Abstract
Background
Community-level group sports participation is a structural aspect of social capital that can potentially impact individual health in a contextual manner. This study aimed to investigate contextual relationship between the community-level prevalence of group sports participation and the risk of all-cause, cardiovascular disease (CVD), and cancer mortality in older adults.
Methods
In this 7-year longitudinal cohort study, data from the Japan Gerontological Evaluation Study, a nationwide survey encompassing 43,088 functionally independent older adults residing in 311 communities, were used. Cause of death data were derived from the Japanese governmental agency, The Ministry of Health, Labour and Welfare, for secondary use. “Participation” was defined as engaging in group sports for one or more days per month. To analyze the data, a two-level survival analysis was employed, and hazard ratios (HRs) and 95% confidence intervals (CIs) were calculated.
Results
Among the participants, 5,711 (13.3%) deaths were identified, with 1,311 related to CVD and 2,349 to cancer. The average group sports participation rate was 28.3% (range, 10.0–52.7%). After adjusting for individual-level group sports participation and potential confounders, a higher community-level group sports participation rate was found to be significantly associated with a lower risk of both all-cause mortality (HR: 0.89, 95% CI: 0.83–0.95) and cancer mortality (HR: 0.89, 95% CI: 0.81–0.98) for every 10% point increase in the participation rate. For CVD mortality, the association became less significant in the model adjusted for all covariates (HR: 0.94, 95% CI: 0.82–1.09).
Conclusions
Our findings support the existence of a preventive relationship between community-level group sports participation and the occurrence of all-cause and cancer mortality among older individuals. Promoting group sports within communities holds promise as an effective population-based strategy for extending life expectancy, regardless of individual participation in these groups.
Similar content being viewed by others
Background
Engaging in sports and exercise as part of a group has several advantages for older adults, including a reduced risk of functional disability [1], depressive symptoms [2], and falls [3], compared to participating in individual sports and exercise without group involvement. The health outcomes achieved through group participation in sports as opposed to individual exercise may be attributed to several factors. These factors include the benefits of physical activity, such as promoting good adherence and a longer duration of exercise. Furthermore, psychological factors such as increased enjoyment, enhanced self-esteem, and decreased stress and social factors, including receiving social support, social capital, and social influence, also play a significant role [4].
Community-level group sports participation has been shown to significantly reduce depressive symptoms [5] and cognitive impairment [6] in older adults. Therefore, older adults residing in communities with higher group sport participation rates, regardless of participation at the individual level, are less likely to exhibit depressive symptoms and cognitive impairment compared to those residing in communities with lower participation rates. These findings may be attributed to the contextual effects facilitated by the presence of social capital within the community [7]. Previous studies [7,8,9] have provided a comprehensive theoretical overview of social capital and described it as “features of social organizations, such as networks, norms, and trust, that facilitate action and cooperation for mutual benefit” [10] or “resources that are accessed by individuals as a result of their membership of a network or a group.” [7] Communities where group sports thrive typically exhibit higher community-level social capital, which, in turn, can facilitate adoption of healthy behaviors among individuals who do not personally participate in the group sports through social contagion, informal social control, and collective efficacy in the community [7]. The empirical evidence from the following studies supports the existence of this effect. Older adults, including those who do not participate in group sports, residing in a community with higher group sport participation rates among older adults are less likely to be homebound and exhibit higher transtheoretical model stages of change for exercise compared to those residing in communities with lower participation rates [11].
As previously mentioned, the beneficial effects of community-level group sports participation on health behaviors and status among older adults have been established. However, it is still unclear whether this participation can actually reduce the risk of mortality. A systematic review was conducted to investigate the relationship between social capital and mortality, including all-cause as well as cause-specific (i.e., cardiovascular disease [CVD] and cancer) mortality [12]. This review revealed a lack of studies specifically focusing on community-level social participation, which pertains to the structural aspects of social capital. Accordingly, we conducted this study to investigate the potential association between community-level group sports participation and the risk of all-cause, CVD, and cancer mortality among older adults. We hypothesized that older adults living in communities with higher group sports participation rates have a lower risk of mortality due to each cause than those living in communities with lower group sports participation rates. If this hypothesis is supported, the promotion of community group sports could be used as an effective population-based strategy for extending life expectancy, regardless of their participation in group sports.
