Abstract
Background
Genetically engineered chimeric antigen receptor (CAR) T lymphocytes are promising therapeutic tools for cancer. Four CAR T cell drugs, including tisagenlecleucel (tisa-cel) and axicabtagene-ciloleucel (axi-cel), all targeting CD19, are currently approved for treating B cell malignancies. Flow cytometry (FC) remains the standard for monitoring CAR T cells using a recombinant biotinylated target protein. Nevertheless, there is a need for additional tools, and the challenge is to develop an easy, relevant, highly sensitive, reproducible, and inexpensive detection method. Molecular tools can meet this need to specifically monitor long-term persistent CAR T cells.
Methods
Based on 2 experimental CAR T cell constructs, IL-1RAP and CS1, we designed 2 quantitative digital droplet (ddPCR) PCR assays. By targeting the 4.1BB/CD3z (28BBz) or 28/CD3z (28z) junction area, we demonstrated that PCR assays can be applied to approved CD19 CAR T drugs. Both 28z and 28BBz ddPCR assays allow determination of the average vector copy number (VCN) per cell. We confirmed that the VCN is dependent on the multiplicity of infection and verified that the VCN of our experimental or GMP-like IL-1RAP CAR T cells met the requirement (< 5 VCN/cell) for delivery to the clinical department, similar to approved axi-cel or tisa-cel drugs.
Results
28BBz and 28z ddPCR assays applied to 2 tumoral (acute myeloid leukemia (AML) or multiple myeloma (MM) xenograft humanized NSG mouse models allowed us to quantify the early expansion (up to day 30) of CAR T cells after injection. Interestingly, following initial expansion, when circulating CAR T cells were challenged with the tumor, we noted a second expansion phase. Investigation of the bone marrow, spleen and lung showed that CAR T cells disseminated more within these tissues in mice previously injected with leukemic cell lines. Finally, circulating CAR T cell ddPCR monitoring of R/R acute lymphoid leukemia or diffuse large B cell lymphoma (n = 10 for tisa-cel and n = 7 for axi-cel) patients treated with both approved CAR T cells allowed detection of early expansion, which was highly correlated with FC, as well as long-term persistence (up to 450 days), while FC failed to detect these events.
Conclusion
Overall, we designed and validated 2 ddPCR assays allowing routine or preclinical monitoring of early- and long-term circulating approved or experimental CAR T cells, including our own IL-1RAP CAR T cells, which will be evaluated in an upcoming phase I clinical trial.
Similar content being viewed by others
Background
It is well known that the immune system is a remarkable barrier against cancer. Improvement of the immune system by ex vivo genetic engineering of immunocompetent T cells to express a chimeric antigen receptor (CAR T cells) has shown impressive and unexpected results in clinical trials for hematologic malignancies [1]. Consequently, treatment of refractory/relapsed (R/R) acute lymphoblastic leukemia (ALL) [2], diffuse large B cell lymphoma (DLBCL), and chronic lymphoid leukemia (CLL) [3] patients has led to approval, by US and EU regulatory agencies, of four autologous CAR T drugs directed against CD19 (tisagenlecleucel/tisa-cel/Kymriah®, Novartis; axicabtagene ciloleucel/axi-cel/Yescarta®, Kite-Gilead; brexucabtagene autoleucel/brexu-cel/Tecartus, Kite-Gilead; and lisocabtagene maraleucel/liso-cel/Breyanzi®, Bristol Meyer Squibb) and one against BCMA (idecabtagene vicleucel/ide-cel/Abecma®, BMS) for multiple myeloma [4]. This success greatly increases the likelihood of developing adoptive immunotherapy for other hematologic malignancies, such as multiple myeloma (MM) [5] and acute myeloid leukemia (AML) [6], as well as for solid tumors [7].
Pivotal clinical trials and routine practice [8] have shown that the first 28 days of peak expansion and the long-term memory persistence of CAR T cells are key factors in the efficiency and clearance of tumor cells. Moreover, adverse events such as cytokine release syndrome (CRS) and immune effector cell-associated neurotoxicity syndrome (ICANS) are observed after this therapy [9].
While an increasing number of patients are now routinely treated with these two approved drugs and many experimental CAR T cells are in development, there is a need for tools for monitoring circulating gene-modified T cells and evaluating the safety of advanced therapy medical products (ATMPs) for quality control of good manufacturing production (GMP) delivery, such as vector copy number per cell or transduction efficiency evaluation.
Independent of allogenic CAR T monitoring that can be performed using chimerism analysis methods, there are several additional ways to detect CAR T cells via in vivo tracking using methods such as PET imaging [10]. Flow cytometry analysis can be performed after indirect cell staining using a biotinylated protein target recognized by the CAR itself or by using monoclonal antibodies, allowing detection of cell surface expression of alternative proteins (truncated ∆CD19 [11], truncated nerve growth factor receptor ∆NGFR [12], short peptide/suicide epitope RQR8 [13], and truncated epidermal growth factor receptor ∆EGFR [14]) or CAR-coupled tags (HA and HIS) from onboard sequences of the CAR constructs.
