Abstract
Background
Genome-wide association studies (GWAS) have revealed numerous loci associated with stroke. However, the underlying mechanisms at these loci in the pathogenesis of stroke and effective stroke drug targets are elusive. Therefore, we aimed to identify causal genes in the pathogenesis of stroke and its subtypes.
Methods
Utilizing multidimensional high-throughput data generated, we integrated proteome-wide association study (PWAS), transcriptome-wide association study (TWAS), Mendelian randomization (MR), and Bayesian colocalization analysis to prioritize genes that contribute to stroke and its subtypes risk via affecting their expression and protein abundance in brain and blood.
Results
Our integrative analysis revealed that ICA1L was associated with small-vessel stroke (SVS), according to robust evidence at both protein and transcriptional levels based on brain-derived data. We also identified NBEAL1 that was causally related to SVS via its cis-regulated brain expression level. In blood, we identified 5 genes (MMP12, SCARF1, ABO, F11, and CKAP2) that had causal relationships with stroke and stroke subtypes.
Conclusions
Together, via using an integrative analysis to deal with multidimensional data, we prioritized causal genes in the pathogenesis of SVS, which offered hints for future biological and therapeutic studies.
Similar content being viewed by others
Introduction
As the second-leading cause of death globally, stroke contributed to 6.55 million people’s deaths in 2019 with disability-adjusted life years (DALYs) increased steadily [1], which warranted novel therapies for treatment of stroke. Although there are many risk factors that are simultaneously associated with stroke, the causal genes responsible for stroke has remained unexplored. Thus, efforts are still required to identify the key molecular signatures in the pathogenesis of stroke to provide a fundamental theory for treatment.
With the development of high-throughput sequencing technology, genome-wide association studies (GWASs) have identified numerous loci associated with stroke [2]. Despite several efforts, the underlying mechanism attributed to stroke risk is elusive, which hinders the translation from identified risk loci to clinical therapy.
Recently, large-scale quantitative trait loci (QTL) data were produced to establish the association between genotype with protein abundance (pQTL) and gene expression (eQTL) [3, 4], which led to continuous emergent of statistical methods facilitating the integration of the multidimensional data [5]. Proteome-wide association studies (PWASs) have been recently used to find candidate genes whose protein abundances are associated with Alzheimer’s disease and depression [6, 7]. Similarly, transcriptome-wide association studies (TWASs) have been applied in the association analyses between gene expression and phenotypes [8]. Besides, Mendelian randomization (MR) and Bayesian colocalization analysis were also widely used to identify candidate genes via integrating QTL and disease GWAS data [9, 10]. Mendelian randomization, which simulates a natural randomized controlled trial (mutations are randomly assigned to gametes during meiosis), can provide causal inference under the three core assumptions [11, 12]. Bayesian colocalization analysis calculates the probability that two traits share a causal genetic variant [13]. Altogether, integrating GWAS data with these multidimensional QTL data shall help prioritize specific pathways and candidate genes to discriminate the potential genes accounting for the pathogenesis of stroke.
Moreover, a previous study pointed out that mononuclear cells in peripheral could be used as a biomarker in ischemic stroke [14]. Thus, in addition to investigating the directly related brain tissue, we also applied our analysis in blood to reach a more comprehensive understanding of stroke pathogenesis.
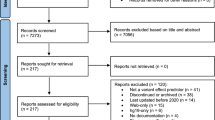
In this study, we conducted an integrative analysis to identify candidate genes for stroke and stroke subtypes by combing brain-derived and blood-derived multi-omics data with genetic data. The overall analysis pipeline is shown in Fig. 1. First, we utilized pQTL and eQTL data derived from brain tissues and GWAS findings of stroke to perform PWAS and TWAS separately. Then, MR, Bayesian colocalization, and Steiger filtering analysis were leveraged to detect the causal relationship between stroke and genomic architecture-associated protein or transcription levels. Second, the integrative analysis was mapped on blood-derived multi-omics data to test the consistency between brain and blood. Our study prioritized candidate genes underlying complex forms of stroke, which could serve as potential treatment targets.
Flowchart of the study. First, we leveraged p/eQTL data derived from the brain tissue with stroke GWASs to conduct a PWAS/TWAS analysis followed by Mendelian randomization (MR), Bayesian colocalization analysis, and Steiger directionality test. Then, we applied similar analysis framework to integrate the proteomic data and eQTL data derived from blood with stroke GWASs. * indicated Bayesian colocalization analysis was only performed for eQTL data
Methods
Stroke GWAS data
The current study utilized stroke GWAS summary datasets obtained from the MEGASTROKE consortium [2]. The stroke GWAS summary datasets used in the main analysis were restricted to European participants, including data for 446,696 European descent individuals (40,585 any stroke cases and 406,111 controls). The ancestry-specific meta-analyses were also conducted for four stroke subtypes, including any ischemic stroke (AIS; 34,217 cases), large artery stroke (LAS; 4,373 cases), cardioembolic stroke (CES; 7,193 cases), and small vessel stroke (SVS; 5,386 cases).
Human brain proteomic and transcriptomic data
We analyzed the proteomes of 400 postmortem brain samples with dorsolateral prefrontal cortex (dPFC) from the ROS/MAP [3]. In more details, the digested peptides were labeled with isobaric tandem mass tag (TMT) and subjected to liquid chromatography coupled to mass spectrometry (LC–MS) for sequencing. Genotypes were derived from either whole-genome sequencing or genome-wide genotyping by either the Illumina OmniQuad Express or Affymetrix GeneChip 6.0 platforms [15]. The quality control process was described in the primary study. Finally, 376 subjects with both proteomic and genetic data passed the quality control for the PWAS.
