Abstract
Introduction
Artificial Intelligence (AI) represents a significant advancement in technology, and it is crucial for policymakers to incorporate AI thinking into policies and to fully explore, analyze and utilize massive data and conduct AI-related policies. AI has the potential to optimize healthcare financing systems. This study provides an overview of the AI application domains in healthcare financing.
Method
We conducted a scoping review in six steps: formulating research questions, identifying relevant studies by conducting a comprehensive literature search using appropriate keywords, screening titles and abstracts for relevance, reviewing full texts of relevant articles, charting extracted data, and compiling and summarizing findings. Specifically, the research question sought to identify the applications of artificial intelligence in health financing supported by the published literature and explore potential future applications. PubMed, Scopus, and Web of Science databases were searched between 2000 and 2023.
Results
We discovered that AI has a significant impact on various aspects of health financing, such as governance, revenue raising, pooling, and strategic purchasing. We provide evidence-based recommendations for establishing and improving the health financing system based on AI.
Conclusions
To ensure that vulnerable groups face minimum challenges and benefit from improved health financing, we urge national and international institutions worldwide to use and adopt AI tools and applications.
Similar content being viewed by others
Introduction
In the era of AI, with the rapid development of information technology (IT) and various data types, areas such as machine learning (ML) and big data [1] have become essential components of decision-making. An important economic and public health concern worldwide is the financial burden of health care and diseases [2]. AI is a broad term related to advancements that make machines “intelligent” and aims to develop an intelligent and autonomous system. ML enables computers to automatically learn and improve their understanding as a subset of AI without explicit programming. The origin of AI can be traced over fifty years back, its rapidly increasing possibilities in various fields have significantly risen during the past few years [1].
As countries are challenged with rising healthcare costs, they seek to protect their citizens and vulnerable groups from unaffordable high healthcare expenditures and to ensure access to comprehensive, non-discriminatory healthcare services [3]. In recent years, policymakers, national public health managers, and academics have become increasingly concerned with financing public health. Additionally, the high data dimensionality caused by the abundance of risk factors for patient expenditure, such as demographics, diagnoses, comorbidities, etc. makes complex and unpredictable systems [4]. To handle the massive health data, new approaches apply numerous machine learning algorithms. AI applications in healthcare management can help to close the gap between available resources and public healthcare demand. As AI develops, more and more healthcare management applications are being used [5].
Another issue that requires systemic thinking is the stability of insurance funds to control out-of-pocket payments; AI can assist in resolving this issue.
[6] [7]. The majority of real-world financial systems exhibit nonlinear and uncertain behaviors that may change over time. As a result, there is a greater need to solve highly nonlinear, time-variant challenges, for which AI is gaining popularity [8]. In other words, these new applications are replacing older ones that could only estimate short-term flow by calculating all relevant variables and establishing current and potential future relationships [9].
Hence, the need to gain a detailed overview of new technologies used for health financing is clear, which is essential to support the pathways toward universal health coverage [10]. This article aims to highlight recent applications of the implementation of AI in health financing in light of recent AI advancements and identify potential future research areas.
Methods
In line with its objectives, we adopted a scoping review framework guided by Arksey and O’Malley’s methodology, including six steps: 1- identifying the research question; 2- identifying relevant studies; 3-selecting included studies; 4-data charting; 5-summarizing and reporting the results; and 6- consultation with experts [11].
Following the first step, we formulated research questions as follows: (1) Which applications of AI in health financing are reported in the literature? (2) What future health financing applications and capabilities can be employed? We then identified relevant studies according to appropriate keywords, and two independent researchers, MR and AB, conducted a comprehensive literature search through three databases: PubMed, Web of Sciences, and Scopus (Table 1). In the third step, two independent authors MR and AB, screened the relevance of titles and abstracts of articles and reviewed the full texts of the relevant articles. We charted the extracted data in the fourth step and collated, summarized, and reported in the fifth step. Finally, we reported the synthesized results to the research team and one external advisor for approval.
Inclusion criteria for study selection
Inclusion criteria were studies published in English on financing health systems (inclusively or exclusively) from 2000 to 2023. Articles without full-text were excluded.
Flow chart of the search strategy
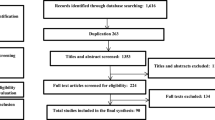
1179 references were identified during the initial search, 218 of which were duplicates, providing 961 articles from the first screen title review. We then excluded 583 articles that did not meet the inclusion criteria, 378 studies met the inclusion criteria for full-text evaluation, and 260 were excluded due to the lack of relevancy or poor methodological quality (Fig. 1). The results of the study are presented in two parts. Initially, we summarize the extracted information, propose a framework, and explain its dimensions.
Charting data
Two authors, MR and AB, synthesized the data by placing similar codes into categories of AI applications in health financing to develop a conceptual framework and began to create descriptions by synthesizing the extracted information. All authors reviewed and discussed the framework until we reached a final consensus.
Results
A Framework for future studies: existing knowledge and future directions
As shown in Fig. 2, the proposed framework has five components. The conceptual framework shows that AI can affect health financing with different applications and capabilities.
AI applications and capabilities
Applications of AI have been used or have a high potential to improve performance in a variety of areas of health financing, including governance, revenue raising, pooling, and strategic purchasing.
1-Governance
1-1 process
Studies have discussed various assorted implications and characteristics for applying AI and advanced data management tools [12] in the governance of health financing. At the macro level, AI can help investigate which social determinants of health (SDH) may cause more cost within a specific patient population [13]. One study introduced the development of an ML framework to automate classifying health projects into different global common goods for health (CGH) categories. The study illustrates the feasibility and efficiency of tracking financing for global CGH [14]. Another study used various datasets to investigate the extremes of micro and macro variables and the country flow of funds to develop a general equilibrium model encompassing regional variation in the type of financial friction and calibrating it to measure variation in regional aggregates [15].
One study provides a simplified simulation system framework for emergency material preparation and dispatch with high operating efficiency [16]. Researchers in another study developed a detailed decision support system called “Cost Calculation Tool” for the leading Austrian social occupational insurance institution (AUVA) that investigates total direct and primary indirect costs of individual injury claims from the time of the incident for all injured individuals up to their death [17]. Furthermore, analyzing the healthcare costs data subset will make cost audit and artificial sampling audit possible [18].
Public option mining is another application of AI in different areas that can potentially improve health financing [19]. Representation of financial information, for instance, transforms concurrent financial time series into images [20], forecasting the incidence of medical cases, or predicting the degree of spread of the disease, are among the initial steps in institutional planning that help plan health control strategies and develop intervention programs based on required medical resources and effective resource allocation strategies [21,22,23].
1–2 Content
In recent years, numerous scientific research studies have focused on sustainable development. The results of AI analysis in one study showed the impact of air pollution change on the acceleration of economic growth in India [24]. AI can also facilitate the efficient monitoring of resource allocation of governments, donors, and development agencies involved in achieving Sustainable Development Goals (SDGs). Future studies can explore the simultaneous social and financial impact of different interventions to improve the efficient use of resources for development and create insights about additional opportunities to substantially impact the well-being of people worldwide [25].
