Abstract
Background
Premature mortality is a meaningful indicator of both population health and health system performance, which varies by geography in Ontario. We used the Local Health Integration Network (LHIN) sub-regions to conduct a spatial analysis of premature mortality, adjusting for key population-level demographic and behavioural characteristics.
Methods
We used linked vital statistics data to identify 163,920 adult premature deaths (deaths between ages 18 and 74) registered in Ontario between 2011 and 2015. We compared premature mortality rates, population demographics, and prevalence of health-relevant behaviours across 76 LHIN sub-regions. We used Bayesian hierarchical spatial models to quantify the contribution of these population characteristics to geographic disparities in premature mortality.
Results
LHIN sub-region premature mortality rates ranged from 1.7 to 6.6 deaths per 1000 per year in males and 1.2 to 4.8 deaths per 1000 per year in females. Regions with higher premature mortality had fewer immigrants and higher prevalence of material deprivation, excess body weight, inadequate fruit and vegetable consumption, sedentary behaviour, and ever-smoked status. Adjusting for all variables eliminated close to 90% of geographic variation in premature mortality, but did not fully explain the spatial pattern of premature mortality in Ontario.
Conclusions
We conducted the first spatial analysis of mortality in Ontario, revealing large geographic variations. We demonstrate that well-known risk factors explain most of the observed variation in premature mortality. The result emphasizes the importance of population health efforts to reduce the burden of well-known risk factors to reduce variation in premature mortality.
Similar content being viewed by others
Introduction
Dying prematurely—before an expected or average age of death—is a signal of unfulfilled life expectancy. Many premature deaths are considered to be avoidable through appropriate prevention or early and effective treatment [1, 2]. Analyses of premature mortality, a robust indicator of population health and health system performance, can be meaningful to health system planning and evaluation [3,4,5]. Geographic variation in premature mortality can indicate missed opportunities within the health system. Monitoring areas with high premature mortality, and elucidating the determinants of geographic inequalities, can support efforts to ensure effective and equitable delivery of public health and health care services.
Analysis of premature mortality in Ontario’s 14 large health service regions, known as Local Health Integration Networks (LHINs), revealed large geographic disparities in premature mortality [6]. Furthermore, gaps between regions were shown to have increased between 1992 and 2015 [6]. These large variations signal where the health system may be falling short or where upstream determinants can be better addressed. Ontario’s Patients First: Action Plan for Health Care acknowledged that access to health care varies across the province, and committed the provincial government to improving health system access and delivery [7]. To support this goal, 76 LHIN sub-regions were formalized in 2017 to serve as the focal point for local population-based planning, performance improvement and service integration [8]. These sub-regions were developed in consultation with community, physician, and government stakeholders, and emphasize the importance of targeting population health efforts at a smaller scale to better meet the needs of diverse populations [8].
Analysis of population health outcomes across the new LHIN sub-regions has not yet been done. Furthermore, no spatial analysis of Ontario mortality has been carried out at any small-area level. This gap reflects the complexity of working with small-area rates, which are often unstable and spatially autocorrelated, in part due to small population counts [9]. Rigorous small-area analysis thus requires application of dedicated spatial analytic techniques. The added benefit of these techniques is that they allow multilevel analysis of individual-, population-, and system-level effects to fully characterize the drivers of population health inequalities [10, 11].
We used population-based mortality data to identify small-area disparities in Ontario premature mortality, using the newly formed LHIN sub-regions as the geographic unit of analysis. Further, we integrated linked demographic and behavioural data to quantify the impact of underlying population-level characteristics on premature mortality and to investigate how fully these population-level differences can explain patterns of premature mortality.
Methods
Data sources
We identified premature deaths from the Ontario Registrar General’s death file (ORG-D), a comprehensive database of population mortality data linked at ICES [12]. ORG-D captures all deaths registered in Ontario and is linked via the Registered Persons’ Database (RPDB), which includes records for all Ontario residents that have received a health card for the province’s single-payer health coverage [12]. The linkage between ORG-D and RPDB has been described in detail elsewhere [13]. Between 2011 and 2015, the linkage rate for ORG-D records was greater than 99%. We assigned each death to one of the 76 sub-regions using postal code information from RPDB.
