Abstract
Background and purpose
To explore the association of systemic inflammatory index (SIRI), systemic immune-inflammatory index (SII) and inflammatory prognosis index (IPI) with 90d outcomes in patients with acute ischemic stroke (AIS) after intravenous thrombolysis.
Methods
The patients who underwent intravenous thrombolysis were enrolled in the present study from September 2019 to December 2022. According to the relevant blood indexes obtained in 24 h after admission, the corresponding values of SIRI, SII and IPI were calculated. The correlation among SIRI, SII, IPI, and admission NIHSS scores was examined by Spearman correlation analysis. ROC curve analysis was conducted to determine the optimal cut-off value of SIRI, SII, IPI, and their corresponding sensitivity and specificity to evaluate their predictive value on admission for poor prognosis. To investigate whether high SIRI, SII, and IPI were independent predictors of poor outcomes within 90 days, variables with P-value < 0.05 during univariate analysis were included in multivariate analysis.
Results
Compared with the good outcome group, the poor outcome group had higher SIRI, IPI, and SII. Spearman correlation analysis showed that the SIRI, IPI, and SII levels significantly correlated with the admission NIHSS score (r = 0.338, 0.356, 0.427, respectively; Ps < 0.001). Univariate analysis and Multivariate logistic regression analysis revealed high SIRI, SII, and IPI values as independent risk factors for poor 90-day prognosis (OR = 1.09, 1.003 and 7.109, respectively).
Conclusions
High SIRI, IPI, and SII values are correlated with poor 90d outcomes in AIS patients undergoing intravenous thrombolysis.
Similar content being viewed by others
Introduction
Approximately 70% of all strokes are cases of acute ischemic stroke (AIS), which results from blockage or a clot that impedes blood vessels carrying blood and oxygen to the brain [1]. This condition is known for its high mortality and disability rates, causing a significant burden on families and society [2]. Intravenous thrombolytic therapy has become the mainstay of treatment for AIS within a 4.5-h time window. Our previous studies found that NLR was associated with the prognosis, recurrence, and death of acute ischemic stroke at 90 days [3]. Herein, we further analyzed the correlation of NLR-based composite inflammatory indicators with the prognosis of AIS patients that underwent intravenous thrombolysis.
In recent years, three novel inflammatory markers have been introduced. We explored the association of systemic inflammatory index (SIRI), systemic immune-inflammatory index (SII), and inflammatory prognosis index (IPI) with 90d outcomes in AIS patients undergoing intravenous thrombolysis by analyzing the correlation with NLR-based composite inflammatory indicators.
SIRI, IPI, and SII represent novel predictive indices derived from the neutrophil-to-lymphocyte ratio (NLR), combining various inflammatory parameters. These composite ratios offer a practical and reproducible approach to predicting prognosis. Moreover, they can be integrated with other biomarkers to develop more robust prediction models, facilitating more precise and timely decision-making in clinical practice. Although some studies have shown that SIRI, IPI and SII can be used as a potential and valuable tool to predict the short-term prognosis of stroke patients, there are few clinical reports, and the study population may have limitations caused by ethnic differences [4]. Therefore, we made a detailed analysis of the relevant cases in local area, in order to explore the relationship between SIRI, IPI, SII and short-term prognosis of patients with hyperacute venous thrombolysis in acute cerebral infarction, in order to provide a predictive tool for precision treatment [5].
Materials and methods
Study design and participants
We used data from the stroke center of Jiangsu Province Hospital of Chinese Medicine from September 2019 to December 2022. An observational cohort study of 232 patients with acute ischemic stroke who underwent intravenous thrombolysis with alteplase (rt-PA) was enrolled. The study included 190 patients with acute ischemic stroke who met the following inclusion criteria: (1) aged over 18 years old; (2) diagnosed with AIS according to the Chinese AIS diagnosis and treatment guidelines; (3) received rt-PA intravenous thrombolysis within 4.5 h of symptom onset [6]; (4) premorbid mRS ≤ 2. Exclusion criteria consisted of (1) bridging therapy patients; (2) patients with malignant tumors, autoimmune diseases, or blood system diseases; (3) acute or chronic infections; (4) severe hepatic or renal insufficiency; (5) patients with missing follow-up data.
