Abstract
Background
Low use of modern methods of contraception has been linked to HIV seropositivity and to migration, but few studies have evaluated the intersection of both risk factors with contraceptive use.
Methods
We analyzed cross-sectional data from sexually active female participants aged 15 to 49 years in the Rakai Community Cohort Study (RCCS) between 2011 and 2013. The RCCS is an open population-based census and individual survey in south-central Uganda. Recent in-migrants (arrival within approximately 1.5 years) into RCCS communities were identified at time of household census. The primary outcome was unsatisfied demand for a modern contraceptive method (injectable, oral pill, implant, or condom), which was defined as non-use of a modern contraceptive method among female participants who did not want to become pregnant in the next 12 months. Poisson regression models with robust variance estimators were used to identify associations and interactions between recent migration and HIV serostatus on unsatisfied contraceptive demand.
Results
There were 3,417 sexually active participants with no intention of becoming pregnant in the next year. The mean age was 30 (± 8) years, and 17.3% (n = 591) were living with HIV. Overall, 43.9% (n = 1,500) were not using any modern contraceptive method. Recent in-migrants were somewhat more likely to have unsatisfied contraceptive demand as compared to long-term residents (adjusted prevalence risk ratio [adjPRR] = 1.14; 95% confidence interval [95%CI]: 1.02–1.27), whereas participants living with HIV were less likely to have unsatisfied contraceptive demand relative to HIV-seronegative participants (adjPRR = 0.80; 95%CI = 0.70–0.90). When stratifying on migration and HIV serostatus, we observed the highest levels of unsatisfied contraceptive demand among in-migrants living with HIV (48.7%); however, in regression analyses, interaction terms between migration and HIV serostatus were not statistically significant.
Conclusions
Unsatisfied contraceptive demand was high in this rural Ugandan setting. Being an in-migrant, particularly among those living with HIV, was associated with higher unsatisfied contraceptive demand.
Plain English summary
Through a cross-sectional study, we explored the relationship between HIV status, migration, and contraceptive use among sexually active women of reproductive age in rural south-central Uganda. People who had moved into the study area within the last 1.5 years were considered in-migrants, compared to long-term residents i.e. people who had not moved. We examined unsatisfied demand for a modern contraceptive method, which is to say female participants who did not want to become pregnant in the next 12 months and were not using at least one of the following contraceptive methods: injectable, oral pill, implant, or condom. We included 3,417 sexually active female participants with no intention of becoming pregnant in the next year. The average age of these women was 30 years, less than 20% were living with HIV, and almost half were not using any modern contraceptive methods. Recent in-migrants were somewhat more likely to have unsatisfied contraceptive demand as compared to long-term residents, whereas participants living with HIV were less likely to have unsatisfied contraceptive demand relative to HIV-negative participants. Being an in-migrant, particularly among those living with HIV, was associated with higher unsatisfied contraceptive demand. This study shows the need for integrating contraceptive and HIV services for mobile populations in East Africa.
Similar content being viewed by others
Background
Addressing women’s demand for contraceptive services can prevent unintended pregnancies [1, 2] and reduce mother-to-child HIV transmission among women living with HIV [3]. In recognition of the importance of contraception as a sexual and reproductive health intervention, total demand satisfied by a modern contraceptive method (the percentage of women 15–49 years who are currently using a modern method of contraception among those who wish to prevent or delay pregnancy), was included in the Sustainable Development Goals, with the goal of satisfying 75% of demand by 2035 [4]. Despite this ambitious goal, much work remains. Family Planning 2030 recently estimated that 19.7% of all women in sub-Saharan Africa as of 2022 have unmet need for contraception [5] – that is, they state a desire to delay or prevent pregnancy but are not using a method of contraception. Recent research highlights persistent equity gaps in meeting demand for contraceptive services across sub-Saharan Africa [6]. While equity gaps have been documented across multiple sociodemographic characteristics, including age, wealth, and education status [6,7,8,9], there are relatively fewer studies evaluating how demand satisfied varies by migration status or among women living with HIV.
