Abstract
Background
Young men who have sex with men (MSM), are a key population at higher risk of HIV infection yet they are underrepresented in research. We conducted a bio-behavioral survey to estimate HIV prevalence and associated risk factors among tertiary student MSM (TSMSM) in Nairobi, Kenya.
Methods
Between February and March 2021, 248 TSMSM aged ≥ 18 years who reported sex with another man in the past year participated in a respondent-driven sampling (RDS) based cross-sectional survey. Participants completed an electronically self-administered behavioral survey and provided a blood sample for HIV antibody testing, alongside urine, anorectal and oropharyngeal swabs for pooled testing of sexually transmitted infections using a multiplex nucleic acid amplification test. RDS-Analyst v.0.72 and Stata v.15 software were used for data analysis. Differences in proportions were examined using chi-square (χ2) test, and unweighted multivariate logistic regression was used to assess factors associated with HIV infection.
Results
HIV prevalence among study participants was 8.3%, whereas the weighted prevalence was 3.6% (95% CI: 1.3–6.0%). Median ages of participants, and at self-reported first anal sex with a man were 21(interquartile range [IQR] 20-22) and 18 (IQR 17-19) years, respectively. A majority (89.3%) of TSMSM owned a smart phone, 46.5% had ever used a geosocial networking app for MSM such as Grindr ® to find a sex partner, and a third (33.6%) met their last sex partner online. Almost three-quarters (71.3%) had > 1 male sex partner in the year before the survey. A third (34.3%) did not use condoms with their last sex partner, 21.2% received money from their last sex partner and 40.9% had taken alcohol/another drug during their last sexual encounter. HIV infection was associated with studying in private institutions (adjusted odds ratio[AOR] = 6.0; 95% confidence intervals [CI] : 1.2–30.0, p = 0.027), preferring a sex partner of any age—younger, same or older (AOR = 5.2; 95 CI: 1.1–25.2, p = 0.041), last sex partner being > 25 years (AOR = 6.4; 95% CI: 1.2–34.6, p = 0.030), meeting the last sex partner online (AOR = 4.2; 95% CI; 1.1–17.0, p = 0.043) and testing positive for Neisseria gonorrhea (AOR = 7.8; 95% CI: 2.0–29.9, p = 0.003).
Conclusions
HIV prevalence among TSMSM in Nairobi is alarmingly high, demonstrating a need for tailored prevention and control interventions for this young key population.
Similar content being viewed by others
Introduction
The incidence of human immunodeficiency virus (HIV) has continued to fall globally [1]. Kenya has made laudable progress in the HIV response as shown by the sustained decline in HIV prevalence among adults (15–49 years) in the general population, from a high of ~ 10% in the mid-1990s to 4.5% in 2020 [2]. Whilst overall incidence has been declining, key populations such as men who have sex with men (MSM) still bear a disproportionate burden of the disease. Globally, despite MSM consisting only 1–3% of the adult male population, almost a quarter (23%) of all new HIV infections in 2020 were among MSM, with MSM having 25-fold greater odds of acquiring HIV than men in the general population [3]. In sub-Saharan Africa, the overall HIV prevalence is approximately 5 times higher among MSM than among men in the general population [4]. In Nairobi—Kenya’s capital, the prevalence of HIV among MSM is 25% [5] compared to 3.1% in the general male population (15–49 years old) [6], with 15.2% of all new HIV infections in the country occurring among MSM [7].
Kenya has a dedicated national program that leads the HIV response among key populations in the country [8]. Despite tremendous progress made in scaling up HIV prevention strategies among key populations, the program still grapples with challenges such as lack of updated bio-behavioral survey data and gaps in reaching adolescent and young key populations [9], including tertiary student MSM (TSMSM). In countries such as China where data is available, HIV prevalence among TSMSM is 4.1%, and despite TSMSM constituting only an estimated 8.5% of the total tertiary student population, they account for over 80% of all HIV infections in the tertiary institutions [10]. In South Africa, TSMSM comprise 6% of male tertiary students and have a HIV prevalence of 4.1%, which is greater than twice that of the general male tertiary student population—1.7% [11].
