Abstract
Background
Consumption of certain foods is associated with long-term weight gains and abdominal fat accumulation in healthy, middle-aged and young, non-obese participants. Whether the same foods might be associated with changes in adiposity in elderly population at high cardiovascular risk is less known.
Objective
Using yearly repeated measurements of both food habits and adiposity parameters, we aimed to investigate how changes in the consumption of specific foods were associated with concurrent changes in weight or waist circumference (WC) in the PREDIMED trial.
Design
We followed-up 7009 participants aged 55–70 years at high cardiovascular risk for a median time of 4.8 years. A validated 137-item semi-quantitative Food Frequency Questionnaire was used for dietary assessment with yearly repeated measurements. We longitudinally assessed associations between yearly changes in food consumption (serving/d) and concurrent changes in weight (kg) or WC (cm).
Results
Yearly increments in weight were observed with increased consumption (kg per each additional increase in 1 serving/d) for refined grains (0.32 kg/serving/d), red meat (0.24), potatoes (0.23), alcoholic beverages (0.18), processed meat (0.15), white bread (0.07) and sweets (0.04); whereas inverse associations were detected for increased consumption of low-fat yogurt (− 0.18), and low-fat milk (− 0.06).
Annual WC gain (cm per each additional increase in 1 serving/d) occurred with increased consumption of snacks, fast-foods and pre-prepared dishes (0.28), processed meat (0.18), alcoholic beverages (0.13), and sweets (0.08); whereas increased consumption of vegetables (− 0.23), and nuts (− 0.17), were associated with reductions in WC.
Conclusions
In this assessment conducted in high-risk subjects using yearly repeated measurements of food habits and adiposity, some ultra-processed foods, refined carbohydrates (including white bread), potatoes, red meats and alcohol were associated with higher weight and WC gain, whereas increases in consumption of low-fat dairy products and plant foods were associated with less gain in weight and WC.
Trial registration
This study was registered at controlled-trials.com with International Standard Randomized Controlled Trial Number (ISRCTN): 35739639. Registration date: 5 October 2005.
Similar content being viewed by others
Introduction
Findings on the relationships between dietary patterns with beneficial or deleterious effects on health are well established and constitute the basis for existing dietary guidelines. However, further food- and nutrient-based research is warranted to elucidate the mechanisms by which dietary patterns exert their effects. Identification the most likely causative foods would strengthen the evidence on which dietary recommendations for preventing obesity and weight gain based on healthy dietary patterns can be developed [1, 2].
Food groups have been addressed in a prospective large and long-term study from three American cohorts, which found that increments in the consumption of potato chips, potatoes, sugar-sweetened beverages (SSB), as well as red and processed meat was linked to higher weight gain, whereas the intake of vegetables, fruits, nuts, whole grain, and yogurt was linked to lower weight gain [3, 4]. A similar study conducted in Europeans, found that a diet high in fruit and dairy products and low in bread, processed meat, margarine, and soft drinks was associated with lower abdominal fat accumulation over time [5]. However, in both cohorts only middle-aged and young individuals (all < 65 years) with no chronic disease, and no obesity (Americans) were evaluated.
Prospective studies on diet and obesity typically evaluated only prevalent, baseline food intake [5] and subsequent changes in weight, or the association between dietary changes within a period of several years and weight changes occurred thereafter. As eating behaviors change over time, Smith et al proposed that the optimal methodology consists on the analysis of changes in diet with concurrent changes in weight, both evaluated along the same timespan [6]. In addition, previous studies [3, 4] only included dietary measurements repeated every 4 years, but none of them repeatedly assessed diet every year. As the induction period for the association between diet and weight gain is likely to be shorter than 4 years, yearly assessments of diet and weight can provide further insights into causally relevant associations.
The PREDIMED trial evaluated the effect of Mediterranean diet (MedDiet) vs a low-fat diet, on cardiovascular disease (CVD) prevention in a large sample of elderly subjects at high CVD risk. Over the course of the trial, all participants experienced small weight losses but (also small) waist circumference (WC) increments; this could be related to the age-related decline in lean body mass and fat mass redistribution, leading to visceral fat accumulation. For this reason, WC might be a better measure of adiposity in elderly populations than other anthropometric measurements such as body weight or body mass index (BMI); this is also supported by the fact that the association between overweight measured using the BMI and mortality is not yet well established in the elderly population [7,8,9]. In the PREDIMED study, those exposed to MedDiet lost slightly more weight and gained less in WC than subjects on control diet [10].
The PREDIMED is unique in having conducted repeated dietary assessments with the same 137-item semi-quantitative Food Frequency Questionnaire (FFQ) at baseline and on a yearly basis thereafter. In addition, the PREDIMED study consists of a population of elderly participants at high cardiovascular risk, for which the evidence on how diet might influence differently overall vs central adiposity is not yet well established. Using these FFQs, we aimed to investigate, in an elderly population at high CVD risk, how yearly changes in dietary factors were simultaneously associated with weight and WC changes measured directly and objectively during each of the 5 first years of follow-up.
