Abstract
Background and purpose
The immune response changes during aging and the progression of Alzheimer’s disease (AD) and related dementia (ADRD). Terminally differentiated effector memory T cells (called TEMRA) are important during aging and AD due to their cytotoxic phenotype and association with cognitive decline. However, it is not clear if the changes seen in TEMRAs are specific to AD-related cognitive decline specifically or are more generally correlated with cognitive decline. This study aimed to examine whether TEMRAs are associated with cognition and plasma biomarkers of AD, neurodegeneration, and neuroinflammation in a community-based cohort of older adults.
Methods
Study participants from a University of Kentucky Alzheimer’s Disease Research Center (UK-ADRC) community-based cohort of aging and dementia were used to test our hypothesis. There were 84 participants, 44 women and 40 men. Participants underwent physical examination, neurological examination, medical history, cognitive testing, and blood collection to determine plasma biomarker levels (Aβ42/Aβ40 ratio, total tau, Neurofilament Light chain (Nf-L), Glial Fibrillary Acidic Protein (GFAP)) and to isolate peripheral blood mononuclear cells (PBMCs). Flow cytometry was used to analyze PBMCs from study participants for effector and memory T cell populations, including CD4+ and CD8+ central memory T cells (TCM), Naïve T cells, effector memory T cells (TEM), and effector memory CD45RA+ T cells (TEMRA) immune cell markers.
Results
CD8+ TEMRAs were positively correlated with Nf-L and GFAP. We found no significant difference in CD8+ TEMRAs based on cognitive scores and no associations between CD8+ TEMRAs and AD-related biomarkers. CD4+ TEMRAs were associated with cognitive impairment on the MMSE. Gender was not associated with TEMRAs, but it did show an association with other T cell populations.
Conclusion
These findings suggest that the accumulation of CD8+ TEMRAs may be a response to neuronal injury (Nf-L) and neuroinflammation (GFAP) during aging or the progression of AD and ADRD. As our findings in a community-based cohort were not clinically-defined AD participants but included all ADRDs, this suggests that TEMRAs may be associated with changes in systemic immune T cell subsets associated with the onset of pathology.
Similar content being viewed by others
Introduction
The innate and adaptive immune system, essential for protecting individuals against infections, injury, and diseases, is profoundly impacted by chronological aging, becoming less protective and more inflammatory [1]. The age-associated decline in T cell function contributes to increased susceptibility to infections such as influenza, COVID-19, pneumonia, and urinary tract infections (UTI) [1, 2]. Beyond aging, changes in adaptive immune responses are exacerbated in Alzheimer’s disease (AD) and related dementias (ADRD) [3,4,5,6,7,8,9,10]. The most common ADRDs in the community include AD, Limbic-predominant age-related TDP-43 encephalopathy (LATE-NC), Lewy body dementia (LBD), vascular contributions to cognitive impairment and dementia (VCID), and multiple-etiology dementias (MED) [11]. The ADRD-associated adaptive immune changes include a decrease in naïve T cells and the accumulation of cytotoxic memory and effector memory T cells [3,4,5,6,7,8,9], which may further weaken the protection against pathogens and vaccine responsiveness. Infections such as pneumonia and UTI are higher in individuals with dementia [12], with the weakened immune system being a major contributor to the greater infection-induced mortality in individuals with dementia [13, 14].
A handful of studies have evaluated the adaptive immune response in ADRD, highlighting a central role for terminally differentiated effector memory T cells (called TEMRAs). TEMRAs are CD4+ or CD8+ T cells that re-express CD45RA. In clinic-based studies, more TEMRAs were associated with increased neurodegenerative pathology and worse cognitive function [5,6,7]. TEMRAs, which are also associated with viral infections such as cytomegalovirus (CMV), dengue, and human immunodeficiency virus (HIV) [3, 15, 16], are known for their T cell effector function, low proliferation capacity, and cytotoxic activity [17,18,19].
While changes in T cell subsets, including TEMRAs, are linked to Alzheimer’s disease (AD) [5,6,7], studies have not made it clear if these changes are specific to AD-related cognitive decline or are more generally correlated with dementia, as prior studies were limited to people with AD-related dementia diagnosed by reduced cognitive scores, computed tomography (CT), magnetic resonance scanning (MRI) for volumetric loss of brain regions, Aβ PET imaging, and reduced CSF Aβ and tau levels [5,6,7]. In addition, the connection between TEMRAs and early stages of cognitive decline is not well established. We analyzed cells by flow cytometry from two groups to identify associations between CD4+ or CD8+ TEMRAs in peripheral blood and early cognitive decline in a community-based cohort of older individuals based on their clinical dementia rating (CDR). Our groups were cognitively healthy control participants (CDR = 0) and individuals with early stages of cognitive decline (CDR = 0.5-1). To test associations between TEMRAs and AD, we measured plasma biomarkers of AD, such as β-amyloid (Aβ) and tau, which asses the risk for establishing AD. We also measured plasma markers neurofilament light (Nf-L) and glial fibrillary acidic protein (GFAP), which assesses neuronal injury and astrocyte-mediated neuroinflammation, respectively. We found that CD8+ TEMRAs are associated with biomarkers of brain injury (Nf-L and GFAP), while CD4+ TEMRAs are associated with low Mental State Examination (MMSE) scores and a biomarker of AD (Aβ42/40).