Demand satisfied with a modern method is increasingly recognized as a better measure to track progress towards meeting contraceptive targets than prevalence estimates of unmet need or contraceptive use, as estimates of both unmet need and the contraceptive prevalence rate generally include women who are not at risk for unintended pregnancy (e.g., women who are pregnant or who are not sexually active) in the denominator; in contrast, demand satisfied is specific to sexually-active women who wish to delay or prevent childbearing and, thus, provides a better measure of the ability of contraceptive programs to meet the needs of women who may benefit from the use of contraception based on their sexual activity and fertility intentions [6, 10]. These considerations are particularly pertinent among women living with HIV, as HIV status has been demonstrated to affect fertility intentions [11, 12], and in turn, demand for contraception. HIV-positive serostatus has been linked to greater unmet need for contraception in multiple settings across the African continent [13,14,15,16], although many of these prior studies employ facility-based samples that limit generalizability to the broader population and were conducted before widespread availability of antiretroviral therapy (ART) [16]. Since the early 2000s, access to ART has gradually increased in sub-Saharan Africa, resulting in higher levels of HIV viral load suppression among women living with HIV [17, 18]. ART scale-up has also occurred during a period of wide-spread commitment to improve access to contraceptive services [19], including among women living with HIV [20]. Little research, however, has explored whether improvements in access to services and increases in contraceptive use in the general population have resulted in improved equity in demand satisfied by HIV serostatus.
Additionally, prior research has shown that migration is a risk factor for HIV acquisition [21, 22] and that women living with HIV are more likely to migrate [23, 24]. Migration can also affect contraceptive need by changing (either increasing or decreasing) sexual exposure between partners through absence from home [25, 26], and through exposing migrants to differing fertility norms [27], or changing opportunities and access to contraceptive services [28]. However, the relationship between contraceptive behavior for contraception and migration is complex and depends in part on both a migrant’s place of origin and destination. For example, one cross-sectional study conducted in Zambia found significantly greater likelihood of experiencing unmet need for contraception among rural non-migrants compared to urban non-migrants and rural-to-rural migrants, but not other groups (i.e. urban-to-rural migrants, urban-to-urban migrants, rural-to-urban migrants) [29]. Another cross-sectional study in Ethiopia found that unmet need for contraception was significantly lower among rural-to-urban migrants compared to rural non-migrants [30]. In both studies, however, the reference group included women who desired to have children, were pregnant, and/or were not sexually active. It is thus not possible to differentiate between the effect of inequitable access to and use of services or differences in fertility intentions and sexual behavior. Few studies have explored whether satisfied contraceptive demand, which addresses this limitation, differs between migrants and non-migrants despite the influence that migration may play on both the demand for contraception and ability of migrants to access health services. In addition to changes in contraceptive access, migration may also lead to interruption in continuity of care among women living with HIV [31], which may include their contraceptive services. HIV-associated stigma may also hinder migrating women living with HIV from accessing both HIV and contraceptive services at their place of destination [32]. Despite strong associations between migration and HIV, and the impact of both on use of contraceptive services, there is very limited research on how these factors interact to influence total demand satisfied by a contraceptive method among African women.
Here, we used data from the Rakai Community Cohort Study (RCCS) [18, 33] in south-central Uganda to assess contraceptive use patterns among sexually active women with no intention of getting pregnant in the next 12 months living with and without HIV. Our objective was to determine whether the relationship between a recent history of migration and demand satisfied varies by HIV serostatus. Given the large population of women living with HIV, increasing migration as countries urbanize, and the ongoing development of dual HIV prevention and contraceptive technologies, understanding the relationship between unsatisfied demand for contraception, migration, and HIV in sub-Saharan Africa is critical to effective delivery of integrated HIV and contraceptive services.
Methods
Study setting and population
For this cross-sectional study nested in a prospective cohort study, we used data from 30 rural agrarian and semi-urban trading communities under surveillance during the fifteenth survey round (R15) of the RCCS, collected between July 2011 and May 2013. The RCCS is a longitudinal open population-based household census and behavioral survey of persons aged 15 to 49 years in south-central Uganda conducted at approximately 18-month intervals. During the RCCS household census, data on in- and out-migration, births, and deaths is obtained [18, 22, 33]. Almost all the migrations are internal, as opposed to cross-border or international, migration. At the time of RCCS survey, data on participant demographics, sexual behaviors and partnerships, and health service utilization, including use of contraceptive methods, are obtained. Though the RCCS is currently ongoing, RCCS survey R15 was the most recent survey visit for which comprehensive data on fertility intention and contraceptive method use were obtained.
Exposure variables
Our primary exposure variables were migration and HIV serostatus. Migration status was a binary exposure variable with participants being classified as either a recent in-migrant or a long-term resident. A recent in-migrant was defined as a woman who moved into an RCCS study community after the most recent previous RCCS household census (RCCS R14, approximately 1.5-year interval between RCCS R14 and R15) with intention to stay in the community. In-migrants were identified at time of household census, which took place approximately 4 weeks before the RCCS survey. Conversely, long-term residents were defined as women with no recent history of migration over the preceding survey interval [22]. HIV serostatus was measured using a validated three-rapid-test (Determine, Stat Pak, and Unigold) algorithm on serum samples collected at time of RCCS survey and confirmed with enzyme-linked immunosorbent assays at the Rakai Health Sciences Program laboratories in Kalisizo, Uganda as previously described [34].