Linked data from the census-derived Ontario Marginalization Index (ON-Marg) were used to measure material deprivation, a proxy of socioeconomic status [14]. ON-Marg assigned individuals to provincial quintiles of material deprivation, based on area-level indicators of socioeconomic status measured by the Canadian Census and Statistics Canada income tax returns [15].
Immigration, Refugees and Citizenship Canada’s (IRCC) permanent resident database was used to identify immigrants in each sub-region [13]. IRCC captures landed immigrants who arrived in Ontario between 1985 and 2012.
We obtained behavioural risk factor data from the Cancer Risk Factors Atlas of Ontario [16]. That publication used seven pooled cycles (2000–2014) of the Canadian Community Health Survey (CCHS) to produce small-area prevalence estimates for modifiable risk factors relevant to chronic disease prevention. Detailed survey methodology for the CCHS is available elsewhere [17].
Primary outcome
We defined our primary outcome, adult premature death, to include all deaths registered in ORG-D between 2011 and 2015 for decedents between the ages of 18 and 74. In doing so, we intended to capture adult deaths from all causes that occurred before full life expectancy was achieved. Specifically, this age range is based on the cut-off used by the Canadian Institute for Health Information [18] and is consistent with definitions of premature mortality in other industrialized nations [19,20,21]. Between 2011 and 2015, we identified 163,920 linked records of adult premature death.
Other variables
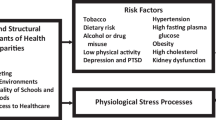
Population-level characteristics were measured to assess the influence of key sociodemographic and behavioural risk factors on premature mortality outcomes across Ontario. These characteristics were grouped into two categories: demographic variables, which included material deprivation and immigrant population size, and health-relevant behavioural factors, which included current alcohol consumption, excess body weight, inadequate fruit and vegetable consumption, sedentary behaviour, and ever-smoked status. All covariates were measured as sex-specific prevalence estimates at the sub-region level. For all statistical models, prevalence estimates were normalized to z-scores based on the distribution across all 76 LHIN sub-regions.
Material deprivation was operationalized as the proportion of each LHIN sub-region’s population in the highest provincial quintile of material deprivation. Material deprivation, which describes the likelihood that an individual cannot afford or attain necessary goods and services, is a measure of low socioeconomic status [22]. Immigrant population size was defined as the percent of residents for each LHIN sub-region that were registered as immigrants with the Canadian government.
All behavioural risk factors were measured in the 12-and-older population, according to pre-existing CCHS variable definitions [16, 17]. Current alcohol consumption was defined as the percent of LHIN sub-region residents who reported drinking alcohol in the 12 months prior to survey date. Excess body weight was defined as the percent of residents categorized as overweight (25 ≤ BMI < 30) or obese (BMI ≥ 30) based on calculations from self-reported height and weight measurements. Inadequate fruit and vegetable consumption was measured as the percent of residents who reported daily consumption of fruits and vegetables fewer than five times. Sedentary behaviour was defined as the percent of sub-region residents who spent more than 15 hours per week watching television or videos, or on the computer. Finally, ever-smoked status was defined as the proportion of sub-region residents who reported being a current or former smoker (either daily or occasional).
Statistical analysis
We calculated 5-year (2011–2015) annualized adult premature mortality rates for all 76 sub-regions. We report sex-specific rates, which have not been age-standardized, as deaths per 1000 per year. We also calculated “excess” deaths in each sub-region as the total number of premature deaths that would have been avoided if that sub-region experienced the premature mortality rate of North West Mississauga (which had the lowest 2011–2015 rate for males and females). Excess death counts reflect the absolute burden of premature mortality and have been included to contextualize the mortality rates observed in each LHIN sub-region.
