “kinematic”, “instrumented measurement”, “inertial”, “sensors”, “accelerometer”, “technologies”, “spatiotemporal”, “temporo-spatial”, “smoothness”, “fluidity”, “trajectory”; 4) “Cerebral Palsy”, “hemiplegia”, “hemiparesis”, “quadriplegia”, “tetraplegia”, “stroke”, “cerebrovascular accident” (the detailed equation is provided in Additional file 1). Search strings were formulated and tailored to the search syntax of each database to ensure a common search strategy.
Inclusion criteria were: (1) Design: full papers; (2) Participants: children and adolescents 0–18 years old with uni- or bilateral cerebral palsy; (3) Construct: exploration of bimanual movements (i.e. both hands used to achieve a goal) during symmetrical or asymmetrical tasks; (4) Type of instruments: quantitative instruments (3DMA, accelerometers, etc.); (5) Outcome measures: quantitative/instrumental measures of UL characteristics (spatiotemporal and/or kinematics and/or quality of movement variables and/or accelerometry) (see Additional file 2). Exclusion criteria were: (1) studies that evaluated spontaneous UL use (either unimanual or bimanual; no specific task) with no information on bimanual movements in the results section; (2) studies out of scope or not relating to motion analysis (e.g., electromyography or only force assessment); (3) conference papers; and (4) studies not published in English. Studies that included participants older than 18 years were also included, even if it was not possible to dissociate the results of the adults from those of the children and adolescents. Studies that included both typically developing children (TDC) and children with CP (unilateral or bilateral) were included, but the data from the TDC were not analyzed.
Two independent reviewers screened the titles and abstracts of the selected papers for inclusion. In case of disagreement, the full article was read and discussed until a consensus was reached.
Assessment of characteristics of studies
The two reviewers extracted all the data independently.
Quality assessment
Intrinsic quality of articles and biomechanical methods (Q-score)
Study quality was assessed using a customized quality assessment scale developed from other scales in the literature used in the field of biomechanics or radiology [14,15,16]. The aim of the scale was to assess the intrinsic quality of each article and the quality of the biomechanical method using a Q score from 0 to 32 (Additional file 3). The first part of the scale was based on previously published quality checklists for systematic reviews as well as scales for the assessment of the quality of studies included in systematic reviews [17,18,19]. It included questions relating to study design and the quality of the reporting of methodologies and results, for example, “were the aims clearly stated?”. The second part of the scale related to the quality of the biomechanical protocol description, data acquisition and analysis, based on a previous scale used in this field [20] and other fields [14,15,16]. The quality rating was carried out independently by two reviewers (MC and AL) and disagreements were resolved by consensus.
Quality of metrological properties (COSMIN score)
For studies that specifically evaluated metrological properties, the Consensus based Standards for the selection of health Measurement Instruments (COSMIN) score risk of bias checklist 2017 [21, 22] was used to calculate a quality score for each metrological property. In this checklist, 3 boxes (“Hypotheses testing for construct validity”, “Reliability” and “Responsiveness”) were used. Each item in the boxes was rated as “very good” (3 points), “adequate” (2 points), “doubtful” (1 point) or “inadequate” (0 points). Convergent validity was assessed with Box 9.a (4 items, score/12), discriminant validity with Box 9.b (3 items, score/9), reliability with Box 6 (3 items, score/9) and responsiveness with Box 10.a (3 items, score/9).
Participants
Number of children and adolescents and demographics (age, sex, type of CP, topography of motor disorders, Manual Ability Classification System [MACS], etc.) were extracted.
Type of instruments
The following motion analysis data were extracted: type of instruments used, model; number, size and position of markers or sensors; sampling frequency (Hz); biomechanical model; specific algorithms and data analysis; protocols performed; starting position of the child; number of trials/sessions; velocity; duration of the protocol. The metrological properties (reliability, validity, responsiveness) were collected for each study. Construct validity was evaluated, including convergent validity (correlation with a gold standard measure or comparison with other outcome measurement instruments), and discriminant validity (ability to discriminate children with CP from another population). Articles in which children with CP were compared to TDC were considered to assess discriminant validity. Within/between rater/session reliability (ability of a test to provide the same measurement twice, e.g., intra-trial, inter-trial, test–retest) was evaluated with the measurement error and responsiveness (ability to detect a change before and after therapy). Studies that determined pre- and post-therapy effects and did not specifically assess the responsiveness of the measure were not considered to assess responsiveness.
Outcome measures
The following outcome measures were explored: spatiotemporal (velocity, duration, acceleration, distance, etc.), kinematic (angular values for the trunk, shoulder, elbow and wrist), quality of movement (smoothness, straightness, etc.) and actimetry (intensity and time). Variables measuring unilateral movement (only the affected UL during bimanual movements) and bilateral measures (both UL during bimanual movements) were distinguished.
Data analysis
A descriptive analysis of samples, type of instruments and outcome measures was performed. Quantitative results are expressed as mean (standard deviation [SD]) and categorical results as number (%). We did not conduct a meta-analysis because of the large number of protocols, heterogeneity of samples and varied outcome measures that prevented such an analysis.
Results
Flow of studies
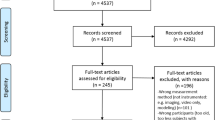
The initial search identified 2015 papers published since 1995 after removal of duplicates. Following screening of titles and abstracts, 285 articles were deemed appropriate for full text screening. Of the 285 articles reviewed, 254 were excluded. The remaining 31 were included in the review (Fig. 1).
