Abstract
Background
Digital interventions may help address low vegetable intake in adults, however there is limited understanding of the features that make them effective. We systematically reviewed digital interventions to increase vegetable intake to 1) describe the effectiveness of the interventions; 2) examine links between effectiveness and use of co-design, personalisation, behavioural theories, and/or a policy framework; and 3) identify other features that contribute to effectiveness.
Methods
A systematic search strategy was used to identify eligible studies from MEDLINE, Embase, PsycINFO, Scopus, CINAHL, Cochrane Library, INFORMIT, IEEE Xplore and Clinical Trial Registries, published between January 2000 and August 2022. Digital interventions to increase vegetable intake were included, with effective interventions identified based on statistically significant improvement in vegetable intake. To identify policy-action gaps, studies were mapped across the three domains of the NOURISHING framework (i.e., behaviour change communication, food environment, and food system). Risk of bias was assessed using Cochrane tools for randomized, cluster randomized and non-randomized trials.
Results
Of the 1,347 records identified, 30 studies were included. Risk of bias was high or serious in most studies (n = 25/30; 83%). Approximately one quarter of the included interventions (n = 8) were effective at improving vegetable intake. While the features of effective and ineffective interventions were similar, embedding of behaviour change theories (89% vs 61%) and inclusion of stakeholders in the design of the intervention (50% vs 38%) were more common among effective interventions. Only one (ineffective) intervention used true co-design. Although fewer effective interventions included personalisation (67% vs 81%), the degree of personalisation varied considerably between studies. All interventions mapped across the NOURISHING framework behaviour change communication domain, with one ineffective intervention also mapping across the food environment domain.
Conclusion
Few digital interventions identified in this review were effective for increasing vegetable intake. Embedding behaviour change theories and involving stakeholders in intervention design may increase the likelihood of success. The under-utilisation of comprehensive co-design methods presents an opportunity to ensure that personalisation approaches better meet the needs of target populations. Moreover, future digital interventions should address both behaviour change and food environment influences on vegetable intake.
Similar content being viewed by others
Background
Low vegetable and legume consumption is a leading modifiable risk factor for non-communicable diseases globally [1, 2], accounting for over 2% of global deaths in 2017 [1]. International guidelines for vegetable intake recommend at least 3 serves/day (≥ 240 g/day) [3]. However, nationally representative survey data from 162 countries found that, in 2020, an average of 88% of the populations of these countries had an inadequate vegetable intake [4].
Interventions designed to address low vegetable intake often target low fruit intake simultaneously [5]; however, this is more likely to increase fruit intake than vegetable intake [6]. This is largely attributable to interventions not addressing barriers to vegetable intake, which are distinct from those of fruit intake, including lower palatability, lack of cooking confidence, and perceived higher cost and time to purchase, prepare and cook vegetable-rich meals [6,7,8,9,10,11]. Interventions that specifically focus on vegetables show promise, but are often setting-specific and delivered face-to-face, such as a workplace interventions [12]. While setting-specificity may be an important component of some personalisation approaches, more scalable approaches are needed to ensure interventions can serve large populations across a wide range of settings [13,14,15].
As an estimated 66% of people globally have access to the internet [16], digital interventions provide an accessible delivery model for increasing vegetable intake in adults [10, 11]. Furthermore, digital interventions are well aligned with the global drive to utilise digital technologies to improve health [17]. For example, 55% of European citizens aged 16–74 reported that they had sought online health information [18], and 88% of Australians reported wanting to access their health information digitally [19]. However, while there is some evidence that digital interventions increase fruit and vegetable intake [20], the effectiveness of digital interventions to increase vegetable intake alone is unclear.
Digital interventions offer the ability to personalise content and delivery to the needs and preferences of the user. Although evidence from randomised controlled trials (RCTs) suggest that personalised dietary advice motivates greater improvement in dietary intake than generalised dietary advice [21], personalisation of digital interventions alone may not be sufficient to increase vegetable intake. To help ensure dietary interventions meet the needs of the user, interventions are increasingly being designed with stakeholders, i.e., using co-design practices [22].
Co-design practices involve the lived experiences of the users, and individuals with technical expertise or service providers in the design process [23]. Research suggests that the use of co-design may help improve consumer engagement and satisfaction with a digital intervention by ensuring it meets their needs [23,24,25]. However, there is limited understanding of whether existing digital interventions to increase vegetable intake have used co-design methods or whether the use of co-design contributes to effectiveness.
Mediators of behaviour change, including knowledge of, attitudes towards, and skills in using vegetables, can be targeted in digital interventions to meet the needs of the user [26, 27]. However, achieving higher vegetable intake is also dependent on complex interactions between individual- and environmental-level influences, such as self-efficacy or access to affordable and healthy foods, which require specific policy actions [7, 8]. The NOURISHING framework [28], which maps interventions according to their alignment with policy actions related to behaviour change communications, the food environment or the food system, is a useful framework for considering such approaches. By mapping across each of these domains, gaps, and opportunities for policy actions for achieving behaviour change can be identified and targeted by digital interventions. Therefore, we aimed to systematically review digital interventions to increase vegetable intake in adults to: 1) describe the effectiveness of the interventions in terms of increased consumption; 2) examine links between effectiveness and use of co-design, personalisation, behavioural theories, and/or a policy framework; and 3) identify other features that contribute to effectiveness.
Methods
The protocol for this systematic review is registered with the international prospective register of systematic reviews (PROSPERO; CRD42022290926). The design and reporting of this review were guided by the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) statement (Additional file 1) and the synthesis without meta-analysis (SWiM) in systematic reviews reporting guidelines [29].
Eligibility criteria
The population, intervention, comparison, outcome (PICO) framework was used to develop the inclusion and exclusion criteria for study selection. Study designs included RCT, pseudo-RCTs, and pre-post interventions. The population included community-dwelling adults (18 years and older). Studies were excluded if they included pregnant and/or lactating women and/or institutionalised adults. Studies on populations for primary and secondary prevention were included. Interventions were included if they were a digital intervention targeting knowledge of, attitudes towards, and skills in using vegetables. In this review, “digital interventions” were interventions that included any of the following digital components: applications (apps; native, web, progressive and hybrid), websites, computer programs, mobile games, Short Message Services (SMS), Social Networking Services (SNS) and wearable devices [10]. Multi-modal interventions with non-digital components (e.g., face-to-face consultations) were included if digital features represented the primary focus of the intervention. The focus of this review was on vegetable intake, so the primary outcome was change in vegetable intake (i.e., measured as serves, portions, or grams/day). Secondary outcomes considered included changes in attitudes, knowledge, skills, self-efficacy, access and/or intentions related to vegetable intake. Studies were excluded if vegetable intake could not be examined separately. Only peer-reviewed original research articles published in English were included.