The Institutional Research Review Board of the Affiliated Hospital of the Nanjing University of Chinese Medicine approved this study which was conducted in accordance with the Declaration of Helsinki (2017NL-012-01).
Definition of inflammatory indicators
The systemic inflammatory index (SIRI) which uses peripheral blood monocytes and the neutrophil-to-lymphocyte ratio (NLR); the systemic immune-inflammatory index (SII), which incorporates platelets and the neutrophil-to-lymphocyte ratio (NLR), and the inflammatory prognosis index (IPI), which takes into account C-reactive protein (CRP), neutrophil-to-lymphocyte ratio (NLR), and serum albumin protein (ALB) as a prognostic index.
Data acquisition
Upon admission, all participants underwent a standard assessment of their demographic characteristics, including sex, age, National Institutes of Health Stroke Scale (NIHSS) score, Modified Rankin Scale (mRS) scale, vascular risk factors (hypertension, diabetes, atrial fibrillation, coronary heart disease, prior stroke, smoking, and alcohol history), and preonset medication (antiplatelet drugs, statins, and anticoagulants).
Within 24 h of admission, all AIS patients underwent assessment using the NIHSS, which ranged from 0 to 42. Patients were classified as mild (NIHSS ≤ 5) and moderate-to-severe (NIHSS > 5) stroke [7]. The modified Rankin score (mRS) was used to assess the 90-day outcomes during follow-up, with a score of 0–2 indicating a favorable prognosis and a score of 3–6 indicating a poor prognosis [8].
Measurement of composite inflammatory ratios based on blood tests
Samples of venous blood were taken within 24 h of admission. If blood tests were conducted more than once during the 24-h period, we used the results of the first test. We recorded the data of neutrophils (N), lymphocytes (L), platelets (PLT), monocytes (M), albumin (ALB), and high-sensitivity C-reactive protein (Hs-CRP). These counts were used to determine the inflammatory biomarkers listed below: neutrophil-to-lymphocyte ratio (NLR = N/L), systemic immune-inflammation index (SII = P × [N/L]), system inflammation response index (SIRI = N × [M/L]) and inflammatory prognosis index (IPI = CRP × NLR/ALB).
Statistical analysis
The Mann–Whitney or T-tests were used to compare continuous factors based on the data distribution, whereas Chi-square tests were used to compare categorical data. The Spearman correlation test examined the association between each indicator and the NIHSS score. Each indicator's ability to discriminate for a 90-day prognosis was tested using the receiver operating characteristic (ROC) curve, and the optimal cut-off value was identified based on the greatest sum of sensitivity and specificity. Risk variables with a P-value of less than 0.05 during univariate analysis were incorporated into the multivariate analysis. The results were presented as odds ratios (ORs) and 95% confidence intervals (CIs). Kaplan–Meier survival curves were plotted based on the optimal cut-off value, and log-rank tests were conducted for each indicator. All statistical analyses were performed using the Statistical Package for the Social Sciences 25.0 (SPSS; IBM, USA), and a two-sided P < 0.05 was statistically significant.
Results
232 AIS patients that underwent intravenous thrombolysis were screened in this study. A total of 42 patients were excluded, due to severe liver and kidney dysfunction, and metastasized tumors (n = 18), bridging treatments after intravenous thrombolysis (n = 10), and incomplete follow-up data (n = 14). Ultimately, a total of 190 subjects were included for the final analysis. A flowchart showing the patient selection is shown in Fig. 1.