Characteristics of included studies
The aim of the studies was mostly to increase understanding of bimanual movement in different conditions (Fig. 2).
Quality assessment
The mean Q-score of the articles included was 22/32 (SD 4.7). Seven articles had a score above 80% [23,24,25,26,27,28,29], nineteen articles had a score between 60 and 80% [30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47] and six articles had a score between 60 and 40% [48,49,50,51,52,53]. Details of the Q-scores of each article are provided in Additional file 4.
Participants
In total, 452 children and young adults with CP, aged from 2 to 25 years (mean age 10.9 years [SD 3.2]) performed bimanual movements in the 31 studies and were included (Table 1). The majority had unilateral CP (uCP), only 3 children had bilateral CP [32, 41]. They were mainly female (318 females/241 males), with right-side impairment (161 left/181 right) and MACS level from I to III. Children under 5 years of age were included in 5/32 studies [23, 26, 35, 38, 49]). Children with uCP and TDC of same ages were included in 14 studies [23,24,25, 31, 33, 34, 36, 37, 39, 41,42,43, 47, 48]. One study compared children with uCP to an adult group [39].
Type of instruments
The 31 studies used 3 different types of measurement systems: (1) 3DMA, including optoelectronic systems (Optotrack®, VICON®, Qualisis®, MIE Medical Research®) [24, 25, 27, 28, 30,31,32,33,34,35,36, 38,39,40,41,42, 44,45,46, 49,50,51,52,53] and electromagnetic systems (Polhemus®) [26, 29]), (2) accelerometers (ActiGraph®) [23, 26] and (3) other instruments (bespoke instrumented cube [43], Kinect device [48] or digitizer with two pens [47]) (Table 2). The 3DMA studies used models with 2 to 41 markers positioned on both ULs. Markers were always positioned on the wrists, they were also positioned on the trunk in 9 studies and on the hips in 1 study [44]. They used between 3 and 13 infrared cameras with a sampling frequency of 50–200 Hz. Few studies reported the biomechanical model used for the data analysis. The studies that used actimetry all used two accelerometers: one on each wrist and none on the trunk [23, 26].
Most of the protocols assessed functional tasks (Table 3). This included daily tasks (ex: placing a hat on the head, opening a drawer, picking up a box, food preparation, playing, etc.) performed in a laboratory setting (n = 13), that were mainly recorded with 3DMA systems [26,27,28,29,30, 33,34,35,36,37,38, 42, 48]. Child-friendly protocols were used, including game scenarios (n = 5), such as 3D virtual environment [48], videogames (Kinect [48], Nintendo Wii [32]) or projection of a scene on a screen [24, 25, 53]. The drawer opening task was the most frequently used (n = 7) [26,27,28, 33,34,35, 38], followed by bimanual reach to grasp tasks (n = 5) [36, 43, 48,49,50,51,52], a box pick-up task (n = 3) [29, 36, 37] and bimanual circular movements (n = 3) [31, 44, 47]. The studies that used actimetry recorded the Assisting hand assessment (AHA) test session, rating the effectiveness of affected hand use during semi-structured, bimanual play activities [23, 26]. No studies evaluated spontaneous bimanual movement during free play or activities of daily living and none evaluated movement in the child’s home environment. Ten studies explored a combination of bimanual tasks (2–5 different tasks). In 5 studies, data from the bimanual tasks were only analysed for the impaired UL and not both ULs [24, 25, 30, 42, 48].
In most studies, the starting position was almost the same: sitting on a chair at a table with the knees and elbows flexed at 90° [24,25,26,27,28,29, 31, 33,34,35, 37,38,39,40, 42,43,44,45,46,47,48,49,50,51,52,53]. The tasks were performed under different conditions: object size, height and grasp-type [34, 39, 51, 53], target position [40, 41, 45, 46, 52], environmental feedback (ex: mirror or opaque screen) [31, 44,45,46], each hand performance of asymmetrical bimanual tasks [26, 29, 33, 35, 47], or increasing difficulty [32]. Participants performed tasks at their self-selected speed, and 3 studies analysed maximum speed [33, 34, 53]. One to 5 trials were recorded, with at least 1 practice trial, except for the accelerometery measures that were recorded directly [23, 26]. The children and adolescents performed between 1 and 4 sessions of each protocol (most often 1 session [23, 25, 28, 29, 32,33,34, 36, 37, 39, 42,43,44,45, 47,48,49,50,51,52,53]. Protocol durations were from a few minutes to 1 h.
Outcome measures
Instrumented measurements were mainly used to calculate spatiotemporal variables during bimanual movements (26/32 studies) [27,28,29,30,31,32,33,34,35, 37,38,39,40,41,42,43,44, 48] (Table 4). Movement time, mean and peak velocity were the most frequently measured. Trunk and upper limb joint (mostly elbow and wrist) kinematics were evaluated in 15 studies [24, 25, 27, 27, 28, 30, 32, 34, 38, 39, 42, 48, 51,52,53]. One study focused on hand movements [36]. Studies that evaluated movement quality analysed smoothness, trajectory (Index of Curvature (IOC) [24], accuracy [29] and circularity [47]. Smoothness was analysed by the number of movement units [30, 40, 41], spectral arc length (SPARC) [24, 43], number of velocity peaks [47, 48], normalized jerk [31], relative phase [45], and dysfluency of hand movement [53]. Four variables were calculated from accelerometery: mean activity count [23], asymmetry index [23], duration of limb use [26] and goal synchronization [26]. Bilateral movements were analysed with 6 specifically developed spatiotemporal variables: task completion time, goal synchronization of the hands, movement overlap time [27, 28, 33,34,35, 38], interlimb coupling [29, 31, 49,50,51,52], continuous relative phase [31, 44, 47] and asynchrony [53]. Task completion time, goal synchronization of the hands and movement overlap time were only analysed in the drawer-opening task [27, 28, 33,34,35, 38].