Search strategy
The search was developed in consultation with a librarian and undertaken in November 2021 and updated in August 2022. Published literature from January 2000 to August 2022 was searched. The year 2000 was selected as this coincided with an increase in the use of digital technologies in nutrition research and is in alignment with similar reviews of digital interventions [30]. The following databases were searched: MEDLINE (Complete), Embase, PsycINFO, Scopus (only extra searching), CINAHL (EbscoHost), Cochrane Library (Wiley), Rural and Remote Health database (INFORMIT), Health and society database (INFORMIT), IEEE Xplore, ClinicalTrials.gov and the Australian New Zealand Clinical Trial Registry. The full search strategy can be found in Additional file 2. Briefly, search terms were combined using the AND/OR operators for digital (‘digital, ‘smartphone’, ‘website’, ‘app’), intervention (‘intervention’, ‘randomized controlled trial’) and outcomes (‘vegetables’). Reference lists from systematic reviews identified in the search and included records were hand-searched to identify any additional studies. Where relevant protocol papers were identified during the search, an attempt was made to find the accompanying trial papers.
Data extraction
Studies were screened using Covidence software by two members of the team (KML, LA), first by title and abstract and then by full text. Discrepancies were resolved by discussion. Duplicates were removed in Covidence. Data were extracted by one reviewer (KML) and checked by a second reviewer (LA). A data extraction template was developed and piloted in Excel specifically for this review. The following information was extracted from each study: study design (setting, intervention and control conditions, duration), intervention features (digital tools used, co-design methods, behaviour change framework and taxonomies used, personalisation, NOURISHING framework policy domains and areas), population (country, age, sex, rurality, primary or secondary prevention); outcome measures (primary or secondary outcome, change in intake, behaviour, attitude, knowledge, skills, self-efficacy, intention and/or access); results for vegetable intake and effectiveness (yes/no determined based on statistically significant results for vegetable intake).
Data synthesis
A descriptive synthesis of the findings from the included studies was conducted. No meta-analysis was undertaken due to the heterogeneous nature of the digital tools used, characteristics of the populations in the included studies and the indicator of vegetable intake reported. The effectiveness and features of all interventions were summarised to better understand the characteristics that may increase likeliness of effectiveness. Features investigated included the population and study design, such as age, sex, rurality, use of co-design practices, behaviour change theory and personalisation methods. Studies were also mapped against the World Cancer Research Fund International’s NOURISHING framework [28]. This framework comprises three broad domains of policy actions (food environment, food system and behaviour change communication), 10 key policy areas within these domains, and the specific policy actions, which should be identified and implemented by policymakers to fit their national contexts and populations [28]. Examples of policy areas for these three domains included using economic tools to address food affordability (food environment domain), supply chain actions (food systems domain) and nutrition education and skills (behaviour change communication domain). We mapped whether the three broad domains and underlying 10 key policy areas were employed in the design of the intervention.
Risk of bias assessment
Two authors (KML, SP) performed an independent assessment of the risk of bias on the included studies, with any discrepancies resolved by consensus. Three Cochrane Risk of Bias tools were used: for randomized trials (RoB 2), for cluster RCTs (CRCT; RoB 2 CRCT) and for non-randomized studies of interventions (ROBINS-I) [31, 32]. The RoB 2 and RoB 2 CRCT domains for risk of bias assessment included randomization process, deviations from the intended interventions, missing outcome data, measurement of the outcome and selection of the reported result. The judgement within each domain was assessed to carry forward to an overall risk of bias judgement as low risk, some concerns or high risk of bias. The ROBINS-I domains for risk of bias assessment include confounding, selection of participants, classifications of interventions, deviations from intended interventions, missing data, measurements of outcomes and selection of reported results. The judgement within each domain was used to inform an overall risk of bias judgement as either low-risk, moderate-risk, serious risk, critical risk or no information reported.
Results
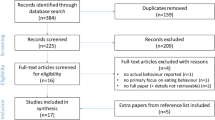
The search strategy retrieved 1,347 records (Fig. 1). After the removal of duplicates, 1,049 articles were screened for inclusion based on their title and abstract. Of these, the full texts of 97 articles were screened. This review included 30 studies [33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62] (Table 1).
Study characteristics
The 30 included studies comprised of RCTs (n = 22) [33,34,35,36,37,38, 40, 41, 43,44,45,46,47, 49,50,51,52,53, 55, 57, 61, 62], a CRCT (n = 1) [48] and non-randomized trials (n = 7) [39, 42, 54, 56, 58,59,60]. Intervention duration ranged from 3 days [35] to 2 years [43, 51]; more than half (n = 17; 57%) of studies had a follow-up period less than 6 months. Most studies were conducted in Australia [41, 42, 45, 48, 52, 58, 61], followed by the United States [35, 37, 38, 49, 53], Spain [34, 43, 50, 56, 59], the Netherlands [40, 51], the United Kingdom [47, 62], Belgium [60], France [44], pan-European [57], Israel [33], Iran [36], Brazil [39], Bangladesh [46], China [54] and Mongolia [55]. The studies included sample sizes ranging from 16 [56] to 5,055 [51], with 16 studies (53%) including a sample of 150 or more participants. The mean age of participants ranged from 18 years [54] to 70 years [38], with many (n = 19) conducted in mid-aged and older adult populations (> 40 years). Two studies delivered the digital interventions exclusively in rural areas [46, 48]. Eleven (37%) interventions recruited populations with health conditions, including hypertension [36, 39, 46], type 2 diabetes mellitus [33, 34, 44, 55], heart disease [43] prostate cancer [38] and overweight or obesity [45, 53]. The remaining studies were conducted in generally healthy populations and were designed to improve diet and/or lifestyle (n = 18) or weight management (n = 1). Over half of the studies (n = 17) were published since 2019.