The eQTL dataset was from the PsychENCODE Consortium covering 1,129,652 eQTLs of 11,120 genes from the prefrontal cortex (PFC) (n = 1387) [4]. We only included the data of SNPs within 1 MB window around each gene. Genotypes were derived either from genome-wide single nucleotide polymorphisms (SNP) arrays or whole genome sequencing.
Human blood proteomic and transcriptomic data
The serum proteomic data was derived from a large population-based study (AGES Reykjavik study; n = 5457) [16]. The AGES Reykjavik study consisting of predominantly European individuals older than 65 years of age, whose phenotype and genotype information were available. The Slow-Off rate Modified Aptamer (SOMAmer), a proteomic profiling platform, was used to determine the serum levels of 4137 human proteins.
The whole-blood eQTL data was derived from the Genotype-Tissue Expression (GTEx) version 6 database (n = 338) [17]. The gene expression data was obtained using paired-end RNA-seq (Illumina TruSeq; Illumina Inc) and the genotype data was from whole-genome sequencing. Full descriptions of donor registration, consent process, biological sample acquisition methods, sample attachment and histopathological examination procedures are available on the official GTEx website [18].
Statistical analysis
Functional Summary-based Imputation (FUSION) software was used to estimate protein weights using proteomic and genetic data from ROS/MAP [8]. Briefly, a linkage disequilibrium (LD) reference panel was used to minimize the influence of LD on the estimated test statistics [8]. Then, the SNP-based heritability for each gene was estimated and we used FUSION to compute the effect of SNPs with significant heritability (P < 0.01) on protein abundance using multiple predictive models, including top1, blup, lasso, enet and bslmm [8]. The weights of protein were obtained from the most predictive model. The protein weights used in the current study were derived from [19] and the expression weights were derived from transcriptomic data generated from dPFC (CommonMind Consortium; n = 452) [20, 21]. Later, we used FUSION to combine the genetic effect of stroke (stroke GWAS z-score) with the protein or expression weights by calculating the linear sum of z-score × weight for the independent SNPs at the locus to perform the PWAS or TWAS. Bonferroni-corrected P value threshold was used to reduce the instance of a false positive. We also calculated the P value adjust for false discovery rate (FDR) using Benjamini-Hochberg (BH) method.
Mendelian randomization [22] used the SNPs as an instrumental variable (IV) to infer the causal relationship between exposure and outcome and the quantitative trait loci data can be integrated to investigate the causal gene of disease [23]. Genome-wide significant (P < 5 × 10–08) SNPs were selected and followed LD clumping to obtain independent SNPs (R2 > 0.001). Then the exposure (QTL data) and outcome (stroke GWAS data) data were harmonized according to the same effect alleles. When only a single independent QTL was available, the Wald ratio was used to estimate the causality of exposure to outcome. Where more than one SNP was available, the inverse-variance weighted (IVW) [24] method was used to combine the ratios of SNP-exposure to SNP-outcome in a fixed-effects meta-analysis or random-effects meta-analysis. A Bonferroni-corrected threshold of P < 0.05/number of genes analyzed was set for multiple comparison. Besides, the Steiger filtering method [25] was employed to test if the causal direction between the hypothesized exposure and outcomes was valid using the directionality_test() function in “TwoSampleMR” package. The Mendelian randomization analysis was performed using the “TwoSampleMR” version 0.5.5 in R version 4.0.
We performed Coloc, a Bayesian test for colocalization, to evaluate the probability of stroke risk loci and p/eQTL shared by a same causal signal [13]. We assigned the default prior probabilities for a SNP being associated with stroke (p1 = 1 × 10−4), a SNP is a significant QTL (p2 = 1 × 10−4) and for a SNP being associated with both traits (p12 = 1 × 10–5) [26]. “coloc.abf” function in coloc R package (version 3.2.1) was used to perform colocalization on the shared SNPs from both the QTL and stroke datasets, and we focused on genes that met the Bonferroni-corrected P value threshold in previous MR analysis. Five mutually exclusive hypotheses was tested: (1) no causal SNP is found for either trait (H0); (2) only trait 1 has a causal SNP (H1); (3) only trait 2 has a causal SNP (H2); (4) both traits have a causal SNP, but the two causal SNPs are different (H3); (5) both traits have a causal SNP, and share the same SNP (H4) [26]. We mainly focused on the last hypothesis H4 and posterior probability (PP) was used to quantify support for H4 (denoted as PPH4). We defined a strong evidence of colocalization at PPH4 ≥ 0.75 [27].
Results
PWAS identified 6 genes associated with stroke
We performed a PWAS of stroke by integrating stroke GWAS results with human brain proteomes using the FUSION pipeline [6]. The PWAS identified 6 genes whose brain protein abundances were associated with stroke (Bonferroni-corrected threshold of P < 0.05/number of genes analyzed) (Fig. 2 and Table 1). The protein abundances of ALDH2 (AS: Z-score: 4.372, P = 1.23 × 10−5; AIS: Z-score: 4.712, P = 2.46×10−6) and SLC44A2 (AS: Z-score: − 4.284, P = 1.84×10−5; AIS: Z-score: − 4.396, P = 1.10 × 10−5) were both associated with AS and AIS, and the protein abundances of PTPN11 (Z-score: − 4.484, P = 7.31 × 10-6) and VPS36 (Z-score: − 4.229, P = 2.35 × 10−5) were also associated with AIS (Additional file 1: Table S1 and S2). However, no significant association was found for LAS (Additional file 1: Table S3). For CES and SVS, the protein abundances of L3HYPDH (CES: Z-score: − 4.153, P = 3.28 × 10−5) and ICA1L (SVS: Z-score: − 4.426, P = 9.60 × 10−6) were associated with them respectively (Additional file 1: Table S4 and S5).
