Abstract
Background
Despite a vast literature, atherosclerosis and the associated ischemia/reperfusion injuries remain today in many ways a mystery. Why do atheromatous plaques make and store a supply of cholesterol and sulfate within the major arteries supplying the heart? Why are treatment programs aimed to suppress certain myocardial infarction risk factors, such as elevated serum homocysteine and inflammation, generally counterproductive?
Methods
Our methods are based on an extensive search of the literature in atherosclerotic cardiovascular disease as well as in the area of the unique properties of water, the role of biosulfates in the vascular wall, and the role of electromagnetic fields in vascular flow. Our investigation reveals a novel pathology linked to atherosclerosis that better explains the observed facts than the currently held popular view.
Results
We propose a novel theory that atherosclerosis can best be explained as being due to cholesterol sulfate deficiency. Furthermore, atheromatous plaques replenish the supply of cholesterol and sulfate to the microvasculature, by exploiting the inflammatory agent superoxide to derive sulfate from homocysteine and other sulfur sources. We argue that the sulfate anions attached to the glycosaminoglycans in the glycocalyx are essential in maintaining the structured water that is crucial for vascular endothelial health and erythrocyte mobility through capillaries. Sulfate depletion leads to cholesterol accumulation in atheromas, because its transport through water-based media depends on sulfurylation. We show that streaming potential induces nitric oxide (NO) release, and NO derivatives break down the extracellular matrix, redistributing sulfate to the microvasculature. We argue that low (less negative) zeta potential due to insufficient sulfate anions leads to hypertension and thrombosis, because these responses can increase streaming potential and induce nitric-oxide mediated vascular relaxation, promoting oxygen delivery. Our hypothesis is a parsimonious explanation of multiple features of atherosclerotic cardiovascular disease.
Conclusions
If our interpretation is correct, then it would have a significant impact on how atherosclerosis is treated. We recommend a high intake of sulfur-containing foods as well as an avoidance of exposure to toxicants that may impair sulfate synthesis.
Similar content being viewed by others
Background
After many years of research, atherosclerosis and the associated risk of myocardial infarction (MI), the number one cause of death worldwide, remains a well-studied but poorly understood condition. Several risk factors have been identified, such as elevated serum low density lipoprotein (LDL), low cholesterol content in high density lipoprotein (HDL), elevated serum homocysteine, diabetes, left ventricular hypertrophy, etc. [1], but it remains controversial whether these risk factors are merely associative or actual causes. Particularly troublesome is the paradoxical reverse epidemiology profile of people suffering from end stage kidney disease [2] and other chronic inflammatory conditions such as systemic lupus erythematosus [3]. Here, the normal risk factors – obesity, high blood pressure, high cholesterol, and high homocysteine – all become protective factors in heart disease risk. And these patients have extremely high risk of heart disease (this is in fact their most common cause of death) [4], despite the inversion of risk factors.
Increasingly, atherosclerosis is framed as an inflammatory condition [5–7], and clearly inflammation plays a critical role in vascular dysfunction. Ischaemic tissue will face necrosis if it is not reperfused, yet reperfusion can also lead to severe tissue damage due to oxidative attack [8]. Inflammation is the one factor that is strongly linked to cardiac disease in association with kidney failure [9, 10]. Others have proposed that atherosclerosis is an infectious disease, as infective agents, especially Chlamydia pneumoniae and Herpes virus, have been found consistently in association with atherosclerotic plaque regions [11, 12].
Results and discussion
In this paper we present an alternative view of atherosclerosis as a set of responses aimed at correcting disturbances in biological water structure caused by depletion of crucial biosulfates – especially sulfurylated1 Footnote 1 cholesterol and glycosaminoglycans (GAGs) -- in the cardiovascular system. Evidence for a role of sulfur deficiency in atherosclerosis will be surveyed in (Evidence for a role of sulfur deficiency in atherosclerosis below). In Sections (The Exogenous Interfacial Water Stress (EIWS) theory of inflammation, Electrokinetic vascular streaming potential and Biosulfates as enablers of healthy blood flow), we consider the biophysics of structured water and vascular streaming potential and the importance of sulfates in maintaining them and in enabling healthy blood flow. In Section (Extracellular matrix sGAG turnover as a mechanism for sulfate redistribution), we discuss how sulfurylated GAG turnover in the vascular system may be used to redistribute sulfate to replenish cholesterol sulfate levels in the capillaries. We will then turn our attention in Section (Glutathione and GGT) to emergency routes -- with damaging side effects – by which the body may replenish vascular sulfate supplies by conversion of less-oxidized sulfur compounds such as glutathione, H2S, and homocysteine to sulfate.
Evidence for a role of sulfur deficiency in atherosclerosis
While many research papers have described in detail the processes that take place in the coronary artery wall in association with the accumulation of fat and cholesterol, few have attempted to explain why these processes are happening. It is particularly surprising that the arteries supplying the heart, arguably the most important organ in the body, should be especially vulnerable to fatty deposits.
In this section we will review the evidence for a role of sulfur deficiency in atherosclerosis. Table 1 provides a chronological list of key research and review papers pointing strongly to involvement of a variety of oxidized and reduced sulfur compounds in this condition. These articles will be discussed in more detail at various points throughout this paper.
Interesting early studies on the New World primate, Cebus fatuella, revealed that a condition strongly resembling atherosclerosis could be produced in the artery wall by feeding these monkeys a high fat, high cholesterol, high choline diet [13]. However, this effect could be eliminated or drastically reduced if the monkeys were simultaneously supplemented with sulfur-containing amino acids. Children with disorders of cysteine metabolism leading to excess serum homocysteine develop arterial damage at an early age that is reminiscent of atherosclerotic cardiovascular disease [14]. The consumption of garlic is inversely correlated with the progression of atherosclerosis, and, in [15] it was argued that the protective benefit is due to the ability of human erythrocytes to convert garlic-derived polysulfides into hydrogen sulfide gas. These observations and others strongly support the model that impaired sulfur supplies to the vasculature plays a critical role in atherosclerosis.
In [16], the argument was developed that atherosclerosis results from a deficiency in a critical nutrient, cholesterol sulfate (Ch-S), and that the atheroma is a locale where endothelial cells, macrophages, and platelets collaborate to produce Ch-S from homocysteine and oxidized LDL. It was argued that an underlying deficiency in Ch-S, due principally to insufficient dietary sulfur and inadequate sun exposure to the skin, leads, over time, to severe depletion of cholesterol and sulfate in the tissues. This deficiency becomes life-threatening with age, and atherosclerotic plaque is a well-choreographed program for renewal of Ch-S. Unfortunately, there is necessarily collateral damage from superoxide exposure, as superoxide is required to oxidize the LDL and to catalyze the reaction that produces sulfate from homocysteine thiolactone [17].
Worldwide geographical data show an inverse relationship between cardiovascular disease and annual sunlight availability [18]. In a study conducted in the British Isles, 49 % of the variance in mortality from coronary heart disease was accounted for by mean annual sunshine hours as measured by the Meteorological Office [19]. However, placebo-controlled trials failed to show any benefit from vitamin D3 supplementation [20]. We propose that the benefit comes from Ch-S synthesis instead. In [16], it was proposed that the protein endothelial nitric oxide synthase (eNOS), along with sunlight, catalyzes sulfate production in erythrocytes, endothelial cells, platelets and keratinocytes in the skin. Thus, eNOS is a dual-purpose enzyme, producing sulfate when it is membrane–bound and producing nitric oxide when it is free in the cytoplasm. We hypothesize that the overuse of sunscreen has played a dual damaging role not only because sunlight catalysis is suppressed but also because the aluminum found in high-SPF sunscreens as an emulsifier actively disrupts eNOS’ function [21]. eNOS is an orphan cytochrome P450 (CYP) enzyme [22], and aluminum is a known disruptor of CYP enzyme function through its displacement of the iron in the heme group [23]. Many other environmental toxicants also disrupt CYP enzymes, including mercury [24, 25], arsenic [26], cadmium [24], glyphosate [27, 28], and lead [25, 29].
There exist a large number of different sulfatases and sulfotransferases that effect sulfuryl group transfer from a source molecule to a target molecule, with an ATP-activated form of sulfate, called 3′-phosphoadenosine-5′-phosphosulfate (PAPS) serving as an intermediary [30, 31]. Sulfotransferase deficiency is associated with remarkable accumulations of Ch-S in red blood cells (7500 μgrams/100 ml vs < 300 in controls) and in plasma (3300 vs. < 350) [32]. This implies that Ch-S produced in erythrocytes and the endothelial wall is essential for distributing both cholesterol and sulfate to the tissues.
The nuclear receptor peroxisome proliferator-activated receptors (PPARs) regulate both lipid metabolism and the inflammatory response in macrophages in the atheroma. A recent experiment showed that 25-hydroxycholesterol sulfate (25HCS) activated PPARγ in macrophages, resulting in the suppression of NF-κB and the subsequent inflammatory response [33]. 25HCS also decreases lipid biosynthesis in both macrophages [34] and the liver [33, 35]. The unsulfurylated form of the molecule had the opposite effect. This supports the idea that inflammation is needed for sulfate synthesis and that sulfate is needed for cholesterol export.
MI is an acute response to interruption of the blood supply to a part of the heart, usually assumed to be caused by the rupture of vulnerable plaque occluding the artery wall. However, in about 10 % of patients, there is no apparent plaque accumulation associated with the acute event. Despite this apparently healthy arterial profile, such individuals experience a similar incidence of death and recurrent MI in long-term follow-up, compared with patients with severe residual stenosis [36]. A most interesting case in this regard is the myocardial dysfunction associated with Chagas disease [37]. Trypanosoma cruzi (Chagas disease) is a parasitic infection that occurs predominantly in South America, where an individual infected early in life experiences a substantially increased risk to premature heart failure many decades later [38, 39]. While there is a substantial impairment in heart function associated with Chagas disease, including cardiomyopathy and left ventricular hypertrophy, people with this condition are remarkably free from atherosclerotic plaque build-up.
We propose that this unusual profile is due to the fact that T. cruzi produces a steroid that remarkably resembles Ch-S. A study revealed that 86 % of the Chagas patients tested had developed autoantibodies against Ch-S – a very specific effect in that closely related steroid sulfates were not affected [37]. Thus, the atheroma is unable to function in the normal role of producing Ch-S, due to the autoimmune reaction this would provoke. As a consequence, the heart develops severe cumulative impairment over time, due to deficiencies in cholesterol and sulfate supplies, ironically caused by the absence of atherosclerosis.