Risk of bias
Risk of bias within 25 (83%) studies was high or serious because of missing outcome data for RCTs or bias due to confounding in non-RCTs (Additional file 3). Most RCTs (n = 17) and the CRCT adequately generated and concealed allocation resulting in no imbalances apparent between groups. Participant blinding was not possible because of the nature of digital health interventions and was not considered to increase risk of bias. The measure of assessment of vegetable intake was considered appropriate in most RCTs and the CRCT except for three studies where insufficient information was provided. Assessors were blinded to the intervention received by participants in 11 studies. Assessment of the outcome could have been influenced by knowledge of intervention received. However, this was deemed unlikely due to the dietary assessment methods and protocols used to assess vegetable intake, where it is unlikely that dietary coders were aware of the intervention allocation. Finally, seven studies did not reference a protocol or trial registration with a pre-specified analysis plan that was finalized before unblinded outcome data were available for analysis, which may be due to publication preceding the development of reporting guidelines.
Characteristics of digital tools
The most common digital tools used in the included studies were apps (n = 19; 63%), followed by SMS messaging (n = 10; 33%) and websites (n = 9; 30%). Some studies also used phone coaching and emails, and some interventions included a ‘dashboard’ feature to summarise resources and goals [39, 47]. Just under half (n = 13; 43%) used a combination of digital tools (Table 2).
Vegetable intake
As shown in Table 1, vegetable intake was a primary outcome in 63% of studies (n = 19). Of these, some studies reported vegetable intake as a component of a Mediterranean diet score (n = 4), International Diet Quality Index (n = 1), m-Alternate Healthy Eating Index [62] or an overall diet quality index for Dominican adults [56]. Vegetable intake was assessed in most studies using brief diet questions [35, 36, 41, 42, 45, 46, 54,55,56, 58, 60], followed by a food frequency questionnaire [33, 37,38,39,40, 48, 51, 57, 61, 62], 24 h recall [57, 59], Mediterranean diet adherence screener [34, 43, 50], and an image-based dietary assessment tool [52].
Co-design practices
As shown in Table 2 and Fig. 2, 40% of studies (n = 12) reported some level of stakeholder input into the intervention design. Only one study, by Lara et al., referred to co-design specifically; a seven-stage, sequential, iterative series of workshops were used for designing, prototyping, testing and optimising the intervention, which was undertaken with researchers, older adults (the target population) and health and social care professionals [47]. This study was designated as using true co-design. Of the studies that reported stakeholder input, health care professionals, such as dietitians and general practitioners, were the most commonly reported stakeholders involved in the design, followed by software engineers. Only five studies reported involving consumers with lived experiences, including young adults (aged 18–30 years) in the Connecting Health and Technology (CHAT) study [52], adults aged over 55 years in the Living, Eating, Activity and Planning through retirement (LEAP) study [47] and Arab adults in a trial of ethnic minority adults with type 2 diabetes mellitis [33].
Personalisation methods
Twenty-three studies (77%) included some level of personalised intervention feedback (Table 2 and Fig. 2). The degrees of personalisation ranged from low (e.g., feedback based on assessment of current diet [52]), to moderate (e.g., personalisation of menus and shopping lists [44]), to high (e.g., individual coaching from a dietitian [38]); only one study reported offering participants the opportunity to customise their personalisation, based on preferred frequency and timing of text messaging [41]. Seven studies provided access to diet or physical activity coaching by a health professional via an app [33, 38, 41, 43, 45, 48, 54], phone calls [38, 41, 48], video calls [43], and SMS messages, emails and online forums [45]. One study personalised content to specifically address barriers to vegetable intake based on participant responses [40], another study used a digital program to design a personalised daily or weekly menu based on user preferences such as taste in foods, season and price range [44], while another study created a personalised video to promote healthy lifestyle behaviours based on age, gender and individual type 2 diabetes risk factors [61]. SMS-based interventions often used the participants’ name within the content [34, 36, 39]. Four studies provided personalised feedback and/or action plans based on demographic characteristics (such as age, sex, ethnicity and culture) and/or participant preferences [34, 36, 39] although limited information was provided on how this personalisation was designed or delivered, or whether personalisation was applied to the dietary component of the intervention. Other studies included some aspects of individualised support, although access to advice and support from dietitians was not provided [42, 62].
Theoretical underpinning and framework
Twenty-one studies (70%) reported embedding behaviour change theories into intervention design and delivery. Social cognitive theory and the trans-theoretical model were the two theories/models used most to underpin the interventions, with behaviour change techniques such as goal setting, motivational interviewing or action planning most frequently used (Table 2 and Fig. 2). When mapping against the NOURISHING framework, all studies aligned with the behaviour change communication domain, with the two policy areas of “nutrition education and skills”, and “nutrition advice and counselling in health care settings” identified. One study also mapped to the food environment domain, with the policy area of “economic tools to address affordability and purchase incentives” identified [42]. In this study, participants accumulated points and received a monetary reward at the end of the intervention relative to the number of healthy dietary choices logged. No studies aligned with the food system domain.
Effectiveness of digital interventions
Only nine studies (30%) reported statistically significant improvements in vegetable intake (i.e., designated as effective interventions) compared with a control group [38, 44, 55] or compared with baseline. In the latter case, this included pre-post interventions [56, 58], uncontrolled randomised trials [42] and RCTs with no statistically significant increase in the control group (and no statistical comparison for between-group changes reported) [35, 54, 60]. There was heterogeneity in the method of reporting improvements in vegetable intake among effective studies, including serves/day and adherence to guidelines. Three studies reported change in serves/day, with the magnitude of this improvement ranging from 0.29 serves/day [38] to 1 serve/day [42]. One study reported that 87% of participants improved vegetable intake compared to 29% of the control group [55], while another study reported a 7% increase in adherence to ≥ 500 g/day of vegetables compared to baseline (and a non-significant increase in the control group) [54]. One pre-post study reporting a 3.75 points increase in vegetable score (as a component of the Global Diet Quality Index; maximum score 100) compared with baseline [56]. Two studies also reported improvements in vegetable intake, but limited data on the magnitude were provided and no statistical comparisons were reported [36, 37]. Three studies reported a decline in vegetable intake compared with baseline, including a 0.2 portion per day decline [47], a 4% decline in participants consuming ≥ 2 serves/day [50] and a further study did not report any data on the magnitude of change [49]. No studies included in this review reported on attitudes towards, knowledge of, skills in respect of, self-efficacy, access to and/or intentions with respect to vegetables.
Features of effective digital interventions
Of the nine effective interventions, sample sizes ranged from 120 to 171 participants (Table 1). A slightly greater percentage of effective interventions were in healthy populations (n = 6/9; 67%) compared with the ineffective interventions (n = 13/21; 62%). Almost half of effective interventions were in younger adults (< 40y; n = 4, 44%), compared with 19% (n = 4) of ineffective interventions. Neither of the two interventions delivered exclusively in rural communities were effective. Vegetable intake was the primary outcome in 78% (n = 7) of the effective interventions, compared with 57% (n = 12) of the ineffective interventions.
