Abstract
Background
Phase-contrast cine cardiovascular magnetic resonance (CMR) of the coronary sinus has emerged as a non-invasive method for measuring coronary sinus blood flow and coronary flow reserve (CFR). However, its clinical utility has not yet been established. Here we performed a meta-analysis to clarify the clinical value of CMR-derived CFR in various cardiovascular diseases.
Methods
An electronic database search was performed of PubMed, Web of Science Core Collection, Cochrane Advanced Search, and EMBASE. We compared the CMR-derived CFR of various cardiovascular diseases (stable coronary artery disease [CAD], hypertrophic cardiomyopathy [HCM], dilated cardiomyopathy [DCM]) and control subjects. We assessed the prognostic value of CMR-derived CFR for predicting major adverse cardiac events (MACE) in patients with stable CAD.
Results
A total of 47 eligible studies were identified. The pooled CFR from our meta-analysis was 3.48 (95% confidence interval [CI], 2.98–3.98) in control subjects, 2.50 (95% CI, 2.38–2.61) in stable CAD, 2.01 (95% CI, 1.70–2.32) in cardiomyopathies (HCM and DCM). The meta-analysis showed that CFR was significantly reduced in stable CAD (mean difference [MD] = −1.48; 95% CI, −1.78 to −1.17; p < 0.001; I2 = 0%; p for heterogeneity = 0.33), HCM (MD = −1.20; 95% CI, −1.63 to −0.77; p < 0.001; I2 = 0%; p for heterogeneity = 0.49), and DCM (MD = −1.53; 95% CI, −1.93 to −1.13; p < 0.001; I2 = 0%; p for heterogeneity = 0.45). CMR-derived CFR was an independent predictor of MACE for patients with stable CAD (hazard ratio = 0.52 per unit increase; 95% CI, 0.37–0.73; p < 0.001; I2 = 84%, p for heterogeneity < 0.001).
Conclusions
CMR-derived CFR was significantly decreased in cardiovascular diseases, and a decreased CFR was associated with a higher occurrence of MACE in patients with stable CAD. These results suggest that CMR-derived CFR has potential for the pathological evaluation of stable CAD, cardiomyopathy, and risk stratification in CAD.
Similar content being viewed by others
Introduction
Evaluating the microcirculation is extremely important in the diagnosis of coronary artery disease (CAD). A new disease concept, ischemic nonobstructive CAD (INOCA), was proposed to describe a condition in which myocardial ischemia occurs despite the absence of an obstructive lesion in the epicardial coronary artery. American Heart Association/American College of Cardiology guidelines also emphasize the importance of microcirculatory disturbances in INOCA. Moreover, microcirculatory disturbances are involved in the pathogenesis of various cardiovascular diseases [1]. The prevalence of microvascular dysfunction (MVD) is higher than ever in many clinical settings [2, 3], and its presence is associated with worse clinical outcomes [4]. Various indices have been proposed to evaluate microcirculatory disturbances, one of which is coronary flow reserve (CFR). CFR is an index of a combination of the epicardial coronary artery and the microvasculature [5]. In the absence of epicardial CAD, impairment of the CFR suggests the presence of MVD. Positron emission tomography (PET) is an established non-imaging modality for evaluating CFR [6]. However, PET imaging has some limitations, including radiation exposure, availability, and high cost. These disadvantages limit the widespread clinical use of PET for assessing CFR.
Phase-contrast cine cardiovascular magnetic resonance (CMR) of the coronary sinus is another method used to quantify myocardial blood flow (MBF) [7]. An estimated 96% of the blood flow is returned through the myocardium through the coronary sinus. Therefore, coronary sinus blood flow can approximate the total MBF. The volume of myocardial blood flow per gram of myocardium can be estimated by dividing the coronary sinus blood flow by the myocardial weight. The ratio of MBF can be used to calculate CFR during pharmacological stress divided by that at rest, which is linearly correlated with PET-derived CFR [7]. Owing to its ability to test without radiation exposure, CMR-derived CFR overcomes the limitations of PET-derived CFR. However, owing to limited evidence, the clinical relevance of CMR-derived CFR is not well known. Therefore, here we performed a meta-analysis to compare CMR-derived CFR findings of patients with cardiovascular diseases and healthy controls. We also assessed the prognostic value of CMR-derived CFR in patients with stable CAD.
Materials and methods
Literature search
We searched the electronic databases PubMed, Web of Science Core Collection, Cochrane Advanced Search, and EMBASE using the search formulas listed in the Appendix (Additional file 1). We performed the database search on May 25, 2022. After screening all abstracts from the search results, potentially relevant studies were reviewed by two reviewers (SK and MA) for final eligibility. A third reviewer resolved disagreements between them. This meta-analysis adhered to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines. This protocol was registered in the University Medical Informatics Network (R000054826). We did not obtain institutional review board approval since this study was a meta-analysis.
Eligibility criteria and outcomes
We included prospective and retrospective studies that included data on CFR evaluated by phase-contrast CMR of the coronary sinus in patients with cardiovascular diseases and CAD risk factors. The subjects included healthy individuals and controls (a group of patients who underwent CMR for some clinical reason but in whom no abnormalities were detected), those with CAD, and those with cardiomyopathy (hypertrophic cardiomyopathy [HCM] and dilated cardiomyopathy [DCM]). Studies of other diseases were excluded from the meta-analysis. We did not include studies on myocardial perfusion reserve using stress-perfusion CMR, as the methodology is completely different. Only articles published in English were included in this study.