Methods
Study design and participants
This study utilized longitudinal cohort data from the Japan Gerontological Evaluation Study (JAGES) [13, 14]. JAGES is an ongoing investigation that focuses on examining social, behavioral, and environmental factors associated with functional decline or cognitive impairment in individuals aged 65 or older, which can lead to a loss of independence. The participant flow for this study is depicted in Fig. 1. The baseline survey was conducted between August 2010 and January 2012. During this time frame, self-reported questionnaires were mailed to a total of 80,744 community-dwelling individuals aged 65 or older who were both physically and cognitively independent. These participants were selected from nine municipalities in six prefectures across Japan. A random sample was drawn from the official residence registers in four municipalities, while the remaining five smaller municipalities conducted a complete census of their older residents. Out of the 51,923 respondents (response rate: 64.3%), valid information on ID, gender, age, and ability to perform activities of daily living was collected from 44,715 respondents (valid response rate: 55.4%). To obtain the community-level group sports participation variable, 1,077 respondents with an unknown area of residence or those residing in community areas with 30 or fewer respondents were excluded. This was done to ensure the accuracy of the data by excluding small sample sizes, resulting in 43,638 respondents nested in 311 areas defined primarily by school districts. This provided a valid sample for creating the community-level variable. During the construction of cohort data to track individuals, 44,083 of the 44,715 valid respondents (98.6%) were successfully linked to mortality records over a 7-year follow-up period, which ended on December 31, 2017. For the present multilevel survival analyses, a sample of 43,088 participants (20,186 men and 22,902 women) was analyzed after excluding respondents who lacked information on the community-level variable.
The current study was conducted in accordance with the principles of the Helsinki Declaration and approved by the Ethics Committee, Chiba University, Japan (approval number: 2493), and the National Center for Geriatrics and Gerontology, Japan (approval number: 992-3). All participants were informed about the voluntary nature of their participation and indicated their consent by completing and returning the questionnaire via mail.
Mortality
Information on the date of death was retrieved from the public long-term care insurance system database administered by the municipal governments. The data on the cause of death were then derived from the secondary use of information maintained by the Ministry of Health, Labour and Welfare, a Japanese governmental agency. In Japan, the cause of death is determined based on the death certificate completed by physicians and then reported to the government. Using the information provided about the participants’ area of residence, date of birth, and date of death, the mortality data were linked to the baseline self-reported questionnaire data. The outcomes, including all-cause, CVD-related (I00-I99), and cancer-related (C00-D48) mortality, were assessed according to the 10th revision of the International Classification of Diseases (ICD-10) [15].
Community- and individual-level independent variables
Participants were evaluated based on their frequency of group sports participation, with response options ranging from four days per week or more to 2–3 days per week, one day per week, 1–3 days per month, a few times per year, or zero. Consistent with previous studies [6, 16], “participation” was defined as engaging in group sports activity at least one day per month. To create a community-level independent variable, individual-level group sports participation data were aggregated by community area. In this regard, we calculated the group sports participation rates by dividing the number of group sports participants by the total number of participants included in the analysis. Previous research has suggested a stronger correlation between the proportion of older individuals reporting poor self-rated health or experiencing depressive symptoms and community-level group sports participation occurring frequently at least one day per month (r = − 0.233 and − 0.355, respectively) compared to participation occurring frequently at least one day per week (r = − 0.210 and − 0.314, respectively) [16].
Covariates
Based on previous studies examining the association between community-level group sports participation and health behaviors and status among older adults [5, 6, 11], several covariates were collected. Information on gender and age was collected as basic demographic characteristics, with age groups categorized as 65–69, 70–74, 75–79, 80–84, or ≥ 85 years. In terms of community-level covariates, population density per km2 of inhabitable area was calculated for each community area using national statistics data and categorized into quartile categories (≥ 10,350, 8,190–10,349, 5,680–8,189, or < 5,680 persons per km2). In terms of individual-level covariates, marital status (married or unmarried), living alone (no or yes), occupational status (employed, retired, or never employed), years of education (≥ 13, 10–12, or < 10 years), alcohol drinking status (none, past, or current), and smoking status (none, past, or current) were collected. Annual equivalent income was calculated by dividing household income by the square root of the number of household members and categorized into three groups: $40,000 or more; $20,000–$39,999; or less than $20,000 per year (1 Dollar = 100 Yen). Body mass index (BMI) was calculated using self-reported height and weight (kg/m2) and categorized as underweight (< 18.5), normal weight (18.5–24.9), or overweight/obese (≥ 25.0). BMI values ≥ 25 were grouped into one category as only a small proportion of older adults in Japan and only 1.9% of the current study sample were considered to be obese (i.e., BMI ≥ 30). Disease status was assessed by yes or no responses and included hypertension, stroke, heart disease, diabetes mellitus, hyperlipidemia, musculoskeletal disorders, and cancer. Self-rated health was assessed on a 4-point Likert scale (very good, good, somewhat poor, or poor). Depressive symptoms were assessed using the short version of the 15-item Geriatric Depression Scale [17, 18] and categorized into three groups: none (0–4 points), mild (5–9 points), or moderate to severe (10–15 points). Instrumental activities of daily living were assessed using the Tokyo Metropolitan Institute of Gerontology Index of Competence [19] and classified as good (5 points) or poor (≤ 4 points). Daily walking time was classified into four groups, as follows: <30, 30–59, 60–89, or ≥ 90 min. For the subgroup analysis, the study sample was further classified into two categories based on whether they met the recommended number of steps for older adults (i.e., 6,000–7,000 steps/day, as recommended by the national health promotion program in Japan), as follows: (a) did not meet criteria—walking duration per day < 60 min; and (b) met the criteria—walking duration per day > 60 min [20, 21].