Of the effective interventions, 33% (n = 3) utilised an app [35, 54, 58], 22% (n = 2) used a website [44, 60] and 11% (n = 1) used SMS messages [55] in isolation, while one study used an app and activity tracker [42] and two studies utilised a combination of four or more delivery modalities (including apps, emails, SMS messages, phone calls, videos and websites) [38, 56]. As shown in Table 2, this contrasted with the ineffective interventions, where 29% (n = 6) utilised an app [33, 34, 36, 39, 40, 62], 10% (n = 2) used a website [47, 51], and 10% (n = 2) used SMS messages [41, 46] in isolation, while 52% (n = 11) used a combination of delivery modalities [37, 43, 45, 48,49,50, 52, 53, 57, 59, 61].
The features of effective and ineffective interventions are compared in Fig. 3. Eighty nine percent (n = 8) of the effective studies referenced behavioural theories in their design (Table 2), including the trans-theoretical model theory [55], the social cognitive theory [38] and the health action process [60]. In contrast, 61% (n = 12) of the ineffective interventions referenced theories. Sixty-seven percent (n = 6) effective interventions delivered personalised information, which included personalised dietary advice from a dietitian [34, 54] and personalised menus and food shopping lists based on taste preferences and calorie needs [44]. Of the ineffective interventions, 81% (n = 17) included personalisation methods. Forty-four percent (n = 4) of the effective interventions included some level of input from stakeholders into the design of the intervention, compared with 38% (n = 8) of the ineffective interventions. This included design input from health care professionals, such as dietitians and general practitioners, and software engineers, but rarely involved meaningful consumer involvement. Only one (ineffective) intervention included true co-design, with iterative workshops with researchers, older adults (the target population) and health and social care professionals (Fig. 3).
Discussion
In this systematic review we identified a paucity of digital interventions that were effective at increasing vegetable intake in adults. Embedding of behaviour change theories and inclusion of stakeholders in the design of the intervention were more common among effective interventions. We also observed that personalisation did not appear to be a feature of effective interventions. However, personalisation methods varied considerably, thus it is possible that the nature or degree of personalisation did not meet the needs of the user. Use of more comprehensive co-design methods may help to ensure that personalisation approaches are informed by the needs of the target population.
This review found that researchers used multiple, heterogenous indictors of vegetable intake when reporting outcomes from interventions, which prohibited quantitative synthesis of the magnitude of change in vegetable intake. Nevertheless, in the studies that reported serves/day, vegetable intake increased by between 0.29 to 1 serve/day, which is comparable to evidence from mass media campaigns (0.6 serves/day) [63] and workplace interventions (0.32 serves/day) [64]. Reviews of the effectiveness of interventions to increase vegetable intake specifically are lacking. Our exclusion of studies that did not report intakes of fruit and vegetables separately was critical for discerning how interventions impacted on vegetable intake alone. Given the considerable health and economic benefit at the population level of even a small increase in vegetable intake [65], future research should report these outcomes consistently, and separately from fruit intake. Further, some studies in this review reported vegetable intake as a secondary outcome, or as part of an overall diet quality scores, such as the Mediterranean diet [47, 50]. As a result, interventions targeting more than just vegetable intake may have dedicated less resources to increasing vegetable intake per se and may not have been suitably powered to detect effects on vegetable intake. Although the use of different indicators did not help explain any differences in intervention effectiveness, future interventions should report the magnitude of between-group changes in vegetable intake to ensure that results can be included in a quantitative synthesis.
Degrees of personalisation varied considerably between studies, with no clear difference in the type or level of personalisation between effective and ineffective interventions. Moreover, understanding of personalisation methods used in the included studies was limited because the reporting of the design and delivery of personalisation was often minimal. Nonetheless, while many studies used personalised feedback and/or action plans based on demographic characteristics and/or participant preferences, only one study offered participants the ability to customise the timing and delivery of their personalised content [41]. A recent study of the personalisation of digital health information identified that the preferred approach differed by age group, where young adults were more satisfied with user-driven personalisation as distinct from system-driven personalisation [66]. While system-driven personalisation offers the advantage of lower cognitive load for the user, a user-driven approach offers a greater sense of autonomy. As a result, certain population groups, such as those with higher digital health literacy, may wish to exert more control over their personalisation [67]. This degree of autonomy should be considered when designing more sophisticated approaches to personalisation, such as artificial intelligence algorithms and machine learning [68]. Digital technologies are well suited to delivering large-scale personalised dietary support, because the content, frequency and timing of the intervention can be modified to meet the needs and preferences of the user [15]. Thus, future digital interventions for increasing vegetable intake may be improved by better reporting of the use of personalisation methods, ensuring that the tool has sufficient flexibility for the content and modality to be personalised and by considering the use of more sophisticated digital techniques to achieve personalisation.
Embedded behaviour change theories were common in both the effective and ineffective interventions. There was no clear difference in the application of these theories between effective or ineffective interventions. However, it is worth noting that all interventions, bar one [42], mapped to the behaviour change communication domain of policy actions outlined in the NOURISHING framework and did not map to the food environment or food system domains. This contrasts with a recent review of settings-based and digital interventions, where studies often mapped to the food environment domain, by including strategies such as free provision of fruit and vegetables in workplaces [5]. In addition, in the review by Wolfenden et al., all interventions that mapped to the food environment domain were effective at increasing fruit and vegetable intake. The lack of behaviour change strategies at the food environment level identified in our review requires further attention in future research. For example, food prescription programs that aim to improve the accessibility and affordability of healthy foods have shown promise for improving vegetable intake and reducing food insecurity [69], and could be integrated into digital healthcare interventions via partnerships with relevant stakeholders, such as health care providers, food markets or foodbanks. This is particularly important in the era of the COVID-19 pandemic, which has increased consumer acceptance and use of digital health initiatives [70], as well as stimulated a concerted global investment in building more food secure communities [71, 72].