Materials and methods
Human subjects
The participants in this study were recruited from a larger cohort study of aging and dementia at the University of Kentucky Alzheimer’s Disease Research Center [20, 21]. Before participating in the study, the participants provided informed consent according to University of Kentucky Institutional Review Board-approved protocols. The AD Research Center recruits older adults from central Kentucky and includes approximately 500 active participants who receive annual follow-up visits. These visits include a variety of measures, such as physical and neurological examinations, medical histories, cognitive testing, and fluid biomarkers. For our analysis, we recruited n = 40 cognitively healthy individuals (CDR = 0) and n = 44 cognitively impaired (CDR = 0.5-1) individuals, with similar numbers based on gender, and cardiovascular disease risk factors and age. The participants were excluded if they had type 2 diabetes, auto-immune disease, or active cancer. Blood samples were collected from 84 participants between August 2020 and June 2021, and clinical evaluations and cognitive testing were performed using the National Alzheimer’s Coordinating Center uniform data set [11, 22]. The de-identified samples were provided to the experimentalists, who were blinded to the participant group identity until all data had been generated.
Peripheral blood mononuclear cell (PBMC) isolation
5-10mls of peripheral blood was taken through venous puncture and stored in acid/citrate/dextrose tubes. PBMCs were isolated by density centrifugation in Ficoll histopaque 1077 using SepMate PBMC isolation tube (StemCell tech, Cat#: 85,415) according to the manufacturer’s protocol. After the cells were washed in buffer (0.1 BSA, 2mM EDTA, 1X PBS), residual red blood cells were removed using red blood cells lysis buffer (EBioscience, cat#: 00-4300-54). The cells were then frozen at a density of 1 × 106/ml in freezing media containing (90%FBS Heat Inactivated (HI), 10% DMSO) and stored at -80 °C in a Mr. Frosty apparatus (Nalgene) for 24 h before being transferred to long-term storage in liquid N2 until use as previously described [23].
Plasma biomarker analysis
The plasma collected from the same blood drawn as the PBMCs underwent analysis on the Quanterix Simoa HD-X for plasma biomarkers as previously described [24].
Flow cytometry
After being thawed, PBMCs were washed with warm RPMI followed by PBS. The cells were then stained with viability marker Ghost dye-Alexa Fluor 700 (Tonbo Biosciences) for 30 min at 4 ̊C, then washed with FACS buffer (1X PBS supplemented with 1% bovine serum albumin and. 1% sodium azide). To prevent unintended antibody binding to Fc receptors, cells were blocked with FcR blocking reagent, human (Miltenyi Biotec) for 10 min at 4 ̊C. The cells were then stained at a 1:50 dilution with antibodies to immune cell targets as follows: CD3-FITC (BD Biosciences, 555,332), CD8-PE (BD Biosciences, 555,635), CD4-APC (BD Biosciences, 555,349), CCR7-buv395 (BD Biosciences, 568,681), CD45RA-bv421 (BD Biosciences, 569,620) for 30 min at 4 ̊C. The cells were then washed twice with FACS buffer and fixed using cytofix from BD Biosciences for 30 min at 4 ̊C, followed by a wash with FACS buffer and resuspension in FACS buffer. Cell populations were acquired using the BD Symphony A3, and Flow v10.8 software was used for analysis. Staining and analysis were performed blinded. Fluorescence-minus-one controls were utilized to identify cell populations, and each experiment had a single-stained control and negative control.
Statistics
Characteristics of participants were assessed with analysis of variance or χ2 tests. Fluid biomarker data were log2 transformed. For categorical comparisons, a parametric t-test or one-way ANOVA were used for the combined data, or the data stratified by gender. Multiple linear regression models were used to adjust mean responses for covariates, as listed in figures and tables. Pairwise effect sizes were calculated using Cohen’s d. The effect size for linear regressions were calculated as R2 or Ω2. For the box-and-whiskers graph, the box shows the median, 25th and 75th percentile, and the whiskers show the minimum and maximum values. Data visualizations were created in JMP Pro v16 or GraphPad Prism v9.4.