TSMSM like other young MSM (YMSM) may be involved in practices that heighten their risk of acquiring HIV. Upon joining tertiary institutions, they interact with peers who have similar same-sex behavior, experience more freedom from parental supervision, and have increased opportunities for socialization [12]. As a result, studies have shown that TSMSM seek casual sex partners online, have sex more often, and engage in condomless sex, group sex and sex work [10]. Additionally, TSMSM have been shown to have early sexual debuts, forced sex experiences, high sex partner turnover, concurrent sex partners, inconsistent condom use, and alcohol and drug use [13]. Taken together, these behaviors increase the risk of HIV infection for TSMSM. In many African countries, including Kenya, these behavioral risks are further amplified by structural factors such as criminalization of same-sex behavior [14], as well as societal stigma and discrimination towards individuals with same sex behavior [15].
Given the potential risk of HIV infection faced by TSMSM, it is important to understand what the HIV prevalence and associated risk factors are for this population. This information would be useful to stakeholders, including: policy makers, service providers, advocacy groups and TSMSM themselves, in informing tailored prevention and control responses for this population, and thereby contribute towards the ambitious goal of ending AIDS as a public health threat by 2030[16]. This study therefore estimated HIV prevalence and associated factors among TSMSM in Nairobi, Kenya.
Methods
Study methods are detailed in the published study protocol [17], and summarized below:
Study design and setting
This was a cross-sectional survey conducted between February and March 2021, just after COVID-19 restrictions were eased in Kenya and tertiary institutions allowed to re-open for in-person learning. Nairobi, the capital city of Kenya, was selected as the study area because of its large population of tertiary students spread across approximately 150 campuses of various universities and colleges [18], including University of Nairobi which is the largest university in the country [19].
Study population
TSMSM were eligible to participate in the survey if they were: aged ≥ 18 years, provided proof of being a registered student in a university or college in Nairobi; were assigned male gender at birth, reported having had consensual receptive or insertive oral or anal sexual intercourse with another man in the last 12 months and provided written informed consent to participate in the study.
Sample size calculation
The sample size for the survey was calculated to estimate the prevalence of HIV among TSMSM, based on World Health Organization’s (WHO) 2017 bio-behavioral survey guidelines for populations at higher risk of HIV infection [20]. A minimum sample size of 200 TSMSM was planned using the Cochran formula [21], with a design effect of 3 to account for clustering, estimated HIV prevalence of 4.1% based on a previous study among TSMSM in South Africa [11], a level of precision of 0.05 and 10% non-response.
Sampling and recruitment process
Respondent-driven sampling (RDS) was used following findings from formative research that demonstrated the appropriateness and acceptability of the method for recruiting TSMSM into the survey [22]. In summary, RDS is a chain referral sampling method that integrates a mathematical model that weights the sample to compensate for the non-random sampling and minimizes old-style snowballing bias [23]. Six seeds were selected from the TSMSM who took part in the formative research. So as to reach varying networks of TSMSM, various characteristics were taken into consideration when selecting seeds, including: age, residence, sexual orientation identity, and preferred sexual role. Each seed and subsequent participants were issued with 3 coupons until the survey had recruited 120 participants (inclusive of seeds), then 2 coupons until the 150th participant, after which no more coupons were issued. Each participant was reimbursed 1000 Kenyan shillings (equivalent to US$ 10) for their time and expenses related to transport to and from the study site, and 300 Kenyan shillings (equivalent to US$ 3) for every peer they recruited into the study.
Data collection tools and procedures
The behavioral survey was conducted by self- administered interview on tablets using a questionnaire set up on REDCap® software (Vanderbilt University). The questionnaire was adapted for this study from a validated questionnaire available from the integrated HIV bio-behavioral surveillance toolbox [24]. The questionnaire contained questions on sociodemographic characteristics and sexual behavior, and was administered in English, the language of instruction in Kenyan tertiary institutions. The survey was conducted at a discreet study site located within the Nairobi central business district. The recruitment coupons had a map showing where the study site was located, and a telephone number which prospective participants could call for directions if they needed to.
