Abstract
Background
Cervical cancer is ranked as the second most common cancer in India. This study aims to assess the cervical cancer burden at the national and subnational level in India, projecting it for the year 2025 in terms of years of life lost (YLLs), years lived with disability (YLDs), and disability-adjusted life years (DALYs).
Methods
Twenty-eight population based cancer registries within the National Cancer Registry Programme network contributed cancer incidence and mortality data for this analysis. The DisMod-II tool, WHO lifetables, disability weights, mortality to incidence ratio, sample registration system, and census data were used to estimate the burden of cervical cancer. The projection estimates for 2025 were performed using a negative binomial regression model.
Results
In 2016, the cervical cancer burden in India was 223.8 DALYs per 100,000 women. The highest age-standardised DALYs were found in the northeast region (290.1 DALYs per 100,000 women) and the lowest in the eastern region (156.1 DALYs per 100,000 women). The states of Mizoram, Arunachal Pradesh, Karnataka, and Nagaland had a higher cervical cancer burden with DALYs exceeding 300 per 100,000 women. The projected cervical cancer burden for India in 2025 was estimated to be 1.5 million DALYs.
Conclusions
The study has found a significant cervical cancer burden across the regions of India, providing a baseline for monitoring impact of actions. Enhancing awareness of cervical cancer, advocating for the significance of screening, and promoting HPV vaccination among adolescents, families, and communities through informative communication campaigns are essential steps in managing and ultimately eliminating cervical cancer in India.
Similar content being viewed by others
Background
Cervical cancer ranks fourth among the most commonly diagnosed cancers as well as the fourth leading cause of cancer mortality in women globally [1]. In 2020, there were an estimated 604,127 cases and 341,831 deaths attributed to cervical cancer. The standardised incidence rates were 13.3 cases per 100,000 women-years and 7.3 deaths per 100,000 women-years. Cervical cancer leads as the most frequently occurring cancer in 23 out of 185 countries and the second most common in 67 countries. In terms of cancer-related deaths, cervical cancer tops the list as the primary cause in 36 countries and is the second most common cause of cancer-related deaths in 49 countries [2].
Of all new cases and deaths worldwide in 2020, India accounted for approximately one-fifth of new cases and nearly one-fourth of deaths due to cervical cancer, making it a major contributor to the global burden of cervical cancer. In India, cervical cancer is the second most common cancer in both incidence (18.3%) and cancer mortality (18.7%) among women in 2020, with a 5-year prevalence of 18.8% [3].
Global cancer statistics shows a decline in the age-standardised incidence rates, deaths, and disability-adjusted life years (DALYs) associated with cervical cancer from 1990 to 2019. However, despite this improvement, cervical cancer remains a significant health concern due to its persistently high absolute numbers of patients [4]. In line with the global trend, India has also witnessed a reduction in the age-standardised incidence and mortality rates of cervical cancer during this period (-21.32% and -32.29%, respectively). However, this declining trend has not been uniform across all states in India. Additionally, the progress in reducing cancer-related premature mortality by only 11.5% between 2015 and 2030 doesn't meet the Sustainable Development Goals' aim of a one-third reduction. This suggests that we are falling short of the target for reducing premature cancer deaths [5]. The variation in the magnitude and significance of this decline underscores the need for assessing the burden of cervical cancer at the regional and state levels [6].
Several factors, such as improved literacy rates, delayed age at marriage, first sexual intercourse and first childbirth, low parity, increased use of contraception, improved menstrual hygiene, and decreased tobacco use among women, have played a significant role in the decline of cervical cancer burden in India [7]. Screening for cervical cancer in India has been implemented through the National Programme for Prevention and Control of Non-Communicable Diseases [NP-NCD] since 2010 [8]. However, the coverage has been extremely poor, with only 1.2% of women aged 15–49 ever having been screened for cervical cancer [9]. Another nationally representative study found that 2.2% of women between the ages of 30–69 reported having undergone cervical cancer screening, with a 3.0% difference between women who were screened in urban (4.0%) and rural (1.3%) areas [10]. India is directing efforts toward the elimination of cervical cancer (a threshold of 4 per 100,000 women-year) by 2030, by focusing on the World Health Organisation strategy of Human Papillomavirus (HPV) vaccination for 90% of adolescent girls, screening 70% of women aged 35 and 45, and treating 90% of pre-cancerous and cancerous women [11]. Furthermore, while several national and state-specific public health insurance schemes are available, they are limited in coverage and fail to protect patients from catastrophic health expenditures [12].