Results
Patient characteristics
The study included 84 participants from the UK-ADRC community cohort, comprising 40 cognitively healthy (mean age 77, range 62–95) and 44 cognitively impaired (mean age 79, range 64–97) individuals, balancing for gender, cognitive status (CDR = 0 vs. CDR = 0.5-1), age, and cardiovascular risk factors, with demographic details in Table 1 and no marked differences by CDR between groups.
Higher percentage of CD4+ TEMRAs in individuals with low MMSE
Prior studies showed an association between greater CD8+ TEMRAs and worse cognitive function in people with probable AD, and greater CD8+ TEMRAs in cognitively healthy people with preclinical AD, defined by cognitive scores, CSF Aβ and tau levels, MRI, and Aβ PET imaging [5, 6]. Yet, it is unclear if changes in CD8+ TEMRAs are an AD-specific phenotype or are seen more generally with cognitive decline, and if the changes are limited to CD8+ T cells or are also seen in CD4+ T cells. As TEMRAs are seen even in preclinical AD, we also wanted to test in a community-based cohort if TEMRAs are seen with early changes in global cognitive function.
Using flow cytometry, we analyzed CD3+CD4+ and CD3+CD8+ T cells (Fig. 1A; Table 1) for naïve and memory phenotypes based on CD45RA and CCR7 staining (Fig. 1A). CD4+ and CD8+ TEMRAs were not associated with CDR (Fig. 1B), which held when adjusted for age and gender (Table 2). CD4+ TEMRAs (p = 0.0292) and CD8+ TEMRAs (p = 0.0779) were negatively associated with MMSE scores < 25 (Fig. 1C). When adjusted for age and gender, the association between MMSE and TEMRAs did not reach statistical significance. However, the effect sizes (Cohen’s d) for the relationship between TEMRAs and MMSE scores remained substantial, particularly for CD4 + TEMRAs (adjusted Cohen’s d = 0.702, p = 0.0531), suggesting a moderate to large effect. The effect size for CD8 + TEMRAs (adjusted Cohen’s d = 0.54, p = 0.101) was smaller in comparison (Table 2). There was no association between CD4+ TEMRAs and CD8+ TEMRAs and MoCA (Fig. 1D; Table 2).
Testing the Association of CD4+ and CD8+ TEMRAs with global cognitive function. (A) Representative flow cytometry gating strategy for lymphocyte subsets. The strategy begins with gating on lymphocytes, excluding doublets and dead cells. T cells are gated on CD3+; CD4+ T cells are CD3+ CD4+; CD8+ T cells are CD3+ CD8+. The CD4+ and CD8+ T cells are then further divided into central memory (TCM): CD45RA−CCR7+, naive: CD45RA+CCR7+, effector memory (TEM): CD45RA−CCR7−, and terminally differentiated effector memory re-expressing CD45RA (TEMRA): CD45RA+CCR7−. Association of CD4+ and CD8+ TEMRAs with (B) CDR (C) MMSE and (D) MoCA. Circles represent individual participants. The red lines represent the mean and 95% confidence interval for the linear regression. See also, Table 2
Associations of TEMRAs with other relevant biological variables
To determine the impact of other biological variables, including gender, age, body mass index (BMI), and apoE genotype, on the frequency of CD4+ TEMRAs and CD8+ TEMRAs, we completed regression models. We found no associations between apoE or BMI and T cell phenotypes (Table 3). Similarly, age was not associated with CD4+ TEMRAs and CD8+ TEMRAs (Table 3). However, age negatively correlated with naïve CD8+ T cells (p = 0.007) (Table 3). While there were no differences in the frequencies of CD4+ TEMRAs and CD8+ TEMRAs by gender, we detected a higher frequency of CD4+ (p = 0.0369) and CD8+ (p = 0.0192) naïve T cells in women while men have a higher frequency of CD4+ TCMs (p = 0.0056) and CD8+ TEMs (p = 0.0137) (Fig. 2).