Two reviewers extracted the study characteristics, including author name, publication year, country of origin, patients’ diseases, and CMR parameters (SK, MA). First, the disease, age, sex, and CMR parameters for each study were extracted (in addition to CFR from phase-contrast cine CMR, which was the focus of the study, MBF calculated from blood flow in the coronary sinus, left ventricular (LV) function, LV volume, and late gadolinium enhancement (LGE). Second, we compared the CFR between cardiovascular disorders and healthy controls. Finally, the hazard ratio (HR) of CFR for the major adverse cardiac event (MACE) was evaluated in patients with CAD.
In the literature, two separate methods are used to calculate CFR. The first method calculates the CFR by dividing the blood flow in the coronary sinus at stress by the blood flow at rest. The second method is to divide the coronary sinus blood flow by the LV myocardial weight to calculate the MBF (mL/min/g) and then divide the MBF at stress by the MBF at rest to calculate CFR. Because the CFR values are the same for both methods, those calculated by these two methods are harmonized. We also used the Newcastle–Ottawa Quality Assessment Scale and Case Control Studies to evaluate the risk of bias [8] (Additional file 1).
Statistical analysis
A random model meta-analysis was performed using RevMan 5.41 (Cochrane Collaboration, London, UK). Using the mean difference (MD), the CFR results were compared between patients with cardiovascular disease (stable CAD, HCM, DCM), and a healthy control HR meta-analysis was performed of stable CAD using the general inverse variance method. Heterogeneity was indicated by I2, where 0% indicated no heterogeneity and 100% indicated strong heterogeneity (p < 0.05), which was considered statistically significant.
Results
Study characteristics
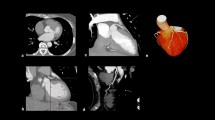
Of the 565 candidate studies, 47 were deemed eligible for inclusion [7, 9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55] (Fig. 1). Fourteen studies presented two populations each [9, 11, 15,16,17, 23, 25, 27, 29, 31, 32, 34, 47, 49], while two studies presented four populations each [30, 35]. Therefore, a total of 67 independent populations were included. Among the 47 studies, 22 were from Japan [19,20,21, 23,24,25,26,27,28,29,30,31,32,33,34,35,36,37, 42, 44, 45, 47], eight from the United States [7, 14, 22, 40, 41, 48, 51, 55], five from Sweden [12, 16, 17, 53, 54], three from Germany and Sweden [11, 15, 46], two from Finland [38, 39], and one each from Australia [18], France [43], Italy [9], Norway [13], Turkey [10], the United Kingdom [49], Switzerland [7], and the Netherlands [50]. Year of publication ranged from 1992 to 2022. In 35 studies, 1.5T CMR systems were used [7, 9,10,11,12, 15,16,17, 19,20,21, 24,25,26,27,28,29,30,31,32, 34,35,36,37,38,39,40, 42, 46,47,48,49, 51, 52, 54]; in nine studies, 3T CMR systems were used [13, 14, 18, 22, 33, 41, 43, 53, 55]; in one study, both 1.5 and 3T CMR units were used [44]; and in one study, a 0.6T CMR system was used [50]. Information on pharmacological stress was extracted from 41 studies. Four studies used the cold pressor test [21, 33, 41, 43], while two studies did not perform any stress testing [9, 50]. Because CPT detects endothelial function–dependent increases in blood flow that differ significantly from pharmacological stress, only resting blood flow was extracted and integrated from the four CPT studies [21, 33, 41, 43]. A total of 28 (68%) studies used adenosine triphosphate infusion, 10 (24%) used dipyridamole, and three (8%) used the regadenoson. However, no study has employed exercise-stress testing. The median value of velocity encoding (VENC) was set at 50 cm/s at rest (range, 40–200 cm/s). Most studies used the same VENC during rest and stress. In six studies, different VENC were used during pharmacological stress. In four studies [10, 12, 40, 48], the VENC during stress was 200 cm/s. In the study by Gyllenhammar et al. [16], the VENC was 120 cm/s. According to Moro et al. [43], the VENC was 150 cm/s. Thirteen studies performed phase-offset correction using adjacent myocardial tissue [21, 28,29,30,31, 33, 35,36,37,38,39, 47, 55], and one study used static tissue regions in the chest wall [55]. The standard imaging parameters and analytical images related to phase-contrast cine CMR are presented (Additional files 1, 2).
CFR of patients with cardiovascular diseases versus controls
Among the control subjects, the pooled CFR from the meta-analysis was 3.48 (range, 2.98–3.98; I2 = 97%; p for heterogeneity < 0.001) (Fig. 2). The estimated CFR was 2.50 (range, 2.38–2.61; I2 = 97%; p for heterogeneity < 0.001) for patients with stable CAD (Fig. 3) and 2.01 (range, 1.70–2.32; I2 = 82%; p for heterogeneity < 0.001) for those with cardiomyopathies (HCM and DCM) (Fig. 4). Coronary sinus blood flow and MBF values are summarized in Figs. 5, 6 and 7. Among the control subjects, mean coronary sinus blood flow was 100 mL/min (range, 83–118 mL/min) at rest and 312 mL/min (range, 251–374 mL/min) during stress, while the mean MBF was 0.79 mL/min/g (range, 0.69–0.90 mL/min/g) at rest and 2.8 mL/min/g (range, 2.13–3.39 mL/min/g) during stress (Fig. 5).