Biological specimen collection and testing
After completing the behavioral survey, participants were offered HIV testing based on the Kenyan national testing algorithm [25]. The testing algorithm is serial and recommends use of a screening test, followed by a confirmatory test if the screening test is positive. In cases where results of the confirmatory test disagree with those of the screening test, clients are referred to a laboratory where their samples are tested using an assay which is distinct from both the screening and confirmatory tests. Capillary blood from a finger prick was drawn by a trained HIV testing counselor. All samples were tested using the Determine® rapid test kit. Non-reactive tests were considered negative for HIV. Samples from those with reactive tests were subsequently tested with HIV-1/2 First Response® kit for confirmation of HIV seropositive status, except for participants who self-reported HIV seropositive status. There were no discordant results. Participants were offered pre and post HIV testing counselling. Participants who tested positive for HIV and were not on treatment were referred to facilities of their choice for HIV care and treatment. Participants who tested negative for HIV and were at high risk for HIV infection were referred for PrEP if not already initiated. Participants also provided urine, anorectal and oropharyngeal swabs for pooled Chlamydia trachomatis (CT), Mycoplasma genitalium (MG), Neisseria gonorrhea (NG) and Trichomonas vaginalis (TV) testing using a multiplex nucleic acid amplification test (Sacace Biotechnologies®, Italy). HIV testing was done at the study site whereas testing for the other sexually transmitted infections (STIs) was done in a licensed and accredited commercial laboratory within the Nairobi metropolis. All participants were offered condoms and water-based lubricants.
Ethical considerations
The study was approved by University of the Witwatersrand Human Research Ethics Committee-Medical and University of Nairobi-Kenyatta National Hospital Ethics and Research Committee. All participants provided written informed consent. The following measures were taken to protect study participants: no identifying information was written on study documents nor laboratory specimens associated with a participant; all paper-based study materials were stored in locked file cabinets, in locked offices and access granted to only authorized study staff; electronic data was stored in a password-protected computer accessible only to authorized study staff; and same-sex sexual behavior was not reported to the authorities. All staff working with participants were trained on the importance of maintaining confidentiality, and signed confidentiality agreements prior to involvement in the study. The study also received a letter of support from the Kenyan Ministry of Health through the National AIDS and STI Control Program (NASCOP).
Data analysis
Data analysis excluded 6 seeds who were purposely selected to begin the RDS recruitment. The weighted HIV prevalence rate with 95% confidence intervals (CI) was calculated using RDS Analyst (RDS-A) software version 0.72 [26], where Gile’s successive sampler (SS) estimator was used for weighting. Gile’s SS estimator takes into consideration the self-reported network sizes of participants, recruitment patterns and estimated size of the study population [27]. As per recommendation [28], an estimated population size of 8406 for TSMSM (1.45% of male tertiary students in the Nairobi metropolis) was used, with 0.95 CI and 1000 bootstraps.
Stata version 15 (College Station, TX: StataCorp LLC) was used for further analysis of the unweighted data. Some continuous variables such as age and self-reported number of sex partners were converted into binary categories. Categorical variables were summarized using proportions, and differences in proportions examined using chi-square (χ2) test. Bivariate analysis and multivariate logistic regression models were used to measure associations between various factors and HIV infection. All exposure variables with a p ≤ 0.2 in bivariate analysis were included in the final multivariate model. Other variables with p > 0.2 but considered to be confounders were included in the multivariate model. Unweighted regression models were used since they have been shown to perform better than weighted regression models for RDS data [29].
Results
Sociodemographic characteristics of TSMSM
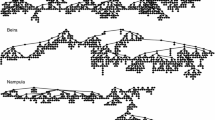
A total of 248 TSMSM were recruited including 6 seeds. The final sample had a minimum of one and maximum of eight recruitment waves, as depicted by the recruitment networks in Fig. 1. The median age of participants was 21 years (IQR 20–22), with 96.3% ≤ 24 years, and the oldest being 30 years old (Table 1). A majority (58.3%) were university students, almost three-quarters (71.9%) were in public institutions and four-fifths (79.3%) resided in college or rented hostels outside their campuses. A majority (89.3%) owned a smart phone at the time of the study.
Recruitment was initiated by six seeds who were issued with 418 coupons, 244 coupons were returned and out of these, 242 met the eligibility criteria for study participation and were subsequently enrolled into the study. The waves of recruitment per seed ranged from 1 to 8. Diamonds and circles indicate seed and non-seed participants, respectively.
Sexual behavior characteristics of TSMSM
The median age at reported anal sexual debut with a man was 18 years (IQR 17–19) and most of the sexual debuts (83.4%) were consensual, as shown in Table 1. Almost three-quarters (71.3%) had more than one sex partner, with 16.2% having participated in group sex within the last year. Approximately half (46.5%) had ever used a geosocial networking app for MSM such as Grindr ® to find a sex partner, with one-third (33.6%) having met their last sex partner online. Approximately two-thirds (65.7%) and more than three-quarters (78.1%) had used condoms and lubricants, respectively, with their last sex partner. One-fifth (21.2%) received money from their last sex partner and less than half (40.9%) had taken alcohol or another drug during their last sexual encounter.