The efforts to estimate the burden of cancer in India, utilizing reliable Population Based Cancer Registry (PBCR) data through simple and replicable methods, were undertaken [13, 14]. The burden of cancer in India was estimated to be 26.7 million DALYs in 2021, with cervical cancer contributing 8.2% to this estimate [13]. This study aimed to determine the extent of the cervical cancer burden across different states in India, with a specific focus on estimating the years of life lost (YLLs), years lived with disability (YLDs), and disability-adjusted life years (DALYs). Additionally, the study aimed to project this burden for the year 2025, to provide a more comprehensive understanding of the current and future impact of cervical cancer on the population.
Methods
Population based cancer registries (PBCRs) under the National Cancer Registry Programme (NCRP) are long-term cancer registries that have provided reliable and consistent cancer burden estimates in the country since 1981. In 2016, there were 28 PBCRs covering 10% of the total population of India, with 3.5% of them being rural, 42.9% being urban, and 53.6% being semi-urban. This study utilised the cervical cancer incidence and mortality data for women of different age groups obtained from 28 different PBCRs under the NCRP in the country [15,16,17].
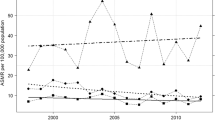
The cervical cancer incidence and mortality were ascertained by the International Classification of Disease (ICD) -10 code “C53” [18]. The level of registration of mortality is low, ranging between 35% and 100% across the states in India [19]. To account for underreported mortality in the country, we searched for the available evidence on the reported mortality to incidence (MI) ratio in India. Two national-level studies were identified, with average MI ratios for cancer of 35.0% and 75.4% [20, 21]. All longitudinal data points with reported MI ratios of 35.0% or higher for cervical cancer from PBCRs between 2005 and 2016 were extracted to estimate an adjusted MI ratio for cervical cancer among Indian women. Gamma distribution was identified as the best fit to the data based on Akaike’s information criteria and Bayesian information criteria (R software, version 4.1.2, R Core Team, Vienna, Austria) (Additional figure 1).
The Markov Chain Monte Carlo(MCMC) method, specifically implemented using STATA 14.2 by StataCorp in College Station, Texas, USA, was employed to estimate a mean MI ratio of 52.5%. This estimation was derived from a dataset consisting of 55 data points, all of which had MI ratios equal to or exceeding 35.0%. The MCMC process involved 10,000 iterations, ensuring convergence for accurate and reliable results. For registries with a reported MI ratio less than 52.5%, the MI ratio was replaced with 52.5% to calculate adjusted mortality numbers for further analysis and burden estimation.
The populations by age for the years 2012 to 2016 were projected for the 28 states and 2 union territories using the difference distribution method, based on data from the 2001 and 2011 Census of India [22]. (Additional Table 1). The cervical cancer incidence and mortality rates were calculated for quinquennial age groups. The incidence rate for a specific age group was calculated by dividing the number of newly diagnosed cervical cancer cases in a given year by the corresponding mid-year population. Similarly, the mortality rate for a particular group was calculated by dividing the number of cervical cancer deaths in a given year (adjusted) by the corresponding mid-year population. Age-specific all-cause mortality for women during 2012–2016 was obtained from the Sample Registration System, Office of the Registrar General of India [23]. The cancer prevalence was estimated using the DISMOD II tool, incorporating input data such as cancer incidence, cause-specific mortality, mortality-incidence ratio, all-cause mortality, and population information [24].
The regional grouping used in the earlier analysis was utilised for this analysis for uniformity [13]. For the regions where PBCRs already existed, those data sources were used, and for the regions where there weren't any or there weren't enough data, the data from the closest PBCRs were used.