The Manhattan plot for the PWAS of stroke and stroke subtypes. The Manhattan plot shows the genes identified using PWAS for AS, AIS, LAS, CES, and SVS, respectively. The red line indicates the significant threshold for Bonferroni correction (P < 0.05/1468). The orange dash line indicates the nominal significance level (P < 0.05)
TWAS identified 7 genes associated with stroke
We then performed TWAS of stroke to provide insight into transcription level using data generated from dPFC (CommonMind Consortium; n = 452) [20]. There were 7 genes whose expression in brain were associated with stroke in TWAS (P < 0.05/number of genes analyzed) (Fig. 3 and Table 2). TWAS identified ATXN2 (AS: Z-score: 4.805, P = 1.55×10−6; AIS: Z-score: 5.137, P = 2.79×10−7) and CDK6 (AS: Z-score: − 4.638, P = 3.52 × 10−6; AIS: Z-score: − 4.463, P = 8.08 × 10−6) whose cis-regulated brain mRNA expression was both associated with AS and AIS, and the expression of NBEAL1 (Z-score: 4.646, P = 3.38 × 10−6) was also associated with AIS (Additional file 1: Table S6 and S7). No significant association was found for LAS (Additional file 1: Table S8). As for CES, only SENP6 (Z-score: − 4.751, P = 2.03 × 10-6) and CAV1 (Z-score: − 4.582, P = 4.62 × 10−6) passed the Bonferroni correction (Additional file 1: Table S9). In the analysis for SVS, NBEAL1 (Z-score: 5.286, P = 1.25 × 10−7), ICA1L (Z-score: 5.109, P = 3.24 × 10−7) and ALS2CR8 (Z-score: 5.009, P = 5.47 × 10−7) showed evidence for association at the mRNA level (Additional file 1: Table S10). Interestingly, ICA1L was also significant in the SVS PWAS, suggesting that ICA1L regulates brain protein abundance via the regulation of brain mRNA expression.
The Manhattan plot for the TWAS of stroke and stroke subtypes. The Manhattan plot shows the genes identified using TWAS for AS, AIS, LAS, CES, and SVS, respectively. The red line indicates the significant threshold for Bonferroni correction (P < 0.05/5371). The orange dash line indicates the nominal significance level (P < 0.05)
ICA1L was causally associated with SVS using MR in brain
MR analysis of brain pQTL and stroke GWAS identified 2 protein biomarkers that provided strong evidence of associations [P < 8.224 × 10–5 (0.05/608)] (Table 3). Genetically predicted higher ALDH2 was associated with higher AS and AIS risk (AS: OR [95% CI] 1.89 [1.41, 2.54]; AIS: OR [95% CI] 2.11 [1.53, 2.91]) and both of them were replicated in PWAS (Additional file 1: Table S11 and 12). However, no evidence was found between protein biomarkers and LAS or CES (Additional file 1: Table S13 and S14). As for SVS, the association between lower ICA1L and higher SVS risk was identified (OR [95% CI] 0.08 [0.03, 0.25]), which was also replicated in PWAS (Additional file 1: Table S15). Steiger filtering showed direct causal associations from changes of ALDH2 to development of AS and AIS (AS: Steiger P Value: 8.78 × 10–14; AIS: Steiger P Value: 9.43 × 10–14) and ICA1L to SVS (Steiger P Value: 1.22 × 10–13) (Table 3).
To figure out whether genes with evidence for being causal in stroke at the protein level were also relevant to stroke at the transcriptional level, we conducted MR analysis using brain eQTL data (Table 3). HDAC9 gene displayed robust causal evidence with AS, AIS, and LAS in the MR (AS: OR [95% CI] 1.29 [1.19, 1.39]; AIS: OR [95% CI] 1.32 [1.21, 1.44]; LAS: OR [95% CI] 2.13 [1.73, 2.63]) (Additional file 1: Table S16, 17 and S18). Nevertheless, no association was found between the expression level and CES (Additional file 1: Table S19). Notably, 4 genes were associated with SVS, of which ICA1L and NBEAL1 were also replicated in TWAS (Additional file 1: Table S20). All genes identified in the MR analysis passed Steiger filtering analysis (Table 3).
Colocalization between stroke risk genes and p/eQTL in brain
We examined the posterior probability for a shared causal variant between a pQTL and stroke for the genes which met the Bonferroni-corrected P value threshold in previous MR analysis. However, only ICA1L met the criterion (PPH4 > 75%) in the analysis of SVS, indicating a shared single variant with SVS (Table 3). At transcriptional level, the colocalization analysis identified all the 6 genes which provided evidence of colocalization (PPH4 > 75%) (Table 3).