Subjects and methods
Study overview and participants
The current study is based on data from the PREDIMED (Prevención con Dieta Mediterránea) trial (ISRCTN35739639) over the first 5 years of follow-up. Details of the trial have been previously published [11, 12]. Briefly, PREDIMED was a randomized, controlled trial started in 2003 in 11 Spanish centers (www.predimed.es), and designed to compare the effect of interventions with MedDiet supplemented with extra-virgin olive oil (EVOO) or nuts vs a control low-fat diet, on primary prevention of CVD. Study population included men and women aged 55–80 years, free of CVD at enrolment, but at high CVD risk due to the presence of either type 2 diabetes (T2D) or at least three major risk factors (hypercholesterolemia, low high-density lipoprotein, overweight/obesity, hypertension, current smoking or family history of premature coronary heart disease). The trial was stopped in December 2010 (median follow-up of 4.8 years), when the evidence of early cardiovascular benefit of MedDiet groups vs control group became identified. All participants provided written informed consent and the study protocol was approved by the institutional review boards of all recruiting centers according to the Declaration of Helsinki. This study followed the STROBE-nut guidelines for reporting [13].
Of the total 7447 participants included in the PREDIMED trial, 291 participants were excluded due to the missing data on diet, anthropometrics or other covariables at baseline, and 147 participants due to total energy intake values outside predefined limits (500–3500 kcal/d (women), 800–4000 kcal/d (men)) [14], resulting in a final number of 7009 participants (see the flow chart in Additional file 1: Figure S1).
Assessment of changes in diet
Data on dietary intake over the last year was assessed with the use of a validated 137-item semi-quantitative FFQ administered by trained dietitians at baseline and yearly during follow-up in a face-to-face interview [15]. Intake of each food item was calculated by multiplying serving size by frequency of consumption (from never to > 6 times/d). Spanish food composition tables were used to derive total energy (kcal/d) and nutrient intake [16, 17]. Food items have been grouped if they shared similarities in nutritional characteristics, and plausibly, were likely to exert similar biologic effects on obesity risk. The exposures of interest were changes in the intake of 31 specific food groups expressed in serving/d, calculated as the difference between yearly measured values and values from the previous year. Detailed information on the specific food groups, and items used to assess dietary change is available in Table 1 and Additional file 1: Table S1.
Assessment of changes in anthropometry
At baseline and at each annual visit body weight, WC (determined midway between the lowest rib and the iliac crest), and height were precisely measured in duplicate (the average of these 2 measurements was the analyzed value) by dietitians trained and hired for the trial. Dietitians used calibrated scales, anthropometric tape and a wall-mounted stadiometer, respectively; and body mass index (BMI) was calculated. Absolute changes in body weight and WC were calculated as the difference between yearly measured values and values from the previous year.
Assessment of other covariables
A general medical questionnaire was administered on a yearly basis to obtain information on age, sex, educational level, smoking status, hormonal replacement therapy in case of women, T2D status (medically-diagnosed condition self-reported by the participant at inclusion). Leisure-time total physical activity (METs. min/d) was assessed with the Minnesota Leisure-Time Physical Activity Questionnaire validated previously in Spanish men and women [18, 19].
Statistical analyses
Characteristics of the study participants at baseline and during follow-up are presented as mean (SD) for continuous and percent for categorical variables. The average yearly change in each characteristic is presented as mean (5th, 95th percentile).
Multivariable generalized estimating equation (GEE) analyses with robust standard error and autoregressive correlations (based on observed correlation matrices), were used to estimate associations between yearly changes in the consumption of each of the 31 food groups (serving/d) yearly changes in weight (kg) and WC (cm) (all continuous variables). All the models were adjusted for the minimally sufficient adjustment set of covariables, determined using Directed Acyclic Graph (DAG) [20], as implemented in DAGitty software (www.dagitty.net) [21] (Additional file 1: Figure S2): time (years, because there were slight variations in the period between successive visits), sex, center, intervention group (combined MedDiets or control group), age, baseline BMI/WC (depending on outcome) and educational level (higher education/technician, secondary education, primary education/illiterate or missing data), as well as yearly measured changes in smoking status (never, current or former) and physical activity (METs. min/d).
Moreover, for food groups for which the associations with changes in anthropometry were statistically significant, the models were additionally adjusted for intake of other foods simultaneously, to estimate mutually adjusted associations. No multi-collinearity was observed between these food groups (tolerance 0.963–0.996).
The principal analyses were conducted by coding and imputing missing data on changes in body weight, WC, and diet during follow-up with carried-forward values (LOCF) up to last follow-up, death, or the date on which the participant was lost to follow-up, whichever occurred first.