The most precarious phase of an MI is reperfusion rather than ischemia, as reperfusion injury can be extensive and life-threatening [40]. Reperfusion injury is associated with systemic exposure to inflammation from superoxide and its reaction products, which is believed to be the principle source of injury [40, 41]. Ischemic reperfusion is characterized by a complex sequence of events leading in extreme cases to systemic inflammation and edema, microvascular dysfunction (the “no flow” phenomenon) and multiple organ failure, the leading cause of death in the critically ill [41].
Thus, a local blockage, for example due to thrombosis or traumatic injury, whether in the heart or elsewhere, can lead, through complex signaling cascades, to a systemic response – a catastrophic failure in the blood transport system – which appears to be the ultimate cause of death in these cases. Most interesting, however, is the observation that suppression of the systemic response through drug intervention results in a substantial worsening of tissue damage via extensive apoptosis at the local site [42]. Thus, the systemic response can lead to a positive outcome: it produces some product that somehow protects cells at the site of injury from apoptosis.
In addition to Ch-S, the sulfurylated glycosaminoglycans (GAGs) that comprise the so-called glycocalyx structures lining the endothelial lumen also appear to contribute importantly to cardiovascular health [43]. These sGAGs contain linear chains of modified sugar molecules such as heparan sulfate and chondroitin sulfate, which can be either attached to membrane-bound proteins or free floating. Pericytes are a specialized cell type that has gained attention in recent years due to the realization that they are essential for the health of capillaries, arterioles and venules, and that they are particularly prevalent in the brain [44]. Pericytes are situated in the microenvironmental niche of the arteriole or venule wall, and they differentiate into different cell types in response to environmental stress signals, to assist with tissue regeneration and repair [45]. Pericytes wrap around endothelial cells and are in close communication with them through junctional complexes. The migration of pericytes depends on paracrine signaling from growth factors like vascular endothelial growth factor (VEGF) and platelet derived growth factor (PDGF). In [46], it was shown that the PDGF-mediated recruitment of pericytes to the capillary wall critically depends on sufficient N-sulfurylation of heparan sulfate proteoglycans (HSPGs) in the glycocalyx. N-deacetylase/N-sulfotransferases (NDSTs) are essential for the sulfurylation process [47], and mice with a deficiency in NDST-1, the major N-sulfurylating enzyme [48], often die in utero, or live for just a few days following birth. Microscopic examination of the brain vasculature revealed severe depletion in pericytes.
The contribution of sGAGs to cardiovascular health rests on their ability to maintain specially-structured water zones in the blood vessels. This topic will be explored in more detail in the following three sections.
The Exogenous Interfacial Water Stress (EIWS) theory of inflammation
As noted above, atherosclerosis is increasingly regarded as an inflammatory condition [5–7]. In earlier reviews, Davidson and Seneff have proposed exogenous interfacial water stress (EIWS) – the disruption of normal interfacial tension between water and biomacromolecules in vivo by exogenous agents such as the aluminum aquo cation -- as the earliest step in the pathogenesis of inflammation and disease [49, 50].
In this section, we will focus on biophysical properties of interfacial water that are relevant for blood flow in the vascular system. In the next section, we will discuss streaming potential, and its important role in inducing nitric oxide synthesis. We will follow this with a section that considers in more detail the roles played by biological sulfate species, including sGAGs and Ch-S, in maintaining healthy interfacial water structure and enabling blood flow.
A full description of the complex biophysics of dynamically-structured water and its electrokinetic properties is beyond the scope of this paper. However, several recent review articles can be cited [51–54]. It has become abundantly clear that water is an active and even key participant in chemical reactions, and is, furthermore, the natural environment for biochemical processes [54]. Moreover, the interaction of water with the solutes and surfaces encountered in biological systems at relatively close range results in water properties that vary substantially from those measured for the pure bulk liquid.
In 2012, Davidson and Seneff [49] presented for the first time a number of novel biophysically-based hypotheses as to the role of interfacial water, sunlight, and the biosulfates in facilitating and enabling microvascular blood flow and gas exchange. The concept of surfactant-induced interfacial water stress was presented, and the conclusion was reached that the initial events in the inflammatory cascade are purely biophysical. The role of the bio-sulfates in maintaining cell membrane function and the role of endothelial nitric oxide synthase-derived nitric oxide in acute shock and Sudden Death Syndrome were described. The concepts, hypotheses, and conclusions in this paper provide building blocks upon which future hypotheses can be generated and tested.
In a series of in vitro experiments, Pollack and coworkers have established that water adjacent to hydrophilic surfaces (interfacial water) differs dynamically from bulk water in several respects, including exhibiting up to ten times higher viscosity [55, 56]. Guo and Friedman [57] and Tielrooij et al. [58] have provided data to support an earlier prediction by Ling [59, 60] that even small organic molecules and solutes can induce formation of “polarized oriented multilayers” of interfacial water.
Pollack and coworkers proposed the term “exclusion zone” for this interfacial water, based on the observation that solutes and suspended particles were excluded from this water at distances up to a few hundred microns from the hydrophilic surface [56]. He proposes that the structured water along biological membranes forms hexamers [61] that closely resemble the structure of ice. He wrote: “We found the honeycomb sheet model more promising, its hexamers lying out of register with those of adjacent sheets. This model could account for the EZ's net charge; plus, it has the advantage of precedent because of its similarity to ice.” ([56], p. 68). Most likely, the exclusion zone is built of such highly structured “liquid crystals” and it induces a charge separation with a voltage drop across the interface with the surrounding bulk water, thus providing a battery-like source of energy.
Del Giudice has compared this interfacial or exclusion zone (EZ) water with Preparata’s proposed water “coherence domains” (CDs), derived via a quantum electrodynamic application of quantum field theory [62]. In earlier work, Preparata also likened water to a plasma in the sense that it contains a roughly equal number of positively and negatively charged particles and thus can conduct electricity and be influenced by magnetic fields [63]. More recently, in a proposed continuum solvent model, Duignan et al. have also described interfacial water as a coherent, plasma-like phase [64].
In addition to the evidence reported for special, “non-bulk” water zones near hydrophilic surfaces [56], neutron reflectivity measurements of Doshi et al. have revealed reversible changes in the size of a reduced-density water region near a model hydrophobic surface, depending on the amounts and kinds of dissolved gases present in the water [65]. Their observation of a decrease in size of the lower-density region in the water as gas concentration was reduced explains the hydrophobic effect and its reportedly lower magnitude in degassed water [65]. Shatalov, Bunkin, and others have published data pointing to an important role for ion-stabilized nanobubbles in modulating interfacial water tension [53, 66, 67]. These studies of the effects of dissolved gases on interfacial water properties provide important insights into the important role of dissolved gases, such as NO, CO, and H2S, as vascular signaling molecules [68]. This subject will be discussed further in Section (Electrokinetic vascular streaming potential) below.
From this brief survey, we can see that essentially all types of surfaces and solutes found in biological systems have important interactions with water that influence interfacial water structure and tension. The sulfur-containing surfaces and solutes of particular interest for maintaining healthy water properties in blood vessels include the sGAGs that, as mentioned above, line the endothelial lumen, and Ch-S, which is present in all cell membranes and, at low levels, in blood plasma [30]. David Grant’s group has provided infrared and NMR spectroscopic evidence to support the view that heparan sulfate proteoglycans (a type of sGAG) impart structure to water in vivo [69]. Importantly, results of infrared photodissociation spectroscopy studies have provided evidence of relatively long-range water ordering properties for sulfate anions [70].
Moreover, one of the hydrophilic surfaces used prominently in Pollack’s studies of EZs comprised sheets of the sulfonate-rich fluoropolymer NafionR [55, 56, 71]. Recent studies of Pollack and coworkers with potential high relevance to water behavior in blood vessels include observations on water flow through submerged NafionR tubes [72] and elegant work on EZ formation near discontinuous NafionR surfaces [73]. Figure 1 depicts the capillary glycocalyx and shows how the NafionR-based tubes can model its behavior. Figure 2 provides physical evidence of the structured water adjacent to Nafion strips, which draws parallels with the architecture of the glycocalyx.
a. Distribution of charge in the exclusion zone and water beyond the exclusion zone as shown by electrical potential measurements and pH- sensitive dye studies. Protons spread in bulk water, although some cling to the negatively charged EZ. b Disposition of charge anticipated in a tubular configuration. (Reproduced from Rohani and Pollack, 2013 [72], with permission from the American Chemical Society. Copyright © 2013)
NafionR strips spaced at 50, 100, 250 & 500 μm edge-to-edge. Exclusion zones form from the NafionR surfaces and merge into an unbroken EZ in 50- and 100 μm-spaced lines. NafionR strips are seen as the bright white squares on the images. At 250 and 500 μm the EZ forms in discrete zones that do not combine. The yellow dashed lines demarcate edges of glass support. Dashed black lines indicate extent of clear EZ. Diagram on the far right indicates the viewing height (arrow) on which the objective was focused. (Reproduced from Figueroa and Pollack (2011) [73] with permission from WIT Press)
The observations of Bunkin et al. of changes in electrostatic potential and the refractive index of water provide additional evidence of a separate phase of water near NafionR surfaces [74]. In addition, Zhao et al. have noted unexpected effects of light on self-assembly of colloidal, sulfate-decorated particles near larger beads in water [75].
Electrokinetic vascular streaming potential
In this section we consider the effects of interfacial water on blood flow in the vascular system. The pumping action of the heart generates pressure that pushes blood through blood vessels. This pressure-induced flow of the blood past the charged sGAGs lining the endothelium generates an electric streaming potential. We will focus on considering a recent paper by Trivedi et al. [76], which demonstrated that the electrokinetic vascular streaming potential (EVSP) caused by blood flow has significant biological effects on endothelial cells [76]. This paper may have solved in one stroke of genius the mystery of why both elevated blood pressure and elevated heart rate might have beneficial effects [76]. In fact, EVSP may be the most important contributor to vascular health.
A key insight is that the blood is filled with negatively charged “particles” in colloidal suspension, which includes both cells such as red blood cells (RBCs) and platelets, as well as lipid particles such as LDL and HDL, serum proteins such as albumin and γ globulins, and fragments of sulfurylated polysaccharides like heparan sulfate. A moving charged particle creates an electromagnetic field, which can be used as a signaling device in biological systems. What Trivedi et al. [76] have shown is that endothelial cells respond to these electromagnetic signals by producing nitric oxide, which has been identified as the endothelial-derived relaxing factor (EDRF) in arteries and veins [77].
