Abstract
Introduction
The primary purpose of this project is to identify the modifiable individual, social and environmental factors associated with stress and to investigate and quantify the effect of persistent stress on chronic disease in a marginalized, primarily minority, urban community.
Methods
This study leveraged data collected as part of Temple Health: Block-By-Block, a longitudinal cohort study conducted over five years in an underserved community. Through in-home visits, 385 subjects completed a Visit 5 Social & Environmental Assessment which measured individual, social, neighborhood, and environmental factors as reported through each participant’s perspectives. A Perceived Stress Scale and a Cumulative Chronic Disease Index was also completed during this visit.
Results
Five of sixteen modifiable risk factors were identified as significant, independent predictors of stress, including general health, employment status, difficulties in paying for basics, home ownership and overall neighborhood quality. These health determinants combined with stress scores significantly predicted chronic disease burden.
Conclusions
This study provides unique, individualized evidence regarding the impact of social determinants of health on levels of stress among community residents, and suggests that stress is an intervening factor in the path to chronic disease. While addressing social determinants of health must be a priority, this study indicates that actionable behavioral and pharmacologic interventions to reduce stress may provide more immediate improvements in prevention and reduction of chronic disease in diverse urban communities.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Since the 1985 Heckler Report documenting the occurrence of approximately 60,000 excess deaths annually among minorities, there has been an irrefutable, mounting effort to address pervasive health disparities in the U.S. [1]. Escalating research efforts, community-engagement initiatives and enhanced access to comprehensive care have spurred progress, however, unacceptable gaps in health equity persist, resulting in poor health, excess medical expenditures and premature death [2]. While all minority and vulnerable populations shoulder these disparities, the burden of chronic disease and decreased life expectancy is particularly disturbing among minority populations from marginalized communities [3, 4]. While it has been long-recognized that a multi-factorial web of genetic, biologic, behavioral, and environmental factors affects development of disease, the important impact of social determinants of health (SDoH) has recently gained substantial attention. The conditions in the environments where people are born, grow, live, work, and age are now known to affect a wide range of health, functioning, and quality of life outcomes [5], however, the role of these factors in direct causation of disease remains poorly delineated.
As early as 1939 Faris and Dunham demonstrated that the collective experience of living in a disadvantaged neighborhood could be linked to a person’s mental health and well-being [6]. In 2008 stress was identified as one of the top 10 determinants of disparities in health [7]. Stress, broadly defined as a situation in which ‘environmental demands, internal demands, or both, tax or exceed the adaptive resources of an individual’ is well documented to be associated with the onset and course of many major mental and physical health conditions [8]. While a link between stress and acute mental illness seems apparent, the role of stress in other diseases is less discernable. Evidence does indicate, however, that stress can directly affect biological processes such as inflammation and immune response that are integral to the development of disease while also driving the use of maladaptive health behaviors such as smoking, decreased exercise and sleep disturbances that put individuals at risk for poor health outcomes [9,10,11]. Perceptions of stress have been associated with a range of chronic conditions and multimorbidity particularly in disadvantaged populations [12,13,14]. While stress may have a rapid onset in response to an acute event, it often has a slow and imperceptible onset progressing to a cumulative chronicity leading to physiologic “wear and tear” that may result in illness [15,16,17,18]. Although the perception of stress is subjective and varies across individuals, studies examining material deprivation, socioeconomic disadvantage, neighborhood disorder and instability point to the negative impact of persistent stress on health [19, 20].
While SDoH have been associated with levels of stress, and stress has been suggested to increase disease onset and progression, the independent role of each has not been thoroughly examined. While such characteristics as age and race are not inherently changeable, SDoH may be modifiable by multi-level social, behavioral and environmental interventions. The primary purpose of this project is to identify the modifiable individual, social and environmental factors associated with stress and to investigate and quantify the effect of persistent stress on chronic disease in a marginalized, primarily minority, urban community.
While rectification of the systemic underlying social and environmental factors deeply embedded in many minority communities will take substantial effort, financial cost, infrastructure improvements and cultural transitions, strategies to reduce and manage stress among the most at-risk populations have a more immediate potential to reduce the current chasm of health disparities.