In order to summarize the observed associations between dietary exposures and anthropometry, two global dietary scores (GDSs) were estimated separately for body weight (GDS-Wt) and WC (GDS-WC). For this purpose, yearly changes in the consumption of each food group, which were found to be independently associated with changes in each of our outcome variables were classified into quintiles (Additional file 1: Table S2). For each quintile, different values were assigned ranging from 1 to 5 for these food groups that were inversely associated, or 5 to 1 for foods associated positively with changes in our outcomes. The final score was created summing all of these values, which could vary from 9 to 45 points for body weight and from 6 to 30 points for WC; a higher score indicated a dietary pattern inversely associated with weight gain or WC gain. This procedure was repeated for each yearly repeated measurement of diet. To allow direct comparison across scores, GDSs were normalized into z-scores.
In order to minimize false discovery rate due to multiple comparisons, GDSs were used as a summary measure of the overall exposure to a dietary pattern associated with anthropometry, to perform further sensitivity analyses. In that way, plausible interactions between foods within each score were taken into account, capturing their potential synergistic effects. Subgroup analyses were conducted to explore consistency of the associations found across selected subsets according to sex, age at enrollment (< 65 or ≥ 65 years), baseline overall obesity (BMI < 30 or ≥ 30 kg/m2), abdominal obesity (WC < 88 (women) and < 102 cm (men) or ≥ 88 (women) and ≥ 102 cm (men)) and diabetes status (yes/no), as well as intervention group (combined MedDiets or control diet). Analysis across intervention groups was also adjusted for propensity scores (built with 30 baseline covariables) to control for minor (not clinically significant) imbalances in baseline covariables. Tests for GDSs by stratum interactions were also performed.
As part of the sensitivity analyses, analyses with use of GDSs, as well as with the food groups that were found to be significantly associated with outcomes, were repeated considering observed data (without LOCF imputation), additionally adjusting for changes in total energy intake (to mitigate the effects of measurement error in collected data using self-reported FFQ), and excluding those patients who died during the follow-up period from any cause (5% participants). Moreover, as reported elsewhere [12], in further sensitivity analyses, we took into account deviations from the randomization protocol, excluding 2nd household members and one small clinic (Site D), where participants were not individually allocated (13% participants). Finally, in order to control for overall healthy dietary pattern associated with our food groups, the multivariable model was additionally adjusted for yearly measured changes in adherence to Mediterranean Diet (MedDiet), assessed with a validated in adult Spanish population 14-item Mediterranean Diet Adherence Screener [22].
Statistical analyses were performed using Stata v15.0 program, with statistical significances set at p < 0.05.
Results
In the overall cohort of PREDIMED (Table 1), the greatest changes in dietary habits were observed for increased consumption of EVOO, nuts, and fruits, as well as for decreased consumption of olive oil, sweets and other vegetable oils. These changes are likely to be partly explained by the effects of the dietary intervention. Changes in weight and WC during follow-up were of small magnitude.
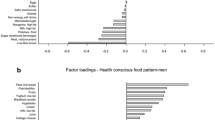
The associations between yearly changes in food group consumption and concurrent body weight and WC changes are shown in Figs. 1 and 2, respectively. Significant increments in weight were observed with increased consumption of refined grains (β 0.32 kg per each increment of 1 additional serving/d; 95% CI 0.09, 0.55 kg), red meat (0.24; 0.02, 0.47), potatoes (0.23; 0.06, 0.40), alcoholic beverages (0.18; 0.11, 0.26), processed meat (0.15; 0.05, 0.25), white bread (0.07; 0.02, 0.12), and sweets (0.04; 0.02, 0.07); whereas lower weight gain was observed with increments in consumption of low-fat yogurt (− 0.18; − 0.33, − 0.04), and low-fat milk (− 0.06; − 0.12, 0.00) (Fig. 1). In turn WC gain occurred with yearly increases in the consumption of snacks, fast-foods and pre-prepared dishes (0.28 cm per each additional increase in 1 serving/d; 0.06, 0.50 cm), processed meat (0.18; 0.03, 0.33), alcoholic beverages (0.13; 0.03, 0.24), and sweets (0.08; 0.04, 0.13); whereas yearly increments in consumption of vegetables (− 0.23; − 0.39, − 0.06) and nuts (− 0.17; − 0.33, − 0.01) were associated with less WC gains (Fig. 2).
Association of yearly changes in food groups intake with concurrent changes in body weight over 5-year of follow-up. β (95% CI) represents the yearly change in body weight (kg) associated with increased/decreased consumption of particular food groups (serving/d). Models used for generalized estimating equation analysis were run separately for each food group and were adjusted for time, sex, center, intervention group, age, baseline BMI and educational level, as well as yearly measured changes in smoking status and physical activity. ASB – artificially-sweetened beverages; EVOO – extra virgin olive oil; SSB – sugar-sweetened beverages
Association of yearly changes in food groups intake with concurrent changes in waist circumference over 5-year of follow-up. β (95% CI) represents the yearly change in waist circumference (cm) associated with increased/decreased consumption of particular food groups (serving/d). Models used for generalized estimating equation analysis were run separately for each food group and were adjusted for time, sex, center, intervention group, age, baseline waist circumference and educational level, as well as yearly measured changes in smoking status and physical activity. ASB – artificially-sweetened beverages; EVOO – extra virgin olive oil; SSB – sugar-sweetened beverages
Mutual adjustment for food groups significantly associated with our outcomes revealed that the overall magnitude and direction of associations shown in Figs. 1 and 2 persisted, showing that the associations of these food groups with anthropometric changes were independent from each other (Table 2). Only the association between increments in consumption of potatoes (0.16 kg; − 0.01, 0.33 kg; p = 0.071), refined grains (0.21; − 0.02, 0.44; p = 0.075), processed meats (0.10; − 0.01, 0.20; p = 0.065) and red meats (0.14; − 0.08, 0.37; p = 0.213) and weight gain were somewhat attenuated (Table 2a).
