Abstract
Background
Pediatric uveitis is a severe inflammatory ocular condition that can lead to sight-threatening complications and can negatively impact quality of life. The retinal microcirculation is often affected in intermediate uveitis and panuveitis. Here, we examined the extraocular (i.e., systemic) microcirculation in pediatric uveitis cases and healthy controls using nailfold capillaroscopy (NFC).
Methods
We performed NFC in 119 children with noninfectious uveitis and 25 healthy pediatric controls, and assessed the following parameters: capillary density (number of capillaries/mm), dilated capillaries (apex > 20 µm), avascular area, the presence of microhemorrhages, and capillary morphology. Differences in NFC parameters between cases and controls were calculated using regression analysis after adjusting for age and sex.
Results
The mean (± SD) age of the patient group was 13.7 (± 3) years, with 56% females; 46%, 18%, and 36% of cases presented as anterior uveitis, intermediate uveitis, and panuveitis, respectively, with an overall mean disease duration of 4.7 (± 4.0) years. Compared to the control group, the pediatric uveitis cases had a significantly higher number of dilated capillaries/mm and a higher prevalence of ramified capillaries. Moreover, compared to the control group the intermediate uveitis cases had a significantly higher number of dilated capillaries, whereas the anterior uveitis cases had a lower capillary density and a higher prevalence of ramified capillaries.
Conclusions
Children with uveitis without systemic disease can present with changes in systemic microcirculation. These changes vary amongst the subtypes of uveitis.
Similar content being viewed by others
Background
Uveitis is a complex, potentially sight-threatening ocular condition characterized by inflammation of the uvea and nearby structures involving the vessels in the retina and sclera [1, 2]. Vessels in the anterior uveal tract may be affected as well, visible as anterior chamber flare caused by the breakdown of the blood-aqueous barrier due to the inflammatory process. Pediatric uveitis can develop in conjunction with a systemic condition, of which juvenile idiopathic arthritis (JIA) is the most common and best-studied. In up to 60% of cases, the etiology remains unknown, and these cases are considered an isolated idiopathic inflammatory eye condition [1, 3,4,5,6]. Inflammatory involvement of the ocular vasculature is common in patients with intermediate uveitis or panuveitis and can include retinal vasculitis, diffuse retinal capillary leakage, and/or macular edema [7,8,9,10]. However, whether changes in the extraocular vascular and/or microcirculation are involved in pediatric patients with uveitis is currently unknown.
Nailfold capillaroscopy (NFC) is a noninvasive diagnostic technique used to evaluate the microcirculation in the nailfold. This technique is commonly used in the medical fields of rheumatology and dermatology, revealing various abnormal patterns associated with diseases such as systemic sclerosis and systemic lupus erythematosus (SLE) [11,12,13,14]. Ocular manifestations, including changes in the retinal or choroidal microcirculation, are described in these rheumatic diseases. More recently, NFC has also been used to detect microvascular abnormalities in ocular diseases, particularly glaucoma [15,16,17]. Moreover, Chen et al. used NFC in adults with uveitis and found abnormalities in the systemic microcirculation that were correlated with peripheral retinal leakage [18]. Because NFC is noninvasive, easy to perform, and relatively rapid, it is highly suitable for use in children [14,15,16,17]. To date, however, the use of NFC in children with uveitis has not been described. Therefore, the primary aim of this study was to compare NFC findings between pediatric uveitis cases and healthy pediatric controls, and to compare findings between uveitis subtypes. Our results may provide new insights into the pathogenesis of this potentially sight-threatening pediatric condition, as well as new insights regarding the development and application of new diagnostic and/or prognostic biomarkers.
Methods
Study population
The participants in this cross-sectional study were recruited between June 2020 and June 2022 at the Ophthalmology Department of the University Medical Center Utrecht (UMCU), the Netherlands, a tertiary referral center. The pediatric control group consisted of children with strabismus and no evidence of a concomitant inflammatory condition. We excluded participants with any cardiovascular or other systemic disease not associated with uveitis, including type 2 diabetes mellitus and hypertension. We also excluded participants with infectious uveitis based on serology or ocular fluid analysis. All cases were diagnosed by a pediatric uveitis specialist at the UMCU Department of Ophthalmology according to the SUN criteria [2]. The presence of associated systemic diseases was assessed in accordance with current diagnostic criteria for pediatric uveitis, and all patients were assessed by pediatricians and/or pediatric rheumatologists [19]. The analytical screening performed prior to classifying uveitis as idiopathic is shown in Additional File 1. All participants and/or their legal guardian provided written informed consent before participating in this study. This study adhered to the tenets of the Declaration of Helsinki and was approved by the UMCU Medical Research Ethics Committee (protocol number: 20–317).