The modernization of the digital economy and financial and economic mechanisms is being facilitated through end-to-end technologies, which promote innovation and enhance the quality of life for the population. AI has the potential to address many of the current challenges faced by nations, such as reducing unemployment, improving public sector efficiency, enhancing environmental conditions, fostering innovation, and increasing national economic competitiveness [26]. These changes will be related to reducing the burden of comorbidities, addressing lifestyle factors such as smoking, and screening for cancers and cardiovascular diseases, that need to be targeted to lower the mortality and cost associated with diseases [27]. One of these innovative approaches adopted by the Global Fund to Fight AIDS, TB, and Malaria (GFATM) to health financing has had significant flow-on effects on the knowledge system that supports efforts to combat the three subject diseases in target countries. By considering itself as part of a more extensive knowledge system, the GFATM can use this influence to build the capacity across that system to learn from implementation and refine its processes accordingly [28].
Clinical and socioeconomic perspectives are suggested to avoid determinants of medical cost and improve healthcare resource utilization [29]. One study investigated the incidence of hemorrhoids and associated risk factors like lifestyle behavioral variables, including body mass index (BMI), alcohol intake, smoking, and exercise [30]. These revolutions help promote healthy lifestyles and disease prevention strategies to strengthen universal health care [31]. Moreover, AI can determine the optimum allocation of resources to the areas needing prioritization for attaining social inclusion goals [31]. Decision-makers can select from several rational resource allocation models depending on the data availability and complexity level. For example, S4HARA (System for HIV/AIDS resource allocation) is a four-step spreadsheet-based model for a rational resource allocation approach. Recommendations of the model are grounded in the cultural, social, and political context [32]. Furthermore, determining the overall performances of healthcare structures based on input-output relations plays a vital role in optimizing resource allocation and investment planning, as it contributes to reducing the uncertainty of future performance [33].
1–3 Context
AI can apply an event-detection approach to extract information about real-world events’ consequences [34, 35]. For instance, the influencing factors of air pollution on government health expenditure and its spatial governance can be explored using a Geographical Detector, (GeoDetector) [36].
Using big data analysis, disabilities can be detected earlier than clinical diagnoses, allowing policymakers to act appropriately to prevent disabilities [37]. Population risk assessment can estimate Socioeconomic costs and indicators [38, 39]. For instance, one study estimated socio-economic burden and co-morbidities by including expenses for outpatient care or hospitalization, medicines, prescriptions, traffic expenses, and lost income paid by the insurer and patients [40]. To forecast macroeconomic variables such as Gross domestic product (GDP) growth, AI has the potential to establish connections between individual economic activities and macro-socioeconomic indicators on various spatial scales, to help understand the current and future state of the economy [41].
2- Revenue raising
2 − 1 Content
One study used GDP and population data as independent variables to predict life expectancy [42]. To address the challenge of increasing demand with limited resources, decision-makers need to explore innovative approaches that could help sustain the quality of services provided to the citizens. One study focused on obtaining additional resources for the public health budget directly from citizens (38). With this background, researchers developed an agent-based simulation model as a decision support tool to compare different co-payment rules and evaluate their impact on the public budget and the health expenses of different groups of citizens [43].
Another study analyzed whether the deductible impacts co-pay distribution among different patient groups. The study recommends that patients with chronic and non-chronic conditions of similar age and income should pay the same amount for fairness [43]. Another study showed that in a publicly funded system of care, a community-based program could be utilized from tools such as the Child and Adolescent Needs and Strengths (CANS) to identify clients likely to benefit from established mental health services. The study proposed using ML methods to learn from data collected through the application of Transformational Collaborative Outcomes Management (TCOM) within a human services system, which can be replicated in various contexts [44].
Big data technology can bring new foundations and challenges to tax management, but the premise is that big data thinking needs to be formed [9]. To gain the optimal tax, collecting precise data, or at least capturing the appropriate magnitude of the total value of the sum of negative externalities, is crucial. Thus, governments (national, regional, local, and/or any other political initiatives) need to use big data to crack the code of what goes wrong and identify options for moving forward. [45]. Another study illustrated that determining the ideal meat tax size requires a comprehensive analysis of foresight and big data. This approach can lead to a double benefit: reducing meat production to an optimal level while generating tax revenue. Generated tax revenue should be invested in a political decision that calls for international negotiations. There are various possibilities, such as development aid, disaster funds, climate change, research, new technology, etc. [45].
In one study, researchers argued that grant funding allocation could be discussed regarding support for regional decision-makers and as a tool for national negotiation. Accordingly, three demand scenarios have been developed, showing how regional and nationally funded grants could be managed to reduce future gaps by comparing the results with current policies [46]. FinTech platform is one of these tools that can raise funds and donations, improve access to quality healthcare services, and help in financing by shifting the dynamics of payment plans and broadening financial access to healthcare services [47].
2–2 Process
Cost information can be incorporated into a data-mining algorithm for each risk factor to estimate the budgets for providing health services for a specific target population [48]. Patient expenditure information and related analysis by AI can help pharmaceutical companies to optimize the medications manufacturing process and other industries for better inventory management. Apart from the healthcare domain, the proposed method could be used to predict weather and earthquakes and for several applications [49]. Prediction of the healthcare cost [50] and other significant variables in health financing, such as healthcare expenditure per capita (pcHCE) [51] or estimation of health expenditure [3] help the health system to have more knowledge-based policies. AI can facilitate the implementation of dynamic strategies for revenue maximization through demand learning, which might result in lower out-of-pocket and impoverishment costs. The proposed method balances the trade-off between exploitation (revenue maximization) and exploration (demand model estimation) [52]. Utilizing methods such as Multi-Criteria Decision Analysis (MCDA) could facilitate the development of a decision support system in healthcare, thereby contributing to the efficient, rational, and fair allocation of resources [53].
The potential use of machine-learning approaches in analyzing complex data can help informed decision-making, alleviate catastrophic health expenditures, and provide the needed budget [5]. Basic medical insurance does not protect households from catastrophic out-of-pocket (OOP) health expenditures. To reduce inequality, it would be beneficial to utilize big data tools and techniques to effectively screen poor households and strengthen the social and medical aid system for them [54,55,56,57].
2–3 Context
AI can facilitate fraud detection in income tax data [58]. A recent ML analysis, the so-called K-Nearest Neighbour (KNN) model, can capture the self-predictive ability of the GDP and improve the performance of traditional time series analysis [59]. The AI-predicted GDP showed that factors obtained from real variables have much more impact than factors obtained from financial and price variables [60]. Related to the prediction of future econometric trends, one paper proposes an empirical mode decomposition (EMD) method designed to improve deep learning for understanding GDP trends and GDP data prediction research [61]. Another study examined the relationship between per capita GDP and total spending on health care. In particular, their analysis confirmed the growth theory through the indirect effects of healthcare expenditure on GDP [62].