A paucity of studies in this review included diverse populations. Similar to other reviews of digital interventions [73], most study populations were female-skewed, and of mid or older age (> 40 years). Disadvantaged populations, such as those with lower socio-economic position and who are culturally and linguistically diverse, were under-represented. Thus, there is potential for selection bias and response bias to have limited the generalisability of the findings from these studies. In addition, the “digital divide” persists, where lower income countries, racial/ethnic minorities, older adults, and individuals who live in lower income households and rural areas have less access to the internet and lower digital literacy [74]. However, global internet use has doubled from 33 to 65% in the last decade [16], and there is some evidence that digital inclusion is increasing [10, 11, 75]. Therefore, there is an opportunity to test the effectiveness of digital interventions in diverse populations to help reduce dietary (and health) inequities and improve digital literacy. Moreover, findings from this review confirm recent research highlighting a lack of nutrition research in rural settings, where there is inequitable access to healthcare and fresh produce, such as fruit and vegetables [13]. As a result, future interventions should consider external validity in other less well-represented population groups such as individuals with lower socioeconomic position and those living in rural settings. Digital interventions are well suited to achieve this because of their potential for linguistic and cultural localisation, national scalability at relatively low cost, and the global drive to improve digital health equity in rural and disadvantaged communities.
Fewer than half of included studies reported on interventions that had been developed with some level of design input from stakeholders. In addition, intervention end users were very rarely involved and only one intervention specifically mentioned the use of co-design approaches. Recent reviews on the use of co-design have shown mixed findings, with one review of co-design in health settings showing widespread use [24], and another review of co-design in nutrition and health interventions in community-dwelling adults identifying no interventions implementing a complete co-design process [25]. A more recent review of the use of co-design specifically in nutrition interventions delivered within a healthcare, community or academic setting identified only two studies reporting a partnership with consumers across all stages of research [76]. Taken together, these findings reinforce the need for consistent use of co-design terminology, better reporting of design and development processes and more widespread utilisation of a translational framework for the evaluation of health interventions, such as the NASSS (non-adoption, abandonment, scale-up, spread, sustainability) framework [77]. Future research should include co-design methods at multiple levels (i.e., stakeholders with lived experience as well as technical expertise) and include stakeholders throughout, from project conception to dissemination.
Outcomes from this research have implications for the use of digital tools to improve public health nutrition and provide insights into future research needs. Despite the potential for digital tools to improve access to dietary interventions, the persistent threat that digital technologies can exacerbate social inequities of health remains [78]. As such, the inclusion of diverse populations groups in the design and implementation of digital interventions remains a priority. Without this, there is a risk that some population groups may experience barriers to the use of digital technologies, including individuals experiencing socio-economic disadvantage, individuals with disabilities, individuals who require cultural adaptations, and those with low food and digital literacy and self-efficacy [79]. Countries with diverse geographic settings and the potential for disparities in internet access, such as Australia, should ensure that digital interventions are tested in rural settings, which would otherwise be a missed opportunity for addressing widening health disparities [80]. Further, with a paucity of co-design research and consideration of environmental influences, this research suggests that the design of digital interventions to increase vegetable intake is not yet optimal in maximising effectiveness.
This review has several strengths and limitations. The main strength was the systematic approach used to search, screen, and synthesise the literature, including the PROSPERO registration of the review protocol and the use of Cochrane risk of bias tools. By limiting the search to articles published in English and including experimental study designs only, it is possible that studies that would be informative for the design of future interventions were missed. As most studies included in this review were rated as high risk for bias, findings should be interpreted with caution. Due to the heterogenous study populations and intervention designs, including small sample sizes, no quantitative synthesis could be performed. Further, intervention outcomes for vegetable intake will be subject to misreporting biases due to the self-report nature of dietary assessment tools available, which includes the potential for participants to introduce bias as their food literacy and understanding of dietary reporting improves. Lastly, grey literature and commercial products for dietary behaviour change were excluded, which may have limited our ability to capture evidence of co-design research and the full range of digital tools designed to increase vegetable intake.
Conclusions
Few digital interventions have been effective in increasing vegetable intake among adults. Embedding behaviour change theories and involving stakeholders in intervention design may increase the likelihood of effectiveness. Personalisation was not a distinctive feature of effective digital interventions, however, this feature remains poorly understood due to considerable variation in its design and reporting. There is an unmet opportunity for the use of more comprehensive co-design methods to ensure personalisation approaches meet the needs of target populations. Furthermore, future digital interventions should consider strategies that address both behaviour change and food environment influences.
Availability of data and materials
Not applicable.
Abbreviations
- BMI:
-
Body mass index
- BL:
-
Baseline
- FFQ:
-
Food frequency questionnaire
- PRISMA:
-
Preferred reporting items for systematic reviews and meta-analyses
- RCT:
-
Randomized controlled trial
- RoB 2:
-
Risk of bias in randomized trials
- ROBINS-I:
-
Risk of bias in non-randomized studies of interventions
References
Afshin A, Sur P, Fay K, Cornaby L, Ferrara G, Salama J, et al. Health effects of dietary risks in 195 countries, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2019;393:1958–72.
Lim SS, Vos T, Flaxman AD, Danaei G, Shibuya K, Adair-Rohani H. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2224–60.
Food-Based Dietary Guidelines. Available online: http://www.fao.org/nutrition/education/food-dietary-guidelines/home/en/ (Accessed 9 May 2022).
Kalmpourtzidou A, Eilander A, Talsma EF. Global Vegetable Intake and Supply Compared to Recommendations: A Systematic Review. Nutrients. 2020;12(6):1558.
Wolfenden L, Barnes C, Lane C, McCrabb S, Brown HM, Gerritsen S, et al. Consolidating evidence on the effectiveness of interventions promoting fruit and vegetable consumption: an umbrella review. Int J Behav Nutr Phys Act. 2021;18(1):11.
Glasson C, Chapman K, James E. Fruit and vegetables should be targeted separately in health promotion programmes: differences in consumption levels, barriers, knowledge and stages of readiness for change. Public Health Nutr. 2011;14(4):694–701.
Godrich S, Kent K, Murray S, Auckland S, Lo J, Blekkenhorst L, et al. Australian Consumer Perceptions of Regionally Grown Fruits and Vegetables: Importance, Enablers, and Barriers. Int J Environ Res Public Health. 2019;17(1):63.
Pollard J, Kirk SFL, Cade JE. Factors affecting food choice in relation to fruit and vegetable intake: a review. Nutr Res Rev. 2002;15(2):373–87.
Livingstone KM, Burton M, Brown AK, McNaughton SA. Exploring barriers to meeting recommendations for fruit and vegetable intake among adults in regional areas: A mixed-methods analysis of variations across socio-demographics. Appetite. 2020;153: 104750.