Primary outcome
Women were surveyed as to whether they were using any modern methods of contraception during the last 12 months. Specifically, they were queried, one by one, on whether they were currently using the following modern contraceptive methods: combined oral contraceptive pill, condom, Depo-Provera, intra-uterine device (IUD), implant, or bilateral tubal ligation. They were also asked if they had any intention of becoming pregnant in the next 12 months. Our primary outcome was unsatisfied demand for a modern contraceptive, which we defined as non-use of modern contraceptive method at the time of the survey among sexually active women in the RCCS with no intention of becoming pregnant in the next 12 months.
Statistical analysis
Women were classified into four groups: (1) HIV-seropositive and recent in-migrant, (2) HIV-seropositive and long-term resident, (3) HIV-seronegative and recent in-migrant, and (4) HIV-seronegative and long-term resident. For each of these four groups, we tabulated their frequency and percent of various sociodemographic characteristics: age (15–24, 25–34, 35–49 years), education level (primary or none, post-primary), marital status (never married, currently married, previously married), socio-economic status (SES: lowest, low-middle, high-middle, highest as determined using a locally validated scale) [35], religion (Muslim, Catholic, Protestant/Pentecostal, other), and occupation (agriculture/housework, non-agriculture (i.e. bar/restaurant/salon, trade/shopkeeper, government/teacher)) and current ART use (yes, no). We also assessed the comparability of these groups using the Chi-squared test.
We then tabulated the use of different types of contraceptive methods (including non-use of any modern methods) by migration and HIV serostatus. We also conducted sensitivity analysis excluding condoms, since condoms are a commonly used method of HIV prevention and tend to have lower efficacy for pregnancy prevention in our study setting as compared to other modern contraceptive methods [36, 37]. Further, we disaggregated unsatisfied contraceptive demand by age (15–24 years versus ≥ 25 years), since it previously has been associated with younger age among individuals living with HIV [16].
Poisson regression with robust variance was used to estimate unadjusted and adjusted prevalence risk ratios (PRR) and 95% confidence intervals (95% CI) of unsatisfied contraceptive demand by migration history and HIV serostatus. Based on our conceptual framework and prior literature review, we included the following as potential confounders in our multivariable model: age, education, marital status, socio-economic status, religion, and occupation. To assess for potential effect modification, we stratified analyses by HIV and migration status and included product (i.e., interaction) terms between HIV and migration status in regression models, which were considered statistically significant at an alpha significance level of 0.05. We also examined the association between unsatisfied contraceptive demand and ART use for the subset of women living with ART. All analyses were conducted using STATA (version BE17; College Station, Texas).
Ethical review
This study was approved by the Western Institutional Review Board and the Research Ethics Committee of the Uganda Virus Research Institute. The study received clearance from the Ugandan National Council for Science and Technology. All study participants provided written informed consent or assent/parental consent for participants aged less than 18 years old.
Results
There were 10,960 individuals residing in RCCS rural and semi-urban trading communities who participated in RCCS R15 including 6,083 women of whom 3,417 were sexually active and did not want to become pregnant in the next year. Of these 3,417 women, 2,346 (68.7%) were long-term residents who were HIV-seronegative, 476 (13.93%) were long-term residents living with HIV, 480 (14.1%) were recent in-migrants who were HIV-seronegative, and 115 (3.37%) were recent in-migrants living with HIV (Table 1). The majority were 25–34 years of age, currently married, and with some primary education. Women living with HIV tended to be older, less likely to be married, and have lower SES compared to women who were HIV-seronegative, while recent in-migrants tended to be younger and employed in occupations outside of agriculture and housework. Of those living with HIV, 54% reported current ART use, although levels of ART use were higher among long-term residents as compared to recent migrants living with HIV.
Table 2 shows the different methods of modern contraceptive use overall and stratified by migration history and HIV serostatus. Depo-Provera was the most commonly used modern contraceptive method (29.4%), followed by condoms (13.7%). Women living with HIV were more likely to report using condoms, irrespective of migration status. Overall, unsatisfied contraceptive demand was high, regardless of migration or HIV status. Recent in-migrants living with HIV had the highest levels of unsatisfied contraceptive demand (48.7%), while long-term residents living with HIV had the lowest levels of unsatisfied contraceptive demand (36.6%); however, lower levels of unsatisfied contraceptive demand observed among long-term residents living with HIV was entirely driven by condom use.