2 Methods
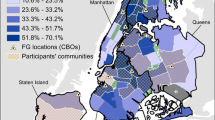
This study leveraged data collected as part of Temple Health: Block-By-Block (THB3), a longitudinal community-based cohort study conducted in 11 zip codes of North Philadelphia with the goal of engaging local residents in community health improvement across the life cycle through research. The patchwork of neighborhoods in North Philadelphia includes a highly diverse population of approximately ½ million residents, two-thirds of whom self-identify as Black or Hispanic. As one of America’s most impoverished, underserved urban neighborhoods, North Philadelphia residents struggle with higher rates of chronic diseases and mortality. Using a door-to-door recruitment strategy from 2015–2019, THB3 accrued more than 1900 subjects and collected a comprehensive scope of descriptive health data via in-home visits every six months from consented community residents [21]. THB3 was approved by Temple University, Research Integrity and Compliance Institutional Review Board which requires careful adherence to the Declaration of Helsinki requirements for human subject research [22]. All subjects completed the informed consent process.
This project and the related data interpretation were guided by a social ecological approach, addressing individual health as a complex entity influenced by a multi-level hierarchy of individual, social, environmental, and societal factors [23]. Additionally, Cohen’s model of the stress process formed the foundation for integrating environmental, psychological and biologic factors into the effects of stress on health [24].
Eligible subjects for this study were 18 years of age or older, able to speak either English or Spanish, and had no cognitive disorders that may interfere with the integrity of the informed consent process. Each had completed a Visit 5 Social & Environmental Stress Assessment no later than 2019 to exclude confounding by the Covid-19 pandemic. Visit 5 occurs early in the 3rd year of THB3 participation, thus at that point in this longitudinal study, participants typically had a well-established relationship with the field specialist who consistently visited them twice each year.
As available and aligned with THB3 objectives, each of the eleven structured THB3 visit assessments was developed to include either previously validated survey instruments and/or adapted survey items from previously published projects. For content areas in which appropriate instruments were not available, new survey items were developed in collaboration with project faculty, staff and external content experts. A consensus approach was used to ensure agreement on the key constructs of interest while meeting appropriate readability levels for participants. The surveys were pre-tested by study team members. All study materials were translated by a certified Spanish translator for administration to Spanish-speaking subjects. Revisions and staff retraining protocols were in place to assure quality and consistency in survey administration.
The Visit 5 Social & Environmental Assessment measured individual, social, neighborhood, and environmental factors as reported through each participant’s perspectives. More specifically, this survey examined individual overall health and employment, social support (close friends, church attendance, club memberships), food insecurity (available food, food purchasing and cost issues, fresh food availability), neighborhood satisfaction and safety (neighborhood appearance, recreational space, property values, safety and crime), and environmental factors in and outside the home (housing conditions, rodents, utilities, public transportation). A key component of this assessment was the measurement of respondent-reported feelings of stress using the 10-item Perceived Stress Scale. The Perceived Stress Scale (PSS), a classic stress assessment instrument, originally developed in 1983 by Cohen and colleagues, was designed to identify and quantify the level at which a respondent perceives their daily life to be unpredictable, uncontrollable and overloaded during the past month. The quantitative score ranges from 0 to 40 with higher scores representing greater perceived stress; a score above 13 is interpreted as ‘moderate’ stress (14–26) and scores between 27–40 represent ‘severe’ stress. This scale has an internal validation of α = 0.78 [25].
Since stress was the focus of this study, an internal validation step was planned based on inclusion in the Visit 5 Assessment of a single-item measure of stress symptoms developed as part of the Nordic Questionnaire for Psychological and Social Factors [26]. The question asks about frequency of feeling stressed (five levels from ‘not at all’ to ‘very much’), defined as situations in which one feels tense, restless, nervous, anxious or unable to sleep. Item responses were to be compared to the PSS score. Diagnoses of fourteen specific chronic diseases were self-reported by the study participants based on “having been told by a physician that they had this condition’. These disease prevalence data were updated at every scheduled six-month home visit. Chronic disease data collected at Visit 5 were used for this specific study. Reported health conditions were summed for each subject to create a Cumulative Chronic Disease Index (CCDI).