Estimation of the burden
The burden of cervical cancer was estimated and reported for each state and region in terms of YLLs, YLDs, and DALYs per 100,000 populations, using the available national cancer registry programme data. YLLs were calculated by multiplying the total number of cervical cancer deaths in a specific age group by the standard life expectancy of that age group. The standard life expectancies of different age groups were obtained from the WHO standard life tables (Additional Table 2). YLDs were estimated by multiplying the total number of prevalent cervical cancer cases in respective five-year age groups by a disability weight of 0.451, which is specific to metastatic cancer according to the Global Burden of Disease Study, 2019 [25]. The sum of the estimated YLLs and YLDs provided the DALY metrics. The burden metrics (YLLs, YLDs, and DALYs) were age standardised using the WHO World Population Standard distribution 2000–2025 [26]. Furthermore, using the available sex and age-specific cancer incidence and estimated mortality information from 2001 to 2016, the cervical cancer burden metrics were projected for 2025. Negative binomial regression was used for prediction as the conditional mean of the burden metrics was less than the conditional variance using IBM SPSS software (Version 27.0; IBM Corp., Armonk, NY, USA).
Data availability statement
The data generated in this study is available within the article. The corresponding author can be contacted at director-ncdir@icmr.gov.in for further clarification if required.
Results
In 2016, the burden of cervical cancer in India was 223.8 DALYs per 100,000 women, with variations across different regions (Table 1, Fig. 1). The highest burden of cervical cancer was found in the northeast region (290.1 DALYs per 100,000 women), followed by the central and northern regions (276.9 and 276.7 DALYs per 100,000 women, respectively). The eastern region had the lowest age-standardised DALYs (156.1 DALYs per 100,000 women). The age group wise percentage distribution of the cervical cancer burden (including age standardised YLLs, YLDs, and DALYs) by region was presented in Additional Table 3.
Across the states and UTs, Mizoram had the highest DALYs (559.6 per 100,000 women), followed by Arunachal Pradesh (380.3 per 100,000 women) and Karnataka (359.1 per 100,000 women). Kerala had the lowest burden with 115.2 DALYs per 100,000 women, followed by Manipur (139.5 DALYs per 100,000 women) and Gujarat (149.6 DALYs per 100,000 women) (Table 1, Fig. 2).
A similar pattern was observed in terms of YLDs and YLLs. Mizoram, Karnataka, Arunachal Pradesh, and Nagaland had the highest YLLs, while Kerala and Manipur had the lowest YLLs. Notably, Arunachal Pradesh had a significantly high burden of disability due to cervical cancer, with 48.0 YLDs per 100,000 women. The age group wise percentage distribution of the cervical cancer burden (age-standardised YLLs, YLDs, and DALYs) was presented in Additional Fig. 2a, b, c. The burden of cervical cancer increased with age and peaked in the age group of 65 to 69 years, with about 60% of the burden experienced by women between 50 and 74 years of age.
Table 2 provides information on the wise crude and age-standardised incidence rates, mortality rates, YLLs, YLDs, and DALYs by registry. In 2016, the crude cervical cancer incidence was reported highest in the Mizoram state PBCR with 19.7 cases per 100,000 women, followed by Barshi rural (17.0 per 100,000 women), Pasighat (16.3 per 100,000 women), Chennai (15.7 per 100,000 women), and Bangalore (15.5 per 100,000 women) registries. However, after age standardisation (for World Standard Population), the incidence rate for Mizoram state increased to 25.2 per 100,000 women. The age-standardised mortality rate due to cervical cancer exceeded 10 per 100,000 women in Pasighat, Bangalore, Mizoram state, and Barshi rural registries after accounting for under-reporting of mortality. The national average age-standardised rates of incidence and mortality for cervical cancer were 12.1 and 6.6 per 100,000 women, respectively.
The projected burden of cervical cancer in India for 2025 was estimated to be 1.5 million DALYs, with 1.4 million DALYs contributed by YLLs. This projection indicated a downward trend, with a 3.4% reduction in the cervical cancer burden in India from 2021 to 2025 (Table 3).
Discussion
This study examined the burden of cervical cancer in India and its states for 2016, analysing data from various population based cancer registries within the National Cancer Registry Programme network. The age-standardised incidence rate of cervical cancer in India for 2016 was estimated at 12.1 per 100,000 women, and the DALYs were 223.8 DALYs per 100,000 women. The highest age standardised DALYs were observed in the northeast region (290.1 DALYs per 100,000 women), while the lowest were found in the eastern region (156.1 DALYs per 100,000 women). The states of Mizoram, Karnataka, Nagaland, and Arunachal Pradesh had a higher total cervical cancer burden, with DALYs exceeding 300 per 100,000 women. The age standardised DALYs were lowest in Kerala (115.2 DALYs per 100,000 women). The burden of cervical cancer in India was projected to be 1.5 million DALYs in 2025, indicating a 3.4% decline from the year 2021.