Then, food groups that showed significant association with each of anthropometry variables were analyzed in combination using a GDS. Overall, yearly increments in each GDS (per 1 SD) were associated with yearly weight changes of − 0.16 kg (95% CI -0.21, − 0.12 kg; p < 0.0001) and WC changes of − 0.27 cm (− 0.35, − 0.20 cm; p < 0.0001) (Table 3). Furthermore, in subgroup analyses we found that the inverse association between diet change and concurrent weight change was stronger among non-diabetics (β − 0.25 kg; 95% CI -0.32, − 0.18 kg; p < 0.0001) than among diabetics (− 0.07 kg; − 0.13, − 0.00 kg; p = 0.037) (p for interaction 0.0001). Moreover, we found that the association between GDS-WC and WC was more pronounced in women (− 0.35 cm; − 0.46, − 0.23 cm; p < 0.0001) than in men (− 0.18 cm; − 0.28, − 0.09 cm; p < 0.0001) (p for interaction 0.019), which could be due to the fact that in women more food groups were significantly associated with changes in WC (Additional file 1: Table S3). Finally, association between GDS-WC and WC was higher in abdominally obese participants (− 0.31 cm; − 0.41, − 0.22 cm; p < 0.0001) than in non-abdominally obese (− 0.18 cm; − 0.31, − 0.05 cm; p = 0.007) (p for interaction 0.042) (Table 3).
The associations between GDS and anthropometry did not change after conducting additional sensitivity analyses (Additional file 1: Table S4).
No relevant changes in effect estimates were detected in the sensitivity analyses conducted for food groups that were significantly associated with weight and WC changes (Additional file 1: Table S5); only, the association between consumption of red meat, processed meat, potatoes, bread and refined grains with weight changes was attenuated after adjusting for concurrent changes in energy intake. On the contrary, associations with WC changes were not modified after adjusting for energy.
Discussion
In our long-term assessment, in an elderly population at high CVD risk, we found that an increments in the consumption of some ultra-processed foods such as snacks, fast-foods, pre-prepared dishes, processed meat, and sweets was associated with changes in WC; whereas increased consumptions of high glycemic index (GI) foods (including white bread, refined grains, potatoes, and sweets) and red and processed meats were associated solely with weight gain. Alcohol intake was associated with higher gains in both weight and WC. In turn, increased intake of some low-fat dairy products was associated with less weight, and intake of vegetables and nuts with less WC gain. In case of the associations between some food items (i.e. potatoes, red and processed meats) and weight change, these associations were attenuated after mutual adjustment for each other or after adjustment for energy; in contrast, most associations with WC changes remained significant after these adjustments. Importantly, these findings were obtained after using repeated yearly measurements of concurrent changes in foods and anthropometry, both evaluated along the same timespan. This is a novelty because previous studies using repeated measurements of diet and weight to assess concurrent changes considered a wider timespan (4 years instead of 1 year) and they relied only in self-reported measures of weight, but not in objectively measured weight and waist [3, 4]. In the PREDIMED trial anthropometric variables were repeatedly collected in duplicate (the average of 2 measurements was the analyzed value) every year by dietitians, specifically trained to follow the measurement protocol of the trial.
This work emphasizes previous findings on importance of carbohydrate quality for obesity prevention [23, 24]. Foods that are low in fiber but high in refined carbohydrates or starches, with a high GI, i.e. white bread, refined grains, potatoes or sweets, were associated with higher weight gains. These results are consistent with previous longitudinal studies [3, 25, 26] and short-term trials [27]. Thus, it is likely that the observed positive link between refined carbohydrates or starches and weight gain is mediated through nutritional factors, such as fiber content, GI and added simple sugars. High-GI foods are less satiating, inducing hunger and overconsumption, and enhance lipogenesis, as compared to low-GI and high-fiber foods [27, 28]. Nevertheless, mutual adjustment for other food groups attenuated the link between refined grains and potatoes with weight gain, suggesting that this association may be explained by combining effect of other unfavorable foods usually consumed with refined grains and potatoes i.e. red and processed meat. Similarly, after adjusting for changes in energy, these associations were attenuated, which may indicate that a plausible mechanism of action is related to alterations of the energy balance.
