Abstract
Background
Although crime and perceived safety are associated with obesity and body mass index (BMI), the pathways are less clear. Two likely pathways by which crime and perceived safety may impact obesity are through distress and physical activity.
Methods
We examined data from 2013 to 2014 for 644 predominantly African-American adults (mean age 57 years; 77% female) living in low-income Pittsburgh, PA neighborhoods, including self-reported perceptions of safety and emotional distress, interviewer-measured height/weight, and physical activity measured via accelerometry. We used secondary data on neighborhood crime from 2011 to 2013. We built a structural equation model to examine the longitudinal direct and indirect pathways from crime to BMI through perceived safety, distress and physical activity.
Results
Long-term exposure to crime was positively associated with lack of perceived safety (β = 0.11, p = 0.005) and lack of perceived safety was positively associated with BMI (β = 0.08, p = 0.03). The beneficial association between physical activity and BMI (β = −0.15, p < 0.001) was attenuated by a negative association between crime and physical activity (β = −0.09, p = 0.01). Although crime was associated with distress we found no evidence of a path from crime to BMI via distress.
Conclusions
Our findings suggest decrements in perceived safety and physical activity are important processes that might explain why neighborhood crime is associated with greater BMI.
Similar content being viewed by others
Background
African Americans are disproportionately affected by obesity [1] and more likely to live in neighborhoods with higher crime rates than whites [2, 3]. Neighborhood crime and perceived lack of safety have been associated with psychological distress [4, 5], poor health [6,7,8,9], limited physical activity [10,11,12,13,14], and obesity [15, 16]. Literature on objective crime measures and their association with obesity, BMI and physical activity supports associations between neighborhood safety and activity [12, 17, 18]. However, the role of crime, varying degrees of perceived safety and the intersection of these factors in influencing resident distress, physical activity, and BMI are not well understood (see reviews [19,20,21]), especially in low-income, African American populations [22, 23].
Neighborhoods provide environments that may promote or limit health-related behaviors [24]. Increasing evidence has shown objectively measured crime and perceived lack of safety to increase stress, limit physical activity because of safety concerns, and therefore influence obesity [12, 25]. Several plausible pathways exist through which neighborhood crime could influence obesity. Chronic activation of the physiologic stress system resulting from crime exposure could lead to obesity, given how cortisol production increases BMI [26,27,28,29]. Another path from crime to obesity could operate through perceived lack of safety to physical activity. Understanding residents’ perceptions of neighborhood safety and their role in resident health could help identify ways to support resilience in disadvantaged neighborhoods [30]. Much of the existing evidence is based on self-reported physical activity and anthropometry, which are subject to reporting bias [31, 32]. Furthermore, much of the cross-sectional research focuses on direct associations between crime/perceived safety and obesity/BMI without considering two mediating pathways through distress and physical activity.
Among the few studies examining pathways, Roman et al., used structural (SEM) equation modeling with data from two deprived Chicago neighborhoods (n = 328, mean age 47 years) to examine the direct and indirect pathways from perceptions of neighborhood violence and disorder to obesity through fear of walking [5]. Perceived violence was positively associated with fear of walking but not with physical activity or obesity. However, this cross-sectional study relied on self-reported anthropometry and physical activity. A cross-sectional study of 864 adults from a low-income and ethnically mixed neighborhood in Salt Lake City, UT used objectively measured anthropometry and physical activity [11]. They found that low perceived safety was associated with high BMI and that lower moderate-to-vigorous physical activity partially explained the relationship between safety and BMI. Yet the authors were unable to examine how crime may relate to perceived safety.
It remains unclear how peoples’ perceptions of crime impact their sense of safety, in part, because no consensus exists on whether the location and timing of crime incidents influences resident perceptions. Understanding the types, location and timing of crimes and their relationship with perceptions of safety is necessary in order to robustly model an indirect pathway whereby crime influences BMI through perceived safety using the objective measure that is most strongly associated with perceived safety.
Prior studies have examined crime across a wide range of geographic areas (e.g., census block group [33], census tract [15], half-mile [15], and 1-mile [13]) surrounding residents’ homes in association with physical activity, diet and BMI. But it is unknown how proximity from crimes, or the timing at which crimes occurred, may be associated with physical activity and health. In one study, agreement was poor between objective measures of crime and perceived fear across 1-, half-, and eighth-mile buffers but agreement appeared to increase with decreasing buffer size [18]. This study was limited by small sample size (n = 303) and crimes were aggregated to an annual rate, ignoring more detailed timing of the occurrences (e.g., a month versus a year ago). In addition, much of the research on the role of crime in neighborhoods has not considered influences on health from crimes occurring with varying degrees of proximity [34].
In sum, limitations of research on neighborhood crime, perceptions, behaviors, obesity, and distress include the lack of studies that use objectively measured data (crime, physical activity, and BMI), to examine longitudinal pathways to resident health, and to examine patterns of association with crime across different levels of crime aggregation (over space and time). To address these gaps, this longitudinal study examined how proximity and timing of crime related to perceptions of safety in two predominantly African American low-income Pittsburgh neighborhoods. We then derived a long-term measure of neighborhood crime based on these associations. In a SEM, we tested direct and indirect pathways from long-term exposure to neighborhood crime (prior 2 years) to BMI a year later through perceived safety and the two likely additional mediating pathways, distress and physical activity.