Flow cytometry analysis is easy and rapid to perform and allows subcellular analysis among CAR T cell populations, but it needs to be performed on fresh samples, and the lack of sensitivity may impair analysis of long-term low-level CAR T cell persistence. Taking advantage of the presence of chimeric fusion nucleotide sequences coding for the CAR, molecular quantitative real-time PCR (qPCR) may be an ideal tool for quantitative determination of rare events, as it is already used in minimal residual disease quantification in oncohematology [15] or CAR T cell monitoring in peripheral blood [16]. More recently, droplet digital PCR (ddPCR), based on the multiplication of partitioned independent PCRs and Poisson statistics [17], has emerged as an easy, robust and reproducible molecular tool that may replace classical qPCR. The advantages consist of easy analysis of the endpoint and direct absolute quantification without the need for reference and calibration target DNA standard curves.
Here, we designed two ddPCR assays that target the T cell activation domain fusion areas CD28/CD3z (28z) and 4.1BB/CD3z (BBz) for tisa-cel and Axi-Cel sequences, respectively, and are useful for our own third-generation experimental IL-1RAP CAR construct [11]. ddPCR was compared to cytometry and qPCR before being applied to our preclinical ATMP production process in two in vivo xenograft experimental murine models (MM and AML) and in samples from patients treated for R/R ALL or BLBCL at different French clinical centers.
Materials and methods
Cell lines, CAR constructs and patient samples
The CEMT (CRL-2265™), HEK293T (CRL-11268™), MM1S (GFP+, Luciferase+, CRL-2974™) and Monomac6 (Luciferase+) cell lines were purchased from the American Type Culture Collection (ATCC) and stored in our master cell bank. Experimental CAR T cells were generated from healthy donors as described previously.
The CAR constructs included both approved CD19 CAR constructs (tisa-cel and axi-cel). We also used two experimental anti-IL-1RAP-CAR and anti-CS1-CAR vectors that mimic the intracellular activation domains of both commercial CAR T drugs. Axi-cel and tisa-cel are usually detected by flow cytometry using a biotinylated recombinant CD19 protein target. Our 2 experimental vectors carry truncated CD19 (∆CD19) and c-Myc Tag sequences, allowing for flow cytometry (FC) detection.
Blood samples were collected from patients treated with axi-cel or tisa-cel. All subjects provided written consent.
Lentiviral supernatant production and CAR T cell manufacturing
Lentiviral supernatant was produced after triple transfection of the HEK293T cell line. Experimental CAR T cells were produced from healthy donors as previously described [11]. Briefly, cells were transduced after an initial activation and CD3+ MACS-selection step using CD3/CD28 beads following an expansion period in the presence of IL-2. Preclinical-grade IL-1RAP CAR T cells were also produced from healthy donors in a Prodigy device (Miltenyi Biotech) according to the manufacturer’s protocol. Briefly, selected CD4+ and CD8+ cells were activated with CD3/CD28+ IL-7/IL-15 (MACS GMP T Cell TransAct, Miltenyi Biotech) before being transduced and expanded for 9 days in a closed tubing set and TexMACS medium (Miltenyi Biotech). In both cases, genetically modified T cells were purified to increase purity to > 99%.
Flow cytometry analysis
CEM-CAR and serial dilutions within the wild-type CEMT cell line and experimental CAR T cells were analyzed by flow cytometry on a BD LSRFortessa™ X-20 cell analyzer after staining with either FITC-cMyc antibodies (Miltenyi Biotec™, Clone SH1-26E7.1.3) for CS1 CAR T cells (Myc-tagged CS1 scFV) or APC-CD19 antibodies (Miltenyi Biotec™, Clone 6D5) for IL-1RAP CAR T cells (truncated CD19 is expressed on the cell surface of gene-modified T cells). 7-AAD staining was also performed to evaluate viability.
For patient monitoring, following incubation of whole blood with an FcR blocking reagent (Miltenyi Biotec), cells were stained with biotinylated human CD19 and Fc tag protein (AcroBiosystems) followed by phycoerythrin-labeled streptavidin (BioLegend). Classical T cell surface markers, including CD3, were also targeted with directly conjugated monoclonal antibodies. After red cell lysis, samples were analyzed in a FACSCanto™ II flow cytometer using FACSDIVA™ 8.0 software (BD Biosciences). The percentage of CAR+ T cells among CD3+ lymphocytes and the absolute number of CAR-T cells (deduced from bead-based absolute enumeration of T cells (BD Biosciences)) were determined.
Primer and probe design
We designed two different quantitative PCR assays, 28z matching axi-cel and the CS1 experimental CAR and 41BBz matching tisa-cel and the IL-1RAP experimental CAR, and a PCR assay targeting GAPDH as a housekeeping reference.
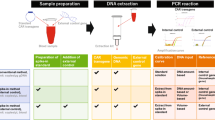
Primers and probes were designed complementary to the sequences coding for the T activation domain of the CAR to match with the 2nd- or 3rd-generation CAR T constructs carrying the CD28 and 4.1BB genes. The CD28 forward primer used in 28z PCR spans the CD28/CD3z junction, and the bifluorescent TaqMan probe specific to CD3z is common for all CARs. The specificity of the primers was assessed by standard PCR performed with experimental CAR plasmid DNA or DNA extracted from left-over axi-cel or tisa-cel CAR T drug bags. For ddPCR, Evagreen (EvaGreen Supermix, Biorad, France) was used as a DNA-binding dye in place of the bifluorescent probe. A schematic representation and the sequences of primers and probes for PCR assays are provided in Fig. 1A and Table 1.