Statistical considerations: Sample size determination was based on Cohen’s D for the intermediate outcome of perceived stress score [27]. Based on an expected moderate effect (Cohen’s D = 0.5) of SDoH variables, a group sample size of 100 per group would provide greater than 87% power to reject the null hypothesis of equal means between PSS scores. The THB3 cohort accrual was determined to be adequate to meet this requirement. This study utilized standard descriptive measures, including both parametric and non-parametric techniques as appropriate [28]. For both discrete (PSS scores) and ordinal (CCDI) dependent variables, the Kruskal Wallis non-parametric test was employed to compare differences by baseline characteristics and SDoH variable responses based on a p-value of < 0.10 to identify differences of potential interest. Given the sample size and the normality of PSS scores, stepwise multivariable linear regression modelling was used to then identify the baseline factors that were independently associated with stress; conclusions were the same with both a forward and backward stepwise approaches. These independent covariates were then included in a final ordinal logistic regression model to examine the relationship between stress and chronic disease as measured by PSS scores and the CCDI. Two-sided p-vales of less than 0.05 were considered statistically significant with no adjustment made for multiple testing. Analysis was performed using SAS™ version 9.4 software [29].
3 Results
There were 358 subjects who met the eligibility criteria and had complete data available at the time of analysis. The characteristics of the study participants are detailed in Table 1. Almost two-thirds of respondents were female; the majority (90%) of the respondents identified as Black or Hispanic. The average age was 52 years and ranged from 18 to 86 years. While most participants spoke English, 24% preferred to speak Spanish. Almost one-quarter of the sample had not graduated high school, and the majority (67%) did not work outside the home. Compared to the overall North Philadelphia population, the study sample includes a greater proportion of Black residents who are slightly older, more likely to have some education beyond high school, but are less likely to be employed.
The mean PSS score among participants was 13.1 ± 8.4, almost identical to the published national norms [30]. For the purpose of validation (Table 2), there was a highly significant (p < 0.0001) association between mean PSS scores and the categorical levels of self-reported stress in the one-item frequency measurement. PSS scores monotonically increased from a low of 7.7 ± 5.9 among those reporting no feelings of stress to a mean PSS of 24.1 ± 7.9 among those reporting feeling very stressed. This strong association provides additional evidence of the PSS instrument as a valid quantitative indicator of perceived stress in this study sample.
An examination of PSS scores by racial/ethnic group demonstrates statistically significant differences in scores with the highest PSS scores being among Hispanics (16.0 ± 8.4) compared to mean scores of 13.5 and 12.2 in NH Blacks and NH whites, respectively (p = 0.0071). Of the 32 individual, family, social, neighborhood and environmental variables tested in univariate analyses, 16 factors were associated with PSS scores (p < 0.10). These included individual (self-reported) characteristics (overall health, employment); family/social factors (close friends, difficulty paying for basics such as food, housing, medical care, heating; adequate food in house; access to nutritious foods; interruptions in home heating; roaches in home; access to washer/dryer; and home ownership) and environmental conditions (building conditions, public transportation access, neighborhood appearance and safety, and overall neighborhood satisfaction and quality).
These sixteen modifiable factors were entered into a multivariable stepwise linear regression model; five of the sixteen factors were identified as statistically significant, independent predictors of PSS scores (Table 3). These factors included: general health, employment status, difficulty in paying for basics, home ownership and overall neighborhood quality. For each of these factors, the mean stress scores are shown for study participants whose responses reflected greater advantage, that is better health, employed, less difficulty paying for basics, home ownership, and good neighborhood quality, compared to those in less beneficial situations. Scores show that for each of the five independent factors a response reflecting a disadvantaged situation was associated with an increase from low to moderate stress as indicated by PSS scores. Of greater note, this model indicates that the PSS score among those persons reporting consistently favorable responses on all five factors was low (PSS = 8), whereas PSS scores increased to 26, bordering on severe stress, among those providing ‘disadvantaged’ responses on all five of the factors.
The chronic conditions included in the CCDI and the prevalence of each in the study sample are provided in Table 4. The high rates of asthma, diabetes, hypertension, mental health problems and Class II obesity, defined as BMI > 35, far exceed national averages [31]. The median CCDI for this community-based sample was 2 with a range of 0 to 9. In a univariate analysis (Table 5), mean PSS scores were statistically significantly associated with CCDI grouped into four ordinal categories (p < 0.01). Among those in the lowest category of CCDI the mean PSS score was 11.5, however, this escalated to 19.0 among subjects reporting 7 or more chronic conditions.