Methods
Study population and participants
Pittsburgh Research on Neighborhoods, Exercise and Health (also known as ‘PHRESH Plus’) was designed to document and evaluate neighborhood investments in greenspace and housing on physical activity and active transport in lower-income African American neighborhoods in Pittsburgh. The sample includes randomly selected households from two communities who are part of a cohort followed over time. The Hill District neighborhood has and continues to undergo neighborhood economic investments, including renovation of greenspace for recreational activities. Homewood, the comparison neighborhood, although experiencing some investment and change, did not experience the same degree of investment. This study uses the PHRESH Plus baseline data (collected Spring 2013), prior to major greenspace and housing renovations, and follow-up data on the same cohort members from a sister PHRESH study (collected in Spring 2014). Data collection included neighborhood-level built and social characteristics, and detailed individual-level data. All study protocols were approved by the institution’s Institutional Review Board.
Outcome variable: Body mass index (BMI) (2014)
Interviewers measured height (without shoes) to the nearest eighth inch using a carpenter’s square and an 8-ft folding wooden ruler marked in inches. Weight was measured to the nearest tenth of a pound using the SECA Robusta 813 digital scale. BMI was calculated as weight in kg divided by height in m2.
Exposure variable: Neighborhood-level crime (2011–2013)
Incident-level crime data was provided by the City of Pittsburgh police department which contained comprehensive lists of all reported crimes in Pittsburgh for 2 years preceding the household survey administration (i.e., 2011–2013). We calculated street network distances from each household to crime locations for all types (e.g., robbery, assault, etc.) using ArcGIS 10.2. We geocoded 95% of the incidents using address information. To assess how different crime measures are associated with perceived safety we first calculated them across varying distances from the residents’ homes, summing the number of crimes that occurred within 1/10-, 1/4-, 1/2-, and 3/4-mile radial distances from each household address. To assess how timing of the criminal activity is associated with perceived safety we summed the number of crimes that occurred within 1 month, 3 months, 6 months, 1 year and 2 years prior to the date the respondent was interviewed in 2013. We created 20 crime measures total (e.g., crimes that occurred within last month and ½ mile of the residents’ residence) for each combination of timing and proximity. Because the crime measures are aggregated to buffers surrounding the respondents’ residence they are respondent-based exposures (i.e., a crime can be counted multiple times in the sample for different individuals depending on their residential location). Thus, we used counts of crime rather than neighborhood population-based rates.
To assess long-term exposure to neighborhood crime we used the measure that was most sensitive to perceived safety and averaged it over the 2 years preceding the interview date.
Intermediate variables (2013)
Perceived safety
Study interviewers administered questionnaires and residents answered the question “Your neighborhood is safe from crime” using a five-point disagree-agree scale. We reverse coded responses so that higher values reflected lack of perceived safety because of neighborhood crime.
Psychological distress
The Kessler 6 (K6) psychological distress scale is a self-report instrument to assess psychological distress [35]. We chose the K6 because it is a well-validated measure of psychological distress that can detect the presence of mild to severe psychological problems with high levels of sensitivity and specificity in a wide variety of populations [36]. As such, it has indeed been linked with cortisol in prior research [37]. Data collectors asked residents the frequency with which they experienced distress symptoms (e.g., “feel hopeless”; “feel restless or fidgety”) in the last 30 days. Responses were on a five-point scale. Scores were summed into a single score where high values reflect distress. K6 scores can be interpreted as no or low distress = 0–4 points, moderate distress = 5–12 points, or severe distress = 13–24 points [38].
Objectively measured physical activity
Participants were given a tri-axial accelerometer (i.e., ActiGraph GT3X+) and asked to wear the device on their non-dominant wrist for 7 consecutive (24 h) days. Data were sampled at 30 hz and summarized into 60 s epochs. Non-wear was determined based on the Choi algorithm using vector magnitude values [39]. Sleep intervals were identified from daily bed and wake times reported by the participant. When these times were not available or irregular (e.g., > 12 h or < 3 h sleep interval; suspected inaccurate date recorded by the participant), further visual inspection of the raw accelerometer signal was used to supplement the recorded data. All sleep interval data was removed from analyses. Further, because participants did not report their bed times on the first day the monitor was worn, the first full 24 h of recording was removed to ensure that no sleep time was included in vector magnitude calculations. Vector magnitude is the square root of the sum of the three squared axes [e.g., (x2 + y2 + z2)1/2]. Data were processed in ActiLife v6.13.1. The daily average of vector magnitude counts per minute was averaged across all days with at least 10 h of wear time. A participant was included in the analysis if he/she had at least 3 days of valid wear and their vector magnitude counts were analyzed continuously. While no vector magnitude cut points for the ActiGraph wrist exist yet for sedentary activity, a 2000 counts per minute cut point was identified in 94 older women to be very low activity [40].