A Schematic representation of the CAR constructs and localization of PCR primers and probes. Localization of primers and probe for 28BBz and 28z PCRs specific for experimental IL-1RAP and tisa-cel CARs and for experimental CS1 and tisa-cel CARs, respectively. The sense primer for 28z PCR spans the CD28/CD3z junction area. FMC63: Single chain of the CD19 antibody. scFv: Single chain of the variable fragment. B Agarose gel electrophoresis of the 28z and 28BBz PCR products. MW: molecular weight marker; bp: base pair
Extraction of genomic DNA from serial dilution of cells and plasmid DNA
Plasmid DNA was extracted using a plasmid DNA extraction kit (Qiagen, Courtaboeuf, France). Genomic DNA (gDNA) isolation was performed from cells or whole peripheral blood from patients using a QiaAmp Blood Extraction Kit (Qiagen, Courtaboeuf, France). DNA concentrations were measured by UV spectrophotometry using a Nanodrop ND2000 (Thermo Fisher, France), and the concentration was adjusted at 20 ng/μl. The absence of PCR inhibitors was checked by control PCR and agarose electrophoresis. Plasmid DNA was diluted into gDNA from the untransduced CEM cell line (from 10e6 to 10e0 copies). CS1- or IL-1RAP-transduced CEM cells were diluted into untransduced CEM cells and analyzed by flow cytometry. Moreover, gDNA was extracted from these 2 serial dilutions.
qPCR and ddPCR amplification reactions
The qPCR mix was prepared by adding 10 µL of 2X TaqMan™ Universal Master Mix II buffer (Thermo Fisher, France), 1 µL of each primer at a concentration of 10 pmol/µL, 0.5 µL of probe at a concentration of 10 pmol/µL, 100 ng (equivalent to 150,000 cells) of DNA and H2O qs to 20 µL. The plate was centrifuged and loaded on a Bio-Rad™ CFX96 Real-Time PCR Detection System. The results were analyzed with the CFX Manager™ v3.1 Software.
Prior to ddPCR, DNA samples were either sonicated for 90 s (Covaris M220 ultrasonicator) or digested with the EcoRI enzyme, which is known to not cut within the amplification area. ddPCR mix was prepared using 10 µL of QX200™ ddPCR™ EvaGreen Supermix (BioRad, France), reverse and forward primers at final concentrations of 150 nM, 100 ng of gDNA (equivalent to 15,000 cells) and nuclease-free water in a total volume of 20 µL. The mixes were then loaded into the DG8™ Cartridge, and droplets were generated automatically with the QX200™ Droplet Generator. The emulsion was transferred to a PCR plate and cycled using the following thermal cycler conditions: predenaturation at 95 °C for 5 min, 40 cycles at 95 °C for 30 s, 60 °C for 1 min, and 4 °C for 5 min, and a final step at 90 °C for 10 min. Data acquisition and analysis were performed with the QX200™ Droplet Reader and QuantaSoft™ Software (Biorad, France).
CAR copy quantification, vector copy number quantification and multiplicity of infection
Typically, CAR quantification is given as the number of transgene copies per µg of gDNA, adjusted from the starting quantity of gDNA used in PCR. In practice, while 100 ng of gDNA is equivalent to 15,000 cells or 30,000 haploid gene copies, it is possible to translate and thus estimate the number of cells, hypothesizing that there is one copy of vector per cell.
Vector copy number (VCN) was assessed by ddPCR after running both target and reference GAPDH PCR. Assuming that there were 2 copies of the GAPDH gene per genome cell, the vector copy number (VCN) was calculated from absolute ddPCR quantification as a ratio of the number of target copies to half the number of reference gene copies normalized by the transduction efficiency percentage.
We also investigated the link between the viral particle number (multiplicity of infection) used for transduction and the transduction efficiency and transgene copy number. Transductions were performed at different MOIs (0.02, 0.04, 0.1, 0.2, 1, 10, 25, and 50) for each CAR, as previously described. Transduction efficiencies were measured at day 9 prior to DNA extraction and ddPCR.
CAR T cell monitoring in AML and MM xenograft tumor murine models
NOD/SCID/IL2Rγc-deficient (NSG) mice (6–8 weeks of age, The Jackson Laboratory, Sacramento, CA, USA) were irradiated (2.5 Gy) and inoculated intravenously (I.V.) with luciferase-expressing MM1-S/CS1+ (MM) or MonoMac-6/IL1RAP+ (AML) cell lines (1.10e6/mouse). Twenty hours later, the mice were infused I.V. with 5.10e6 CS1- or 10.10e6 IL-1RAP CAR T cells. For each model (n = 8 mice), the controls consisted of irradiated mice only (n = 1), mice infused with CAR T cells only (n = 3) or mice xenografted with tumor cell lines (n = 1). Tumor growth was studied by luminescence imaging (IVIS 152 Lumina Series III, Perkin Elmer, Waltham, MA, USA). Peripheral blood was harvested every 3 days by submandibular bleeding. At the end of the experiment (day 30), the mice were euthanized, and the bone marrow, spleen and lung were harvested for DNA isolation and ddPCR. All animal procedures were carried out according to the guidelines of our animal experimentation house. The area under the curve (AUC) was calculated from day 0 to day 28 using GraphPad Prism 8.0 software.