Taj F, Klein MCA, van Halteren A. Digital Health Behavior Change Technology: Bibliometric and Scoping Review of Two Decades of Research. JMIR Mhealth Uhealth. 2019;7(12): e13311.
Nour M, Chen J, Allman-Farinelli M. Efficacy and External Validity of Electronic and Mobile Phone-Based Interventions Promoting Vegetable Intake in Young Adults: Systematic Review and Meta-Analysis. J Med Internet Res. 2016;18(4): e58.
Noy S, Patrick R, Ryan I, Nuttman S, Henderson-Wilson C. Scoping study of community interventions that promote vegetable consumption 2017. Available from: https://www.deakin.edu.au/__data/assets/pdf_file/0007/1251295/2018-01-31-ScopingStudyVegConsumption-WEB.pdf. Accessed 8 Jan 2023.
Alston L, Partridge SR. Limited dietary interventions in rural Australian communities: A systematic review. Nutr Diet. 2020;78(1):57–68.
Rekhy R, McConchie R. Promoting consumption of fruit and vegetables for better health. Have campaigns delivered on the goals? Appetite. 2014;79:113–23.
Celis-Morales C, Lara J, Mathers JC. Personalising nutritional guidance for more effective behaviour change. Proc Nutr Soc. 2015;74(2):130–8.
Statistica Research Department. Internet and social media users in the world 2022. 2023. Available from: https://www.statistica.com/statistics/617136/digital-population-worldwide/ (Accessed 9 Jan 2023)
Petersen A. Digital Health and Technological Promise: A Sociological Inquiry (1st ed.). Routledge: 2019. https://doi.org/10.4324/9781315200880. Accessed 8 Jan 2023.
Eurostat. Internet activities. 2022. Available from: https://ec.europa.eu/eurostat/ (Accessed 9 Jan 2023)
Australian Digital Health Agency. Digital Health Survey. 2021. Available from: https://nationalstrategy.digitalhealth.gov.au/ (Accessed 9 Jan 2023)
Rodriguez Rocha NP, Kim H. eHealth Interventions for Fruit and Vegetable Intake: A Meta-Analysis of Effectiveness. Health Educ Behav. 2019;46(6):947–59.
Jinnette R, Narita A, Manning B, McNaughton SA, Mathers JC, Livingstone KM. Does Personalized Nutrition Advice Improve Dietary Intake in Healthy Adults? A Systematic Review of Randomized Controlled Trials. Adv Nutr. 2021;12(3):657–69.
O’Brien N, Heaven B, Teal G, Evans EH, Cleland C, Moffatt S, et al. Integrating Evidence From Systematic Reviews, Qualitative Research, and Expert Knowledge Using Co-Design Techniques to Develop a Web-Based Intervention for People in the Retirement Transition. J Med Internet Res. 2016;18(8): e210.
Singleton A, Raeside R, Partridge SR, Hayes M, Maka K, Hyun KK, et al. Co-designing a Lifestyle-Focused Text Message Intervention for Women After Breast Cancer Treatment: Mixed Methods Study. J Med Internet Res. 2021;23(6):e27076-e.
Slattery P, Saeri AK, Bragge P. Research co-design in health: a rapid overview of reviews. Health Res Policy Syst. 2020;18(1):17.
Tay BSJ, Cox DN, Brinkworth GD, Davis A, Edney SM, Gwilt I, et al. Co-Design Practices in Diet and Nutrition Research: An Integrative Review. Nutrients. 2021;13(10):3593.
Campbell MK, McLerran D, Turner-McGrievy G, Feng Z, Havas S, Sorensen G, et al. Mediation of adult fruit and vegetable consumption in the National 5 A Day for Better Health community studies. Ann Behav Med. 2008;35(1):49–60.
Brimblecombe J, Ferguson M, Barzi F, Brown C, Ball K. Mediators and moderators of nutrition intervention effects in remote Indigenous Australia. Br J Nutr. 2018;119(12):1424–33.
Hawkes C, Jewell J, Allen K. A food policy package for healthy diets and the prevention of obesity and diet-related non-communicable diseases: the NOURISHING framework. Obes Rev. 2013;14(S2):159–68.
Campbell M, McKenzie JE, Sowden A, Katikireddi SV, Brennan SE, Ellis S, et al. Synthesis without meta-analysis (SWiM) in systematic reviews: reporting guideline. BMJ. 2020;368: l6890.
Western MJ, Armstrong MEG, Islam I, Morgan K, Jones UF, Kelson MJ. The effectiveness of digital interventions for increasing physical activity in individuals of low socioeconomic status: a systematic review and meta-analysis. Int J Behav Nutr Phys Act. 2021;18(1):148.
Sterne JAC, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366: l4898.
Sterne JA, Hernán MA, Reeves BC, Savović J, Berkman ND, Viswanathan M, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 2016;355: i4919.
Abu-Saad K, Murad H, Barid R, Olmer L, Ziv A, Younis-Zeidan N, et al. Development and Efficacy of an Electronic, Culturally Adapted Lifestyle Counseling Tool for Improving Diabetes-Related Dietary Knowledge: Randomized Controlled Trial Among Ethnic Minority Adults With Type 2 Diabetes Mellitus. J Med Internet Res. 2019;21(10): e13674.
Alonso-Domínguez R, García-Ortiz L, Patino-Alonso MC, Sánchez-Aguadero N, Gómez-Marcos MA, Recio-Rodríguez JI. Effectiveness of A Multifactorial Intervention in Increasing Adherence to the Mediterranean Diet among Patients with Diabetes Mellitus Type 2: A Controlled and Randomized Study (EMID Study). Nutrients. 2019;11(1):162.
Bhurosy T, Middlestadt SE, Lin HC, Thiagarajah K, Fly AD. A Randomized mHealth Trial to Promote Vegetable Intake Through Counting and Goal Setting. J Nutr Educ Behav. 2020;52(12):1111–9.
Bozorgi A, Hosseini H, Eftekhar H, Majdzadeh R, Yoonessi A, Ramezankhani A, et al. The effect of the mobile “blood pressure management application” on hypertension self-management enhancement: a randomized controlled trial. Trials. 2021;22(1):413.
Brown ON, O’Connor LE, Savaiano D. Mobile MyPlate: a pilot study using text messaging to provide nutrition education and promote better dietary choices in college students. J Am Coll Health. 2014;62(5):320–7.