Correlation between ideal retirement age and life expectancy [63], identifying the prevalence of pain and trends of pain associated with chronic diseases and personal out-of-pocket medical expenditures over time [64], and evaluating the association between low-value care with excess out-of-pocket cost are other AI-related analysis [65] that can be used by policymakers for advocacy to increase health revenues.
3- Pooling
3 − 1 Context
In pooling, computational intelligence techniques are used to model the behavior of medical reviewers - professionals who assess whether medical requests should be allowed [66]. To make a more in-depth analysis of the relationship between public services and balanced economic development, one study constructs the measurement indicators of balanced economic development, public services, and local fiscal revenue and expenditure and empirically tests the endogenous relationship and influencing factors between them [67]. These findings can be used for fund pooling in territories and areas as local communities to improve access to healthcare for all. Additionally, another study has shown that economic growth positively enhances the quality and quantity of public service supply [67]. Further, costs related to increased cancer incidence and mortality rates worsen the loss ratio of cancer insurance products and create a financial crisis for insurers. Analysis of the same annual medical cost for the elderly compared to other ages can help risk pooling by preventive strategies [68].
3 − 2 Content
AI can examine the choice environment of private online health insurance exchanges, which provide alternate venues for consumers to shop for various insurance plans. Theoretically, these estimates can help consumers identify the highest-value health plans [69]. OptiHealth is a recommender framework for selecting Pareto optimal health insurance plans. The recommender uses actuarial data to estimate the total annual cost for each plan and then recommends a small number of Pareto optimal plans [70]. Exploring the heterogeneity not just along socioeconomic variables but also according to some other characteristics of policy impacts can change the policy impact assessment from “whether the policy is effective” to “who the policy is effective for.” Therefore, the result has reference value for policymakers to formulate “optimal policy rules” and improve the qualification, re-design of the eligibility criteria, and subsidy standards of medical insurance [71, 72].
AI can also help the application of techniques for classifying the beneficiaries of an operator of health insurance, according to their financial sustainability, via their sociodemographic characteristics and healthcare cost history [66]. Identifying high-risk patients and the expense and indirect costs of implementing mitigation strategies helps better pool the health system. For example, financial toxicity mitigation tools resulted in financial navigators, charity aid, or insurance copay assistance programs. They guided shared decision-making concerning high-risk patient populations to align treatment decisions with their (spending) preferences and values [73].
Insurance companies need to convince their clients about the advantages they can receive, including direct monetary rewards through customized offers with lower premiums due to their healthy lifestyle choices; and/or indirect rewards such as coaching for well-being by using explainable AI techniques in the classifiers used by the risk assessment service. [25]. health programs could use AI to identify impactable high utilizers, possibly reduce inappropriate healthcare spending, understand better impactable healthcare conditions, and progress toward interventions to reduce inappropriate healthcare utilization [74]. AI methodologies can be applied in need-based and optimal insurance packages based on definite criteria. It will not only allow employers and insurance companies to design suitable insurance schemes for the provision of healthcare benefits but will also prevent financial losses in the long run [75]. Using clustering techniques in this field will also provide opportunities and solutions for decision-makers to monitor insurance coverage based on socioeconomic, geospatial, and demographic variables in general and health insurance in particular [76,77,78].
3–3 Process
One study sought to develop and test a tool to accurately predict an individual’s risk of financial toxicity based on clinical, demographic, and patient-reported data before initiation of treatment, which resulted in a financial burden for the health system. Such analyses can help create a learning health system [73]. Related systems can provide risk assessment based on behavior for the health insurance sector [79]. To simplify the analysis of healthcare costs for the insurer and patient, the most important variables can be extracted to predict the healthcare insurance costs [80, 81]. For instance, chronic kidney disease (CKD) represents a heavy burden on the healthcare system because of the increasing number of patients, high risk of progression to end-stage renal disease, and poor prognosis of morbidity and mortality. One study aimed to forecast its prevalence through developing a machine-learning model that uses comorbidity and medication data. The model proposed in this study could be a valuable tool for policymakers in predicting the trends of diseases in the population, close monitoring of people at risk, early detection of diseases, better allocation of resources, and patient-centric management [82]. Finally, by AI applications, health insurance premiums can be predicted based on various parameters, such as age, gender, body mass index, number of children, smoking habits, and geolocation [83].
4- Strategic purchasing
4 − 1 Context
The Internet of Everything (IoE) allows for the management and monitoring of numerous IoE nodes spread out across a smart city. This enables the support of various applications in different domains, including energy and resource management, intelligent transportation systems, and e-health [84]. New vectors can also be added to the health insurance packages to help the health and insurance sector construct mathematical risk equation models with parameters to map real-life risk conditions [85]. Resource allocation strategies can be developed for prioritizing limited healthcare capacity based on the computational characterization of spatiotemporal patterns of the disease transmission risks [86]. Developing a risk adjustment model of patient expenditures according to their vital signs, health status and lifestyle indicators, demographics, diagnoses, comorbidities, disease history, insurance, income level, and secondary diagnoses [87] have the potential to identify characteristic profiles of high utilizers of health care (85). This may help create clusters based on individuals’ demographic, economic, and health-related conditions and examine the clusters on future expenditures commonly used in healthcare utilization studies [88]. The design of injury prevention strategies [89] and allocation of resources such as GPs reflect the location-specific higher healthcare demand [90].
4 − 2 Content
To improve resource management, cost containment, and responsibility in healthcare, it is crucial to establish information systems that can aid hospital managers in financial management, resource allocation, and activity planning [91,92,93,94]. The impacts of different operating strategies can be identified by building and validating computer simulation models, which leads to higher efficiency for the hospital’s resources without decreasing the quality of patient care [95].
Training the payment prediction model for individuals’ future payment behavior [96] or predicting coming days in the hospital using features extracted from customer demographics, past hospital admission, and hospital procedure claim data [97] can bring the benefits of providing references for medical management with specific diseases that could reduce the expense through effective control. This might reduce the cost of healthcare, which may decrease health insurance burdens in the future [98]. Data mining methods can be used to determine the key financial indicators in public hospitals, which might help improve their respective financial performances [99]. This decision support system also allows the government to predict preventive actions and resource allocation in the health sector [100].
Nationally representative physician data on their payment arrangements and practice characteristics can be used to create a parsimonious typology for incentive arrangements [101]. Supervised learning approaches, such as Random Forest, could substantially improve the prediction accuracy of counter-verification in PBF (performance-based financing) and thus increase the cost-effectiveness of verification [102]. The utilization of big data can enhance the accuracy and promptness of information in infrastructural healthcare Project Finance (PF). The collaboration between public and private partners, facilitated by networking big data and interoperable databases, can increase the creation of value, leading to better value for money and lower risk. Big data can also simplify supply chain processes, widen economic opportunities, and facilitate sustainable planning for intelligent healthcare investments [103]. AI can facilitate cost-benefit analysis, which will contribute to the efficiency of human resources strategies to demonstrate the return on investment [104].