The signal has both a DC and an AC component. The AC component is synchronous with the heart rate, as the suspended particles accelerate and decelerate in response to the force field of the beating heart. The paper showed that there was a significant (nonlinear) increased response to a 2Hz signal (corresponding to a heart rate of 120 beats per minute) compared to a 1Hz signal (60 bpm). Hence, increasing heart rate has a direct effect of inducing increased NO production, and therefore vascular relaxation [77].
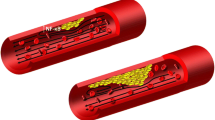
Figure 3 provides a schematic of the principle that vascular flow is critically dependent on the negative charge provided by sulfate ions attached to the glycosaminoglycans in the capillary wall and to cholesterol in the plasma membrane of red blood cells. Electrostatic repulsion prevents RBCs from adhering to the capillary wall, and the encasement of the glycocalyx within structured water, formed in response to the kosmotropic properties of sulfate, provides a smooth surface further protecting from adhesion. The RBCs are propelled toward the venous end of the capillary by the electromagnetic field induced by the voltage drop across the capillary. The RBCs themselves act as moving charged particles that create a circular magnetic force around the capillary wall. This force induces nitric oxide release from the endothelial cells, which promotes vascular relaxation and increases flow.
Schematic of the bottle brush structure of the glycocalyx, including the lipid bilayer at the top, and the branching trees of glycosylated proteins with sulfates in the heparan sulfate chains providing negative charge and kosmotropic effects on the surrounding water, with strong analogies to Pollack’s NafionR strips experiments shown in Fig. 2
The experimental results presented in [76] virtually prove, by process of elimination, that structured water in the interphase of the endogenous biofilm of the endothelial glycocalyx is the “target” of the EVSP. Based in substantial part on Trivedi et al. [76], we propose the hypothesis that interfacial water is also the target of extremely low frequency electromagnetic (ELF EM) energy from the environment, in vivo, including that energy afforded by the EVSP to the interfacial water found in the EGL of the vascular endothelium, systemically, including that of the heart.
We find to be quite striking the interpretations derived from the seminal experiments in the Trivedi [76] paper, which demonstrated that the effect of EVSP on the NO signal is not simply tied to the depolarization effect on the endothelial cells. They propose several sites of action of the ELF fields on the pathways that are directly responsible for producing the NO signal in the presence of extracellular calcium. Their experiments with ELF electrical stimulation under calcium-free solutions show increases in NO production in an amplitude- and frequency-dependent manner. The conclusion is that the field itself acts on a target that potentiates NO production without requiring calcium flux.
Having excluded many of “the usual suspects” as targets of the ELF EM field of the EVSP, including those associated with calcium flux, Trivedi et al. suggest that “the likely mechanism that links these fields to cellular effects is the electroconformational coupling of an applied periodic electric field to membrane-associated processes, which has been established both theoretically and experimentally.” [76] Of course, this view is fully compatible with the EIWS theory, in which an underlying tenet is that protein structure and function are “slaved” to biological water dynamics [78], and effectively invites our proposal that a logical candidate for the biological target of the ELF EM energy of the EVSP is the interfacial water itself.
The classical formula for streaming potential, known as the Helmholtz-Smoluchowski (HS) equation, is very enlightening, because its magnitude is proportional to zeta potential and blood pressure, and inversely proportional to blood viscosity. Zeta potential, in turn, depends on the amount of negative charge around the charged particles. According to A.V. Delgado et al. [79], electrokinetic or zeta-potential, ζ, is identified as the potential at the plane where slip with respect to bulk solution is postulated to occur ([79], p. 1759). When RBCs are deficient in Ch-S in their membranes, this will be reflected in a lowered (less negative) zeta potential. This can be counterbalanced by increasing the blood pressure to compensate, which could be the main beneficial effect of high blood pressure, a so-called “pathological” condition associated with cardiovascular disease.
Furthermore, viscosity, the denominator term in the HS equation, can also be manipulated by reducing the total count of RBCs in circulation. This will have a significant effect in reducing viscosity, thus increasing EVSP. This may be the source of the essential anemia associated with certain end-stage diseases like kidney failure and cancer [80, 81]. eNOS dysfunction is a known factor in kidney disease [82], and we propose that this has to do with insufficient sulfate synthesis by eNOS. When zeta potential falls (to less negative values) due to insufficient supplies of sulfates to maintain adequate negative charge around RBCs and other suspended particles, a compensatory mechanism sets in, for example through increased hepcidin synthesis and reduced erythropoietin-induced renewal of RBCs [83]. RBCs also experience a shorter lifespan when they are deficient in Ch-S [84], promoting a reduction in the hematocrit and therefore in blood viscosity.
It should be noted that the HS equation assumes homogeneity of the inner tube surface through which the fluid flows, but this situation might not apply at the capillary scale, where the electrical double layer (EDL) of vicinal water is strongly curved, polarized, anisotropic and surface conductive, and the interface is heterogeneous [85]. In addition, Bharti et al. [86] found that electroviscous effects on flow through cylindrical microchannels were stronger in shear-thinning liquids (for which viscosity decreases with increasing shear stress) than in Newtonian liquids (which display a linear response between applied shear stress and deformation rate). Human blood plasma is thought to behave as a shear-thinning liquid, just as do many biological solutions of protein and DNA [87].
Moreover, theoretical studies by Zhao et al. [78] indicate that the HS velocity of non-Newtonian fluids through cylindrical microchannels depends on the channel radius, an effect they attributed to nonlinear coupling among the electrostatics, channel geometry, and non-Newtonian hydrodynamics [78]. They also proposed a method for enhancement of electro-osmotic flows of power-law fluids under a combined DC and AC electric field [78], such as would be introduced by the beating heart.
Our final comment on the finding of EVSP-induced release of NO by endothelial cells relates to the biophysics of dissolved gases such as NO, CO, and H2S, which play complex signaling roles in blood homeostasis [68]. As noted in Section (The Exogenous Interfacial Water Stress (EIWS) theory of inflammation) above, Doshi and coworkers found that the size of a reduced-density water region near a hydrophobic surface depended strongly on the amounts and types of dissolved gases present [65], which could in turn influence the interaction between hydrophobic surfaces and the water in between them. They proposed further that lower-density water near a surface “should reduce their viscosity and boundary conditions for flow… from no-slip to partial or full-slip, which will have a significant impact on transport properties in small channels and on drag reduction in general” [65]. Their work maps directly to properties of the endothelial surface in capillaries, likely reflected as near frictionless flow or squeezing of RBCs through capillaries whose internal diameters of ca. 4–9 μm are nearly the same or even smaller than the average RBC diameter of ca. 7.8 μm [88].
Biosulfates as enablers of healthy blood flow
With the remarks made in the previous two sections, we can begin to see how biological sulfates in the vascular system can influence important properties relating to interfacial water structure and blood flow. In this section we will continue our discussion with a more detailed consideration of how biosulfates, most notably sGAGs and Ch-S, may play essential roles in maintaining blood flow and electrokinietic properties. As discussed earlier [49], sulfurylated glycolipids, sGAGs, and sterol sulfates, including Ch-S, are ubiquitous in biological systems. These biosulfates generate the net surface charge density, as well as the specific surface charge density, and are determinants of bio-membrane viscosity and permeability [49]. They are also expected to have strongly electron-donating inductive effects on interfacial water.
To start our more detailed discussion, we propose that the HSPGs decorating the endothelial glycocalyx layer (EGL) of capillary endothelial cells provide a bottle-brush architecture similar to that reported by Banquy et al. for a synthetic mimic of the lubricating protein lubricin [89]. Figure 4 provides a schematic of the bottle-brush architecture of the glycocalyx. We suggest that the roughness of the bottle-brush, HSPG-decorated EGL induces capillary behavior of the blood, as implied by the molecular theory of capillarity [90]. This capillarity, when aided by (a) the amphiphilic Ch-S in endothelial and erythrocyte membranes and blood plasma, (b) a high (negative) ZP, and (c) high interfacial water tension, effectively facilitates the electrokinetic pulling of deformable RBCs through the microvasculature.
Schematic of a red blood cell moving through a capillary, propelled by the force field generated by the voltage drop between the artery and the vein. The moving RBC creates an electromagnetic field that induces the release of nitric oxide from the capillary wall. This relaxes the vessel and further promotes flow
Sherman [91] has argued, through simple physical considerations based on Laplace’s equation of capillarity, that blood will flow out of capillaries into both the arteries and the veins when the surface tension is too high in the capillary, due to the inverse relationship between the size of the vessel and the pressure [91]. (We use the term “surface tension” here to refer to the amount of work needed to create an extra unit of liquid area at a liquid–vapor interface, while “interfacial tension” is understood to apply to the amount of work needed to create an extra unit of liquid area at a liquid-liquid or liquid–solid interface.) Interfacial water tension within a capillary lumen has both an endothelial water interface component and an erythrocyte water interface component, which may be represented by vectors normal to the endothelial and erythrocytic surfaces, respectively. We propose that, to avoid an intracapillary no flow or no reflow phenomenon, these vectors must dynamically negate each other’s force. We argue that anionic amphiphilic surfactants are essential to maintaining this balance. Cationic kosmotropes (water-structuring solutes) typically contract the surface (increase the surface tension), whereas anionic kosmotropes typically expand the surface (decrease the surface tension). The rate of surface tension lowering of anionic surface-active agents by electrolytes is largely determined by the charge of the added positive ion [92]. When an ionic surfactant is used to produce bubbles [93], the sign of microbubble charge is determined by the polar head of the surfactant.
More specifically, we propose that Ch-S acts as the key biosurfactant enabling healthy blood flow in the microvasculature, fulfilling a role similar to that played by sodium dodecyl sulfate (SDS) in SDS- polyacrylamide gel microelectrophoresis. In recent high-speed video studies of aqueous droplets moving electrophoretically through oil, Hamlin et al. found that, at relatively low or high surfactant concentration, the droplets responded to reversal of the electric field by quickly accelerating and then decelerating in the opposite direction, “concurrent with a transient rearrangement of tracer particles on the droplet’s surface” [94]. Of note, one of the surfactants, SDS, is structurally similar to the amphiphilic sterol sulfate, Ch-S. Hence, the role we have postulated for Ch-S in enhancing microvascular blood flow might involve facilitation of a metastable Marangoni-type fluctuation in mass transfer along the interface due to changing surface tension gradients. This effect would enable erythrocytes to flow, in conjunction with ELF EM energy provided under our hypothesis, to the EGL target by the EVSP. The thorough studies of Colacicco dealing with the role of SDS in the electrical potential at an oil–water interface [95] also have implications with respect to how Ch-S might be involved in generation and maintenance of the cellular resting electrical potential, action potential, electrokinetics, and zeta potentials.