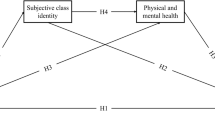
Statistical analyses
Since there was no statistically significant interaction between community-level group sports participation and gender for each mortality outcome, the analysis was conducted on the entire participant population without stratification by gender. The multilevel analysis framework assumes that individual outcomes are influenced in part by the community areas in which individuals reside. In this study, multilevel survival analysis was used to calculate hazard ratios (HRs) and 95% confidence intervals (CIs) for mortality during the follow-up period. The HR of community-level group sports participation was estimated based on a 10-percentage point change in the aggregated percentages of group sports participation. Three multivariate models were employed for the analyses. The crude model included both community-level and individual-level group sports participation, as well as cross-level interaction terms. Model 1 consecutively incorporated age group and gender, while Model 2 sequentially included all covariates except daily walking time. To address potential bias resulting from missing values, multiple imputations were performed under the assumption of missingness at random (i.e., missingness is related to other variables measured in the same survey for each participant). Incomplete variables were imputed using a multivariate normal imputation method. A total of 20 imputed datasets were created, encompassing all variables used in the present analyses. The estimated parameters were combined using Rubin’s combination methods [22, 23]. To ensure the robustness of the results, a sensitivity analysis was conducted by excluding individuals with a history of stroke, heart disease, or cancer at baseline. Additionally, subgroup analyses stratified by daily walking time (i.e., < 60 or ≥ 60 min) were performed. Supplementary analyses were conducted to explore the dose–response relationship between the frequency of individual-level participation in group sports (ref. zero vs. a few times per year, 1–3 days per month, and 1 day per week or more) and each mortality outcome. All statistical analyses were performed using STATA/MP 17.0 (Stata Corp., College Station, TX, USA).
Results
Table 1 summarizes the descriptive data for individual- and community-level variables as well as cumulative mortality. The present study included 43,088 participants, contributing a total of 272,347 person-years. The maximum follow-up duration was 2,709 days, and the mean follow-up duration was 2,309 days. A total of 5,711 deaths (13.3%) were identified, with 1,311 related to CVD and 2,349 related to cancer. The mortality rates per 1,000 persons per year were 21.0 for all-cause mortality, 4.8 for CVD mortality, and 8.6 for cancer mortality. After applying multiple imputations, the estimated group sports participation rate was calculated for each community area. The average participation rate was 28.3%, with a standard deviation of 7.0% and a range of 10.0–52.7%.
Table 2 summarizes the results from the multilevel survival analyses. In the crude model and the models adjusted by gender and age (Model 1), a higher community-level group sports participation rate was associated with a reduced risk of all mortality outcomes. In the fully adjusted model (Model 2), a higher participation rate was significantly associated with a lower risk of all-cause mortality (HR: 0.89, 95% CI: 0.83–0.95) and cancer mortality (HR: 0.89, 95% CI: 0.81–0.98) for every 10% point increase in the participation rate. Individual-level group sports participation was also found to lower the risk of all mortality outcomes across all models. However, no significant cross-level interactions were identified. Supplementary Table 1 presents the results of the sensitivity analysis, excluding participants with a history of stroke, heart disease, or cancer at baseline. Supplementary Table 2 shows the results of the subgroup analyses stratified by daily walking time (i.e., < 60 or ≥ 60 min). These results were comparable to those observed in the main analysis.