The results of AI analysis can offer valuable guidance for policymakers to address the uneven distribution of medical resources, enhance regional public health systems, and facilitate government coordination in allocating medical resources at various levels. This can ultimately improve the overall performance of the medical and health service system and promote its balanced and coordinated development [105]. However, these findings must be refined and customized to suit specific diseases. One study introduced a tool to estimate the disease burden for the population and health system. These tools can also create regional snapshots focusing on particular populations through national and regional public health policies [106]. Finally, AI can help the primary healthcare network (PHCN) to develop monitoring systems and resource allocation monitoring [107].
4 − 3 Process
Insights for insurance industries or individuals to understand the magnitude of healthcare fraud within different healthcare systems help design better strategies to combat fraud [108]. AI also helps to model the detection of abusive utilization patterns in various payment arrangements [109].
The length of hospital stay or the magnitude of medical expenses can also be used for cost-effective analysis [110]. The frequency and patterns of prescriptions used for treatment [111], safety rate of treatment interventions regardless of age [112], and risk asses of return visits [113] guide to reevaluating and providing effective interventions.
Morbidity Related Groups (MRG) is a new system, adapted from the Diagnosis-Related-Group-System (DRG), which has been developed to control expenditure through the classification and compensation of hospital cases [114]. One study aimed to identify super-utilizers and low users; an established technique was used to categorize patients into four expenditure groups [115]. In another study, researchers sought to anticipate variations in patients’ medical expenses for the following year and pinpoint significant factors contributing to this forecast. They focused on the impact of pharmacotherapy and other medical aspects, such as hospitalizations and visits to outpatient physicians [2]. Additionally, AI has the potential to enhance resource allocation decisions by providing a more efficient alternative to a hospital’s current approach that employs a DRG grouper [116].
AI capabilities for e-Health and digital health provide a powerful forum for debate on cost-effective resource allocation [117]. AI can transform the existing healthcare delivery models by inducing a redesign of public accountability systems and the traditional relationships between professionals and patients. The outcome will be a transformative change integrating digital technologies into public sector modernization. AI has a great potential to empower patients while improving their health, personalized experiences, and individual well-being [118]. The “smart” financial service model in the era of AI has also played a profound and revolutionary role in the reform of financial operation mechanisms [119]. In one study, researchers developed two financial road maps for the low performer hospitals to improve their financial performance [120].
The architecture of a system developed for the Polish National Health Fund (NHF) branch has been introduced in one study. The experience with controlling system modeling can be used to extend the developed model by new data structures, relations, inference rules, tools for result data visualization, and implementation of solutions to the contextual data analysis [121]. Another study investigated the accuracy of laboratory tests, improved patients’ safety, and reduced unnecessary costs associated with wrong orders [122]. One study associated the link between the rate of oral antibiotic prescriptions and the diagnosis of infectious diseases [123]. Predicting successful visit payments, helping to identify patients in need of financial support, allowing for the development of customized and patient-oriented payment plans, assisting the patients in benefiting from state-funded programs and navigating through the network restrictions, out-of-pocket costs, and confusion surrounding healthcare costs and billing systems [13] are among other applications of AI to improve patients’ satisfaction. By providing a clear picture of the insurance options, patients can apply for affordable health insurance or state-funded programs and overcome obstacles to enrollment [13].
Conclusions
This paper discussed a number of AI applications in health financing, including governance, revenue raising, pooling, and strategic purchasing of health financing. To address health problems related to financing, AI applications should be established and improved. In addition to providing insights into complex data sets that would be difficult or impossible for humans to analyze, artificial intelligence can transform health system financing, processes, and policy-making. Despite the challenges associated with implementing AI in healthcare systems, such as maintaining patient privacy and ethical standards, its benefits are evident. To improve outcomes in health financing, we encourage policymakers to continue exploring ways to incorporate artificial intelligence into their decision-making processes.
The potential of AI is enormous, and methods should be developed outside of the finance industry. Future research can concentrate on examining actual health finance data, including the inclusion of beneficiaries and looking into the effects of weighting various variables. It would be beneficial to investigate AI applications on other health building blocks. In order to confirm the efficacy of the various strategies proposed in this study, real-world data or simulated data can be used for testing. The impact of AI technology on financial issues, management and strategic aspects of it, and how it might be implemented in other health building blocks all require cross-disciplinary studies.
The structure for initiatives to encourage sustainable financing can be provided by AI. Providing health services and initiatives might be given priority by politicians to ensure financial sustainability while simultaneously achieving health goals. The results show that AI applications can be considered as a new paradigm in health financing, which can be added to the development literature.
The present study has several strengths that contribute to the field of AI applications. First of all, the findings of this future study will shed light on how AI might be used to improve health financing. Our research discussed a sizable number of AI applications, offering insightful information for future capacity development and sustainable policy creation. Our study’s findings can be used as a foundation for using sophisticated models, which is a novel addition to the body of literature. We are hopeful that our work will help scientists choose and use these models and tools efficiently. In particular, our study can offer a starting point for future research on AI techniques to investigate complicated relationships between numerous components or design a platform that can be used by health systems to manage health financing.
The absence of negative impacts and ethical issues pertaining to technological breakthroughs, which would have offered useful insights, is one of the study’s limitations. It would have been beneficial to investigate AI applications in every aspect of health financing from different perspectives. Finally, our study did not examine the potential of AI in other health building blocks and solely concentrated on the finance area.
Data availability
Not applicable.
Abbreviations
- AI:
-
Artificial Intelligence
- GDP:
-
Gross domestic product
- ML:
-
Machine learning
- GFATM:
-
Global Fund to Fight AIDS, TB, and Malaria
References
Kunwar, M. Artificial intelligence in finance: Understanding how automation and machine learning is transforming the financial industry. Bachelor Thesis. Centria University of Applied Sciences, Finland. 2019.
Jödicke AM, Zellweger U, Tomka IT, Neuer T, Curkovic I, Roos M, et al. Prediction of health care expenditure increase: how does pharmacotherapy contribute? BMC Health Serv Res. 2019;19(1):1–11.
Akca N, Sonmez S, Yilmaz A. Determinants of health expenditure in OECD countries: a decision tree model. Pakistan J Med Sci. 2017;33(6):1490.
Li L, Bagheri S, Goote H, Hasan A, & Hazard G. Risk adjustment of patient expenditures: A big data analytics approach. Paper presented at the Big Data, 2013 IEEE International Conference on. 2013. https://doi.org/10.1109/BigData.2013.6691790.
