Abstract
Objective
Airborne infection from aerosolized SARS-CoV-2 poses an economic challenge for businesses without existing heating, ventilation, and air conditioning (HVAC) systems. The Environmental Protection Agency notes that standalone units may be used in areas without existing HVAC systems, but the cost and effectiveness of standalone units has not been evaluated.
Study design
Cost-effectiveness analysis with Monte Carlo simulation and aerosol transmission modeling.
Methods
We built a probabilistic decision-analytic model in a Monte Carlo simulation that examines aerosol transmission of SARS-CoV-2 in an indoor space. As a base case study, we built a model that simulated a poorly ventilated indoor 1000 square foot restaurant and the range of Covid-19 prevalence of actively infectious cases (best-case: 0.1%, base-case: 2%, and worst-case: 3%) and vaccination rates (best-case: 90%, base-case: 70%, and worst-case: 0%) in New York City. We evaluated the cost-effectiveness of improving ventilation rate to 12 air changes per hour (ACH), the equivalent of hospital-grade filtration systems used in emergency departments. We also provide a customizable online tool that allows the user to change model parameters.
Results
All 3 scenarios resulted in a net cost-savings and infections averted. For the base-case scenario, improving ventilation to 12 ACH was associated with 54 [95% Credible Interval (CrI): 29–86] aerosol infections averted over 1 year, producing an estimated cost savings of $152,701 (95% CrI: $80,663, $249,501) and 1.35 (95% CrI: 0.72, 2.24) quality-adjusted life years (QALYs) gained.
Conclusions
It is cost-effective to improve indoor ventilation in small businesses in older buildings that lack HVAC systems during the pandemic.
Similar content being viewed by others
Introduction
SARS-CoV-2 may be transmitted person-to-person via exhaled respiratory aerosols that accumulate within poorly ventilated spaces [1,2,3,4,5]. Airborne transmission of SARS-CoV-2 therefore poses major public health and economic challenges as commercial spaces re-open [3]. To meet this challenge, newer commercial spaces can upgrade existing heating, ventilation, and air conditioning (HVAC) systems [6,7,8,9]. One standard is 12 air exchanges per hour (ACH), the recommended ventilation for emergency department waiting rooms [10].
However, older buildings tend not to have HVAC systems installed. When HVAC systems are not present, the Environmental Protection Agency (EPA) recommends alternative means of disinfecting the air [11]. These may include standalone filtration systems containing high efficiency particulate air (HEPA) or electrostatic units, which filter particles down to the sub-micrometer size [11]. However, standalone HEPA filtration units are not designed for high-volume air filtration, and the size and quantity of such units to achieve 12 ACH may not be practical. This is particularly true in poorly ventilated bars, cafes, and restaurants because customers intermingle without face coverings [12, 13].
Given that standalone HEPA filtration units may be only marginally effective and are relatively expensive, we evaluated their cost-effectiveness. In this paper, we provide data for an example setting (a poorly ventilated restaurant), but our online model can be modified for any scenario.
Methods
We built a decision-analytic model that is designed to assist local and federal regulators in setting standards for improving the indoor air ventilation in poorly ventilated indoor commercial spaces for the prevention of SARS-CoV-2 infections via aerosolized particles. The model is designed to compute the incremental cost-effectiveness ratio (ICER), which is the net cost of an intervention divided by the number of quality-adjusted life years (QALYs) gained [14]. The ICER can be used to compare commonly deployed health or medical interventions to assess whether they are affordable [15, 16]. We followed guidelines for conducting our cost-effectiveness analyses [17], including estimation of costs from a societal perspective. We based our analysis on a standardized space for the purposes of this paper. We based the range of actively infectious cases and full vaccination rates from New York City between March 1, 2020 through March 1, 2022. More importantly, we provided an online interface that allows the user to tailor the model input parameters. This online model can be used to estimate the cost-effectiveness of improving the indoor ventilation rate over a range of costs, spaces, and viral transmission rates (https://openupuniversities.shinyapps.io/Airborne_Transmission_Covid19/).
Characteristics of the standardized space
Each restaurant, café, or bar is unique with respect to the size, number of customers, hours of operation, and the time that customers spend in the establishment. This variation presents challenges for understanding the airflow and filtration needs for any given business. In this paper, we used a small, poorly ventilated restaurant space as an example so that the reader can get a general idea of the cost-effectiveness of standalone ventilation. In addition, our customizable interface can allow both regulators and restaurant owners to obtain estimates for a range of settings.