HIV prevalence, differences in proportions, and associated factors
The HIV prevalence among the study participants was 8.3%. The weighted HIV prevalence for the study population (TSMSM in Nairobi) was 3.6% (95% CI: 1.3%—6.0%). Three-quarters (77.3%) of those who tested positive for HIV knew of their HIV serostatus prior to testing in the study and all of these participants reported being on antiretroviral therapy. As illustrated in Table 1, HIV prevalence was significantly higher among TSMSM studying in private institutions (16.2% vs 5.2%, p = 0.005), residing at home with their families (16.0% vs 6.2%, p = 0.026), who preferred older sex partners (22.2% vs 4.8%, p = 0.001), whose last sex partner was > 25 years old (24.3% vs 5.4%, p < 0.001), who had more than one sex partner in the last year (11.0% vs 1.4%, p = 0.015), who had ever used a geosocial networking app for MSM (15.2% vs 2.3%, p < 0.001), who met their last sex partner online (16.0% vs 4.4%, p = 0.002) and those who tested positive for MG (20.0% vs 6.9%, p = 0.024) and NG (22.2% vs 5.8%, p = 0.001).
The results of bivariate and multivariate logistic regression are presented in Table 2. In multivariate analysis, independent risk factors for HIV infection were: studying in private institutions (Adjusted Odds Ratio [AOR] = 6.0; 95% CI: 1.2–29.9, p = 0.027), preferring a sex partner of any age (AOR = 5.1, 95% CI: 1.1–25.2, p = 0.041), having a last sex partner > 25 years old (AOR = 6.4; 95% CI: 1.2–34.6, p = 0.030), meeting the last sex partner online (AOR = 4.2; 95% CI; 1.1–17.0, p = 0.043) and testing positive for NG (AOR = 7.8, 95% CI: 2.0–29.9, p = 0.003).
Discussion
Our study found an estimated HIV prevalence of 8.3% among study participants and a RDS-weighted HIV prevalence of 3.6% (95% CI: 1.3–6.0%) among TSMSM in Nairobi. The weighted HIV prevalence observed among TSMSM in our study (96% aged 18–24 years) was six times higher than that of young Kenyan men in the general population aged 18–24 years, which is 0.6%[6]. Accordingly, the recent call to have programming that caters for the HIV prevention needs of YMSM in Africa [30], is quite relevant for TSMSM in Nairobi. The weighted HIV prevalence observed is comparable to the 4.1% HIV prevalence found among TSMSM in both China [10] and South Africa [11]. Notably, with only 77.3% of study participants knowing their HIV status to be seropositive before the study, there is need to scale up HIV testing in this population so as to reach the first 95 of the UNAIDS fast-track 95-95-95 [31]. HIV self-testing is readily available and acceptable in Kenya [32], and should thus be harnessed to increase testing rates in this key population.
Higher HIV prevalence was observed among TSMSM studying in private institutions and staying at home with their families. We hypothesize that most TSMSM who study in private institutions and stay with their families have predominantly lived most of their lives in the city, which is more liberal than the rural areas of the country. Therefore, it is likely that these TSMSM could have started experimenting with anal sex at an earlier age than their rural counterparts who due to costs, mostly tend to join the public institutions and stay either in campus or rented accommodation outside their campuses. For these reasons, there could be an increased exposure period for the former, leading to the elevated risk of HIV infection. Indeed, even higher HIV prevalence (30.3%) than we found, has been observed among YMSM in urban Indonesia [33], a country where it is not illegal to be homosexual.
Meeting sex partners online was significantly associated with HIV infection. This finding is consistent with that of a previous study in Kenya which showed that MSM who sought sex partners online had four-fold greater odds of having HIV infection compared to those who sought sex partners from physical sites [34]. Additional research in sub-Saharan Africa has demonstrated that MSM who seek sex partners online have higher prevalent HIV infection and are more likely to be younger [35], like our study participants. Young MSM, including TSMSM who use the internet to find sex partners are a critical population to target for HIV interventions, since they are inclined to have increased levels of sexual risk behavior, and the internet itself may be a promising mechanism to deliver interventions [36]. Like in our study where 89.6% owned a smart phone, another study showed that 95.6% of tertiary students in Kenya own smart phones [37], and use the phones to access the internet. Future YMSM-focused risk reduction interventions should leverage the internet to host campaigns and safe sex messaging efforts to directly and discretely reach TSMSM who predominantly seek sex partners online. This is necessary since TSMSM—as a result of criminalization of homosexuality, societal stigma and discrimination, may be afraid to seek services from programs that largely depend on physical outreach, thus resulting in missed opportunities for HIV prevention.