Validation of metrological properties
In total, 22 studies evaluated one or more metrological properties of their instrumented measures [23,24,25,26,27,28,29,30,31, 33,34,35,36,37,38,39,40,41,42,43, 46, 48] (Table 5).
Convergent validity
The mean COSMIN score of the studies that assessed convergent validity was 10/12 points.
Seven of the 31 studies evaluated correlations between the variables calculated from the instrumented assessments and scores on clinical assessments. Of these 7 studies, 3 used unimanual clinical assessments (MACS, Jebsen–Taylor Hand Function Test (JTHFT), [23, 26, 29, 42, 48]) and 5 used bimanual assessments (AHA, Abilhand-Kids, Children’s Hand-use Experience Questionnaire (CHEQ) [24, 25, 28, 29, 35, 42]).
Among those that used unimanual clinical assessments, no correlation was found between MACS level and movement time or kinematic values [42]. Moderate correlations were found between JTHFT and goal synchronisation (r = 0.634, p < 0.05), and total task duration (r = 0.39, p < 0.05) [29].
Among those that used bimanual clinical assessments, the highest correlation was found between the AHA score and Arm Profile Score (APS) (a kinematic index) (r = − 0.84, P < 0.001) [24]. Low to moderate correlations were found between AHA score and bilateral movement measures (total movement time and goal synchronisation) (r = -0.3 p < 0.05) [28] and no correlation was found for normalized movement overlap [28, 35]. The AHA “smoothness of movement” item was moderately and significantly correlated with the SPARC and IOC quality of movement parameters [23]. Poor to good significant correlations were found between Abilhand-Kids and the maximum angular value (MAX) and range of motion (ROM) (r = 0.36–0.58, p < 0.03) [25, 42], and movement time (r = 0.769, p = 0.001) [42]. CHEQ sub-scores for the affected hand were significantly correlated with total task duration (r = 0.41–51, p < 0.05), temporal coupling (r = 0.36, p < 0.05) and spatial accuracy (r = 0.41–0.59; p < 0.05) [29].
Discriminant validity
The mean COSMIN score of the studies that assessed discriminant validity was 8/9 points.
Twelve studies compared children and adolescents with uCP and TDC [23,24,25, 31, 33, 34, 36, 37, 39, 42, 43, 48]. The main results were that children with uCP had restricted ROM of shoulder elevation, plane of elevation, elbow extension, supination, wrist extension and wrist adduction/abduction, and vertical and lateral hand movements compared to TDC during bimanual tasks [24, 25, 36, 37, 39, 42, 48].
Children and adolescents with uCP had altered spatiotemporal variable values, with longer movement durations [31, 37, 42, 48] and lower peak velocities [39, 48] compared to TDC. Children and adolescents with uCP used their hands less often at the same time (less goal-synchronized), with less interlimb coupling [33, 34] than TDC. Hand trajectories were less smooth [24, 31, 43, 48] and also less straight [24] in children and adolescents with uCP. The duration of use of each UL was more asymmetrical in children with uCP because the affected UL was underused as compared with TDC [23].
Reliability
The mean COSMIN score of the studies that assessed reliability was 14/15 points.
Reliability was evaluated in 2 studies, either within-session [24] or both within and between sessions [25]. These studies explored 2 different versions of a protocol (‘Be An Airplane Pilot’ (BE API) and BE API 2.0). Within session reliability was assessed during 3 or 4 movement cycles for each task. Between-session reliability was assessed at an interval of 2 and 4 weeks. Reliability was assessed with correlated multiple correlations (CMC), intraclass correlation coefficients (ICC) and measurement errors (minimum detectable change [MDC] and standard error of measurement [SEM]). Within- and between-session reliability were high for kinematic variables: CMC > 0.82; ICC > 0.85, SEM 4.78° and moderate for smoothness and trajectory (ICC > 0.53).
Responsiveness
The mean COSMIN score of the studies that assessed responsiveness was 8/12 points.
The main objective of the studies was to evaluate the effect of an intervention but not specifically the responsiveness of the measures. Seven studies performed assessments pre- and post-intervention: Constraint-Induced Movement Therapy (CIMT) [30, 35], Hand and Arm Bimanual Intensive Therapy (HABIT) [26, 35, 38], structured practice [27] and synchronized metronome training [40, 41]. All outcome measures changed significantly post-intervention except after CIMT [30]. After HABIT, goal synchronization time (p < 0.05) [26, 35], movement overlap (p = 0.005) [35] and % time of bimanual movements (p = 0.001) increased [38], and kinematic variables improved (trunk displacement decreased [26%, p < 0.05] and UL joint excursion [30%, p < 0.01] and elbow extension increased [25%, p < 0.05] on the affected side) [38]. Similar findings were reported for structured/unstructured practice although kinematic variables only improved for structured practice [27]. Two studies reported significant changes in smoothness, distance and ROM of elbow, wrist and shoulder after metronome training [40, 41].