Testing the Association of gender with T cell subsets. The frequency of CD4+ (A) and CD8+ (B) T-cell subsets in the blood of women (♀) and men (♂). Circles represent individual participants. See also, Table 3
TEMRAs correlated with plasma markers of neurodegeneration and neuroinflammation
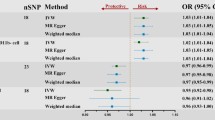
Prior studies stratified their study participants as either controls or clinical / biomarker defined preclinical AD or probable AD [5,6,7]. Our community-based study was stratified by cognitive status but was not limited to AD. Therefore, we tested if plasma biomarkers of AD (Aβ42/Aβ40 ratio and total-tau), neurodegeneration, and brain injury (Nf-L and GFAP) would show a greater association with TEMRAs than what was seen for cognitive status. Aβ42/Aβ40 ratio was positively correlated with the frequency of CD4+ TEMRAs (p = 0.036, Fig. 3A); however, this association did not hold following adjustments for age and gender (Table 4). We found no association between the frequency of CD8+ TEMRAs and the Aβ42/Aβ40 ratio (Fig. 3B; Table 4). CD8+ naïve T cells correlated negatively with Aβ42/Aβ40 ratio; however, this correlation was not significant after accounting for age and gender (Table 4). While there was no association between CD4+ TEMRAs (Fig. 3C; Table 4) and CD8+ TEMRAs with total tau (Fig. 3D; Table 4), we identified a negative correlation between total tau and CD4+ central memory T cells and a positive correlation between total tau and CD4+ naïve T cells (Table 4). These results suggest that the change in TEMRAs may be more indicative of neurodegeneration in general, than an AD-specific change.
TEMRAs correlated with plasma markers of neurodegeneration and neuroinflammation. Correlation between the percentage of CD4+ and CD8+ TEMRA s in the blood of individuals and plasma levels of AD-related biomarkers (A, B) Aβ42/40, (C, D) total tau, (E, F) Nf-L, and (G, H) GFAP. The red lines represent the mean and 95% confidence interval for the linear regression. The p-values and R2 values shown are for the unadjusted analysis. See also Table 4. Markers are for individual participants
Next, we tested the association of T cell subsets and brain injury biomarkers Nf-L (Fig. 3E, F) and GFAP (Fig. 3G, H). Frequency of CD8+ TEMRAs (p = 0.005; Fig. 3F) but not CD4+ TEMRAs (p = 0.07 Fig. 3E) positively correlated with plasma Nf-L. Plasma Nf-L positively correlated with CD4+ central memory T cells (Table 4), however, we found negative correlations between Nf-L and CD4+ and CD8+ naïve T cells (Table 4). Plasma GFAP levels correlated with CD8+ TEMRAs (p = 0.032 Fig. 3H), but not CD4+ TEMRAs (p = 0.163 Fig. 3G). We conclude that CD8+ TEMRAs are associated with early neurodegeneration and/or acute brain injury in the study participants.
Discussion
Terminally differentiated effector memory T cells have been linked to AD-related cognitive decline [5,6,7]. This study aimed to test whether worse cognitive function was associated with greater proportions of these TEMRAs in a community-based cohort of older individuals. We found more CD4+ TEMRAs in individuals with lower MMSE scores. We also found that T cell subsets varied by gender, but not specifically for CD4+ TEMRAs and CD8+ TEMRAs. In our study, CD8+ TEMRAs, previously linked to AD-related cognitive decline defined by CSF AD-biomarkers, cognition, and imaging [5,6,7], correlate with plasma biomarkers of brain injury (Nf-L and GFAP). In our community-based aging cohort, we also found that terminally differentiated effector memory T cells were also associated with both cognitive impairment and brain injury biomarkers. Our findings suggest that TEMRAs may be related to changes in systemic immune T cell subsets associated with neuronal injury in dementia, including AD.
Studies from multiple groups have shown that CD8+ TEMRAs accumulate in the blood of pre-clinical, MCI, and AD patients [5,6,7]. Although we did not see significant increases in CD8+ TEMRAs in our cognitively impaired participants classified by CDR and MoCA, we note a trend towards more CD8+ TEMRAs in our participants with low MMSE scores. The lack of difference could be because the cognitive decline seen in our participants could be from multiple etiologies. For example, studies using brains from the University of Kentucky brain bank have shown that 50% of individuals with dementia can have three or four proteinopathies (tau neurofibrillary tangles, Aβ, α-synuclein and transactive response DNA-binding protein 43 (TDP-43)) that could contribute to differences in the immune response [11]. Prior studies only included patients positive for Aβ, probable AD, or MCI due to AD [5,6,7], which suggests that the accumulation of CD8+ TEMRAs seen may be specific to AD. However, increases in CD8+ TEMRAs were also seen in cognitively healthy individuals with PET imaging positive for Aβ [6], implying that an individual doesn’t have to be cognitively impaired to have a higher frequency of CD8+ TEMRAs. Thus, the accumulation of CD8+ TEMRAs may be more associated with the pathology or injury caused by the accumulation of Aβ than overt cognitive decline.