Chan JM, Van Blarigan EL, Langlais CS, Zhao S, Ramsdill JW, Daniel K, et al. Feasibility and Acceptability of a Remotely Delivered, Web-Based Behavioral Intervention for Men With Prostate Cancer: Four-Arm Randomized Controlled Pilot Trial. J Med Internet Res. 2020;22(12): e19238.
Debon R, Bellei EA, Biduski D, Volpi SS, Alves ALSA, Portella MR, et al. Effects of using a mobile health application on the health conditions of patients with arterial hypertension: A pilot trial in the context of Brazil’s Family Health Strategy. Sci Rep. 2020;10(1):6009.
Elbert SP, Dijkstra A, Oenema A. A Mobile Phone App Intervention Targeting Fruit and Vegetable Consumption: The Efficacy of Textual and Auditory Tailored Health Information Tested in a Randomized Controlled Trial. J Med Internet Res. 2016;18(6): e147.
Fjeldsoe BS, Goode AD, Phongsavan P, Bauman A, Maher G, Winkler E, et al. Get Healthy, Stay Healthy: Evaluation of the Maintenance of Lifestyle Changes Six Months After an Extended Contact Intervention. JMIR mHealth uHealth. 2019;7(3):e11070-e.
Gilson ND, Pavey TG, Wright OR, Vandelanotte C, Duncan MJ, Gomersall S, et al. The impact of an m-Health financial incentives program on the physical activity and diet of Australian truck drivers. BMC Public Health. 2017;17(1):467.
Goni L, de la O V, Barrio-López MT, Ramos P, Tercedor L, Ibañez-Criado JL, et al. A Remote Nutritional Intervention to Change the Dietary Habits of Patients Undergoing Ablation of Atrial Fibrillation: Randomized Controlled Trial. J Med Internet Res. 2020;22(12):e21436.
Hansel B, Giral P, Gambotti L, Lafourcade A, Peres G, Filipecki C, et al. A Fully Automated Web-Based Program Improves Lifestyle Habits and HbA1c in Patients With Type 2 Diabetes and Abdominal Obesity: Randomized Trial of Patient E-Coaching Nutritional Support (The ANODE Study). J Med Internet Res. 2017;19(11): e360.
Hebden L, Cook A, Ploeg HP, King L, Bauman A, Allman-Farinelli M. A mobile health intervention for weight management among young adults: a pilot randomised controlled trial. J Hum Nutr Diet. 2014;27(4):322–32.
Jahan Y, Rahman MM, Faruque ASG, Chisti MJ, Kazawa K, Matsuyama R, et al. Awareness Development and Usage of Mobile Health Technology Among Individuals With Hypertension in a Rural Community of Bangladesh: Randomized Controlled Trial. J Med Internet Res. 2020;22(12):N.PAG-N.PAG.
Lara J, O’Brien N, Godfrey A, Heaven B, Evans EH, Lloyd S, et al. Pilot Randomised Controlled Trial of a Web-Based Intervention to Promote Healthy Eating, Physical Activity and Meaningful Social Connections Compared with Usual Care Control in People of Retirement Age Recruited from Workplaces. PLoS ONE. 2016;11(7): e0159703.
Lombard C, Harrison C, Kozica S, Zoungas S, Ranasinha S, Teede H. Preventing Weight Gain in Women in Rural Communities: A Cluster Randomised Controlled Trial. PLoS Med. 2016;13(1): e1001941.
Pope ZC, Barr-Anderson DJ, Lewis BA, Pereira MA, Gao Z. Use of Wearable Technology and Social Media to Improve Physical Activity and Dietary Behaviors among College Students: A 12-Week Randomized Pilot Study. Int J Environ Res Public Health. 2019;16(19)3579.
Recio-Rodriguez JI, Agudo-Conde C, Martin-Cantera C, González-Viejo MN, Fernandez-Alonso MDC, Arietaleanizbeaskoa MS, et al. Short-Term Effectiveness of a Mobile Phone App for Increasing Physical Activity and Adherence to the Mediterranean Diet in Primary Care: A Randomized Controlled Trial (EVIDENT II Study). J Med Internet Res. 2016;18(12): e331.
Schulz DN, Kremers SPJ, Vandelanotte C, van Adrichem MJG, Schneider F, Candel MJJM, et al. Effects of a web-based tailored multiple-lifestyle intervention for adults: a two-year randomized controlled trial comparing sequential and simultaneous delivery modes. J Med Internet Res. 2014;16(1): e26.
Kerr DA, Harray AJ, Pollard CM, Dhaliwal SS, Delp EJ, Howat PA, et al. The connecting health and technology study: a 6-month randomized controlled trial to improve nutrition behaviours using a mobile food record and text messaging support in young adults. Int J Behav Nutr Phys Act. 2016;13(1):52.
Turner-McGrievy GM, Beets MW, Moore JB, Kaczynski AT, Barr-Anderson DJ, Tate DF. Comparison of traditional versus mobile app self-monitoring of physical activity and dietary intake among overweight adults participating in an mHealth weight loss program. J Am Med Informatics Assoc. 2013;20(3):513–8.
Wang M, Guo Y, Zhang Y, Xie S, Yu Z, Luo J, et al. Promoting healthy lifestyle in Chinese college students: evaluation of a social media-based intervention applying the RE-AIM framework. Eur J Clin Nutr. 2021;75(2):335–44.
Wang X, Liu D, Du M, Hao R, Zheng H, Yan C. The role of text messaging intervention in Inner Mongolia among patients with type 2 diabetes mellitus: a randomized controlled trial. BMC Med Inform Decis Mak. 2020;20(1):90.
Cantisano LM, Gonzalez-Soltero R, Blanco-Fernández A, Belando-Pedreño N. ePSICONUT: An e-Health Programme to Improve Emotional Health and Lifestyle in University Students. Int J Environ Res Public Health. 2022;19(15):9253.
Celis-Morales C, Livingstone KM, Marsaux CFM, Macready AL, Fallaize R, O’Donovan CB, et al. Effect of personalized nutrition on health-related behaviour change: evidence from the Food4me European randomized controlled trial. Int J Epidemiol. 2016;46(2):578–88.
Hendrie GA, Hussain MS, Brindal E, James-Martin G, Williams G, Crook A. Impact of a Mobile Phone App to Increase Vegetable Consumption and Variety in Adults: Large-Scale Community Cohort Study. JMIR Mhealth Uhealth. 2020;8(4): e14726.
Perez-Junkera G, Vázquez-Polo M, Eizagirre FJ, Benjumea L, Tutau C, Esteban B, et al. Application of a Platform for Gluten-Free Diet Evaluation and Dietary Advice: From Theory to Practice. Sensors. 2022;22(3):732.