The age standardised incidence rate of cervical cancer estimated in this study is consistent with the estimates provided using the Global Burden of Disease (GBD) data, as reported by Singh et al. [6]. While the rankings of states differed between the current study and the GBD study, several states, including Mizoram, Karnataka, Tamil Nadu, Arunachal Pradesh, and Maharashtra, exhibited high incidence and mortality in both studies.
This study explored the regional variations in the burden of cervical cancer in India. The central and northeastern regions, which are comparatively less advanced (in terms of the Human Development Index (Additional Table 4)) when compared to the southern and western regions, demonstrated a higher burden of cervical cancer in terms of DALYs [27]. Other studies have also observed intra-country variation in cervical cancer burden and related cancer risk factors, which is associated with the socioeconomic status of the country [4, 28, 29].
Social changes, economic development, demographic transition, and an improved lifestyle were associated with the control of cervical cancer in high-income countries [30]. An increase in the female literacy rate, along with improvements in reproductive factors, including an increase in the age of marriage, age at first pregnancy, contraception use, and sexual practices, have been cited as reasons for the decreasing cervical cancer burden in India [10, 31]. According to the National Family Health Survey-5 (NFHS-5), 31.8% of women aged 20- 24 years in Assam reported being married before their 18 years of age, while the corresponding figure in Kerala was 6.3% [9]. Among cervical cancer cases in India, the prevalence of HPV infection was high, ranging from 87.8% to 96.7% [32]. Early marriage or early age at first intercourse can increase the risk of HPV infection, slowly progressing to cancer in a substantial number of women [4]. Implementation of the national family planning program and Mission Pariwar Vikas under the National Health Mission has increased accessibility to contraceptives and family planning services, contributing to fertility rates of less than 2 in the Indian population [33].
Another potential reason for the higher cervical cancer burden in the northeastern states could be related to unsafe sexual practices. The top three states with the highest HIV infection rates in India are located in the northeastern region, with Mizoram having the highest rate at 2.32% [34]. Mizoram has also been noted to have the highest cervical cancer burden in our study, which adds evidence to the above-cited reason [35]. The downward trend in cervical cancer burden projections reflects findings from other studies, both globally and nationally [4, 36].
Using a modelling approach, vaccination with a single dose and catch-up was found to be more impactful in preventing cervical cancer in India [37]. The recent recommendation by the National Technical Advisory Group for Immunization to include HPV vaccination in the universal immunization programme for adolescent girls of age 9- 14 years, with a one-time catch-up, is a step forward in cervical cancer control in India [38]. With the current 2% screening coverage, India has to improve the screening coverage by 35.0 times to achieve the target of 70% screening coverage [39]. Scaling up HPV vaccination with 90% coverage and two lifetime screenings will lead to the elimination of cervical cancer in India by approximately 2070 [40]. Concerted efforts to increase awareness of HPV vaccination, screening, and cervical cancer among the community and provide adequate training, logistics, and infrastructure to the health system for screening, referral, and follow-up will contribute to the prevention, control, and eventual elimination of cervical cancer in India.
Strengths and limitations
This study reports the burden of cervical cancer in terms of YLDs, YLLs, and DALYs for each state and region in India, utilizing data from 28 population based cancer registries distributed across the country. The use of population-based registries ensures that almost 100% of incident cases in the target populations are captured, resulting in a more accurate estimation of the burden. However, it is important to note that vital registration systems in LMIC countries may only register a fraction of deaths, potentially leading to an underestimation of cause-specific deaths. To address this, the study calculated a national average MI ratio and adjusted the mortality figures to account for this under-registration, thus providing a more comprehensive and precise assessment of the burden of cervical cancer in India. Notably, the average MI ratio aligns with the five-year age-standardised relative survival of 51.7% estimated for cervical cancer patients in India, validating the methodology used for calculating the average MI ratio [41].