Five genes were causally associated with stroke in blood
We investigated whether the genes associated with stroke in brain could be expressed through blood data. Applying MR to serum proteomic data, 4 genes with 8 significant causal associations with stroke survived from corrections for multiple testing methods and passed the Steiger filtering analysis (Additional file 1: Table S21). Of these, the concentration of MMP12 was inversely associated with AS, AIS, and LAS risk (AS: OR [95% CI]: 0.90 [0.87, 0.94]; AIS: OR [95% CI]: 0.89 [0.85, 0.93]; LAS: OR [95% CI]: 0.78 [0.70, 0.86]), while ABO was positively associated with AIS, LAS, and CES risk (AIS: OR [95% CI]: 1.03 [1.02, 1.05]; LAS: OR [95% CI] 1.09 [1.05, 1.13]; CES: OR [95% CI] 1.07 [1.04, 1.10]) (Additional file 1: Table S22–S25). As for SVS, results showed no gene survived corrections for multiple testing (Additional file 1: Table S26). We next repeated MR analysis using the whole-blood eQTL data. However, only CKAP2 displayed robust evidence with AIS in MR (Additional file 1: Table S27–3S1). It should be noted that those genes identified in blood were different from the genes identified in brains, indicating a distinct pathogenic mechanism in blood.
Summary findings
Using PWAS, TWAS, MR and Bayesian colocalization analyses, ICA1L and NBEAL1 were proved to be causal for stroke in brains (Fig. 4). Although there was evidence that ALDH2 was associated with stroke in PWAS and MR, they did not reach the Bayesian colocalization’s criterion. Comparative analyses illustrated that there was no overlap between genes identified in brains and those in blood.
The Venn plots of the significant genes among four approaches for stroke and stroke subtypes. Brain pQTL and brain eQTL indicate the MR analysis using brain pQTL and brain eQTL data respectively. The red dots implicate where the significant associations are found for each gene among AS, AIS, LAS, CES, and SVS
Discussion
We conducted an integrative analysis of PWAS, TWAS, MR and Bayesian colocalization to identify causal genes for stroke and stroke subtypes using brain- and blood-derived data. Collectively, 16 genes were identified in brains, of which ICA1L showed causal for SVS at both protein and transcriptional level, while NBEAL1 showed causal for SVS at transcriptional level only. Furthermore, 5 different genes (MMP12, ABO, SCARF1, F11, and CKAP2) were discovered in blood, which indicated two distinct pathogenesis for stroke in brain and blood.
Of the identified genes, ICA1L was previously discovered in a GWAS of cerebral small vessel disease [28] and its genetically elevated expression was associated with lacunar stroke in TWAS [29]. Employing a larger population of stroke in our pipeline, the results further verified the important role of ICA1L in SVS. ICA1L and its major binding partner PICK1 involved in cellular functions required dynamic remodeling of the actin cytoskeleton [30, 31], suggesting a potential role of actin cytoskeleton in the pathogenesis of SVS. However, it is worth noting that there was a diverse direction for ICA1L at protein and transcriptional level, and the expression in specific tissue may partly explain it. ICA1L mainly expresses in brain and testis tissues and its active participation in spermiogenesis has been identified [30]. Since stroke shows a marked sex bias with men having greater incidence of stroke [32], potential differential expression of ICA1L between male and female may account for this divarication.
By integrative analysis of TWAS, MR and colocalization analysis using brain-derived data, we prioritized another gene (NBEAL1), which showed evidence of being associated with SVS. Neurobeachin-like 1 protein, encoded by NBEAL1, is one of the nine proteins that share a highly conserved domain known as the BEACH (Beige and Chediak-Higashi) domain [33]. NBEAL1 have been detected previously in a GWAS of cerebral small vessel disease [28] and was found to affect cellular cholesterol metabolism and LDL uptake and was associated with coronary artery diseases [33], indicating that NBEAL1 may influence the risk of stroke by LDL. Furthermore, a recent study also connected NBEAL1 with white matter hyperintensity volumes [34]. And the highest lesion burden was found in patients with small artery occlusion [35], which pointed out the close relationship between NBEAL1 and SVS. However, the biological functions of NBEAL1 in the pathogenesis of SVS is still elusive and need further investigations. Recalling the genes identified in each method, only a small part of genes was replicated in other approaches and this might be due to several reasons. Apart from the differences in statistical processing and measurement errors, the relationship between mRNAs and proteins could also be affected by difference in translation efficiency, protein degeneration, contextual confounds and protein-level buffering [36]. Furthermore, the sample sizes and number of genes analyzed in the transcriptome and proteome data varied considerably. Although the rest of 16 causal genes identified by the integrative analysis were only replicated in one or two analyses, some of them (e.g. ALDH2, CDK6, HDAC9, and SLC44A2) were previously reported linked to stroke, which also demonstrate the reliability of our integrative analysis in a way. ALDH2, which is associated with a poorer functional outcome of ischemic stroke [37] and increases the risk and susceptibility to hypertension or diabetes [38], has been found to protect against stroke by clearing the toxic aldehydes, for example, 4-hydroxy-2-nonenal (4-HNE) [39]. However, in the Bayesian colocalization analysis, there was insufficient evidence to show the abundance of ALDH2 and stroke shared common causal variants (PPH4 < 75%). The causal relationship between ALDH2 and stroke still need further study. CDK6 has been identified as a key regulator of atherosclerosis for CDK6 knockdown can suppress proliferation of HASMC and HUASMC [40]. A previous study has also shown the down-regulation of CDK6 in the penumbra surrounding the infarction region comparing with control [41], which supports the inverse association between expression of CDK6 and the risk of AS and AIS in our TWAS analysis. In MR analysis, we found a causal relationship between an increased expression of HDAC9 and the higher risk of AS, AIS, and LAS. HDAC9, whose enhanced expression is associated with increasing calcification and decreasing contractility in human aortic vascular smooth muscle cells [42], has also been identified in a GWAS for large vessel stroke [43]. Likewise, the SLC44A2 rs2288904-A polymorphism showed protective effect in venous thrombosis [44], implicating its potential role in stroke by modulating thrombosis. Collectively, although there is relatively insufficient evidence for the associations of these genes with stroke in our integrative analysis, some of them have been reported to play an important role in the pathogenesis of stroke, which deserves further replication in population with larger sample size.
