Abstract
Background
This study aimed to assess the baseline characteristics and clinical outcomes of coronavirus disease 2019 (COVID-19) in pediatric patients with rheumatic and musculoskeletal diseases (RMD) and identify the risk factors associated with symptomatic or severe disease defined as hospital admission, intensive care admission or death.
Methods
An observational longitudinal study was conducted during the first year of the SARS-CoV-2 pandemic (March 2020–March 2021). All pediatric patients attended at the rheumatology outpatient clinics of six tertiary referral hospitals in Madrid, Spain, with a diagnosis of RMD and COVID-19 were included. Main outcomes were symptomatic disease and hospital admission. The covariates were sociodemographic and clinical characteristics and treatment regimens. We ran a multivariable logistic regression model to assess associated factors for outcomes.
Results
The study population included 77 pediatric patients. Mean age was 11.88 (4.04) years Of these, 30 patients (38.96%) were asymptomatic, 41 (53.25%) had a mild-moderate COVID-19 and 6 patients (7.79%) required hospital admission. The median length of hospital admission was 5 (2–20) days, one patient required intensive care and there were no deaths. Previous comorbidities increased the risk for symptomatic disease and hospital admission. Compared with outpatients, the factor independently associated with hospital admission was previous use of glucocorticoids (OR 3.51; p = 0.00). No statistically significant risk factors for symptomatic COVID-19 were found in the final model.
Conclusion
No differences in COVID-19 outcomes according to childhood-onset rheumatic disease types were found. Results suggest that associated comorbidities and treatment with glucocorticoids increase the risk of hospital admission.
Similar content being viewed by others
Background
Severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) infection causes COVID-19 disease, which may present with a myriad of clinical symptoms and signs [1].
Since the first confirmed case of SARS-CoV-2 infection in January 2020, the current COVID-19 outbreak has had considerable impact in Spain, especially in the Madrid region, where a higher incidence of COVID-19 cases has been recorded [2].
The incidence and severity of COVID-19 disease seems to be higher in patients with risk factors such as advanced age and associated comorbidities, mainly hypertension, diabetes, heart disease, and previous respiratory diseases [3,4,5]. Autoimmune systemic disorders may be considered another risk factor for severity and COVID-19 in these patients has been associated with a higher risk of hospital admission [6].
In contrast with infected adults, most infected children appear to have a milder clinical course, and asymptomatic infections are not uncommon [7]. The admission rate to intensive care for pediatric patients with COVID-19 is around 2–3%, and fatal cases are rare (0,08%) [8, 9].
Children may develop a multisystemic inflammatory syndrome in association with COVID-19 (MIS-C) [10]. However, information on the clinical course of the disease in patients with autoimmune or autoinflammatory conditions is scarce.
Regarding therapies, studies in adult patients with rheumatic and musculoskeletal diseases (RMD) have demonstrated that most synthetic and biological disease-modifying antirheumatic drugs are not associated with worse outcomes in COVID-19. However, patients with poorly controlled active RMD or receiving treatments such as glucocorticoids may have an increased risk of both infection and severe disease [6, 11].
There is growing evidence that pediatric patients with autoimmune/inflammatory diseases receiving immunomodulatory therapy and with SARS-CoV-2 infection are not at a significantly increased risk of poor outcomes [12]. Prior to this study, several small case series of COVID-19 in pediatric patients with RMD have been reported [13, 14]. Evidence on the possible risk factors for poor outcome in pediatric patients with rheumatic disease and COVID-19 and data on outcome of hospital admissions for these patients is scarce.
Therefore, due to a paucity of research data about COVID-19 in pediatric patients with rheumatic diseases, we conducted this study to obtain a general picture of pediatric patients with RMDs and COVID-19 in the region of Madrid. Thus, the purpose was to assess the baseline characteristics and clinical outcomes of COVID-19 in pediatric patients with RMDs and determine the risk factors associated with the development of mild, moderate or severe COVID-19.
Methods
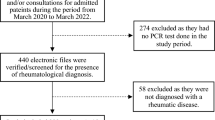
The COVID-SORCOM registry is a multicenter regional registry established to analyse the clinical characteristics and outcomes of COVID-19 in patients with RMD in Madrid, Spain. Aretrospective observational study of children and adolescents with RMD included in this registry was performed, during the period March 2020–March 2021. Clinical and demographic characteristics, COVID-19 data, and outcomes of these patients were analysed.