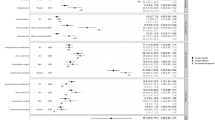
Figure 1 shows unsatisfied contraceptive demand by HIV, migration status, and by age. For younger women (< 25 years old), those living with HIV had the greatest levels of unsatisfied contraceptive demand; however, for older women (> = 25 years old), in-migrants had higher levels of unsatisfied contraceptive demand as compared to long-term residents. Overall, younger women tended to have higher unsatisfied contraceptive demand.
Table 3 shows unadjusted and adjusted associations between HIV and migration and unsatisfied contraceptive demand. Participants living with HIV were significantly less likely to have unsatisfied demand as compared to HIV-seronegative women (adjPRR = 0.80; 95% CI 0.70–0.90); however, the lower levels of unsatisfied demand among those living with HIV were entirely driven by higher levels of condom use in this group (Supplemental Table 1). Conversely, recent in-migrants had a 14% higher prevalence of unsatisfied contraceptive demand as compared to long-term residents (adjPRR = 1.14; 95% CI 1.02–1.27). There was some evidence of a positive interaction between HIV serostatus and recent migration, such that the impact of migration on unsatisfied contraceptive demand was greater among participants living with HIV; however, results were not statistically significant (interaction p-value = 0.096). Furthermore, among participants living with HIV, unsatisfied contraceptive demand was 35.2% among participants who self-reported ART use and 33.2% among those who did not. Older female age, lower SES, and agricultural work were all associated with higher levels of unsatisfied contraceptive demand in adjusted analyses.
Discussion
In this cross-sectional study assessing how the prevalence of non-use of contraception differed among recent in-migrants and long-term residents by HIV status in rural south-central Uganda, we observed that unsatisfied contraceptive demand among sexually active female participants with no intention of getting pregnant in the next year was 43.9% (including condoms, or 57.2% excluding condoms). We found that unsatisfied demand was significantly higher among recent in-migrants compared to long-term residents, and that women living with HIV had a 20% lower risk of unsatisfied contraceptive demand as compared to HIV-seronegative women. Our interaction analyses further suggested possible effect modification by migration on HIV, such that the impact of migration on unsatisfied demand was greater among those with HIV.
We have previously reported that migrating girls and women in Uganda tend to have higher risk of HIV acquisition and lower levels of ART use if living with HIV [22, 23, 38]. We similarly found lower levels of ART use among female in-migrants participants living with HIV in this study. In this study, we additionally find that recent in-migrants tend to have significantly higher levels of unsatisfied contraceptive demand. Taken together, these data suggest that migrating persons may generally have reduced access to health services in Uganda and that contraceptive and HIV programs in Uganda should consider the unique needs of mobile persons [21, 28, 29]. Unlike migration and ART use, prior literature on the association between migration and contraceptive use in Africa is mixed [29, 30]. Multiple studies have found differences in contraceptive use between migrant and non-migrant populations, but these are frequently explained by other characteristics, such as age and fertility intention of individuals and the communities into which migrants and non-migrants live [39, 38, 40]. Differences in study design and outcomes further complicate comparisons with our study as most prior studies have examined the impact of migration by examining where a person is migrating to or from (i.e., rural to rural vs. rural to urban), which we did not do here. In addition, previous studies frequently include women with no need for contraception in their denominators (i.e. looking at contraceptive use generally without accounting for pregnancy desire), and thus cannot determine whether differences in contraceptive behavior are due to differences in fertility intentions between migrants and non-migrants, or other factors, such as access [30, 38, 39]. Migration may impact contraceptive need and use through disrupting care networks, particularly among users of short-acting contraception (injectable, pill, condom) who rely on regular contact with the health system. Emerging long-acting dual prevention HIV and contraceptive technologies may be one way to help close gaps in unsatisfied contraceptive demand and HIV risk during periods of migration [41]. Additional research is needed, however, to disentangle the exact mechanisms by which migration may affect access to contraceptive services across a range of different settings and migration contexts, including reasons for migration (e.g., marriage versus employment).
Condom use was associated with lower levels of unsatisfied contraceptive demand among women living with HIV in this study. In addition to preventing pregnancy, condoms also prevent HIV transmission and are one of the most effective means of preventing HIV when used correctly [42]. However, condoms have lower levels of typical use effectiveness for pregnancy prevention as compared to other modern contraceptive methods [43], which increases the risk of unintended pregnancy when used as the only method of contraception. For women living with HIV who wish to prevent pregnancy, dual method use (i.e. using a condom and an additional form of contraception) is frequently advised, but is generally low across populations [44,45,46]. When excluding condoms from modern contraceptive methods, we observed no association between HIV serostatus and unsatisfied contraceptive demand. Higher levels of condom use among participants living with HIV may be because these women are more motivated to use condoms for both contraception and prevention of HIV transmission to their partners and because of better access to contraceptive services through HIV services [47, 48]. While limited access to condoms through HIV services during migration may partly explain the high levels of unsatisfied contraceptive demand among recently migrating women living with HIV, we also observed lower levels of all other modern contraceptive methods among this subgroup relative to long-term residents also living with HIV. Integration of contraception and HIV services holds promise to address unsatisfied demand for contraception, improve dual method use, improve condom use, and identify HIV-positive women through integrated counseling and service provision [49, 50]. Integration of services has, however, faced a number of challenges, including financial restrictions from donors, human resource limitations, and inadequate policies and oversight [51, 52].