Using blood as a surrogate has been widely found to establish associations with brain-related traits. And a previous study has found that there were strong correlations between brain and blood (rb ≥ 0.7) from cis-eQTL or mQTL data [45]. In our MR analysis between levels of blood proteomes and stroke risk, we found 4 genes (MMP12, SCARF1, ABO, and F11), of which MMP12, ABO, and F11 were replicated, compared with a previous study that analyzed the association of circulating biomarker levels with stroke and stroke subtypes using a different study sample [46]. These candidate genes identified in blood are different from those discovered in brains. Similarly, in a recently published research, MR was used to analyzed the causal effect of pQTL data derived from CSF, plasma, and brain with seven neurological traits [19]. However, there was no overlap between results in plasma and brain for stroke after multiple testing correction [19]. The biological mechanisms of these genes with stroke pathogenesis reported already can partly explain this difference. ApoE/MMP-12 double knockouts mice showed reduced and more stable plaques in the brachiocephalic artery [47], indicating that MMP12 might participate in the stability of plaques [48]. A previous study reported an increased risk of thrombosis with the non-O blood groups (A, B or AB) [49], and this effect was hypothesized to affect von Willebrand Factor (vWF) clearance [50]. Similarly, genetic variation in F11 was also associated with both deep vein thrombosis and the level of coagulation factor XI [51]. Taken together, these genes identified in MR from blood proteomes mainly focus on coagulation and atherosclerosis, which finally cause stroke. Besides, given that different tissues have different expression profiles, the differences among methods of tissue collection, extraction and analysis further lead to only a small overlap of genes derived from brains and blood.
In general, our study has a key advantage-we integrated multidimensional QTL data to provide comprehensive insights into complex biological systems of stroke from both brains and blood. Comparatively, using single method or single dimensional data (e.g. TWAS and MR) to identify stroke candidate genes has some limitations. First, methodologically, the accuracy of TWAS relied on training cohort size and the quality of the training data [8]. As for MR, the power of MR depended on the proportion of total variance of the exposure explained by the genetic variants and the strength of the causal association between exposure and outcome [52]. Second, dimensionally, only using single dimensional data (protein or transcriptional level) to identify the underlying genes for stroke pathogenesis is insufficient, leading to false positive results. Therefore, our integrative analyses bring data from genome, transcriptome, and proteome together through multi approaches, and contribute to identifying the key causal genes in the pathogenesis of stroke. Besides, two genes (SLC25A44 and LRCH1), whose expression were significantly associated with stroke after Bonferroni correction, were identified as candidate genes in a recent TWAS in adipose [53]. These genes were not discovered in our integrative analysis, indicating a tissue-specific expressional pattern. Using the directly related brain tissue, our analysis could prioritize candidate genes more relevant with stroke.
There are also some limitations in our study. First, the genes tested in PWAS were relatively smaller than those tested in TWAS, resulting in fewer genes identified in the two analyses. And this can be addressed by using a larger brain sample dataset. Second, gene expression is a highly complicated process, varying in time and space. Our study only investigated the candidate genes in brains and blood, future work may focus on other tissues. Third, we only performed the analysis in one dataset for each stroke subtype, which needs further validation using larger stroke GWAS datasets. Nevertheless, it is worth noting that some genes were replicated in analyses for several stroke subtypes, which validated their potential role to some degree. Fourth, it is insufficient to elucidate the numerous stroke GWAS-identified loci from protein and transcriptional level. Methylation data can be integrated into the analysis to reach a more comprehensive understanding of disease progression. Fifth, our study mainly focused on European subjects, and it should be careful to extend our results to other ethnicities. In addition, functional genomic approaches and biological experiments are necessary to understand the complex biology of stroke and illustrate the molecular mechanisms behind.
In conclusion, this integrative analysis identified ICA1L and NBEAL1, whose expression and protein abundances are associated with the risk of small-vessel stroke. Our study offered hints for future biological and therapeutic studies to identify their potential roles in stroke pathogenesis.
Data availability
The data of brain pQTL from the Religious Orders Study/Memory and Aging Project (ROS/MAP) study is available through https://doi.org/10.7303/syn23627957. Above data from ROS/MAP is available for general research use according to the following requirements for data access and data attribution (https://adknowledgeportal.org/DataAccess/Instructions). The data of brain eQTL from the PsychENCODE Consortium are accessible in BESD format through https://cnsgenomics.com/software/smr/#eQTLsummarydata. The data from AGES Reykjavik study is available from www.sciencemag.org/cgi/content/full/science.aaq1327/DC1. The data from the AGES Reykjavik study was acquired through collaboration (AGES_data_request@hjarta.is) under a data usage agreement with the IHA. GTEx can be accessed at https://gtexportal.org/home/datasets (GTEx Analysis V6). The GWAS datasets of the stroke analyzed during the current study are available from https://www.megastroke.org/.