The inclusion criteria were age < 18 years, a diagnosis of a pediatric RMD (according to ICD-10) and COVID-19 disease confirmed with a positive SARS-CoV-2 polymerase chain reaction (PCR) test, a positive rapid antigen test or detection of antibodies against SARS-CoV-2. Patients with a clinical diagnosis based only on typical symptoms and epidemiological data during the first weeks of the pandemic due to the lack of widely available diagnostic tests, were also included.
The severity of COVID-19 was defined on the basis of clinical features, laboratory testing, and chest radiograph imaging, distinguishing between asymptomatic infection and symptomatic infection (the latter was further classified as mild, moderate, severe, or critical) [15]. Patients with mild disease were those with symptomatic infection who did not require admission; patients with moderate disease those who required hospital admission due to symptoms, patients with severe disease were those who required intensive care, and patients with critical disease those with severe disease and a poor outcome with significant sequelae or death.
Primary outcomes analysed were presence of symptomatic COVID-19 and hospital admission.
Recorded co-variables included:
1) Sociodemographic baseline characteristics including sex, age, and RMD duration.
2) Type of RMD, classified into the following 3 groups: a) chronic inflammatory arthritis: juvenile idiopathic arthritis (JIA) (excluding the systemic subtype), enthesitis-related arthritis, and anterior chronic uveitis associated to JIA; b) multisystemic autoimmune disorders: systemic lupus erythematosus, idiopathic inflammatory myopathy, scleroderma and pediatric vasculitis and c) autoinflammatory diseases: systemic JIA, PFAPA syndrome, chronic recurrent multifocal osteomyelitis and monogenic autoinflammatory syndromes (TRAPS, CAPS, FMF, MKD).
3) Disease activity according to the attending physician’s criteria (clinical remission on and off medication, low, moderate or high disease activity).
4) Baseline comorbidities.
5) Treatment for rheumatic disease: a) glucocorticoids (according to dose: 0 mg, 0-10 mg, > 10 mg), b) nonsteroidal anti-inflammatory drugs (NSAIDs), c) conventional synthetic disease-modifying antirheumatic drugs (csDMARDs); d) targeted synthetic/biologic DMARDs (ts/bDMARDs).
For the hospital admission episode for COVID-19, clinical, laboratory, and treatment data until discharge were recorded.
Patient characteristics were expressed as the mean and standard deviation or median and interquartile range for continuous variables; categorical variables were expressed as percentages. Characteristics of patients with asymptomatic COVID-19 and those with symptoms, including need for hospital admission were compared. Continuous variables were analysed using the Mann-Whitney U test, and discrete variables were analyzed using Fisher’s exact test. Univariable logistic regression analyses were performed to assess differences between asymptomatic or symptomatic cases, hospital admissions due to COVID-19 and covariables. Multivariable logistic regression models (adjusted for age, sex) were tested in a stepwise manner to examine the possible effect of sociodemographic, clinical, and therapeutic factors on symptomatic COVID-19 and COVID-19 hospital admissions. The model also included all other variables with a p < 0.1 from the univariable regression analysis. The results were expressed as the odds ratio (OR) with 95% confidence intervals. Study data were collected and managed using REDCap electronic data capture tools hosted at SORCOM [16, 17]. The study was approved by the Hospital Ramon y Cajal Institutional Ethics Committee (approval number 136–20).
All analyses were performed using Stata v.13 statistical software (Stata Corp., College Station, TX, USA). A two-tailed p value < 0.05 was considered statistically significant.
Results
Patient characteristics
In total, 77 pediatric patients with rheumatic diseases and COVID-19 were included in the study.
Of these, 66.23% were diagnosed with a positive SARS-CoV-2 polymerase chain reaction (PCR) test, 27.27% based on detection SARS-CoV-2 antibodies, and 6.49% had a clinical diagnosis. Fifty-five (71.43%) patients were female and the mean age of patients was 11.88 (SD 4.04) years. Mean time since diagnosis of RMD was 5.78 (SD 4.21) years and most of the patients had a diagnosis of oligoarticular or polyarticular JIA with or without associated uveitis (n = 42, 54.54%). Other diagnoses were systemic lupus erythematosus (n = 8, 10.38%), systemic JIA (n = 5, 6.49%) and monogenic autoinflammatory syndrome (n = 5, 6.49%).
Additional comorbidities included obesity (2 patients), chronic renal disease (2), asthma (1), chronic heart disease (1), previous macrophage activation syndrome (1) and a duplicated collecting system (1) (Main characteristics of pediatric patients with COVID-19 and rheumatic diseases are shown in Table 1).