Another significant risk factor identified for HIV infection was having reported the last sex partner being > 25 years. This is consistent with the findings of a study in the USA which showed that among YMSM, the odds of HIV infection were significantly elevated as the age of sexual partners increased [38]. This could be explained by the fact that risk of HIV infection generally increases with age, thus increasing the risk of HIV infection among YMSM who have sex with older male partners. In addition, practices that increase the risk of HIV infection such as condomless anal sex have been shown to be common in age-disparate sexual relationships among MSM, and are significantly associated with unrecognized HIV infection [39]. Previous research has shown that YMSM are motivated to seek older MSM partners for economic and social support [40]. Subsequently, the economic power imbalance between YMSM and older MSM may diminish the former’s ability to negotiate for safer sex [41], with YMSM previously reporting sexual coercion by older MSM [42]. Since the YMSM—older MSM partnerships are more likely to persist than wane, HIV prevention programs for YMSM should include information about the HIV risk associated with older MSM partners and skills for negotiating for safer sex, particularly the correct and consistent use of condoms. Additionally, TSMSM should be provided with more tools for HIV prevention, including oral pre-exposure prophylaxis (PrEP) which is available in Kenya [43], and offers YMSM more control on usage as compared to condoms which need negotiation between sex partners. As well, since YMSM may choose more pleasurable (condomless sex) over safer sex, PrEP would offer them the opportunity to enjoy sex without fear of HIV infection, the risk of acquiring other STIs notwithstanding [44].
A notable independent risk factor for HIV infection that was observed in our study was testing positive for NG. This coupled with the high prevalence of CT observed (58.7%) has implications for HIV control and prevention. The causal relationship between prevalent CT/NG and incident HIV has previously been established, with CT/NG shown to increase both the risk of HIV acquisition and transmission [45]. Among MSM, rectal CT/NG re-infection has been associated with increased risk of HIV seroconversion [46], with modelling studies demonstrating that 10.4% of incident HIV infections are attributable to CT/NG infection [47]. TSMSM should therefore be encouraged to have diagnostic STI screening often, depending on sexual activity and risk-taking, and thereafter receive appropriate care. This would help mitigate the deleterious synergy between STI and HIV, as well as forestall morbidities such as infertility that occur secondary to some STI.
Although not independently associated with HIV infection in our study, other behaviors that increase the risk of HIV infection were common. These include engaging in condomless sex, group sex, transactional sex, alcohol and drug use during sex, as well as having multiple sex partners. These findings are consistent with what has been observed among TSMSM in China [10] and South Africa [13]. Behavioral change is therefore urgently needed in this population to augment the biomedical tools available for HIV prevention.
To our knowledge, this study was the first one to assess the prevalence and associated factors of HIV among TSMSM in Kenya, and possibly in sub-Saharan Africa using the RDS method. These findings should be viewed in light of some limitations. Firstly, RDS is not a classical probabilistic sampling method. To offset this limitation, when calculating our sample size, we applied a design effect of 3 to account for the clustering that occurs due to homophily and minimize the traditional bias associated with snowball sampling. We also excluded from analysis the 6 seeds who were purposely selected to start off recruitment. Secondly, since we asked about what happened in the past year, there was a possibility of recall bias. To mitigate this, we aimed to include in our questionnaire either single or multiple choice questions and have very few instances where participants needed to type out answers. We also limited the number of questions about events that happened more than 12 months before the study. Thirdly, we asked questions about sexual behavior which may be affected by social desirability bias. To minimize this, participants self-administered the survey on an online platform accessed through tablet computers, since this has been shown to be more effective in offsetting this kind of bias, as compared to face-to-face interviews [48]. Fourthly, the cross-sectional nature of the study limits causal inference of the independent risk factors identified for HIV infection. Finally, though we used a comprehensive set of variables in the logistic regression analysis, we cannot rule out the possibility of residual confounding from other variables such as experiences of stigma, discrimination and violence. Despite these limitations, this survey offers valuable lessons on the burden of HIV and associated factors among TSMSM, and hopefully portends the development of tailored interventions for the HIV response in this key yet understudied population.