Before closing this section, it is worth noting that Davidson and Seneff [49, 50] have proposed yet another way in which sulfur insufficiency may give rise to impaired blood flow. While the cardiovascular complications of diabetes are often attributed to loss of nitric-oxide-mediated vasodilation, an alternative pathophysiology was suggested, involving impaired microvascular perfusion due to (a) decreased fluidity and deformability of the RBC membrane related to biosulfate deficiency in the endothelial glycocalyx layer (EGL); and (b) increased capillary endothelial interfacial (surface) tension [49, 91]. This proposed mechanism disagrees with Burton’s basic assumption of flow being arrested by active arteriolar constriction [91–96].
If adequate supplies of sulfate are essential for maintaining blood vessel health, then the organism needs the capability to redistribute existing sulfate resources wherever needed in the cardiovascular system and to convert (oxidize) more-reduced sulfur compounds to sulfate if other sources of sulfate are insufficient. As mentioned above, we previously proposed an eNOS- and sunlight-catalyzed mechanism as a normal route for sulfate biosynthesis [16]. In the following three sections of the present paper, we will consider sulfate redistribution mechanisms and alternative, emergency sulfate synthesis pathways that generate, as side effects, various forms of blood vessel damage and other symptoms associated with cardiovascular disease.
Extracellular matrix sGAG turnover as a mechanism for sulfate redistribution
In the preceding section, we presented our hypothesis that Ch-S plays an essential role in enabling healthy blood flow through the capillaries. In this section, we discuss the deposition of cholesterol in the cardiovascular system when insufficient sulfate is available to make Ch-S. We will then propose a mechanism by which capillary levels of Ch-S can be replenished, in event of a deficiency, by recruitment of sulfate released by sGAG turnover in the extracellular matrix (ECM) of atherosclerotic regions.
Cholesterol is made by all cells in the body, but, being lipophilic, does not easily migrate from intracellular synthesis or storage sites to the plasma membrane. Sulfurylation will make the molecule amphiphilic, enabling it to facilitate blood flow through capillaries as discussed above, and reducing or eliminating the need to package cholesterol inside a lipoprotein particle for transport within the water-based cell cytoplasm. In addition, Ch-S shows a 10-fold higher rate of exchange between two lipid membranes than does cholesterol [97], which can be expected to greatly accelerate uptake by HDL, the lipoprotein that can remove cholesterol from the atheroma.
ApoE is the lipoprotein that escorts Ch-S from the Golgi apparatus to the plasma membrane, and ultimately delivers it to HDL-A1 [98]. ApoE’s antioxidant properties probably allow it to protect Ch-S in transit from oxidative damage. Indeed, ApoE promotes both cholesterol egress from the macrophages in the plaque and sulfurylation of the glycocalyx [98], and this hints that Ch-S might play an intermediary role. SULT2B1b is the specific sulfotransferase that sulfurylates cholesterol. It also sulfurylates oxysterols such as 7α-hydroxycholesterol and 27-hydroxycholesterol with nearly the same affinity [99]. Sulfurylation significantly reduces the cytotoxicity of these oxysterols, which are present in the atheroma. It is plausible that oxysterols, which are more water soluble than cholesterol itself, are exploited to deliver sulfate to the extracellular matrix.
Platelets also tend to accumulate in cardiovascular plaque, and, if supplied with activated sulfate in the form of PAPS, they exuberantly produce Ch-S [100]. They release it, specifically, to HDL-A1 [98]. They will accept no other lipid particle as the recipient. Significantly, HDL-A1 is the only form of HDL that is atheroprotective [101].
There is strong evidence from studies on plaque formation that cholesterol is actively recruited into the atheroma. Contrary to the widely perceived model that cholesterol passively enters the artery wall from the luminal side, a provocative paper published by Subbotin in 2012 [102] proposed that cardiovascular disease is initiated by neovascularization of the tunica intima, and that cholesterol is actively recruited directly from the newly formed capillaries. He also argues that this process begins early in life. We propose that this cholesterol is accumulated as a reserve supply, which will be conjugated with sulfate to form Ch-S as soon as sulfate becomes available.
A study on the export of cholesterol from macrophages in cardiovascular plaque into plasma discovered that only 40 % of the cholesterol was extracted into HDL-A1, and a significant percentage of the rest, surprisingly, was extracted by serum albumin [103], despite the fact that the cholesterol acceptor activity for albumin is 280-fold lower than that of apoA1. This supports our hypothesis that it is sulfoconjugated prior to export. Ch-S and DHEA sulfate bind tightly to albumin, in direct contrast to their unsulfurylated counterparts [30, 104]. Furthermore, increased uptake by albumin was associated with increased risk to cardiovascular events [103]. We hypothesize that this may reflect Ch-S depletion in albumin. DHEA sulfate, but not DHEA, inhibits NF-κB synthesis, suggesting that sulfate deficiency is a driver of inflammation [105].
Clearly, insufficient sulfate supplies will impair production and transport of Ch-S to the microvasculature to fulfill its proposed surfactant and electrophoretic functions as described in Section (Biosulfates as enablers of healthy blood flow) above. In the remainder of this section, we will discuss our hypothesis for a mechanism by which sulfate needed for Ch-S can be harvested by taking advantage of sGAG turnover in the extracellular matrix (ECM) of the cardiovascular system.
The sGAG-rich glycocalyx plays an important regulatory role in vascular permeability [106]. The sulfurylation patterns in these complex sugar chains are intricate and tightly regulated [107]. Changes in vascular glycocalyx structure regulate cellular adhesion, proliferation, migration and signalling in association with cardiovascular disease [108]. Extracellular proteoglycans, including sGAGs and the sulfate-free hyaluronan (HA), maintain hydration, mechanical properties, and concentration gradients of critical signalling molecules [109].
A remarkable series of investigations by Hauss et al. in the 1960’s [110, 111] measured the uptake of sulfur into sGAGs in the artery wall and its biological half-life as a function of age. Their studies revealed that the amount of sulfur that is taken up by the sGAGs is highest very early in life and decays exponentially over time, and that the retention cycle also decreases with age. However, the incorporation of sulfur into sGAGs in diseased regions where cardiovascular plaque accumulates is several fold higher than what would be predicted based on the age curve (see Fig. 5). The simplest explanation is that the atheroma is actively engaged in accumulating sGAGs for redistribution.
Sulfur Incorporation into GAGs with Age. Incorporation of 35Sulfur into chondroitin sulphuric acids (CSA) of the connective tissue of normal human aortae (x) and atherosclerotic human aortae (o) in in vitro experiment. (Redrawn from [110], with permission from Elsevier)
Hyaluronan (HA) concentration is increased dramatically in association with smooth muscle cell migration and proliferation following arterial injury, along with that of versican, a chondroitin-sulfate-enriched proteoglycan [112]. Both HA and versican are found in high concentrations in atherosclerotic plaque, particularly in association with the trailing edge of migrating smooth muscle cells. A postmortem study of stented arterial regions showed that chondroitin sulfate and HA were the predominant components of the neointimal proteoglycans [113], and vessel injury at the stent site was proposed as a factor inducing this buildup. Like the sulfate and sulfamidate groups of sGAGs, the multiple carboxylate groups attached to HA could also effect a structuring of the surrounding water [50], resulting in a clear solute free zone surrounding the smooth muscle cells [112]. Versican is tethered to the HA matrix, and when HA is degraded, the versican is also released into the surrounding space.
A pericellular matrix gel forms around these aggregated HA-versican fibrillar complexes produced by migrating smooth muscle cells but then appears to dissolve into the medium about one hour later [112]. The main purpose of the matrix may well be to produce materials (HA and versican) that can be degraded to enable redistribution of the building blocks to distant cells. This degradation can be accomplished with NO and/or one of its reactive oxidant derivatives. NO gas degrades heparin and heparan sulfate (HS) at concentrations as low as 400 ppm. NO oxidizes rapidly to HNO2, which can also break down HS chains that are attached to membrane proteins such as syndicans and glypicans [114]. On the other hand, peroxynitrite (ONOO−), the product of reaction of NO with superoxide, is particularly effective at breaking down HA, which will permit the release and redistribution of fragments of both HA and the attached chondroitin sulfate chains, thereby providing a sulfate source to replenish depleted supplies in the myocardial microvasculature.
In support of this hypothesis, Kruse et al. have reported that significant decreases in HS content and increases in the amounts of chondroitin sulfate/dermatan sulfate relative to HS are observed in association with elevated cholesterol levels in human aorta [115]. Thus, there is an inverse relationship between cholesterol retention and heparan sulfate supply. Furthermore, the observed redistribution of sGAG content away from HS (which inhibits smooth muscle cell proliferation) toward chondroitin sulfate-rich GAG is consistent with a move toward enabling smooth muscle proliferation to free up stored sulfate for possible use in generating Ch-S.
An in-depth discussion of the connection between diabetes and CVD is beyond the scope of this paper, but it is worth noting that the advanced glycation end products (AGEs) associated with hyperglycemia and diabetes also trigger processes that promote inflammation and smooth muscle cell proliferation, leading to generation of reactive oxygen species (ROS) and induction of an atherosclerotic profile [116]. Oxidative stress is a well-established risk factor for vascular disease [117]. H2S, in addition to its antioxidant effects, can protect from diabetes by increasing the cellular levels of phosphatidylinositol 3,4,5-trisphosphate (PIP3), a positive regulator of glucose metabolism [118].
Glutathione and GGT
In the preceding section, we discussed a possible mechanism by which the cardiovascular system could relieve a shortage of Ch-S and avoid a crisis in capillary blood flow by redistributing sulfate from sGAGs. We will now turn our attention to ways in which the total biosulfate supply can be replenished by “emergency” conversion of less-oxidized sulfur compounds. As noted in Section (Evidence for a role of sulfur deficiency in atherosclerosis) above, we have proposed elsewhere [16] that, under normal, non-inflammatory conditions, sulfate synthesis from thiol- and sulfane-type substrates (HS−, glutathione persulfate, thiosulfate, etc.) in RBCs, platelets, and other endothelial cells can be facilitated by eNOS and sunlight. In the present section, we will consider other sulfate biosynthesis routes from thiols that can be utilized if sunlight exposure is inadequate or if eNOS function is impaired through exposure to environmental toxicants.
Sulfur homeostasis in plants is a good model for sulfur management in biological systems more generally [119]. Plants utilize glutathione (GSH) as the main form of reduced sulfur storage [120]. The concentration of GSH is much higher than the concentration of free cysteine in plant cells, and this may be because it is less reactive than free cysteine, and therefore more attractive for sulfur storage. The same may be true for animals. A study exposing rats to a GSH synthase inhibitor resulted in a three-fold reduction in tissue GSH along with indicators of oxidative stress and hypertension. This was linked to reduced synthesis of nitric oxide (NO) in the vascular wall [121].