While 8 of the patients (10.53%) had high RMD activity at the time of COVID-19 diagnosis, most (89.47%) had low activity or were in clinical remission.
Prior to COVID-19 infection, only nine of the patients were taking glucocorticoids (11.68%) and 3 were taking NSAIDs on a regular basis (3.90%). Almost half of the patients were taking csDMARDs, mainly methotrexate (n = 26, 33.77%), antimalarial agents (n = 7, 9.09%) and mycophenolate mofetil (n = 6, 7.79%). Over half of the patients (51.95%) were taking ts/bDMARDs, mainly anti-TNF therapy, etanercept being the most frequently prescribed drug (19.48%), followed by adalimumab (14.29%). Only one patient was taking a Janus-Kinase (JAK) inhibitor. Additionally, 3 patients were taking Angiotensin-converting-enzyme (ACE) inhibitors and two were on oral anticoagulation agents.
COVID-19 outcomes
Of the 77 patients, 47 had at least one COVID-19-related symptom (mainly fever, headache or cough), while 30 patients were asymptomatic. Symptomatic patients were older (14 [8.5–16] vs 12 [9.5–15]) than asymptomatic ones, without significant differences. No patients were diagnosed with the pediatric multisystemic inflammatory syndrome. Overall, 81.52% of patients maintained all their immunosuppressive treatment without changes. Around 20% of patients went to the emergency room due to their symptoms.
Patients with multisystemic autoimmune disorders were more frequently symptomatic due to COVID-19 (71.4% with symptoms), followed by those with autoinflammatory diseases (66.6%). However, there were no significant differences between RMD groups regarding symptomatic disease.
As shown in Table 2, most patients had mild disease, with fever as the most prevalent symptom. No patients had critical disease. Six patients required hospital admission (7.79% of all patients), with a median of 5 days duration (IQR 2–20) and one patient required pediatric intensive care. In each RMD diagnostic category there were two cases of hospital admission. Half of the admitted patients were on bDMARDS (2 on Infliximab, 1 on Canakinumab) (the sociodemographic and clinical characteristics of these patients are described in Table 3).
The only patient who required admission to a Pediatric Intensive Care Unit had a recent diagnosis of systemic JIA, was on treatment with Canakinumab and glucocorticoids (> 10 mg prednisone/day), and had associated comorbidities. This patient developed pneumonia and a pleural effusion and was treated with antibiotic therapy and lopinavir/ritonavir. A catheter-associated right iliac vein appeared as a probably multifactorial complication. A few days later The patient’s condition improved after a few days and the recovery was complete at discharge.
No laboratory or imaging tests were performed for asymptomatic and mildly symptomatic patients and none received specific treatment for COVID-19.
Multivariable model for symptomatic infection
The multivariable logistic regression model for symptomatic infection was adjusted for age, sex and previous comorbidities. None of the variables included in the final model were associated with a statistically significant result. Comorbidities dropped from the final model because predict failure perfectly. Exposure to DMARDs [biological (OR: 1.02 [0.34–3.09]; p = 0.95) or synthetic (OR: 1.24 [0.44–3.46]; p = 0.67)]), and exposure to glucocorticoids (OR: 1.27 [0.47–3.47]; p = 0.62)), did not achieve statistical significance and was not analysed in the final model. Although, long-term treatment with antimalarials seemed to be protective, significance was not demonstrated in the final model (OR: 0.11 [0.007–1.88]; p = 0.13). (Table 4).
Multivariable model for hospital admission
In the multivariable logistic regression model adjusted for hospital admission, exposure to higher doses of glucocorticoids was the only variable associated with a higher odds of hospital admission. Exposure to DMARDs, −regardless of whether they were biological (OR: 1.97 [0.23–16.57]; p = 0.53) or synthetic (OR: 1.20 [0.15–9.56]; p = 0.86)-, did not reach statistical significance in the final model. Comorbidities were not analysed in the final model (OR: 3.45 [0.41–28.48]; p = 0.25). (Table 4).
Discussion
This study conducted at six tertiary care referral hospitals presents the baseline characteristics and outcomes of pediatric patients with rheumatic diseases infected with SARS-CoV-2, contributing to the current knowledge in this area.
In the COVID-SORCOM registry, the majority (61%) of pediatric patients with RMD and COVID-19 had symptomatic infections. Fever, headache and cough were the predominant clinical features at presentation, with similar rates to those observed in a recent international, multicenter study of pediatric COVID-19 [18].