Conclusions
In summary, HIV prevalence among TSMSM in Nairobi is 6 times higher than that of Kenyan young men of comparable age. As a result, urgent efforts to develop bespoke HIV prevention and control interventions for this population are called for. Such interventions should seek to enhance HIV testing (including through HIV self-testing), as well as promote STI screening and treatment. TSMSM should be provided with education messages on the attendant risk of HIV infection in age-disparate relationships, and empowered to practice safer sex through use of both condoms and PrEP. Further, there is need for collaboration between tertiary institutions and relevant agencies of the ministry of health such as National AIDS and STI Control Program (NASCOP), in providing HIV prevention and control services to TSMSM so as to avert new HIV infections in this population. Given its widespread availability and use in Kenya, the internet is an innovative tool that should be harnessed for delivery of these interventions.
Availability of data and materials
The datasets used and/or analyzed during this study is not publicly available, but may be available from the corresponding author upon reasonable request, and with permission from University of the Witwatersrand Human Research Ethics Committee-Medical and University of Nairobi-Kenyatta National Hospital Ethics and Research Committee.
References
GBD 2019 HIV Collaborators. Global, regional, and national sex-specific burden and control of the HIV epidemic, 1990–2019, for 204 countries and territories: the Global Burden of Diseases Study 2019”. Lancet HIV. 2021;8(10):e633–51.
National AIDS Control Council (NACC). The second Kenya AIDS strategic framework II, 2020/21, 2024/25—sustain gains, bridge gaps and accelerate progress,” Nairobi: Government of Kenya, 2020. [Online]. https://nacc.or.ke/wp-content/uploads/2021/01/KASFII_Web22.pdf. Accessed 11 Nov 2021.
Joint United Nations Programme on HIV/AIDS (UNAIDS). 2021 global AIDS update—confronting inequalities. Geneva, Switzerland; 2021.
Hessou PHS, et al. Comparison of the prevalence rates of HIV infection between men who have sex with men (MSM) and men in the general population in sub-Saharan Africa: a systematic review and meta-analysis. BMC Public Health. 2019;19(1):1634.
Smith AD, Kimani J, Kabuti R, Weatherburn P, Fearon E, Bourne A. HIV burden and correlates of infection among transfeminine people and cisgender men who have sex with men in Nairobi, Kenya: an observational study. Lancet HIV. 2021;8(5):e274–83.
National AIDS and STI Control Programme (NASCOP) Kenya. “Preliminary Kenya population-based HIV impact assessment (KENPHIA) Report, Nairobi, Kenya: NASCOP. 2020.
Kenya National AIDS Control Council. Kenya HIV prevention response and modes of transmission analysis report_March 2009. 2009.
National AIDS and STI Control Programme (NASCOP) Kenya. National AIDS and STI Control Programme Organogram. [Online]. https://www.nascop.or.ke/organogram/. Accessed 11 Jan 2022.
Musyoki H, Bhattacharjee P, Sabin K, Ngoksin E, Wheeler T, Dallabetta G. A decade and beyond: learnings from HIV programming with underserved and marginalized key populations in Kenya. J Int AIDS Soc. 2021;24(Suppl 3):e25729–e25729.
Fan S, et al. HIV and syphilis and sexual risk behaviours among men who have sex with men attending university in China: a systematic review and meta-analysis. Sex Health. 2019;16(6):554–65.
Higher Education HIV/AIDS Programme South Africa (HEAIDS). HIV Prevalence and Related Factors: Higher Education Sector Study South Africa. Johannesburg, South Africa; 2009.
Renn K. LGBTQ students on campus: issues and opportunities for higher education leaders. Higher Education Today, 2017. [Online]. https://www.higheredtoday.org/2017/04/10/lgbtq-students-higher-education/. Accessed 10 Jun 2021.
Brink JG, Unit E, Africa S. Considerations for South African higher education: a national student men who have sex with men sexual behavior survey. S Afr J High Educ. 2017;31(4):184–207.
“Laws of Kenya Cap 63: The Penal Code.” [Online]. http://www.kenyalaw.org/lex/actview.xql?actid=CAP.63. Accessed 18 Aug 2021.
Delany-moretlwe S, Cowan FM, Busza J, Bolton-moore C, Kelley K, Fairlie L. Providing comprehensive health services for young key populations: needs, barriers and gaps. J Int AIDS Soc. 2015;18(Suppl 1):29–40.
Joint United Nations Programme on HIV/AIDS (UNAIDS). AIDS and the sustainable development goals, UNAIDS. [Online]. https://www.unaids.org/en/AIDS_SDGs. Accessed 06 May 2021.