Synthesis of outcome measures evaluated for clinical and research purposes
Spatiotemporal variables were evaluated both for research and clinical practice. Bilateral variables were used for research [28, 38, 44, 47, 49,50,51,52] and clinical practice (pre-post intervention [27, 35, 37]) but only one study evaluated convergent validity: goal synchronization was correlated with the unimanual JTHFT assessment [33]).
The outcome measures that underwent the most validity assessments were ROM, MAX, APS, SPARC and IOC (convergent, discriminative validity and reliability) for research purposes [24, 25]. Accelerometery variables (mean activity count and asymmetry index) were used for convergent, discriminative validity and pre-post therapy, both in research and clinical settings [23, 26]. Kinematic (ROM), spatiotemporal variables (peak velocity, movement time, number of movement units and movement duration) [27, 30, 35, 37, 40, 41, 48] and quality of movement variables (smoothness) were used to assess the effect of therapy.
Discussion
This systematic review of studies that used instrumented assessments of bimanual movements, most often 3DMA, in children and young adults with uCP aged from 2 to 25 years, found that the majority of studies were of good to very good quality (mean Q score 22/32). The protocols evaluated were varied, involving 1 to 5 bimanual tasks that mostly represented activities of daily living or were part of a game scenario. Spatiotemporal variables were most often evaluated, including 6 variables specifically developed for the assessment of bimanual movement: task completion time, goal synchronization, movement overlap time, interlimb coupling, continuous relative phase and asynchrony. The instrumented measures demonstrated moderate to good discriminant and convergent validity, but reliability and responsiveness assessments were lacking. All types of variables discriminated between children and adolescents with CP and TDC and were used to assess UL therapy efficacy with relevant results, therefore demonstrating their potential for clinical and research purposes.
Types of instruments
A wide variety of instruments has been used to quantitatively evaluate bimanual movements, depending on the objective or variables of interest (ex: accelerometers for actimetry). Most studies used 3DMA, probably because this was the first tool to be developed and because it has been shown to be consistent and accurate for gait analysis, for which it has become the gold standard [11]. However, the 3DMA system set-up for UL recordings appears to lack consensus with regard to the number of cameras, markers, etc. 3DMA is performed in a laboratory setting to measure standardized, reliable movements that may differ from those performed in daily life. We recommend the use of 3DMA as it provides an objective and accurate measure, which complements the clinical assessment but with more technical standardization. The results of this review also highlighted that other recently developed technologies, which involve smaller and less constraining systems, e.g. accelerometers, can be used [23, 26]. However, no studies have yet used these instruments to provide out-of-laboratory assessments and to investigate bimanual movements directly in daily situations (e.g. at home), likely because real-life measures are less standardized, require greater tolerance for longer recordings, and the analysis of bimanual data from the real-life setting is challenging [13]. Accelerometers or inertial measurement units should be increasingly used to measure UL performance in the home setting, i.e., how the child spontaneously uses their impaired UL in real life. Another pertinent suggestion is to adapt daily life objects to perform direct recordings in the child’s usual environment (e.g., toys, etc.) and to get away from the context of evaluation [41]. We recommend the development of tools that allow direct measurement of UL movements in real-life situations with as few constraints on the child as possible. This is necessary to improve understanding of the effects of therapies and to adapt them to the real difficulties encountered in daily life (Additional file 5).
Protocols
The protocols lacked standardization, they involved different data collection procedures and, most importantly, different bimanual tasks. The choice of tasks for bimanual movement assessment is a real challenge because of the large variety of movements that can be performed with both ULs (symmetrical/asymmetrical, free/constrained, with/without object, proximal/distal, etc.). Hung et al. proposed a unique task, ‘the drawer-opening task’ [26,27,28, 33,34,35, 38], mainly to study coordination, however, most protocols used several tasks to provide a comprehensive and global assessment of bimanual movement. Based on the results of this review, we recommend the use of a set of 3 to 5 tasks both to provide an overview of the performance of different bimanual movements and to ensure precision, while also maintaining the attention and participation of the child during the assessment. To evaluate spontaneous movements as they are performed in daily life, tasks that involve interaction with objects should be evaluated: bimanual UL movement is often induced by the need to grasp, manipulate or hold objects. Some studies particularly focused on interaction with objects (size and shape) [34, 39, 51, 53] and factors that interfered with interaction and how information was processed (visual disturbance) [31, 44,45,46] to evaluate all the situations that the child may face in daily life and to contribute to the understanding of bimanual function. In laboratory conditions, we recommend the assessment of simple daily movements (e.g., dressing, drinking and holding) or tasks within a game scenario [24, 25, 32, 48, 53] to better reflect spontaneous bimanual movements, whilst still being reproducible. The environment could be enhanced by video games or virtual reality [47]. The results of the review also support the need to directly assess bimanual movement in real-life situations (at home or school) (Additional file 5).