Using an ordinal logistic regression model with PSS score (continuous measure) as the primary independent variable, the original five modifiable factors associated with stress as covariates, and CCDI defined by 4 ordinal categories as the dependent variable, the association between PSS and CCDI was highly significant (p = 0.017) (refer to Fig. 1). These data indicate that even with adjustment for SDoH, stress as measured by the PSS score, remains a significant independent factor in the causal pathway to chronic disease.
Five modifiable multi-level factors reflecting social determinants of health were significantly associated with perceived stress. In a multivariable logistic regression adjusted for these variables, increased stress score was independently associated with the Cumulative Chronic Disease Index, suggesting a two-tiered opportunity to intervene in biologic sequelae that lead to disease. Multi-modality strategies to reduce stress may yield short-term, individualized effects on chronic disease burden; more protracted societal efforts to address highly needed improvements in the social determinants of health should eventually have a greater, universal impact
4 Discussion
The social determinants of health, while previously ignored or merely considered as ancillary impediments to disease management, are now recognized as fundamental drivers of health affliction, surpassing biologic or genetic characteristics in shaping population health. Stress has many biologic repercussions that are associated with development of chronic disease [9, 10], thus it is important to explore the intricate relationship between SDoH, stress and chronic disease.
This study sample depicts the complex, socioeconomic underpinnings that are the landscape of daily living in an under-resourced, densely populated, urban community. This study provides evidence suggesting that these adverse circumstances, under the umbrella of the SDoH, are associated with significantly higher levels of perceived stress among neighborhood residents. In the future, more evidence needs to be generated to confirm the relationship between perceived stress, as measured by such self-reported instruments as the PSS score used in this investigation, and detrimental biologic markers of stress. The prevalence of chronic disease is demonstrated to be high in this study sample, indicating the need for community health improvement in such marginalized urban areas is vast. These data support previous investigations that showed perceived stress to be associated with increased chronic disease [19, 20]. In fact, this study confirms that self-reported perception of stress adjusted for the five identified SDoH measures is significantly associated with cumulative chronic disease. While biologic pathways including inflammation and immune response have been shown to be affected by stress and lead to disease [9, 10], the opportunities to intervene at the individual level in the deleterious effects of stress are numerous including both behavioral and pharmacologic.
In striving for the ultimate goal of health equity through social equality, we must examine the etiologic pathway from disparities to disease and intervene using direct approaches that will yield the most immediate improvement in individual and community health. The SDoH are solidly integrated into many aspects of today’s society. Over the past decade, efforts have been directed to better document and correct the most deleterious SDoH. The Institute of Medicine has recommended social and behavioral health domains be captured in the electronic health record although admittedly costs, required training and privacy barriers remain hurdles in this effort [32]. While modifiable, the reality is that centuries of social evolution have created and magnified these health threats. Correcting them will require extensive time, funding, culture change and even neighborhood re-designs. Addressing management of stress through behavioral interventions that lead to either decreased perceived stress or increased resiliency may be a short-term effective step to reducing chronic disease. Additionally, pharmacologic therapies that decrease inflammation and enhance immune response are currently available and could be leveraged for the most at-risk individuals.
A unique strength of this study is the data capture directly from the community residents in real time, providing personal assessments and perspectives regarding the individual, family, social, and neighborhood factors that are part of their daily existence. The limitations of this study are also important to acknowledge. All data are self-reported by participants, the accuracy of some information, particularly that of the prevalence of chronic conditions, was not verified in medical, financial or legal records. While interactions between each participant and their field specialist were typically well-established and comfortable, this relationship may have led to more desirable subject responses. The effect of this potential response bias on study conclusions cannot be determined or measured. While suggestive, this study does not provide evidence regarding the temporal relationship between stress and chronic disease. It does, however, provide compelling, quantitative evidence that factors highly common in diverse, low socioeconomic urban areas increase individual perceptions of stress and, as suggested by others [9, 10], stress may lead to chronic disease.