Although it was assumed that states within a particular region would have similar cervical cancer epidemiology, the availability of functioning cancer registries remains a significant limitation. Estimates for states without a registry were based on the nearest registry, but it's important to note that healthcare in India primarily falls under state responsibility. Consequently, screening rates and treatment effectiveness can vary even among states in the same region. Additionally, variations in socioeconomic development levels among states within a region can lead to differences in health-promoting behaviours among populations. Furthermore, most of the registries in this study are urban-based, which limits their ability to provide estimations segregated by urban and rural areas and hinders generalisability to the entire state.
Implications of practice and future research
Cervical cancer is a global target for disease elimination. Understanding the subnational level burden of cervical cancer and its projection will aid policymakers in surveillance towards the target as well as allocate resources for locally feasible interventions in high-burden areas. The findings from this study can serve as a baseline for future research on cervical cancer burden and trends in India, allowing for subnational comparisons. Further research can explore the impact of social and economic factors on cervical cancer burden, offering insights into strategies to address health inequities associated with cervical cancer.
Conclusion
The burden of cervical cancer in India is significant, with a higher burden in the central and northeastern regions of the country. These findings emphasize the urgent need to scale up cervical cancer screening and prevention efforts nationwide. Increasing awareness about cervical cancer and promoting the importance of screening and HPV vaccination among adolescents, families, and communities through targeted information, education, and communication campaigns will aid in controlling and eliminating cervical cancer in India. By prioritizing these efforts, India can make significant strides towards reducing the cervical cancer burden and realizing the goal of elimination.
Availability of data and materials
The study used secondary data sources for the analysis and are available upon request from the corresponding author.
References
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin. 2021;71(3):209–49.
Global Cancer Observatory: Cancer Today. Lyon, France: International Agency for Research on Cancer. 2020. Available from: https://gco.iarc.fr/today. Cited 2023 Mar 7
Singh D, Vignat J, Lorenzoni V, Eslahi M, Ginsburg O, Lauby-Secretan B, et al. Global estimates of incidence and mortality of cervical cancer in 2020: a baseline analysis of the WHO Global Cervical Cancer Elimination Initiative. Lancet Glob Health. 2023;11(2):e197–206.
Zhang X, Zeng Q, Cai W, Ruan W. Trends of cervical cancer at global, regional, and national level: data from the Global Burden of Disease study 2019. BMC Public Health. 2021;21(1):894.
Kulothungan V, Ramamoorthy T, Mohan R, Mathur P. Assessing progress of India in reduction of premature mortality due to four noncommunicable diseases towards achieving the WHO 25_25 goal and the sustainable development goals. Sustainable Development. 2023;1–11. https://doi.org/10.1002/sd.2761
Singh M, Jha RP, Shri N, Bhattacharyya K, Patel P, Dhamnetiya D, et al. Secular trends in incidence and mortality of cervical cancer in India and its states, 1990–2019: data from the Global Burden of Disease 2019 Study. BMC Cancer. 2022;22(1):149.
Bhatla N, Meena J, Kumari S, Banerjee D, Singh P, Natarajan J, et al. Cervical cancer prevention efforts in India. Indian J Gynecol Oncol. 2021;19(3):41.
Banerjee B. National Programme for Prevention and Control of Cancer, Diabetes, Cardiovascular Diseases and Stroke (NPCDCS). In: DK Taneja’s Health Policies and Programmes in India. Jaypee Brothers Medical Publishers (P) Ltd.; 2017. p. 429–429.
International Institute for Population Sciences (IIPS) and ICF. 2021. National Family Health Survey (NFHS-5), 2019–21: India: Volume 2022. Available from: https://dhsprogram.com/pubs/pdf/FR375/FR375.pdf. Cited 2023 Feb 14.
Indian Council of Medical Research – National Centre for Disease Informatics and Research. National Noncommunicable Disease Monitoring Survey(NNMS) 2017–18.2020. Available from: https://www.ncdirindia.org/nnms/. Cited 2023 Feb 14.
World Health Organization. Draft: global strategy towards the elimination of cervical cancer as a public health problem.2019. Available from: https://www.who.int/publications/m/item/draft-global-strategy-towards-eliminating-cervical-cancer-as-a-public-health-problem. Cited: 2022 Mar 5.
Singh MP, Chauhan AS, Rai B, Ghoshal S, Prinja S. Cost of treatment for cervical cancer in India. Asian Pac J Cancer Prev. 2020;21(9):2639–46.