Clinical data
Demographic data obtained from all participants included age at NFC assessment and sex; in addition, the following disease-specific information was collected for the patients with uveitis: date of uveitis diagnosis, uveitis anatomic subtype (anterior uveitis, intermediate uveitis, or panuveitis), uveitis disease duration, presence (and type, if applicable) of an associated systemic disease, and laboratory results of antinuclear antibody (ANA) testing. ANA positivity was defined as a titer of ≥ 1:160 detected on the HEp-2 indirect immunofluorescence assay on 2 occasions at least 3 months apart [20]. The following ophthalmological findings were reported: presence of anterior chamber flare of 1 + or higher, presence of cystoid macular edema (CME), papillitis, retinal vasculitis and/or retinal capillary leakage on fluorescein angiography (FA). CME was defined as the presence of macular thickening with cyst formation visible on macular OCT and/or FA [21,22,23]. Papillitis was defined as the presence of optic disc hyperfluorescence and/or leakage on FA, inflammatory optic disc swelling, and/or retinal nerve fiber layer thickness of > 130 µm on OCT while excluding all other noninflammatory causes of optic disc swelling [24]. In order to monitor changes in NFC findings over time, a small prospective cohort consisting of 20 patients in original cohort of noninfectious uveitis cases underwent two additional NFC measurements 6 and 12 months after the first measurement. These 20 patients did not use any systemic medication the first NFC measurement.
Nailfold capillaroscopic technique
A standardized NFC technique from the European Alliance of Associations for Rheumatology (EULAR) study group on Microcirculation in Rheumatic Diseases was used for the examination and classification [12, 14, 25]. Prior to the NFC examination (CapillaryScope 200 Pro, Dino-Lite), each participant was acclimatized for at least 15 min at room temperature (20–24°C). The nailfold of all fingers, except for the thumbs, was examined after applying a drop of immersion oil on the nailfold bed to improve resolution. NFC was performed by a single observer, first at low (50x) magnification in order to determine the distribution of any obvious abnormalities and to obtain an overview of the nailfold area (1–2 images were obtained). Next, four consecutive images were obtained at 200 × magnification for assessing the detailed morphology of the capillaries. The images were analyzed at a later stage by the same observer who obtained the images. Three different second observers also analyzed images for the presence of hemorrhages and to determine the capillary morphology. The intraclass correlation coefficient for the assessment of hemorrhages and abnormal morphology was 0.57–0.88; all cases with a low correlation were discussed together until consensus was reached. During the analysis, the first and second observers were both blinded with respect to the participants’ details. DinoCapture 2.0 software was used to analyze the images [26].
The following NFC parameters were assessed at 200 × magnification:
-
Capillary density, defined as the number of capillary loops per mm in the distal row using the “90º method”, where a capillary loop was considered to be a distal loop if the apex of the capillary made an angle of ≥ 90º with the apex of its adjacent capillaries [27].
-
Density of dilated capillaries, defined as the number of dilated capillaries with an apical limb diameter of 20–50 µm per mm [12, 14].
-
Microhemorrhages visible as hemosiderin deposits within the distal row of the nailfold, caused by the rupture of one or more capillaries [12, 14].
-
Avascular areas, defined as the absence of capillaries in the distal row with a minimum of 200 µm between adjacent capillaries [18].
-
Capillary morphology, scored per capillary per image as normal, multiple crossings, tortuous, bushy, ramified, nonconvex, or bizarre shaped [12, 27]. The definitions of each capillary morphology are shown in Table 1. Capillaries with busy, ramified, nonconvex, and bizarre morphologies were also classified as having an abnormal morphology [12, 14, 25]. The percentage of each morphology type was calculated by dividing the total number of capillaries of that morphology type by the total number of capillaries assessed per image.
To obtain the NFC parameters at the participant level, mean values were calculated, except for the presence of microhemorrhages, in which the presence of a microhemorrhage in at least one image was considered positive for that participant. We also assessed the quality of the images and excluded any participant in which fewer than 25% of the images were deemed eligible for assessment [14]. Figure 1 shows a representative NFC image of a pediatric control.