This relates to the observation, now thoroughly confirmed, that elevated γ-glutamyl transferase (GGT), an enzyme that breaks GSH down into its component amino acids, is an outstanding serum marker for a host of modern diseases, including liver dysfunction, cardiovascular disease [122, 123], digestive disorders, Alzheimer’s disease, metabolic syndrome, obesity, diabetes, musculoskeletal disorders, cancer and death [124–127], with high significance. Ischemia depletes glutathione in both liver [128] and brain [129]. Elevated serum GGT strongly predicts carotid plaque, which, in turn, is highly predictive of future cardiovascular disease [130].
While GSH is mostly known as an antioxidant, extracellular GSH can exhibit a pro-oxidant effect in the presence of GGT [131]. GGT, by splitting off glutamate, produces cysteinyl glycine, which is more acidic than glutathione (pKa 6.4 vs. 8.56, respectively) [132], making it more reactive in converting Fe+3 to Fe+2. However, another factor that may be at play is the fact that the carboxylate group of the glutamate residue in GSH chelates with iron, reducing its bioavailability for reaction with the sulfhydryl group of the cysteine moiety [133]. GGT separates the glutamate from the other two amino acids, facilitating iron reduction to Fe+2 and subsequent redox reactions. In the presence of free iron (Fe+3), this can lead to the Fenton reaction and subsequent production of superoxide.
While the research literature does not provide any explanation for a possible beneficial effect of this superoxide production, we propose that it is necessary in order to promote oxidation of the sulfur atom in cysteinyl-glycine to sulfate. We hypothesize that cysteine is liberated from GSH for subsequent breakdown to supply sulfur as a substrate for sulfate production. In oxidative cysteine catabolism, cysteine dioxygenase oxidizes the sulfur in cysteine, leading ultimately to the production of taurine, pyruvate and sulfate [134]. Cysteine might also be converted to homocysteine and subsequently homoycysteine thiolactone, which can also be substrate for sulfate synthesis through a pathway requiring vitamin C and vitamin A as well as superoxide [17]. Elevated serum homocysteine is a strong risk factor for cardiovascular disease [14, 135–137]. In fact, homocysteine is known to induce vascular oxidation damage [138, 139]. We propose that the need for homocysteine and for superoxide is driven by the insufficient supply of Ch-S to the tissues.
Another available pathway is to produce hydrogen sulfide gas (H2S) from cysteine by enzymatic action of cystathionine γ lyase (CSE). H2S has only relatively recently been recognized as a signaling gas on par with nitric oxide [68], and it has been shown to induce vascular relaxation as well [140]. H2S offers similar protective effects as NO without the issue of reacting with superoxide to produce the toxic metabolite ONOO− [141–143]. H2S in small concentrations promotes angiogenesis and protects against both atherosclerosis and hypertension [144]. CSE is present in both vascular smooth muscle cells (SMCs) [145] and blood lymphocytes [68]. It has only recently been realized that H2S can be used by mammalian mitochondria as an energy source during times of hypoxia.
In experiments on vascular smooth muscle cells, it was shown that stress-induced calcium entry causes CSE to migrate to the mitochondria, where cysteine is already available in high concentration [146]. These authors wrote: “The notion that eukaryotes do not need H2S in the energy metabolism process should be revised. In SMCs, mitochondrial CSE translocation and H2S production confer resistance to hypoxia by increasing ATP synthesis.” We argue that, in addition to this, it is also an important substrate for sulfate synthesis. The CSE enzymatically produces H2S from cysteine, along with pyruvate as a by-product, another energy source that also reduces electron leakage. H2S is quickly oxidized by the electron transport chain to sulfate and thiosulfate [146], and helps maintain ATP levels in a hypoxic environment. Thiosulfate can be converted to sulfate in a reaction catalyzed by thioredoxin reductase, which can be used in certain microorganisms and possibly even in mammalian cells as an energy source for further ATP production, restoring H2S and completing the cycle [147].
We can now explain the refractory statin resistance observed in the context of certain highly inflammatory conditions such as lupus or kidney failure. Here, cardiovascular mortality is increased by up to 33 to 50 fold [148], yet, despite this, serum LDL is often not elevated, or may even be abnormally low. A recent investigation revealed that, in these cases, smooth muscle cells in the aorta use coenzyme A reductase to synthesize their own cholesterol for local storage, and these cells show resistance to statin therapy compared to hepatic cells [3]. This suggests to us that the cholesterol is desperately needed to maintain blood stability.
Although supportive evidence of our hypothesis is strong, further in vitro studies specifically addressing the concept of cholesterol sulfate’s role in protection from atherosclerosis are needed. In addition, clinical trials involving dietary modification to include enrichment in sulfur-containing amino acids and other sulfur sources, along with increased sun exposure to the skin and avoidance of environmental toxicants, will be an important step towards validating our hypothesis.
Conclusion
In this paper, we have put forward the novel hypothesis that impaired cholesterol sulfate supply to the heart is the key pathology behind atherosclerosis. This explains why regions of the artery wall with increased sulfate uptake and recycling in the endothelial glycocalyx also have excess cholesterol storage. We offer key insight into the importance of sulfates to vascular health through arguments based on the unique properties of water and the EIWS theory of disease. We hypothesize that CYP enzyme disruption by multiple environmental toxicants may be a significant factor in atherosclerosis, as eNOS contains a CYP structural motif that is likely essential for sulfate synthesis. We argue that the accumulation of cholesterol in the artery wall is a reflection of impaired cholesterol transport due to low bioavailability of sulfate to the vasculature. The constant remodeling of the extracellular matrix in occluded arterial regions reflects the need to break down and distribute to the capillaries the sGAGs that must populate the glycocalyx to maintain vascular health and enable blood flow. Supportive evidence comes from the observation that the differentiation, mobilization, and proliferation of SMCs in the artery wall is accompanied by rapid synthesis and release of chondroitin sulfate.
While the view that atherosclerosis is an inflammatory disease is gaining in popularity today [149], anti-inflammatory pharmaceutical drugs increase the risk to heart disease [150]. Elevated homocysteine is a strong risk factor for atherosclerosis, yet attempts to correct it have met with failure. Administration of B vitamin supplements in an attempt to reduce serum homocysteine has been effective, but did not result in any clinical improvement in cardiac disease risk [151–153]. All of these seemingly contradictory results can be explained if we assume the point of view that the inflammation is needed to induce superoxide production, which will allow sulfate production with homocysteine, H2S, and superoxide as substrates. Any attempt to reduce either the superoxide or the homocysteine levels will further impair the supply of sulfate to the capillary glycocalyx.
Platelet complement activation, a key factor in atherogenesis, leads to inflammation and thrombosis, both of which may be necessary for the intense regeneration of sulfate at the injury site and its mobilization, in order to restore vascular health. A recent review article on platelet activation summarized as follows: “We hypothesize that platelets focus complement activation to sites of vascular injury, and that interactions between platelets and the complement system contribute to acute and chronic inflammation and thrombosis.” ([154], p. 5). We have argued here that the inflammation renews sulfate supplies and the thrombosis reduces viscosity. Vascular flow is improved, and this leads to nitric oxide production, mediated by EVSP. Nitric oxide reaction products break down and redistribute locally-produced sGAGs.
Based on a review of the literature, this paper describes several novel means by which the biosulfates play essential roles in enabling microvascular blood flow, including their impact on the hemorheological parameters - the zeta potential, streaming potential, capillarity, viscosity, and interfacial tension, without which a “no flow” situation would surely exist. It argues that lifestyle is causal and simple lifestyle changes may have profound benefits. These include eating strictly organic sulfur-rich foods and making special efforts to avoid environmental toxicants and to promote sun exposure to the skin without sunscreen.
Notes
Throughout this paper, as a significant nomenclatural point, we have adopted use of the words “sulfurylate” and “sulfurylation,” in strong preference to the words “sulfate”, “sulfation”, and “sulfonation”. Biochemically, sulfate ester and sulfamidate formation occur most commonly via sulfuryl group transfer. Use of the term “sulfation” is likely to only apply to in vitro electrophilic aromatic substitution and olefinic addition reactions, which involve carbocation intermediates. Whereas in vivo only 3 oxygen atoms transfer with the sulfuryl group to an acceptor ROH or RNH2 molecule to produce a sulfate ester or sulfamidate, respectively. Such a mechanism of “sulfuryl” group transfer via “sulfurylation” has important mechanistic implications, which are highly-analogous to “phosphoryl” group transfer via “phosphorylation” in organophosphorus chemistry.
Abbreviations
- 25HCS:
-
25-hydroxycholesterol sulfate
- AGEs:
-
Advanced glycation endproducts
- CDs:
-
Coherence domains
- CSE:
-
Cystathionine gamma lyase
- CYP:
-
Cytochrome P450
- Ch-S:
-
Cholesterol sulfate
- ECM:
-
Extracellular matrix
- EDL:
-
Electrical double layer
- EDRF:
-
Endothelial-derived relaxing factor
- EGL:
-
Endothelial glycocalyx layer
- EIWS:
-
Exogenous interfacial water stress
- EVSP:
-
Electrokinetic vascular streaming potential
- EZ:
-
Exclusion zone
- GAGs:
-
Glycosaminoglycans
- GGT:
-
Gamma glutamyl transferase
- GSH:
-
Glutathione
- HA:
-
Hyaluronan
- HDL:
-
High density lipoprotein
- HS:
-
Heparan sulfate
- HSPGs:
-
Heparan sulfate proteoglycans
- LDL:
-
Low density lipoprotein
- MI:
-
Myocardial infarction
- NDSTs:
-
N-deacetylase/N-sulfotransferases
- NF:
-
Necrosis factor
- NO:
-
Nitric oxide
- PAPS:
-
3′-phosphoadenosine-5′-phosphosulfate
- PDGF:
-
Platelet derived growth factor
- PPAR:
-
Peroxisome proliferator-activated receptor
- RBCs:
-
Red blood cells
- ROS:
-
Reactive oxygen species
- SDS:
-
Sodium dodecyl sulfate
- SMCs:
-
Smooth muscle cells
- VEGF:
-
Vascular endothelial growth factor
- eNOS:
-
Endothelial nitric oxide synthase
References
Anderson KM, Odell PM, Wilson PWF, Kannel WB. Cardiovascular disease risk profiles. Am Heart J. 1991;121(1, Part 2):293–8.