We used a Bayesian hierarchical approach to model the effect of sub-region on premature mortality, adjusting sequentially for demographic and behavioural covariates. Bayesian hierarchical models are commonly used in small-area disease mapping, because they stabilize small-area rate estimates while accounting for patterns of spatial autocorrelation that violate the assumptions of other approaches [10, 11]. Specifically, the Besag-York-Mollié model [23] our analysis is based on has been found to be a highly robust approach to small-area disease mapping [24].
We fit two-level Bayesian hierarchical Poisson models. In the first level, the observed number of premature deaths in a given sub-region is decomposed to the age-standardized expected number of deaths in that region multiplied by a sub-region-specific standardized mortality ratio (SMR). We calculated the expected deaths for each sub-region using sex- and age-specific premature mortality rates for all Ontario. Age-standardizing the expected death counts accounts for differences in age structure across LHIN sub-region populations which may influence model estimates.
The second level contains the covariates which determine a region’s mortality ratio, and includes both fixed and random effects. We used fixed effects to represent the effect of population-level demographic and behavioural covariates, and random effects to represent the direct system-level sub-region effect. The random effects contain both spatially structured and unstructured components, which vary independently. The full model specification and implementation is described in Additional file 1.
We specified three age-standardized, sex-stratified models. The first, unadjusted model, contained only random effects. The second, demographics-only model, adjusted for population material deprivation and immigrant proportion as of 2012. The third, demographics plus behaviours model, introduced five population-level behaviours: alcohol consumption, excess body weight, inadequate fruit and vegetable consumption, sedentary behaviour, and ever-smoked status. We fit models using Markov chain Monte Carlo (MCMC) sampling methods with non-informative priors.
From each model, we extracted relative risk estimates and 95% credible intervals for all fixed-effect covariates, and adjusted SMR estimates for each individual sub-region. To compare models, we calculated the global variance in SMR estimates. This global variance statistic quantifies sub-region variation in premature mortality, after adjusting for model covariates. It can be used to calculate how much geographic disparity is explained by population differences.
We also calculated the spatial component of variance, which ranges from 0 to 1 and is defined as the proportion of random effect variance attributable to the spatial random effect [25]. A spatial component of variance approaching 1 suggests unexplained spatial variance.
To ensure the appropriateness of our spatial models, we repeated our analysis using generalized linear mixed models with no structured spatial component. These model results were compared to output from the Bayesian models. The residual terms from these models were tested for spatial autocorrelation using a Moran’s I statistic.
Software
Descriptive statistics were prepared using SAS software version 9.4 [26]. Models were fit in R version 3.3.4 [27], using the package R2WinBUGS [28] to call Bayesian statistical program WinBUGS version 1.4.3 [29].
Results
Premature mortality rates
Adult premature mortality rates by LHIN sub-region are mapped in Fig. 1. Among males, the province-wide mortality rate was 3.78 deaths per 1000 per year, compared to 2.50 deaths per 1000 per year among females. A total of 163,920 premature deaths were recorded between 2011 and 2015. Excess deaths by LHIN sub-region are mapped in Additional file 1: Figure S1.
Large geographic disparities were seen in both males and females. Mortality rates ranged from 1.71 (North West Mississauga) to 6.57 (Rural Hastings) premature deaths per 1000 per year in males, and from 1.22 (North West Mississauga) to 4.83 (Northern) premature deaths per 1000 per year in females. In each sub-region, premature mortality rates were higher in males than in females.
In males and females, low premature mortality rates were concentrated in south-central Ontario with a secondary cluster in southeast Ontario near the eastern (Québec) border. These clusters represent the metropolitan areas surrounding Toronto and Ottawa, both of which are large, urban centres. Premature mortality rates were comparatively higher throughout the rest of the province, particularly in the north.