Statistical analysis
All statistical analyses were performed using the R software package version 4.2.2. The intraclass correlation coefficient between observers was calculated for the assessment of capillary morphology. Descriptive statistics are used to report demographics and to describe the NFC parameters per group. Except where indicated otherwise, summary data are represented as the mean and standard deviation (for continuous variables) or percentage (for categorical variables). To compare NFC parameters between groups, we performed a multivariable regression analysis, adjusted for age and sex. Differences were considered significant at P < 0.05, and all tests were 2-tailed.
Results
Initially, a total of 154 patients and controls were examined with NFC, after which 10 participants (9 patients and 1 control) were excluded based on an insufficient number of assessable images. Thus, a total of 144 participants (119 patients and 25 controls) were included in our analysis. The demographics and clinical features of these groups are summarized in Table 2. Twelve of the 38 patients diagnosed with JIA-associated uveitis received systemic treatment for their uveitis. In the other patients systemic treatment was indicated for both JIA and uveitis.
Comparison between cases and controls
We found significant differences between the patient group and the control group with respect to the number of dilated capillaries per mm, the prevalence of ramified capillaries, and the mean percentage of ramified capillaries (defined as the number of ramified capillaries divided by the total number of capillaries). Analysis of patients without an associated systemic disease (n = 61) showed similar results (data not shown). No other NFC parameters differed significantly between the two groups, even when we combined the four abnormal morphologies (busy, ramified, nonconvex, and bizarre) into one category (Table 3).
Uveitis subtypes
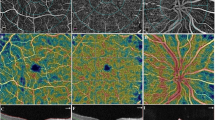
Next, we analyzed the NFC parameters in the pediatric controls and in each of the three specific uveitis subtypes (anterior uveitis, intermediate uveitis, and panuveitis); the results are summarized in Fig. 2. We found that mean capillary density was significantly lower in the patients with anterior uveitis (7.0 ± 0.7) compared to the control group (7.5 ± 0.7, P = 0.008). Moreover, 54% of the patients with anterior uveitis (30/55 cases) had a capillary density < 7/mm, compared to 20% (5/25) of the pediatric controls (P = 0.01). We also found that the patients with intermediate uveitis had a significantly higher number of dilated capillaries per mm compared to the pediatric controls (P < 0.001). Finally, the mean percentage of ramified capillaries was higher in the patients with anterior uveitis and in the patients with panuveitis compared to the pediatric controls.
Nailfold capillaroscopy findings for pediatric controls (PC; n = 25), anterior uveitis cases (AU, n = 55), intermediate uveitis cases (IU, n = 21), panuveitis cases (Pan, n = 43). A. NFC image of a 16-year-old boy diagnosed with panuveitis showing a dilated capillary (left, arrowhead) and boxplot summarizing the median number of dilations per linear mm in each subgroup (right). B. NFC image of the same 16-year-old boy diagnosed with panuveitis showing ramified capillaries (left, arrowheads) and boxplot summarizing the mean percentage of ramified capillaries in each subgroup (right). C. NFC image of a 16-year-old girl diagnosed with anterior uveitis showing low capillary density (< 7 capillaries per linear mm) (left) and boxplot summarizing mean capillary density in each subgroup (right). *P < 0.05 versus the control group, determined using linear regression analysis adjusted for age and sex
We also found differences in certain NFC parameters when we compared the 55 patients with anterior uveitis with the intermediate uveitis and panuveitis patients combined (n = 64). Specifically, the patients with anterior uveitis had a lower mean capillary density (7.0/mm vs. 7.3/mm, respectively, P = 0.008), a higher percentage of abnormally shaped capillaries (6% vs. 4%, respectively, P = 0.02), and a higher percentage of tortuous capillaries (7% vs. 4%, respectively, P = 0.02); all other parameters were similar between these two subgroups.
In addition, we found no difference between the 38 patients with JIA-associated uveitis and the 16 patients with idiopathic chronic anterior uveitis (data not shown). When comparing the presence of anterior chamber flare in patients with anterior uveitis, we found a higher percentage of bushy capillaries in patients without the presence of flare compared to patients with anterior chamber flare (n = 17, 0.9% vs. n = 38, 0.3%; P = 0.04). The other NFC-parameters were not significantly different. Also no difference was found within the different types of JIA.
Additionally, we compared ANA-positive patients (n = 60) to ANA-negative patients (n = 59), and found that ANA-positive patients had a significantly lower capillary density (7.0 vs. 7.3, respectively, P = 0.02) and more microhemorrhages (P = 0.04) compared to ANA-negative patients.