Monitoring of patients treated with approved CAR T cell drugs
ddPCR assays were performed retrospectively or prospectively for peripheral blood monitoring of axi-cel- or tisa-cel-treated patients (B-ALL or DLBCL) from different clinical centers and compared with flow cytometry monitoring using biotinylated recombinant CD19 protein. CD19+ cell quantification was also performed by flow cytometry. Among 17 patients monitored over a period covering early extension (D0 to D28) and long-term persistence (up to D450), 10 patients were infused with axi-cel, and 7 were infused with tisa-cel. Patient characteristics and outcomes are provided in Table 2.
Results
Quantitative PCR assays amplify both DNA from experimental and approved drugs
We first verified that our own PCR assays designed from the known sequences of the experimental CAR sequences matched and amplified sequences from genomic DNA extracted from axi-cel or tisa-cel CAR T drug bags. As reported in Fig. 1B, PCR products of the expected size were detected for the 28z plasmid and axi-cel (137 bp) or for the 28BBz plasmid and tisa-cel (145 bp). Fw28z/Rv3z PCR amplified both experimental plasmids (297 bp) but not tisa-cel DNA because the CD28 sequence was missing. To confirm this hypothesis, Sanger sequencing of the PCR products obtained after amplification from axi-cel and tisa-cel DNA showed 100% homology between all respective sequences (data not shown).
The TaqMan qPCR method was first applied to the experimental plasmids IL-1RAP and CS1 serially diluted into human genomic DNA from healthy donors or to genomic DNA extracted from CEM gene-modified T cells diluted into normal CEM cells. As reported in Fig. 2A, B and Additional file 1: Table S1, both 28z and 28BBz PCR assays were able to detect one copy of plasmid in the starting nucleic material. Regression curves were linear for either plasmid or cell DNA dilutions, with correlation coefficients of R2 = 0.928 and 0.8652 or R2 = 0.9975 and 0.9683, respectively, for 28z or 28BBz PCR. Remarkably, the 28z PCR requires fewer amplification cycles (Ct) than the 28BBz PCR to detect one copy of plasmid (34.53 ± 0.34 and 39.68 ± 0.67, respectively).
A Real time qPCR of DNA plasmids. 28z and 28BBz plasmids were serially diluted in untransduced CEM DNA and amplified by PCR with both Fw28z/Rv3z and GAPDH primer pairs. Amplification curves are provided (left). Ct is plotted against log transgene dilution, and linear regression equations and correlation coefficients are provided (right) for n = 4 independent experiments. B Flow cytometry-based CAR T cell detection. CS1- or IL-1RAP-transduced CEM cell lines were serially diluted in an untransduced CEM cell line. The percentage of the starting transduced cell population is provided. Representative experiment. SSC-A: side scatter. C Real-time qPCR of genomic DNA from serially diluted CAR-transduced cells. Genomic DNA was extracted from CS1- or IL-1RAP-transduced CEM cells serially diluted in untransduced CEM and amplified by 28z, 28BBz and GAPDH qPCR. Amplification curves are provided (left). Ct is plotted against log transgene dilution, and linear regression equations and correlation coefficients are provided (right) for n = 4 independent experiments. RFU: relative fluorescence units; Ct: cycle threshold; Ct: cycle threshold
Quantitative ddPCR is more or more sensitive than flow cytometry
Validated qPCR assays were then switched to ddPCR assays and applied to the same plasmid DNA or gDNA cell dilutions. As reported Fig. 3A and Additional file 1: Table S2, 28z and 28BBz ddPCR are also able to detect copies of the target throughout the dilution range for plasmid DNA (up to one copy) but are only able to detect up to 10-e3 copies for gDNA cell dilutions, even if the target is always detectable (28z PCR). Flow cytometry detection (Fig. 2B, Additional file 1: Table S3) allowed us to detect precisely 10E−3 after either CS1 or CD19 staining, while ddPCR allowed detection at a level of 10e−3 (for 28 BBz) and 10E−6 (for 28z).