Presence of comorbidities was associated with an increased likelihood of symptomatic COVID-19 in patients with RMD, although under 8% of the patients required hospital admission.
Data from this study also reflect the uncertainties regarding treatment options for COVID-19 with different protocols emerging as knowledge of the disease progressed. In general, admitted patients received few experimental treatments for COVID-19 and in almost all cases symptoms resolved without serious or chronic complications. Patients exposed to disease-modifying agents did not appear to be at higher risk of severe disease or hospital admission due to COVID-19. However, results suggest that pediatric patients with RMD and chronic prior exposure to glucocorticoids have a greater risk of hospital admission, regardless of other factors. Although the number of patients in this study was limited, results are similar to data reported in adult patients with RMD and COVID-19 [6, 11]. Interpretation of data on glucocorticoid use may be challenging, as pediatric rheumatologists generally aim to maintain the lowest possible doses and patients with higher doses usually have more severe disease and/or higher disease activity.
The possibility of a less favorable outcome of COVID-19 in patients taking rituximab has recently been discussed [19,20,21]. In this cohort, only one patient with systemic lupus erythematosus had received rituximab in the 3 months prior to infection and, although presentation was with symptomatic disease, hospital admission was not required. This patient was also on hydroxychloroquine and mycophenolate mofetil, and the latter was discontinued until complete recovery from SARS-CoV-2 infection.
Although available data have shown that COVID-19 in children with RMD undergoing immunomodulatory treatment is not usually associated with severe disease, conventional clinical practice includes temporary interruption of immunomodulatory treatment when there is a concomitant infection [22]. In this cohort, most physicians maintained immunomodulatory treatment in patients with asymptomatic infections. Also, in most patients with symptomatic COVID-19, DMARDs (biological or synthetic) were maintained. Due to uncertainty, during the first wave the proportion of treatments which were discontinued was higher, but after this period, treatment was only stopped in very few cases. There is no evidence that continuing DMARDs during COVID-19 can alter the clinical course of SARS-CoV-2 infection and the benefits of keeping the disease inactive outweigh the risks [19, 22, 23].
The type of RMD seems to play an important role in the probability of hospital admission in adult patients and COVID-19, and patients with systemic autoimmune conditions seem to have the highest risk compared to patients with chronic inflammatory arthritis [6, 18]. However, this was not observed in the current pediatric population and a higher risk for any of the outcomes was not demonstrated.
No patients who required admission developed associated complications, except for an adolescent female with systemic lupus erythematosus and secondary antiphospholipid syndrome who had an episode of deep vein thrombosis of a lower limb. Thrombotic complications seem very uncommon in children with SARS-CoV-2, however, in adolescents with previous thrombotic risk factors thromboprophylaxis must be considered [24].
A large majority of children with asymptomatic disease were in remission. This reflects the importance of keeping the disease under control to avoid symptomatic COVID-19. Patients with high or moderate disease activity may be at greater risk for infections, including SARS-CoV-2.
The strengths of the study include the comprehensive analysis of pediatric patients with RMD and COVID-19 during the peak of the pandemic. All data were entered by the patients´ own rheumatology healthcare providers, the registry collects information on specific RMD diagnoses and includes cases from the major pediatric rheumatology units in Madrid suggesting that these findings may be more representative than single-centre studies..
However, the COVID-SORCOM registry is voluntary and does not capture all cases of COVID-19 in pediatric patients with RMD. This approach to data collection places limitations on causal conclusions and temporal relationships and therefore only limited inferences may be made based on these results. Due to the database design and inherent reporting bias the data may not be used to analyse the incidence of COVID-19 in this patient population.
Although the limited sample size makes this a descriptive study with exploratory analyses, detailed information on this population may be obtained. Preliminary results are in line with data published in the adult population with RMD, and may assist with the decision-making process and patient monitoring. Although further studies are required, children with RMD and/or receiving immunomodulatory therapies do not appear to have a significantly increased risk for severe COVID-19 and preventive measures should be similar to those recommended for the general population [22, 25].
In conclusion, overall outcomes in children and adolescents with RMD appear to be generally favorable, and most patients have non-severe infections. Rarely, COVID-19 may be severe in children and comorbidities and the use of glucocorticoids could be considered risk factors in the RMD pediatric population as well as in adults.