Among the stable CAD patients, mean coronary sinus blood flow was 102 mL/min (range, 94–110 mL/min) at rest and 240 mL/min (range, 222–257 mL/min) during stress, while the MBF was 0.9 mL/min/g (range, 0.8–1.0 mL/min/g) at rest and 2.0 mL/min/g (range, 1.8–2.2 mL/min/g) during stress (Fig. 6).
Among the patients with cardiomyopathies, the mean coronary sinus blood flow was 127 mL/min (range, 99–155 mL/min) at rest and 253 mL/min (range, 171–336 mL/min) during stress, while the mean MBF was 0.7 mL/min/g (range, 0.5–0.8 mL/min/g) at rest and 1.8 mL/min/g (range, 1.0–2.7 mL/min/g) during stress (Fig. 7). The meta-analysis showed that the mean CFR was significantly reduced among the patients with stable CAD (MD = -1.48; 95% CI, -1.78 to -1.17; p < 0.001; I2 = 0%; p for heterogeneity = 0.48) (Fig. 8A), HCM (MD = -1.20; 95% CI, − 1.63 to − 0.77; p < 0.001; I2 = 0%; p for heterogeneity = 0.49) (Fig. 8B), and DCM (MD = -1.53; 95% CI, − 1.93 to − 1.13; p < 0.001; I2 = 0%; p for heterogeneity = 0.45) (Fig. 8C) compared to the control subjects.
Comparison of CFR between cardiovascular diseases and controls. A–C Meta-analysis showed that CFR was significantly decreased in various cardiovascular diseases, such as CAD, HCM, and DCM, compared with control subjects. CAD coronary artery disease, CFR coronary flow reserve, DCM dilated cardiomyopathy, HCM hypertrophic cardiomyopathy
Association between CFR and MACE
Four studies showed outcomes data for patients with stable CAD [22, 27, 30, 35] (Table 1). All studies defined the outcome as a composite endpoint (MACE). Indorkar et al. [22] defined MACE as death, nonfatal myocardial infarction (MI), heart failure hospitalization, sustained ventricular tachycardia, and late revascularization. Kanaji et al. [25] defined MACE as all-cause death, nonfatal MI, hospitalization for congestive heart failure, and stroke. In another study, Kanaji et al. [27] defined MACE as cardiac death, MI, clinically driven remote revascularization (> 3 months after the index percutaneous coronary intervention), or hospitalization for heart failure (HF). Kato et al. [35] defined MACE as cardiovascular death, acute MI, unstable angina, HF hospitalization, or ventricular tachyarrhythmia necessitating defibrillation. A meta-analysis revealed that a higher CMR-derived CFR was significantly associated with a lower MACE rate (HR = 0.52 per unit increase; 95% CI, 0.37–0.73; p < 0.001; I2 = 84%; p for heterogeneity < 0.001) (Fig. 9).
Forest plot of the hazard ratio of CFR among patients with CAD. The meta-analysis revealed that a higher CMR-derived CFR was significantly associated with a lower rate of MACE (HR = 0.52 per unit increase; 95% CI, 0.37–0.73; p < 0.001; I2 = 84%, p for heterogeneity < 0.001). CAD coronary artery disease, CFR coronary flow reserve, CI confidence interval, CMR cardiac magnetic resonance, MACE major adverse cardiac events
Discussion
The main findings of this study are as follows: (1) CMR-derived CFR was substantially decreased in patients with cardiovascular diseases versus control subjects; and (2) a decreased CFR was associated with a higher rate of MACE among patients with stable CAD. These results suggest that CMR-derived CFR might be applicable as a non-invasive marker to identify abnormal microvascular function in patients with various cardiovascular diseases.
Importance of microvascular function and CFR assessment by PET imaging
The epicardial coronary arteries (diameter > 400 μm) are conductance vessels, whereas the pre-arterioles (diameter 100–400 μm) and intramural arterioles (diameter < 100 μm) are resistance vessels [5]. Myocardial flow distribution is mainly regulated by small vessels such as the pre-arterioles or arterioles. In MVD, several structural and functional abnormalities occur in these small vessels, such as microvascular remodeling and endothelial dysfunction [56]. These abnormalities are related to attenuated vasodilator response of the smooth muscle cells of vessels resistive to adenosine and dipyridamole associated with impaired CFR. CFR is a functional measure of the epicardial coronary artery and the coronary microcirculation. In the absence of epicardial stenotic disease, a decreased CFR can be a surrogate marker of coronary microvascular dysfunction [57]. PET is the most firmly established non-invasive quantitative assessment method for MBF and CFR. Recent data have demonstrated that the prevalence of a CFR impairment is higher than expected in patients with known or suspected CAD [5]. Moreover, the predictive value of PET-derived CFR is well established [6]. Based on robust clinical evidence, the United States Food and Drug Administration approved the application of 82Rubidium and 13N-Ammonia PET for assessing CFR [5]. However, the utility of PET for evaluating myocardial perfusion has not yet been established.
CFR assessment using phase-contrast cine MRI of the coronary sinus
Despite the rich clinical evidence of PET imaging for assessing CFR, it features some limitations, such as radiation exposure, limited accessibility, and high cost. Phase-contrast cine CMR of the coronary sinus is also used to quantify CFR. This method has an absolute advantage over PET in that it does not involve radiation exposure. The coronary sinus theoretically drains approximately 96% of the total LV myocardial blood flow [58]; therefore, the LV myocardial blood flow can be calculated by measurement of coronary sinus blood flow. Previous studies reported that phase-contrast cine CMR-derived coronary sinus blood flow correlates well with myocardial blood flow by PET [7]. This evidence demonstrates the high accuracy of CMR-derived CFR.