Flowchart of patient selection. CHD: coronary heart disease; AF: atrial fibrillation; NIHSS: National Institutes of Health Stroke Scale; MPV: mean platelet volume; NLR: neutrophil-to-lymphocyte ratio; CRP: C-reactive protein; IPI: inflammatory prognosis index; SII: systemic immune-inflammation index; SIRI: system inflammation response index; RBG: random blood glucose
Patient characteristics
Baseline characteristics of the study participants are provided in Table 1. Compared to the good prognosis group, the poor prognosis group had higher age, baseline NIHSS scores, neutrophil counts, premorbid mRS scores, and Random Blood Glucose (RBG), NLR, SIRI, IPI, and SII values but lower lymphocyte counts.
Correlation between IPI, SII, and SIRI level and admission NIHSS score in different groups of AIS patients
Spearman correlation analysis revealed a significant correlation between IPI, SII, and SIRI values with NIHSS score (r = 0.338, 0.356, and 0.427, respectively, P < 0.05). IPI, SII, and SIRI levels in moderate-to-severe AIS patients (NIHSS score ≥ 5) remained higher than in mild AIS patients (NIHSS score < 5) (median: 0.101 vs. 0.034, 675.669 vs. 377.752, 1.685 vs. 1.010), according to the Mann–Whitney U-test (Fig. 2A–C).
The differences between IPI, SII, and SIRI level and admission NIHSS Score. A Differences in IPI levels between two groups of AIS patients. B Differences in SII levels between two groups of AIS patients. C Differences in SIRI levels between two groups of AIS patients. IPI: inflammatory prognosis index; SII: systemic immune-inflammation index; SIRI: system inflammation response index; NIHSS: National Institutes of Health Stroke Scale
Levels of composite inflammatory indicators with different prognosis
Figure 3 shows the violin plots of SIRI, IPI, and SII between the two groups. Patients in the good prognosis group had lower SIRI, IPI, and SII levels than in the poor prognosis group (P < 0.05).
The violin plot of composite inflammatory ratios. The violin plot of the distribution of SIRI, IPI, and SII among different prognosis groups (P < 0.05). IPI: inflammatory prognosis index; SII: systemic immune-inflammation index; SIRI: system inflammation response index; NIHSS: National Institutes of Health Stroke Scale
Prognostic value of SIRI, IPI, and SII in AIS patients
ROC analysis revealed that a SIRI cut-off value of 1.298 × 109 /L demonstrated a sensitivity of 0.758 and a specificity of 0.618 for poor 3-month outcome, with an AUC of 0.720 (95% CI 0.612–0.751, P < 0.05) (Fig. 4). The SII index's predictive accuracy was poor. A 3-month poor outcome was differentiated by the SII cut-off value of 392.903 × 109 /L, which had a sensitivity of 0.879, a specificity of 0.465, and an AUC of 0.715 (95% CI 0.546–0.826; P < 0.05). An IPI cut-off value of 0.223 yielded a sensitivity of 0.424 and specificity of 0.873 for a poor 3-month outcome, with an AUC of 0.701 (95% CI 0.604–0.826, P < 0.05).
The ROC value of SIRI, IPI, and SII in predicting poor short-term outcomes in AIS patients. The AUC of IPI was 0.701 with a sensitivity of 0.424 and a specificity of 0.873; the AUC of SII was 0.715 with a sensitivity of 0.879 and a specificity of 0.465; the AUC of SIRI was 0.720 with a sensitivity of 0.758 and a specificity of 0.618. IPI: inflammatory prognosis index; SII: systemic immune-inflammation index; SIRI: system inflammation response index
Univariate and multivariate logistic analysis of SIRI, SII, IPI, and poor 3-month outcome in AIS patients
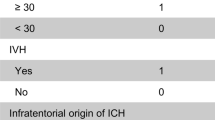
During univariate regression analysis, the admission NIHSS scores, premorbid mRS, NLR, SIRI, SII, and IPI were significantly associated with poor outcomes at 3 months (P < 0.05). To ascertain whether elevated SIRI, SII, and IPI were independent prognostic markers of poor outcomes within 3 months, variables with P < 0.05 during the binary analysis were included in multivariate analysis.