Kulothungan V, Sathishkumar K, Leburu S, Ramamoorthy T, Stephen S, Basavarajappa D, et al. Burden of cancers in India - estimates of cancer crude incidence, YLLs, YLDs and DALYs for 2021 and 2025 based on National Cancer Registry Program. BMC Cancer. 2022;22(1):527.
Kulothungan V, Ramamoorthy T, Sathishkumar K, et al. Burden of female breast cancer in India: estimates of YLDs, YLLs, and DALYs at national and subnational levels based on the national cancer registry programme. Breast Cancer Res Treat. 2024. https://doi.org/10.1007/s10549-024-07264-3.
Indian Council of Medical Research – National Centre for Disease Informatics and Research. Report of National Cancer Registry Programme (2012–2016).2020. Available from: https://www.ncdirindia.org/All_Reports/Report_2020/resources/NCRP_2020_2012_16.pdf. Cited 2023 Mar 27.
Sathishkumar K, Chaturvedi M, Das P, Stephen S, Mathur P. Cancer incidence estimates for 2022 & projection for 2025: Result from National Cancer Registry Programme, India. Indian J Med Res. 2022;156(4&5):598–607.
Chaturvedi M, Sathishkumar K, Lakshminarayana SK, Nath A, Das P, Mathur P. Women cancers in India: Incidence, trends and their clinical extent from the National Cancer Registry Programme. Cancer Epidemiol. 2022;80:102248.
World Health Organisation. WHO methods and data sources for global burden of disease estimates 2000 – 2019.2020. Available from: https://cdn.who.int/media/docs/default-source/gho-documents/global-health-estimates/ghe2019_daly-methods.pdf. Cited 2023 Mar 14.
Kumar GA, Dandona L, Dandona R. Completeness of death registration in the Civil Registration System, India (2005 to 2015). Indian J Med Res. 2019;149(6):740–7. https://doi.org/10.4103/ijmr.IJMR_1620_17.
Parkin DM, Bray F. Evaluation of data quality in the cancer registry: principles and methods Part II. Completeness. Eur J Cancer (Oxford, England: 1990). 2009;45(5):756–64.
Dhillon PK, Mathur P, Nandakumar A, Fitzmaurice C, Kumar GA, Mehrotra R, et al. The burden of cancers and their variations across the states of India: the Global Burden of Disease Study 1990–2016. Lancet Oncol. 2018;19(10):1289–306.
Office of the Registrar General & Census Commissioner, India. Ministry of Home Affairs, Government of India. Available from: https://censusindia.gov.in/. Cited 2023 Mar 14.
Office of the Registrar General & Census Commissioner, India. Ministry of Home Affairs, Government of India. SRS Statistical Report. Available from: https://censusindia.gov.in/vital_statistics/SRS_Statistical_Report.html. Cited 2023 Mar 27.
Barendregt JJ, Van Oortmarssen GJ, Vos T, Murray CJ. A generic model for the assessment of disease epidemiology: the computational basis of DisMod II. Popul Health Metrics. 2003;1(1):4.
Institute for Health Metrics and Evaluation (IHME). Global Burden of Disease Study 2019 (GBD 2019) Disability Weights. 2020. https://doi.org/10.6069/1W19-VX76. Cited 2023 Mar 14.
Ahmad OB, Pinto CB, Lopez AD, Murray CJL , Lozano R, Inoue M. Age standardization of rates: a new WHO standard. Geneva: World Health Organization 2001;9(10):1–4.
Global Data Lab. Sub-national HDI (v5.0). Available from: https://globaldatalab.org/shdi/table/shdi/IND/?levels=1+4&years=2019&extrapolation=0. Cited 2022 Dec 10.
Ramamoorthy T, Leburu S, Kulothungan V, Mathur P. Regional estimates of noncommunicable diseases associated risk factors among adults in India: results from National Noncommunicable Disease Monitoring Survey. BMC Public Health. 2022;22:1069.
Seenappa K, Kulothungan V, Mohan R, Mathur P. District-Wise Heterogeneity in Blood Pressure Measurements, Prehypertension, Raised Blood Pressure, and Their Determinants Among Indians: National Family Health Survey-5. Int J Public Health. 2024;69. https://doi.org/10.3389/ijph.2024.1606766
Soerjomataram I, Bray F. Planning for tomorrow: global cancer incidence and the role of prevention 2020–2070. Nat Rev Clin Oncol. 2021;18(10):663–72.