To date, clinical evidence of CMR-derived CFR is relatively limited. Therefore, here we performed a meta-analysis to determine its clinical relevance. Compared with controls, we found a significant decrease in CFR in various cardiovascular diseases, such as CAD and cardiomyopathies (Figs. 2, 3 and 4). Moreover, CMR-derived CFR can provide prognostic information for patients with CAD. Regarding its technical aspects, setting VENC and phase-offset correction is essential to an accurate evaluation of the blood flow within the coronary sinus. The median VENC was 50 cm/s at rest (40–200 cm/s). Suboptimal VENC settings can lead to aliasing, which can lead to blood flow under- or overestimations. A 40 cm/s VENC at adenosine loading is generally not considered sufficient to increase coronary flow by a factor of 3 to 4, especially during stress; therefore, the VENC should be increased appropriately.
Regarding phase offset correction, 13 studies used adjacent myocardial tissue and one used static tissue regions at the chest wall. Other studies did not perform phase offset correction. Some studies reported the importance of the impact of phase offset correction but did not explain why phase offset correction was not performed. In addition, because of our limited technical knowledge of phase offset correction, we could not adequately determine its importance (whether it is absolutely necessary) in this study. Further research on this topic is required. Evaluation of the effect of medical therapy, such as angiotensin-converting enzyme inhibitors/angiotensin receptor blockers and statins on CFR, is of interest. A recent meta-analysis showed the impact of medical therapies on CFR [59]. However, CMR data were not included thus, further studies are warranted to assess the utility of phase-contrast CMR in the serial impact of medical therapies on CFR.
We believe that our data will contribute to the accurate assessment of CFR using phase-contrast cine CMR of the coronary sinus. However, the relationship between the CMR-derived CFR and stress-perfusion CMR should be recognized. Although this study shows great potential for CMR-derived CFR, the mainstream method remains stress-perfusion CMR. CMR-derived CFR should be performed within a protocol featuring stress-perfusion CMR. However, CMR-CFR has the potential to assess the global microcirculation, which is difficult to assess using stress-perfusion CMR, and may add new CMR value to the diagnosis of INOCA in the post-ischemia era [60].
Limitations
Our study has several limitations. First, evidence of the prognostic value of CMR-derived CFR mainly targets patients with known or suspected CAD. However, this should be recognized as a limitation because event definitions differed among the studies integrated here. The predictive value of future adverse events for other cardiovascular diseases remains unknown. Second, CMR-derived CFR can assess global and not regional CFR. It is important to remember that stress-perfusion CMR is the mainstream examination method for diagnosing ischemia, whereas phase-contrast cine CMR is an ancillary examination. For example, regional ischemia can occur in patients with a reduced or normal CFR, and stress-perfusion CMR is important. Recent American Heart Association/American College of Cardiology guidelines also recommend a combination of ischemia and CFR for the evaluation of INOCA and do not recommend using CFR alone for risk stratification. Third, in the present study, data were integrated with and without phase-offset correction. This should be recognized as a limitation because the possibility of a significant impact of phase-offset correction on MBF values cannot be denied. Fourth, it is important to reiterate that CMR-derived CFR is not a microcirculation-specific index but rather a composite index of epicardial and endocardial coronary perfusion. That is, the studies included in this review did not necessarily exclude epicardial coronary artery stenosis by invasive X-ray coronary angiography or coronary computed tomography; therefore, caution must be exercised in interpreting the results. Fifth, several studies used CPT as a stress method, but we integrated only resting status data in the present meta-analysis since CPT exhibits an endothelial function–dependent blood flow-increasing response, creating the need to clearly distinguish it from endothelial function–independent blood flow-increasing responses to other agents (e.g., adenosine, regadenoson, adenosine triphosphate, and dipyridamole).
Conclusions
Phase-contrast cine CMR-derived CFR was significantly decreased in stable CAD and cardiomyopathy, while a decreased CFR was associated with the occurrence of adverse cardiovascular events in patients with stable CAD. These results suggest that CMR-derived CFR has great potential for the pathological evaluation of stable CAD, cardiomyopathy, and risk stratification in CAD.
Availability of data and materials
The datasets analyzed in the current study are available from the corresponding author upon reasonable request.
Abbreviations
- CAD:
-
Coronary artery disease
- CFR:
-
Coronary flow reserve
- CI:
-
Confidence interval
- CMR:
-
Cardiovascular magnetic resonance
- CSF:
-
Coronary sinus flow
- DCM:
-
Dilated cardiomyopathy
- HCM:
-
Hypertrophic cardiomyopathy
- HF:
-
Heart failure
- HR:
-
Hazard ratio
- INOCA:
-
Ischemia with no obstructive coronary artery disease
- LGE:
-
Late gadolinium enhancement
- LV:
-
Left ventricle/left ventricular
- MACE:
-
Major adverse cardiac events
- MBF:
-
Myocardial blood flow
- MD:
-
Mean difference
- MI:
-
Myocardial infarction
- MVD:
-
Microvascular dysfunction
- PET:
-
Positron emission tomography
- VENC:
-
Velocity encoding
References
Del Buono MG, Montone RA, Camilli M, Carbone S, Narula J, Lavie CJ, Niccoli G, Crea F. Coronary microvascular dysfunction across the spectrum of cardiovascular diseases: JACC state-of-the-art review. J Am Coll Cardiol. 2021;78:1352–71.