We also assessed the association between NFC parameters and inflammatory vascular involvement of the retina based on FA findings in 47 patients. We found that capillary density was significantly higher in the patients with papillitis (7.4/mm) compared to the patients without papillitis (7.1/mm, P = 0.04); however, this difference was no longer significant after we corrected for uveitis subtype. In contrast, we found no significant association between CME, retinal vasculitis and/or retinal capillary leakage on FA and any of the NFC parameters.
Finally, we compared patients with a capillary density < 7/mm (n = 50) to patients with a capillary density ≥ 7/mm (n = 69). We found that patients with a capillary density < 7/mm had a longer duration of uveitis, and more patients were treated with biological agents for adequate disease control compared to patients with a capillary density ≥ 7/mm when adjusting for age, sex, and duration of uveitis. We did not found an association with disease activity, and use of medication.
Follow-up NFC data
A total of 20 patients in the uveitis group underwent two follow-up NFC measurements 6 and 12 months after the first measurement. We found no significant difference in NFC parameters between the first NFC measurement and either of the two follow-up measurements (data not shown). Interestingly, however, we found that the percentage of microhemorrhages decreased—albeit not significantly—between the initial NFC measurement (55%) and the 6-month and 12-month measurements (33% and 35%, respectively).
Discussion
In this study, we report significant differences in NFC parameters between children with noninfectious uveitis and pediatric controls, suggesting involvement of the systemic microcirculation in pediatric uveitis. Our results also suggest that the systemic microcirculation is affected even in idiopathic cases of uveitis that present without an identified systemic condition. Previous studies have shown that several inflammatory indicators such as the neutrophil/lymphocyte ratio, interleukins, and the platelet/lymphocyte ratio are elevated in the serum of patients with noninfectious uveitis [28,29,30,31,32,33,34,35,36,37,38,39]. These increased indicators are associated with both the activity and the severity of uveitis, likely implying activation of the systemic immune system (i.e., an inflammatory index). Our results support the notion that uveitis is not exclusively an intraocular inflammation but can also indicate systemic involvement. Although the long-term consequences of these changes in the microcirculation are currently unknown, our findings underscore the complexity of this potentially sight-threatening condition in children and provides new insights for developing diagnostic and prognostic biomarkers to monitor the microcirculation.
A previous cross-sectional case–control study in adults with uveitis found differences in NFC assessment, with a higher number of dilated capillaries and lower capillary density in the patient group [18]. Although we found no difference in capillary density between our entire pediatric uveitis group and the control group, we did find a significantly lower capillary density in the patients with anterior uveitis. This difference between studies might be due—at least in part—to differences between adult patients and pediatric patients and/or the slightly higher percentage of anterior uveitis patients in the previous study in adults (54%) [18] compared to our study (46%).
Recently, Melsens et al. reported that healthy children have a similar capillary density as adults and that the same cut-off value used for adults (≥ 7 capillaries per linear mm) can also be used in children [14]. Although not statistically significant, we found that 42% of the children with uveitis in our study had a capillary density < 7/mm compared to 20% of pediatric controls; this difference may be attributed in part to the fact that nearly half of the patients in our study had anterior uveitis, as anterior uveitis is often accompanied by a systemic disease such as JIA. However, the presence of JIA cannot fully explain this finding, as we found no difference between JIA-associated uveitis and idiopathic chronic anterior uveitis (data not shown). In addition, these two subtypes of uveitis are considered to be clinically identical, as they share genetic risk alleles and cannot be distinguished based solely on ophthalmological features [40, 41]. Moreover, recent studies in children with JIA found no changes in NFC parameters between patients with JIA (but for whom the presence of uveitis was unknown) and controls, indicating that arthritis might not be the cause of the changes in the microcirculation [14, 42]. Despite no association was found between lower capillary density and disease activity in this study, we do believe that a lower capillary density might be associated with a worse disease control. To reach an adequate disease control these patients needed the addition of a biological agent in contrary to patients with higher capillary density.
Interestingly, we found that the patients with intermediate uveitis had the highest number of dilated capillaries per mm. Intermediate uveitis is often accompanied by signs of inflammatory involvement of the retina such as intraocular perivasculitis, vasculitis, and periphlebitis. In contrast to other studies in adults [18, 43], we found no apparent correlation between abnormalities in the retinal and nailfold microcirculation.
While vessels in the anterior uveal tract may potentially be affected especially in anterior uveitis, there is currently no practical method available to directly visualize them in clinical practice. However, the measurement of the anterior chamber flare could potentially serve as a clinical representation of this inflammatory process and the consequent breakdown of the blood-aqueous barrier as a result of it. We found no association between anterior chamber flare and NFC-parameters, with the exception of bushy capillaries. However, the found differences were very small, which might question the clinical relevance of this finding. The ciliary body might also be affected in anterior uveitis. However, it is difficult to investigate possible abnormalities regarding the vasculature with the current methods of examination.
