Abstract
Background
Women’s physical activity varies across the adult lifespan. However, changes in physical activity among mid-aged women are not well understood. We analysed 21 years of data from women born in 1946–51 to identify: (1) trajectories of physical activity in the transition from mid- to old-age and (2) determinants of different physical activity trajectories.
Methods
Data were from the 1946–51 cohort of the Australian Longitudinal Study on Women’s Health (N = 10,371). Surveys were mailed at three-year intervals from 1998 (age 47–52) to 2019 (age 68–73) to collect data on physical activity, sociodemographic factors (country of birth, area of residence, educational attainment, marital status, income management, paid work hours, living with children age < 18, providing care), health indicators (menopause status, BMI, physical and mental health, chronic conditions), and health behaviours (smoking, alcohol status). Group-based trajectory modelling was used to identify trajectories of physical activity. Multinomial logistic regression models were used to examine the determinants of physical activity trajectories.
Results
Five trajectories were identified: Low-stable (13.3% of participants), Moderate-stable (50.4%), Moderate-increasing (22.2%), High-declining (7.7%), and High-stable (6.6%). Sociodemographic characteristics (area of residence, education, income management, living with children, and providing care) were determinants of physical activity trajectories, but the strongest factors were BMI, physical and mental health. Women who were overweight/obese and had poor physical and mental health were less likely to be in the High-stable group than in any other group. Changes in these variables (increasing BMI, and declining physical and mental health) and in marital status (getting married) were positively associated with being in trajectories other than the High-stable group.
Conclusions
Although most women maintained physical activity at or above current guidelines, very low physical activity levels in the Low-stable group, and declining levels in the High-declining group are concerning. The data suggest that physical activity promotion strategies could be targeted to these groups, which are characterised by socioeconomic disadvantage, high (and increasing) BMI, and poor (and worsening) physical and mental health. Removing barriers to physical activity in these women, and increasing opportunities for activity, may reduce chronic disease risk in older age.
Similar content being viewed by others
Introduction
Physical activity (PA) is a well-known protective factor for chronic diseases and functional decline [1,2,3]. Recent studies have reported that higher PA in the transition from mid to older age reduces the risk of adverse health outcomes in later life [4,5,6,7]. This is important because the worldwide economic burden of physical inactivity is significant; inactivity cost healthcare systems $53.8 billion in 2013 [8], and the cost of inaction on physical inactivity reaches $47.6 billion annually [9]. Furthermore, as the risks of physical inactivity [10], multimorbidity [11], and dementia [12] are higher in women than in men, developing public health strategies to promote women’s PA during midlife is vital to reducing gender inequity and improving population health.
Many previous studies have investigated the correlates and determinants of PA in various populations, and have identified individual demographic, psychological, social, and environmental factors that affect PA levels [13,14,15,16]. Although some socioeconomic factors are common determinants of PA in men and women [17], other sociodemographic factors, such as living with children, may affect men and women differently, due to socially structured gender roles [18, 19]. Most of the documented determinants of PA relate to the availability of ‘free time’ (e.g., paid work and caring responsibilities) as well as motivation and ability to access activity opportunities, which reflect an array of factors relating to socioeconomic status, education, social support, living and working environments, and health [14]. In this mid-age cohort, menopause, which is known to affect health [20], may also affect PA.
Understanding these determinants during mid-age is important for developing interventions that will help women maintain PA levels at this life stage, and keep them above the disability threshold as they age [21]. However, most studies have measured PA at a single time point [22, 23], even though baseline measures of some sociodemographic factors, health indicators, and health behaviours may change over time [24]. For example, there may be changes in marital status, work hours, and provision of care for children and other family members, all of which impact discretionary time, and are associated with levels of PA [19, 25]. In mid-age, increasing body mass index (BMI) and declining physical and mental health may also be associated with changing patterns of PA [25, 26].
Previous research with women has shown that at the group level, PA increases in mid-age and rapidly declines in older age [27, 28]. However, at the individual level, there may be different PA trajectories at this life stage, which may be influenced by socioeconomic and health characteristics. Although data from the British Regional Heart study have been used to show trajectories of PA in British men across 20 years [29], little is known about individual trajectories of PA in women during the transition from mid-age to early old age. To our knowledge, no previous studies have examined associations between changing sociodemographic and health factors, and trajectories of PA in mid-older women.
Therefore, in this study, we used 21 years of data from a nationally representative cohort of Australian women born in 1946–51 to identify: (1) different PA trajectories in the transition from mid- to early old age; and (2) associations of sociodemographic, behavioural and health factors, and changes in these, with the different PA trajectories.
Methods
Study participants
We used data from the 1946–51 cohort of the Australian Longitudinal Study on Women’s Health (ALSWH), an ongoing prospective study [30]. Participants were randomly selected from women born in 1946–51 who were registered with Australia’s universal health insurance system (Medicare), which helps to pay for out-of-hospital health services. The Medicare database includes almost all Australian citizens and some temporary residents [31].