Conclusions
Overall, no differences in COVID-19 outcomes in pediatric patients according to type of childhood-onset rheumatic disease were found. Some factors may increase the likelihood of complicated symptomatic infection and hospital admission. In this clinical registry, results were in concordance with data reported elsewhere in adult patients with RMD and COVID-19, and special caution should be exerted in patients with thrombotic risk, with comorbidities or with previous exposure to corticosteroids. This study provides novel results in childhood-onset rheumatic disease patients regarding susceptibility to moderate-severe COVID-19.
Availability of data and materials
The datasets generated and analyzed for the present study are available from the corresponding author on reasonable request.
Abbreviations
- ACE:
-
Angiotensin-converting-enzyme inhibitors
- CAPS:
-
Cryopyrin-associated periodic syndrome
- COVID-19:
-
Coronavirus disease 2019
- DMARD:
-
Disease-modifying anti-rheumatic drug
- csDMARDs:
-
Classic DMARDs
- ts/bDMARDs:
-
Targeted synthetic or biologic DMARDs
- FMF:
-
Familial Mediterranean fever
- JAK:
-
Janus-Kinase
- JIA:
-
Juvenile idiopathic arthritis
- HIDS:
-
Hyperimmunoglobulin-D syndrome
- IQR:
-
Interquartile Range
- MIS-C:
-
Multisystem inflammatory syndrome in children
- MKD:
-
Mevalonate kinase deficiency
- NSAID:
-
Nonsteroidal anti-inflammatory drugs
- PCR:
-
Polymerase chain reaction
- PFAPA:
-
Periodic fever, adenopathy, pharyngitis and aphthous stomatitis
- RMD:
-
Rheumatic and musculoskeletal diseases
- SARS:
-
Severe acute respiratory syndrome
- TNF:
-
Tumor necrosis factor
- TRAPS:
-
TNF- receptor associated periodic syndrome
References
Fernandez-Gutierrez B. COVID-19 with pulmonary involvement. An autoimmune disease of known cause. Reumatol Clin [internet]. 2020;16(4):253–4. https://doi.org/10.1016/j.reuma.2020.04.001.
Pollán M, Pérez-Gómez B, Pastor-Barriuso R, Oteo J, Hernán MA, Pérez-Olmeda M, et al. Prevalence of SARS-CoV-2 in Spain (ENE-COVID): a nationwide, population-based seroepidemiological study. Lancet. 2020;396(10250):535–44.
Jordan RE, Adab P, Cheng KK. Covid-19: risk factors for severe disease and death. BMJ [Internet]. 2020;368(March):1–2. https://doi.org/10.1136/bmj.m1198.
Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet [Internet]. 2020;395(10223):507–13. https://doi.org/10.1016/S0140-6736(20)30211-7.
Wang Q, Liu J, Shao R, Han X, Su C, Lu W. Risk and clinical outcomes of COVID-19 in patients with rheumatic diseases compared with the general population: a systematic review and meta-analysis. Rheumatol Int [Internet]. 2021. https://doi.org/10.1007/s00296-021-04803-9.
Freites Nuñez DD, Leon L, Mucientes A, Rodriguez-Rodriguez L, Font Urgelles J, Madrid García A, et al. Risk factors for hospital admissions related to COVID-19 in patients with autoimmune inflammatory rheumatic diseases. Ann Rheum Dis. 2020;79(11):1393–9.
Lu X, Zhang L, Du H, et al. SARS-CoV-2 Infection in Children. N Engl J Med. 2020;382(17):1663–5. https://doi.org/10.1056/NEJMc2005073.
Zimmermann P, Curtis N. COVID-19 in children, pregnancy and neonates: a review of epidemiologic and clinical features. Pediatr Infect Dis J. 2020;39(6):469–77.
Liguoro I, Pilotto C, Bonanni M, Ferrari ME, Pusiol A, Nocerino A, et al. SARS-COV-2 infection in children and newborns: a systematic review. Eur J Pediatr. 2020;179(7):1029–46.
Rubens JH, Akindele NP, Tschudy MM, Sick-Samuels AC. Acute covid-19 and multisystem inflammatory syndrome in children. BMJ. 2021;372:1–6.
Gianfrancesco M, Hyrich KL, Hyrich KL, Al-Adely S, Al-Adely S, Carmona L, et al. Characteristics associated with hospitalisation for COVID-19 in people with rheumatic disease: data from the COVID-19 global rheumatology Alliance physician-reported registry. Ann Rheum Dis. 2020;79(7):859–66.