Low-fat dairy products have been included in American Dietary Guidelines for disease prevention and overall health. In line with these recommendations we found an inverse association between the intake of both low-fat milk and low-fat yogurt and changes in weight; while no association was found for whole-fat milk and yogurt. The plausible mechanism might be related to calcium, casein or biopeptides, whether it could be related to fat content deserves future investigations. For comparison, prior longitudinal studies evaluating dairy-obesity relationships showed protective roles for high-fat dairy products against weight gain, and reported null association for low-fat dairy in younger and healthier American cohorts [29, 30]. The discrepancy between the findings across longitudinal studies might be attributed to differences in exposure variable categorization and measurement (baseline intake or changes over time); or to the fact that whole-fat dairy is not consumed much in this cohort, potentially limiting the ability to detect possible associations.
In concordance with a majority of prior prospective reports [3, 4, 31], this study supports the hypothesis that red and processed meat predict long-term weight gains. This positive association might be attributed to high-energy density, high content of cholesterol, saturated fatty acid (SFA), sodium and other additives as nitrates (processed meat), as well as synergistic effect with detrimental dietary or lifestyle patterns associated with meat intake [26, 32]. It has been also postulated that intake of dietary protein may help to maintain lean mass in older adults [33], thus the use of body weight as outcome rather than adiposity might be misleading. In our previous analysis conducted in other cohort of older subjects with overweight/obesity and metabolic syndrome, we have postulated that alternative measures of WC might serve as plausible options to assess changes in adiposity, in case in which more precise methods cannot be applied. In this regard, our investigation found positive associations between processed meat and red meat (the latter statistically non-significant), with WC changes. This is in line with the results from a recent systematic review and meta-analysis of observational studies [32].
Regarding alcohol use, prior studies reported a positive association with weight gain among heavy drinkers and spirits drinkers, whereas light-to-moderate alcohol intake, especially wine, was found protective [34]. In our investigation, overall alcohol intake was consistently and positively associated with weight and WC gain, as well as in two other large longitudinal studies among middle-aged Europeans and Americans [3, 5]. Our secondary analysis showed that the different alcohol subtypes showed similar associations with weight and waist. Despite high energy content, the plausible mechanisms may include appetite enhancement [35] and lipid oxidation reduction [36], but also consumption of alcohol might mirror unhealthy lifestyles that lead to overall and abdominal obesity. However, futures studies with comprehensive set of confounders and modifiers (frequency, subtypes, alcohol history and obesity tendency) are warranted.
Recently, an increased attention has been given to the detrimental association between SSB consumption and obesity or weight gain [37]. In turn, in our analysis we could not support those findings. However, the point estimates and most of the confidence interval showed results that were compatible with increased weight and WC in association with SSB consumption. The wide confidence intervals could be attributed to the fact that previous studies included participants of younger age groups [3, 5], in which the consumption of SSB is usually higher than that observed in the PREDIMED cohort.
Convenient and palatable ultra-processed foods contribute to obesity epidemic, supplying excessive amount of SFA, trans fat, added sugars, and sodium [38, 39]. In this regard, in our study WC gain was associated with higher consumption of sweets, snacks, fast-foods and pre-prepared dishes. Similarly, prior large longitudinal studies of younger US and European citizens found that fast foods, French fries, potato chips, sweets were associated with higher WC [5, 40]. Thus, abdominal obesity prevention should put particular attention on these foods, which due to its hyper-palatability and conveniency tend to be consumed in excess replacing healthier and more satiating options.
Dietary fiber has been associated with less visceral fat [41], and the possible mechanisms include satiety effect released by increasing food volume and lowering glycemic and insulinemic response to a meal [42], as well as improvement of gut microbiome. An inverse association of vegetables intake with WC changes in our study is in accordance with previous longitudinal studies using baseline dietary information [5, 40]. However, unlike in those studies, we did not reveal an inverse association with fruits; this might be attributed to the seasonal fluctuations in fruits intake and warrants future studies. Furthermore, nuts are a special case of fiber-rich food that is also rich in fats, albeit mostly unsaturated. It is likely that despite fiber and bioactive compounds, vegetable protein and fatty acids found in nuts exert anti-obesity effect by increasing thermogenesis, resting energy expenditure and oxidation [43, 44]. Previous analysis based on the present cohort showed that an increase in vegetable fat intake from natural sources as nuts and EVOO, implemented in the setting of MedDiet, has significant effect on weight reduction and lesser age-related increases in WC [10]. In this longitudinal analysis we found nuts negatively associated with changes in WC, but not weight. Future investigations should establish whether the association on abdominal obesity is due to specific nutrient properties or displacement of unfavorable foods.
We acknowledge several study limitations, as these analyses are exploratory within the PREDIMED trial, and findings are limited to white, elderly Spanish subjects at high CVD risk. Whilst changes in adiposity were objectively measured at each time point (WC and body weight), anthropometry is less accurate than direct methods (i.e. imaging techniques) to assess changes in body composition in elderly. Although food groups intake was assessed using validated FFQ, the self-reporting may always be biased. However, data on dietary intake were collected yearly to capture changes over follow-up, and a dietitian checked the FFQ with the participant to ensure that no missing data exist. Moreover, the use of FFQ does not capture sufficient details on how the food is prepared and consumed. Despite using portion sizes, residual and unmeasured variation in portion sizes might influence the associations. Due to the high number of food groups studied chance finding cannot be excluded, and as in any observational study the causality cannot be inferred.