The baseline survey was mailed in 1996 (Survey 1) when participants were 45–50 years (N = 13,714), and the recruited participants were generally representative of women the same age in the Australian population [31, 32]. Eight follow-up surveys were mailed at three-year intervals from 1998 (age 47–52) to 2019 (age 68–73). Further details of recruitment methods, response rates and data collection have been described elsewhere [30], and full details of the study can be found at http://www.alswh.org.au. All participants consented to join the ALSWH study, which has ethical approval from the Human Research Ethics Committees (HRECs) of the Universities of Newcastle and Queensland (approval number 2004000224).
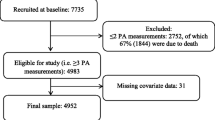
Because the PA measure used in 1996 (Survey 1) was different from those in the following surveys, and to minimise bias in identifying trajectories, only data from women who were enrolled in the cohort in 1996 and then completed at least four additional follow-up surveys from 1998 to 2019 were included in the analyses (N = 10,371).
Physical activity
PA was assessed using the modified self-administered version of the Active Australia Survey, which has acceptable reliability and validity among mid-aged women [33]. In each survey, participants reported time spent in the previous week in walking briskly (‘for recreation or exercise or to get to or from places’), moderate leisure-time physical activities (‘like social tennis, moderate exercise classes, recreational swimming, dancing’), and vigorous leisure-time activities (‘like aerobics, competitive sport, vigorous cycling, running, swimming’). Minutes per week spent in each activity were multiplied by a metabolic equivalent (MET) score (3.33 for walking and moderate intensity activity and 6.66 for vigorous activity), and MET.minutes/week were summed to provide total weekly PA. A threshold of 500 MET.minutes/week was used to define meeting the lower range of the current PA guidelines [1, 34]. This is equivalent to 150 min at 3.33 METs or 75 min at 6.66 METs, or various combinations of walking, moderate, and vigorous activity, as described in the 2014 report on the revision of Australia's Physical Activity Guidelines [34]. Outliers (defined as > 3321.7 MET.minutes/week [1.5 times the interquartile range [IQR] above the 75th percentile]) were truncated to 3321.7 MET.minutes/week.
Potential determinants of different PA trajectories
Since a wide range of factors influence PA levels [13,14,15,16], and some of these change over time [24], we selected sociodemographic, behavioural and health characteristics at age 47–52, which have been shown in previous studies to have significant associations with PA [14, 19, 25], and changes in the variables from age 47–52 to 56–61, as the potential determinants of PA trajectories.
Sociodemographic, behavioural and health characteristics at age 47–52
Sociodemographic, behavioural and health characteristics were reported and measured at age 47–52 and categorised as shown in Table 1. The complete list of variables is shown in Supplementary table 1. Sociodemographic characteristics included country of birth, area of residence, educational attainment, marital status, ability to manage on income, weekly paid work hours, living with children age < 18, providing care for grandchildren, and providing care for someone with long-term illness, disability, or frailty. Household income was not included because its missing rate was high (27.9%). Instead, ability to manage on income (missing rate: 6.8%), which is correlated with PA, was used as a proxy for financial stability [35]. Menopause status was determined using questions about hysterectomy, oophorectomy, hormone treatment, and menstrual pattern [36], and categorised as shown in Table 1. We used reported height and weight to calculate BMI [37], which was categorised as underweight (< 18.5 kg/m2), normal weight (18.5–24.9 kg/m2), overweight (25.0–29.9 kg/m2), or obese (≥ 30.0 kg/m2) following the WHO recommendation [38]. Physical health (PH) and mental health (MH) were assessed using the component summary scores from the SF-36 questionnaire, categorised in quartiles [39, 40]. Number of chronic conditions was from a list which included: type 2 diabetes, heart disease, hypertension, stroke, low iron level, asthma, bronchitis/emphysema, osteoporosis, breast cancer, cervical cancer, skin cancer, depression, and anxiety, categorised as 0, 1, 2 or ≥ 3. Smoking and alcohol habits, based on frequency and quantity of tobacco use and alcohol consumption, and frequency of short-term risk drinking [41], were categorised as shown in Table 1.
Changes in sociodemographic, behavioural and health characteristics from Survey 2 (age 47–52) to Survey 5 (age 56–61).
Variables indicating changes in area of residence, marital status, ability to manage on income, paid work hours, living with children age < 18, provision of care for grandchildren or someone requiring care, BMI, PH, MH, smoking status, and alcohol status, from age 47–52 (Survey 2, 1998) to 56–61 (Survey 5, 2007) were created and categorised as shown in Tables 3 and 5.
Statistical analysis
Physical activity trajectories
Group-based trajectory modelling was used to identify clusters of women who followed a similar trajectory of PA over 21 years using the STATA plugin traj [42]. The number of groups (2–5) and polynomials (linear, quadratic, cubic) were determined based on goodness-of-fit of the model. The best-fit model was selected using Bayesian information criterion (BIC), Akaike information criterion (AIC), and log-likelihood. The adequacy of the model was confirmed based on the following criteria: posterior probabilities of group membership (> 0.7 probability of an individual belonging to each of the trajectory groups); the odds of correct classification > 5 [43]. Full information maximum likelihood estimation was used for the group-based trajectory modelling to account for missing data, assuming these were missing at random.