Lan Z, Zhou G, Zhang Y, Duan Y, Yan W, & Chi C. Healthcare expenditure prediction for crowd with co-existing medical conditions. IEEE Explore. 2019;19(1):303–307. https://doi.org/10.1109/BIGCOM.2019.00052.
Muremyi R, Haughton D, Kabano I, Niragire F. Prediction of out-of-pocket health expenditures in Rwanda using machine learning techniques. Pan Afr Med J. 2020;37(1).
Dzau VJ, Balatbat C. Strategy, coordinated implementation, and sustainable financing needed for COVID-19 innovations. The Lancet. 2020;396(10261):1469–71.
Bahrammirzaee A. A comparative survey of artificial intelligence applications in finance: artificial neural networks, expert system and hybrid intelligent systems. Neural Comput Appl. 2010;19(8):1165–95.
Wang WR. Research on China’s Tax Policy for Responding to Public Health Emergencies under the Background of Big Data. In2020 International Conference on Modern Education and Information Management (ICMEIM). IEEE. 2020. p. 232–235.
Organization WH. Digital technologies for health financing: what are the benefits and risks for UHC? Some Initial Reflections.” Health Financing Working Paper No. 19. Geneva, Switzerland: World Health Organization. Available at https://iris.who.int/handle/10665/343505.
Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32.
Gupta S and Tripathi P. “An emerging trend of big data analytics with health insurance in india”, Proc. Int. Conf. Innov. Challenges Cyber Secur. (ICICCS-INBUSH). 2016. p. 64–69.
Davis S, Nourazari S, Granovsky R, Fard N. Predicting a Need for Financial Assistance in Emergency Department Care. InHealthcare 2021;(Vol. 9, No. 5, p. 556). MDPI.
Dixit S, Mao W, McDade KK, Schäferhoff M, Ogbuoji O, Yamey G. Tracking financing for global common goods for health: a machine learning approach using natural language processing techniques. Front Public Health. 2022;10:4509.
Moll B, Townsend RM, Zhorin V. Economic development, flow of funds, and the equilibrium interaction of financial frictions. Proceedings of the National Academy of Sciences. 2017;114(24):6176-84.
Du L. Medical emergency resource allocation model in large-scale emergencies based on artificial intelligence: algorithm development. JMIR Med Inf. 2020;8(6):e19202.
Rauner MS, Schaffhauser-Linzatti MM, Bauerstaetter J. Decision support system for social occupational injury insurance institutions: cost analysis and targeted resource allocation. CEJOR. 2015;23(1):1–29.
Ji Z. Building of a standardized health insurance monitoring model based on data mining. Int J Simul Syst Sci Technol. 2016;17(18):101–4.
Sen AP, Singh Y, Meiselbach MK, Eisenberg MD, Anderson GF. Participation, pricing, and enrollment in a Health Insurance Public Option: Evidence from Washington State’s Cascade Care Program. Milbank Q. 2022;100(1):190–217.
Dhar V, Sun C, Batra P. Transforming finance into vision: concurrent financial time series as convolutional nets. Big Data. 2019;7(4):276–85.
Mary Ann F. Quioc, Shaneth C. Ambat, and Ace C. Lagman. Medical Cases Forecasting for the Development of Resource Allocation Recommender System. In Proceedings of IEEE 4th International Conference on Computer and Communication Systems (ICCCS ’19). 2019. IEE
Chen P-T. Medical big data applications: intertwined effects and effective resource allocation strategies identified through IRA-NRM analysis. Technol Forecast Soc Chang. 2018;130:150–64.
Mulay N, Bishnoi V, Charotia H, Asthana S, Dhama G, Arora A. Pandemic spread prediction and healthcare preparedness through financial and mobility data. In2020 19th IEEE International Conference on Machine Learning and Applications (ICMLA) 2020. p. 1340–1347). IEEE.
Mele M, Nieddu L, Abbafati C, Quarto A. An ANN experiment on the Indian economy: can the change in pollution generate an increase or decrease in GDP acceleration? Environ Sci Pollut Res. 2021;28(27):35777–89.
Gonzales Martínez R. Which social program supports sustainable grass-root finance? Machine-learning evidence. Int J Sustainable Dev World Ecol. 2020;27(5):389–95.
Veselovsky MY, Pogodina TV, Ilyukhina RV, Sigunova TA, Kuzovleva NF. Financial and economic mechanisms of promoting innovative activity in the context of the digital economy formation. Entrepreneurship and Sustainability Issues. 2018;5(3):672–81.
Prodel M, Finkielsztejn L, Roustand L, Nachbaur G, De Leotoing L, Genreau M et al. Costs and mortality associated with HIV: a machine learning analysis of the French national health insurance database. J Public Health Res. 2022;11(2).
Van Kerkhoff L, Szlezák N. Linking local knowledge with global action: examining the Global Fund to Fight AIDS, Tuberculosis and Malaria through a knowledge system lens. Bull World Health Organ. 2006;84(8):629–35.
Kim J, Rhee CK, Yoo KH, Kim YS, Lee SW, Park YB et al. The health care burden of high grade Chronic Obstructive Pulmonary Disease in Korea: analysis of the Korean Health Insurance Review and Assessment Service data. Int J Chronic Obstr Pulm Dis. 2013:561–8.
Hong J, Kim I, Song J, Ahn BK. Socio-demographic factors and lifestyle associated with symptomatic hemorrhoids: big data analysis using the National Health insurance service-National Health screening cohort (NHIS-HEALS) database in Korea. Asian J Surg. 2022;45(1):353–9.
Nayak B, Bhattacharyya SS, Krishnamoorthy B. Democratizing health insurance services; accelerating social inclusion through technology policy of health insurance firms. Bus Strategy Dev. 2019;2(3):242–52.
Lasry A, Carter MW, Zaric GS. S4HARA: system for HIV/AIDS resource allocation. Cost Eff Resource Allocation. 2008;6(1):1–19.
Muriana C, Piazza T, Vizzini G. An expert system for financial performance assessment of health care structures based on fuzzy sets and KPIs. Knowl Based Syst. 2016;97:1–10.
Lee J-w, Choi Y-E, Kim D-w, Lee S, Cho K-H. Trends in socioeconomic costs of morbid obesity among Korean adults, 2009–2013: Data from National Health Insurance Service. Obesity research & clinical practice. 2018;12(4):389 – 93.
Carta S, Consoli S, Piras L, Podda AS, & Recupero DR. Event detection in finance using hierarchical clustering algorithms on news and tweets. PeerJ Computer Science. 2021;7:e438. https://doi.org/10.7717/peerjcs.438.
Xia Q, Zhang X, Hu Y, Tian W, Miao W, Wu B, et al. The superposition effects of air pollution on government health expenditure in China—spatial evidence from GeoDetector. BMC Public Health. 2022;22(1):1–15.
Jeong S-H, Lee TR, Kang JB, Choi M-T. Analysis of Health Insurance Big Data for Early Detection of disabilities: Algorithm Development and Validation. JMIR Med Inf. 2020;8(11):e19679.