Individual-level covariates (2013)
Below, we describe the variables we used as covariates in models. Residents provided information on date of birth, gender, education (categorized into at least some college/bachelor’s degree versus less than college), and marital/cohabitation status (married or living with a partner versus living alone). We also included annual income per capita (we imputed missing values n = 45). We did not control for race/ethnicity because the majority of the sample (92%) self-identified as Black or African American. To capture physical activity limitation we used their responses to the question “Does your health limit you when walking one block?” which we dichotomized to “a little or a lot” versus “not at all.” To account for unmeasured differences across neighborhoods that could confound associations between crime and obesity, we controlled for neighborhood, using a binary indicator of Hill District versus Homewood. Social networks may mitigate negative effects of crime on health and well-being [7] by providing positive support and social cohesion [41] and might also influence whether crimes occur in one’s neighborhood. Therefore, we also controlled for social network size which was measured using a previously validated scale [42]. Participants reported the number of people they knew (e.g., family, close friends, neighbors, etc.). The number of people in each category was summed to compute each participant’s social network size.
Analytic sample
We excluded residents if they did not live in Hill District or Homewood at the time of the 2013 interview (n = 27) (i.e., if they had moved out of the neighborhood from initial enrollment into the study), were missing accelerometry data (n = 98), had less than 3 valid (≥ 10 h) accelerometer days (n = 15), were lost to follow up in 2014 when the BMI outcome was collected (n = 248), were missing crime data (n = 8), or were missing response to the question about perceived safety (n = 198). The final analytic sample included 644 adults who wore the accelerometer for an average of 5.7 ± 0.6 days. We calculated T-tests (continuous variables) and Chi-Square tests (categorical variables) to compare the included versus excluded (n = 397) residents. We compared all covariate, intermediate and, outcome variables between excluded individuals and individuals included, and only age and social network size differed. Those individuals excluded were younger (mean age 53 years vs 57 years among the included, p = < 0.001) and had fewer social network members (mean 28 vs 48 among the included, p = < 0.001).
Statistical analyses
We performed descriptive analyses and tested multivariable models using Stata 14.0 (StataCorp, College Station, TX). We calculated means and standard deviations (continuous variables) and percentages (categorical variables) of individual-level – and neighborhood-level crime. To identify the timing and proximity of crime most sensitive (based on relative magnitude of association) to perceived safety, we used logit models to predict perceived safety as a function of 20 different crime measures. We estimated separate models for counts of crime by time and proximity. We controlled for age, gender, education, married or living with a partner, physical limitation, neighborhood, social network size, and household income in these crime-safety tests. To illustrate the magnitude of the associations we plotted a three-dimensional bar graph of the logit estimates (y-axis) by crime timing (x-axis) and distance (z-axis).
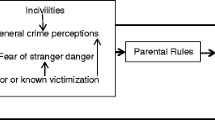
To examine longitudinal indirect pathways from crime to later BMI through perceived safety, psychological distress and physical activity, we used Mplus version 7.11 [43] to build a SEM. We used the measure of crime that emerged as the best predictor of perceived safety in the above analyses and averaged it over the 2 years preceding the respondents’ interview to derive a measure that is sensitive to perceived safety and also captures long-term exposure to crime. We allowed for a direct pathway from crime to BMI. Given that there may be bidirectional associations between distress and physical activity [44, 45], we also tested whether distress and physical activity covaried (double-headed curved arrow in Fig. 1). Figure 1 presents our conceptual model. We controlled for the above-mentioned covariates to address confounding of associations between: (1) crime and BMI (exposure to outcome); (2) perceived safety, physical activity, and BMI (mediators to outcome); (3) crime, perceived safety, distress, and physical activity (exposure to mediators) that were not likely to be affected by crime [46]. A statistically non-significant Chi-Square test statistic [47], Root Mean Square Error of Approximation (RMSEA) < 0.06 [48], and Comparative Fit Index (CFI) values approaching 1.0 [49] imply the model fits the data well.
Results
In 2013, the analytic sample was on average 57 years of age, low-income (mean per capita income $13,400), burdened with low mobility, and overweight in 2014 (mean body mass index (kg/m2) was 31 kg/m2 (Table 1 ).
About one fifth of the cohort was married or living with a partner (19%), and an average vector magnitude of 2140 cpm suggests very low activity [40, 50]. The cohort reports relatively low distress with a mean of 4.3. The average number of crime exposures ranged from about 2 to 1424 depending on distance from residence and time frame (Table 2).
We associated 1) residents’ perceived neighborhood safety with 2) counts of crimes in varying time frames preceding the 2013 interview and 3) distance from the residence. Figure 2 shows plots of the magnitude of the logit beta estimates (y-axis) across the time frame of the crimes (x-axis) and the distance from residents’ residence (z-axis). Most estimates were statistically significant (p < 0.05, data not shown). Magnitude of the association between crime and perceived safety increased as distance between crime and participants’ residence decreased and as timing was closer to the interview. Perceived safety was most strongly associated with crimes that occurred within 1/10-mile from the resident’s home, and those that that happened within the month preceding the interview. Although the correlation between perceived safety and crimes within 1/10-mile and 1 month was not significant (Pearson’s correlation coefficient = 0.06, p = 0.11), which is likely due to the small number of crimes that occurred within 1/10 mile and the 1 month timeframe.
To address temporality, we created an average of crime over a longer period of time. First, we derived a monthly count of crime for each respondent for each month over 2 years (2011–2013) preceding the date of the resident’s interview (2013). Next, we averaged the monthly counts across the 2 years by summing the counts and dividing by 24 (mean = 1.84 crimes per month SD = 1.5). This captures the importance of crime timing to concurrent perceptions of safety, while providing an indicator of such over a longer period of time in order to better predict slow-changing BMI.