Determinants of different physical activity trajectories
We conducted analyses to elucidate the trajectories of (a) probability of meeting the PA recommendation (≥ 500 MET.minutes/week) [1, 34], and (b) total PA (MET.minutes/week). However, as the adequacy of the model examining trajectories of meeting guidelines (a) was not acceptable (due to poor posterior probabilities, < 0.7) (Supplementary Fig. 1 and Supplementary table 2), we did not conduct analyses to examine the determinants of meeting guidelines.
Multinomial logistic regression models were conducted to investigate the association of sociodemographic, behavioural and health characteristics at age 47–52, and changes in selected variables from age 47–52 to 56–61, with PA trajectories. For this, the R package nnet was used [44]. The models were adjusted for age and PA trajectory was the dependent variable. Independent variables were (1) sociodemographic factors, health indicators and health behaviours at age 47–52, and (2) changes in explanatory factors from age 47–52 to 56–61. These variables were included using a hierarchical model in two blocks, with variables from the first block retained for the next stage if the p-value was ≤ 0.20. Each odds ratio (OR) was calculated by dividing the odds of being in one trajectory group (e.g., Low-stable, compared with High-stable) in each category of the exposure variable (e.g., higher degree) by the odds of being in these groups (e.g., Low-stable vs High-stable) in the referent category (e.g., < 12 years education) of the exposure variable. ORs < 1/ > 1 indicate that the participants in one category of the exposure group (i.e., higher degree) are, respectively, less likely/more likely than the reference group (e.g., < 12 years of education) to be in each trajectory group, compared with the High-stable group.
The proportion of participants with missing values in the full model, which included sociodemographic, behavioural and health characteristics at age 47–52 and changes in variables from age 47–52 to 56–61 was 41.4%; this was largely due to failure to respond to one complete survey. As missing at random (MAR) is likely in many situations [45], we used a multiple imputation procedure which handles not only MAR but also missing completely at random and missing not at random [45], and conducted multiple imputations, using the R package MICE [46]. Fifty data sets were created, and the combined ORs and 95% confidence intervals (CI) of each data set were used to obtain the estimates.
Group-based trajectory modelling was carried out using STATA 16.0 (StataCorp, Texas, USA). Multinomial logistic regression models and multiple imputation were conducted using R 3.6.3 (R Foundation for Statistical Computing, Vienna, Austria).
Results
Of the 13,714 women in the original cohort, data from 10,371 (75.6%) were included in this analysis; 6,969 participants provided valid responses to all surveys. The comparison of characteristics at age 47–52 of the analytic and non-analytic samples is shown in Table 1. Because of the large sample size, there were small but statistically significant differences in most characteristics (except age, living with children, and providing care for someone requiring care) between women whose data were and were not included in the analyses. However, with the exception of education, there were no meaningful differences in the characteristics of the women in analytic and non-analytic samples (Table 1).
PA trajectories from age 47–52 to 68–73 are shown in Fig. 1. Model fitting and adequacy are shown in Supplementary table 2. We selected the five trajectories of the cubic polynomials model, which met the adequacy criteria; posterior probabilities ranged from 0.741 to 0.865, and the odds of correct classification ranged from 5.32 to 90.25 (Supplementary table 3). PA trajectories were labelled Low-stable (13.3% of participants), Moderate-stable (50.4%), Moderate-increasing (22.2%), High-declining (7.7%), and High-stable (6.6%) (Fig. 1).
Box plots in Fig. 2 are used to show the medians and IQRs of PA at each survey for each of the PA trajectories, and the data are shown in Table 2. Medians of PA values in the Low-, Moderate-, and High-stable trajectory groups were fairly consistent over time. In the Low-stable group, median PA was zero at every survey from age 50–55. In the Moderate-stable group, median PA was between 400 and 600 MET.minutes/week at each survey. Median PA in the High-stable group was > 2000 MET.minutes/week at every survey and close to 3000 MET.minutes/week at age 59–64.
In contrast with the three ‘stable’ trajectories (Low, Moderate, and High), median PA in the High-declining group declined markedly, from 2647 MET.minutes/week at 47–52 years to 799 MET.minutes/week at age 68–73, while in the Moderate-increasing group, PA increased from 799 MET.minutes/week at age 47–52 to a high of 1798 MET.minutes/week at age 62–70 years (Fig. 2 and Table 2).
Characteristics of the participants in each trajectory group are shown in Table 3, and the ORs for being in each group, compared with the High-stable PA group, are shown in Tables 4 (characteristics at age 47–52) and 5 (changes in explanatory variables). As expected, demographic characteristics, such as education, ability to manage on income, and living with children, varied across the Low, Moderate and High trajectory groups. For example, women with any post-school education were less likely to be in the Low-stable trajectory group, and those with a university degree were also less likely to be in the High-declining group (than the High-stable group). When compared with those in the High-stable group, women who reported always having difficulty managing on income were over-represented in every group, and those who were living with children were more likely to be in the Moderate-stable or Moderate-increase trajectory groups. Women in paid work, and those who were post-menopause, were less likely to be in the High-declining trajectory group, and those who lived in an outer regional area, and provided care for grandchildren (occasionally) were more likely to be in the High-declining group (than the High-stable group).
BMI, PH and MH were strong determinants of PA trajectory. Compared with being in the High-stable group, women who were overweight or obese and those in the lower PH and MH quartiles were over-represented in every other trajectory group.