We also found that having higher SES was associated with lower prevalence of unsatisfied contraceptive demand. Disparities in contraceptive use and demand satisfied have been identified across a range of sociodemographic characteristics, including wealth and education [6, 7, 53]. Disparities by wealth are particularly problematic, as wealth is generally highly correlated with other socioeconomic characteristics, such as residence and education [6]. This is reflected by our observation that women working in agriculture, who tend to be of lower SES and live in rural settings, also had significantly higher levels of unsatisfied contraceptive demand. Disparities by socioeconomic status likely exist for a number of reasons, from lower accessibility of services due to limited economic resources [54], lower quality counseling [55], and restricted autonomy [56] to make independent decisions related to contraceptive use relative to wealthier women [57]. Lastly, consistent with prior studies, we observed higher levels of unsatisfied contraceptive demand among older women, which likely reflects lower perceived risk of pregnancy [58, 59], though research on the unique contraceptive needs of women over age 35 in Africa is limited.
This study had some important limitations. First, this was a cross-sectional study. Consequently, we were unable to assess temporal or causal relationships between migration and HIV on unsatisfied contraceptive demand. Second, this study was done in a small number of communities in southcentral Uganda, so results may not be generalizable to other populations. Relatedly, migration events captured in this study were to a predominantly rural area (RCCS communities), and so results may not be applicable to populations migrating to urban environments or migration across country borders. Regarding measuring current use of contraceptive methods, the RCCS questionnaire asked about use in a yes/no format, so we were unable to tease out differences by frequency of condom use or partner type. Our sample size of participants living with HIV and recently migrating was limited and may have affected our ability to detect significant interactions between HIV and migration. Finally, the data for this study were collected more than a decade ago, and may not fully resemble modern associations between HIV, migration, and modern contraceptive use. For instance, while in this study we found that current use of ART among women living with HIV was at 35.2%, more recent data from the RCCS indicate that ART coverage has increased to > 70% among women in this cohort [18]. Family planning service provision has also improved globally since 2012, with the launch of the London Summit and FP2020 (now FP2030) initiatives. Modern contraceptive use in Uganda has increased from 22% among all women in 2014 to 41% in 2022 [60], though unsatisfied demand remains relatively high at approximately 40% [61]. Despite these changes, however, implementation of integrated contraceptive services and HIV services still remains a major challenge due to siloed (and decreasing) funding and overburdened health providers [49, 62]. Despite these limitations, this study has several notable strengths, including its population-based study design and restriction to women who were not intending to get pregnant in the next year. To the best of our knowledge, this is the first study in sub-Saharan Africa to evaluate the interaction between HIV and migration on unsatisfied contraceptive demand. Integrating contraceptive services and HIV services – and exploring implementation strategies for such integration – may be of great benefit to women living with HIV in this context, especially for mobile populations.
Conclusion
Unsatisfied modern contraceptive demand is high among girls and women in rural south-central Uganda, particularly among persons with a recent history of migration. Impact of migration on use of modern contraceptives may be greater for those living with HIV, particularly if access to HIV services in interrupted during the migration process. Future research should consider exploring differentiated integrated contraceptive and HIV services for mobile populations in sub-Saharan Africa, including dual HIV prevention and contraceptive methods.
Availability of data and materials
The datasets analyzed during the current study are available from the corresponding author upon reasonable request.
Abbreviations
- adjPRR:
-
Adjusted prevalence risk ratio
- ART:
-
Antiretroviral therapy
- CI:
-
Confidence interval
- HIV:
-
Human immunodeficiency virus
- IUD:
-
Intra-uterine device
- RCCS:
-
Rakai Community Cohort Study
References
Moreau C, Shankar M, Helleringer S, Becker S. Measuring unmet need for contraception as a point prevalence. BMJ Glob Health. 2019;4(4):e001581.
Sully EA, Biddlecom A, Darroch JE, Riley T, Ashford LS, Lince-Deroche N, et al. Adding it up: investing in sexual and reproductive health 2019. New York: Guttmacher Institute; 2020. Available from: https://www.guttmacher.org/report/adding-it-up-investing-in-sexual-reproductive-health-2019.