Our lack of differences in CD8+ TEMRAs led us to examine the influence of other important biological variables. In contrast to other studies, we did not find any significant differences in CD8+ TEMRAs by gender, however in line with previous studies, women in the cohort, irrespective of cognitive status, have significantly more CD4+ and CD8+ naïve T cells [3]. Women in the cohort also have significantly fewer CD4+ central memory and CD8+ effector memory T cells compared to men. The difference in naïve populations suggests that most women in our cohort may have more T cells that are not cytotoxic and can respond to new antigens; however, this was not tested. More effector memory T cells in men suggest that they are in a more cytotoxic state, with populations that can secrete proinflammatory cytokines or are ready for antigen restimulation. Overall, however, the increased percentage of CD8+ naïve T cells potentially contributes to our lack of differences in our CD8+ TEMRAs.
CD4+ TEMRAs in healthy individuals are found in the blood at a lower frequency (0.3–18%) [25] than their CD8+ counterparts. The two cell types share similarities, including the ability to secrete perforin and granzyme and relatively reduced proliferative capacities [17], In contrast to the CD8+ TEMRAs, we did see more CD4+ TEMRAs in participants with lower MMSE scores, which agrees with previous studies showing more CD4+ TEMRAs in people with AD [7]. CD4+ memory and cytotoxic T cells have also been shown to be associated with patients with Parkinson’s disease [8,9,10], suggesting a degree of specificity in T cell changes to different neurodegenerative diseases. Our results agree with this interpretation as the early stages of cognitive decline, and the multiple possible disease etiologies causing that decline in our study participants could lead to mixed CD4+ and CD8+ responses in our group analysis. Future studies using pathologically-confirmed consensus diagnosis would test this hypothesis. Recent studies also show a role for mitochondria in TEMRAs, with CD4+ TEMRAs having more mitochondrial content and fewer mitochondrial nodes when compared to CD8+ TEMRAs [26]. As different mitochondria abnormalities are seen in PD vs. AD, for example, these changes in mitochondria could be responsible for potential specificity in T cell changes to different neurodegenerative diseases.
While studies have shown evidence of TEMRA-induced protective functions in the setting of dengue [15, 17], the function of these cells in neurodegenerative disease is unknown. Previous studies found evidence of CD8+ T cells in the brain with AD pathology and suggested that these cells contribute to neuronal injury and neuroinflammation [5, 27]. In agreement with this suggestion, we found a positive correlation between CD8+ TEMRAs and plasma biomarkers of neuronal injury (Nf-L) and neuroinflammation (GFAP). In a mouse model of tauopathy, depleting T cells or using an immune checkpoint blockade (PDCD1) reduced neurodegeneration [27], which agrees with other studies in models of neurodegenerative disease [28,29,30], suggesting a provocative hypothesis that T cells could be directly causing neurodegeneration in AD.
In contrast to a protective function, increased abundance of circulating TEMRAs is also associated with high cytotoxicity and anti-viral functions [17,18,19]. When CD4+ and CD8+ T cells differentiate into TEMRAs, they stop expressing the co-stimulatory molecules CD28 and CD27,molecules crucial for T-cell activation, proliferation, and survival [31]. TEMRAs upregulate CD57, a senescence marker associated with decreased telomere length and low proliferative capacity [32]. Viral infections lead to the accumulation of CD8+ TEMRAs, [33, 34] leading to the idea that the accumulation of TEMRAs during aging and the progression of AD could be due to latent viral infections [3, 5, 6]. While studies have shown that infections with viruses such as herpes simplex virus (HSV) and CMV are associated with the development of AD [35, 36], recent studies in pre-clinical AD find the accumulation of CD8+ TEMRAs was independent of latent, reactivated, or acute Herpesviridae background infections [6]. This suggests that TEMRAs can also accumulate in the absence of viral infections, again highlighting a potential neuroinjury response.
Our study has limitations. Firstly, our participants are from a community-based cohort at a single site. While we tried to balance cardiovascular disease risk factors between the groups, one study can never entirely represent the community cohort. Moreover, the cohort mainly comprises highly educated white individuals, which does not reflect the broader elderly population. Future studies must be done in a larger cohort with more racial, ethnic, and socioeconomic diversity. Studies have shown that in populations at risk for developing AD, there are differences in cortical thickness and white matter hyperintensity (WMH) [37] and well as CSF AD biomarkers and vascular markers across race and ethnicity [38]. These data suggest that having a more diverse population could potentially change the outcome of the results presented in this study. Furthermore, we did not assay for any viral infection, so we don’t know if any participants in our group had latent or prior viral infections such as CMV, HIV, or HSV, which could skew TEMRA populations in both cognitively normal and impaired people.