Outcome measures
Spatiotemporal variables were the most often analysed. They were mainly used to describe the characteristics of bimanual movements and to evaluate the effect of therapies. Six bilateral variables were specifically developed to assess bilateral movements. Most bilateral variables were spatiotemporal and were designed for the ‘drawer-opening task’ [26,27,28, 33,34,35, 38] whereas other bilateral variables explored coordination between both hands [31, 44, 47, 53]. These variables may constitute important indicators since children and adolescents with CP use different motor coordination patterns during daily bimanual activities. Moreover, understanding coordination patterns could guide researchers and clinicians in the development of intervention programs that aim to improve bimanual hand coordination performance [6]. However, these variables have only been partially validated; reliability and responsiveness have yet to be determined. With regards to UL kinematics, similar variables to those used in unimanual assessments have been used to assess each UL separately, often to compare the ULs, however, no variables have been specifically developed to evaluate joint angles during bimanual movements. Quality of movement variables, i.e., smoothness or straightness, provide information that is difficult to obtain precisely with clinical assessments; this is a real advantage of motion analysis. However, there is also no consensus on the best way to measure some of these quality of movement variables (e.g. smoothness was measured using 6 different methods [24, 30, 31, 40, 41, 43, 45, 47, 48, 53]) and none have been completely validated. This finding highlights the difficulty of determining relevant UL variables that could be assessed across all types of bimanual tasks. According to the results of this review, we recommend that a comprehensive assessment of UL impairment should include spatiotemporal, kinematic and quality of movement parameters, including specific bilateral variables (goal synchronization, movement overlap time, etc.). This would help to better characterize pathological movements and to further determine those that are most relevant to guide the focus of therapies in clinical practice (Additional file 5).
Validation of instrumented measures
The results of this review showed that most measures have not been fully validated. Reliability and responsiveness properties have not been sufficiently assessed, despite their importance. A representative example is the “drawer task”: it was used in 7 studies but only convergent and discriminant validity have been confirmed. Discriminant validity was the most evaluated: all the tools were able to differentiate between children with CP and TDC for all types of variables and bimanual tasks. Moreover, other types of discriminant validity were also evaluated, i.e. comparison between uni and bimanual movements [40, 41, 46, 47, 49,50,51,52] and comparison of the affected and non-affected ULs during asymmetrical tasks [29, 33, 40, 41]. Future studies should include an evaluation of reliability since we found only 2 studies that assessed this property [24, 25]. Given the complexity of UL movements and the use of different instruments/markers, reliability must be evaluated because factors such as the child’s position could impact the accuracy and interpretation of the measure. In this review, we were unable to properly report on the responsiveness of the tools as it was not the main objective of the studies included. However, most studies demonstrated changes in the values of variables after different interventions, whatever the protocol and variables assessed. Therefore, instrumented assessments appear to be good indicators of therapy efficacy. Regarding convergent validity, the highest correlations were found for assessments of the impaired UL during bimanual tasks, the AHA and APS (a kinematic deviation index of the impaired UL), whereas bilateral variables were not correlated, demonstrating the pertinence of evaluating both ULs to better reflect bimanual function.
Limitations
This review has some limitations. The lack of standardization of protocols and systems made direct comparisons of results between studies challenging. The quality of the articles included ranged widely (from 13 to 30/32): full descriptions of data acquisition and adherence to biomechanical recommendations (e.g., International Society of Biomechanics) were frequently missing. Furthermore, no studies reported a priori sample size calculations, therefore the statistical power is unknown. Among the articles included, 8 were from the same team [26,27,28, 33,34,35,36, 38]. The quality scale developed was provided to help interpretation but has not been previously validated, therefore, the quality results should be interpreted with caution. The age range of the children and adolescents who were compared in this review was very wide: analysis by age is necessary as toddlers and young adults may have different bimanual function. The results could not be generalized to all children and adolescents with CP as there was a lack of assessment in younger children and those with bilateral CP. Future research, involving younger children (pre-schoolers), and taking into account the different degrees of UL impairment (MACS 3–5) and diversity of CP type (bilateral CP, dyskinetic), will improve our understanding of bimanual movements and their development in these children and adolescents (Additional file 5).
Conclusion
This systematic review reported a large number of instrumented measurements of bimanual movements in children with CP, in good- to high-quality studies. These assessments involved different systems (3DMA, accelerometers, etc.) and different bimanual tasks (drawer-opening task, reach to grasp, etc.), and spatiotemporal parameters were mostly calculated in bimanual conditions. Some specific variables were developed for the evaluation of bimanual function (ex: goal synchronization). However, the metrological properties of these instruments were not fully evaluated, especially reliability and responsiveness. The complementary information provided by instrumented measures in relation to clinical assessments of bimanual function was highlighted. Development of other relevant variables and validation of these tools are required before they can be used as research outcomes or in clinical practice. Studies that involve younger children and real-life assessments will improve our understanding of bimanual function in these children.
Availability of data and materials
All data generated or analysed during this study are included in this published article and its Additional files.
Abbreviations
- 3DMA:
-
3D motion analysis
- AHA:
-
Assisting hand assessment
- APS:
-
Arm profile score
- BE API:
-
Be an airplane pilot
- CHEQ:
-
Children’s Hand-use Experience Questionnaire
- CIMT:
-
Constraint-induced movement therapy
- CMC:
-
Correlated multiple correlations
- COSMIN:
-
Consensus based Standards for the selection of health Measurement Instruments
- CP:
-
Cerebral palsy
- HABIT:
-
Hand and arm bimanual intensive therapy
- ICC:
-
Intraclass correlation coefficients
- IOC:
-
Index of curvature
- JTHFT:
-
Jebsen–Taylor hand function test
- MACS:
-
Manual ability classification system
- MAX:
-
Maximum angular value
- MDC:
-
Minimum detectable change
- ROM:
-
Range of motion
- SEM:
-
Standard error of measurement
- SPARC:
-
Spectral arc length
- TD:
-
Typically developing
- uCP:
-
Unilateral cerebral palsy
- UL:
-
Upper limb
References
Gordon AM, Bleyenheuft Y, Steenbergen B. Pathophysiology of impaired hand function in children with unilateral cerebral palsy. Dev Med Child Neurol. 2013;55:32–7. https://doi.org/10.1111/dmcn.12304.