Pepine CJ, Anderson RD, Sharaf BL, Reis SE, Smith KM, Handberg EM, Johnson BD, Sopko G, Bairey Merz CN. Coronary microvascular reactivity to adenosine predicts adverse outcome in women evaluated for suspected ischemia results from the National Heart, Lung and Blood Institute WISE (Women’s Ischemia Syndrome Evaluation) study. J Am Coll Cardiol. 2010;55:2825–32.
Hage C, Svedlund S, Saraste A, Faxén UL, Benson L, Fermer ML, Gan LM, Shah SJ, Lam CSP, Lund LH. Association of coronary microvascular dysfunction with heart failure hospitalizations and mortality in heart failure with preserved ejection fraction: a follow-up in the PROMIS-HFpEF study. J Card Fail. 2020;26:1016–21.
Radico F, Zimarino M, Fulgenzi F, Ricci F, Di Nicola M, Jespersen L, Chang SM, Humphries KH, Marzilli M, De Caterina R. Determinants of long-term clinical outcomes in patients with angina but without obstructive coronary artery disease: a systematic review and meta-analysis. Eur Heart J. 2018;39:2135–46.
Taqueti VR, Di Carli MF. Coronary microvascular disease pathogenic mechanisms and therapeutic options: JACC state-of-the-art review. J Am Coll Cardiol. 2018;72:2625–41.
Gupta A, Taqueti VR, van de Hoef TP, Bajaj NS, Bravo PE, Murthy VL, Osborne MT, Seidelmann SB, Vita T, Bibbo CF, Harrington M, Hainer J, Rimoldi O, Dorbala S, Bhatt DL, Blankstein R, Camici PG, Di Carli MF. Integrated noninvasive physiological assessment of coronary circulatory function and impact on cardiovascular mortality in patients with stable coronary artery disease. Circulation. 2017;136:2325–36.
Schwitter J, DeMarco T, Kneifel S, von Schulthess GK, Jörg MC, Arheden H, Rühm S, Stumpe K, Buck A, Parmley WW, Lüscher TF, Higgins CB. Magnetic resonance-based assessment of global coronary flow and flow reserve and its relation to left ventricular functional parameters: a comparison with positron emission tomography. Circulation. 2000;101:2696–702.
Deeks JJ, Dinnes J, D’Amico R, Sowden AJ, Sakarovitch C, Song F, Petticrew M, Altman DG. Evaluating non-randomised intervention studies. Health Technol Assess. 2003;7:iii–x, 1–173.
Aquaro GD, Todiere G, Barison A, Strata E, Marzilli M, Pingitore A, Lombardi M. Myocardial blood flow and fibrosis in hypertrophic cardiomyopathy. J Card Fail. 2011;17:384–91.
Aras A, Anik Y, Demirci A, Balci NC, Kozdag G, Ural D, Komsuoglu B. Magnetic resonance imaging measurement of left ventricular blood flow and coronary flow reserve in patients with chronic heart failure due to coronary artery disease. Acta Radiol. 2007;48:1092–100.
Bietenbeck M, Florian A, Shomanova Z, Meier C, Yilmaz A. Reduced global myocardial perfusion reserve in DCM and HCM patients assessed by CMR-based velocity-encoded coronary sinus flow measurements and first-pass perfusion imaging. Clin Res Cardiol. 2018;107:1062–70.
Carlsson M, Jogi J, Bloch KM, Heden B, Ekelund U, Stahlberg F, Arheden H. Submaximal adenosine-induced coronary hyperaemia with 12 h caffeine abstinence: implications for clinical adenosine perfusion imaging tests. Clin Physiol Funct Imaging. 2015;35:49–56.
Cuypers J, Leirgul E, Samnøy S, Larsen TH, Berg A, Schulze-Neick I, Greve G. Assessment of coronary flow reserve in the coronary sinus by cine 3T-magnetic resonance imaging in young adults after surgery for tetralogy of Fallot. Pediatr Cardiol. 2012;33:65–74.
Dandekar VK, Bauml MA, Ertel AW, Dickens C, Gonzalez RC, Farzaneh-Far A. Assessment of global myocardial perfusion reserve using cardiovascular magnetic resonance of coronary sinus flow at 3 Tesla. J Cardiovasc Magn Reson. 2014. https://doi.org/10.1186/1532-429X-16-24.
Drakos S, Chatzantonis G, Bietenbeck M, Evers G, Schulze AB, Mohr M, Fonfara H, Meier C, Yilmaz A. A cardiovascular magnetic resonance imaging-based pilot study to assess coronary microvascular disease in COVID-19 patients. Sci Rep. 2021;11:15667.
Gyllenhammar T, Carlsson M, Jogi J, Arheden H, Engblom H. Myocardial perfusion by CMR coronary sinus flow shows sex differences and lowered perfusion at stress in patients with suspected microvascular angina. Clin Physiol Funct Imaging. 2022;42:208–19.
Gyllenhammar T, Fernlund E, Jablonowski R, Jögi J, Engblom H, Liuba P, Arheden H, Carlsson M. Young patients with hypertrophic cardiomyopathy, but not subjects at risk, show decreased myocardial perfusion reserve quantified with CMR. Eur Heart J Cardiovasc Imaging. 2014;15:1350–7.
Halabi A, Nolan M, Potter E, Wright L, Asham A, Marwick TH. Role of microvascular dysfunction in left ventricular dysfunction in type 2 diabetes mellitus. J Diabetes Complications. 2021;35: 107907.