In conclusion, our study does confirm the impact of SDoH on levels of perceived stress among community residents, and suggests that stress is a critical independent factor in the path to chronic disease. Actionable community interventions targeting the individual, social and environmental factors identified in this study may reduce stress. Further research to delineate the biologic repercussions of stress in the onset of chronic disease may provide additional pharmacologic and behavioral opportunities for primary prevention and reduction of chronic disease in diverse urban communities.
Data Availability
Based on the very sensitive nature of some of the data used to support this study, these data have not been made publicly available. The corresponding author and principal investigator of this study agrees to make necessary data available upon request from interested researchers.
References
Heckler MM, U.S. Department of Health and Human Services Task Force on Black and Minority Health. Report of the secretary’s task force on black and minority health volume 1: executive summary. Washington DC: U.S. Department of Health and Human Services; 1985.
LaVeist TA, Perez-Stable EJ, Richard P, Anderson A, Isaac LA, Santiago R, Okoh C, Breen N, Farhat T, Assenov A, Gaskin DJ. The economic burden of racial, ethnic, and educational health inequities in the US. J Am Med Assoc. 2023. https://doi.org/10.1001/jama.2023.5965.
Singh GK, Lee H. Marked disparities in life expectancy by education, poverty level, occupation, and housing tenure in the United States, 1997–2014. Int J Matern Child Health AIDS. 2021. https://doi.org/10.21106/ijma.402.
Bethea TN, Palmer JR, Rosenberg L, Cozier YC. Neighborhood socioeconomic status in relation to all-cause, cancer, and cardiovascular mortality in the black women’s health study. Ethn Dis. 2016. https://doi.org/10.18865/ed.26.2.157.
World Health Organization. Closing the gap in a generation: health equity through action on the social determinants of health-final report -Final report of the commission on social determinants of health. https://www.who.int/publications/i/item/WHO-IER-CSDH-08.1. Accessed 2 Jul 2024.
Faris REL, Dunham HW. Mental disorders in urban areas: an ecological study of schizophrenia and other psychoses. Chicago, I: University of Chicago Press; 1939.
Brondolo E, Byer K, Gianaros P, Liu C, Prather A, Thomas K, Woods-Giscombe CL. Stress and health disparities: contexts, mechanisms, and interventions among racial/ethnic minority and low socioeconomic status populations. American Psychological Association. 2017. https://www.apa.org/pi/health-equity/resources/stress-report. Accessed 1 Jul 2024.
Lazarus RS. Psychological stress and the coping process. New York: McGraw-Hill; 1966.
Albert MA, Durazo EM, Slopen N, Zaslavsky AM, Buring JE, Silva T, Chasman D, Williams DR. Cumulative psychological stress and cardiovascular disease risk in middle aged and older women: rationale, design, and baseline characteristics. Am Heart J. 2017. https://doi.org/10.1016/j.ahj.2017.06.012.
Jackson JS, Knight KM, Rafferty JA. Race and unhealthy behaviors: chronic stress, the HPA axis, and physical and mental health disparities over the life course. Am J Public Health. 2010. https://doi.org/10.2105/AJPH.2008.143446.
Plascak JJ, Hohl B, Barrington WE, Beresford SAA. Perceived neighborhood disorder, racial-ethnic discrimination and leading risk factors for chronic disease among women: California behavioral risk factor surveillance system, 2013. SSM Popul Health. 2018. https://doi.org/10.1016/j.ssmph.2018.07.001.
Riahi SM, Yousefi A, Saeedi F, Martin SS. Associations of emotional social support, depressive symptoms, chronic stress, and anxiety with hard cardiovascular disease events in the United States: the multi-ethnic study of atherosclerosis (MESA). BMC Cardiovasc Disord. 2023. https://doi.org/10.1186/s12872-023-03195-x.
Vancampfort D, Koyanagi A, Ward PB, Veronese N, Carvalho AF, Solmi M, Mugisha J, Rosenbaum S, De Hert M, Stubbs B. Perceived Stress and its relationship with chronic medical conditions and multimorbidity among 229, 293 community-dwelling adults in 44 low- and middle-income countries. Am J Epidemiol. 2017. https://doi.org/10.1093/aje/kwx159.