The standardized restaurant was open for a total of 3 h for lunch service and 6 h for dinner service. We assumed that the restaurant has a seating capacity of 30 occupants in a 1000 square foot space and a ceiling height of 9 feet, and that each occupant is seated for one-hour at lunch and 1.5-h during dinner. The model assumptions are listed in Table 1.
Temporal evolution of concentration of viable viral copies in an indoor space
In a previous published work, two co-authors developed a model [18] and online tool [19] for the temporal concentration of aerosolized viral copies in the air under well-mixed conditions for an infected individual present in an indoor space. It should be noted that stratification of infectious aerosols and, therefore, a deviation from well-mixed conditions, will occur across different indoor settings. Differences in room geometry, temperature, or positioning of the HEPA units will impact the results [20]. However, the motion of occupants [21] characteristic of busy settings such as those investigated in this work adds mixing to the room air leading to a condition closer to well-mixed aerosols [22]. Specialist advice should be taken when positioning such standalone units. The model considers the evaporation and settling of virus-laden droplets of various sizes exhaled by an infected individual in terms of plaque forming units (PFUs). These are evaluated from a combination of reduced-order modeling and previous experimental measurements. The details are described elsewhere [18]. In brief, the concentration of PFUs dispelled by an infected person in an indoor space can be shown as:
where, \(C\left(t\right):\) concentration of viral PFUs over time and \(C\left({t}_{0}\right)\) represents the concentration at baseline; \({n}_{inf}:\) number of infected individuals in the room; \({N}_{gen}:\) generating factor for viral particles emitted by continuous exhalation of the infected person while speaking per time unit. The generating factor of 0.059 PFU/second [18] was estimated using a viral load at the sputum of the infected person of 1010 virus RNA copies/ml. While the mean virus RNA copies/ml of the infected sputum for the original strains of Covid-19 was estimated as 7 × 106 [23], the emerging evidence shows that the number of viral copies is almost 1000 times larger for the Delta variant [24], the most common Covid-19 strain at the time of publication. Therefore, to be conservative, we assumed a 1010 virus RNA copies/ml for the Delta variant. We then applied a conversion factor of 0.01 to estimate PFUs (infectious units) from RNA copies [18]. Here, the aerosol cut-off diameter—the size below which particles are carried by the ventilation air flow—was assumed to be 20 μm. The exhalation flow rate was assumed to be 0.211 l/second representing a sedentary activity [18]; \(V:\) Volume of the room. We showed our analysis for a 1000 ft2 restaurant area size with a ceiling height of 9 ft; \(\lambda :\) Natural viral decay rate. An exponential decay at a rate of 0.636 per hour was assumed [25]; \(\kappa :\) Settling rate of aerosols by gravity. A value of 0.39 per hour was assumed [18]; \(\nu :\) ventilation rate of the room with outside air; and \(s:\) sterilization rate through air filters or air cleaners.
Risk of infection in an indoor space through long-range transmission of airborne, aerosolized SARS-CoV-2 particles
For an average susceptible individual sitting in the restaurant, we calculated the risk of SARS-CoV-2 infection based on the number of viral PFUs that the individual is exposed to for the duration of a lunch event (1 h) or a dinner event (1.5 h). A susceptible individual is defined as a person who is disease-free at the start of lunch or dinner service and is at risk of contracting the disease while sitting in the restaurant. We assumed that if \(N\) people are sitting in the restaurant for an event, based on the prevalence of disease in the surrounding community (denoted by \(Pr\)), there would be, on average, \(N\cdot Pr\) infected individuals and \(N-N\cdot Pr\) susceptible individuals for that event. We calculated the number of PFU units that a susceptible individual is exposed to during an event (denoted by \({nPFU}_{exposed}\)) as follows:
where, \({t}_{1}\) and \({t}_{2}:\) represents respectively the starting and ending time of the event; \(N\cdot Pr:\) represent the average number of infected people in the event; \({C}_{PFU}\left(t\right):\) represents the temporal concentration of viral PFU units (see the section “Temporal evolution of concentration of viable viral copies”); and \(Inhalation\_rate\): Inhalation rate of 0.521 L/second for an average person with a sedentary activity person (e.g., sitting and speaking) [26].