Abbreviations
- 4-HNE:
-
4-Hydroxy-2-nonenal
- AIS:
-
Any ischemic stroke
- BH:
-
Benjamini-Hochberg
- CES:
-
Cardioembolic stroke
- dPFC:
-
Dorsolateral prefrontal cortex
- DALYs:
-
Disability-adjusted life years
- FUSION:
-
Functional Summary-based Imputation
- FDR:
-
False discovery rate
- GTEx:
-
Genotype-Tissue Expression
- GWASs:
-
Genome-wide association studies
- IVW:
-
Inverse-variance weighted
- LAS:
-
Large artery stroke
- LD:
-
Linkage disequilibrium
- MR:
-
Mendelian randomization
- MS:
-
Mass spectrometry
- PFC:
-
Prefrontal cortex
- PP:
-
Posterior probability
- PWASs:
-
Proteome-wide association studies
- QTL:
-
Quantitative trait loci
- ROS/MAP:
-
Religious Orders Study/Memory and Aging Project
- SNP:
-
Single nucleotide polymorphisms
- SOMAmer:
-
Slow-Off rate Modified Aptamer
- SVS:
-
Small vessel stroke
- TMT:
-
Tandem mass tag
- TWASs:
-
Transcriptome-wide association studies
- vWF:
-
Von Willebrand Factor
References
Roth GA, Mensah GA, Johnson CO, Addolorato G, Ammirati E, Baddour LM, Barengo NC, Beaton AZ, Benjamin EJ, Benziger CP, et al. Global burden of cardiovascular diseases and risk factors, 1990–2019: update from the GBD 2019 Study. J Am Coll Cardiol. 2020;76:2982–3021.
Malik R, Chauhan G, Traylor M, Sargurupremraj M, Okada Y, Mishra A, Rutten-Jacobs L, Giese AK, van der Laan SW, Gretarsdottir S, et al. Multiancestry genome-wide association study of 520,000 subjects identifies 32 loci associated with stroke and stroke subtypes. Nat Genet. 2018;50:524–37.
Wang M, Beckmann ND, Roussos P, Wang E, Zhou X, Wang Q, Ming C, Neff R, Ma W, Fullard JF, et al. The Mount Sinai cohort of large-scale genomic, transcriptomic and proteomic data in Alzheimer’s disease. Sci Data. 2018;5:180185.
Akbarian S, Liu C, Knowles JA, Vaccarino FM, Farnham PJ, Crawford GE, Jaffe AE, Pinto D, Dracheva S, Geschwind DH, et al. The PsychENCODE project. Nat Neurosci. 2015;18:1707–12.
Montaner J, Ramiro L, Simats A, Tiedt S, Makris K, Jickling GC, Debette S, Sanchez JC, Bustamante A. Multilevel omics for the discovery of biomarkers and therapeutic targets for stroke. Nat Rev Neurol. 2020;16:247–64.
Wingo AP, Liu Y, Gerasimov ES, Gockley J, Logsdon BA, Duong DM, Dammer EB, Robins C, Beach TG, Reiman EM, et al. Integrating human brain proteomes with genome-wide association data implicates new proteins in Alzheimer’s disease pathogenesis. Nat Genet. 2021;53:143–6.
Wingo TS, Liu Y, Gerasimov ES, Gockley J, Logsdon BA, Duong DM, Dammer EB, Lori A, Kim PJ, Ressler KJ, et al. Brain proteome-wide association study implicates novel proteins in depression pathogenesis. Nat Neurosci. 2021;24:810–7.
Gusev A, Ko A, Shi H, Bhatia G, Chung W, Penninx BW, Jansen R, de Geus EJ, Boomsma DI, Wright FA, et al. Integrative approaches for large-scale transcriptome-wide association studies. Nat Genet. 2016;48:245–52.
Baird DA, Liu JZ, Zheng J, Sieberts SK, Perumal T, Elsworth B, Richardson TG, Chen CY, Carrasquillo MM, Allen M, et al. Identifying drug targets for neurological and psychiatric disease via genetics and the brain transcriptome. PLoS Genet. 2021;17:e1009224.
Li M, Lyu C, Huang M, Do C, Tycko B, Lupo PJ, MacLeod SL, Randolph CE, Liu N, Witte JS, Hobbs CA. Mapping methylation quantitative trait loci in cardiac tissues nominates risk loci and biological pathways in congenital heart disease. BMC Genom Data. 2021;22:20.
Hemani G, Zheng J, Elsworth B, Wade KH, Haberland V, Baird D, Laurin C, Burgess S, Bowden J, Langdon R, et al. The MR-Base platform supports systematic causal inference across the human phenome. Elife. 2018;7:e34408.
Lawlor DA, Harbord RM, Sterne JA, Timpson N, Davey Smith G. Mendelian randomization: using genes as instruments for making causal inferences in epidemiology. Stat Med. 2008;27:1133–63.
Giambartolomei C, Vukcevic D, Schadt EE, Franke L, Hingorani AD, Wallace C, Plagnol V. Bayesian test for colocalisation between pairs of genetic association studies using summary statistics. PLoS Genet. 2014;10:e1004383.
Moore DF, Li H, Jeffries N, Wright V, Cooper RA Jr, Elkahloun A, Gelderman MP, Zudaire E, Blevins G, Yu H, et al. Using peripheral blood mononuclear cells to determine a gene expression profile of acute ischemic stroke: a pilot investigation. Circulation. 2005;111:212–21.
De Jager PL, Ma Y, McCabe C, Xu J, Vardarajan BN, Felsky D, Klein HU, White CC, Peters MA, Lodgson B, et al. A multi-omic atlas of the human frontal cortex for aging and Alzheimer’s disease research. Sci Data. 2018;5:180142.