The presence of comorbidities were considered as potential risk factors for AIS. These factors were included as confounding variables, despite not showing a statistically significant difference between age, smoking, alcohol history and prognosis. However, based on multivariate logistic regression analysis, it was found that high SIRI, SII, and IPI values were independently associated with poor prognosis at 3 months (OR = 1.091, 1.003, 7.109; P < 0.05) (Table 2).
Kaplan–Meier survival curve of each indicator
This study also investigated whether each indicator was associated with 90-day recurrence or mortality. The information on recurrence or mortality is given in Table 3. As shown in Fig. 5, SIRI > 1.298 × 109, SII > 392.903 × 109, and IPI > 0.223 were associated with the risk of 90-day recurrence or mortality.
Kaplan–Meier survival curve for 90-day outcome in patients with AIS. A Kaplan–Meier survival curve for 90-day mortality in AIS patients according to SIRI; B Kaplan–Meier survival curve for 90-day mortality in AIS patients according to SII; C Kaplan–Meier survival curve for 90-day mortality in AIS patients according to IPI. Kaplan–Meier survival curve showed that SIRI > 1.298, SII > 392.903, and IPI > 0.223 were associated with a low risk of 90-day recurrence or mortality (P < 0.05). IPI: inflammatory prognosis index; SII: systemic immune-inflammation index; SIRI: system inflammation response index
Discussion
SIRI, IPI, and SII are linked to the advancement of cardiovascular and neoplastic illnesses, according to several clinical studies [9,10,11]. The platelet–neutrophil interaction contributes to clinical ischemia illness and micro thrombosis in stroke, according to several human clinical trials and animal studies [12,13,14]. Neutrophils have been linked to stroke severity, infarct size, and prognosis in studies [17]. Although the neutrophil-to-lymphocyte ratio has been associated with the prognosis of AIS, research on composite inflammatory markers such SIRI, IPI, and SII is lacking. The link between SIRI, IPI and SII and the short-term prognosis of intravenous thrombolysis in AIS patients was further investigated in our study. We discovered that SIRI, IPI, and SII performed well in predicting AIS patients' 90-day prognosis. A higher risk of death or recurrence was linked to higher SIRI, IPI, and SII levels. Additionally, SIRI, IPI, and SII were independently linked with short-term prognosis in AIS patients, according to results from univariate and multivariate binary logistic regression.
There have been many studies on the inflammatory reaction in the acute stage of cerebral infarction. In eMCA rats, the circulating neutrophil count increased after tPA administration significantly more than in the control group, according to Shi et al. [32]; at an early stage, there is a noticeable buildup of neutrophils and T cells in the microvascular lumen of the ipsilateral cerebral hemisphere. At the same time, it was discovered that in patients, the population of neutrophils and T cells in peripheral blood rose quickly after tPA infusion [33], indicating that tPA may have worsened the patient's internal environment's imbalance of homeostasis before it led to further issues. The study [34] also discovered that lymphocyte–endothelial cell interactions encourage microvascular dysfunction and inflammatory factor production, which result in neuronal cell death and disruption of the blood–brain barrier, and that blocking lymphocyte and neutrophil transport can lessen intracerebral hemorrhage brought on by tPA. Therefore, it is reasonable to think that intravenous thrombolysis is involved in the progression of inflammation while undergoing therapeutic treatment.
It is not clear how intravenous thrombolysis leads to the increase of SIRI, IPI and SII and short-term poor prognosis in patients with acute cerebral infarction. Here are some potential mechanisms: stroke occurrence can result in significant damage of synaptic glial cells, astrocytes, and neurons. The blood–brain barrier is damaged and brain edema is exacerbated during AIS, where neutrophils are first produced in the infarction core and penumbra [15]. These neutrophils release inflammatory factors that cause damage to the endothelial cell membrane and basement membrane [16]. Microglia are activated and circulating leukocytes penetrate periinfarct or infarct foci in the acute phase of ischemic stroke, according to preclinical and clinical proof-of-concept studies. After a stroke, resident and invading cells collaborate to control the inflammatory response [35]. It has been proved that a significant number of inflammatory chemicals are released during an acute ischemic stroke [36].