A ddPCR sensitivity assessment by plasmid dilutions. Both plasmids were diluted in nontransduced CEM cell gDNA, and CEM-CAR was diluted in an untransduced CEM cell line. ddPCR (28z and 28BBz) was applied to plasmid dilution (top) and to gDNA extracted from the cell line dilution (bottom). Positive and negative droplets were delimited by the threshold (pink line). The CAR copy number is plotted against plasmid copy numbers or cell dilution factors. Linear regression curves and correlation coefficients are provided for n = 4 independent experiments. CAR DNA plasmids (10e6 copies) or CAR + cell lines (undiluted) are considered as positive PCR controls. NT: not transduced sample. B Vector copy number. (vector copy number (VCN, transgene copies/CAR T cells, Y left axis, red circles) is plotted against multiplicity of infection (MOI) calculated from 28z and 28BBz ddPCR and reference housekeeping gene (GAPDH) ddPCR normalized to the transduction efficiency percentage. Transduction efficiency (TE, blue squares) obtained by flow cytometry (FC, %) is provided (Y right axis). (Left) Average VCN measured for axi-cel (n = 4) and tisa-cel (n = 8) obtained from leftover bags of CAR T cell products and for IL-1RAP CAR T cells produced under experimental (n = 4) or GMP-like conditions (n = 4). *p < 0.05
Vector copy number, analyzed by ddPCR, is dependent on the MOI but meets the regulatory requirement for the “GMP-like” IL-1RAP CAR T cell preclinical production process
Mean vector copy number per cell was quantified with ddCPR targeting CAR T vector sequences and a GAPDH housekeeping gene to estimate the number of genome equivalents (assuming that there were 2 copies of the gene per cell). The results were normalized according to the percentage of gene-modified T cells obtained by flow cytometry (experimental or GMP-like IL-1RAP CAR, n = 4) or from the drug leaflet (n = 4 or 8, respectively, for axi-cel or tisa-cel) provided with the infusion bags. As reported in Fig. 3B, for an MOI < 1 [0.02–0.2], the average VCN per cell remained under 1 [0.4 to 0.8 and 0.1 to 0.6 for CS1 (28z) and IL-1RAP (28BBz) CAR, respectively]. However, when the MOI is ≥ 1 [1–50], the mean VCN per cell increased linearly [1.1 to 2.1 (R2 = 0.9) and 1.2 to 2.8 (R2 = 0.94) for CS1 (28z) and IL-1RAP (28BBz) CAR, respectively]. Accordingly, transduction efficiency, assessed by flow cytometry, correlated with VCN according to MOI.
We then quantified the average VCN for DNA extracted from leftover bags of axi-cel or tisa-cel samples (Table 3). The means VCN was 1.5 ± 0.6 (n = 4) and 0.9 ± 0.39 (n = 8) for transduction efficiencies of 70.3 ± 9.67% and 17.7 ± 11.74%, respectively. For IL-1RAP CAR T cell production, either experimental or GMP-like, we did not note a significant difference between the average VCN per cell of IL-1RAP CAR T cells, with values of 2 ± 0.34 (n = 4) and 2.2 ± 0.87 (n = 4) for transduction efficiencies of 27.4 ± 9.67% and 29.6 ± 17.50%, respectively (Fig. 3C).
ddPCR allows in vivo monitoring of experimental CAR T cells in mouse tumor xenograft models
We then applied our 28z and 28bbz ddPCR assays to peripheral blood harvested from mice (n = 3, in each group) xenografted or not with tumor cell lines (AML, Monomac-6/IL-1RAP CAR for 28BBz and MM, MM1S/CS1 CAR for 28z). In the MM1S/CS1 model, after early CAR T cell responses, the mice were challenged again with a new infusion of the tumor cell line. At the end of the experiment, after serial harvesting of PB, organs (marrow, spleen, and lungs) were collected (Fig. 4A). We demonstrated that our ddPCR assays are able to monitor the early expansion of circulating CAR T cells in both models and allow us to calculate the area under the curve (AUC0-28). For the AML model, we showed a difference in CAR T cell expansion in the presence (AUC0-28 = 56911 ± 16668, n = 3) and absence (AUC0-28 = 40452 ± 11403, n = 3) of target cells. For the MM model, we did not detect a significant difference between CAR T cell expansion in mice xenografted (mean AUC0-28 = 18895 ± 5373, n = 3) or not (mean AUC0-28 = 17302 ± 6061, n = 3) with tumor cells. However, in the MM model, when the mice were challenged again with the tumor, we clearly observed a second peak expansion in 4 out of 6 mice independent of whether the mice were grafted or not with tumor MM1S cells at day 0 (Fig. 4B).
In vivo CAR T cell monitoring method for xenograft tumor murine models. A Schematic workflow summarizing the xenografting of MM1S or Monomac-6 tumor cell lines (day 0) one day after mouse irradiation (2.5 Gy). On day 1, CS1 or IL-1RAP CAR T cells were intravenously injected. Biological samples were harvested kinetically (PB, day 2 to day 30 or 50) or at the end of the experiment (organs, day 30, Monomac-6/IL-1RAP) and processed for gDNA extraction and ddPCR. For the MM1S/CS1 model, mice were challenged again with tumor cells; n = 3 mice (12 in total) were included in each group. B Individual early (day 0 to day 50) longitudinal monitoring of CS1 and IL-1RAP monitoring with 28z and 28BBz ddPCR, respectively. Green and blue curves represent ddPCR CAR T cell monitoring for mice grafted or not with the target tumors, respectively. The mean CAR transgene copy number detected in each group is plotted (n = 3 mice/group). Arrows show the second CAR T cell expansion peaks following the second tumor injection. AUC: area under the curve day 0 to 28, calculated with GraphPad software. C Monitoring CAR T cells in organs. Transgene copies/µg of DNA obtained by 28BBz ddPCR on gDNA extracted from organs of n = 3 individual mice receiving IL-1RAP CAR T cells after grafting (green) or not (blue) of Monomac6 tumor cells. Each quantification was performed in duplicate. (−) and (+) are negative and positive PCR controls as respectively no template or IL-1RAP CAR+ cell line DNA
Finally, we showed that the 28BBz ddPCR assay is useful for quantifying the homing of CAR T cells. As shown in Fig. 4C, IL-1RAP CAR T cells were found (on day 31) in all the investigated organs, such as the bone morrow (n = 3), spleen (n = 3) and lung (n = 3), with a trend of higher amounts in mice grafted with AML tumor cells.
ddPCR allows patient monitoring of early increases and long-term circulation in the peripheral blood of both approved CD19 CAR T cells
We finally performed a prospective and retrospective study by applying both designed ddPCR assays for longitudinal follow-up (up to 500 days) of real-life DLBCL (n = 13) or B-ALL (n = 4) patients receiving either axi-cel (n = 10) or tisa-cel CAR-T cells (n = 7) (Fig. 5). For all of the patients, ddPCR was able to detect early expansion of CAR T cells, with a perfect match between ddPCR and flow cytometry. Similar kinetics, with early loss of CAR T cells after peak expansion, were detected by flow cytometry. However, in the vast majority of patients (16 out 17), ddPCR detects the persistence of circulating CAR T cells for up to 450 days (UPN #11).