Baek C, Rutenberg N. Addressing the family planning needs of HIV-positive PMTCT clients: baseline findings from an operations research study. Washington DC: Horizons Research Update; 2005.
Fabic MS, Choi Y, Bongaarts J, Darroch JE, Ross JA, Stover J, et al. Meeting demand for family planning within a generation: the post-2015 agenda. Lancet. 2015;385(9981):1928–31.
Family planning 2030. Data Dashboard unmet need(all women). 2021. Available from: https://fp2030.org/data-dashboard. Cited 2022 8/27/2022.
Choi Y, Fabic MS. Monitoring progress in equality for the sustainable development goals: a case study of meeting demand for family planning. Glob Health Sci Pract. 2018;6(2):390–401.
Ewerling F, Victora CG, Raj A, Coll CVN, Hellwig F, Barros AJD. Demand for family planning satisfied with modern methods among sexually active women in low- and middle-income countries: who is lagging behind? Reprod Health. 2018;15(1):42.
Hellwig F, Coll CV, Ewerling F, Barros AJ. Time trends in demand for family planning satisfied: analysis of 73 countries using national health surveys over a 24-year period. J Glob Health. 2019;9(2):020423.
Chandrashekhar TS, Kiran A, Ishwar T. Inequalities in demand satisfied with modern methods of family planning among women aged 15–49 years: a secondary data analysis of Demographic and Health Surveys of six South Asian countries. BMJ Open. 2022;12(6):e049630.
Barros AJD, Boerma T, Hosseinpoor AR, Restrepo-Méndez MC, Wong KLM, Victora CG. Estimating family planning coverage from contraceptive prevalence using national household surveys. Glob Health Action. 2015;8(1):29735.
Hoffman IF, Martinson FEA, Powers KA, Chilongozi DA, Msiska ED, Kachipapa EI, et al. The year-long effect of HIV-positive test results on pregnancy intentions, contraceptive use, and pregnancy incidence among Malawian women. J Acquir Immune Defic Syndr. 2008;47(4):477–83.
Taulo F, Berry M, Tsui A, Makanani B, Kafulafula G, Li Q, et al. Fertility intentions of HIV-1 infected and uninfected women in Malawi: a longitudinal study. AIDS Behav. 2009;13(1):20–7.
Wanyenze RK, Matovu JKB, Kamya MR, Tumwesigye NM, Nannyonga M, Wagner GJ. Fertility desires and unmet need for family planning among HIV infected individuals in two HIV clinics with differing models of family planning service delivery. BMC Womens Health. 2015;15(1):5.
Jhangri GS, Heys J, Alibhai A, Rubaale T, Kipp W. Unmet need for effective family planning in HIV-infected individuals: results from a survey in rural Uganda. J Fam Plann Reprod Health Care. 2012;38(1):23–9.
Kassie MD, Habitu YA, Berassa SH. Unmet need for family planning and associated factors among women living with HIV in Gondar city, Northwest Ethiopia: cross-sectional study. Pan Afr Med J. 2021;38:22.
Mekie M, Addisu D, Taklual W, Melkie A. The level of unmet need for family planning and its predictors among HIV-positive women in Ethiopia: a systematic review and meta-analysis. Biomed Res Int. 2021;2021:3139272.
Joint United Nations Programme on HIV/AIDS. UNAIDS DATA 2021. Geneva: UNAIDS; 2021. Available from: https://www.unaids.org/sites/default/files/media_asset/JC3032_AIDS_Data_book_2021_En.pdf.
Grabowski MK, Serwadda DM, Gray RH, Nakigozi G, Kigozi G, Kagaayi J, et al. HIV prevention efforts and incidence of HIV in Uganda. N Engl J Med. 2017;377(22):2154–66.
Scoggins S, Bremner J. FP2020: the arc of progress 2019–2020. Washington, DC: Family Planning 2020; 2021.
Laryea DO, Amoako YA, Spangenberg K, Frimpong E, Kyei-Ansong J. Contraceptive use and unmet need for family planning among HIV positive women on antiretroviral therapy in Kumasi, Ghana. BMC Womens Health. 2014;14:126.
Dzomba A, Tomita A, Govender K, Tanser F. Effects of migration on risky sexual behavior and HIV acquisition in South Africa: a systematic review and meta-analysis, 2000–2017. AIDS Behav. 2019;23(6):1396–430.
Olawore O, Tobian AAR, Kagaayi J, Bazaale JM, Nantume B, Kigozi G, et al. Migration and risk of HIV acquisition in Rakai, Uganda: a population-based cohort study. Lancet HIV. 2018;5(4):e181–9.