In our initial model, the covariance path between distress and physical activity was not statistically significant (p = 0.35) and model fit was not ideal (RMSEA = 0.00, CFI = 1.00, Chi-Square = 0.00 (0 df) p = < 0.001). The SEM model deleting this path fit the data well (RMSEA = 0.00, CFI = 1.00, Chi-Square = 0.02 (1 df) p = 0.88. Figure 3 presents this result. For clarity, we present only associations that were statistically significant (p < 0.05). Long-term exposure to crime was indirectly associated with BMI through perceived safety. We saw a positive association between the average monthly number of nearby crimes and lack of perceived safety (β = 0.11, p = 0.005) and lack of perceived safety was positively associated with BMI a year later (β = 0.08, p = 0.03). Physical activity also appeared to serve as an indirect pathway between crime and later BMI. Crime was associated with reduced physical activity (β = −0.09, p = 0.009), and physical activity was negatively associated with BMI (β = −0.15, p < 0.001). Crime was also associated with distress, but because distress was not predictive of BMI, distress does not serve as a pathway between crime and this outcome, nor does it explain associations between perceived safety and BMI. Finally, we find no direct association between crime and BMI, suggesting that the indirect paths through perceived safety and physical activity, account entirely for the association between these two variables.
Discussion
We found that objectively measured long-term exposure to crime is associated with higher BMI at a later point in time through two separate paths, lack of perceived safety and decreased physical activity. Unexpectedly, distress did not explain associations between objectively measured crime, lack of perceived safety and BMI, suggesting other processes could be at play along this particular path. Future work may be warranted exploring other potential pathways. For example, lack of perceived safety may impact neighborhood cohesion or disorder and subsequently have downstream impacts on BMI via social fragmentation and isolation [51,52,53] that promote poor dietary behaviors. Our covariate measure of social network size may not have adequately captured such a process.
Lack of perceived safety appeared to mediate the pathway between objective crime and BMI. Thus, it is possible that perception of crime is more acutely relevant to BMI than objectively reported crime events in one’s neighborhood. This is consistent with other studies showing that perceptions of neighborhood conditions are more strongly associated with health outcomes than objective measures [54,55,56].
Perceived safety was not associated with physical activity, contradicting prior findings indicating that residents who felt safe in their neighborhood were more likely to walk [12, 57, 58] and be physically active [11]. However, some studies have found no association between safety perceptions and physical activity [10]. One of the first studies to examine how changes in crime and perceptions associated with walking over time found little evidence that perceived safety or police-reported crime associated with walking [13]. Fear is another reaction to crime and is a distinct construct from perceived safety, although the two constructs are correlated and both empirically linked with health [59]. Given the apparent links between neighborhood crime, fear and health [8, 60], fear may be more salient to physical activity than perceived safety. A longitudinal study in Perth, Australia, (n = 531) among adults (mean age 40 years) reported that perceived safety was associated with increased time walking [12]. Yet, in an earlier publication this same group reported that fear of crime was also associated with walking time and the effect size was stronger for fear than for perceived safety (22 min/wk. vs 20 min/wk). Future research should test whether fear is more salient to ones’ decision to engage in physical activity than perceived safety. While future research should examine pathways through which both perceived safety and fear may mediate associations between crime, and BMI, it is beyond the scope of this paper. Our survey asked the residents how safe their neighborhood was from crime so we opted to use this specific measure of perceived safety.
Our study population is urban, low-income, predominantly African American and sedentary so findings may not be generalizable. Given uncertainty in cut points, we analyzed vector magnitude as a continuous variable where vector magnitude is a volume measure of activity that may (or not) happen in the neighborhood. The average vector magnitude in our study was 2124.7 which is not much more than the 2000 cut point identified in 94 older women as sedentary [40]. Nonetheless, it is an important group of interest to both the study of crime and the study of overweight.
Another issue underlying inconsistencies may be the approaches used to quantify feeling safe in prior studies, such as using composite scores that include questions about walking at night and aesthetics [61, 62], unattended dogs, and safety jogging [63], or worry about being attacked [64]. These measures may tap into slightly different aspects of perceived safety or they may confound perceived safety with other variables. That is, composite measures of perceived safety may conflate other safety-related issues with safety specific to crime. For this reason, we opted to use a single-item measure that directly asked how safe their neighborhood was from crime.
Our finding that lack of perceived safety was associated with higher BMI is consistent with other studies [65,66,67]. Of the few that examine both physical activity and BMI [11, 66, 68, 69], perceived social nuisances (e.g., incivilities) among 14,836 English adults were positively associated with obesity but it was not mediated by physical activity [69]. While the strengths of Poortinga’s study include measured anthropometry and examination of mediation by physical activity they lacked objective measures of crime and physical activity. Another study among 9252 American adults living in urban areas found a positive association between county-level crime and BMI but not between county-level crime and walking [70]. Yet, this study was limited by variation within counties and by modeling physical activity and BMI separately, which does not address potential mediating pathways. Our pathway findings do support the theory that African American adults living in deprived neighborhoods are obese because crime deters physical activity [19] since we found associations between crime, perceived safety, and physical activity.
Some research suggests that people living in deprived areas with high crime rates experience stress that translates into dysregulation of the hypothalamic-pituitary-adrenal that can cause higher BMI [27, 71]. Our findings suggest that high levels of crime increase distress. In another large longitudinal study of older Australian adults that used objective measures of crime an increase in risk of experiencing distress was associated with an increase in neighborhood crime [72]. However, this study did not include perceptions of safety and our findings suggest that distress does not play a role in pathways from crime to BMI.