Plaete J, De Bourdeaudhuij I, Verloigne M, Crombez G. Acceptability, feasibility and effectiveness of an eHealth behaviour intervention using self-regulation: “MyPlan.” Patient Educ Couns. 2015;98(12):1617–24.
Williams SL, To Q, Vandelanotte C. What is the effectiveness of a personalised video story after an online diabetes risk assessment? A Randomised Controlled Trial. PLoS ONE. 2022;17(3): e0264749.
Zenun Franco R, Fallaize R, Weech M, Hwang F, Lovegrove JA. Effectiveness of Web-Based Personalized Nutrition Advice for Adults Using the eNutri Web App: Evidence From the EatWellUK Randomized Controlled Trial. J Med Internet Res. 2022;24(4): e29088.
Pollard CM, Miller MR, Daly AM, Crouchley KE, O’Donoghue KJ, Lang AJ, et al. Increasing fruit and vegetable consumption: success of the Western Australian Go for 2&5®campaign. Public Health Nutr. 2008;11(3):314–20.
Kushida O, Murayama N. Effects of environmental intervention in workplace cafeterias on vegetable consumption by male workers. J Nutr Educ Behav. 2014;46(5):350–8.
Deloitte Access Economics. The impact of increasing vegetable consumption on health expenditure 2016 [Available from: https://www2.deloitte.com/au/en/pages/economics/articles/increasing-vegetable-consumption-health-expenditure-impact.html].
Nguyen MH, Bol N, King AJ. Customisation versus Personalisation of Digital Health Information: Effects of Mode Tailoring on Information Processing Outcomes. Eur J Health Commun. 2020;1(1):30–54.
Smit ES, Bol N. From self-reliers to expert-dependents: identifying classes based on health-related need for autonomy and need for external control among mobile users. Media Psychol. 2020;23(3):391–414.
Livingstone KM, Ramos-Lopez O, Pérusse L, Kato H, Ordovas JM, Martínez JA. Precision nutrition: A review of current approaches and future endeavors. Trends Food Sci Technol. 2022;128:253–64.
Little M, Rosa E, Heasley C, Asif A, Dodd W, Richter A. Promoting Healthy Food Access and Nutrition in Primary Care: A Systematic Scoping Review of Food Prescription Programs. Am J Health Promot. 2022;36(3):518–36.
Sturgiss E, Desborough J, Hall Dykgraaf S, Matenge S, Dut G, Davis S, et al. Digital health to support primary care provision during a global pandemic. Aust Health Rev. 2022;46(3):269–72.
England PH. Community-centred public health: taking a whole system approach 2020 [Available from: https://www.gov.uk/government/publications/community-centred-public-health-taking-a-whole-system-approach.
Gilmore B, Ndejjo R, Tchetchia A, de Claro V, Mago E, Diallo AA, et al. Community engagement for COVID-19 prevention and control: a rapid evidence synthesis. BMJ Glob Health. 2020;5(10): e003188.
Hutchesson MJ, Gough C, Müller AM, Short CE, Whatnall MC, Ahmed M, et al. eHealth interventions targeting nutrition, physical activity, sedentary behavior, or obesity in adults: A scoping review of systematic reviews. Obes Rev. 2021;22(10): e13295.
Nguyen A, Mosadeghi S, Almario CV. Persistent digital divide in access to and use of the Internet as a resource for health information: Results from a California population-based study. Int J Med Inform. 2017;103:49–54.
Thomas J, Barraket J, Parkinson S, Wilson C, Holcombe-James I, Kennedy J, Mannell K, Brydon A. Australian Digital Inclusion Index: 2021. Melbourne: RMIT, Swinburne University of Technology, and Telstra; 2021.
Meloncelli N, Young A, Christoffersen A, Rushton A, Zhelnov P, Wilkinson SA, et al. Co-designing nutrition interventions with consumers: A scoping review. J Hum Nutr Diet. 2022. https://doi.org/10.1111/jhn.13082.
Abimbola S, Patel B, Peiris D, Patel A, Harris M, Usherwood T, et al. The NASSS framework for ex post theorisation of technology-supported change in healthcare: worked example of the TORPEDO programme. BMC Med. 2019;17(1):233.
Weiss D, Rydland HT, Øversveen E, Jensen MR, Solhaug S, Krokstad S. Innovative technologies and social inequalities in health: A scoping review of the literature. PLoS ONE. 2018;13(4): e0195447.
Resta P, Laferrière T, McLaughlin R, Kouraogo A. Issues and Challenges Related to Digital Equity: An Overview. In: Voogt J, Knezek G, Christensen R, Lai K-W, editors. Second Handbook of Information Technology in Primary and Secondary Education. Cham: Springer International Publishing; 2018. p. 987–1004.
Alston L, Jacobs J, Allender S, Nichols M. A comparison of the modelled impacts on CVD mortality if attainment of public health recommendations was achieved in metropolitan and rural Australia. Public Health Nutr. 2020;23(2):339–47.
Acknowledgements
We would like to thank Rachel West for help with the design and implementation of the literature search.
Funding
KML is supported by a National Health and Medical Research Council (NHMRC) of Australia Emerging Leadership Fellowship (APP1173803). LCB is supported by an NHMRC of Australia Emerging Leadership Investigator Grant (ID1172987) and a National Heart Foundation of Australia Post-Doctoral Research Fellowship (ID102498). JR was supported by a National Heart Foundation of Australia Postdoctoral Fellowship (ID102585).
Author information
Authors and Affiliations
Contributions
All authors had input into the design of the study and the development of the search strategy and protocol. KML and LA conducted the search, with input from a Deakin University librarian. KML and LA screened studies for inclusion and extracted data. SP and KML conducted the Risk of Bias, KML prepared the PRISMA data, KML, SP and LA extracted the study characteristics. KML and LA drafted the manuscript with all co-authors contributing critical review to drafts of the manuscript. All authors approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent to publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
PRIMSA checklist.
Additional file 2.
Search strategy.
Additional file 3.
Cochrane Risk of Bias for RCTs, cluster RCTs and non-RCTs.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Livingstone, K.M., Rawstorn, J.C., Partridge, S.R. et al. Digital behaviour change interventions to increase vegetable intake in adults: a systematic review. Int J Behav Nutr Phys Act 20, 36 (2023). https://doi.org/10.1186/s12966-023-01439-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12966-023-01439-9