In summary, the accumulation of CD8+ TEMRAs is either specific for AD, as shown by others [5,6,7], or is associated with neuronal injury and neuroinflammation caused by ADRD. CD4+ TEMRAs may also be important in progressing AD and AD-related dementia. As we see more CD4+ TEMRAs in our cohort, future studies should focus on whether CD4+ TEMRAs are an early sign of AD or ADRD progression. Furthermore, since CD4+ T cells are well known to assist with CD8+ T cell memory function, studies should determine how the presence of CD4+ TEMRAs impacts the accumulation of CD8+ TEMRAs to determine the interplay between the two. The question remains if their relationship is dependent or independent of each other and how it contributes to ongoing pathology, though a better understanding of these critical immune populations could shed light on potential therapeutic strategies for millions at risk for ADRD.
Data availability
All data generated in this study are available in the main text. Additional data are available following reasonable request to the University of Kentucky Alzheimer Disease Research Center.
Abbreviations
- AD:
-
Alzheimer’s Disease
- ADRD:
-
Alzheimer’s disease and related dementia
- PBMCs:
-
Peripheral blood mononuclear cells
- TEMRAs:
-
Terminally differentiated memory T cells
- TCM:
-
Central memory T cells
- TEM:
-
Effector memory T cells
- Aβ:
-
β amyloid
- Nf-L:
-
Neurofilament light
- GFAP:
-
Glial fibrillary acidic protein
- CDR:
-
Clinical dementia rating scale
- MMSE:
-
Mini-Mental State Examination
- MoCA:
-
Montreal Cognitive Assessment
- WMH:
-
White matter hyperintensity
- TDP-43:
-
Transactive response DNA-binding protein 43
References
Lutshumba J, Nikolajczyk BS, Bachstetter AD. Dysregulation of systemic immunity in aging and dementia. Front Cell Neurosci. 2021;15:652111.
Guo L, Li X, Gould T, Wang ZY, Cao W. T cell aging and Alzheimer’s disease. Front Immunol. 2023;14:1154699.
Fang Y, Doyle MF, Chen J, Mez J, Satizabal CL, Alosco ML, Qiu WQ, Lunetta KL, Murabito JM. Circulating immune cell phenotypes are associated with age, sex, CMV, and smoking status in the Framingham Heart Study offspring participants. Aging. 2023;15(10):3939–66.
Thyagarajan B, Faul J, Vivek S, Kim JK, Nikolich-Zugich J, Weir D, Crimmins EM. Age-related differences in T-Cell subsets in a nationally Representative Sample of people older Than Age 55: findings from the Health and Retirement Study. J Gerontol Biol Sci Med Sci. 2022;77(5):927–33.
Gate D, Saligrama N, Leventhal O, Yang AC, Unger MS, Middeldorp J, Chen K, Lehallier B, Channappa D, De Los Santos MB, et al. Clonally expanded CD8 T cells patrol the cerebrospinal fluid in Alzheimer’s disease. Nature. 2020;577(7790):399–404.
Gericke C, Kirabali T, Flury R, Mallone A, Rickenbach C, Kulic L, Tosevski V, Hock C, Nitsch RM, Treyer V et al. Early beta-amyloid accumulation in the brain is associated with peripheral T cell alterations. Alzheimers Dement 2023.
Larbi A, Pawelec G, Witkowski JM, Schipper HM, Derhovanessian E, Goldeck D, Fulop T. Dramatic shifts in circulating CD4 but not CD8 T cell subsets in mild Alzheimer’s disease. J Alzheimers Dis. 2009;17(1):91–103.
Saunders JA, Estes KA, Kosloski LM, Allen HE, Dempsey KM, Torres-Russotto DR, Meza JL, Santamaria PM, Bertoni JM, Murman DL, et al. CD4 + regulatory and effector/memory T cell subsets profile motor dysfunction in Parkinson’s disease. J Neuroimmune Pharmacol. 2012;7(4):927–38.
Wang P, Yao L, Luo M, Zhou W, Jin X, Xu Z, Yan S, Li Y, Xu C, Cheng R, et al. Single-cell transcriptome and TCR profiling reveal activated and expanded T cell populations in Parkinson’s disease. Cell Discov. 2021;7(1):52.
Contaldi E, Magistrelli L, Comi C. T lymphocytes in Parkinson’s Disease. J Parkinsons Dis. 2022;12(s1):S65–74.
Karanth S, Nelson PT, Katsumata Y, Kryscio RJ, Schmitt FA, Fardo DW, Cykowski MD, Jicha GA, Van Eldik LJ, Abner EL. Prevalence and clinical phenotype of Quadruple misfolded proteins in older adults. JAMA Neurol. 2020;77(10):1299–307.
Ryvicker M, Barron Y, Shah S, Moore SM, Noble JM, Bowles KH, Merrill J. Clinical and demographic profiles of Home Care patients with Alzheimer’s Disease and related dementias: implications for information transfer Across Care settings. J Appl Gerontol. 2022;41(2):534–44.