Burnett J, Suchting R, Green CE, Cannell MB, Dyer CB. Socioecological indicators of senior financial exploitation: an application of data science to 8,800 substantiated mistreatment cases. J Elder Abuse Negl. 2020;32(2):105–20.
Koschinsky J, Marwell NP, Mansour R. Does health service funding go where the need is? A prototype spatial access analysis for new urban contracts data. BMC Health Serv Res. 2022;22(1):1–12.
Park Y, Kim J, Lee B, Kim T, Lee E. Annual prevalence and economic burden of genital warts in Korea: Health Insurance Review and Assessment (HIRA) service data from 2007 to 2015. Epidemiol Infect. 2018;146(2):177–86.
Chu B and Qureshi S. “Comparing Out-of-Sample Performance of Machine Learning Methods to Forecast U.S. GDP Growth,” Computational Economics. 2022;1–43. https://link.springer.com/article/10.1007/s10614-022-10312-z.
Rubi MA, Bijoy HI, and Bitto AK, “Life expectancy prediction based on GDP and population size of Bangladesh using multiple linear regression and ANN model,” 2021 12th International Conference on Computing Communication and Networking Technologies (ICCCNT), 2021. p. 1–6. https://doi.org/10.1109/ICCCNT51525.2021.9579594.
Sonnessa M, Tànfani E, Testi A. An agent-based simulation model to evaluate alternative co-payment scenarios for contributing to health systems financing. J Oper Res Soc. 2017;68(5):591–604.
Troy JD, Torrie RM, & Warner DN. A machine learning approach for identifying predictors of success in a medicaid-funded, community-based behavioral health program using the child and adolescent needs and strengths (CANS). Child Youth Serv Rev. 2021;126:106010. https://doi.org/10.1016/j.childyouth.2021.106010.
Jarka C, Tinggaard SG, Tomas Z. A global meat tax: from big data to a double dividend. Agric Econ. 2018;64(6):256–64.
Lodi A, Tubertini P, Grilli R, Mazzocchetti A, Ruozi C, Senese F. Needs forecast and fund allocation of medical specialty positions in Emilia-Romagna (Italy) by system dynamics and integer programming. Health Syst. 2016;5(3):213–36.
Lucero-Prisno DE, Olayemi AH, Ekpenyong I, et al. Prospects for financial technology for health in Africa. DIGITAL HEALTH. 2022;8. https://doi.org/10.1177/20552076221119548.
Chae YM, Ho SH, Cho KW, Lee DH, Ji SH. Data mining approach to policy analysis in a health insurance domain. Int J Med Informatics. 2001;62(2–3):103–11.
Kaushik S, Choudhury A, Natarajan S, Pickett LA, Dutt V. Medicine expenditure prediction via a variance-based generative adversarial network. IEEE Access. 2020;8:110947–58.
Nomura Y, Ishii Y, Chiba Y, Suzuki S, Suzuki A, Suzuki S, et al. Does last year’s cost predict the present cost? An application of machine leaning for the Japanese area-basis public health insurance database. Int J Environ Res Public Health. 2021;18(2):565.
Ceylan Z, Atalan A. Estimation of healthcare expenditure per capita of Turkey using artificial intelligence techniques with genetic algorithm-based feature selection. J Forecast. 2021;40(2):279–90.
Elreedy D, Atiya AF, Shaheen SI. Novel pricing strategies for revenue maximization and demand learning using an exploration–exploitation framework. Soft Comput. 2021;25(17):11711–33.
Angelis A, Kanavos P, Montibeller G. Resource allocation and priority setting in health care: a multi-criteria decision analysis problem of value? Global Policy. 2017;8:76–83.
Cinaroglu S. Modelling unbalanced catastrophic health expenditure data by using machine-learning methods. Intell Syst Acc Finance Manage. 2020;27(4):168–81.
Xu Y, Zhou Y, Pramono A, Liu Y, Jia C. A 25-Year Trend of Catastrophic Health expenditure and its inequality in China: evidence from Longitudinal Data. Risk Manage Healthc Policy. 2022;15:969.
Muremyi R, Haughton D, Kabano I, Niragire F. Prediction of out-of-pocket health expenditures in Rwanda using machine learning techniques, Pan Afr. Med. 2020;37:357. https://doi.org/10.11604/pamj.2020.37.357.27287.
Cinaroglu S. The impact of oversampling with “ubSMOTE” on the performance of machine learning classifiers in prediction of catastrophic health expenditures. Operations Research for Health Care. 2020;27:100275.
Babu SK, Vasavi S. Predictive analytics as a service on Tax Evasion using gaussian regression process. Helix. 2017;7(5):1988–93.
Maccarrone G, Morelli G, Spadaccini S. GDP Forecasting: Machine Learning, Linear or Autoregression ?, Frontiers in Artificial Intelligence, 4, 1–9. Disponible sur https://doi.org/10.3389/frai.2021.757864; consulté le 04/06/2023. [Page 10.]
Soybilgen B, Yazgan E. Nowcasting us gdp using tree-based ensemble models and dynamic factors. Comput Econ. 2021;57(1):387–417.
Lin S-L. Application of empirical mode decomposition to improve deep learning for US GDP data forecasting. Heliyon. 2022;8(1):e08748.
Mele M, Randazzo L. On the Chinese’health expenditure: from Toda-Yamamoto to machine learning approach. J Chin Economic Bus Stud. 2020;18(4):289–309.
Yan S, Zhou Y, Zhang Y. Analysis of Balance of Income and Expenditure and Optimal Retirement Age of Pension Insurance Co-Ordination Account Based on Improved Machine Learning Algorithm. Computational Intelligence and Neuroscience, 2022. https://doi.org/10.1155/2022/5870893.
Shin SM. Prevalence and trends of pain associated with chronic Diseases and personal out-of-pocket medical expenditures in Korea. Korean J Pain. 2017;30(2):142–50.
Iloabuchi C, Dwibedi N, LeMasters T, Shen C, Ladani A, Sambamoorthi U. Low-value medical care in the pandemic—is this what the doctor ordered?, The Lancet Global Health,9 (9): e1203-e1204, ISSN 2214-109X, https://www.sciencedirect.com/science/article/pii/S2214109X21002527.
Rebouças SMDP, Oliveira DABd, Soares RA, Ferreira EMDM, Gouveia MJ. Classification of the financial sustainability of health insurance beneficiaries through data mining techniques. J Spat Organizational Dynamics. 2016;4(3):229–42.
Luo W, Li Y. Basic Public Services, Financial Competition and Economic Growth of Urban Agglomeration on Yangtze River Delta Based on Big Data. InJournal of Physics: Conference Series. 2021 (Vol. 1852, No. 4, p. 042042). IOP Publishing.
Yue JC, Wang H-C, Leong Y-Y, Su W-P. Using Taiwan National Health Insurance Database to model cancer incidence and mortality rates. IET Intell Transp Syst. 2018;78:316–24.