Braendvik SM, Elvrum A-KG, Vereijken B, Roeleveld K. Relationship between neuromuscular body functions and upper extremity activity in children with cerebral palsy. Dev Med Child Neurol. 2010;52:e29-34. https://doi.org/10.1111/j.1469-8749.2009.03490.x.
Klingels K, Demeyere I, Jaspers E, De Cock P, Molenaers G, Boyd R, et al. Upper limb impairments and their impact on activity measures in children with unilateral cerebral palsy. Eur J Paediatr Neurol. 2012;16:475–84. https://doi.org/10.1016/j.ejpn.2011.12.008.
Blinch J, Doan JB, Gonzalez CLR. Complexity of movement preparation and the spatiotemporal coupling of bimanual reach-to-grasp movements. Exp Brain Res. 2018;236:1801–13. https://doi.org/10.1007/s00221-018-5264-9.
Klevberg GL, Østensjø S, Krumlinde-Sundholm L, Elkjær S, Jahnsen RB. Hand function in a population-based sample of young children with unilateral or bilateral cerebral palsy. Phys Occup Ther Pediatr. 2017;37:528–40. https://doi.org/10.1080/01942638.2017.1280873.
Wang T-N, Howe T-H, Liang K-J, Chang T-W, Shieh J-Y, Chen H-L. Bimanual motor performance in everyday life activities of children with hemiplegic cerebral palsy. Eur J Phys Rehabil Med. 2021. https://doi.org/10.23736/S1973-9087.21.06504-7.
Chang TW, Hsiao LC, Huang KL, Liu YC, Chen HL, Wang TN. Investigating bimanual motor performance on daily bimanual tasks in children with hemiplegic cerebral palsy. J Neurol Sci. 2017;381:112–3. https://doi.org/10.1016/j.jns.2017.08.355.
de Oliveira RHS, de Brito Brandão M, de Melo Mambrini JV, Mancini MC. Interest of children with unilateral spastic cerebral palsy in bimanual daily activities. Scand J Occup Ther. 2019. https://doi.org/10.1080/11038128.2018.1561938.
Demont A, Gedda M, Lager C, de Lattre C, Gary Y, Keroulle E, et al. Evidence-based, implementable motor rehabilitation guidelines for individuals with cerebral palsy. Neurology. 2022. https://doi.org/10.1212/WNL.0000000000200936.
Francisco-Martínez C, Prado-Olivarez J, Padilla-Medina JA, Díaz-Carmona J, Pérez-Pinal FJ, Barranco-Gutiérrez AI, et al. Upper limb movement measurement systems for cerebral palsy: a systematic literature review. Sensors. 2021;21:7884. https://doi.org/10.3390/s21237884.
Gage JR. Gait analysis. An essential tool in the treatment of cerebral palsy. Clin Orthop Relat Res. 1993;288:126–34.
Jaspers E, Desloovere K, Bruyninckx H, Molenaers G, Klingels K, Feys H. Review of quantitative measurements of upper limb movements in hemiplegic cerebral palsy. Gait Posture. 2009;30:395–404. https://doi.org/10.1016/j.gaitpost.2009.07.110.
Braito I, Maselli M, Sgandurra G, Inguaggiato E, Beani E, Cecchi F, et al. Assessment of upper limb use in children with typical development and neurodevelopmental disorders by inertial sensors: a systematic review. J Neuroeng Rehabil. 2018. https://doi.org/10.1186/s12984-018-0447-y.
Borotikar B, Lempereur M, Lelievre M, Burdin V, Salem DB, Brochard S. Dynamic MRI to quantify musculoskeletal motion: a systematic review of concurrent validity and reliability, and perspectives for evaluation of musculoskeletal disorders. PLoS ONE. 2017;12:e0189587. https://doi.org/10.1371/journal.pone.0189587.
Pons C, Borotikar B, Garetier M, Burdin V, Ben Salem D, Lempereur M, et al. Quantifying skeletal muscle volume and shape in humans using MRI: a systematic review of validity and reliability. PLoS ONE. 2018;13:e0207847. https://doi.org/10.1371/journal.pone.0207847.
Pons C, Rémy-Néris O, Médée B, Brochard S. Validity and reliability of radiological methods to assess proximal hip geometry in children with cerebral palsy: a systematic review. Dev Med Child Neurol. 2013;55:1089–102. https://doi.org/10.1111/dmcn.12169.
von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: guidelines for reporting observational studies. Int J Surg. 2014;12:1495–9. https://doi.org/10.1016/j.ijsu.2014.07.013.
Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health. 1998;52:377–84. https://doi.org/10.1136/jech.52.6.377.
Whiting P, Rutjes AWS, Reitsma JB, Bossuyt PMM, Kleijnen J. The development of QUADAS: a tool for the quality assessment of studies of diagnostic accuracy included in systematic reviews. BMC Med Res Methodol. 2003;3:25. https://doi.org/10.1186/1471-2288-3-25.