Andersen SW, Blot WJ, Shu X, Sonderman JS, Steinwandel M, Hargreaves MK, Zheng W. Associations between neighborhood environment, health behaviors, and mortality. Am J Prev Med. 2018. https://doi.org/10.1016/j.amepre.2017.09.002.
Matheson FI, Moineddin R, Dunn JR, Creatore MI, Gozdyra P, Glazier RH. Urban neighborhoods, chronic stress, gender and depression. Soc Sci Med. 2006. https://doi.org/10.1016/j.socscimed.2006.07.001.
Cockerham WC, Hamby BW, Oates GR. The social determinants of chronic disease. Am J Prevent Med. 2017. https://doi.org/10.1016/j.amepre.2016.09.010.
Institute of Medicine. Unequal treatment: confronting racial and ethnic disparities in health care. National Academies of Science; 2003.
Cohen S, Janicki-Deverts D, Miller GE. Psychological stress and disease. J Am Med Assoc. 2007. https://doi.org/10.1001/jama.298.14.1685.
Ross CE, Mirowsky J. Neighborhood disadvantage, disorder, and health. J Health Soc Behav. 2001. https://doi.org/10.2307/3090214.
Wheaton B. The nature of stressors. In: A handbook for the study of mental health: social contexts, theories, and systems. New York, NY: Cambridge University Press; 1999. pp. 176–197.
Fisher SG, Devlin A. Development of an urban community-based cohort to promote health disparities research. Int J Public Health. 2019. https://doi.org/10.1007/s00038-019-01267-4.
World Medica Association, WMA Declaration of Helsinki—Ethical Principles for Medical Research Involving Human Subjects, 2013. https://www.wma.net/policies-post/wma-declaration-of-helsinki-ethical-principles-for-medical-research-involving-human-subjects/.
Kaplan GA, Everson SA, Lynch JW. The contribution of social and behavioral research to an understanding of the distribution of disease: a multilevel approach. In: Smedley BD, Syme SL, editors. Promoting health: intervention strategies from social and behavioral research. Washington DC: National Academies Press; 2000. p. 31–55.
Cohen S, Gianaros PJ, Manuck SB. A stage model of stress and disease. Assoc Psychol Sci. 2016. https://doi.org/10.1177/1745691616646305.
Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Sci Soc Behav. 1983. https://doi.org/10.2307/2136404.
Elo A-L, Leppanen A, Jahkola A. Validity of a single-item measure of stress symptoms. Scand J Work Environ Health. 2003. https://doi.org/10.5271/sjweh.752.
Cohen J. Statistical power analysis for the behavioral sciences. New York, NY: Routledge Academic; 1988.
Daniel WW. Biostatistics: a foundation for analysis in the health sciences. 6th ed. New York, NY: John Wiley & Sons; 1995.
SAS version 9.4. Cary, NC: SAS Institute Inc.; 2013.
Cohen S, Williamson GM. Perceived stress in a probability sample of the United States. In: Spacapan S, Oakamp, editors. The social psychology of health. Newbury Park, CA: Sage; 1988.
Centers for Disease Control and Prevention. Chronic Diseases in America. https://www.cdc.gov/chronic-disease/data-surveillance/index.html.
Institute of Medicine. Capturing social and behavioral domains and measures in electronic health records: Phase 2. Washington DC: National Academies Press; 2015.
Funding
This study was partially funded through a grant from The Commonwealth of Pennsylvania, Department of Health: SAP#4100068727 (2015–2018) and the generous support of the Temple University President’s Strategic Initiative.
Author information
Authors and Affiliations
Contributions
All authors contributed to the conceptualization and design or data acquisition, analysis and interpretation. Conceptualization and design were completed by S.F. and F.R.; Data Acquisition was the responsibility of N.V.; Data analysis and Interpretation was directed and completed by S.F. and F.R; All authors including S.F., N.V. and F.R. actively contributed to manuscript writing & review.
Corresponding author
Ethics declarations
Ethics approval
This study was approved by Temple University, Research Integrity and Compliance Institutional Review Board. All subjects completed the informed consent process.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Fisher, S.G., Volquez-Young, N. & Ramsey, F. Influence of socio-environmental factors on stress and chronic disease in an urban population. Discov Public Health 21, 30 (2024). https://doi.org/10.1186/s12982-024-00158-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12982-024-00158-1