Mwaniki SW, Mugo PM, Palanee-Phillips T. Project BESPOKE (integrated bio-behavioral assessment of HIV and STI among young tertiary student men who have sex with men in Nairobi, Kenya): a respondent-driven sampling survey protocol. Front Public Health. 2021;9:1452.
Study in Kenya. Universities and Colleges in Nairobi County. 2021. [Online]. https://studyinkenya.co.ke/universities-and-colleges-in-nairobi-county?page=1. Accessed 24 Sep 2021.
University of Nairobi. About us: students. 2021. [Online]. https://www.uonbi.ac.ke/students. Accessed 16 Oct 2021.
F. 360 WHO, CDC, UNAIDS. Biobehavioural survey guidelines for populations at risk for HIV. Geneva: World Health Organization; 2017.
Cochran WG. Sampling techniques. 3rd ed. New York: Wiley; 1977.
Mwaniki SW, Kaberia PM, Mugo PM, Palanee-Phillips T. ‘My friends would believe my word’: appropriateness and acceptability of respondent-driven sampling in recruiting young tertiary student men who have sex with men for HIV/STI research in Nairobi, Kenya. medRxiv 2021. 10.21.21265250
Respondent Driven Sampling. [Online]. http://www.respondentdrivensampling.org/. Accessed 24 Sep 2021.
University of California San Francisco (UCSF). Integrated HIV Bio-behavioural Surveillance Toolbox. [Online]. https://globalhealthsciences.ucsf.edu/resources/integrated-hiv-bio-behavioral-surveillance-toolbox. Accessed 24 Sep 2021.
National AIDS and STI Control Programme (NASCOP) Kenya. Kenya HIV testing services guidelines. 2016. [Online]. https://www.nascop.or.ke/hiv-testing-services/. Accessed 11 Jan 2022.
Handcock M, Fellows I, Gile K. RDS analyst: software for the analysis of respondent-driven sampling data, version 0.72.” [Online]. http://wiki.stat.ucla.edu/hpmrg/index.php/RDS_Analyst_Install. Accessed 07 Oct 2021.
Gile KJ. Improved inference for respondent-driven sampling data with application to HIV prevalence estimation. J Am Stat Assoc. 2011;106(493):135–46.
UNAIDS (Joint United Nations Programme on HIV/AIDS). Recommended population size estimates of men who have sex with men. 2020. [Online]. https://www.unaids.org/sites/default/files/media_asset/2020-recommended-population-size-estimates-of-men-who-have-sex-with-men_en.pdf. Accessed 07 Oct 2021.
Avery L, Rotondi N, McKnight C, Firestone M, Smylie J, Rotondi M. Unweighted regression models perform better than weighted regression techniques for respondent-driven sampling data: results from a simulation study. BMC Med Res Methodol. 2019;19(1):1–13.
Bekker L-G. HIV control in young key populations in Africa. Lancet Child Adolesc Heal. 2019;3(7):442–4.
UNAIDS Joint United Nations Programme on HIV/AIDS. Fast-track: accelerating action to end the AIDS epidemic by 2030. Geneva: UNAIDS; 2014.
Mugo PM, et al. Uptake and acceptability of oral HIV self-testing among community pharmacy clients in Kenya: a feasibility study. PLoS ONE. 2017;12(1): e0170868.
Johnston LG, et al. Alarmingly high HIV prevalence among adolescent and young men who have sex with men (MSM) in Urban Indonesia. AIDS Behav. 2021;25(11):3687–94.
Bhattacharjee P, et al. HIV prevalence, testing and treatment among men who have sex with men through engagement in virtual sexual networks in Kenya: a cross-sectional bio-behavioural study. J Int AIDS Soc. 2020;23(S2): e25516.
Stahlman S, et al. Characteristics of men who have sex with men in southern Africa who seek sex Online: a cross-sectional study. J Med Internet Res. 2015;17(5):1–12.
Zou H, Fan S. Characteristics of men who have sex with men who use smartphone geosocial networking applications and implications for HIV interventions: a systematic review and meta-analysis. Arch Sex Behav. 2017;46(4):885–94.
Ojino R, Mich L. Mobile applications in university education: the case of Kenya. J E-Learn Knowl Soc 2018; 14(1).
Hurt CB, et al. Sex with older partners is associated with primary HIV infection among men who have sex with men in North Carolina. JAIDS J Acquir Immune Defic Syndr. 2010;54(2):185–90.