Supplementary Table 3 presents the results of supplementary analyses examining the dose–response relationship between the frequency of individual-level participation in group sports and each mortality outcome. Across all causes of mortality, increased frequency of individual-level participation in group sports was associated with a lower mortality risk.
Discussion
To the best of our knowledge, this is the first study to investigate the contextual relationship between the community-level prevalence of group sports participation and mortality among older adults. After adjusting for individual-level group sports participation and potential confounders, a 10-percentage point increase in community-level group sports participation rate was found to be associated with an 11% decrease in the risks of all-cause and cancer-related mortality. The results were found to be robust regardless of the daily walking time. These findings suggest that promoting group sports within the community could be an effective strategy for extending life expectancy, benefiting both those who actively participate in the groups and those who do not.
A study conducted in England found that higher levels of social activity, including participation in sports clubs, at the community level were associated with a reduced risk of all-cause mortality among adults residing in the community [24]. Similar findings were reported in our study of older population in Japan. We hypothesize that the contextual effect of group-level social capital on individual-level health outcomes can be explained through three pathways: social contagion, informal social control, and collective efficacy. Social contagion suggests that behaviors spread more rapidly within tightly knit social networks [7], promoting healthy lifestyle changes such as smoking cessation [25]. Informal social control refers to the ability of individuals in a community to maintain social order, for instance, by intervening when they witness deviant behavior [7]. In the context of this study, group sports participants may encourage older individuals, whether engaged in individual or group-based activities, to engage in more physical activity. Collective efficacy, similar to the concept of self-efficacy at the group level, refers to the collective’s ability to mobilize and take collective action [7, 26]. Communities with numerous group sports and participants may develop facilities, industries, systems, or regulations that promote health and align with the community’s opinions and actions. The widespread participation in group sports at the group level may have positive spillover effects [5]. Based on the transtheoretical model, older adults residing in communities with high group sports participation rates, even if they do not participate themselves, were less likely to be homebound and had higher stages of change for exercise than those residing in communities with low participation rates [11].
In terms of causes of mortality, divergent trends were observed between CVD and cancer. In the case of CVD mortality, the association became less significant in the model adjusted for covariates, whereas it remained significant in the case of cancer-related mortality. This suggests that communities with higher group sports participation rates may have a lower risk of CVD mortality due to “compositional effects.” These effects are associated with residing in communities where a greater proportion of older adults possess favorable individual factors, which were also adjusted for in Model 2 (e.g., socioeconomic status, health behaviors, and health status). In contrast, for cancer-related mortality, the contextual effects identified for all-cause mortality may persist irrespective of these individual factors. A study conducted in Sweden [27], which included all individuals aged 65 and older, demonstrated that low community-level social capital, as measured by voting participation rates, was linked to an elevated risk of cancer, coronary heart disease, and stroke. However, the Swedish report only adjusted for socioeconomic factors such as income, educational level, and marital status, rather than individual health behaviors and status, as was done in the present study. Further research is warranted to elucidate the mechanisms by which the level of social and civic participation at the community level influences the risk of mortality from specific causes.
The present study has several strengths. First, the study included a large sample of older adults from nine municipalities across a diverse range of urban settings nationwide. Second, extensive longitudinal data were obtained from national certification records, resulting in a high follow-up rate over a 7-year period. However, certain limitations should be acknowledged. First, due to the limited number of events, the analysis did not include a detailed breakdown of the causes of mortality for CVD and cancer. It is worth noting that a report of Swedish adults found a consistent negative association between community-level social capital, as measured by voting participation rates, and mortality from lung [28] and colorectal cancers [29] in men and women, as well as prostate cancer [30] in men. Second, the results may be susceptible to selection bias due to the relatively low valid response rate (55.4%). According to a previous study, both the response rate and the percentage of group sports participants were significantly lower among older individuals than among younger individuals [31]. As a result, the participants in this study may have had a relatively lower risk of mortality, potentially underestimating the relationship. Third, the influence of unmeasured confounders, particularly community-level variables that were not adequately accounted for, cannot be ignored. Future investigations into available open data using geographic information systems are required to examine the impact of the physical environment more comprehensively.
Conclusions
After adjusting for individual-level group sports participation and other covariates, older adults residing in communities with higher group sports participation rates have a lower risk of all-cause and cancer-related mortality than those residing in communities with lower group sports participation rates. These findings indicate a contextually preventive association between community-level group sports participation and all-cause and cancer-related mortality among older individuals. The promotion of group sports within a community may be an effective population-based strategy for extending life expectancy, benefiting both those who actively participate in group sports and those who do not.