Emilsson V, Ilkov M, Lamb JR, Finkel N, Gudmundsson EF, Pitts R, Hoover H, Gudmundsdottir V, Horman SR, Aspelund T, et al. Co-regulatory networks of human serum proteins link genetics to disease. Science. 2018;361:769–73.
Yang J, Yu X, Zhu G, Wang R, Lou S, Zhu W, Fu C, Liu J, Fan L, Li D, et al. Integrating GWAS and eQTL to predict genes and pathways for non-syndromic cleft lip with or without palate. Oral Dis. 2020;27(7):1747–54.
GTEx. https://wwwww.gtexportal.org. Accessed 24 Aug 2021.
Yang C, Farias FHG, Ibanez L, Suhy A, Sadler B, Fernandez MV, Wang F, Bradley JL, Eiffert B, Bahena JA, et al. Genomic atlas of the proteome from brain, CSF and plasma prioritizes proteins implicated in neurological disorders. Nat Neurosci. 2021;24:1302–12.
Fromer M, Roussos P, Sieberts SK, Johnson JS, Kavanagh DH, Perumal TM, Ruderfer DM, Oh EC, Topol A, Shah HR, et al. Gene expression elucidates functional impact of polygenic risk for schizophrenia. Nat Neurosci. 2016;19:1442–53.
Expression weights. http://gusevlab.org/projects/fusion/. Accessed 25 Aug 2021.
Davey Smith G, Hemani G. Mendelian randomization: genetic anchors for causal inference in epidemiological studies. Hum Mol Genet. 2014;23:R89-98.
Porcu E, Rüeger S, Lepik K, Santoni FA, Reymond A, Kutalik Z. Mendelian randomization integrating GWAS and eQTL data reveals genetic determinants of complex and clinical traits. Nat Commun. 2019;10:3300.
Burgess S, Butterworth A, Thompson SG. Mendelian randomization analysis with multiple genetic variants using summarized data. Genet Epidemiol. 2013;37:658–65.
Hemani G, Tilling K, Davey Smith G. Orienting the causal relationship between imprecisely measured traits using GWAS summary data. PLoS Genet. 2017;13:e1007081.
Burgess S, Davey Smith G, Davies NM, Dudbridge F, Gill D, Glymour MM, Hartwig FP, Holmes MV, Minelli C, Relton CL, Theodoratou E. Guidelines for performing Mendelian randomization investigations. Wellcome Open Res. 2019;4:186.
Kia DA, Zhang D, Guelfi S, Manzoni C, Hubbard L, Reynolds RH, Botía J, Ryten M, Ferrari R, Lewis PA, et al. Identification of candidate parkinson disease genes by integrating genome-wide association study, expression, and epigenetic data sets. JAMA Neurol. 2021;78:464–72.
Chung J, Marini S, Pera J, Norrving B, Jimenez-Conde J, Roquer J, Fernandez-Cadenas I, Tirschwell DL, Selim M, Brown DL, et al. Genome-wide association study of cerebral small vessel disease reveals established and novel loci. Brain. 2019;142:3176–89.
Traylor M, Persyn E, Tomppo L, Klasson S, Abedi V, Bakker MK, Torres N, Li L, Bell S, Rutten-Jacobs L, et al. Genetic basis of lacunar stroke: a pooled analysis of individual patient data and genome-wide association studies. Lancet Neurol. 2021;20:351–61.
He J, Xia M, Tsang WH, Chow KL, Xia J. ICA1L forms BAR-domain complexes with PICK1 and is crucial for acrosome formation in spermiogenesis. J Cell Sci. 2015;128:3822–36.
Carman PJ, Dominguez R. BAR domain proteins-a linkage between cellular membranes, signaling pathways, and the actin cytoskeleton. Biophys Rev. 2018;10:1587–604.
Zuo W, Zhang W, Chen NH. Sexual dimorphism in cerebral ischemia injury. Eur J Pharmacol. 2013;711:73–9.
Bindesboll C, Aas A, Ogmundsdottir MH, Pankiv S, Reine T, Zoncu R, Simonsen A. NBEAL1 controls SREBP2 processing and cholesterol metabolism and is a susceptibility locus for coronary artery disease. Sci Rep. 2020;10:4528.
Traylor M, Zhang CR, Adib-Samii P, Devan WJ, Parsons OE, Lanfranconi S, Gregory S, Cloonan L, Falcone GJ, Radmanesh F, et al. Genome-wide meta-analysis of cerebral white matter hyperintensities in patients with stroke. Neurology. 2016;86:146–53.
Giese AK, Schirmer MD, Dalca AV, Sridharan R, Donahue KL, Nardin M, Irie R, McIntosh EC, Mocking SJT, Xu H, et al. White matter hyperintensity burden in acute stroke patients differs by ischemic stroke subtype. Neurology. 2020;95:e79–88.
Buccitelli C, Selbach M. mRNAs, proteins and the emerging principles of gene expression control. Nat Rev Genet. 2020;21:630–44.
Cheng X, Xu J, Gu M, Wang M, Sun B, Li Z, Ni G, Wang G, Weng Z, Shi Y, et al. Genetic variants in ALDH2 predict risk of ischemic stroke in a Chinese population. Gene. 2018;678:49–54.
Chauhan G, Debette S. Genetic risk factors for ischemic and hemorrhagic stroke. Curr Cardiol Rep. 2016;18:124.