For SIRI, which was employed to investigate the part that monocytes play in AIS using NLR. Monocytes have early migration and infiltration in AIS. They differentiate into macrophages under the influence of OX-LDL, ingest low-density lipoprotein to produce foam cells, and subsequently release a variety of inflammatory substances [18]. By secreting VEGF, activated monocytes also make blood vessels more permeable and break down the blood–brain barrier [19]. Our findings confirmed that the SIRI index performs better in representing the status of systemic inflammatory response and is an independent predictor of prognosis than peripheral blood cell ratios like NLR, LMR, and PLR. Poor 90-day prognosis in AIS patients was independently predicted by a high SIRI index. We found that for AIS patients with SIRI > 1.298 × 109, the incidence of poor prognosis, including the risk of recurrence or death, was increased at 90 days.
According to the available data, IPI is correlated with CRP, NLR, and ALB (IPI = CRP × NLR/ALB). The primary protein in human blood, albumin, regulates colloid osmotic pressure and body nutrition [21]. Numerous physiological processes carried out by albumin include thrombus formation, platelet aggregation inhibition, anti-oxidation, and anti-inflammation [22]. Albumin has been demonstrated to have neuroprotective benefits in investigations on AIS animal models, and clinical research have confirmed that low albumin levels might negatively impact AIS prognosis [23, 24]. The degree of inflammation in the body during the beginning of an infection is clinically reflected by the CRP index. The severity, infarct size, and prognosis of AIS patients have all been linked to CRP levels [25]. The vascular endothelium, among other cells, may interact with CRP to induce vascular inflammation, unstable or even rupture atherosclerotic plaque, and subsequently generate thrombi [26, 27]. A growing body of evidence points to a link between elevated CRP levels and the risk of cardiovascular and cerebrovascular events, as well as death from any cause [28,29,30]. A meta-analysis consistently demonstrated an association between CRP levels and the probability of death in AIS [31].
For SII, it has been determined that the condition replicates three critical pathophysiological processes in AIS: thrombosis, inflammation, and immune response. A high SII is indicative of thrombogenic and immunological dysregulation states, both of which have been linked to serious adverse outcomes [20]. Our findings demonstrate that the best SII threshold (392.903 × 109) performs well in predicting the prognosis of AIS patients at 90 days. Its accuracy is, however, less than that of the SIRI and IPI index.
There are several limitations in this study that should be acknowledged. It is crucial to remember that this was a retrospective analysis based on stroke registration data rather than a multi-center clinical trial. Future research should think about doing multi-center prospective studies as it presents a possible bias and reduces the generalizability of the findings. The analysis did not include any patients who had mechanical thrombectomy, which may have limited the data' application to this particular subgroup. Finally, it needs to be understood that composite inflammatory indices might change a lot while a patient is in the hospital. Instead of relying exclusively on measurements taken prior to thrombolysis or at admission, future research should concentrate on dynamically monitoring these indices throughout the whole treatment process.
Our findings corroborate that higher SIRI, SII, and IPI values indicate greater disease severity at admission and an increased incidence of poor outcomes at 90-day prognosis. As a result, these indices offer a new approach to conducting stratified interventions in AIS patients, potentially leading to improved prognosis in clinical practice.
Conclusion
To be honest, we are the first NLR-based comprehensive analysis of SIRI, SII, and IPI and the short-term prognosis of intravenous thrombolysis therapy for acute cerebral infarction, and the inflammatory indicators after stroke are significantly related to the short-term prognosis. SIRI, SII and IPI, which are easily accessible blood indicators without subjective bias, will provide theoretical support for early intervention in patients with acute cerebral infarction.