Data availability
The data generated and/or analysed during the current study are not publicly available due to it sensitive nature and source of origin being the JAGES but are available from the JAGES on reasonable request. Requests for JAGES data can be sent to dataadmin.ml@jages.net.
Abbreviations
- BMI:
-
Body mass index
- CI:
-
Confidence intervals
- CVD:
-
Cardiovascular disease
- HR:
-
Hazard ratios
- JAGES:
-
Japan Gerontological Evaluation Study
References
Kanamori S, Kai Y, Kondo K, Hirai H, Ichida Y, Suzuki K, et al. Participation in sports organizations and the prevention of functional disability in older Japanese: the AGES cohort study. PLoS ONE. 2012;7:e51061.
Kanamori S, Takamiya T, Inoue S, Kai Y, Tsuji T, Kondo K. Frequency and pattern of exercise and depression after two years in older Japanese adults: the JAGES longitudinal study. Sci Rep. 2018;8:11224.
Hayashi T, Kondo K, Kanamori S, Tsuji T, Saito M, Ochi A, et al. Differences in falls between older adult participants in group exercise and those who exercise alone: a cross-sectional study using Japan gerontological evaluation study (JAGES) data. Int J Environ Res Public Health. 2018;15:1413.
Kanamori S, Takamiya T, Inoue S. Group exercise for adults and elderly: determinants of participation in group exercise and its associations with health outcome. J Phys Fit Sports Med. 2015;4:315–20.
Tsuji T, Miyaguni Y, Kanamori S, Hanazato M, Kondo K. Community-level sports group participation and older individuals’ depressive symptoms. Med Sci Sports Exerc. 2018;50:1199–205.
Tsuji T, Kanamori S, Miyaguni Y, Hanazato M, Kondo K. Community-level sports group participation and the risk of cognitive impairment. Med Sci Sports Exerc. 2019;51:2217–23.
Kawachi I, Berkman LF. Social capital, social cohesion, and health. In: Berkman LF, Kawachi I, Glymour MM, editors. Social epidemiology second edition. New York: Oxford University Press; 2014. pp. 290–319.
Coleman J. Foundations of social theory. Cambridge: Harvard University Press; 1990.
Putnam RD. Bowling alone: the collapse and revival of American community. New York: Simon & Schuster; 2000.
Putnam RD, Leonardi R, Nanetti RY. Making democracy work: civic traditions in modern Italy. Princeton, NJ: Princeton University Press; 2013.
Tsuji T, Kanamori S, Miyaguni Y, Kondo K. Community-level sports group participation and health behaviors among older non-participants in a sports group: a multilevel cross-sectional study. Int J Environ Res Public Health. 2021;18:531.
Choi M, Mesa-Frias M, Nuesch E, Hargreaves J, Prieto-Merino D, Bowling A, et al. Social capital, mortality, cardiovascular events and cancer: a systematic review of prospective studies. Int J Epidemiol. 2014;43:1895–920.
Kondo K. Progress in aging epidemiology in Japan: the JAGES project. J Epidemiol. 2016;26:331–6.
Kondo K, Rosenberg M, World Health Organization. Advancing universal health coverage through knowledge translation for healthy ageing: lessons learnt from the Japan Gerontological Evaluation Study. World Health Organization. 2018. https://apps.who.int/iris/handle/10665/279010. Accessed 26 Aug 2023.
Centers for Disease Control and Prevention. International Classification of Diseases, Tenth Revision (ICD-10). https://www.cdc.gov/nchs/icd/icd10.htm. Accessed 26 Aug 2023.
Saito M, Kondo N, Aida J, Kawachi I, Koyama S, Ojima T, et al. Development of an instrument for community-level health related social capital among Japanese older people: the JAGES project. J Epidemiol. 2017;27:221–7.
Burke WJ, Roccaforte WH, Wengel SP. The short form of the Geriatric Depression Scale: a comparison with the 30-item form. J Geriatr Psychiatry Neurol. 1991;4:173–8.
Wada T, Ishine M, Kita T, Fujisawa M, Matsubayashi K. Depression screening of elderly community-dwelling Japanese. J Am Geriatr Soc. 2003;51:1328–9.
Koyano W, Shibata H, Nakazato K, Haga H, Suyama Y. Measurement of competence: reliability and validity of the TMIG Index of competence. Arch Gerontol Geriatr. 1991;13:103–16.