Long-term monitoring and follow-up of CAR T cells in treated DLBCL or B-ALL patients. Ten patients (DLBCL) receiving axi-cel and 7 (4 B-ALL and 3 DLBCL) receiving tisa-cel were monitored using 28BBz or 28z ddPCR (blue lines, left Y-axis) on gDNA extracted from circulating PB cells. CD19 CAR T cell numeration (red lines, right Y-axis), obtained by FC, is plotted (green lines, right Y-axis) on the same respective graph. AUC: area under the curve day 0 to 28, calculated with GraphPad software. (*) highlights patients in whom CD19+ cells reappear
Remarkably, in two B-ALL patients (UPN #14, Phi+ and #17) receiving tisa-cel, we noted in flow cytometry analysis that CD19+ leukemic cells reappear in the PB after being undetectable, whereas tisa-cel CAR T cells were always detectable by ddPCR.
Discussion
The use of CD19 CAR T cells has been successful for treating R/R B cell malignancies such as ALL [18] or DLBCL, leading to several drug approvals by regulatory agencies, and this approach will be approved for other B-malignancies such as MM or CLL, and in the near future for AML and solid tumors in the long term. This success has underlined the need to precisely monitor CAR-expressing T cells.
Indeed, the administration of CAR T cells in clinical trials or in routine clinical practice has shown that early expansion and long-term persistence are predictive elements of the therapeutic response [19]. Longitudinal quantification of CAR T cells can inform CAR T cell engraftment and provide indirect information on adverse events such as cytokine release syndrome (CRS) and immune effector cell-associated neurotoxicity (iCANS) [9].
Moreover, in the case of relapse after CAR T cell infusion, it may be helpful to understand whether this relapse is caused by the loss of antigen by leukemic cells or other mechanisms independent of the presence or persistence of CAR T cells. This is well illustrated in our study, where 2 patients had detectable tisa-cel CAR T cells in the long term, while B cell numbers increased in the PB. Overall, it is now well established that direct monitoring of CAR T cells will help clinicians optimize and adapt treatment.
Today, there are different ways to quantify CAR T cells by flow cytometry using specific biotinylated targets or anti-scFv antibodies [20]. Because this method discriminates T cell subpopulations within circulating gene-modified T cells, its sensitivity remains limited. One way to increase sensitivity is to move toward the minimal residual disease (MRD) flow procedure by analyzing a large number of PB cells [21].
Other more sensitive molecular methods are available, taking advantage of the presence of additional nucleotide sequences integrated within the host genome of CAR T cells. LTR PCR is a well-proven and robust method that is used for routine HIV virus quantification and can be used for CAR T cell quantification by the presence of the LTR sequence promoter in lentiviral constructs [22]. However, in all the lentiviral backbones used for CAR constructs, the LTRs are deleted (self-inactivating (SIN) vector) to ensure safety and prevent self-replication. Such modifications may alter PCR primer annealing. Moreover, LTR PCR primers may cross-react with residual integrated homologous off-target sequences originating from previous infections.
Other approaches that target T cell signaling sequences in quantitative PCR assays, real-time (qPCR) [16] or endpoint PCR (dPCR) [23,24,25] are suitable for CAR T cell quantification. Here, we designed our own ddPCR assays based on 2 experimental CARs with known sequences, which were validated and tested in murine experiments. We demonstrated that our ddPCR assays also matched axi-cel and tisa-cel and allowed patient monitoring in the early or late stage of their treatment. While our ddPCR targets the T cell receptor junction sequence, it can easily be applied to a large panel of CAR T cells, such as brexu-cel (same construct as axi-cel), liso-cel and ide-cel, which carry the 4.1BB/CD3z junction. Moreover, ddPCR offers several advantages, as it does not need a reference standard curve, allows direct absolute quantification, is less sensitive to potential PCR inhibitors and is more accurate [17]. We noted that 28BBz is as sensitive as flow cytometry and less sensitive than 28z PCR. Analyzing a larger number of droplets or partitions may help to increase the sensitivity of the 28BBz PCR.
Another aspect is that ex vivo CAR T cell products need to meet quality control standards after manufacturing, such as vector copy number per cell, to meet regulatory requirements before injection [26, 27]. Using our own design ddPCR assay, quantification of VCN in the axi-cel medical product, previously quantified by the manufacturer, allowed us to validate the assay. Importantly, in preparation for a future phase I clinical trial, we were able to show that our IL-1RAP CAR T cells, produced at an MOI of 2 via either a research (Beads CD3/CD28+ IL-2) or GMP-like (soluble CD3/CD28+ IL-7/IL-15, in the cliniMACS prodigy device) protocol process, meet the regulatory requirements under a VCN threshold of 5 copies/transduced cell.