Lempereur M, Brochard S, Mao L, Rémy-Néris O. Validity and reliability of shoulder kinematics in typically developing children and children with hemiplegic cerebral palsy. J Biomech. 2012;45:2028–34. https://doi.org/10.1016/j.jbiomech.2012.05.020.
Mokkink LB, de Vet HCW, Prinsen CAC, Patrick DL, Alonso J, Bouter LM, et al. COSMIN risk of bias checklist for systematic reviews of patient-reported outcome measures. Qual Life Res. 2018;27:1171–9. https://doi.org/10.1007/s11136-017-1765-4.
Terwee CB, Mokkink LB, Knol DL, Ostelo RWJG, Bouter LM, de Vet HCW. Rating the methodological quality in systematic reviews of studies on measurement properties: a scoring system for the COSMIN checklist. Qual Life Res. 2012;21:651–7. https://doi.org/10.1007/s11136-011-9960-1.
Beani E, Maselli M, Sicola E, Perazza S, Cecchi F, Dario P, et al. Actigraph assessment for measuring upper limb activity in unilateral cerebral palsy. J Neuroeng Rehabil. 2019;16:30. https://doi.org/10.1186/s12984-019-0499-7.
Cacioppo M, Marin A, Rauscent H, Le Pabic E, Gaillard F, Brochard S, et al. A new child-friendly 3D bimanual protocol to assess upper limb movement in children with unilateral cerebral palsy: development and validation. J Electromyogr Kinesiol. 2020;55:102481. https://doi.org/10.1016/j.jelekin.2020.102481.
Gaillard F, Cacioppo M, Bouvier B, Bouzille G, Newman CJ, Pasquet T, et al. Assessment of bimanual performance in 3-D movement analysis: validation of a new clinical protocol in children with unilateral cerebral palsy. Ann Phys Rehabil Med. 2019. https://doi.org/10.1016/j.rehab.2019.06.008.
Gordon AM, Schneider JA, Chinnan A, Charles JR. Efficacy of a hand-arm bimanual intensive therapy (HABIT) in children with hemiplegic cerebral palsy: a randomized control trial. Dev Med Child Neurol. 2007;49:830–8. https://doi.org/10.1111/j.1469-8749.2007.00830.x.
Hung Y-C, Brandão MB, Gordon AM. Structured skill practice during intensive bimanual training leads to better trunk and arm control than unstructured practice in children with unilateral spastic cerebral palsy. Res Dev Disabil. 2017;60:65–76. https://doi.org/10.1016/j.ridd.2016.11.012.
Hung Y-C, Robert MT, Friel KM, Gordon AM. Relationship between integrity of the corpus callosum and bimanual coordination in children with unilateral spastic cerebral palsy. Front Hum Neurosci. 2019. https://doi.org/10.3389/fnhum.2019.00334.
Rudisch J, Butler J, Izadi H, Zielinski IM, Aarts P, Birtles D, et al. Kinematic parameters of hand movement during a disparate bimanual movement task in children with unilateral Cerebral Palsy. Hum Mov Sci. 2016;46:239–50. https://doi.org/10.1016/j.humov.2016.01.010.
Cope SM, Liu X-C, Verber MD, Cayo C, Rao S, Tassone JC. Upper limb function and brain reorganization after constraint-induced movement therapy in children with hemiplegia. Dev Neurorehabil. 2010;13:19–30. https://doi.org/10.3109/17518420903236247.
Feltham MG, Ledebt A, Bennett SJ, Deconinck FJA, Verheul MHG, Savelsbergh GJP. The “mirror box” illusion: effect of visual information on bimanual coordination in children with spastic hemiparetic cerebral palsy. Mot Control. 2010;14:68–82. https://doi.org/10.1123/mcj.14.1.68.
Howcroft J, Klejman S, Fehlings D, Wright V, Zabjek K, Andrysek J, et al. Active video game play in children with cerebral palsy: potential for physical activity promotion and rehabilitation therapies. Arch Phys Med Rehabil. 2012;93:1448–56. https://doi.org/10.1016/j.apmr.2012.02.033.
Hung Y-C, Charles J, Gordon AM. Bimanual coordination during a goal-directed task in children with hemiplegic cerebral palsy. Dev Med Child Neurol. 2004;46:746–53. https://doi.org/10.1111/j.1469-8749.2004.tb00994.x.
Hung Y-C, Charles J, Gordon AM. Influence of accuracy constraints on bimanual coordination during a goal-directed task in children with hemiplegic cerebral palsy. Exp Brain Res. 2010;201:421–8. https://doi.org/10.1007/s00221-009-2049-1.
Hung Y-C, Casertano L, Hillman A, Gordon AM. The effect of intensive bimanual training on coordination of the hands in children with congenital hemiplegia. Res Dev Disabil. 2011;32:2724–31. https://doi.org/10.1016/j.ridd.2011.05.038.
Hung Y-C, Meredith GS. Influence of dual task constraints on gait performance and bimanual coordination during walking in children with unilateral cerebral palsy. Res Dev Disabil. 2014;35:755–60. https://doi.org/10.1016/j.ridd.2014.01.024.
Hung Y-C, Spingarn A. Whole body organization during a symmetric bimanual pick up task for children with unilateral cerebral palsy. Gait Posture. 2018;64:38–42. https://doi.org/10.1016/j.gaitpost.2018.05.028.