National Institute of Health and Nutrition. Health Japan 21 (the second term) Analysis and Assessment Project. https://www.nibiohn.go.jp/eiken/kenkounippon21/en/index.html. Accessed 19 Feb 2024.
Tsuji I. Current status and issues concerning Health Japan 21 (second term). Nutr Rev. 2022;78:14–7.
Carpenter JR, Kenward MG. Multiple imputation and its application. 1st ed. New York: Wiley; 2013.
Rubin DB. Multiple imputation for nonresponse in surveys. New York: Wiley; 2004.
Mohan J, Twigg L, Barnard S, Jones K. Social capital, geography and health: a small-area analysis for England. Soc Sci Med. 2005;60:1267–83.
Christakis NA, Fowler JH. The collective dynamics of smoking in a large social network. N Engl J Med. 2008;358:2249–58.
Sampson RJ, Raudenbush SW, Earls F. Neighborhoods and violent crime: a multilevel study of collective efficacy. Science. 1997;277:918–24.
Sundquist K, Hamano T, Li X, Kawakami N, Shiwaku K, Sundquist J. Linking social capital and mortality in the elderly: a Swedish national cohort study. Exp Gerontol. 2014;55:29–36.
Hamano T, Li X, Sundquist J, Sundquist K. Neighborhood linking social capital as a predictor of lung cancer: a Swedish national cohort study. Cancer Epidemiol. 2019;61:23–9.
Hamano T, Li X, Sundquist J, Sundquist K. Is neighbourhood linking social capital associated with colorectal cancer incidence and mortality? A national cohort study from Sweden. J Prim Prev. 2021;42:493–510.
Hamano T, Li X, Sundquist J, Sundquist K. Neighborhood social capital and incidence and mortality of prostate cancer: a Swedish cohort study. Aging Clin Exp Res. 2021;33:3333–42.
Kondo K. Exploring inequalities in health: a large-scale social epidemiological survey for care prevention in Japan. Tokyo: Igaku-Shoin Ltd.; 2007.
Acknowledgements
This study used data from the Japan Gerontological Evaluation Study.
Funding
This work was supported by the Japan Society for the Promotion of Science KAKENHI [JP15H01972, JP16K16595, JP19K02200, JP20K19534, JP20H00557, JP21K11108, JP21KK0168, JP21H00848, and JP23H00060]; Health Labour Sciences Research Grant [H28-Choju-Ippan-002]; Japan Agency for Medical Research and Development [JP18dk0110027, JP18ls0110002, JP18le0110009, JP20dk0110034, JP21lk0310073, JP21dk0110037, and JP22lk0310087]; Open Innovation Platform with Enterprises, Research Institute and Academia [JPMJOP1831]; JST RISTEX Japan [JPMJRS22B1]; Innovative Research Program on Suicide Countermeasures [1-4]; Sasakawa Sports Foundation; Japan Health Promotion & Fitness Foundation; Chiba Foundation for Health Promotion & Disease Prevention; the 8020 Research Grant for fiscal 2019 from the 8020 Promotion Foundation [adopted number 19-2-06], Meiji Yasuda Life Foundation of Health and Welfare; Research Funding for Longevity Sciences from National Center for Geriatrics and Gerontology [29-42, 30-22, 20-19, and 21-20]. The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the respective funding organizations.
Author information
Authors and Affiliations
Contributions
TT conceived and designed the study, collected, analyzed, and interpreted the data, and wrote the article; EO, MS, MY, MH, and TO collected the data and critically revised the article; SK critically revised the article; and KK collected the data, critically revised the article, and was the principal investigator for the JAGES. All authors have read and approved the final version of the manuscript and agree with the order of presentation of the authors.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The current study was conducted in accordance with the principles of the Helsinki Declaration and approved by the Ethics Committee, Chiba University, Japan (approval number: 2493), and the National Center for Geriatrics and Gerontology, Japan (approval number: 992-3). All participants were informed about the voluntary nature of their participation and indicated their consent by completing and returning the questionnaire via mail. This study adhered to the STROBE checklist (Supplementary Table 4).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Tsuji, T., Okada, E., Saito, M. et al. Community-level group sports participation and all-cause, cardiovascular disease, and cancer mortality: a 7-year longitudinal study. Int J Behav Nutr Phys Act 21, 44 (2024). https://doi.org/10.1186/s12966-024-01592-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12966-024-01592-9