We calculated the risk of infection (denoted by \({p}_{inf}\)) for an average individual based on the number of viral PFUs the individual is exposed to during an event as follows:
where \({p}_{d}\) represents the probability of infection per exposure to one viral PFU. We calculated \({p}_{d}\) as 0.0024 [95% Confidence Interval (CI) 0.0013–0.0053] based on an infectious dose 50 (ID50) of 280 (95% CI 130–530) PFUs [18, 27]. The ID50 indicates the number of viral particles required to cause infection in 50% of the individuals exposed to these particles. We varied the probability of infection of exposure to one viral PFU to test the cost-effectiveness for a range of airborne transmissibility values of SARS CoV-2 for past and potential future variants.
The above modeling approach considers only infection through the inhalation of accumulated aerosols, often referred to as the “long-range” mode of airborne transmission. Thus, transmission through the close-range mode—that is, when infectious aerosols were inhaled directly from the exhaled breath of an infected individual by a susceptible person in its vicinity—was assumed to be on par between the comparison arms and was disregarded.
Costs
We modeled the cost of installing standalone air filtration units with HEPA filters, which trap ultrafine particles down to the sub-micrometer size [11]. Based on the restaurant’s size and cubic feet per minute (CFM) airflow of the standalone units, we calculated the number of units required to produce the equivalent of 12 ACH in the room. These units were assumed to be uniformly installed in the room to create different points of air disturbance.
We modeled direct and indirect costs of hospitalizations due to Covid-19 [28, 29]. For indirect costs of hospitalizations, we assumed a 21-day absence from work spanning the time spent in the hospital time spent at home after hospital discharge. We assumed 8 h of work lost per day at a value of $25/hour [30]. We assumed a 14-day quarantine for symptomatic infections for lost productivity and leisure time of 8 h per day. Future values were discounted at 3% [14, 17]. All costs were adjusted to 2020 US dollars (Table 2).
Health-related quality of life
We modeled losses of QALYs associated with a Covid-19 symptomatic infection and Covid-19 hospitalization [31]. A QALY is a metric capturing both longevity and health-related quality of life (HRQL). A QALY can be conceptualized as a year of life lived in perfect health and is calculated as the product of the life years remaining and the HRQL score. We also modeled changes in QALYs for the proportion of infected individuals who suffer from long-haul Covid-19 symptoms [31]. Finally, we modeled losses of QALYs associated with a Covid-19 premature death [32]. We discounted future values at 3% [14, 17].
Analysis
We compared two interventions: (1) no improvement in the baseline ventilation rate of 0.8 ACH (‘status quo’), and (2) improving the room ventilation rate to 12 ACH. Our mathematical model was probabilistic and was developed in a Monte Carlo simulation of 5000 iterations, with each iteration randomly drawing from probability distributions of the input parameters. Table 2 shows the model inputs along with their probability distribution.
We performed our analyses for different conditions defined by the mean year-round prevalence of actively infectious cases in the surrounding communities where the restaurant is located and the proportion of patrons that are vaccinated. For the base case model, we assumed a 2% mean year-round prevalence of actively infectious cases in the surrounding community and a 70% full-vaccination rate among customers sitting in the restaurant, defined as 2 doses of an FDA approved vaccine in the US. We modeled the random daily incidence rate from a normal distribution and summed the daily incidence rates over the past 12 days to obtain the daily prevalence of actively infectious cases. This assumes an average of 12 days of infectiousness for an exposed individual beginning 2 days prior to symptom onset (for symptomatic cases) plus 10 days following the initial symptom onset [33, 34].
For the best-case scenario (minimum number of infections), we assumed a year-round prevalence of actively infectious cases of 0.1% in the surrounding community and a 90% full-vaccination rate among customers sitting in the restaurant.
For the worst-case scenario (maximum number of infections), we assumed a year-round prevalence of actively infectious cases of 3% in the surrounding community and a 0% full-vaccination rate among customers sitting in the restaurant.
The time horizon of the model was one year and the analytic horizon was lifetime. The outcomes of the model were incremental direct and indirect costs, infections averted, QALYs gained, and ICER for improving the ventilation rate. We also conducted one-way sensitivity analyses over all core input parameters of the model to measure the robustness of model outcomes against changes in these parameters.