Kalantar-Zadeh K, Block G, Humphreys MH, Kopple JD. Reverse epidemiology of cardiovascular risk factors in maintenance dialysis patients. Kidney Int. 2003;63:793–808.
Chen Y, Ku H, Zhao L, Wheeler DC, Li L-C, Li Q, et al. Inflammatory stress induces statin resistance by disrupting 3-hydroxy-3-methylglutaryl-CoA reductase feedback regulation. Arterioscler Thromb Vasc Biol. 2014;34:365–76.
Sarnak MJ, Levey AS, Schoolwerth AC, Coresh J, Culleton B, Hamm LL, et al. Kidney disease as a risk factor for development of cardiovascular disease. Circulation. 2003;108:2154–69.
Yudkin JS, Kumari M, Humphries SE, Mohamed-Ali V. Inflammation, obesity, stress and coronary heart disease: is interleukin-6 the link? Atherosclerosis. 2000;148(2):209–14.
Danesh J, Whincup P, Walker M, Lennon L, Thomson A, Appleby P, et al. Low grade inflammation and coronary heart disease: prospective study and updated meta-analyses. BMJ. 2000;321:199.
Koenig W. Inflammation and coronary heart disease: an overview. Cardiol Rev. 2001;9(1):31–5.
Kingston R, Kelly CJ, Murray P. The therapeutic role of taurine in ischaemia-reperfusion injury. Curr Pharm Des. 2004;10(19):2401–10.
Zimmermann J, Herrlinger S, Pruy A, Metzger T, Wanner C. Inflammation enhances cardiovascular risk and mortality in hemodialysis patients. Kidney Int. 1999;55(2):648–58.
Qureshi AR, Alvestrand A, Divino-Filho JC, Gutierrez A, Heimbürger O, Lindholm B, et al. Inflammation, malnutrition, and cardiac disease as predictors of mortality in hemodialysis patients. J Am Soc Nephrol. 2002;13 Suppl 1:S28.
Danesh J, Collins R, Peto R. Chronic infections and coronary heart disease: is there a link? Lancet. 1997;350(9075):430–6.
Ravnskov U, McCully KS. Infections may be causal in the pathogenesis of atherosclerosis. Am J Med Sci. 2012;344(5):391–4.
Mann GV. Effects of sulfur compounds on hypercholesteremia and growth in cysteine-deficient monkeys. Am J Clin Nutr. 1960;8:491–7.
McCully KS. Vascular pathology of homocysteinemia: implications for the pathogenesis of arteriosclerosis. Am J Pathol. 1969;56(1):111–28.
Benavides GA, Squadrito GL, Mills RW, Patel HD, Isbell TS, Patel RP, et al. Hydrogen sulfide mediates the vasoactivity of garlic. Proc Natl Acad Sci U S A. 2007;104(46):17977–82.
Seneff S, Lauritzen A, Davidson R, Lentz-Marino L. Is endothelial nitric oxide synthase a moonlighting protein whose day job is cholesterol sulfate synthesis? Implications for cholesterol transport, diabetes and cardiovascular disease. Entropy. 2012;14:2492–530.
McCully KS. Chemical pathology of homocysteine. V. Thioretinamide, thioretinaco, and cystathionine synthase function in degenerative diseases. Ann Clin Lab Sci. 2011;41(4):300–12.
Grimes DS, Hindle E, Dyer T. Sunlight, cholesterol and coronary heart disease. Q J Med. 1996;89:579–89.
MacPherson A, Bacsó J. Relationship of hair calcium concentration to incidence of coronary heart disease. Sci Total Environ. 2000;255(1–3):11–9.
Wood AD, Secombes KR, Thies F, Aucott L, Black AJ, Mavroeidi A, et al. Vitamin D3 supplementation has no effect on conventional cardiovascular risk factors: A parallel-group, double-blind, placebo-controlled RCT. J Clin Endocrinol Metab. 2012;97(10):3557–68.
Tian Q-Y, Sun D-H, Zhao M-G, Zhang W-H. Inhibition of nitric oxide synthase (NOS) underlies aluminum-induced inhibition of root elongation in Hibiscus moscheutos. New Phytol. 2007;174(2):322–31.
Marletta MA. Nitric oxide synthase: aspects concerning structure and catalysis. Cell. 1994;78(6):927–30.
Jeffery EH, Jansen HT, Dellinger JA. In viva interactions of aluminum with hepatic cytochrome P-450 and metallothionein. Fundam Appl Toxicol. 1987;8:541–8.
Alexidis AN, Rekka EA, Kourounakis PN. Influence of mercury and cadmium intoxication on hepatic microsomal CYP2E and CYP3A subfamilies. Res Commun Mol Pathol Pharmacol. 1994;85(1):67–72.
Hesham M, Korashy HM, El-Kadi AO. Modulation of TCDD-mediated induction of cytochrome P450 1A1 by mercury, lead, and copper in human HepG2 cell line. Toxicol in Vitro. 2008;22(1):154–8.
Anwar-Mohamed A, El-Sherbeni AA, Kim SH, Althurwi HN, Zordoky BN, El-Kadi AO. Acute arsenic toxicity alters cytochrome P450 and soluble epoxide hydrolase and their associated arachidonic acid metabolism in C57Bl/6 mouse heart. Xenobiotica. 2012;42(12):1235–47.
Samsel A, Seneff S. Glyphosate’s suppression of cytochrome P450 enzymes and amino acid biosynthesis by the gut microbiome: Pathways to modern diseases. Entropy. 2013;15:1416–63.
Samsel A, Seneff S. Glyphosate, pathways to modern diseases II: Celiac sprue and gluten intolerance. Interdiscip Toxicol. 2013;6(4):159–84.
Meredith PA, Campbell BC, Moore MR, Goldberg A. The effects of industrial lead poisoning on cytochrome P450 mediated phenazone (antipyrine) hydroxylation. Eur J Clin Pharmacol. 1977;12(3):235–9.
Strott CA, Higashi Y. Cholesterol sulfate in human physiology: what’s it all about? J Lipid Res. 2003;44:1268–78.
Hobkirk R. Steroid sulfotransferases and steroid sulfate sulfatases: characteristics and biological roles. Can J Biochem Cell Biol. 1985;63(11):1127–44.
Bergner EA, Shapiro LJ. Increased cholesterol sulfate in plasma and red blood cell membranes of steroid sulfatase deficient patients. J Clin Endocrinol Metab. 1981;53(1):221–3.
Xu L, Shen S, Ma Y, Kim JK, Rodriguez-Agudo D, Heuman DM, et al. 25-Hydroxycholesterol-3-sulfate attenuates inflammatory response via PPAR signaling in human THP-1 macrophages. Am J Physiol Endocrinol Metab. 2012;302(7):E788–99.
Ma Y, Xu L, Rodriguez-Agudo D, Li X, Heuman DM, Hylemon PB, et al. 25-Hydroxycholesterol-3-sulfate regulates macrophage lipid metabolism via the LXR/SREBP-1 signaling pathway. Am J Physiol Endocrinol Metab. 2008;295:E1369–79.
Ren S, Li X, Rodriguez-Agudo D, Gil G, Hylemon P, Pandak WM. Sulfated oxysterol, 25HC3S, is a potent regulator of lipid metabolism in human hepatocytes. Biochem Biophys Res Commun. 2007;360:802–8.
Kereiakes DJ, Topol EJ, George BS, Stack RS, Abbottsmith CW, Ellis S, et al. Myocardial infarction with minimal coronary atherosclerosis in the era of thrombolytic reperfusion. J Am Coll Cardiol. 1991;17:304–12.
Avila JL, Rojas M, Avila A. Cholesterol sulphate-reactive autoantibodies are specifically increased in chronic chagasic human patients. Clin Exp Immunol. 1996;103:40–6.
Freitas HFG, Chizzola PR, Paes AT, Lima ACP, Mansur AJ. Risk stratification in a Brazilian hospital-based cohort of 1220 outpatients with heart failure: role of Chagas’ heart disease. Int J Cardiol. 2005;102(2):239–47.
Laranja FS, Dias E, Nobrega G, Miranda A. Chagas’ disease: a clinical, epidemiologic, and pathologic study. Circulation. 1956;14:1035–60.
Collard CD, Gelman S. Pathophysiology, clinical manifestations, and prevention of IschemiaReperfusion injury. Anesthesiology. 2001;94(6):1133–8.
Seal JB, Gewertz BL. Vascular dysfunction in ischemia-reperfusion injury. Ann Vasc Surg. 2005;19:572–84.
Chen LW, Egan L, Li ZW, Greten FR, Kagnoff MF, Karin M. The two faces of IKK and NF-κB inhibition: prevention of systemic inflammation but increased local injury following intestinal ischemia-reperfusion. Nat Med. 2003;9:575–81.
Reitsma S, Slaaf DW, Vink H, van Zandvoort MAMJ, oude Egbrink MGA. The endothelial glycocalyx: composition, functions, and visualization. Pflugers Arch Eur J Physiol. 2007;454:345–59.
Armulik A, Abramsson A, Betsholtz C. Endothelial/pericyte interactions. Circ Res. 2005;97:512–23.
Birbrair A, Zhang T, Wang Z-M, Messi ML, Mintz A, Delbono O. Pericytes at the intersection between tissue regeneration and pathology. Clin Sci (Lond). 2015;128(2):81–93.
Abramsson A, Kurup S, Busse M, Yamada S, Lindblom P, Schallmeiner E, et al. Defective N-sulfation of heparan sulfate proteoglycans limits PDGF-BB binding and pericyte recruitment in vascular development. Genes Dev. 2007;21:316–31.
Malojčić G, Glockshuber R. The PAPS-independent aryl sulfotransferase and the alternative disulfide bond formation system in pathogenic bacteria. Antioxid Redox Signal. 2010;13:1247–59.
Grobe K, Ledin J, Ringvall M, Holmborn K, Forsberg E, Esko JD, et al. Heparan sulfate and development: Differential roles of the N-acetylglucosamine N-deacetylase/N-sulfotransferase isozymes. Biochim Biophys Acta. 2002;1573:209–15.
Davidson RM, Seneff S. The initial common pathway of inflammation, disease, and sudden death. Entropy. 2012;14:1399–442.
Davidson RM, Lauritzen A, Seneff S. Biological water dynamics and entropy: a biophysical origin of cancer and other diseases. Entropy. 2013;15(9):3822–76.
Wall S. The history of electrokinetic phenomena. Curr Opin Colloid Interface Sci. 2010;15:119–24.
Ball P. Water as an active constituent in cell biology. Chem Rev. 2008;108:74–108.