Ding Y, Zhou Y, Liu C, Liu X, He N. Sex with older partners, condomless anal sex and unrecognized HIV infection among Chinese men who have sex with men. AIDS Care. 2018;30(3):305–11.
Arrington-Sanders R, Leonard L, Brooks D, Celentano D, Ellen J. Older partner selection in young African–American men who have sex with men. J Adolesc Heal. 2013;52(6):682–8.
Anema A, et al. Intergenerational sex as a risk factor for HIV among young men who have sex with men: a scoping review. Curr HIV/AIDS Rep. 2013;10(4):398–407.
Braun V, Schmidt J, Gavey N, Fenaughty J. Sexual coercion among gay and bisexual men in Aotearoa/New Zealand. J Homosex. 2009;56(3):336–60.
AVAC (AIDS Vaccine Advocacy Coalition). PrEP watch Kenya. [Online]. https://www.prepwatch.org/country/kenya/. Accessed 18 Jan 2022.
Traeger MW, et al. Association of HIV preexposure prophylaxis with incidence of sexually transmitted infections among individuals at high risk of HIV infection. JAMA. 2019;321(14):1380–90.
Fleming DT, Wasserheit JN. From epidemiological synergy to public health policy and practice: the contribution of other sexually transmitted diseases to sexual transmission of HIV infection. Sex Health. 1999;75:3–17.
Bernstein KT, Marcus JL, Nieri G, Philip SS, Klausner JD. Rectal gonorrhea and chlamydia reinfection is associated with increased risk of HIV seroconversion. JAIDS J Acquir Immune Defic Syndr. 2010;53(4):537–43.
Jones J, et al. Proportion of incident HIV cases among men who have sex with men attributable to gonorrhea and chlamydia: a modeling analysis. Sex Transm Dis. 2019;46(6):357–63.
Adebajo S, et al. Comparison of audio computer assisted self-interview and face-to-face interview methods in eliciting HIV-related risks among men who have sex with men and men who inject drugs in Nigeria. PLoS ONE. 2014;9(1):1–6.
Acknowledgements
The authors would like to thank Joshua Kimani of Partners for Health and Development in Africa (PHDA) for hosting the data collection at the TRANSFORM study site in Nairobi, Kenya, as well as other staff from PHDA (Rhoda Wanjiru, Monica Okumu, Mary Wanjiru, Hellen Babu, Evelyn Ombunga, Elizabeth Rwenji, Ibrahim Lwingi, Zaina Jama, Pauline Ngurukiri and Laisa Lumumba) for their invaluable support with acquisition of data. We are equally grateful to Babatunde Adedokun of the Department of Medicine and Center for Global Health, University of Chicago, Chicago, USA for his guidance throughout the data analysis process. Finally, we thank all the study participants without whom the study would not have been possible.
Funding
SWM was supported by the Consortium for Advanced Research Training in Africa (CARTA). CARTA is jointly led by the African Population and Health Research Center and the University of the Witwatersrand and funded by the Carnegie Corporation of New York (Grant No. G-19-57145), SIDA (Grant No:54100113), Uppsala Monitoring Center, Norwegian Agency for Development Cooperation (NORAD), and by the Wellcome Trust [reference no. 107768/Z/15/Z] and the UK Foreign, Commonwealth & Development Office, with support from the Developing Excellence in Leadership, Training and Science in Africa (DELTAS Africa) programme. The statements made and views expressed are solely the responsibility of the Fellow.
Author information
Authors and Affiliations
Contributions
SWM, PMM, TPP conceptualized the study, designed the study protocol and its instruments. SWM and PMK acquired and analyzed the data. PMK prepared Fig. 1. PMM and TPP reviewed the manuscript. SWM acquired funding for the study, drafted the manuscript and incorporated authors’ contributions. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by University of the Witwatersrand Human Research Ethics Committee-Medical (Ref. No. M200215) and University of Nairobi-Kenyata National Hospital Ethics and Research Committee (Ref. No. P990/12/2019). All participants provided written informed consent to participate.
Competing interests
The authors have no competing interests or other interests that might be perceived to influence the results and/or discussion reported in this paper.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Mwaniki, S.W., Kaberia, P.M., Mugo, P.M. et al. HIV prevalence and associated risk factors among young tertiary student men who have sex with men (MSM) in Nairobi, Kenya: a respondent-driven sampling survey. AIDS Res Ther 20, 7 (2023). https://doi.org/10.1186/s12981-023-00502-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12981-023-00502-6