Besides the long-term prospective design, direct measurements of anthropometry, and assessment of concurrent changes in diet with anthropometry evaluated along the same timespan, strengths of this study also include large sample size, wide spectrum of foods comprised only healthy or unhealthy items, use of standardized protocols and validated tools for anthropometry and dietary measurements, assessment of habitual dietary pattern (without energy-restrictions, supplementation or physical activity program), control for covariables, and inclusion of LOCF method. In contrary to prior observational studies [3,4,5], study sample included elderly participants with a great prevalence of obesity and health risk, who comprise increasing component in our societies.
In conclusion, this prospective study on concurrent changes in diet and anthropometry performed among elderly subjects at high CVD risk, revealed that rather than focusing on total calories amount, modifications in the consumption of specific food groups have a potential to prevent overall and abdominal obesity. Future studies with more precise imaging techniques are warranted to confirm findings on WC. Finally, the effect of dietary patterns rather than individual food groups, in combination with other lifestyle determinants should be studied, in order to better extrapolate these findings into public health recommendations.
Availability of data and materials
The datasets generated and/or analyzed during the current study are not publicly available due to the PREDIMED confidentiality policies.
Abbreviations
- BMI:
-
Body mass index
- CVD:
-
Cardiovascular disease
- DAG:
-
Directed acyclic graph
- EVOO:
-
Extra-virgin olive oil
- FFQ:
-
Food Frequency Questionnaire
- GDS:
-
Global dietary score
- GDS-WC:
-
Global dietary score for waist circumference
- GDS-Wt:
-
Global dietary score for body weight
- GEE:
-
Generalized estimating equation
- GI:
-
Glycemic index
- LOCF:
-
Last observation carried-forward
- MedDiet:
-
Mediterranean diet
- PREDIMED:
-
Prevención con Dieta Mediterránea
- SFA:
-
Saturated fatty acid
- SSB:
-
Sugar-sweetened beverages
- T2D:
-
Type 2 diabetes
- WC:
-
Waist circumference
References
Mozaffarian D, Mande H, Griffin T, Mason JB, Micha R. Topics and comments to be examined in the review of the scientific evidence supporting the development of the 2020–2025 Dietary Guidelines for Americans. Docket No. FNS-2018–0005-000; 2018.
Tapsell LC, Neale EP, Satija A, Hu FB. Foods, nutrients, and dietary patterns: interconnections and implications for dietary guidelines. Adv Nutr. 2016;7:445–54.
Mozaffarian D, Hao T, Rimm EB, Willett WC, Hu FB. Changes in diet and lifestyle and long-term weight gain in women and men. N Engl J Med. 2011;364:2392–404.
Smith JD, Hou T, Ludwig DS, Rimm EB, Willett W, Hu FB, et al. Changes in intake of protein foods, carbohydrate amount and quality, and long-term weight change: results from 3 prospective cohorts. Am J Clin Nutr. 2015;101:1216–24.
Romaguera D, Ängquist L, Du H, Jakobsen MU, Forouhi NG, Halkjær J, et al. Food composition of the diet in relation to changes in waist circumference adjusted for body mass index. PLoS One. 2011;6:e23384.
Smith JD, Hou T, Hu FB, Rimm EB, Spiegelman D, Willett WC, et al. A comparison of different methods for evaluating diet, physical activity, and long-term weight gain in 3 prospective cohort studies. J Nutr. 2015;145:2527–34.
Flegal KM, Kit BK, Orpana H, Graubard BI. Association of all-Cause Mortality with Overweight and Obesity Using Standard Body Mass Index Categories. JAMA. 2013;309:71.
Adams KF, Schatzkin A, Harris TB, Kipnis V, Mouw T, Ballard-Barbash R, et al. Overweight, obesity, and mortality in a large prospective cohort of persons 50 to 71 years old. N Engl J Med. 2006;355:763–78.
Afshin A, Forouzanfar MH, Reitsma MB, Sur P, Estep K, Lee A, et al. Health effects of overweight and obesity in 195 countries over 25 years. N Engl J Med. 2017;377:13–27 Massachussetts Medical Society.
Estruch R, Martínez-González MA, Corella D, Salas-Salvadó J, Fitó M, Chiva-Blanch G, et al. Effect of a high-fat Mediterranean diet on bodyweight and waist circumference: a prespecified secondary outcomes analysis of the PREDIMED randomised controlled trial. Lancet Diabetes Endocrinol. 2019;7:e6–17 Lancet Publishing Group.
Martínez-González MA, Corella D, Salas-Salvadó J, Ros E, Covas MI, Fiol M, et al. Cohort profile: design and methods of the PREDIMED study. Int J Epidemiol. 2012;41:377–85.