Hamaya R, Fukuda T, Sugano A, Kanaji Y, Hada M, Kanno Y, Yuki H, Hoshino M, Yonetsu T, Kakuta T. Impact of regional functional ischemia on global coronary flow reserve in patients with stable coronary artery disease. J Cardiol. 2019;73:263–70.
Hamaya R, Sugano A, Kanaji Y, Fukuda T, Kanno Y, Yonetsu T, Usui E, Hoshino M, Hada M, Ohya H, Sumino Y, Yuki H, Murai T, Lee T, Kakuta T. Absolute myocardial blood flow after elective percutaneous coronary intervention evaluated on phase-contrast cine cardiovascular magnetic resonance imaging. Circ J. 2018;82:1858–65.
Ichikawa Y, Kitagawa K, Kato S, Dohi K, Hirano T, Ito M, Sakuma H. Altered coronary endothelial function in young smokers detected by magnetic resonance assessment of myocardial blood flow during the cold pressor test. Int J Cardiovasc Imaging. 2014;30:73–80.
Indorkar R, Kwong RY, Romano S, White BE, Chia RC, Trybula M, Evans K, Shenoy C, Farzaneh-Far A. Global coronary flow reserve measured during stress cardiac magnetic resonance imaging is an independent predictor of adverse cardiovascular events. JACC Cardiovasc Imaging. 2019;12:1686–95.
Kanaji Y, Hirano H, Sugiyama T, Hoshino M, Horie T, Misawa T, Nogami K, Ueno H, Hada M, Yamaguchi M, Sumino Y, Hamaya R, Usui E, Yonetsu T, Sasano T, Kakuta T. Pre-percutaneous coronary intervention pericoronary adipose tissue attenuation evaluated by computed tomography predicts global coronary flow reserve after urgent revascularization in patients with non-ST-segment-elevation acute coronary syndrome. J Am Heart Assoc. 2020;9: e016504.
Kanaji Y, Sugiyama T, Hoshino M, Misawa T, Nagamine T, Yasui Y, Nogami K, Ueno H, Hirano H, Hada M, Yamaguchi M, Hamaya R, Usui E, Yonetsu T, Sasano T, Kakuta T. Physiological significance of pericoronary inflammation in epicardial functional stenosis and global coronary flow reserve. Sci Rep. 2021;11:19026.
Kanaji Y, Sugiyama T, Hoshino M, Yasui Y, Nogami K, Ueno H, Yun T, Nagamine T, Misawa T, Hada M, Yamaguchi M, Hamaya R, Usui E, Murai T, Yonetsu T, Sasano T, Kakuta T. Prognostic value of coronary sinus flow quantification by cardiac magnetic resonance imaging in patients with acute myocardial infarction. J Am Heart Assoc. 2022;11: e023519.
Kanaji Y, Yonetsu T, Hamaya R, Murai T, Usui E, Hoshino M, Yamaguchi M, Hada M, Kanno Y, Fukuda T, Ohya H, Sumino Y, Sugano A, Lee T, Hirao K, Kakuta T. Impact of elective percutaneous coronary intervention on global absolute coronary flow and flow reserve evaluated by phase-contrast cine-magnetic resonance imaging in relation to regional invasive physiological indices. Circ Cardiovasc Interv. 2018;11: e006676.
Kanaji Y, Yonetsu T, Hamaya R, Murai T, Usui E, Hoshino M, Yamaguchi M, Hada M, Kanno Y, Ohya H, Sumino Y, Hirano H, Yuki H, Horie T, Sugano A, Lee T, Hirao K, Kakuta T. Prognostic value of phase-contrast cine-magnetic resonance imaging-derived global coronary flow reserve in patients with non-ST-segment elevation acute coronary syndrome treated with urgent percutaneous coronary intervention. Circ J. 2019;83:1220–8.
Kato S, Fukui K, Kawaguchi J, Ishii N, Koga M, Kusakawa Y, Kusama I, Nakachi T, Nakagawa T, Terauchi Y, Uchino K, Kimura K, Umemura S. Relationship between coronary flow reserve evaluated by phase-contrast cine cardiovascular magnetic resonance and serum eicosapentaenoic acid. J Cardiovasc Magn Reson. 2013;15:106.
Kato S, Fukui K, Kodama S, Azuma M, Iwasawa T, Kimura K, Tamura K, Utsunomiya D. Incremental prognostic value of coronary flow reserve determined by phase-contrast cine cardiovascular magnetic resonance of the coronary sinus in patients with diabetes mellitus. J Cardiovasc Magn Reson. 2020;22:73.
Kato S, Fukui K, Kodama S, Azuma M, Nakayama N, Iwasawa T, Kimura K, Tamura K, Utsunomiya D. Prognostic value of resting coronary sinus flow determined by phase-contrast cine cardiovascular magnetic resonance in patients with known or suspected coronary artery disease. J Cardiovasc Magn Reson. 2021;23:97.
Kato S, Fukui K, Kodama S, Azuma M, Nakayama N, Iwasawa T, Kimura K, Tamura K, Utsunomiya D. Cardiovascular magnetic resonance assessment of coronary flow reserve improves risk stratification in heart failure with preserved ejection fraction. J Cardiovasc Magn Reson. 2021;23:112.
Kato S, Fukui K, Saigusa Y, Kubota K, Kodama S, Asahina N, Hayakawa K, Iguchi K, Fukuoka M, Iwasawa T, Utsunomiya D, Kosuge M, Kimura K, Tamura K. Coronary flow reserve by cardiac magnetic resonance imaging in patients with diabetes mellitus. JACC Cardiovasc Imaging. 2019;12:2579–80.