Dhillon PK, Yeole BB, Dikshit R, Kurkure AP, Bray F. Trends in breast, ovarian and cervical cancer incidence in Mumbai, India over a 30-year period, 1976–2005: an age–period–cohort analysis. Br J Cancer. 2011;105(5):723–30.
Sreedevi A, Javed R, Dinesh A. Epidemiology of cervical cancer with special focus on India. Int J Women’s Health. 2015;7:405–14.
Department of Health and Family Welfare. Ministry of Health and Family Welfare, Government of India. Annual Report 2015–16.2016. Available from: https://main.mohfw.gov.in/sites/default/files/56325632145668965478.pdf. Cited 2023 Mar 3.
National AIDS Control Organisation. Ministry of Health & Family Welfare. Government of India. HIV Facts & Figures. Available from: http://naco.gov.in/hiv-facts-figures. Cited 2022 Dec 6.
Ramamoorthy T, Sathishkumar K, Das P, Sudarshan KL, Mathur P. Epidemiology of human papillomavirus related cancers in India: findings from the National Cancer Registry Programme. Ecancermedicalscience. 2022;7(16):1444. https://doi.org/10.3332/ecancer.2022.1444. PMID:36405943;PMCID:PMC9666279.
Sathishkumar K, Vinodh N, Badwe RA, Deo SVS, Manoharan N, Malik R, et al. Trends in breast and cervical cancer in India under National Cancer Registry Programme: An Age-Period-Cohort analysis. Cancer Epidemiol. 2021;74:101982.
Man I, Georges D, de Carvalho TM, Ray Saraswati L, Bhandari P, Kataria I, et al. Evidence-based impact projections of single-dose human papillomavirus vaccination in India: a modelling study. Lancet Oncol. 2022;23(11):1419–29.
Press Information Bureau. Government of India. Centre urges States to create awareness and take steps for prevention of cervical cancer among girl students. Available from: https://pib.gov.in/PressReleseDetailm.aspx?PRID=1885597. Cited 2023 Feb 22.
Bruni L, Serrano B, Roura E, Alemany L, Cowan M, Herrero R, et al. Cervical cancer screening programmes and age-specific coverage estimates for 202 countries and territories worldwide: a review and synthetic analysis. Lancet Glob Health. 2022;10(8):e1115–27.
Brisson M, Kim JJ, Canfell K, Drolet M, Gingras G, Burger EA, et al. Impact of HPV vaccination and cervical screening on cervical cancer elimination: a comparative modelling analysis in 78 low-income and lower-middle-income countries. Lancet. 2020;395(10224):575–90.
Sathishkumar K, Sankarapillai J, Mathew A , Nair R A, Gangane N, Khuraijam S, et al. Survival of patients with cervical cancer in India – findings from 11 population based cancer registries under National Cancer Registry Programme. Lancet Regional Health Southeast Asia. 2023;100296. https://doi.org/10.1016/j.lansea.2023.100296 Published: October 13, 2023.
Funding
None.
Author information
Authors and Affiliations
Contributions
TR, VK and PM designed the study and oversaw the research. TR, PM and VK developed the concept and drafted the manuscript. TR, VK, RM, NT prepared the tables and figures. TR, VK, SK, RM, NT and SB checked pooled data for accuracy, contributed to data preparation and analysis. TR, VK, RM, NT and SB reviewed the results. Authors TR and VK performed statistical modelling and finalized the results. Authors TR, PM, VK, SK and SB reviewed all versions of the manuscript. TR, VK, and PM finalized the manuscript. All authors reviewed and agreed to the contents of the finalized manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All the data comes from secondary, unidentifiable records. The methods performed were in accordance with the relevant guidelines and regulations. The study has been approved by the Institutional Ethics Committee at ICMR-NCDIR, Bengaluru. The approval number is NCDIR/IEC/3020/2020.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Ramamoorthy, T., Kulothungan, V., Sathishkumar, K. et al. Burden of cervical cancer in India: estimates of years of life lost, years lived with disability and disability adjusted life years at national and subnational levels using the National Cancer Registry Programme data. Reprod Health 21, 111 (2024). https://doi.org/10.1186/s12978-024-01837-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12978-024-01837-7