Ball P. Nanobubbles are not a superficial matter. Chem Phys Chem. 2013;13:2173–7.
Fogarty AC, Duboue-Dijon E, Sterpone F, Hynes JT, Laage D. Biomolecular hydration dynamics: a jump model perspective. Chem Soc Rev. 2013;42:5672–83.
Pollack GH. Cells, gels and the engines of life. Ebner and Sons: New York, NY, USA; 2001.
Pollack GH. The fourth phase of water: beyond solid, liquid, and vapor. 1st ed. New York, NY, USA: Ebner & Sons; 2013.
Guo F, Friedman JM. Charge density-dependent modifications of hydration shell waters by Hofmeister ions. J Am Chem Soc. 2009;131:11010–8.
Tielrooij KJ, Garcia-Araez N, Bonn M, Bakker HJ. Cooperativity in ion hydration. Science. 2010;328:10069.
Ling GN. A revolution in the physiology of the living cell. Krieger Pub. Co: Malibar, FL USA; 1992.
Ling GN. A new theoretical foundation for the polarized-oriented multilayer theory of cell water and for inanimate systems demonstrating long-range dynamic structuring of water molecules. Physiol Chem Phys Med NMR. 2003;35(2):91–130.
Dahlke EE, Olson RM, Leverentz HR, Truhlar DG. Assessment of the accuracy of density functionals for prediction of relative energies and geometries of low-lying isomers of water hexamers. J Phys Chem A. 2008;112:3976–84.
Del Giudice E, Tedeschi A, Vitiello G, Voeikov V. Coherent structures in liquid water close to hydrophilic surfaces. J Phys Conf Ser. 2013;442:012–28.
Preparata G. QED coherence and matter. Singapore: World Scientific; 1995.
Duignan TT, Parsons DF, Ninham BW. A continuum solvent model of the multipolar dispersion solvation energy. J Phys Chem B. 2013;117:9412–20.
Doshi DA, Watkins EB, Israelachvili JN, Majewski J. Reduced water density at hydrophobic surfaces: effect of dissolved gases. Proc Natl Acad Sci U S A. 2005;102:9458–62.
Shatalov VM. Mechanism of the biological impact of weak electromagnetic fields and the in vitro effects of blood degassing. Biophysics. 2012;57:808–13.
Bunkin NF, Ninham BW, Ignatiev PS, Kozlov VA, Shkirin AV, Starosvetskij AV. Long-living nanobubbles of dissolved gas in aqueous solutions of salts and erythrocyte suspensions. J Biophotonics. 2011;4:150–64.
Wang R. Two’s company, three’s a crowd: can H2S be the third endogenous gaseous transmitter? FASEB J. 2002;16(13):1792–8.
Grant D, Long WF, Moffat CF, Williamson FB. A study of Ca(2+)-heparin complex-formation by polarimetry. Biochem J. 1992;282(Pt 2):601–4.
O’Brien JT, Prell JS, Bush MF, Williams ER. Sulfate ion patterns water at long distance. J Am Chem Soc. 2010;132:8248–9.
Yoo H, Paranji R, Pollack GH. Impact of hydrophilic surfaces on interfacial water dynamics probed with NMR spectroscopy. J Phys Chem Lett. 2011;2(6):532–6.
Rohani M, Pollack GH. Flow through horizontal tubes submerged in water in the absence of a pressure gradient: mechanistic considerations. Langmuir. 2013;29:6556–61.
Figueroa XA, Pollack GH. Exclusion zone formation from discontinuous Nafion surfaces. Int J Des Nat Ecodyn. 2011;6:286–96.
Bunkin NF, Ignatiev PS, Kozlov VA, Shkirin AV, Zakharov SD, Zinchenko AA. Studies of the phase states of water close to Nafion interface. Water. 2013;4:129–54.
Zhao Q, Zheng J, Chai B, Pollack GH. Unexpected effect of light on colloidal crystal spacing. Langmuir. 2008;24:1250–5.
Trivedi DP, Hallock KJ, Bergethon PR. Electric fields caused by blood flow modulate vascular endothelial electrophysiology and nitric oxide production. Bioelectromagnetics. 2013;34(1):22–30.
Ignarro LJ, Buga GM, Wood KS, Byrns RE, Chaudhuri G. Endothelium-derived relaxing factor produced and released from artery and vein is nitric oxide. PNAS USA. 1987;84(24):9265–9.
Zhao C, Yang C. Electroosmotic flows of non-Newtonian power law fluids in a cylindrical microchannel. Electrophoresis. 2013;34:662–7.
Delgado AV, González-Caballero F, Hunter RJ, Koopal LK, Lyklema J. Measurement and interpretation of electrokinetic phenomena. Pure Appl Chem. 2005;77:1753–805.
Wander K, Shell-Duncan B, McDade TW. Evaluation of iron deficiency as a nutritional adaptation to infectious disease: an evolutionary medicine perspective. Am J Hum Biol. 2009;21(2):172–9.
Zarychanski R, Houston DS. Anemia of chronic disease: a harmful disorder or an adaptive, beneficial response? CMAJ. 2008;179(4):333–7.
Forbes MS, Thornhill BA, Park MH, Chevalier RL. Lack of endothelial nitric-oxide synthase leads to progressive focal renal injury. Am J Pathol. 2007;170(1):87–99.
Ganz T. Hepcidin, a key regulator of iron metabolism and mediator of anemia of inflammation. Blood. 2003;102(3):783–8.
Bleau G, Bodley FH, Longpré J, Chapdelaine A, Roberts KD. Cholesterol sulfate. I. Occurrence and possible biological functions as an amphipathic lipid in the membrane of the human erythrocyte. Biochim Biophys Acta Biomembranes. 1974;352(1):1–9.
Butt H-J, Graf K, Kappl M. Physics and chemistry of interfaces. Weinheim, Germany: Wiley-VCH Verlag & Co. KGaA; 2003.
Bharti RP, Harvie DJE, Davidson MR. Electroviscous effects in steady fully developed flow of a power-law liquid through a cylindrical microchannel. Int J Heat Fluid Flow. 2009;30:804–11.
Brust M, Schaefer C, Doerr R, Pan L, Garcia M, Arratia PE, et al. Rheology of human blood plasma: viscoelastic versus newtonian behavior. Phys Rev Lett. 2013;110:078305.
Guyton AC, Hall JE. Textbook of medical physiology. 10th ed. Philadelphia: W. B. Saunders Company; 2000. p. 162 and 382.
Banquy X, Burdynska J, Lee DW, Matyjaszewski K, Israelachvili J. Bioinspired bottle-brush polymer exhibits low friction and Amontons-like behavior. J Am Chem Soc. 2014;136:6199–202.
Rowlinson JS, Widom B. Molecular theory of capillarity. Oxford, UK: Oxford Press; 1989.
Sherman IA. Interfacial tension effects in the microvasculature. Microvasc Res. 1981;22:296–307.
Burcik EJ, Vaughn CR. The effect of pH on the rate of surface tension lowering. J Colloid Sci. 1951;6:522–7.
Yoon R-H, Yordan JL. Zeta-potential measurements on microbubbles generated using various surfactants. J Colloid Interface Sci. 1986;113:430–8.
Hamlin BS, Ristenpart WD. Transient reduction of the drag coefficient of charged droplets via the convective reversal of stagnant caps. Phys Fluids. 2012;24(1):012101.
Colacicco G. Electrical potential at an oil/water interface. Nature. 1965;207:936–8.
Burton AC. On the physical equilibrium of the small blood vessels. Amer J Physiol. 1951;164:319–29.
Rodrigues SF, Granger DN. Role of blood cells in ischaemia reperfusion induced endothelial barrier failure. Cardiovascular Res. 2010;87:291–9.
Paka L, Kako Y, Obunike JC, Pillarisetti S. Apolipoprotein E containing high density lipoprotein stimulates endothelial production of heparan sulfate rich in biologically active heparin-like domains: a potential mechanism for the anti-atherogenic actions of vascular apolipoprotein E. J Biol Chem. 1999;274:4816–23.
Fuda H, Javitt NB, Mitamura K, Ikegawa S, Strott CA. Oxysterols are substrates for cholesterol sulfotransferase. JLR. 2007;48:1343–52.
Yanai H, Javitt NB, Higashi Y, Fuda H, Strott CA. Expression of cholesterol sulfotransferase (SULT2B1b) in human platelets. Circulation. 2004;109(1):92–6.
Navab M, Reddy ST, Van Lenten BJ, Fogelman AM. HDL and cardiovascular disease: atherogenic and atheroprotective mechanisms. Nat Rev Cardiol. 2011;8(4):222–32.
Subbotin VM. Neovascularization of coronary tunica intima (DIT) is the cause of coronary atherosclerosis. Lipoproteins invade coronary intima via neovascularization from adventitial vasa vasorum, but not from the arterial lumen: a hypothesis. Theor Biol Med Model. 2012;9:11.
Li XM, Tang WH, Mosior MK, Huang Y, Wu Y, Matter W, et al. Paradoxical association of enhanced cholesterol efflux with increased incident cardiovascular risks. Arterioscler Thromb Vasc Biol. 2013;33(7):1696–705.
Plager JE. The binding of androsterone sulfate, etiocholanolone sulfate, and dehydroisoandrosterone sulfate by human plasma protein. J Clin Invest. 1965;44:1234–9.
Iwasaki Y, Asai M, Yoshida M, Nigawara T, Kambayashi M, Nakashima N. Dehydroepiandrosterone-sulfate inhibits nuclear factor-κB- dependent transcription in hepatocytes, possibly through antioxidant ef- fect. J Clin Endocrinol Metab. 2004;89(7):3449–54.
Nieuwdorp M, Meuwese MC, Vink H, Hoekstra JBL, Kastelein JJP, Stroes ESG. The endothelial glycocalyx: a potential barrier between health and vascular disease. Curr Opin Lipidol. 2005;16(5):507–11.
Lamanna WC, Kalus I, Padva M, Baldwin RJ, Merry CL, Dierks T. The heparanome – the enigma of encoding and decoding heparan sulfate sulfation. J Biotechnol. 2007;129(2):290–307.
Gupta V, Grande-Allen KJ. Effects of static and cyclic loading in regulating extracellular matrix synthesis by cardiovascular cells. Cardiovasc Res. 2006;72:375–83.
Kennett EC, Chuang CY, Degendorfer G, Whitelock JM, Davies MJ. Mechanisms and consequences of oxidative damage to extracellular matrix. Biochem Soc Trans. 2011;39(5):1279–87.