Pereira B, Xu XN, Akbar AN. Targeting inflammation and immunosenescence to improve vaccine responses in the Elderly. Front Immunol. 2020;11:583019.
Gilstrap L, Zhou W, Alsan M, Nanda A, Skinner JS. Trends in Mortality Rates among Medicare enrollees with Alzheimer Disease and related dementias before and during the early phase of the COVID-19 pandemic. JAMA Neurol. 2022;79(4):342–8.
Tian Y, Babor M, Lane J, Schulten V, Patil VS, Seumois G, Rosales SL, Fu Z, Picarda G, Burel J, et al. Unique phenotypes and clonal expansions of human CD4 effector memory T cells re-expressing CD45RA. Nat Commun. 2017;8(1):1473.
Meraviglia S, Di Carlo P, Pampinella D, Guadagnino G, Presti EL, Orlando V, Marchetti G, Dieli F, Sergi C, T-Cell. Subsets (T(CM), T(EM), T(EMRA)) and poly-functional Immune response in patients with human immunodeficiency virus (HIV) infection and different T-CD4 cell response. Ann Clin Lab Sci. 2019;49(4):519–28.
Patil VS, Madrigal A, Schmiedel BJ, Clarke J, O’Rourke P, de Silva AD, Harris E, Peters B, Seumois G, Weiskopf D et al. Precursors of human CD4(+) cytotoxic T lymphocytes identified by single-cell transcriptome analysis. Sci Immunol 2018, 3(19).
Appay V, van Lier RA, Sallusto F, Roederer M. Phenotype and function of human T lymphocyte subsets: consensus and issues. Cytometry A. 2008;73(11):975–83.
Salumets A, Tserel L, Rumm AP, Turk L, Kingo K, Saks K, Oras A, Uibo R, Tamm R, Peterson H, et al. Epigenetic quantification of immunosenescent CD8(+) TEMRA cells in human blood. Aging Cell. 2022;21(5):e13607.
Schmitt FA, Nelson PT, Abner E, Scheff S, Jicha GA, Smith C, Cooper G, Mendiondo M, Danner DD, Van Eldik LJ, et al. University of Kentucky Sanders-Brown healthy brain aging volunteers: donor characteristics, procedures and neuropathology. Curr Alzheimer Res. 2012;9(6):724–33.
Bachstetter AD, Lutshumba J, Winford E, Abner EL, Martin BJ, Harp JP, Van Eldik LJ, Schmitt FA, Wilcock DM, Stowe AM, et al. A blunted T(H)17 cytokine signature in women with mild cognitive impairment: insights from inflammatory profiling of a community-based cohort of older adults. Brain Commun. 2023;5(5):fcad259.
Abner EL, Kryscio RJ, Cooper GE, Fardo DW, Jicha GA, Mendiondo MS, Nelson PT, Smith CD, Van Eldik LJ, Wan L, Schmitt FA. Mild cognitive impairment: statistical models of transition using longitudinal clinical data. Int J Alzheimers Dis 2012, 2012:291920.
Nicholas DA, Proctor EA, Agrawal M, Belkina AC, Van Nostrand SC, Panneerseelan-Bharath L, Jones ARt, Raval F, Ip BC, Zhu M, et al. Fatty acid metabolites combine with reduced beta oxidation to activate Th17 inflammation in human type 2 diabetes. Cell Metab. 2019;30(3):447–e461445.
Winder Z, Sudduth TL, Anderson S, Patel E, Neltner J, Martin BJ, Snyder KE, Abner EL, Jicha GA, Nelson PT, Wilcock DM. Examining the association between blood-based biomarkers and human post mortem neuropathology in the University of Kentucky Alzheimer’s Disease Research Center autopsy cohort. Alzheimers Dement. 2023;19(1):67–78.
Burel JG, Qian Y, Lindestam Arlehamn C, Weiskopf D, Zapardiel-Gonzalo J, Taplitz R, Gilman RH, Saito M, de Silva AD, Vijayanand P, et al. An Integrated Workflow To Assess Technical and Biological variability of Cell Population frequencies in Human Peripheral blood by Flow Cytometry. J Immunol. 2017;198(4):1748–58.
Strickland M, Lee S, Neo SY, Balachander A, Low I, Mustafah S, Goh WI, Wright GD, Larbi A, Pender SLF. Mitochondrial dysfunction in CD4 + T effector memory RA + cells. Biology (Basel) 2023, 12(4).
Chen X, Firulyova M, Manis M, Herz J, Smirnov I, Aladyeva E, Wang C, Bao X, Finn MB, Hu H, et al. Microglia-mediated T cell infiltration drives neurodegeneration in tauopathy. Nature. 2023;615(7953):668–77.