Availability of data and materials
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Abbreviations
- AIS:
-
Acute ischemic stroke
- NLR:
-
Neutrophil-to-lymphocyte ratio
- PLR:
-
Platelet-to-lymphocyte ratio
- LMR:
-
Lymphocyte-to-monocyte ratio
- HT:
-
Hemorrhagic transformation
- OTT:
-
Onset to treatment time
- PAO:
-
Proximal arterial occlusion
- TOAST:
-
Trial of Org 10172 in Acute Stroke Treatment
- TC:
-
Total cholesterol
- TG:
-
Triglyceride
- HDL:
-
High-density lipoprotein
- LDL:
-
Low-density lipoprotein
- FBG:
-
Fasting blood glucose
- Hs-CRP:
-
Hypersensitive C-reactive protein
- OR:
-
Odds ratio
- 95% CI:
-
95% Confidence interval
- AUC:
-
Area under the curve
References
Phipps MS, Cronin CA. Management of acute ischemic stroke. BMJ. 2020;368: l6983.
Ma Q, Li R, Wang L, Yin P, Wang Y, Yan C, Ren Y, Qian Z, Vaughn MG, McMillin SE, et al. Temporal trend and attributable risk factors of stroke burden in China, 1990–2019: an analysis for the Global Burden of Disease Study 2019. Lancet Public Health. 2021;6:e897–906.
Cao X, Zhu Q, Xia X, Yao B, Liang S, Chen Z, Wu M. The correlation between novel peripheral blood cell ratios and 90-day mortality in patients with acute ischemic stroke. PLoS ONE. 2020;15: e0238312.
Gong P, Liu Y, Gong Y, Chen G, Zhang X, Wang S, Zhou F, Duan R, Chen W, Huang T, et al. The association of neutrophil to lymphocyte ratio, platelet to lymphocyte ratio, and lymphocyte to monocyte ratio with post-thrombolysis early neurological outcomes in patients with acute ischemic stroke. J Neuroinflamm. 2021;18:51.
Huang YW, Yin XS, Li ZP. Association of the systemic immune-inflammation index (SII) and clinical outcomes in patients with stroke: a systematic review and meta-analysis. Front Immunol. 2022;13:1090305.
Mendelson SJ, Prabhakaran S. Diagnosis and management of transient ischemic attack and acute ischemic stroke: a review. JAMA. 2021;325:1088–98.
Tsivgoulis G, Katsanos AH, Sandset EC, Turc G, Nguyen TN, Bivard A, Fischer U, Khatri P. Thrombolysis for acute ischaemic stroke: current status and future perspectives. Lancet Neurol. 2023;22:418–29.
Shi K, Tian DC, Li ZG, Ducruet AF, Lawton MT, Shi FD. Global brain inflammation in stroke. Lancet Neurol. 2019;18:1058–66.
Dziedzic EA, Gąsior JS, Tuzimek A, Paleczny J, Junka A, Dąbrowski M, Jankowski P. Investigation of the associations of novel inflammatory biomarkers-Systemic Inflammatory Index (SII) and Systemic Inflammatory Response Index (SIRI)-with the severity of coronary artery disease and acute coronary syndrome occurrence. Int J Mol Sci. 2022;23:9553.
Hirahara N, Tajima Y, Matsubara T, Fujii Y, Kaji S, Kawabata Y, Hyakudomi R, Yamamoto T, Uchida Y, Taniura T. Systemic immune-inflammation index predicts overall survival in patients with gastric cancer: a propensity score-matched analysis. J Gastrointest Surg. 2021;25:1124–33.
Zhou Z, Sehn LH, Rademaker AW, Gordon LI, Lacasce AS, Crosby-Thompson A, Vanderplas A, Zelenetz AD, Abel GA, Rodriguez MA, et al. An enhanced International Prognostic Index (NCCN-IPI) for patients with diffuse large B-cell lymphoma treated in the rituximab era. Blood. 2014;123:837–42.
Denorme F, Portier I, Rustad JL, Cody MJ, de Araujo CV, Hoki C, Alexander MD, Grandhi R, Dyer MR, Neal MD, et al. Neutrophil extracellular traps regulate ischemic stroke brain injury. J Clin Invest. 2022;132: e154225.