There were few significant associations between changes in these determinants and PA trajectory group (Table 5). Compared with the High-stable group, women who married between age 47–52 and 56–61 were over-represented in the Low-, Moderate-stable and Moderate-increasing groups, while those who reported adverse changes in managing on income (easy to difficult) were more likely to be in the High-declining group. Women who started paid work were less likely to be in the Low-stable group. Women who changed from normal or overweight to obese were more likely to be in the Low-stable, Moderate-stable, and High-declining groups, and those with declining PH and MH were more likely to be in the Low- and Moderate-stable groups. Conversely, those whose health improved were less likely to be in the Low- and Moderate-stable groups (Table 5).
Discussion
Our aims were to identify different PA trajectories in the transition from mid- to early old age, and the associations of sociodemographic and health factors, and changes in these, with the trajectories. Using data which spanned 21 years (when the women were between 47–52 and 68–73 years), we identified five PA distinct trajectories. The majority of women (70%) maintained fairly consistent PA levels over time, but with starkly contrasting median PA of zero (Low-stable), 400–600 MET.minutes/week (Moderate-stable), or 2000–3000 MET.minutes/week (High-stable). PA levels in the Moderate-stable group are commensurate with meeting the lower range of the current PA guidelines (150 min/week of moderate-to-vigorous PA [MVPA] ≈ 500 MET.minutes/week), and in the High-stable group are well above the upper range of the recommendation (300 min/week of MVPA or 1000 MET.minutes/week) [1, 34].
Two trajectories of changing PA were also identified; one small group (8% of the participants) whose initially high PA levels (> 2000 MET.minutes/week) declined markedly over time to around 800 MET.minutes/week; and a larger group (22%), whose initially moderate PA levels (around 800 MET.minutes/week) increased to almost 1800 MET.minutes/week by the age of 70. It is notable that median PA levels in every trajectory group (except the Low group – 0 MET.minutes/week) declined after age 70. Since lower PA increases the risk of adverse health outcomes [4], removing barriers to PA among mid-aged women with low or declining trajectories, and increasing opportunities for PA, may increase PA levels and consequently reduce chronic disease risk in older age [1, 3, 5].
These five trajectories contrast with the three relatively stable trajectories described for men using data from the British Regional Heart study [29]. The difference may reflect the fact that the British researchers conducted their first follow-up survey 12 years after baseline, and may have missed any earlier increases or decreases in PA, such as those we saw in about one-third of our sample during the first 12 years of follow-up in this ALSWH study.
When we examined the determinants of the different trajectories using the data from surveys 2 (age 47–52) and 5 (age 56–61), we found that BMI, and health were the strongest determinants of PA trajectories, especially in the Low-stable trajectory group where PA levels were remarkably low. Our findings clearly show markedly lower levels of overweight and obesity, and better PH and MH in the High-stable trajectory group. Moreover, women with increasing BMI were over-represented in three trajectory groups (Low-stable, Moderate-stable and High-declining) but not in the Moderate-increasing and High-stable groups. This is consistent with previous analyses of ALSWH data which illustrate the current weight gain epidemic in Australia, and indicates that women with high levels of PA are protected against high weight gain [47]. Worsening PH and MH were most marked in the Low- and Moderate-stable groups.
Many sociodemographic characteristics (including area of residence, education, ability to manage on income, hours of paid work, living with children, and caring duties) were also associated with the PA trajectories. Some of these associations were in line with expectations, while others were counter-intuitive. For example, as expected from our own and others’ research [15, 19], providing care (for grandchildren or others) was associated with declining PA. However, our findings on living with children (more likely in both the moderate-stable and increasing groups) and paid work (less likely in the declining group) point to the complex relationships between women’s paid work and caring roles, and PA patterns [48]. It is possible that women in paid work (with and without children) may have more opportunities and resources to support their leisure time activities.
Despite the fact that PA improves psychological well-being and sleep quality among menopausal women [49, 50], menopause symptoms may be a barrier to remaining active at this life stage. There were, however, few indications that menopause was associated with PA trajectory, except that the High-declining group were less likely to be post-menopausal.
Strengths and limitations
The main strength of this study is that we used data from a nationally representative cohort with 21 years of follow-up. The ALSWH data, which were collected from 8 surveys at three-year intervals, provide a rare opportunity to examine long-term PA trajectories and the potential for non-linear changes over time. Another strength was that, in addition to the potential sociodemographic and health determinants of the trajectories, we assessed associations with changes in determinants over the first 12 years of follow-up.