Kato S, Kitagawa K, Yoon YE, Nakajima H, Nagata M, Takase S, Nakamori S, Ito M, Sakuma H. Detection of diminished response to cold pressor test in smokers: assessment using phase-contrast cine magnetic resonance imaging of the coronary sinus. Magn Reson Imaging. 2014;32:217–23.
Kato S, Saito N, Kirigaya H, Gyotoku D, Iinuma N, Kusakawa Y, Iguchi K, Nakachi T, Fukui K, Futaki M, Iwasawa T, Kimura K, Umemura S. Impairment of coronary flow reserve evaluated by phase contrast cine-magnetic resonance imaging in patients with heart failure with preserved ejection fraction. J Am Heart Assoc. 2016. https://doi.org/10.1161/JAHA.115.002649.
Kato S, Saito N, Nakachi T, Fukui K, Iwasawa T, Taguri M, Kosuge M, Kimura K. Stress perfusion coronary flow reserve versus cardiac magnetic resonance for known or suspected CAD. J Am Coll Cardiol. 2017;70:869–79.
Kawada N, Sakuma H, Yamakado T, Takeda K, Isaka N, Nakano T, Higgins CB. Hypertrophic cardiomyopathy: MR measurement of coronary blood flow and vasodilator flow reserve in patients and healthy subjects. Radiology. 1999;211:129–35.
Kirigaya H, Kato S, Gyotoku D, Yamada N, Iinuma N, Kusakawa Y, Iguchi K, Miki Y, Nakachi T, Fukui K, Iwasawa T, Kimura K. Higher CHADS2 score is associated with impaired coronary flow reserve: a study using phase contrast cine magnetic resonance imaging. Int J Cardiol. 2016;221:800–5.
Koskenvuo JW, Hartiala JJ, Knuuti J, Sakuma H, Toikka JO, Komu M, Saraste M, Niemi P. Assessing coronary sinus blood flow in patients with coronary artery disease: a comparison of phase-contrast MR imaging with positron emission tomography. AJR Am J Roentgenol. 2001;177:1161–6.
Koskenvuo JW, Sakuma H, Niemi P, Toikka JO, Knuuti J, Laine H, Komu M, Kormano M, Saraste M, Hartiala JJ. Global myocardial blood flow and global flow reserve measurements by MRI and PET are comparable. J Magn Reson Imaging. 2001;13:361–6.
Lund GK, Watzinger N, Saeed M, Reddy GP, Yang M, Araoz PA, Curatola D, Bedigian M, Higgins CB. Chronic heart failure: global left ventricular perfusion and coronary flow reserve with velocity-encoded cine MR imaging: initial results. Radiology. 2003;227:209–15.
Maroules CD, Chang AY, Kontak A, Dimitrov I, Kotys M, Peshock RM. Measurement of coronary flow response to cold pressor stress in asymptomatic women with cardiovascular risk factors using spiral velocity-encoded cine MRI at 3 Tesla. Acta Radiol. 2010;51:420–6.
Misawa T, Kanaji Y, Sugiyama T, Hoshino M, Yamaguchi M, Hada M, Nagamine T, Teng Y, Nogami K, Ueno H, Yasui Y, Sayama K, Matsuda K, Yonetsu T, Sasano T, Kakuta T. Effect of percutaneous coronary intervention on global hemodynamics and the prevalence of residual microvascular dysfunction. Microcirculation. 2022;29: e12745.
Moro PJ, Flavian A, Jacquier A, Kober F, Quilici J, Gaborit B, Bonnet JL, Moulin G, Cozzone PJ, Bernard M. Gender differences in response to cold pressor test assessed with velocity-encoded cardiovascular magnetic resonance of the coronary sinus. J Cardiovasc Magn Reson. 2011. https://doi.org/10.1186/1532-429X-13-54.
Nakamori S, Sakuma H, Dohi K, Ishida M, Tanigawa T, Yamada A, Takase S, Nakajima H, Sawai T, Masuda J, Nagata M, Ichikawa Y, Kitagawa K, Fujii E, Yamada N, Ito M. Combined assessment of stress myocardial perfusion cardiovascular magnetic resonance and flow measurement in the coronary sinus improves prediction of functionally significant coronary stenosis determined by fractional flow reserve in multivessel disease. J Am Heart Assoc. 2018;7:e007736.
Sakuma H, Takeda K, Nakagawa T. Assessment of coronary flow reserve using fast phase contrast cine MR imaging. Nihon Rinsho. 1997;55:1833–8.
Shomanova Z, Florian A, Bietenbeck M, Waltenberger J, Sechtem U, Yilmaz A. Diagnostic value of global myocardial perfusion reserve assessment based on coronary sinus flow measurements using cardiovascular magnetic resonance in addition to myocardial stress perfusion imaging. Eur Heart J Cardiovasc Imaging. 2017;18:851–9.
Sugimoto Y, Kato S, Fukui K, Iwasawa T, Utsunomiya D, Kimura K, Tamura K. Impaired coronary flow reserve evaluated by phase-contrast cine magnetic resonance imaging in patients with atrial fibrillations. Heart Vessels. 2021;36:775–81.
Watzinger N, Lund GK, Saeed M, Reddy GP, Araoz PA, Yang M, Schwartz AB, Bedigian M, Higgins CB. Myocardial blood flow in patients with dilated cardiomyopathy: quantitative assessment with velocity-encoded cine magnetic resonance imaging of the coronary sinus. J Magn Reson Imaging. 2005;21:347–53.