De Meyer SF, Denorme F, Langhauser F, Geuss E, Fluri F, Kleinschnitz C. Thromboinflammation in stroke brain damage. Stroke. 2016;47:1165–72.
Carmona-Mora P, Knepp B, Jickling GC, Zhan X, Hakoupian M, Hull H, Alomar N, Amini H, Sharp FR, Stamova B, Ander BP. Monocyte, neutrophil, and whole blood transcriptome dynamics following ischemic stroke. BMC Med. 2023;21:65.
Iadecola C, Anrather J. The immunology of stroke: from mechanisms to translation. Nat Med. 2011;17:796–808.
Santos-Lima B, Pietronigro EC, Terrabuio E, Zenaro E, Constantin G. The role of neutrophils in the dysfunction of central nervous system barriers. Front Aging Neurosci. 2022;14: 965169.
Dmytriw AA, Dibas M, Phan K, Efendizade A, Ospel J, Schirmer C, Settecase F, Heran MKS, Kühn AL, Puri AS, et al. Acute ischaemic stroke associated with SARS-CoV-2 infection in North America. J Neurol Neurosurg Psychiatry. 2022;93:360–8.
Anselmo AC, Gilbert JB, Kumar S, Gupta V, Cohen RE, Rubner MF, Mitragotri S. Monocyte-mediated delivery of polymeric backpacks to inflamed tissues: a generalized strategy to deliver drugs to treat inflammation. J Control Release. 2015;199:29–36.
Xie L, Zhang S, Huang L, Peng Z, Lu H, He Q, Chen R, Hu L, Wang B, Sun B, et al. Single-cell RNA sequencing of peripheral blood reveals that monocytes with high cathepsin S expression aggravate cerebral ischemia-reperfusion injury. Brain Behav Immun. 2023;107:330–44.
Colicchia M, Perrella G, Gant P, Rayes J. Novel mechanisms of thrombo-inflammation during infection: spotlight on neutrophil extracellular trap-mediated platelet activation. Res Pract Thromb Haemost. 2023;7: 100116.
Ma X, Yang J, Wang X, Wang X, Chai S. The clinical value of systemic inflammatory response index and inflammatory prognosis index in predicting 3-month outcome in acute ischemic stroke patients with intravenous thrombolysis. Int J Gen Med. 2022;15:7907–18.
Acharya P, Jakobleff WA, Forest SJ, Chinnadurai T, Mellas N, Patel SR, Kizer JR, Billett HH, Goldstein DJ, Jorde UP, Saeed O. Fibrinogen albumin ratio and ischemic stroke during venoarterial extracorporeal membrane oxygenation. Asaio J. 2020;66:277–82.
Pascoe MC, Skoog I, Blomstrand C, Linden T. Albumin and depression in elderly stroke survivors: an observational cohort study. Psychiatry Res. 2015;230:658–63.
Wang A, Zhang Y, Xia G, Tian X, Zuo Y, Chen P, Wang Y, Meng X, Han X. Association of serum albumin to globulin ratio with outcomes in acute ischemic stroke. CNS Neurosci Ther. 2023;29:1357–67.
Kitagawa K, Hosomi N, Nagai Y, Kagimura T, Ohtsuki T, Maruyama H, Origasa H, Minematsu K, Uchiyama S, Nakamura M, Matsumoto M. Cumulative effects of LDL cholesterol and CRP levels on recurrent stroke and TIA. J Atheroscler Thromb. 2019;26:432–41.
Cai Z, He W, Zhuang FJ, Chen Y. The role of high high-sensitivity C-reactive protein levels at admission on poor prognosis after acute ischemic stroke. Int J Neurosci. 2019;129:423–9.
Wei P, Han B, Zhang WJ, Bai J, Jiang CY, Qiu CR, Zhang Q, Fu Q, Yang XJ. Effect of ticagrelor on the serum level of hs-CRP, ESM-1 and short-term prognosis of patients with acute STEMI. Exp Ther Med. 2017;13:604–8.