Population-level risk factors
Table 1 shows the distribution of measured population risk factors. Regions have been grouped into three categories by premature mortality rate. The categories were assigned according to the 95% credible interval estimated for each region’s SMR by the unadjusted model. We classified regions with 95% credible intervals entirely above 1 (the mortality ratio for Ontario) as “Higher than Ontario”, those with intervals entirely below 1 as “Lower than Ontario”, and those with intervals spanning 1 as “Neither Higher nor Lower.”
Thirty-nine sub-regions were classified as “Higher than Ontario” according to this approach, with 25 “Lower than Ontario” and 12 “Neither Higher nor Lower”. In general, sub-regions with higher premature mortality had fewer immigrants and higher prevalence of excess body weight, inadequate fruit and vegetable consumption, sedentary behaviour, and ever-smoked status.
Model output
The results from the Bayesian hierarchical Poisson models are presented in Table 2. In the final (demographics plus behaviours) model, four of seven modelled risk factors had a statistically significant effect on premature mortality (p ≤ 0.05) for males and females: material deprivation, immigrant population, alcohol consumption, and ever-smoked status. Increased prevalence of high material deprivation and ever-smoked status was associated with increased premature mortality risk, while large immigrant populations and higher prevalent alcohol consumption were associated with decreased mortality risk. The direction and approximate size of all effects were consistent between sexes.
Compared to the unadjusted model, adjusting for socioeconomic status and immigrant population size reduced sub-region variation in premature mortality by approximately 80%. Adjusting further for five health-relevant behaviours (current alcohol consumption, excess body weight, inadequate fruit and vegetable consumption, sedentary behaviour, and ever-smoked status) reduced the variation by an additional 10%. The final model covariates explained close to 90% of sub-regional variation in premature mortality in males and females.
For the final (demographics plus behaviours) model, the spatial component of variance was 0.608 for males and 0.570 for females. Since values closer to 1 indicate strong spatial structuring, this finding indicates that our models have residual spatial variance and suggests unresolved system-level disparities.
The results of our analysis using generalized linear mixed models are available in Additional file 1: Table S1. Estimates and confidence intervals were not meaningfully different from the Bayesian models’ output. However, the generalized linear mixed model approach assumes that spatial variation in premature mortality is randomly distributed, which as we have seen is untrue. Moran’s I tests for these models showed significant residual spatial autocorrelation for the random effect-only model (Moran’s I = 0.14, p = 0.001), but not for the demographics only (Moran’s I = 0.02, p = 0.25) or demographics and behaviours model (Moran’s I = − 0.03, p = 0.72).
Discussion
Summary of main results
We conducted the first spatial analysis of premature mortality using Ontario’s newly formalized LHIN sub-regions. We used Bayesian spatial analytic techniques to model the effect of LHIN sub-region on adult premature mortality in Ontario, adjusting for population-level demographic and behavioural characteristics. Our study showed large disparities in premature mortality at the LHIN sub-region level. Adjusting for socioeconomic status and immigrant population explained most of the geographic variation in premature mortality. Adjusting for five key behaviours further reduced sub-region variation; however, some variation remains unchanged. Additionally, we found empirical evidence that the spatial pattern of premature mortality outcomes in Ontario is not fully accounted for by population demographics or health behaviours.
Explanation of findings
Our study revealed a clear geographic pattern of premature mortality, with low rates clustering around large urban centres in Ottawa and Toronto. This is consistent with evidence showing elevated mortality risk in rural environments [30,31,32]. However, it is worth noting that low-mortality clusters were not seen around any of Ontario’s smaller urban centres, such as Kingston or Sudbury. Our findings also show that population-level differences in demographic makeup have the largest sub-regional impact on premature mortality outcomes. The highest premature mortality risk was seen in sub-regions with fewer immigrants and higher material deprivation. This confirms a substantial immigrant health advantage, previously noted in Ontario for mortality [33] and cardiovascular disease [34]. It also confirms the importance of region-level socioeconomic status to population health, which has been seen consistently elsewhere [35, 36].