The study has several limitations. First, participants with PA data from fewer than four surveys were excluded from the primary analysis, which may have introduced selection bias. However, we confirmed that the characteristics of the analytic and non-analytic samples were similar. One exception was for educational attainment, with over-representation of women with a University degree. This may explain the higher prevalence of meeting PA guidelines at age 47–52 in this cohort (54.6%), than in national survey estimates (44.1% for women age 45–54) [51]. However, the ALSWH women were age 47–52 in 1998, so our data may not be directly comparable with data from women of the same age today, due to modern day secular influences (period effects) [52]. We also acknowledge that the two groups may have differed in terms of unmeasured characteristics that may influence physical activity. Second, we obtained PA data using a self-reported questionnaire, which focuses mostly on leisure-time activity and recreational and transport-related walking. It does not include work-related activities [33]. Although self-report surveys may overestimate PA, our survey has acceptable reliability and validity [33, 53] and does not overestimate activity to the same extent as other self-report measures [53, 54]. Although use of accelerometers or Global Positioning System devices may reduce measurement bias, use of these devices to assess PA in 10,000 participants at three-year intervals for 21 years would be logistically and financially challenging. In any event, these measures were not widely available when the study began [55], and it is important to use the same PA measure over time in prospective studies [56]. Self-report may also introduce error in other variables, especially BMI. Although we have shown acceptable reliability and validity for the BMI measure in our cohort [37], we acknowledge that underweight women are more likely to over-report, and obese women tend to under-report their weight [37], and that there may be unreported changes in height at this life stage [57]. We accounted for missing values for height using protocols developed by the ALSWH researchers [58]. Third, we acknowledge that there may be complex bidirectional associations between BMI and health variables with PA, and that reverse causality cannot be ruled out [59]. However, our aim was to investigate predictors of PA trajectories, not causal relationships. Finally, although we used a wide range of sociodemographic, behavioural and health characteristics, additional potential determinants of PA trajectories may have been omitted.
Conclusions
Trajectories of PA appear to remain stable, at low, moderate, or high levels, for the majority of mid-aged women. However, around 30% show marked changes in PA at this life stage (22% increasing and 8% declining). Our findings are encouraging, because most women maintained PA levels at or above current guidelines, and the ‘increasers’ seemed to be overcoming known constraints to PA, such as living with children, or caring for grandchildren. Of concern were the very low levels of PA in the Low-stable group, and the declining levels in the High-declining group, which, if maintained, are likely to increase the risk of adverse health outcomes [4, 60]. Increasing BMI and worsening health were notable in the low, moderate and declining PA trajectory groups. Our data suggest that promotion strategies, which address barriers to PA and increase capability, motivation, and opportunities [61] should be targeted to women with low or declining PA in mid-age, for improved health in older age [1, 3].
Availability of data and materials
The dataset analysed in this study was provided by The Australian Longitudinal Study of Women’s Health. Information on how to access the data can be found at https://www.alswh.org.au/how-to-access-the-data/alswh-data.
Abbreviations
- AIC:
-
Akaike information criterion
- BIC:
-
Bayesian information criterion
- BMI:
-
Body mass index
- CI:
-
Confidence interval
- HRT:
-
Hormone replacement therapy
- IQR:
-
Interquartile range
- MH:
-
Mental health
- OCP:
-
Oral contraceptive
- OR:
-
Odds ratio
- PA:
-
Physical activity
- PH:
-
Physical health
References
Bull FC, Al-Ansari SS, Biddle S, Borodulin K, Buman MP, Cardon G, et al. World Health Organization 2020 Guidelines on physical activity and sedentary behaviour. Br J Sports Med. 2020;54(24):1451–62. https://doi.org/10.1136/bjsports-2020-102955.
Rovio S, Kåreholt I, Helkala EL, Viitanen M, Winblad B, Tuomilehto J, et al. Leisure-time physical activity at midlife and the risk of dementia and Alzheimer’s disease. Lancet Neurol. 2005;4(11):705–11. https://doi.org/10.1016/s1474-4422(05)70198-8.
Bauman A, Merom D, Bull FC, Buchner DM, Fiatarone Singh MA. Updating the evidence for physical activity: Summative reviews of the epidemiological evidence, prevalence, and interventions to promote “active aging.” Gerontologist. 2016;56(Suppl 2):S268–80. https://doi.org/10.1093/geront/gnw031.
Mok A, Khaw KT, Luben R, Wareham N, Brage S. Physical activity trajectories and mortality: population based cohort study. BMJ. 2019;365:l2323. https://doi.org/10.1136/bmj.l2323.
Ahmadi MN, Inan-Eroglu E, Mishra GD, Salis A, Stamatakis E. Associations of changes in physical activity and diet with incident obesity and changes in adiposity: Longitudinal findings from the UK Biobank. Prev Med. 2023;168:107435. https://doi.org/10.1016/j.ypmed.2023.107435.
Yang Y, Dixon-Suen SC, Dugué PA, Hodge AM, Lynch BM, English DR. Physical activity and sedentary behaviour over adulthood in relation to all-cause and cause-specific mortality: a systematic review of analytic strategies and study findings. Int J Epidemiol. 2022;51(2):641–67. https://doi.org/10.1093/ije/dyab181.
Gomes GAO, Brown WJ, Codogno JS, Mielke GI. Twelve year trajectories of physical activity and health costs in mid-age Australian women. Int J Behav Nutr Phys Act. 2020;17(1):101. https://doi.org/10.1186/s12966-020-01006-6.
Ding D, Lawson KD, Kolbe-Alexander TL, Finkelstein EA, Katzmarzyk PT, van Mechelen W, et al. The economic burden of physical inactivity: a global analysis of major non-communicable diseases. The Lancet. 2016;388(10051):1311–24. https://doi.org/10.1016/S0140-6736(16)30383-X.