Estruch R, Ros E, Salas-Salvadó J, Covas M-I, Corella D, Arós F, et al. Primary prevention of cardiovascular disease with a Mediterranean diet supplemented with extra-virgin olive oil or nuts. N Engl J Med. 2018;378:e34.
Lachat C, Hawwash D, Ocké MC, Berg C, Forsum E, Hörnell A, et al. Strengthening the reporting of observational studies in epidemiology—nutritional epidemiology (STROBE-nut): an extension of the STROBE statement. PLoS Med. 2016;13:e1002036.
Willett W. Issues in analysis and presentation of dietary data. In: Willett W, editor. Nutritional epidemiology. 3rd ed. New York: Oxford University Press; 2013. p. 306.
Fernández-Ballart JD, Piñol JL, Zazpe I, Corella D, Carrasco P, Toledo E, et al. Relative validity of a semi-quantitative food-frequency questionnaire in an elderly Mediterranean population of Spain. Br J Nutr. 2010;103:1808–16.
Mataix, J. Tablas de Composición de Alimentos [food composition tables]. 4th ed. Granada, Spain: Universidad de Granada; 2003.
Moreiras O, Carbajal A, Cabrera L, Cuadrado C. Tablas de composición de alimentos: guía de prácticas [food composition tables: practical guides]. 19th ed. Madrid, Spain: Ediciones Piramide; 2018.
Elosua R, Marrugat J, Molina L, Pons S, Pujol E. Validation of the Minnesota leisure time physical activity questionnaire in Spanish men. Am J Epidemiol. 1994;139:1197–209.
Elosua R, Garcia M, Aguilar A, Molina L, Covas M-I, Marrugat J. Validation of the Minnesota Leisure Time Physical Activity Questionnaire in Spanish Women. Med Sci Sports Exerc. 2000;32:1431–7 American College of Sports Medicine.
Greenland S, Pearl J, Robins JM. Caual diagrams for epidemiologic research. Epidemiology. 1999;10:37–48.
Textor J, van der Zander B, Gilthorpe MS, Liśkiewicz M, Ellison GT. Robust causal inference using directed acyclic graphs: The R package “dagitty”. Int J Epidemiol. 2016;45:1887–94.
Schröder H, Fitó M, Estruch R, Martínez-González MA, Corella D, Salas-Salvadó J, et al. A short screener is valid for assessing Mediterranean diet adherence among older Spanish men and women. J Nutr. 2011;141:1140–5 Oxford University Press.
Reynolds A, Mann J, Cummings J, Winter N, Mete E, Te Morenga L. Carbohydrate quality and human health: a series of systematic reviews and meta-analyses. Lancet. 2019;393:434–45.
Santiago S, Zazpe I, Bes-Rastrollo M, Sánchez-Tainta A, Sayón-Orea C, de la Fuente-Arrillaga C, et al. Carbohydrate quality, weight change and incident obesity in a Mediterranean cohort: the SUN project. Eur J Clin Nutr. 2015;69:297–302.
Bautista-Castaño I, Sánchez-Villegas A, Estruch R, Martínez-González MA, Corella D, Salas-Salvadó J, et al. Changes in bread consumption and 4-year changes in adiposity in Spanish subjects at high cardiovascular risk. Br J Nutr. 2013;110:337–46.
Fogelholm M, Anderssen S, Gunnarsdottir I, Lahti-Koski M. Dietary macronutrients and food consumption as determinants of long-term weight change in adult populations: a systematic literature review. Food Nutr Res. 2012;56:19103.
Bornet FRJ, Jardy-Gennetier A-E, Jacquet N, Stowell J. Glycaemic response to foods: impact on satiety and long-term weight regulation. Appetite. 2007;49:535–53.
Ludwig DS. Dietary glycemic index and obesity. J Nutr. 2000;130:280S–3S.
Wang H, Fox CS, Troy LM, Mckeown NM, Jacques PF. Longitudinal association of dairy consumption with the changes in blood pressure and the risk of incident hypertension: the Framingham heart study. Br J Nutr. 2015;114:1887–99.
Rautiainen S, Wang L, Lee I-M, Manson JE, Buring JE, Sesso HD. Dairy consumption in association with weight change and risk of becoming overweight or obese in middle-aged and older women: a prospective cohort study. Am J Clin Nutr. 2016;103:979–88.
Vergnaud A-C, Norat T, Romaguera D, Mouw T, May AM, Travier N, et al. Meat consumption and prospective weight change in participants of the EPIC-PANACEA study. Am J Clin Nutr. 2010;92:398–407.
Rouhani MH, Salehi-Abargouei A, Surkan PJ, Azadbakht L. Is there a relationship between red or processed meat intake and obesity? A systematic review and meta-analysis of observational studies. Obes Rev. 2014;15:740–8.
Houston DK, Nicklas BJ, Ding J, Harris TB, Tylavsky FA, Newman AB, et al. Dietary protein intake is associated with lean mass change in older, community-dwelling adults: the health, aging, and body composition (health ABC) study. Am J Clin Nutr. 2008;87:150–5.