Together, demographic and behavioural population characteristics explained a large proportion of LHIN sub-region variations in premature mortality. However, residual spatial variation suggests that there is a systematic component underlying sub-region differences in premature mortality not explained by the population-level traits we have considered. This may be the result of system-level factors, such as access to care and risk factor control, which have been shown to modify mortality risk [37]. The implication is that population characteristics are not solely responsible for the large geographic disparities demonstrated in Ontario premature mortality. Geographic disparities may be exacerbated by system-level inequities that impact residents’ access to services and care.
Limitations
We used population-level prevalence estimates for all measured covariates, rather than individual-level risk factor data. As such, the patterns of premature mortality identified by our analysis may be sensitive to our use of LHIN sub-regions, and the same patterns may not be seen if the analysis was repeated with a different unit of aggregation. This is an instance of the modifiable areal unit problem [38] and may limit the generalizability of our findings. Also, the CCHS prevalence estimates are designed to be representative of the non-institutionalized Canadian population aged 12 and older, which differs from our study’s target population of all Ontario adults [39]. We also were unable to examine premature deaths in childhood, due to data limitations on exposure information relevant for paediatric populations. This is an important area of future study. Finally, it is difficult to quantify the variability underlying our behavioural risk factor estimates, which may have impacted the precision of our parameter estimates in a way that is difficult to quantify. However, the approach used to generate prevalence estimates was independently validated [40].
Conclusion
Comprehensive population-level vital statistics data reveal large geographic disparities in premature mortality in Ontario’s LHIN sub-regions. A majority of sub-regional variation can be explained by differences in population characteristics and behaviours, most notably material deprivation and immigrant status. However, residual variation shows a strong spatial component, which suggests that unexplained differences in premature mortality are systematic in nature. Future work should focus on quantifying the impact of system-level impacts (for example, access to care or behavioural interventions) on premature mortality outcomes. Additionally, greater effort is needed to understand which interventions may mitigate the negative mortality effects of low socioeconomic status and key behavioural risk factors.
Availability of data and materials
The dataset used in this study is held securely in coded format at ICES. Although data sharing agreements prohibit ICES from making the dataset publicly available, access may be granted to those who meet the conditions for confidential access, available at www.ices.on.ca/DAS.
Abbreviations
- CCHS:
-
Canadian Community Health Survey
- IRCC:
-
Immigration, Refugees and Citizenship Canada
- LHIN:
-
Local Health Integration Network
- ON-Marg:
-
Ontario Marginalization Index
- ORG-D:
-
Ontario Registrar General’s death file
- RPDB:
-
Registered Persons’ Database
References
Norheim OF, Jha P, Admasu K, Godal T, Hum RJ, Kruk ME, et al. Avoiding 40% of the premature deaths in each country, 2010-2013: review of national mortality trends to help quantify the UN Sustainable Development Goal for health. The Lancet. 385(9964):239–52.
Shiels MS, Chernyavskiy P, Anderson WF, Best AF, Haozous EA, Hartge P, et al. Trends in premature mortality in the USA by sex, race, and ethnicity from 1999 to 2014: an analysis of death certificate data. Lancet (London, England). 2017;389(10073):1043–54.
Turnock BJ. Understanding and measuring health. In: Public Health: what it is and how it works. 5th ed. Burlington: Jones & Bartlett Learning; 2012.
World Health Organization. World health statistics 2009. Geneva: WHO; 2009.
Canadian Institute for Health Information. National consensus conference on population health indicators: final report. Ottawa: CIHI; 1999.
Buajitti E, Watson T, Kornas K, Bornbaum C, Henry D, Rosella L. Ontario atlas of adult mortality, 1992-2015: trends in Local Health Integration Networks. Toronto: Population Health Analytics Lab; 2018.
Ministry of Health and Long-Term Care. Patients first: action plan for health care. Toronto: Queen’s Printer for Ontario; 2015.
Update: Health System Integration [press release]. Toronto, ON: Queen’s Printer for Ontario, February 3, 2017.