We also found that the association between number of crimes and lack of perceived safety got progressively stronger as the reference period was defined closer in time to interview and distance from residents’ homes was smaller. We provide evidence that when and where crimes occur is important to consider in studies that link objective measures of crime with resident perceptions of safety. Thus, researchers might not need a long reference period or wide area of assessment in studies of crime and perceived safety. However, in the case when the study outcome is slow to change, such as with BMI, it is also important to consider a method of aggregating such a measure to tap a longer history of immediate (proximal in time and space) exposure.
No consensus exists about the geographic area that best represents a neighborhood [73] and to our knowledge only one study examined how counts of crime aggregated within different distances from residents homes associated with perceived safety [18]. Among 303 adults living in Winston-Salem, NC the number of police service calls within 1-, 1/2-, and 1/8-mile and normalized by population size had low agreement with perceived safety (weighted kappas [95% CI]: 1-mile, .12 [.04–.20]; half-mile, .18 [.10–.26]; eighth-mile, .22 [.14–.30]). However, agreement appears to have been highest when using the crime rate within the closest distance. To our knowledge, no study has explored how the timing of when crimes occur influences perceptions of safety and key health outcomes.
Our study is longitudinal, capturing changes in environment, perceptions, behaviors or health. However, this study has limitations. We could not control for how long participants lived at their current address, which could contribute to a mismeasurement of their crime exposure. However, we did collect information regarding years lived in neighborhood of residence. The participants in our study are a stable population. Only 6% reported living in their neighborhood for less than a year, while 80% of the residents reported living in their neighborhood for over 5 years, and 50% of the residents reported living in their neighborhood for 20 years or more. Participants excluded from this analysis were younger which may have biased our results. Residential location choice is complex and driven by more than health-related preferences. Yet, individual behaviors and health may be tied to unobserved characteristics (e.g., health consciousness [74]) that underlie an individual’s residential location. Thus, residential selection could bias our results. We lacked dietary data at this assessment, so we were unable to test alternate pathways through energy balance. Lastly, our participants were mostly sedentary, so the lack of variation may have limited our ability to detect associations with physical activity.
Despite these limitations we present longitudinal data from a low-income and predominantly African American cohort living in underserved urban neighborhoods that includes historic crime data combined with individual-level perceptions, behaviors, and objectively measured anthropometry and physical activity. Accelerometry is superior to self-report where over-reporting can bias estimates [75]. Similarly, measured heights and weights are less vulnerable to reporting bias than self-report [32]. Further, our study population is often at increased risk of residing in disadvantaged neighborhoods [2, 3], limited physical activity [75, 76] and suffering higher rates of inactivity-related cardiometabolic conditions [77,78,79]. To our knowledge, this is the first analysis linking objective measures of crime and perceived safety, to psychological distress, accelerometry-derived activity, and measured anthropometry in an older, disadvantaged, and predominantly African American population.
Conclusion
This work adds evidence that among African Americans living in urban low-income neighborhoods, lack of perceived safety in one’s neighborhood because of high crime rates is associated with higher BMI, independent of physical activity and distress. Importantly, crime is also associated with higher BMI through less physical activity, but this process is a separate one. Neighborhood investments that reduce crime and improve resident perception of safety remain critical for the wellbeing of communities. Public health professionals and policy makers may consider crime and perception of safety as salient neighborhood factors that could exacerbate obesity in the United States.
Abbreviations
- BMI:
-
Body mass index
- CFI:
-
Comparative fit index
- RMSEA:
-
Root mean square error of approximation
- SEM:
-
Structured equation modeling
References
World Health Organization: WHO global Infobase. 2011.
White K, Borrell LN. Racial/ethnic residential segregation: framing the context of health risk and health disparities. Health Place. 2011;17(2):438–48.
Williams DR, Collins C. Racial residential segregation: a fundamental cause of racial disparities in health. Public Health Rep. 2001;116(5):404–16.
Roberts B, Stickley A, Petticrew M, McKee M. The influence of concern about crime on levels of psychological distress in the former soviet union. J Epidemiol Community Health. 2012;66(5):433–9.
Roman CG, Knight CR, Chalfin A, Popkin SJ. The relation of the perceived environment to fear, physical activity, and health in public housing developments: evidence from Chicago. J Public Health Policy. 2009;30(Suppl 1):S286–308.
Kitchen P, Williams A. Quality of life and perceptions of crime in Saskatoon, Canada. Soc Indic Res. 2010;95(1):33–61.
Lorenc T, Clayton S, Neary D, Whitehead M, Petticrew M, Thomson H, Cummins S, Sowden A, Renton A. Crime, fear of crime, environment, and mental health and wellbeing: mapping review of theories and causal pathways. Health Place. 2012;18(4):757–65.
Ross CE, Mirowsky J. Neighborhood disadvantage, disorder, and health. J Health Soc Behav. 2001;42(3):258–76.
White M, Kasl SV, Zahner GEP, Will JC. Perceived crime in the neighborhood and mental-health of women and children. Environ Behav. 1987;19(5):588–613.