Kate Grabowski M, Lessler J, Bazaale J, Nabukalu D, Nankinga J, Nantume B, et al. Migration, hotspots, and dispersal of HIV infection in Rakai, Uganda. Nat Commun. 2020;11(1):976.
Dzomba A, Kim H-Y, Tomita A, Vandormael A, Govender K, Tanser F. Predictors of migration in an HIV hyper-endemic rural South African community: evidence from a population-based cohort (2005–2017). BMC Public Health. 2022;22(1):1141.
McGrath N, Eaton JW, Newell M-L, Hosegood V. Migration, sexual behaviour, and HIV risk: a general population cohort in rural South Africa. Lancet HIV. 2015;2(6):e252–9.
Camlin CS, Hosegood V, Newell M-L, McGrath N, Bärnighausen T, Snow RC. Gender, migration and HIV in rural KwaZulu-Natal, South Africa. PLoS One. 2010;5(7):e11539.
Majelantle R, Navaneetham K. Migration and fertility: a review of theories and evidences. J Glob Econ. 2013;1:1.
Moyo RC, Nkhoma D. Association of migration and family planning use among women in Malawi: evidence from 2019/2020 Malawi Multiple Indicators Survey. Contracept Reprod Med. 2023;8(1):52.
Almonte MT, Lynch CA. Impact of internal female migration on unmet need for modern contraception in Zambia. Reprod Health. 2019;16(1):169.
Groene EA, Kristiansen D. Unmet need for family planning after internal migration: analysis of Ethiopia 2017–2018 PMA survey data. Popul Space Place. 2021;27(1):e2376.
Camlin CS, Charlebois ED. Mobility and its effects on HIV acquisition and treatment engagement: recent theoretical and empirical advances. Curr HIV/AIDS Rep. 2019;16(4):314–23.
Ross J, Cunningham CO, Hanna DB. HIV outcomes among migrants from low-income and middle-income countries living in high-income countries: a review of recent evidence. Curr Opin Infect Dis. 2018;31(1):25–32.
Chang LW, Grabowski MK, Ssekubugu R, Nalugoda F, Kigozi G, Nantume B, et al. Heterogeneity of the HIV epidemic in agrarian, trading, and fishing communities in Rakai, Uganda: an observational epidemiological study. Lancet HIV. 2016;3(8):e388–96.
Galiwango R, Musoke R, Lubyayi L, Ssekubugu R, Kalibbala S, Ssekweyama V, et al. Evaluation of current rapid HIV test algorithms in Rakai, Uganda. J Virol Methods. 2013;192(1–2):25–7.
Santelli JS, Chen I, Makumbi F, Wei Y, Nalugoda F, Lutalo T, et al. Household wealth and HIV incidence over time, rural Uganda, 1994–2018. AIDS. 2021;35(11):1835–43.
Ahmed S, Lutalo T, Wawer M, Serwadda D, Sewankambo NK, Nalugoda F, et al. HIV incidence and sexually transmitted disease prevalence associated with condom use: a population study in Rakai, Uganda. AIDS. 2001;15(16):2171–9.
Brahmbhatt H, Santelli J, Kaagayi J, Lutalo T, Serwadda D, Makumbi F. Pregnancy incidence and fertility desires among couples by HIV status in Rakai, Uganda. J Acquir Immune Defic Syndr. 2019;80(5):494–502.
Akinyemi JO, Odimegwu CO, Adebowale AS. The effect of internal migration, individual and contextual characteristics on contraceptive use among Nigerian women. Health Care Women Int. 2017;38(10):1075–94.
Ochako R, Askew I, Okal J, Oucho J, Temmerman M. Modern contraceptive use among migrant and non-migrant women in Kenya. Reprod Health. 2016;13(1):67.
Cau BM. Female migration, local context and contraception use in urban Mozambique. Afr J Reprod Health. 2016;20(1):52–61.
Friedland BA, Mathur S, Haddad LB. The promise of the dual prevention pill: a framework for development and introduction. Front Reprod Health. 2021;3:682689.
Stover J, Teng Y. The impact of condom use on the HIV epidemic. Gates Open Res. 2021;5:91.
World Health Organization. Family planning/contraception methods. Geneva: WHO; 2020. Available from: https://www.who.int/news-room/fact-sheets/detail/family-planning-contraception.
Prata N, Sreenivas A, Bellows B. Potential of dual-use policies to meet family planning and HIV prevention needs: a case study of Zimbabwe and Mozambique. J Fam Plann Reprod Health Care. 2008;34(4):219–26.
Mesfin Y, Argaw M, Geze S, Tefera B. Dual contraceptive use and factor associated with people living with HIV/AIDS: a systematic review and meta-analysis. Infect Dis Obstet Gynecol. 2021;2021:5440722.