Conclusion
Overall, we designed 2 ddPCR assays targeting the T signaling fusion area used in almost all CARs, which can be applied to experimental or approved (axi-cel or tisa-cel) CAR T cell quality control analysis and patient monitoring. The 28 BBz ddPCR assay will be elevated to the GMP level for application in quality control of our in-house IL-1RAP CAR T cell academic production process before being evaluated in an upcoming phase I clinical trial.
Availability of data and materials
All raw data are available on demand.
Abbreviations
- CAR:
-
Chimeric antigen receptor
- Tisa-cel:
-
Tisagenlecleucel
- Axi-cel:
-
Axicabtagene-ciloleucel
- Brexu-cel:
-
Brexucabtagene autoleucel
- Ide-cel:
-
Idecabtagene vicleucel
- FC:
-
Flow cytometry
- IL-1RAP:
-
Interleukine 1 receptor accessory protein
- CS1:
-
SLAM family member 7, CD319
- CD3z:
-
CD3 zeta
- VCN:
-
Virus copy number
- ddPCR:
-
Digital droplet PCR
- R/R:
-
Refractory/relapsed
- ALL:
-
Acute lymphoblastic leukemia
- DLBCL:
-
Diffuse large B cell lymphoma
- CLL:
-
Chronic lymphoid leukemia
- MM:
-
Multiple myeloma
- AML:
-
Acute myeloid leukemia
- CRS:
-
Cytokine release syndrome
- ICANS:
-
Immune effector cell-associated neurotoxicity syndrome
- BCMA:
-
B-cell maturation antigen
- qPCR:
-
Real time quantitative real-time PCR
- scFv:
-
Single Chain Fragment Variable
- gDNA:
-
Genomic DNA
- GMP:
-
Good manufacturing production
- ATMPs:
-
Advanced therapy medical products
- AUC:
-
Area under the curve
- MOI:
-
Multiplicity of infection
- UPN:
-
Unique Personal Number
- LTR:
-
Long terminal repeat
- CV:
-
Coefficient of variation
- SD:
-
Standard deviation
References
June CH, Sadelain M. Chimeric antigen receptor therapy. N Engl J Med. 2018;379(1):64–73.
Maude SL, Laetsch TW, Buechner J, Rives S, Boyer M, Bittencourt H, et al. Tisagenlecleucel in children and young adults with B-cell lymphoblastic leukemia. N Engl J Med. 2018;378(5):439–48.
Faitschuk E, Hombach AA, Frenzel LP, Wendtner CM, Abken H. Chimeric antigen receptor T cells targeting Fc mu receptor selectively eliminate CLL cells while sparing healthy B cells. Blood. 2016;128(13):1711–22.
Munshi NC, Anderson LD Jr, Shah N, Madduri D, Berdeja J, Lonial S, et al. Idecabtagene vicleucel in relapsed and refractory multiple myeloma. N Engl J Med. 2021;384(8):705–16.
Cohen AD, Garfall AL, Stadtmauer EA, Melenhorst JJ, Lacey SF, Lancaster E, et al. B cell maturation antigen-specific CAR T cells are clinically active in multiple myeloma. J Clin Invest. 2019;129(6):2210–21.
Cummins KD, Gill S. Will CAR T cell therapy have a role in AML? Promises and pitfalls. Semin Hematol. 2019;56(2):155–63.
Ramakrishna S, Barsan V, Mackall C. Prospects and challenges for use of CAR T cell therapies in solid tumors. Expert Opin Biol Ther. 2020;20(5):503–16.
Kochenderfer JN, Somerville RPT, Lu T, Yang JC, Sherry RM, Feldman SA, et al. Long-duration complete remissions of diffuse large B cell lymphoma after anti-CD19 chimeric antigen receptor T cell therapy. Mol Ther. 2017;25(10):2245–53.
Neelapu SS. Managing the toxicities of CAR T-cell therapy. Hematol Oncol. 2019;37(Suppl 1):48–52.
Li M, Wang Y, Liu M, Lan X. Multimodality reporter gene imaging: construction strategies and application. Theranostics. 2018;8(11):2954–73.
Warda W, Larosa F, Neto Da Rocha M, Trad R, Deconinck E, Fajloun Z, et al. CML hematopoietic stem cells expressing IL1RAP can be targeted by chimeric antigen receptor-engineered T cells. Cancer Res. 2019;79(3):663–75.
Casucci M, Falcone L, Camisa B, Norelli M, Porcellini S, Stornaiuolo A, et al. Extracellular NGFR spacers allow efficient tracking and enrichment of fully functional CAR-T cells co-expressing a suicide gene. Front Immunol. 2018;9:507.
Philip B, Kokalaki E, Mekkaoui L, Thomas S, Straathof K, Flutter B, et al. A highly compact epitope-based marker/suicide gene for easier and safer T-cell therapy. Blood. 2014;124(8):1277–87.
Wang X, Chang WC, Wong CW, Colcher D, Sherman M, Ostberg JR, et al. A transgene-encoded cell surface polypeptide for selection, in vivo tracking, and ablation of engineered cells. Blood. 2011;118(5):1255–63.