Sayon-Orea C, Martinez-Gonzalez MA, Bes-Rastrollo M. Alcohol consumption and body weight: a systematic review. Nutr Rev. 2011;69:419–31.
Yeomans MR. Alcohol, appetite and energy balance: is alcohol intake a risk factor for obesity? Physiol Behav. 2010;100:82–9.
Suter PM, Tremblay A. Is alcohol consumption a risk factor for weight gain and obesity? Crit Rev Clin Lab Sci. 2005;42:197–227.
Luger M, Lafontan M, Bes-Rastrollo M, Winzer E, Yumuk V, Farpour-Lambert N. Sugar-sweetened beverages and weight gain in children and adults: a systematic review from 2013 to 2015 and a comparison with previous studies. Obes Facts. 2017;10:674–93 Karger Publishers.
Moubarac J-C, Parra DC, Cannon G, Monteiro CA. Food classification systems based on food processing: significance and implications for policies and actions: a systematic literature review and assessment. Curr Obes Rep. 2014;3:256–72.
de Mendonça RD, Pimenta AM, Gea A, de la Fuente-Arrillaga C, Martinez-Gonzalez MA, Lopes ACS, et al. Ultraprocessed food consumption and risk of overweight and obesity: the University of Navarra Follow-Up (SUN) cohort study. Am J Clin Nutr. 2016;104:1433–40.
Halkjær J, Tjønneland A, Overvad K, Sørensen TIA. Dietary predictors of 5-year changes in waist circumference. J Am Diet Assoc. 2009;109:1356–66.
Davis JN, Alexander KE, Ventura EE, Toledo-Corral CM, Goran MI. Inverse relation between dietary fiber intake and visceral adiposity in overweight Latino youth. Am J Clin Nutr. 2009;90:1160–6.
Lundin EA, Zhang JX, Lairon D, Tidehag P, Åman P, Adlercreutz H, et al. Effects of meal frequency and high-fibre rye-bread diet on glucose and lipid metabolism and ileal excretion of energy and sterols in ileostomy subjects. Eur J Clin Nutr. 2004;58:1410–9.
Tindall AM, Petersen KS, Lamendella R, Shearer GC, Murray-Kolb LE, Proctor DN, et al. Tree nut consumption and adipose tissue mass: mechanisms of action. Curr Dev Nutr. 2018;2.
Jackson CL, Hu FB. Long-term associations of nut consumption with body weight and obesity. Am J Clin Nutr. 2014;100:408S–11S American Society for Nutrition.
Acknowledgements
We thank all the volunteers for the participation and personnel for their contribution in the PREDIMED trial.
Funding
The research leading to these results was supported by the official Spanish Institutions for funding scientific biomedical research, CIBER Fisiopatología de la Obesidad y Nutrición (CIBEROBN) and Instituto de Salud Carlos III (ISCIII), and through specific grants/contracts: the “FOLIUM” program within the FUTURMed project. Talent for the medicine within the future from the Fundación Instituto de Investigación Sanitaria Illes Balears (financed by 2017 annual plan of the sustainable tourism tax and at 50% with charge to the ESF Operational Program 2014–2020 of the Balearic Islands) [JK]; ERC Advanced Research Grant (340918) [MAM-G as PI]. None of the funding sources took part in the design, collection, analysis or interpretation of the data, or in the decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Contributions
JK, DR, and MAM-G conceived the study and wrote the article, JK, DR, VP, and MAM-G analyzed the data. JK, DR, VP, MF, CR, RE, EMA, NB, MF, EG-G, ER, JL, FA, LS-M, XP, ET, JVS, MB, HS, and MAM-G designed and conducted the project, and obtained the data. All authors revised the manuscript for important intellectual content and read and approved the final manuscript. JK, DR, and MAM-G are the guarantors of this work and, as such, had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
All participants provided written informed consent, and the study protocol and procedures were approved according to the ethical standards of the Declaration of Helsinki by The International Review Board (IRB) of Hospital Clinic in Barcelona, Spain (July 2002). Following this, IRBs of all other centers approved.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Additional file 1: Figure S1.
Flow chart summarizing selection of PREDIMED participants for the present study. Figure S2. Directed acyclic graph (DAG). Table S1. Characterization of food items belonging to each food group. Table S2. Correlations matrix between food groups (serving/d) within each global dietary score (GDS). Table S3. Sensitivity analyses: Association of yearly changes in food groups intake with concurrent changes in waist circumference over 5-year of follow-up by sex. Table S4. Sensitivity analysis: association of changes in global dietary score (GDS) with body weight and waist circumference changes over 5-year of follow-up. Table S5. Sensitivity analysis: association of changes in food groups intake for which associations with body weight (A) and waist circumference (B) changes over 5-year of follow-up were statistically significant.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Konieczna, J., Romaguera, D., Pereira, V. et al. Longitudinal association of changes in diet with changes in body weight and waist circumference in subjects at high cardiovascular risk: the PREDIMED trial. Int J Behav Nutr Phys Act 16, 139 (2019). https://doi.org/10.1186/s12966-019-0893-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12966-019-0893-3