Mollie A, Richardson S. Empirical Bayes estimates of cancer mortality rates using spatial models. Statistics in medicine. 1991;10(1):95–112.
Carlin BP, Banerjee S. Hierarchical multivariate CAR models for spatio-temporally correlated survival data. In: Bernardo J, Bayarri MJ, Berger JO, Dawid AP, Heckerman D, Smith AFM, et al., editors. Bayesian statistics, vol. 7. Oxford: Oxford University Press; 2003. p. 45–63.
Chen JT. Multilevel and hierarchical models for disease mapping. In: Boscoe FP, editor. Geographic health data: fundamental techniques for analysis. Wallingford, Oxfordshire: CAB International; 2013.
Ontario Ministry of Health and Long-Term Care. Health analyst’s toolkit. Toronto: Ontario Ministry of Health and Long-Term Care; 2012.
Chiu M, Lebenbaum M, Lam K, Chong N, Azimaee M, Iron K, et al. Describing the linkages of the immigration, refugees and citizenship Canada permanent resident data and vital statistics death registry to Ontario’s administrative health database. BMC Med Inform and Decis Mak. 2016;16(1):135.
Matheson FI, Dunn JR, Smith KLW, Moineddin R, Glazier RH. Ontario Marginalization Index (ON-MARG) User Guide Version 1.0. Toronto: Centre for Research on Inner City Health; 2012.
Matheson FI. Ontario Agency for Health Protection and Promotion (Public Health Ontario). 2011 Ontario marginalization index: technical document. Toronto: St. Michael’s Hospital; 2017.
Cancer Care Ontario. Cancer Risk Factors Atlas of Ontario. Toronto: Cancer Care Ontario; 2017.
Béland Y. Canadian community health survey–methodological overview. Health reports. 2002;13(3):9.
Canadian Institute for Health Information. Health Indicators 2012. Ottawa; 2012.
Page A, Tobias M, Glover J, Wright C, Hetzel D, Fisher E. Australian and New Zealand Atlas of Avoidable Mortality Adelaide: PHIDU, University of Adelaide; 2006.
Scottish Government. Long-term monitoring of health inequalities: March 2017 report. Edinburgh: Scottish Government; 2017.
Tobias M, Jackson G. Avoidable mortality in New Zealand, 1981–97. Australian and New Zealand Journal of Public Health. 2001;25(1):12–20.
OECD. Society at a glance 2006: OECD social indicators. Paris: OECD Publishing; 2007.
Besag J, York J, Mollié A. Bayesian image restoration, with two applications in spatial statistics. Annals of the Institute of Statistical Mathematics. 1991;43(1):1–20.
Lawson AB, Biggeri AB, Boehning D, Lesaffre E, Viel JF, Clark A, et al. Disease mapping models: an empirical evaluation. Disease Mapping Collaborative Group. Statistics in medicine. 2000;19(17-18):2217–41.
Wakefield J. Disease mapping and spatial regression with count data. Biostatistics. 2007;8(2):158–83.
SAS Institute Inc. SAS® 9.4. Cary: SAS Institute Inc; 2012.
R Core Team. R: A language and environment for statistical computing. Vienna: R Foundation for Statistical Computing; 2017.
Sturtz S, Ligges U, Gelman A. R2WinBUGS: a package for running WinBUGS from R. Journal of Statistical software. 12:3):1–16.
Lunn DJ, Thomas A, Best N, Spiegelhalter D. WinBUGS - a Bayesian modelling framework: concepts, structure, and extensibility. Statistics and Computing. 2000;10(4):325–37.
Eberhardt MS, Pamuk ER. The importance of place of residence: examining health in rural and nonrural areas. American Journal of Public Health. 2004;94(10):1682–6.
Smith KB, Humphreys JS, Wilson MGA. Addressing the health disadvantage of rural populations: how does epidemiological evidence inform rural health policies and research? Australian Journal of Rural Health. 2008;16(2):56–66.