Bracy NL, Millstein RA, Carlson JA, Conway TL, Sallis JF, Saelens BE, Kerr J, Cain KL, Frank LD, King AC. Is the relationship between the built environment and physical activity moderated by perceptions of crime and safety? Int J Behav Nutr Phys. 2014;11 https://doi.org/10.1186/1479-5868-1111-1124.
Brown BB, Werner CM, Smith KR, Tribby CP, Miller HJ. Physical activity mediates the relationship between perceived crime safety and obesity. Prev Med. 2014;66:140–4.
Foster S, Hooper P, Knuiman M, Christian H, Bull F, Giles-Corti B. Safe RESIDential environments? A longitudinal analysis of the influence of crime-related safety on walking. Int J Behav Nutr Phys Act. 2016;13:22.
Kerr Z, Evenson KR, Moore K, Block R, Diez Roux AV. Changes in walking associated with perceived neighborhood safety and police-recorded crime: the multi-ethnic study of atherosclerosis. Prev Med. 2015;73:88–93.
Van Dyck D, Cerin E, De Bourdeaudhuij I, Salvo D, Christiansen LB, Macfarlane D, Owen N, Mitas J, Troelsen J, Aguinaga-Ontoso I, et al. Moderating effects of age, gender and education on the associations of perceived neighborhood environment attributes with accelerometer-based physical activity: the IPEN adult study. Health Place. 2015;36:65–73.
Mujahid MS, Diez Roux AV, Shen M, Gowda D, Sanchez B, Shea S, Jacobs DR Jr, Jackson SA. Relation between neighborhood environments and obesity in the multi-ethnic study of atherosclerosis. Am J Epidemiol. 2008;167(11):1349–57.
Pham do Q, Ommerborn MJ, Hickson DA, Taylor HA, Clark CR. Neighborhood safety and adipose tissue distribution in African Americans: the Jackson heart study. PLoS One. 2014;9(8):e105251.
McDonald NC. The effect of objectively measured crime on walking in minority adults. Am J Health Promot. 2008;22(6):433–6.
McGinn AP, Evenson KR, Herring AH, Huston SL, Rodriguez DA. The association of perceived and objectively measured crime with physical activity: a cross-sectional analysis. J Phys Act Health. 2008;5(1):117–31.
Foster S, Giles-Corti B. The built environment, neighborhood crime and constrained physical activity: an exploration of inconsistent findings. Prev Med. 2008;47(3):241–51.
Van Cauwenberg J, De Bourdeaudhuij I, De Meester F, Van Dyck D, Salmon J, Clarys P, Deforche B. Relationship between the physical environment and physical activity in older adults: a systematic review. Health Place. 2011;17(2):458–69.
Ding D, Gebel K. Built environment, physical activity, and obesity: what have we learned from reviewing the literature? Health Place. 2012;18(1):100–5.
Feng J, Glass TA, Curriero FC, Stewart WF, Schwartz BS. The built environment and obesity: a systematic review of the epidemiologic evidence. Health Place. 2010;16(2):175–90.
Kumanyika SK, Gary TL, Lancaster KJ, Samuel-Hodge CD, Banks-Wallace J, Beech BM, Hughes-Halbert C, Karanja N, Odoms-Young AM, Prewitt TE, et al. Achieving healthy weight in African-American communities: research perspectives and priorities. Obes Res. 2005;13(12):2037–47.
Sallis JF, Bauman A, Pratt M. Environmental and policy interventions to promote physical activity. Am J Prev Med. 1998;15(4):379–97.
Rachele JN, Ghani F, Loh VH, Brown WJ, Turrell G. Associations between physical activity and the neighbourhood social environment: baseline results from the HABITAT multilevel study. Prev Med. 2016;
Barrington WE, Stafford M, Hamer M, Beresford SA, Koepsell T, Steptoe A. Neighborhood socioeconomic deprivation, perceived neighborhood factors, and cortisol responses to induced stress among healthy adults. Health Place. 2014;27:120–6.
Champaneri S, Xu X, Carnethon MR, Bertoni AG, Seeman T, DeSantis AS, Diez Roux A, Shrager S, Golden SH. Diurnal salivary cortisol is associated with body mass index and waist circumference: the multiethnic study of atherosclerosis. Obesity. 2013;21(1):E56–63.
Karb RA, Elliott MR, Dowd JB, Morenoff JD. Neighborhood-level stressors, social support, and diurnal patterns of cortisol: the Chicago community adult health study. Soc Sci Med. 2012;75(6):1038–47.
Do DP, Diez Roux AV, Hajat A, Auchincloss AH, Merkin SS, Ranjit N, Shea S, Seeman T. Circadian rhythm of cortisol and neighborhood characteristics in a population-based sample: the multi-ethnic study of atherosclerosis. Health Place. 2011;17(2):625–32.
Ball K, Abbott G, Cleland V, Timperio A, Thornton L, Mishra G, Jeffery RW, Brug J, King A, Crawford D. Resilience to obesity among socioeconomically disadvantaged women: the READI study. Int J Obes. 2012;36(6):855–65.
Helmerhorst HJ, Brage S, Warren J, Besson H, Ekelund U. A systematic review of reliability and objective criterion-related validity of physical activity questionnaires. Int J Behav Nutr Phys Act. 2012;9:103.
Villanueva EV. The validity of self-reported weight in US adults: a population based cross-sectional study. BMC Public Health. 2001;1:11.