Santos AC, Willumsen J, Meheus F, Ilbawi A, Bull FC. The cost of inaction on physical inactivity to public health-care systems: a population-attributable fraction analysis. Lancet Glob Health. 2023;11(1):e32–9. https://doi.org/10.1016/S2214-109X(22)00464-8.
Mielke GI, da Silva ICM, Kolbe-Alexander TL, Brown WJ. Shifting the Physical Inactivity Curve Worldwide by Closing the Gender Gap. Sports Med. 2018;48(2):481–9. https://doi.org/10.1007/s40279-017-0754-7.
Abad-Díez JM, Calderón-Larrañaga A, Poncel-Falcó A, Poblador-Plou B, Calderón-Meza JM, Sicras-Mainar A, et al. Age and gender differences in the prevalence and patterns of multimorbidity in the older population. BMC Geriatr. 2014;14(1):75. https://doi.org/10.1186/1471-2318-14-75.
Chêne G, Beiser A, Au R, Preis SR, Wolf PA, Dufouil C, et al. Gender and incidence of dementia in the Framingham Heart Study from mid-adult life. Alzheimers Dement. 2015;11(3):310–20. https://doi.org/10.1016/j.jalz.2013.10.005.
Trost SG, Owen N, Bauman AE, Sallis JF, Brown W. Correlates of adults’ participation in physical activity: review and update. Med Sci Sports Exerc. 2002;34(12):1996–2001. https://doi.org/10.1097/00005768-200212000-00020.
Uijtdewilligen L, Peeters GM, van Uffelen JG, Twisk JW, Singh AS, Brown WJ. Determinants of physical activity in a cohort of young adult women. Who is at risk of inactive behaviour? J Sci Med Sport. 2015;18(1):49–55. https://doi.org/10.1016/j.jsams.2014.02.005.
Giles-Corti B, Donovan RJ. The relative influence of individual, social and physical environment determinants of physical activity. Soc Sci Med. 2002;54(12):1793–812. https://doi.org/10.1016/s0277-9536(01)00150-2.
Koeneman MA, Verheijden MW, Chinapaw MJ, Hopman-Rock M. Determinants of physical activity and exercise in healthy older adults: a systematic review. Int J Behav Nutr Phys Act. 2011;8:142. https://doi.org/10.1186/1479-5868-8-142.
Hosseinpoor AR, Stewart Williams J, Amin A, Araujo de Carvalho I, Beard J, Boerma T, et al. Social determinants of self-reported health in women and men: understanding the role of gender in population health. PLoS One. 2012;7(4):e34799. https://doi.org/10.1371/journal.pone.0034799.
Ballantyne PJ. The social determinants of health: a contribution to the analysis of gender differences in health and illness. Scand J Public Health. 1999;27(4):290–5.
Brown WJ, Heesch KC, Miller YD. Life events and changing physical activity patterns in women at different life stages. Ann Behav Med. 2009;37:294–305. https://doi.org/10.1007/s12160-009-9099-2.
Davis SR, Lambrinoudaki I, Lumsden M, Mishra GD, Pal L, Rees M, et al. Menopause Nat Rev Dis Primers. 2015;1:15004. https://doi.org/10.1038/nrdp.2015.4.
Peeters G, Dobson AJ, Deeg DJ, Brown WJ. A life-course perspective on physical functioning in women. Bull World Health Organ. 2013;91(9):661–70. https://doi.org/10.2471/blt.13.123075.
Ding D, Ramirez Varela A, Bauman AE, Ekelund U, Lee IM, Heath G, et al. Towards better evidence-informed global action: lessons learnt from the Lancet series and recent developments in physical activity and public health. Br J Sports Med. 2020;54(8):462–8. https://doi.org/10.1136/bjsports-2019-101001.
Hamer M, Kivimaki M, Steptoe A. Longitudinal patterns in physical activity and sedentary behaviour from mid-life to early old age: a substudy of the Whitehall II cohort. J Epidemiol Community Health. 2012;66(12):1110–5. https://doi.org/10.1136/jech-2011-200505.
Mielke GI. Relevance of Life Course Epidemiology for Research on Physical Activity and Sedentary Behavior. J Phys Act Health. 2022;19(4):225–6. https://doi.org/10.1123/jpah.2022-0128.
Pavey TG, Kolbe-Alexander TL, Uijtdewilligen L, Brown WJ. Which Women are Highly Active Over a 12-Year Period? A Prospective Analysis of Data from the Australian Longitudinal Study on Women’s Health. Sports Med. 2017;47(12):2653–66. https://doi.org/10.1007/s40279-017-0732-0.
Greendale GA, Sternfeld B, Huang M, Han W, Karvonen-Gutierrez C, Ruppert K, et al. Changes in body composition and weight during the menopause transition. JCI Insight. 2019;4(5). https://doi.org/10.1172/jci.insight.124865.
Shaw BA, Liang J, Krause N, Gallant M, McGeever K. Age differences and social stratification in the long-term trajectories of leisure-time physical activity. J Gerontol B Psychol Sci Soc Sci. 2010;65(6):756–66. https://doi.org/10.1093/geronb/gbq073.