Nailfold capillaroscopic changes are extensively described and investigated in several rheumatic diseases such as systemic sclerosis, SLE, and dermatomyositis [11,12,13,14]. Interestingly, in literature, ocular manifestations, including abnormalities in the microcirculation of the retina and choroid, are described in these rheumatic diseases [44,45,46,47,48,49,50]. Several of these studies use optical coherence tomography angiography (OCT-A) as a non-invasive tool to assess the retinal and choroidal microcirculation [44, 45, 47, 49, 50]. Jakhar et al. revealed that patients with systemic sclerosis with retinal disease have more severe NFC changes [51]. Studies investigating a possible association between NFC changes and retinal/choroidal microcirculatory changes are currently lacking. Therefore, future research addressing this topic might provide valuable information regarding the interaction between the microcirculation of the nailfold and the retina/choroid.
One strength of our study is that we included a relatively large cohort of children with uveitis. Furthermore, we assessed the NFC images using a standardized protocol based on the international consensus definitions established by the EULAR Study Group on Microcirculation in Rheumatic Diseases [12, 25]; these definitions were used recently in a standardized assessment of children [14]. In addition, the majority of the images was assessed by two observers who were blinded with respect to the participant’s details.
Despite these strengths, our study also has some limitations that warrant discussion. First, the pediatric control group was not age-matched to the patient group, resulting in a significant difference in age between the two groups; however, we corrected for both age and sex in of our analyses. Second, data whether patients with JIA-associated uveitis were receiving immunosuppressive drugs primarily for arthritis or for uveitis was not always clearly available in this study. Third, our prospective study did not show any apparent change in NFC findings, even after one year; however, this may have been too short of a follow-up period to detect changes, as a previous study involving patients with systemic sclerosis found that the median time to progression of the NFC pattern (i.e., the time after which 50% of patients did progress) was nearly four times as long as our follow-up period [52]. Although not statistically significant, we did observe a decrease in microhemorrhages in our prospective study. Whether this is due to effects of treatment is currently unclear due to the small number of patients. The clinical repercussions of the findings in this study are currently unknown and are yet to be determined in future studies. Longitudinal studies with repeated NFC measurements for a longer follow-up period are therefore needed in order to determine whether NFC findings have prognostic value with respect to predicting the course of disease severity in noninfectious uveitis. Furthermore, it would be interesting to investigate whether NFC findings can be used to predict disease relapse, the need for additional systemic treatment, and/or treatment response in patients with pediatric uveitis. On the other hand, future studies investigating the underlying pathophysiology are also needed in order to identify biomarkers specific to uveitis-associated inflammation and/or neoangeogenesis. Such studies will likely provide valuable information regarding the underlying disease mechanisms and may provide simple prognostic indicators that can be used to guide the precision care of patients with noninfectious uveitis.
Conclusions
Pediatric uveitis can present with changes in the systemic microcirculation, with specific differences based on the subtype of uveitis. Our results suggest that noninfectious pediatric uveitis is not always limited to intraocular inflammation, but may also include systemic inflammation. The changes observed in the systemic microcirculation do not appear to be correlated with retinal vascular inflammation involvement in our clinically heterogenous cohort. Thus, whether capillary changes reflect vascular involvement in specific uveitis subtypes—for example, intermediate uveitis—warrants further investigation. Nevertheless, our findings provide important new insights into this severe, potentially sight-threatening condition in children and provide input for designing both prospective studies and translational studies.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ANA:
-
Antinuclear antibody
- CME:
-
Cystoid macular edema
- EULAR:
-
European Alliance of Associations for Rheumatology
- FA:
-
Fluorescein angiography
- IQR:
-
Interquartile range
- JIA:
-
Juvenile idiopathic arthritis
- NFC:
-
Nailfold capillaroscopy
- OCT:
-
Optical coherence tomography
- SD:
-
Standard deviation
References
Cunningham J. Uveitis in children. Ocul Immunol Inflamm. 2000;8:251–61.
Jabs DA, Nussenblatt RB, Rosenbaum JT, Atmaca LS, Becker MD, Brezin AP, et al. Standardization of uveitis nomenclature for reporting clinical data. Results of the first international workshop. Am J Ophthalmol. 2005;140:509–16.
Angeles-Han ST, Rabinovich CE. Uveitis in children. Curr Opin Rheumatol. 2016;28:544–9.