Roman CG, Chalfin A. Fear of walking outdoors. A multilevel ecologic analysis of crime and disorder. Am J Prev Med. 2008;34(4):306–12.
Morenoff JD. Neighborhood mechanisms and the spatial dynamics of birth weight. Am J Sociol. 2003;108(5):976–1017.
van Hees VT, Gorzelniak L, Dean Leon EC, Eder M, Pias M, Taherian S, Ekelund U, Renstrom F, Franks PW, Horsch A, et al. Separating movement and gravity components in an acceleration signal and implications for the assessment of human daily physical activity. PLoS One. 2013;8(4):e61691.
Arnaud B, Malet L, Teissedre F, Izaute M, Moustafa F, Geneste J, Schmidt J, Llorca PM, Brousse G. Validity study of Kessler's psychological distress scales conducted among patients admitted to French emergency Department for Alcohol Consumption-Related Disorders. Alcohol Clin Exp Res. 2010;34(7):1235–45.
Berger M, Leicht A, Slatcher A, Kraeuter AK, Ketheesan S, Larkins S, Sarnyai Z: Cortisol awakening response and acute stress reactivity in first nations people. Sci Rep-Uk. 2017. 7 Digital ObjectIdentifier. doi:10.1038/srep41760.
Kessler RC, Barker PR, Colpe LJ, Epstein JF, Gfroerer JC, Hiripi E, Howes MJ, Normand SL, Manderscheid RW, Walters EE, et al. Screening for serious mental illness in the general population. Arch Gen Psychiatry. 2003;60(2):184–9.
Choi L, Ward SC, Schnelle JF, Buchowski MS. Assessment of wear/nonwear time classification algorithms for triaxial accelerometer. Med Sci Sports Exerc. 2012;44(10):2009–16.
Kamada M, Shiroma EJ, Harris TB, Lee IM. Comparison of physical activity assessed using hip- and wrist-worn accelerometers. Gait Posture. 2016;44:23–8.
Ross CE, Jang SJ. Neighborhood disorder, fear, and mistrust: the buffering role of social ties with neighbors. Am J Community Psychol. 2000;28(4):401–20.
Vardavas E, Marcum SC. Modeling influenza vaccination behavior via inductive REasoning games. In: d'Onofrio A, editor. Modeling the interplay between human behavior and spread of infectious disease. Manfredi P: Springer; 2012.
Muthén LK, Muthén BO. Mplus User's Guide. Los Angeles, CA: Muthén & Muthén; 1998-2010.
Stults-Kolehmainen MA, Sinha R. The effects of stress on physical activity and exercise. Sports Med. 2014;44(1):81–121.
Perales F, Pozo-Cruz JD, Pozo-Cruz BD. Impact of physical activity on psychological distress: a prospective analysis of an Australian national sample. Am J Public Health. 2014;104(12):e91–7.
Valeri L, Vanderweele TJ. Mediation analysis allowing for exposure-mediator interactions and causal interpretation: theoretical assumptions and implementation with SAS and SPSS macros. Psychol Methods. 2013;18(2):137–50.
Bollen KA. Front Matter, in Structural Equations with Latent Variables. Hoboken: Wiley; doi:10.1002/9781118619179.fmatter.
Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new laternatives. Struct Equ Model. 1999;6(1):1–55.
Tucker LR, Lewis C. Reliability coefficient for maximum likelihood factor-analysis. Psychometrika. 1973;38(1):1–10.
Koster A, Shiroma EJ, Caserotti P, Matthews CE, Chen KY, Glynn NW, Harris TB. Comparison of sedentary estimates between activPAL and hip- and wrist-worn ActiGraph. Med Sci Sports Exerc. 2016;
Ross CE. Fear of victimization and health. J Quant Crim. 1993;9:159–75.
Kawachi I, Kennedy BP, Wilkinson RG. Crime: social disorganization and relative deprivation. Soc Sci Med. 1999;48(6):719–31.
Sampson RJ, Raudenbush SW, Earls F. Neighborhoods and violent crime: a multilevel study of collective efficacy. Science. 1997;277(5328):918–24.
Weden MM, Carpiano RM, Robert SA. Subjective and objective neighborhood characteristics and adult health. Soc Sci Med. 2008;66(6):1256–70.
Mackenbach JD, Lakerveld J, Van Lenthe FJ, Teixeira PJ, Compernolle S, De Bourdeaudhuij I, Charreire H, Oppert JM, Bardos H, Glonti K, et al. Interactions of individual perceived barriers and neighbourhood destinations with obesity-related behaviours in Europe. Obes Rev. 2016;17(Suppl 1):68–80.
Troxel WM, Shih RA, Ewing B, Tucker JS, Nugroho A, D'Amico EJ. Examination of neighborhood disadvantage and sleep in a multi-ethnic cohort of adolescents. Health Place. 2017;45:39–45.
Foster C, Hillsdon M, Thorogood M. Environmental perceptions and walking in English adults. J Epidemiol Community Health. 2004;58(11):924–8.
Jack E, McCormack GR. The associations between objectively-determined and self-reported urban form characteristics and neighborhood-based walking in adults. Int J Behav Nutr Phys Act. 2014;11:71.
Hinkle JC. Emotional fear of crime vs. perceived safety and risk: implications for measuring "fear" and testing the broken windows thesis. Am J Crim Justice. 2015;40(1):147–68.