Brown WJ, Pavey T. Physical Activity in Mid-Age and Older Women : Lessons from the Australian Longitudinal Study on Women’ s Health. Kinesiology Review. 2016;5(1):87–97. https://doi.org/10.1123/kr.2015-0057.
Aggio D, Papachristou E, Papacosta O, Lennon LT, Ash S, Whincup PH, et al. Trajectories of self-reported physical activity and predictors during the transition to old age: a 20-year cohort study of British men. Int J Behav Nutr Phys Act. 2018;15(1):14. https://doi.org/10.1186/s12966-017-0642-4.
Dobson AJ, Hockey R, Brown WJ, Byles JE, Loxton DJ, McLaughlin D, et al. Cohort Profile Update: Australian Longitudinal Study on Women’s Health. Int J Epidemiol. 2015;44(5):1547–47a-47f. https://doi.org/10.1093/ije/dyv110.
Brown WJ, Bryson L, Byles JE, Dobson AJ, Lee C, Mishra G, et al. Women’s Health Australia: recruitment for a national longitudinal cohort study. Women Health. 1998;28(1):23–40. https://doi.org/10.1300/j013v28n01_03.
Lee C, Dobson AJ, Brown WJ, Bryson L, Byles J, Warner-Smith P, et al. Cohort Profile: the Australian Longitudinal Study on Women’s Health. Int J Epidemiol. 2005;34(5):987–91. https://doi.org/10.1093/ije/dyi098.
Brown WJ, Burton NW, Marshall AL, Miller YD. Reliability and validity of a modified self-administered version of the Active Australia physical activity survey in a sample of mid-age women. Aust N Z J Public Health. 2008;32(6):535–41. https://doi.org/10.1111/j.1753-6405.2008.00305.x.
Brown WJ, Bauman AE, Bull FC, Burton NW. Development of Evidence-based Physical Activity Recommendations for Adults (18–64 years). Available from: https://www.health.gov.au/sites/default/files/documents/2021/03/development-of-evidence-based-physical-activity-for-adults-18-to-64-years.pdf. Accessed Sept 2023.
Peeters G, Beard JR, Deeg DJH, Tooth LR, Brown WJ, Dobson AJ. Longitudinal associations between lifestyle, socio-economic position and physical functioning in women at different life stages. Eur J Ageing. 2019;16(2):167–79. https://doi.org/10.1007/s10433-018-0484-1.
Berecki-Gisolf J, Begum N, Dobson AJ. Symptoms reported by women in midlife. Menopause. 2009;16(5):1021–9. https://doi.org/10.1097/gme.0b013e3181a8c49f.
Burton NW, Brown W, Dobson A. Accuracy of body mass index estimated from self-reported height and weight in mid-aged Australian women. Aust N Z J Public Health. 2010;34(6):620–3. https://doi.org/10.1111/j.1753-6405.2010.00618.x.
Australian Longitudinal Study on Women’s Health. Body mass index – Young and Mid-aged. Available from: https://alswh.org.au/wp-content/uploads/2020/08/DDSSection3BMI.pdf. Accessed Sept 2023.
Brazier JE, Harper R, Jones NM, O’Cathain A, Thomas KJ, Usherwood T, et al. Validating the SF-36 health survey questionnaire: new outcome measure for primary care. BMJ. 1992;305(6846):160–4. https://doi.org/10.1136/bmj.305.6846.160.
Mishra GD, Hockey R, Dobson AJ. A comparison of SF-36 summary measures of physical and mental health for women across the life course. Qual Life Res. 2014;23(5):1515–21. https://doi.org/10.1007/s11136-013-0586-3.
National Health and Medical Research Council. Australian Guidelines to Reduce Health Risks from Drinking Alcohol. . Available from: https://www.nhmrc.gov.au/about-us/publications/australian-guidelines-reduce-health-risks-drinking-alcohol#download. Accessed Nov 2023.
Jones BL, Nagin DS. A Stata Plugin for Estimating Group-Based Trajectory Models. Available from: https://kilthub.cmu.edu/articles/journal_contribution/A_Stata_Plugin_for_Estimating_Group-Based_Trajectory_Models/6470963. Accessed 4 Oct 2022.
Nagin DS, Odgers CL. Group-based trajectory modeling in clinical research. Annu Rev Clin Psychol. 2010;6:109–38. https://doi.org/10.1146/annurev.clinpsy.121208.131413.
Venables WN, Ripley BD. Modern Applied Statistics with S; 2002.
Pedersen AB, Mikkelsen EM, Cronin-Fenton D, Kristensen NR, Pham TM, Pedersen L, et al. Missing data and multiple imputation in clinical epidemiological research. Clin Epidemiol. 2017;9:157–66. https://doi.org/10.2147/clep.S129785.
Buuren Sv, Groothuis-Oudshoorn K. MICE: Multivariate imputation by chained equations in R. Journal of Statistical Software. 2011;45(3). https://doi.org/10.18637/jss.v045.i03.
Brown WJ, Flores TR, Keating SE, Mielke GI. Trajectories and determinants of weight gain in two cohorts of young adult women born 16 years apart. Int J Obes (Lond). 2021;45(7):1553–64. https://doi.org/10.1038/s41366-021-00819-0.