Tugal-Tutkun I. Pediatric uveitis. J Ophthalmic Vis Res. 2011. p. 259–69.
Smith JA, Mackensen F, Sen HN, Leigh JF, Watkins AS, Pyatetsky D, et al. Epidemiology and Course of disease in childhood uveitis. Ophthalmology. 2009;116:1544-1551.e1. https://doi.org/10.1016/j.ophtha.2009.05.002.
Ferrara M, Eggenschwiler L, Stephenson A, Montieth A, Nakhoul N, Araùjo-Miranda R, et al. The challenge of pediatric uveitis: tertiary referral center experience in the United States. Ocul Immunol Inflamm. 2019;27:410–7. https://doi.org/10.1080/09273948.2017.1420202.
Lee RWJ, Dick AD. Current concepts and future directions in the pathogenesis and treatment of non-infectious intraocular inflammation. Eye. Nature Publishing Group; 2012. p. 17–28.
Hoeve M, Ayuso VK, Schalij-Delfos NE, Los LI, Rothova A, De Boer JH. The clinical course of juvenile idiopathic arthritis-associated uveitis in childhood and puberty. Br J Ophthalmol. 2012;96:852–6.
Kalinina Ayuso V, Makhotkina N, van Tent-Hoeve M, de Groot-Mijnes JDF, Wulffraat NM, Rothova A, et al. Pathogenesis of juvenile idiopathic arthritis associated uveitis: The known and unknown. Surv Ophthalmol. Elsevier; 2014. p. 517–31. Available from: https://www.sciencedirect.com/science/article/pii/S0039625714000733?via%3Dihub. [Cited 2020 Apr 15].
Kalinina Ayuso V, Ten Cate HAT, Van Den Does P, Rothova A, De Boer JH. Young age as a risk factor for complicated course and visual outcome in intermediate uveitis in children. Br J Ophthalmol. 2011;95:646–51.
Smith V, Vanhaecke A, Herrick AL, Distler O, Guerra MG, Denton CP, et al. Fast track algorithm: How to differentiate a “scleroderma pattern” from a “non-scleroderma pattern”. Autoimmun Rev. Elsevier; 2019. p. 102394. Available from: https://www.sciencedirect.com/science/article/pii/S1568997219302010. [Cited 2020 Apr 8].
Smith V, Herrick AL, Ingegnoli F, Damjanov N, De Angelis R, Denton CP, et al. Standardisation of nailfold capillaroscopy for the assessment of patients with Raynaud’s phenomenon and systemic sclerosis. Autoimmun Rev. 2020;19:102458. https://doi.org/10.1016/j.autrev.2020.102458.
Tavakol ME, Fatemi A, Karbalaie A, Emrani Z, Erlandsson BE. Nailfold capillaroscopy in rheumatic diseases: which parameters should be evaluated? Biomed res int. Hindawi Limited. 2015;2015:974530.
Melsens K, Cutolo M, Schonenberg-Meinema D, Foeldvari I, Leone MC, Mostmans Y, et al. Standardized nailfold capillaroscopy in children with rheumatic diseases: a worldwide study. Rheumatology. 2023;62:1605–15.
Philip S, Najafi A, Tantraworasin A, Pasquale LR, Ritch R. Nailfold capillaroscopy of resting peripheral blood flow in exfoliation glaucoma and primary open-angle glaucoma. JAMA Ophthalmol. 2019;137:618–25.
Cousins CC, Kang JH, Bovee C, Wang J, Greenstein SH, Turalba A, et al. Nailfold capillary morphology in exfoliation syndrome. Eye (Basingstoke). 2017;31:698–707.
Erol MK, Balkarli A, Toslak D, Dogan B, Durmaz D, Süren E, et al. Evaluation of nailfold videocapillaroscopy in central serous chorioretinopathy. Graefe’s Archive Clin Experiment Ophthalmol. 2016;254:1889–96.
Chen X, Yao X, Chi Y, Guo C, Zhang J, Li J, et al. A Cross-sectional observational study of nailfold capillary morphology in uveitis. Curr Eye Res. 2018;43:1342–50.
Nederlands Oogheelkundig Gezelschap. Uveitis. 2020. Available from: https://richtlijnendatabase.nl/richtlijn/uveitis/uveitis_-_startpagina.html
Martini A, Ravelli A, Avcin T, Beresford MW, Burgos-Vargas R, Cuttica R, et al. Toward new classification criteria for juvenile idiopathic arthritis: first steps, pediatric rheumatology international trials organization international consensus. J Rheumatol. 2019;46:190–7.