Stafford M, Chandola T, Marmot M. Association between fear of crime and mental health and physical functioning. Am J Public Health. 2007;97(11):2076–81.
Chandola T. The fear of crime and area differences in health. Health Place. 2001;7(2):105–16.
Craig CL, Brownson RC, Cragg SE, Dunn AL. Exploring the effect of the environment on physical activity - a study examining walking to work. Am J Prev Med. 2002;23(2):36–43.
Wilson DK, Kirtland KA, Ainsworth BE, Addy CL: Socioeconomic status and perceptions of access and safety for physical activity. Ann Behav Med 2004, 28(1):20-28.
Jackson J. A psychological perspective on vulnerability in the fear of crime. Psychol Crime Law. 2009;15(4):365–90.
Tamayo A, Karter AJ, Mujahid MS, Warton EM, Moffet HH, Adler N, Schillinger D, Hendrickson O'Connell B, Laraia B. Associations of perceived neighborhood safety and crime with cardiometabolic risk factors among a population with type 2 diabetes. Health Place. 2016;39:116–21.
Christian H, Giles-Corti B, Knuiman M, Timperio A, Foster S. The influence of the built environment, social environment and health behaviors on body mass index. Results from RESIDE. Prev Med. 2011;53(1–2):57–60.
Lange D, Wahrendorf M, Siegrist J, Plachta-Danielzik S, Landsberg B, Muller MJ. Associations between neighbourhood characteristics, body mass index and health-related behaviours of adolescents in the Kiel obesity prevention study: a multilevel analysis. Eur J Clin Nutr. 2011;65(6):711–9.
Lovasi GS, Bader MD, Quinn J, Neckerman K, Weiss C, Rundle A. Body mass index, safety hazards, and neighborhood attractiveness. Am J Prev Med. 2012;43(4):378–84.
Poortinga W. Perceptions of the environment, physical activity, and obesity. Soc Sci Med. 2006;63(11):2835–46.
Doyle S, Kelly-Schwartz A, Schlossberg M, Stockard J. Active community environments and health: the relationship of Walkable and safe communities to individual health. J Am Plan Assoc. 2006;72(1):19–31.
Daniel M, Moore DS, Decker S, Belton L, DeVellis B, Doolen A, Campbell MK. Associations among education, cortisol rhythm, and BMI in blue-collar women. Obesity. 2006;14(2):327–35.
Astell-Burt T, Feng X, Kolt GS, Jalaludin B. Does rising crime lead to increasing distress? Longitudinal analysis of a natural experiment with dynamic objective neighbourhood measures. Soc Sci Med. 2015;138:68–73.
Diez Roux AV, Mair C. Neighborhoods and health. Ann N Y Acad Sci. 2010;1186:125–45.
Cervero R. Transit-oriented development's ridership bonus: a product of self-selection and public policies. Environ Plan A. 2007;39(9):2068–85.
Tucker JM, Welk GJ, Beyler NK. Physical activity in U.S.: adults compliance with the physical activity guidelines for Americans. Am J Prev Med. 2011;40(4):454–61.
Parks SE, Housemann RA, Brownson RC. Differential correlates of physical activity in urban and rural adults of various socioeconomic backgrounds in the United States. J Epidemiol Community Health. 2003;57(1):29–35.
Beckles GL, Zhu J, Moonesinghe R. Centers for disease C, prevention: diabetes - United States, 2004 and 2008. MMWR Suppl. 2011;60(1):90–3.
May AL, Freedman D, Sherry B, Blanck HM. Obesity - United States, 1999-2010. Mmwr-Morbid Mortal W. 2013;62(3):120–8.
Keenan NL, Rosendorf KA. Centers for disease C, prevention: prevalence of hypertension and controlled hypertension - United States, 2005-2008. MMWR Suppl. 2011;60(1):94–7.
Acknowledgments
The authors express sincere appreciation and gratitude to La’Vette Wagner, field coordinator of the Pittsburgh Hill/Homewood Research on Eating, Shopping, and Health study and the data collection staff. The authors thank the Hill House Association, Operation Better Block, and Homewood Children’s Village. Without their participation, the study could not have happened.
Funding
Funding was provided by the National Cancer Institute (Grant No. R01CA164137 “Impact of Greenspace Improvement on Physical Activity in a Low Income Community” and National Heart Lung Blood Institute (Grant No. R01 HL122460 “Neighborhood Change: Impact on Sleep and Obesity-Related Health Disparities”).
Availability of data and materials
Data for research purposes are will be available upon request after the study is complete.
Author information
Authors and Affiliations
Contributions
ASR conceptualized, performed statistical analyses, and drafted the manuscript. TD and WT acquired the data. RB and GPH created variables and data sets. NC, MGD, RLC, WT and TD made substantial contributions to conception and design of the study. All authors involved in drafting the manuscript, revising critically for important content, agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved, and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All study protocols were approved by the institution’s Institutional Review Board.
Consent for publication
Not applicable
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Richardson, A.S., Troxel, W.M., Ghosh-Dastidar, M. et al. Pathways through which higher neighborhood crime is longitudinally associated with greater body mass index. Int J Behav Nutr Phys Act 14, 155 (2017). https://doi.org/10.1186/s12966-017-0611-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12966-017-0611-y