Janda A, Schuetz C, Canna S, Gorelik M, Heeg M, Minden K, et al. Therapeutic approaches to pediatric COVID-19: an online survey of pediatric rheumatologists. Rheumatol Int [internet]. 2021;(0123456789). https://doi.org/10.1007/s00296-021-04824-4.
Surrey R, Hospitals C. Letter to Editor Rheumatology Letter to Editor. Rheumatology. 2017;35:25–6.
Villacis-Nunez DS, Rostad CA, Rouster-Stevens K, Khosroshahi A, Chandrakasan S, Prahalad S. Outcomes of COVID-19 in a cohort of pediatric patients with rheumatic diseases. Pediatr Rheumatol. 2021;19(1):1–8.
Dong Y, Mo X, Hu Y, Qi X, Jiang F, Jiang Z, Tong S. Epidemiology of COVID-19 Among Children in China. Pediatrics. 2020;145(6):e20200702. https://doi.org/10.1542/peds.2020-0702.
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)-a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–81.
Harris PA, Taylor R, Minor BL, Elliott V, Fernandez M, O'Neal L, McLeod L, Delacqua G, Delacqua F, Kirby J, Duda SN; REDCap Consortium. The REDCap consortium: Building an international community of software platform partners. J Biomed Inform. 2019;95:103208. https://doi.org/10.1016/j.jbi.2019.103208.
Götzinger F, Santiago-García B, Noguera-Julián A, Lanaspa M, Lancella L, Calò Carducci FI, et al. COVID-19 in children and adolescents in Europe: a multinational, multicentre cohort study. Lancet Child Adolesc Heal. 2020;4(9):653–61.
Nuño L, Novella Navarro M, Bonilla G, Franco-Gómez K, Aguado P, Peiteado D, et al. Clinical course, severity and mortality in a cohort of patients with COVID-19 with rheumatic diseases. Ann Rheum Dis. 2020;79(12):1659–61.
Bachiller-Corral J, Boteanu A, Garcia-Villanueva MJ, de la Puente C, Revenga M, Diaz-Miguel MC, et al. Risk of severe coronavirus infection (COVID-19) in patients with inflammatory rheumatic diseases. J Rheumatol. 2021;jrheum:200755.
Schäfer M, Strangfeld A, Hyrich KL, Carmona L, Gianfrancesco M, Lawson-Tovey S, Mateus EF, Gossec L, Robinson PC, Yazdany J, Machado PM. Response to: 'Correspondence on 'Factors associated with COVID-19-related death in people with rheumatic diseases: results from the COVID-19 Global Rheumatology Alliance physician reported registry'' by Mulhearn et al. Ann Rheum Dis. 2021:annrheumdis-2021-220134. https://doi.org/10.1136/annrheumdis-2021-220134.
Wahezi DM, Lo MS, Rubinstein TB, Ringold S, Ardoin SP, Downes KJ, et al. American College of Rheumatology Guidance for the Management of Pediatric Rheumatic Disease during the COVID-19 pandemic: version 1. Arthritis Rheum. 2020;72(11):1809–19.
Batu ED, Lamot L, Sag E, Ozen S, Uziel Y. How the COVID-19 pandemic has influenced pediatric rheumatology practice: results of a global, cross-sectional, online survey. Semin Arthritis Rheum [internet]. 2020;50(6):1262–8. https://doi.org/10.1016/j.semarthrit.2020.09.008.
Alonso DA, Murias S, Garde AM-A, Arandes AS, Pareja M. Prevalence of thrombotic complications in children with SARS- CoV-2; 2021. p. 1–4.
Haşlak F, Yıldız M, Adrovic A, Barut K, Kasapçopur Ö. Childhood rheumatic diseases and COVID-19 pandemic: an intriguing linkage and a new horizon. Balkan Med J. 2020;37(4):184–8.
Acknowledgements
We wish to thank all rheumatology providers who entered data into the registry.
Funding
None funding.
Author information
Authors and Affiliations
Contributions
DC and LL wrote the manuscript, which was critically revised by AB, JB and LA. All authors contributed to manuscript revisions and read and approved the submitted version.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Hospital Ramon y Cajal Institutional Ethics Committee (approval number 136–20).
Consent for publication
The final manuscript has been read and approved by all authors.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Clemente, D., Udaondo, C., de Inocencio, J. et al. Clinical characteristics and COVID-19 outcomes in a regional cohort of pediatric patients with rheumatic diseases. Pediatr Rheumatol 19, 162 (2021). https://doi.org/10.1186/s12969-021-00648-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12969-021-00648-5