Wong CA, Kulhari S, McGeoch EJ, Jones AT, Weiner J, Polsky D, et al. Shopping on the public and private health insurance marketplaces: consumer decision Aids and plan presentation. J Gen Intern Med. 2018;33(8):1400–10.
Boccanera F, Brodsky A, editors. OptiHealth: A Recommender Framework for Pareto Optimal Health Insurance Plans. In Proceedings of the 19th International Conference on Enterprise Information Systems (ICEIS 2017). (1):599–609. https://doi.org/10.5220/0006334905990609.
Chen H, Xing J, Yang X, Zhan K. Heterogeneous Effects of Health Insurance on Rural Children’s Health in China: a Causal Machine Learning Approach. Int J Environ Res Public Health. 2021;18(18):9616.
Kreif N, DiazOrdaz K, Moreno-Serra R, Mirelman A, Hidayat T, Suhrcke M. Estimating heterogeneous policy impacts using causal machine learning: a case study of health insurance reform in Indonesia. Health Serv Outcomes Res Method. 2022;22(2):192–227.
Sidey-Gibbons C, Pfob A, Asaad M, et al. Development of machine learning algorithms for the prediction of financial toxicity in localized breast Cancer following surgical treatment. JCO Clin Cancer Inform 2021;5:338–347. https://doi.org/10.1200/CCI.20. 00088.
Yang C, Delcher C, Shenkman E, Ranka S, editors. Identifying high health care utilizers using post-regression residual analysis of health expenditures from a state Medicaid program. AMIA 2017 American Medical Informatics Association Annual Symposium, November 4-8, 2017.
Matloob I, Khan SA, Hussain F, Butt WH, Rukaiya R, Khalique F. Need-based and optimized health insurance package using clustering algorithm. Appl Sci. 2021;11(18):8478.
Zahi S, Achchab B, editors. Clustering of the population benefiting from health insurance using K-means. Paper presented at the 4th International Conference on Smart City Applications, Casablanca, Morocco, October 2–4.
Mueller E, Sandoval JO, Mudigonda S, Elliott M. A cluster-based machine learning ensemble approach for geospatial data: estimation of health insurance status in Missouri. ISPRS Int J Geo-Information. 2018;8(1):13.
Mueller ED, Sandoval J, Mudigonda SP, Elliott M. Extending cluster-based ensemble learning through synthetic population generation for modeling disparities in health insurance coverage across Missouri. J Comput Social Sci. 2019;2(2):271–91.
Pnevmatikakis A, Kanavos S, Matikas G, Kostopoulou K, Cesario A, Kyriazakos S. Risk assessment for personalized health insurance based on real-world data. Risks. 2021;9(3):46.
Mladenovic SS, Milovancevic M, Mladenovic I, Petrovic J, Milovanovic D, Petković B, et al. Identification of the important variables for prediction of individual medical costs billed by health insurance,” Technol Soc. 2020;62. https://doi.org/10.1016/J.TECHSOC.2020.101307.
Dutta K, Chandra S, Gourisaria MK, Harshvardhan G, editors. A data mining based target regression-oriented approach to modelling of health insurance claims. 2021 5th International Conference on Computing Methodologies. and Communication (ICCMC); 2021. p. 1168–1175.
Krishnamurthy S, KS K, Dovgan E, Luštrek M, Gradišek Piletič B, Srinivasan K, Li Y-C, Gradišek A, Syed-Abdul S. Machine Learning Prediction Models for Chronic Kidney Disease Using National Health Insurance Claim Data in Taiwan. Healthcare. 2021;9(5):546. https://doi.org/10.3390/healthcare9050546.
Kaushik K, Bhardwaj A, Dwivedi AD, Singh R. Machine learning-based regression framework to predict health insurance premiums. Int J Environ Res Public Health. 2022;19(13):7898.
Jamil SU, Khan MA, ur Rehman S. Intelligent Task Off-Loading and Resource Allocation for 6G Smart City Environment. In Proceedings of the 2020 IEEE 45th Conference on Local Computer Networks (LCN), Sydney, NSW, Australia, 16–19 November 2020. p. 441–444.
Singh A, Ramkumar K. Risk assessment for health insurance using equation modeling and machine learning. Int J Knowledge-based Intell Eng Syst. 2021;25(2):201–25.
Ren J, Liu M, Liu Y, Liu J. Optimal resource allocation with spatiotemporal transmission discovery for effective Disease control. Infect Dis Poverty. 2022;11(1):1–11.
Anzilli L, Giove S. Multi-criteria and medical diagnosis for application to health insurance systems: a general approach through non-additive measures. Decisions Econ Finan. 2020;43(2):559–82.
Agterberg J, Zhong F, Crabb R, Rosenberg M. Cluster analysis application to identify groups of individuals with high health expenditures. Health Serv Outcomes Res Method. 2020;20(2):140–82.
Wang FT, Chang Y, Chien WC, Li HH. Injury and medical expenditure in emergency department visits of older veterans. Geriatr Gerontol Int. 2016;16(12):1254–62.
Kauhl B, Schweikart J, Krafft T, Keste A, Moskwyn M. Do the risk factors for type 2 Diabetes Mellitus vary by location? A spatial analysis of health insurance claims in Northeastern Germany using kernel density estimation and geographically weighted regression. Int J Health Geogr. 2016;15(1):1–12.
Ong AKS, Prasetyo YT, Tayao KNM, Mariñas KA, Ayuwati ID, Nadlifatin R, et al. Socio-Economic factors affecting Member’s satisfaction towards National Health Insurance: an evidence from the Philippines. Int J Environ Res Public Health. 2022;19(22):15395.
Hung M, Zhang W, Chen W, Bounsanga J, Cheng C, Franklin JD, et al. Patient-reported outcomes and total health care expenditure in prediction of patient satisfaction: results from a national study. JMIR Public Health and Surveillance. 2015;1(2):e4360.
Laagu MA, Arifin AS, editors. Analysis the issue of increasing national health insurance (BPJS Kesehatan) rates through community perspectives on social media: a case study of Drone Emprit. 2020 International Conference on Smart Technology and Applications (ICoSTA) 2020;1–7.
Ruland CM, & Ravn IH. An information system to improve financial management, resource allocation and activity planning: evaluation results. Studies in health technology and informatics.2001;(2):1203–1206.
Romano E, Iuliano D. A simulation/optimisation approach to support the resource allocation in service firms. Int J Procure Manage. 2018;11(1):53–75.
Ying JJ, Huang P, Chang C, Yang D. A preliminary study on deep learning for predicting social insurance payment behavior. In Proceedings of the 2017 IEEE International Conference on Big Data (Big Data), Boston, MA, USA, 11–14 December 2017; p. 1866–1875.