Canadian Institute for Health Information. How healthy are rural Canadians? An assessment of their health status and health determinants. Ottawa: CIHI; 2006.
Khan AM, Urquia M, Kornas K, Henry D, Cheng SY, Bornbaum C, et al. Socioeconomic gradients in all-cause, premature and avoidable mortality among immigrants and long-term residents using linked death records in Ontario, Canada. Journal of Epidemiology and Community Health. 2017;71(7):625–32.
Tu JV, Chu A, Maclagan L, Austin PC, Johnston S, Ko DT, et al. Regional variations in ambulatory care and incidence of cardiovascular events. Canadian Medical Association Journal. 2017;189(13):E494–501.
Bosma H, Dike van de Mheen H, Borsboom GJJM, Mackenbach JP. Neighborhood socioeconomic status and all-cause mortality. American Journal of Epidemiology. 2001;153(4):363–71.
Pickett KE, Pearl M. Multilevel analyses of neighbourhood socioeconomic context and health outcomes: a critical review. Journal of Epidemiology and Community Health. 2001;55(2):111–22.
Prentice JC, Pizer SD. Delayed access to health care and mortality. Health Services Research. 2007;42(2):644–62.
Fotheringham AS, Wong DWS. The modifiable areal unit problem in multivariate statistical analysis. Environment and Planning A: Economy and Space. 1991;23(7):1025–44.
Statistics Canada. Canadian Community Health Survey 2003: user guide for the public use microdata file. Ottawa: Statistics Canada; 2005.
Seliske L, Norwood TA, McLaughlin JR, Wang S, Palleschi C, Holowaty E. Estimating micro area behavioural risk factor prevalence from large population-based surveys: a full Bayesian approach. BMC Public Health. 2016;16(1):478.
Acknowledgements
Not applicable.
Funding
This study was funded by the Canadian Institutes for Health Research Operating Grant (FRN-142498). LR is supported by a Canada Research Chair in Population Health Analytics.
This study was supported by the Institute for Clinical Evaluative Sciences (ICES), which is funded by an annual grant from the Ontario Ministry of Health and Long-Term Care (MOHLTC). The opinions, results, and conclusions reported in this paper are those of the authors and are independent from the funding sources. No endorsement by ICES or the Ontario MOHLTC is intended or should be inferred. Parts of this material are based on data and information compiled and provided by MOHLTC, the Canadian Institute for Health Information (CIHI), and the Office of the Registrar General (ORG). Parts of this material are based on data and information compiled and provided by Immigration, Refugees, and Citizenship Canada. However, the analyses, conclusions, opinions, and statements expressed herein are those of the authors, and not necessarily those of MOHLTC, CIHI, or ORG.
Author information
Authors and Affiliations
Contributions
EB and LR conceived the manuscript, and drafted and finalized all the manuscript content. EB conducted the statistical analysis. TW assisted with the data acquisition and statistical analysis. CB and KK assisted with the manuscript preparation and interpretation. DH contributed to the study conceptualization, manuscript review, and interpretation. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the University of Toronto Health Sciences Research Ethics Board (Protocol 32405).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional file
Additional file 1:
Model specification and implementation. Provides a more detailed overview of the model specification and implementation processes employed in our analyses than is described in the main manuscript. Figure S1. Excess premature deaths by sex and LHIN sub-region, Ontario, 2011–2015. Map showing the absolute number of excess deaths registered in Ontario LHIN sub-regions between 2011 and 2015 inclusive. Table S1. Results of generalized linear mixed models. Table showing the results of sensitivity analysis using generalized linear mixed models in place of Bayesian hierarchical spatial models. (PDF 1631 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Buajitti, E., Watson, T., Norwood, T. et al. Regional variation of premature mortality in Ontario, Canada: a spatial analysis. Popul Health Metrics 17, 9 (2019). https://doi.org/10.1186/s12963-019-0193-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12963-019-0193-9