Miller YD, Brown WJ. Determinants of Active Leisure for Women with Young Children—an “Ethic of Care” Prevails. Leis Sci. 2005;27(5):405–20. https://doi.org/10.1080/01490400500227308.
Hybholt M. Psychological and social health outcomes of physical activity around menopause: A scoping review of research. Maturitas. 2022;164:88–97. https://doi.org/10.1016/j.maturitas.2022.07.014.
Sternfeld B, Guthrie KA, Ensrud KE, LaCroix AZ, Larson JC, Dunn AL, et al. Efficacy of exercise for menopausal symptoms: a randomized controlled trial. Menopause. 2014;21(4):330–8. https://doi.org/10.1097/GME.0b013e31829e4089.
Australian Institute of Health Welfare. Insufficient physical activity. AIHW. Available from: https://www.aihw.gov.au/reports/australias-health/insufficient-physical-activity. Accessed 3 May 2023.
Allman-Farinelli MA, Chey T, Bauman AE, Gill T, James WP. Age, period and birth cohort effects on prevalence of overweight and obesity in Australian adults from 1990 to 2000. Eur J Clin Nutr. 2008;62(7):898–907. https://doi.org/10.1038/sj.ejcn.1602769.
Timperio A, Salmon J, Rosenberg M, Bull FC. Do logbooks influence recall of physical activity in validation studies? Med Sci Sports Exerc. 2004;36(7):1181–6. https://doi.org/10.1249/01.mss.0000132268.74992.d8.
Brown W, Bauman A, Chey T, Trost S, Mummery K. Comparison of surveys used to measure physical activity. Aust N Z J Public Health. 2004;28(2):128–34. https://doi.org/10.1111/j.1467-842x.2004.tb00925.x.
Troiano RP, McClain JJ, Brychta RJ, Chen KY. Evolution of accelerometer methods for physical activity research. Br J Sports Med. 2014;48(13):1019–23. https://doi.org/10.1136/bjsports-2014-093546.
Bauman A, Phongsavan P, Schoeppe S, Owen N. Physical activity measurement- a primer for health promotion. Promot Educ. 2006;13(2):92–103. https://doi.org/10.1177/10253823060130020103.
Sorkin JD, Muller DC, Andres R. Longitudinal change in height of men and women: implications for interpretation of the body mass index: the Baltimore Longitudinal Study of Aging. Am J Epidemiol. 1999;150(9):969–77. https://doi.org/10.1093/oxfordjournals.aje.a010106.
Australian Longitudinal Study on Women’s Health. Estimated Height – Young and Mid-aged. Available from: https://alswh.org.au/wp-content/uploads/2020/08/DDSSection3Height.pdf. Accessed Sept 2023.
Carrasquilla GD, García-Ureña M, Fall T, Sørensen TIA, Kilpeläinen TO. Mendelian randomization suggests a bidirectional, causal relationship between physical inactivity and adiposity. eLife. 2022;11:e70386. https://doi.org/10.7554/eLife.70386.
Lee IM, Shiroma EJ, Lobelo F, Puska P, Blair SN, Katzmarzyk PT. Effect of physical inactivity on major non-communicable diseases worldwide: an analysis of burden of disease and life expectancy. Lancet. 2012;380(9838):219–29. https://doi.org/10.1016/s0140-6736(12)61031-9.
Michie S, van Stralen MM, West R. The behaviour change wheel: A new method for characterising and designing behaviour change interventions. Implement Sci. 2011;6(1):42. https://doi.org/10.1186/1748-5908-6-42.
Acknowledgements
The research on which this paper is based was conducted as part of the Australian Longitudinal Study on Women’s Health by the University of Queensland and the University of Newcastle. We are grateful to the Australian Government Department of Health and Aged Care for funding and to the women who provided the survey data.
Funding
The Australian Longitudinal Study on Women’s Health is funded by the Australian Government Department of Health. YN is supported by a postdoctoral research fellowship from the Japan Society for the Promotion of Science (22J00945). GM is supported by a National Health and medical Research Council Investigator Grant (APP2008702). The organizations named here had no influence on study design; data collection, data analysis; or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
WJB contributed to the design of the ALSWH and acquisition of data, all authors were involved in the conception and design of this study, YN and GIM conducted the analyses, all authors interpreted the data; YN prepared the first draft, and all authors critically reviewed and revised. All authors approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The ALSWH study has ethical approval from the Human Research Ethics Committees (HRECs) of the Universities of Newcastle and Queensland (approval numbers 2004000224). All participants consented to join the study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Supplementary table 1.
Complete list of variables. Supplementary figure 1. Trajectories of meeting physical activity recommendation probability. Supplementary table 2. Goodness-of-fit and adequacy of the model (probability of meeting physical activity recommendation). Supplementary table 3. Goodness-of-fit and adequacy of the model (total physical activity).
Additional file 2:
STROBE Statement—Checklist of items that should be included in reports of cohort studies.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Nemoto, Y., Brown, W.J. & Mielke, G.I. Trajectories of physical activity from mid to older age in women: 21 years of data from the Australian Longitudinal Study on Women’s Health. Int J Behav Nutr Phys Act 21, 4 (2024). https://doi.org/10.1186/s12966-023-01540-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12966-023-01540-z