Wijesurendra RS, Liu A, Notaristefano F, Ntusi NAB, Karamitsos TD, Bashir Y, Ginks M, Rajappan K, Betts TR, Jerosch-Herold M, Ferreira VM, Neubauer S, Casadei B. Myocardial perfusion is impaired and relates to cardiac dysfunction in patients with atrial fibrillation both before and after successful catheter ablation. J Am Heart Assoc. 2018. https://doi.org/10.1161/JAHA.118.009218.
van Rossum AC, Visser FC, Hofman MB, Galjee MA, Westerhof N, Valk J. Global left ventricular perfusion: noninvasive measurement with cine MR imaging and phase velocity mapping of coronary venous outflow. Radiology. 1992;182:685–91.
Akhtar M, Ordovas K, Martin A, Higgins CB, Michaels AD. Effect of chronic sustained-release dipyridamole on myocardial blood flow and left ventricular function in patients with ischemic cardiomyopathy. Congest Heart Fail. 2007;13:130–5.
Schwitter J, Kozerke S, Bremerich J, Baltes C, AttenhoferJost C, Birkhäuser M, Boesiger P, Buser P. Oral administration of 17beta-estradiol over 3 months without progestin co-administration does not improve coronary flow reserve in post-menopausal women: a randomized placebo-controlled cross-over CMR study. J Cardiovasc Magn Reson. 2007;9:665–72.
Bloch KM, Carlsson M, Arheden H, Ståhlberg F. Quantifying coronary sinus flow and global LV perfusion at 3T. BMC Med Imaging. 2009;9:9.
Gyllenhammar T, Kanski M, Engblom H, Wuttge DM, Carlsson M, Hesselstrand R, Arheden H. Decreased global myocardial perfusion at adenosine stress as a potential new biomarker for microvascular disease in systemic sclerosis: a magnetic resonance study. BMC Cardiovasc Disord. 2018;18:16.
Hair J, Timmins L, El Sayed R, Samady H, Oshinski J. Effect of patient-specific coronary flow reserve values on the accuracy of MRI-based virtual fractional flow reserve. Front Cardiovasc Med. 2021;8: 663767.
Egashira K, Inou T, Hirooka Y, Yamada A, Maruoka Y, Kai H, Sugimachi M, Suzuki S, Takeshita A. Impaired coronary blood flow response to acetylcholine in patients with coronary risk factors and proximal atherosclerotic lesions. J Clin Invest. 1993;91:29–37.
Watson CJ, Gupta SK, O’Connell E, Thum S, Glezeva N, Fendrich J, Gallagher J, Ledwidge M, Grote-Levi L, McDonald K, Thum T. MicroRNA signatures differentiate preserved from reduced ejection fraction heart failure. Eur J Heart Fail. 2015. https://doi.org/10.1002/ejhf.244.
Setoguchi M, Hashimoto Y, Sasaoka T, Ashikaga T, Isobe M. Risk factors for rehospitalization in heart failure with preserved ejection fraction compared with reduced ejection fraction. Heart Vessels. 2014. https://doi.org/10.1007/s00380-014-0532-5.
Yong J, Tian J, Yang X, Xing H, He Y, Song X. Effects of oral drugs on coronary microvascular function in patients without significant stenosis of epicardial coronary arteries: a systematic review and meta-analysis of coronary flow reserve. Front Cardiovasc Med. 2020;7: 580419.
Maron DJ, Hochman JS, Reynolds HR, Bangalore S, O’Brien SM, Boden WE, Chaitman BR, Senior R, López-Sendón J, Alexander KP, Lopes RD, Shaw LJ, Berger JS, Newman JD, Sidhu MS, Goodman SG, Ruzyllo W, Gosselin G, Maggioni AP, White HD, Bhargava B, Min JK, Mancini GBJ, Berman DS, Picard MH, Kwong RY, Ali ZA, Mark DB, Spertus JA, Krishnan MN, Elghamaz A, Moorthy N, Hueb WA, Demkow M, Mavromatis K, Bockeria O, Peteiro J, Miller TD, Szwed H, Doerr R, Keltai M, Selvanayagam JB, Steg PG, Held C, Kohsaka S, Mavromichalis S, Kirby R, Jeffries NO, Harrell FE Jr, Rockhold FW, Broderick S, Ferguson TB Jr, Williams DO, Harrington RA, Stone GW, Rosenberg Y. Initial invasive or conservative strategy for stable coronary disease. N Engl J Med. 2020;382:1395–407.
Acknowledgements
We thank Afshin Farzaneh-Far, MD, Department of Medicine, Duke University School of Medicine, for providing the data.
Funding
Japan Society for the Promotion of Science, Grant-in-Aid for Scientific Research (C).
Author information
Authors and Affiliations
Contributions
TT, SK, and MA analyzed and interpreted the data. TT, SK, NH, MI, and DD contributed significantly to writing the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
IRB approval was not obtained, as this study was a meta-analysis.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Search formulas; Newcastle–Ottawa quality assessment scale case control studies; Representative Imaging parameter for phase-contrast cine MRI of the coronary sinus.
Additional file 2.
Flow measurement of coronary sinus using phase contrast images.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Tanigaki, T., Kato, S., Azuma, M. et al. Coronary flow reserve evaluated by phase-contrast cine cardiovascular magnetic resonance imaging of coronary sinus: a meta-analysis. J Cardiovasc Magn Reson 25, 11 (2023). https://doi.org/10.1186/s12968-023-00912-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12968-023-00912-5