Xie Y, Schreier G, Chang DC, Neubauer S, Liu Y, Redmond SJ, et al. Predicting days in hospital using health insurance claims. IEEE J Biomedical Health Inf. 2015;19(4):1224–33.
Huang, Yen-Chun, Shao-Jung Li, Mingchih Chen, and Tian-Shyug Lee. 2021. “The Prediction Model of Medical Expenditure Appling Machine Learning Algorithm in CABG Patients” Healthcare 9, no. 6: 710. https://doi.org/10.3390/healthcare9060710.
Ozgulbas N, Koyuncugil AS. Financial profiling of public hospitals: an application by data mining. Int J Health Plann Manag. 2009;24(1):69–83.
Skylakha S, Sakthivel P, Arunselvan K. Empirical study on application of machine learning techniques for resource allocation in health care using KPI. J Supercomputing. 2020;76(4):2266–74.
Landon BE, Reschovsky JD, Pham HH, Kitsantas P, Wojtuskiak J, Hadley J. Creating a parsimonious typology of physician financial incentives. Health Serv Outcomes Res Method. 2009;9(4):219–33.
Grover D, Bauhoff S, Friedman J. Using supervised learning to select audit targets in performance-based financing in health: an example from Zambia. PLoS ONE. 2019;14(1):e0211262.
Moro Visconti R, Morea D. Big data for the sustainability of healthcare project financing. Sustainability. 2019;11(13):3748.
Oliver S, Leary A. Return on investment: workload, complexity and value of the CNS. Br J Nurs. 2012;21(1):32–7.
Wan S, Chen Y, Xiao Y, Zhao Q, Li M, Wu S. Spatial analysis and evaluation of medical resource allocation in China based on geographic big data. BMC Health Serv Res. 2021;21(1):1–18.
Tuppin P, Rivière S, Rigault A, Tala S, Drouin J, Pestel L, et al. Prevalence and economic burden of Cardiovascular Diseases in France in 2013 according to the national health insurance scheme database. Arch Cardiovasc Dis. 2016;109(6–7):399–411.
Pur A, Bohanec M, Lavrač N, Cestnik B. Primary health-care network monitoring: a hierarchical resource allocation modeling approach. Int J Health Plann Manag. 2010;25(2):119–35.
Li J, Lan Q, Zhu E, Xu Y, Zhu D. A Study of Health Insurance Fraud in China and Recommendations for Fraud Detection and Prevention. J Organizational End User Comput (JOEUC). 2022;34(4):1–19.
Shin H, Park H, Lee J, Jhee WC. A scoring model to detect abusive billing patterns in health insurance claims. Expert Syst Appl. 2012;39(8):7441–50.
Ahn E. Introducing big data analysis using data from National Health Insurance Service. Korean J Anesthesiology. 2020;73(3):205–11.
Chien P-S, Tseng Y-F, Hsu Y-C, Lai Y-K, Weng S-F. Frequency and pattern of Chinese herbal medicine prescriptions for urticaria in Taiwan during 2009: analysis of the national health insurance database. BMC Complement Altern Med. 2013;13(1):1–7.
Yoshida N, Mano Y, Matsuda T, Sano Y, Inoue K, Hirose R, et al. Complications of colonoscopy in Japan: an analysis using large-scale health insurance claims data. J Gastroenterol Hepatol. 2021;36(10):2745–53.
Hu Y-H, Tai C-T, Chen SC-C, Lee H-W, Sung S-F. Predicting return visits to the emergency department for pediatric patients: applying supervised learning techniques to the Taiwan National Health Insurance Research Database. Computer methods and programs in biomedicine. 2017;144:105–12.
Emcke T, Ostermann T, Heidbreder M, Schuster R. Comparison of Different Implementations of a Process Limiting Pharmaceutical Expenditures Required by German Law, Proceedings of the 10th International Joint Conference on Biomedical Engineering and Technologies (BIOSTEC). HealthInf. 2017;5:35–40.
Hyer JM, Ejaz A, Tsilimigras DI, Paredes AZ, Mehta R, Pawlik TM. Novel machine learning approach to identify preoperative risk factors associated with super-utilization of medicare expenditure following Surgery. JAMA Surg. 2019;154(11):1014–21.
Sarkar I, et al., Improving hospital-wide early resource allocation through machine learning, in: MEDINFO 2015: EHealth-enabled Health: Proceedings of the 15th World Congress on Health and Biomedical Informatics, IOS Press, 2015. p. 315.
Jakovljevic M, Matter-Walstra K, Sugahara T, Sharma T, Reshetnikov V, Merrick J, et al. Cost-effectiveness and resource allocation (CERA) 18 years of evolution: maturity of adulthood and promise beyond tomorrow. BioMed Central; 2020. pp. 1–6.
Mattei P. Digital governance in tax-funded European healthcare systems: from the Back office to patient empowerment. Isr J Health Policy Res. 2020;9(1):1–5.
Ma M. Research on the Development of Hospital Intelligent Finance Based on Artificial Intelligence. Computational intelligence and neuroscience. 2022 Aug 9;2022:6549766.
Ozgulbas N, Koyuncugil AS. Developing road maps for financial decision making by CHAID Decision Tree. In: Proceeding of international conference on information management and engineering. IEEE Computer Society Press; 2009. p. 723–7.
Andreasik AC, Umpirowicz S. A semantic web technologies-based system for controlling the correctness of medical procedures in Polish National Health Fund. In: Proceedings of the international conference on knowledge management and information sharing (KMIS-2011), Set´ubal, Portugal. 2011. p. 331–6.
Islam MM, Yang H-C, Poly TN, Li Y-CJ. Development of an artificial intelligence–based automated recommendation system for clinical laboratory tests: retrospective analysis of the national health insurance database. JMIR Med Inf. 2020;8(11):e24163.
Hashimoto H, Saito M, Sato J, Goda K, Mitsutake N, Kitsuregawa M, et al. Indications and classes of outpatient antibiotic prescriptions in Japan: a descriptive study using the national database of electronic health insurance claims, 2012–2015. Int J Infect Dis. 2020;91:1–8.
Funding
The authors received no specific funding for this work.
Author information
Authors and Affiliations
Contributions
“AT and MR conceived the study. AT supervised all evaluation phases; he is the guarantor. MR drafted the manuscript. AT and HRR provided feedback on the result and edited the manuscript. MR and AB categorized AI applications independently and created descriptions by synthesizing the extracted information. AAF, AB, and SS edited the manuscript. All authors read and approved the final manuscript.“
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study received ethical approval from the Ethical Committee of the Tehran University of Medical Sciences (Approval ID: IR.TUMS.SPH.REC.1401.063); written informed consent was provided by all participants; all methods were carried out in accordance with relevant guidelines and regulations.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ramezani, M., Takian, A., Bakhtiari, A. et al. The application of artificial intelligence in health financing: a scoping review. Cost Eff Resour Alloc 21, 83 (2023). https://doi.org/10.1186/s12962-023-00492-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12962-023-00492-2