Agarwal A, Pichi F, Invernizzi A, Gupta V. Disease of the Year: Differential Diagnosis of Uveitic Macular Edema. Ocul Immunol Inflamm. Taylor and Francis Ltd; 2019. p. 72–88.
Fardeau C, Champion E, Massamba N, Lehoang P. Uveitic macular edema. Eye (Basingstoke). 2016;30:1277–92.
Kempen JH, Sugar EA, Jaffe GJ, Acharya NR, Dunn JP, Elner SG, et al. Fluorescein angiography versus optical coherence tomography for diagnosis of uveitic macular edema. Ophthalmology. 2013;120:1852–9.
Kouwenberg CV, Blom LA, Vellinga SC, Bozkir I, de Boer JH, Ayuso VK-K. The role of the retinal nerve fiber layer thickness on OCT in the evaluation of papillitis in childhood uveitis: evaluating papillitis in pediatric uveitis using OCT-RNFL. Am J Ophthalmol. 2023;254:62–8.
Smith V, Beeckman S, Herrick AL, Decuman S, Deschepper E, De Keyser F, et al. An EULAR study group pilot study on reliability of simple capillaroscopic definitions to describe capillary morphology in rheumatic diseases. Rheumatology (United Kingdom). 2016;55:883–90.
Dino-Lite. Dino-Lite Software. Available from: https://www.dino-lite.eu/en/support-download/software. [Cited 2020 Jun 10].
Hofstee HMA, Serné EH, Roberts C, Hesselstrand R, Scheja A, Moore TL, et al. A multicentre study on the reliability of qualitative and quantitative nail-fold videocapillaroscopy assessment. Rheumatology. 2012;51:749–55.
John Curnow S, Murray PI, Williams L. Inflammatory mediators of uveitis: cytokines and chemokines. Curr Opin Ophthalmol. 2006. Available from: www.bdbiosciences.com.
G-J Ooi K, Galatowicz G, Calder VL, Lightman SL. Cytokines and Chemokines in Uveitis-Is there a Correlation with Clinical Phenotype?. Clin Med Res. Available from: http://www.clinmedres.org
Vidovic Valentincic N, De Groot-Mijnes JDF, Kraut A, Korosec P, Hawlina M, Rothova A. Intraocular and serum cytokine profiles in patients with intermediate uveitis. 2011.
Jawad S, Liu B, Agron E, Nussenblatt RB, Sen HN. Elevated serum levels of interleukin-17A in uveitis patients. Ocul Immunol Inflamm. 2013;21:434–9.
Zelazowska-Rutkowska B, Mrugacz M, Cylwik B. Comparison of the diagnostic power of serum IL-6, IL-8 and TNF-α for the idiopathic anterior uveitis in children. Clin Lab. 2017;63:1889–95.
Walscheid K, Neekamp L, Heiligenhaus A, Weinhage T, Heinz C, Foell D. Increased circulating proinflammatory t lymphocytes in children with different forms of anterior uveitis: results from a pilot study. Ocul Immunol Inflamm. 2019;27:788–97.
Yildiz Balci S, Turan-Vural E, Turkyilmaz O, Esen F, Aksaray S. Complete blood count parameters and neutrophil-to-lymphocyte ratio values as markers for differentiation between systemic infectious and non-infectious uveitis. Int Ophthalmol. 2020;40:3033–41.
Kurtul BE, Ozer PA. Neutrophil-to-lymphocyte ratio in ocular diseases: a systematic review. Int J Ophthalmol. 2019;12:1951–8.
Ozgonul C, Sertoglu E, Ayyildiz O, Mumcuoglu T, Kucukevcilioglu M, Gokce G, et al. Novel biomarkers for patients with idiopathic acute anterior uveitis: Neutrophil to lymphocyte ratio and platelet to lymphocyte ratio. Int J Ophthalmol. 2017;10:262–6.
Kuiper JJW, Verhagen FH, Hiddingh S, Wennink RAW, Hansen AM, Casey KA, et al. A network of serum proteins predict the need for systemic immunomodulatory therapy at diagnosis in noninfectious uveitis. Ophthalmol Sci. 2022;2:100175.
Balamurugan S, Das D, Hasanreisoglu M, Toy B, Akhter M, Anuradha V, et al. Interleukins and cytokine biomarkers in uveitis. Indian J Ophthalmol. 2020;68:1750–63 (Wolters Kluwer Medknow Publications).