Suthahar N, Wang D, Aboumsallem JP, Shi C, de Wit S, Liu EE, Lau ES, Bakker SJL, Gansevoort RT, van der Vegt B, et al. Association of initial and longitudinal changes in C-reactive protein with the risk of cardiovascular disease, cancer, and mortality. Mayo Clin Proc. 2023;98:549–58.
Zacho J, Tybjaerg-Hansen A, Nordestgaard BG. C-reactive protein and all-cause mortality–the Copenhagen City Heart Study. Eur Heart J. 2010;31:1624–32.
McCabe JJ, Walsh C, Gorey S, Harris K, Hervella P, Iglesias-Rey R, Jern C, Li L, Miyamoto N, Montaner J, et al. C-reactive protein, interleukin-6, and vascular recurrence after stroke: an individual participant data meta-analysis. Stroke. 2023;54:1289.
Kaptoge S, Di Angelantonio E, Lowe G, Pepys MB, Thompson SG, Collins R, Danesh J. C-reactive protein concentration and risk of coronary heart disease, stroke, and mortality: an individual participant meta-analysis. Lancet. 2010;375:132–40.
Shi K, Zou M, Jia DM, Shi S, Yang X, Liu Q, Dong JF, Sheth KN, Wang X, Shi FD. tPA mobilizes immune cells that exacerbate hemorrhagic transformation in stroke. Circ Res. 2021;128:62–75.
Ying A, Cheng Y, Lin Y, Yu J, Wu X, Lin Y. Dynamic increase in neutrophil levels predicts parenchymal hemorrhage and function outcome of ischemic stroke with r-tPA thrombolysis. Neurol Sci. 2020;41:2215–23.
Wang R, Zhu Y, Liu Z, Chang L, Bai X, Kang L, Cao Y, Yang X, Yu H, Shi MJ, et al. Neutrophil extracellular traps promote tPA-induced brain hemorrhage via cGAS in mice with stroke. Blood. 2021;138:91–103.
DeLong JH, Ohashi SN, O’Connor KC, Sansing LH. Inflammatory responses after ischemic stroke. Semin Immunopathol. 2022;44:625–48.
Iadecola C, Buckwalter MS, Anrather J. Immune responses to stroke: mechanisms, modulation, and therapeutic potential. J Clin Invest. 2020;130:2777–88.
Acknowledgements
This publication was made possible by support from brain center in Jiangsu Province Hospital of Chinese Medicine.
Funding
This work was supported by National Natural Science Foundation of China (Grant Nos. 82274428, 81973794), National Administration of Traditional Chinese Medicine: Evidence-Based Capacity Building Project (2019XZZX-NB007), 333 high level talents training project in Jiangsu (Grant No. BRA 2016507), Jiangsu Province Administration of Chinese Medicine (ZT202102).
Author information
Authors and Affiliations
Contributions
FM and LL were mainly involved in study design, data analysis, data interpretation, and manuscript preparation. LX, JW and AZ were mainly involved in data acquisition and data analysis. JL, JC, YL, and LL were mainly involved in data acquisition. ZC and WL were mainly involved in data analysis and manuscript preparation. QZ, YZ and MW were mainly involved in study design, data interpretation, and manuscript preparation. The authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Ethics Committee of the Affiliated Hospital of Nanjing University of Chinese Medicine (2017NL-012-01). Informed consent was obtained from participants or their legal representatives.
Consent for publication
All the authors agree to publish.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ma, F., Li, L., Xu, L. et al. The relationship between systemic inflammation index, systemic immune-inflammatory index, and inflammatory prognostic index and 90-day outcomes in acute ischemic stroke patients treated with intravenous thrombolysis. J Neuroinflammation 20, 220 (2023). https://doi.org/10.1186/s12974-023-02890-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12974-023-02890-y