Guo JM, Liu AJ, Zang P, Dong WZ, Ying L, Wang W, Xu P, Song XR, Cai J, Zhang SQ, et al. ALDH2 protects against stroke by clearing 4-HNE. Cell Res. 2013;23:915–30.
Kang L, Jia H, Huang B, Lu S, Chen Z, Shen J, Zou Y, Wang C, Sun Y. Identification of differently expressed mrnas in atherosclerosis reveals CDK6 is regulated by circHIPK3/miR-637 axis and promotes cell growth in human vascular smooth muscle cells. Front Genet. 2021;12:596169.
Demyanenko S, Uzdensky A. Profiling of signaling proteins in penumbra after focal photothrombotic infarct in the rat brain cortex. Mol Neurobiol. 2017;54:6839–56.
Malhotra R, Mauer AC, Lino Cardenas CL, Guo X, Yao J, Zhang X, Wunderer F, Smith AV, Wong Q, Pechlivanis S, et al. HDAC9 is implicated in atherosclerotic aortic calcification and affects vascular smooth muscle cell phenotype. Nat Genet. 2019;51:1580–7.
Bellenguez C, Bevan S, Gschwendtner A, Spencer CC, Burgess AI, Pirinen M, Jackson CA, Traylor M, Strange A, Su Z, et al. Genome-wide association study identifies a variant in HDAC9 associated with large vessel ischemic stroke. Nat Genet. 2012;44:328–33.
Constantinescu-Bercu A, Grassi L, Frontini M, Salles C II, Woollard K, Crawley JT. Activated alphaIIbbeta3 on platelets mediates flow-dependent NETosis via SLC44A2. Elife. 2020;9:e53353.
Qi T, Wu Y, Zeng J, Zhang F, Xue A, Jiang L, Zhu Z, Kemper K, Yengo L, Zheng Z, et al. Identifying gene targets for brain-related traits using transcriptomic and methylomic data from blood. Nat Commun. 2018;9:2282.
Chong M, Sjaarda J, Pigeyre M, Mohammadi-Shemirani P, Lali R, Shoamanesh A, Gerstein HC, Paré G. Novel drug targets for ischemic stroke identified through mendelian randomization analysis of the blood proteome. Circulation. 2019;140:819–30.
Johnson JL, George SJ, Newby AC, Jackson CL. Divergent effects of matrix metalloproteinases 3, 7, 9, and 12 on atherosclerotic plaque stability in mouse brachiocephalic arteries. Proc Natl Acad Sci USA. 2005;102:15575–80.
Traylor M, Makela KM, Kilarski LL, Holliday EG, Devan WJ, Nalls MA, Wiggins KL, Zhao W, Cheng YC, Achterberg S, et al. A novel MMP12 locus is associated with large artery atherosclerotic stroke using a genome-wide age-at-onset informed approach. PLoS Genet. 2014;10:e1004469.
Sabino Ade P, Ribeiro DD, Domingheti CP, Rios DR, Dusse LM, Carvalho M, Fernandes AP. ABO blood group polymorphisms and risk for ischemic stroke and peripheral arterial disease. Mol Biol Rep. 2014;41:1771–7.
Jenkins PV, O’Donnell JS. ABO blood group determines plasma von Willebrand factor levels: a biologic function after all? Transfusion. 2006;46:1836–44.
Bezemer ID, Bare LA, Doggen CJ, Arellano AR, Tong C, Rowland CM, Catanese J, Young BA, Reitsma PH, Devlin JJ, Rosendaal FR. Gene variants associated with deep vein thrombosis. JAMA. 2008;299:1306–14.
Sekula P, Del Greco MF, Pattaro C, Köttgen A. Mendelian randomization as an approach to assess causality using observational data. J Am Soc Nephrol. 2016;27:3253–65.
Yang J, Yan B, Fan Y, Yang L, Zhao B, He X, Ma Q, Wang W, Bai L, Zhang F, Ma X. Integrative analysis of transcriptome-wide association study and gene expression profiling identifies candidate genes associated with stroke. PeerJ. 2019;7:e7435.
Acknowledgements
We appreciated the generous sharing of GWAS summary statistics from the MEGASTROKE consortium. We thank the ROS and MAP, the PsychENCODE Consortium, the AGES Reykjavik study, and the GTEx project for their kind dedication. The MEGASTROKE project received funding from sources specified at http://www.megastroke.org/acknowledgments.html. The author list of MEGASTROKE is available in Additional file 1: Table 32.
Funding
This study was supported by grants from the National Natural Science Foundation of China (91849126), Shanghai Municipal Science and Technology Major Project (No. 2018SHZDZX01) and ZHANGJIANG LAB, Tianqiao and Chrissy Chen Institute, and the State Key Laboratory of Neurobiology and Frontiers Center for Brain Science of Ministry of Education, Fudan University.
Author information
Authors and Affiliations
Contributions
BSW collected and organized data, carried out the statistical analysis and prepared the first draft of the manuscript. SFC, SYH, YNO, YTD and SDC collected and organized data and participated in the writing of the manuscript. QD and JTY participated in the study design, reviewing and editing the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The data analyzed during the current study come from the studies where written informed consent was received prior to participation.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:
Supplementary Tables 1–32.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Wu, BS., Chen, SF., Huang, SY. et al. Identifying causal genes for stroke via integrating the proteome and transcriptome from brain and blood. J Transl Med 20, 181 (2022). https://doi.org/10.1186/s12967-022-03377-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12967-022-03377-9