Weinstein JE, Pepple KL. Cytokines in uveitis. Curr Opin Ophthalmol. Lippincott Williams and Wilkins; 2018. p. 267–74.
Wennink RAW, de Boer JH, Hiddingh S, Haasnoot AMJW, Ayuso VK, de Hoop T, et al. Next-generation HLA sequence analysis uncovers shared risk alleles between clinically distinct forms of childhood uveitis. Invest Ophthalmol Vis Sci. 2021;62:19.
Heiligenhaus A, Klotsche J, Niewerth M, Horneff G, Ganser G, Haas JP, et al. Similarities in clinical course and outcome between juvenile idiopathic arthritis (JIA)-associated and ANA-positive idiopathic anterior uveitis: Data from a population-based nationwide study in Germany. Arthritis Res Ther. 2020;22:1–11.
Li AR, Burke CD, Purvis CS, Lee LW. Association between nailfold capillaroscopy abnormalities and autoimmune disease in pediatric populations. Pediatr Dermatol. 2022;39:197–204.
Tian J, Xie Y, Li M, Oatts J, Han Y, Yang Y, et al. The relationship between nailfold microcirculation and retinal microcirculation in healthy subjects. Front Physiol. 2020;11:880.
Shi W-Q, Han T, Liu R, Xia Q, Xu T, Wang Y, et al. Retinal microvasculature and conjunctival vessel alterations in patients with systemic lupus erythematosus—an optical coherence tomography angiography study. Front Med (Lausanne). 2021;8:724283.
Liu R, Wang Y, Xia Q, Xu T, Han T, Cai S, et al. Retinal thickness and microvascular alterations in the diagnosis of systemic lupus erythematosus: a new approach. Quant Imaging Med Surg. 2022;12:823–37.
Silpa-archa S, Lee JJ, Foster CS. Ocular manifestations in systemic lupus erythematosus. Br J Ophthalmol. 2016;100:135–41.
Kök M, Ayan A, Fatih Küçük M, Erol MK, Yaprak L. Evaluation of the direct effects on retinal and choroidal microvascularity of systemic scleroderma. Microvasc Res. 2021;136:104166.
Szucs G, Szekanecz Z, Aszalos Z, Gesztelyi R, Zsuga J, Szodoray P, et al. A wide spectrum of ocular manifestations signify patients with systemic sclerosis. Ocul Immunol Inflamm. 2021;29:81–9.
Rommel F, Prangel D, Prasuhn M, Grisanti S, Ranjbar M. Correlation of retinal and choroidal microvascular impairment in systemic sclerosis. Orphanet J Rare Dis. 2021;16:27.
Yılmaz Tuğan B, Sönmez HE, Güngör M, Yüksel N, Karabaş L. Preclinical ocular microvascular changes in juvenile dermatomyositis: a pilot optical coherence tomography angiography study. Microvasc Res. 2022;143:104382.
Jakhar D, Grover C, Singal A, Das G. Nailfold capillaroscopy and retinal findings in patients with systemic sclerosis: Is there an association? Indian Dermatol Online J. 2020;11:382.
Sulli A, Paolino S, Pizzorni C, Ferrari G, Pacini G, Pesce G, et al. Progression of nailfold capillaroscopic patterns and correlation with organ involvement in systemic sclerosis: a 12 year study. Rheumatology (United Kingdom). 2020;59:1051–8.
Acknowledgements
Not applicable.
Funding
This work was supported by funding from the Oogfonds and Dr. F.P. Fischer-Stichting, which contributed through UitZicht. The ODAS Stichting also funded the study. The funders did not play a role in the study design, collection, analysis, interpretation, or reporting of these data.
Author information
Authors and Affiliations
Contributions
CK, VKA, and JdB conceptualized and designed the study. CK designed the instruments for collecting the data and collected the data. CK, JS, EdG, and VKA scored the nailfold capillaroscopic images. CK carried out the initial analyses and drafted the manuscript. JS supervised the data analyses. VKA coordinated and supervised the data collection and data analyses. JdB supervised the data collection and data analyses. All authors (CK, JS, EdG, JdB, VKA) critically reviewed and revised the manuscript, providing important intellectual input. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study adhered to the tenets of the Declaration of Helsinki and was approved by the UMCU Medical Research Ethics Committee (protocol number: 20–317).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1
. Supplementary Material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Kouwenberg, C.V., Spierings, J., de Groot, E.L. et al. Involvement of the systemic microcirculation in pediatric uveitis. Pediatr Rheumatol 21, 109 (2023). https://doi.org/10.1186/s12969-023-00896-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12969-023-00896-7