Hung Y-C, Ferre CL, Gordon AM. Improvements in kinematic performance after home-based bimanual intensive training for children with unilateral cerebral palsy. Phys Occup Ther Pediatr. 2018;38:370–81. https://doi.org/10.1080/01942638.2017.1337663.
Hung Y-C, Zeng W. Accuracy constraints improve symmetric bimanual coordination for children with and without unilateral cerebral palsy. Dev Neurorehabil. 2020;23:176–84. https://doi.org/10.1080/17518423.2019.1616845.
Johansson A-M, Domellöf E, Rönnqvist L. Short- and long-term effects of synchronized metronome training in children with hemiplegic cerebral palsy: a two case study. Dev Neurorehabil. 2012;15:160–9. https://doi.org/10.3109/17518423.2011.635608.
Johansson A-M, Domellöf E, Rönnqvist L. Timing training in three children with diplegic cerebral palsy: short- and long-term effects on upper-limb movement organization and functioning. Front Neurol. 2014. https://doi.org/10.3389/fneur.2014.00038.
Klotz M, Drongelen S, Rettig O, Wenger P, Gantz S, Dreher T, et al. Motion analysis of the upper extremity in children with unilateral cerebral palsy—an assessment of six daily tasks. Res Dev Disabil. 2014;35:2950–7. https://doi.org/10.1016/j.ridd.2014.07.021.
Mutalib SA, Mace M, Burdet E. Bimanual coordination during a physically coupled task in unilateral spastic cerebral palsy children. J Neuroeng Rehabil. 2019. https://doi.org/10.1186/s12984-018-0454-z.
Smorenburg ARP, Ledebt A, Feltham MG, Deconinck FJA, Savelsbergh GJP. The positive effect of mirror visual feedback on arm control in children with spastic hemiparetic cerebral palsy is dependent on which arm is viewed. Exp Brain Res. 2011;213:393–402. https://doi.org/10.1007/s00221-011-2789-6.
Smorenburg ARP, Ledebt A, Deconinck FJA, Savelsbergh GJP. Matching accuracy in hemiparetic cerebral palsy during unimanual and bimanual movements with (mirror) visual feedback. Res Dev Disabil. 2012;33:2088–98. https://doi.org/10.1016/j.ridd.2012.06.004.
Smorenburg ARP, Ledebt A, Deconinck FJA, Savelsbergh GJP. Practicing a matching movement with a mirror in individuals with spastic hemiplegia. Res Dev Disabil. 2013;34:2507–13. https://doi.org/10.1016/j.ridd.2013.05.001.
Volman MJ, Wijnroks A, Vermeer A. Bimanual circle drawing in children with spastic hemiparesis: effect of coupling modes on the performance of the impaired and unimpaired arms. Acta Physiol (Oxf). 2002;110:339–56. https://doi.org/10.1016/S0001-6918(02)00041-0.
Shum LC, Valdes BA, Hodges NJ, Van der Loos HFM. Error augmentation in immersive virtual reality for bimanual upper-limb rehabilitation in individuals with and without hemiplegic cerebral palsy. IEEE Trans Neural Syst Rehabil Eng. 2020;28:541–9. https://doi.org/10.1109/TNSRE.2019.2959621.
Sugden D, Utley A. Interlimb coupling in children with hemiplegic cerebral palsy. Dev Med Child Neurol. 1995;37:293–309. https://doi.org/10.1111/j.1469-8749.1995.tb12008.x.
Utley A, Sugden D. Interlimb coupling in children with hemiplegic cerebral palsy during reaching and grasping at speed. Dev Med Child Neurol. 1998;40:396–404.
Utley A, Steenbergen B, Sugden DA. The influence of object size on discrete bimanual co-ordination in children with hemiplegic cerebral palsy. Disabil Rehabil. 2004;26:603–13. https://doi.org/10.1080/09638280410001696674.
Utley A, Sugden DA, Lawrence G, Astill S. The influence of perturbing the working surface during reaching and grasping in children with hemiplegic cerebral palsy. Disabil Rehabil. 2007;29:79–89. https://doi.org/10.1080/09638280600947989.
Van Thiel E, Steenbergen B. Shoulder and hand displacements during hitting, reaching, and grasping movements in hemiparetic cerebral palsy. Mot Control. 2001;5:166–82. https://doi.org/10.1123/mcj.5.2.166.
Acknowledgements
We wish to thank Johanna Robertson for language assistance and constructive criticism.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
MC contributed to the design of the study, the screening of the papers, data extraction and analysis, and writing and revision of the paper. AL contributed to the screening of the papers, data extraction and analysis, and writing and revision of the papers. SB and ML contributed to the design of the study and revision of the paper. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Table S1.
Search strategy used for systematic review.
Additional file 2: Table S2.
‘Design, Participants, Construct, Type of instruments, Outcome measures’ following the COSMIN standard for systematic reviews of Patient‐Reported Outcome Measures [21].
Additional file 3.
Article quality was evaluated with a customized scale.
Additional file 4: Table S3.
Results of the Q-score (quality assessment) of each article.
Additional file 5.
Synthesis of recommendations for quantitative bimanual assessments.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Cacioppo, M., Loos, A., Lempereur, M. et al. Bimanual movements in children with cerebral palsy: a systematic review of instrumented assessments. J NeuroEngineering Rehabil 20, 26 (2023). https://doi.org/10.1186/s12984-023-01150-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12984-023-01150-7