Joshi B, Velhal G, Chauhan S, Kulkarni R, Begum S. Linking HIV & family planning services to improve dual methods of contraception among women infected with HIV in Mumbai, Maharashtra, India. Indian J Med Res. 2016;143(4):464–73.
Thurman TR, Taylor TM, Luckett B, Spyrelis A, Nice J. Condom use correlates among youth living with HIV in South Africa: lessons for promoting safer sex. Vulnerable Child Youth Stud. 2024;19(1):211–22.
Conserve D, Sevilla L, Younge S, Mbwambo J, King G. Condom use among HIV-positive sexually active adults and partner’s HIV status in Dar es Salaam, Tanzania. J Health Care Poor Underserved. 2012;23(1):191–203.
Haberlen SA, Narasimhan M, Beres LK, Kennedy CE. Integration of family planning services into HIV care and treatment services: a systematic review. Stud Fam Plann. 2017;48(2):153–77.
Narasimhan M, Yeh PT, Haberlen S, Warren CE, Kennedy CE. Integration of HIV testing services into family planning services: a systematic review. Reprod Health. 2019;16(1):61.
Nkhoma L, Sitali DC, Zulu JM. Integration of family planning into HIV services: a systematic review. Ann Med. 2022;54(1):393–403.
Kangudie DM, Guidigbi H, Mensah S, Bala AA, Delate R. Effective integration of sexual reproductive health and HIV prevention, treatment, and care services across sub-Saharan Africa: where is the evidence for program implementation? Reprod Health. 2019;16(1):56.
Blumenberg C, Hellwig F, Ewerling F, Barros AJD. Socio-demographic and economic inequalities in modern contraception in 11 low- and middle-income countries: an analysis of the PMA2020 surveys. Reprod Health. 2020;17(1):82.
Dias JG, de Oliveira IT. Multilevel effects of wealth on women’s contraceptive use in Mozambique. PLoS One. 2015;10(3):e0121758.
Jain AK. Examining progress and equity in information received by women using a modern method in 25 developing countries. Int Perspect Sex Reprod Health. 2016;42(3):131–40.
OlaOlorun FM, Anglewicz P, Moreau C. From non-use to covert and overt use of contraception: identifying community and individual factors informing Nigerian women’s degree of contraceptive empowerment. PLoS One. 2020;15(11):e0242345.
Adebowale AS, Gbadebo B, Afolabi FR. Wealth index, empowerment and modern contraceptive use among married women in Nigeria: are they interrelated? J Public Health. 2016;24(5):415–26.
Sedgh G, Ashford LS, Hussain R. Unmet need for contraception in developing countries: examining women’s reasons for not using a method. New York: Guttmacher Institute; 2016.
Godfrey EM, Chin NP, Fielding SL, Fiscella K, Dozier A. Contraceptive methods and use by women aged 35 and over: a qualitative study of perspectives. BMC Womens Health. 2011;11(1):5.
Makerere University SoPHatCoHSatBMGIfPaRHatJHBSo. Uganda round 1 HQFQ survey. 2014.
Makerere University SoPHatCoHSaTBMGIfPaRHaTJHBSo. Uganda phase 3 SQ survey. 2022.
FP/HIV-10-01E FHI. Family planning and HIV integration: approaching the tipping point. 2011.
Acknowledgements
We thank the Rakai Health Sciences Program as well as the participants of the Rakai Community Cohort Study who made this study possible. We also thank Joseph Ssekasanvu and Xinyi Feng who supported the biostatistical analyses presented in this manuscript.
Funding
This study was supported by the National Institute of Allergy and Infectious Diseases (R01AI087409, U01AI075115, U01AI100031), the National Institute of Child Health and Development (R01HD050180, R01HD070769), the National Institute of Mental Health (F31MH095649, R01MH099733), and the National Institutes of Health Fogarty International Center (D43TW010557). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the paper.
Author information
Authors and Affiliations
Contributions
PN and MKG conceptualized the study. PN drafted the manuscript with the support of PTY, LWC, LZ, and MKG. RS and TL provided insight into the data analysis and framing. All authors reviewed and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical approval for this study embedded within the RCCS was given by the Johns Hopkins School of Medicine’s Institutional Review Board and the Uganda Virus Research Institute’s Research and Ethics Committee. All study participants provided written informed consent or assent/parental consent for participants aged less than 18 years old.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Namusisi, P., Yeh, P.T., Ssekubugu, R. et al. The intersection between migration, HIV, and contraceptive use in Uganda: a cross-sectional population-based study. Reprod Health 21, 65 (2024). https://doi.org/10.1186/s12978-024-01796-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12978-024-01796-z