Laurent C, Dorothee G, Hunot S, Martin E, Monnet Y, Duchamp M, Dong Y, Legeron FP, Leboucher A, Burnouf S, et al. Hippocampal T cell infiltration promotes neuroinflammation and cognitive decline in a mouse model of tauopathy. Brain. 2017;140(1):184–200.
Rosenzweig N, Dvir-Szternfeld R, Tsitsou-Kampeli A, Keren-Shaul H, Ben-Yehuda H, Weill-Raynal P, Cahalon L, Kertser A, Baruch K, Amit I, et al. PD-1/PD-L1 checkpoint blockade harnesses monocyte-derived macrophages to combat cognitive impairment in a tauopathy mouse model. Nat Commun. 2019;10(1):465.
Baruch K, Deczkowska A, Rosenzweig N, Tsitsou-Kampeli A, Sharif AM, Matcovitch-Natan O, Kertser A, David E, Amit I, Schwartz M. PD-1 immune checkpoint blockade reduces pathology and improves memory in mouse models of Alzheimer’s disease. Nat Med. 2016;22(2):135–7.
Weng NP, Akbar AN, Goronzy J. CD28(-) T cells: their role in the age-associated decline of immune function. Trends Immunol. 2009;30(7):306–12.
Verma K, Ogonek J, Varanasi PR, Luther S, Bunting I, Thomay K, Behrens YL, Mischak-Weissinger E, Hambach L. Human CD8 + CD57- TEMRA cells: too young to be called old. PLoS ONE. 2017;12(5):e0177405.
Derhovanessian E, Maier AB, Hahnel K, Beck R, de Craen AJM, Slagboom EP, Westendorp RGJ, Pawelec G. Infection with cytomegalovirus but not herpes simplex virus induces the accumulation of late-differentiated CD4 + and CD8 + T-cells in humans. J Gen Virol. 2011;92(Pt 12):2746–56.
Wertheimer AM, Bennett MS, Park B, Uhrlaub JL, Martinez C, Pulko V, Currier NL, Nikolich-Zugich D, Kaye J, Nikolich-Zugich J. Aging and cytomegalovirus infection differentially and jointly affect distinct circulating T cell subsets in humans. J Immunol. 2014;192(5):2143–55.
Carbone I, Lazzarotto T, Ianni M, Porcellini E, Forti P, Masliah E, Gabrielli L, Licastro F. Herpes virus in Alzheimer’s disease: relation to progression of the disease. Neurobiol Aging. 2014;35(1):122–9.
Lovheim H, Olsson J, Weidung B, Johansson A, Eriksson S, Hallmans G, Elgh F. Interaction between cytomegalovirus and Herpes Simplex Virus Type 1 Associated with the risk of Alzheimer’s Disease Development. J Alzheimers Dis. 2018;61(3):939–45.
Turney IC, Lao PJ, Rentería MA, Igwe KC, Berroa J, Rivera A, Benavides A, Morales CD, Rizvi B, Schupf N, et al. Brain aging among racially and ethnically diverse middle-aged and older adults. JAMA Neurol. 2023;80(1):73–81.
Butts B, Huang H, Hu WT, Kehoe PG, Miners JS, Verble DD, Zetterberg H, Zhao L, Trotti LM, Benameur K, et al. sPDGFRβ and neuroinflammation are associated with AD biomarkers and differ by race. The ASCEND Study. Alzheimer’s & Dementia; 2023.
Acknowledgements
Our sincere thanks go out to all the research participants and their families. Illustrations were created using BioRender.com. We would like to thank Tiffany L. Sudduth with her help with the plasma biomarker data.
Funding
National Institutes of Health grant: P30GM127211 (ADB, BSN), T32AG057461 (JL, LVE), P30AG072946 (ADB, BSN, GAJ, DMW), UF1NS125488 (DMW, GAJ), R56AG069685 (BSN), R56AG074613 (AMS), and AHA 19EIA34760279 (AMS).
Author information
Authors and Affiliations
Contributions
EW and ADB conceptualized the study, performed the data analysis, prepared the figures, and wrote the manuscript. EW, JL, BJM, DMW, and GAJ completed experiments and/or were involved in recruitment and evaluation of study participants. BSN and AMW contributed to the design and interpretation of the results and participated in drafting the manuscript. All authors have read, given final approval of the version to be published, and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Winford, E., Lutshumba, J., Martin, B.J. et al. Terminally differentiated effector memory T cells associate with cognitive and AD-related biomarkers in an aging-based community cohort. Immun Ageing 21, 36 (2024). https://doi.org/10.1186/s12979-024-00443-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12979-024-00443-2