Juul-Dam KL, Ommen HB, Nyvold CG, Walter C, Valerhaugen H, Kairisto V, et al. Measurable residual disease assessment by qPCR in peripheral blood is an informative tool for disease surveillance in childhood acute myeloid leukaemia. Br J Haematol. 2020;190(2):198–208.
Wang H, Du X, Chen WH, Lou J, Xiao HL, Pan YM, et al. Establishment of a quantitative polymerase chain reaction assay for monitoring chimeric antigen receptor T cells in peripheral blood. Transpl Proc. 2018;50(1):104–9.
Vogelstein B, Kinzler KW. Digital PCR. Proc Natl Acad Sci USA. 1999;96(16):9236–41.
Maude SL, Shpall EJ, Grupp SA. Chimeric antigen receptor T-cell therapy for ALL. Hematol Am Soc Hematol Educ Program. 2014;2014(1):559–64.
Mueller KT, Maude SL, Porter DL, Frey N, Wood P, Han X, et al. Cellular kinetics of CTL019 in relapsed/refractory B-cell acute lymphoblastic leukemia and chronic lymphocytic leukemia. Blood. 2017;130(21):2317–25.
Demaret J, Varlet P, Trauet J, Beauvais D, Grossemy A, Hego F, et al. Monitoring CAR T-cells using flow cytometry. Cytom B Clin Cytom. 2020;100(2):218–24.
Kruse A, Abdel-Azim N, Kim HN, Ruan Y, Phan V, Ogana H, et al. Minimal residual disease detection in acute lymphoblastic leukemia. Int J Mol Sci. 2020;21(3):1054.
Baras A, Bocket L, Beauvais D, Hallaert C, Varlet P, Yakoub-Agha I, et al. A real-time quantitative PCR targeting the viral vector for the monitoring of patients treated with axicabtagene ciloleucel. J Mol Diagn. 2020;23(4):447–54.
Davis L, Riccitelli N, Valencia N, Ch’en IL, Tangri S, Brogdon JL, et al. Monitoring of tisagenlecleucel transgene DNA using a quantitative polymerase chain reaction assay. Mol Ther Methods Clin Dev. 2021;20:535–41.
Fehse B, Badbaran A, Berger C, Sonntag T, Riecken K, Geffken M, et al. Digital PCR assays for precise quantification of CD19-CAR-T cells after treatment with axicabtagene ciloleucel. Mol Ther Methods Clin Dev. 2020;16:172–8.
Mika T, Maghnouj A, Klein-Scory S, Ladigan-Badura S, Baraniskin A, Thomson J, et al. Digital-droplet PCR for quantification of CD19-directed CAR T-cells. Front Mol Biosci. 2020;7:84.
Kunz A, Gern U, Schmitt A, Neuber B, Wang L, Huckelhoven-Krauss A, et al. Optimized assessment of qPCR-based vector copy numbers as a safety parameter for GMP-Grade CAR T cells and monitoring of frequency in patients. Mol Ther Methods Clin Dev. 2020;17:448–54.
Lu A, Liu H, Shi R, Cai Y, Ma J, Shao L, et al. Application of droplet digital PCR for the detection of vector copy number in clinical CAR/TCR T cell products. J Transl Med. 2020;18(1):191.
Acknowledgements
CRB SUD TUMOROTHEQUE Biobanques collection BB-0033-00046. EPIGENExp (EPIgenetics and GENe EXPression Technical Platform), Université Bourgogne Franche-Comté, F-25000 Besançon, France.
Funding
Association Nausicaa Combat sa Leucémie (nonprofit association-loi 1901 FR); Gift 2017-03, 2018, 2019 and 2020. This work was supported by the MiMedi project funded by BPI France (Grant No. DOS0060162/00) and the European Union through the European Regional Development Fund of the Region Bourgogne-Franche-Comte (Grant No. FC0013440). French Blood Center, Grants 2018 and 2019. EU project T2EVOLVE Grant Agreement No. 945393. UMR1098 RIGHT is a member of the OPALE Carnot Institute. Rafik Haberbache has a fellowship from Grand Besançon Metrople (GBM).
Author information
Authors and Affiliations
Contributions
Conceptualization and study design: RH, WW, EH, MD, CF. Methodology, experiments and data analysis: RH, CB, WW, CN, LB, EH, AD, MNdR, RT, CF. Original draft and figures: RH, WW, CN, MNdR, MD, CF. Clinical advice and patient collection: IYA, FV, VA, XR, PS, DC, OC, SCZ, POR, CT, NB. Writing, review and/or revision of the manuscript: RH, CF, WW, MD. Overall supervision and research funding: CF, MD. All authors reviewed the manuscript and contributed to improving the paper. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Research involving human material have been performed in accordance with the Declaration of Helsinki. Animal experiment have been performed according to the local ethics committee of the animal house of University of Franche-Comté.
Consent for publication
Not applicable.
Competing interests
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Supplementary data, Haderbache et al, qPCR, ddPCR and cytometry sensitivity and reproducibility
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Haderbache, R., Warda, W., Hervouet, E. et al. Droplet digital PCR allows vector copy number assessment and monitoring of experimental CAR T cells in murine xenograft models or approved CD19 CAR T cell-treated patients. J Transl Med 19, 265 (2021). https://doi.org/10.1186/s12967-021-02925-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12967-021-02925-z