Hauss WH, Junge-Hülsing G, Holländer HJ. Changes in metabolism of connective tissue associated with ageing and arterio- or atherosclerosis. J Atheroscler Res. 1962;2(1–2):50–61.
Hauss WH, Gerlach U, Junge-Hülsing G, Themann H, Wirth W. Studies on the “nonspecific mesenchymal reaction” and the “transit zone” in myocardial lesions and atherosclerosis. Ann N Y Acad Sci. 1969;156(1):207–18.
Evanko SP, Angello JC, Wight TN. Formation of hyaluronan- and versican-rich pericellular matrix is required for proliferation and migration of vascular smooth muscle cells. Arterioscler Thromb Vasc Biol. 1999;19:1004–13.
Farb A, Sangiorgi G, Carter AJ, Walley VM, Edwards WD, Schwartz RS, et al. Pathology of acute and chronic coronary stenting in humans. Circulation. 1999;99:44–52.
Tumova S, Woods A, Couchman JR. Heparan sulfate proteoglycans on the cell surface: versatile coordinators of cellular functions. Int J Biochem Cell Biol. 2000;32(3):269–88.
Kruse R, Merten M, Yoshida K, Schmidt A, Völker W, Buddecke E. Cholesterol-dependent changes of glycosaminoglycan pattern in human aorta. Basic Res Cardiol. 1996;91(5):344–52.
Basta G, Schmidt AM, de Caterina R. Advanced glycation end products and vascular inflammation: implications for accelerated atherosclerosis in diabetes. Cardiovasc Res. 2004;63:582–92.
Förstermann U. Oxidative stress in vascular disease: causes, defense mechanisms and potential therapies. Nat Rev Cardiol. 2008;5:338–49.
Manna P, Jain SK. Hydrogen sulfide and L-cysteine increase phosphatidylinositol 3,4,5-trisphosphate (PIP3) and glucose utilization by inhibiting phosphatase and tensin homolog (PTEN) protein and activating phosphoinositide 3-kinase (PI3K)/serine/threonine protein kinase (AKT)/protein kinase Cζ/λ (PKCζ/λ) in 3T3l1 adipocytes. J Biol Chem. 2011;286(46):39848–59.
Lewandowska M, Sirko A. Recent advances in understanding plant response to sulfur-deficiency stress. Acta Biochim Pol. 2008;55(3):457–71.
Rennenberg H, Schmitz K, Bergmann L. Long-distance transport of sulfur in Nicotiana tabacum. Planta. 1979;147:57–62.
Vaziri ND, Wang XQ, Oveisi F, Rad B. Induction of oxidative stress by glutathione depletion causes severe hypertension in normal rats. Hypertension. 2000;36:142–6.
Wannamethee G, Ebrahim S, Shaper AG. Gamma-glutamyltransferase: determinants and association with mortality from ischemic heart disease and all causes. Am J Epidemiol. 1995;142:699–708.
Emdin M, Passino C, Michelassi C, Titta F, L’Abbate A, Donato L, et al. Prognostic value of serum gamma-glutamyl transferase activity after myocardial infarction. Eur Heart J. 2001;22:1802–7.
Claessen H, Brenner H, Drath C, Arndt V. Gamma-glutamyltransferase and disability pension: a cohort study of construction workers in Germany. Hepatology. 2010;51(2):482–90.
Lee DS, Evans JC, Robins SJ, Wilson PW, Albano I, Fox CS, et al. Gamma glutamyl transferase and metabolic syndrome, cardiovascular disease, and mortality risk: the Framingham Heart Study. Arterioscler Thromb Vasc Biol. 2007;27:127–33.
Corti A, Franzini M, Paolicchi A, Pompella A. Gamma-glutamyltransferase of cancer cells at the crossroads of tumor progression, drug resistance and drug targeting. Anticancer Res. 2010;30:1169–82.
Onat A, Can G, Örnek E, Çiçek G, Ayhan E, Doğan Y. Serum-glutamyltransferase:independent predictor of risk of diabetes, hypertension, metabolic syndrome, and coronary disease. Obesity (Silver Spring). 2012;20(4):842–8.
Marubayashi S, Dohi K, Yamada K, Kawasaki T. Changes in the levels of endogenous coenzyme Q homologs, −tocopherol, and glutathione in rat liver after hepatic ischemia and reperfusion, and the effect of pretreatment with coenzyme Q10. Biochim Biophys Acta General Subjects. 1984;797(1):1–9.
Anderson MF, Sims NR. The effects of focal ischemia and reperfusion on the glutathione content of mitochondria from rat brain subregions. J Neurochem. 2002;81:541–9.
Toshikuni N, Asaji T, Nakanishi Y, Nagasawa S-Y, Uenishi H, Tsutsumi M. Elevated serum gamma-glutamyl transpeptidase levels and fatty liver strongly predict the presence of carotid plaque. J Atheroscler Thromb. 2015. [ePub ahead of print].
Paolicchi A, Dominici S, Pieri L, Maellaro E, Pompella A. Glutathione catabolism as a signaling mechanism. Biochem Pharmacol. 2002;64:1027–35.
Stark AA, Pagano DA, Arad A, Siskindovitch S, Zeiger E. Effect of pH on mutagenesis by thiols in Salmonella typhimurium TA102. Mutat Res. 1989;224:89–94.
Spear N, Aust SD. Thiol-mediated NTA-Fe(III) reduction and lipid peroxidation. Arch Biochem Biophys. 1994;312(1):198–202.
Joseph CA, Maroney MJ. Cysteine dioxygenase: structure and mechanism. Chem Commun (Camb.). 2007;3338–3349.
Arnesen E, Refsum H, Bonaa KH, Ueland PM, Forde OH, Nordrehaug JE. Serum total homocysteine and coronary heart disease. Int J Epidemiol. 1995;24(4):704–9.
Wald DS, Law M, Morris JK. Homocysteine and cardiovascular disease: evidence on causality from a meta-analysis. BMJ. 2002;325:1202–6.
McCully KS. Homocysteine, folate, vitamin b6, and cardiovascular disease. JAMA. 1998;279(5):392–3.
De Bree A, Verschuren WM, Kromhout D, Kluijtmans LA, Blom HJ. Homocysteine determinants and the evidence to what extent homocysteine determines the risk of coronary heart disease. Pharmacol Rev. 2002;54:599–618.
Steed MM, Tyagi N, Sen U, Schuschke DA, Joshua IG, Tyagi SC. Functional consequences of the collagen/elastin switch in vascular remodeling in hyperhomocysteinemic wild-type, eNOS−/−, and iNOS−/− mice. Am J Physiol Lung Cell Mol Physiol. 2010;299(3):L301–11.
Bucci M, Papapetropoulos A, Vellecco V, Zhou Z, Zaid A, Giannogonas P, et al. cGMP-dependent protein kinase contributes to hydrogen sulfide-stimulated vasorelaxation. PLoS One. 2012;7(12):e53319.
Qiao W, Chaoshu T, Hongfang J, Junbao D. Endogenous hydrogen sulfide is involved in the pathogenesis of atherosclerosis. Biochem Biophys Res Commun. 2010;396:18–26.
Xu S, Liu Z, Liu P. Targeting hydrogen sulfide as a promising therapeutic strategy for atherosclerosis. Int J Cardiol. 2014;172:313–7.
Lefer DJ. A new gaseous signaling molecule emerges: cardioprotective role of hydrogen sulfide. Proc Natl Acad Sci U S A. 2007;104:179078.
Liu Y-H, Lu M, Hu L-F, Wong PT, Webb GD, Bian J-S. Hydrogen sulfide in the mammalian cardiovascular system. Antioxid Redox Signal. 2012;17(1):141–85.
Zhao W, Zhang J, Lu Y, Wang R. The vasorelaxant effect of H2S as a novel endogenous gaseous KATP channel opener. EMBO J. 2001;20:6008–16.
Fu M, Zhang W, Wu L, Yang G, Lia H, Wang R. Hydrogen sulfide (H2S) metabolism in mitochondria and its regulatory role in energy production. Proc Natl Acad Sci U S A. 2012;109(8):2943–8.
Olson KR, Deleon ER, Gao Y, Hurley K, Sadauskas V, Batz C, et al. Thiosulfate: a readily accessible source of hydrogen sulfide in oxygen sensing. Am J Physiol Regul Integr Comp Physiol. 2013;305:R592–603.
Levey AS, Beto JA, Coronado BE, Eknoyan G, Foley RN, Kasiske BL, et al. Controlling the epidemic of cardiovascular disease in chronic renal disease: what do we know? What do we need to learn? Where do we go from here? National Kidney Foundation Task Force on Cardiovascular Disease. Am J Kidney Dis. 1998;32:853–906.
Libby P. Inflammation and cardiovascular disease mechanisms. Am J Clin Nutr. 2006;83(2):456S–60.
Ray WA, Stein CM, Daugherty JR, Hall K, Arbogast PG, Griffin MR. COX-2 selective non-steroidal anti-inflammatory drugs and risk of serious coronary heart disease. Lancet. 2002;369(9339):1071–3.
Lonn E, Yusuf S, Arnold MJ, Sheridan P, Pogue J, Micks M, et al. Homocysteine lowering with folic acid and B vitamins in vascular disease. N Engl J Med. 2006;354:1567–77.
Bnaa KH, Njlstad I, Ueland PM, Schirmer H, Tverdal A, Steigen T, et al. Homocysteine lowering and cardiovascular events after acute myocardial infarction. N Engl J Med. 2006;354:1578–88.
Ebbing M, Bleie O, Ueland PM, Nordrehaug JE, Nilsen DW, Vollset SE, et al. Mortality and cardiovascular events in patients treated with homocysteine-lowering B vitamins after coronary angiography: a randomized controlled trial. JAMA. 2008;300:795–804.
Peerschke EI, Yin W, Ghebrehiwet B. Platelet mediated complement activation. Adv Exp Med Biol. 2008;632:81–91.
Acknowledgements
This research is supported in part by Quanta Computers, Taiwan, under the auspices of the Qmulus program. Gerald Koenig alerted us to the role of GGT in cardiovascular disease.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
All authors (SS, RMD, AL, AS, GW) were involved in the research to develop the theories expressed in this paper. The composing of the initial draft was done mainly by SS, RMD and AL. GW drew the original figures (not reproduced from previous work), figures 3 and 4. All authors were involved in refinements of the text. All authors read and approved the final manuscript.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Seneff, S., Davidson, R.M., Lauritzen, A. et al. A novel hypothesis for atherosclerosis as a cholesterol sulfate deficiency syndrome. Theor Biol Med Model 12, 9 (2015). https://doi.org/10.1186/s12976-015-0006-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12976-015-0006-1