Results
Base-case scenario
(2% prevalence of disease in the surrounding community where the restaurant is located and 70% full-vaccination rate among of restaurant customers). Improving the room ventilation rate to 12 ACH was associated with 54 [95% credible interval (CrI): 29, 86] infections averted in the standardized restaurant over one year. This produced cost savings of $152,701 (95% CrI: $80,663, $249,501), and 1.35 (95% CrI: 0.72, 2.24) incremental QALYs gained. Table 3 shows the complete results.
The best-case scenario
(0.1% prevalence of disease in the surrounding community where the restaurant is located and 90% full-vaccination rate among restaurant customers). This scenario reflects conditions far better than were observed for the United States for the pandemic through October of 2021. It was associated with cost savings of $2,003 (95% CrI: − $881, $5968) and 0.05 (95% CrI: 0.03, 0.09) QALYs gained.
The worst-case scenario
(3% prevalence of disease in the surrounding community where the restaurant is located and 0% full-vaccination rate among restaurant customers). In this scenario, improving the room ventilation rate to 12 ACH was associated with 135 (95% CrI: 76, 213) infections averted, $455,277 (95% CrI: $247,879, $734,424) savings in costs, and 3.66 (95% CrI: 1.98, 6.02) increases in QALYs gained.
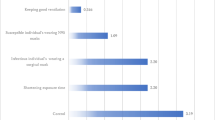
Figure 1 shows the results of the one-way sensitivity analyses. In all sensitivity analyses, improving the room ventilation rate was cost-saving (dominant strategy) in the base-case scenario, meaning standalone air filtration units reduced airborne infections, increased QALYs gained, and resulted in savings for the commercial establishment.
One-way sensitivity analysis (tornado diagram) for each of the core input parameters of the model. The range of each value represents the incremental cost-effectiveness ratio associated with varying model input parameters over a range of plausible values for the base-case model scenario (1000 ft2 restaurant space, 2% prevalence of actively infectious cases, a 70% vaccination rate, and an upgrade from 0.8 ACH to 12 ACH). QALYs quality-adjusted life years; ACH air changes per hour. Note in all the sensitivity analyses, improving the ventilation rate to 12 ACH saved money and improved health. Therefore, the negative incremental cost-effectiveness ratios on the x-axis can be interpreted as decreases in costs associated with improving the ventilation rate for one QALY gained. We encourage the reader to utilize the online model to obtain model outputs specific to the scenario that they wish to evaluate
Figure 2 shows the probabilistic distribution of differential costs and differential QALYs of improving the room ventilation rate across all the Monte Carlo simulation runs. For the base-case and worst-case scenarios, in all the simulation runs, improving the ventilation rate resulted in cost savings and QALYs gained. Under the best-case scenario, 89% of the simulations resulted in cost savings and QALYs gained, and the 95% credible interval for ICER ranged from cost-saving (for intervention) to $30,503/QALY (< $50,000/QALY gained).
The cost-effectiveness plane representing the incremental costs versus incremental QALYs for improving the ventilation rate of an exemplary 1000 ft2 restaurant space to 12 ACH for: A the base-case scenario (mean year-round prevalence of 2% in the surrounding community where the restaurant is located and when 70% of the customers are vaccinated); B the best-case scenario (mean year-round prevalence of 0.1% in the surrounding community where the restaurant is located and when 90% of the restaurant customers are vaccinated); and (C) the worst-case scenario (mean year-round prevalence of 3% in the surrounding community where the restaurant is located and when no customer is vaccinated). The dots in the plot show the probabilistic runs of the Monte Carlo simulation with 5000 iterations. QALYs quality-adjusted life years; ACH air changes per hour
Scenario analysis for a range of airborne transmissibility values
Because the variants of SARS CoV-2 are constantly changing (e.g., transition from Delta to Omicron BA.2), we conducted a scenario analysis to test the cost-effectiveness for different values of the airborne transmissibility of SARS CoV-2 (by changing the probability of infection per exposure to one viral PFU). When the airborne transmissibility was reduced by 50% (for variants with 50% lower rates of airborne spread), the standalone units were associated with $74,327 savings in costs and 0.67 increases in QALYs gained. When the airborne transmissibility was increased by 50% (for variants with 50% higher airborne spread), the standalone units were associated with $230,557 savings in costs and 2.02 increases in QALYs gained. Our online model allows the user to change the airborne transmissibility of SARS Cov-2 as new evidence emerges.
Discussion
In this study, we evaluated the cost-effectiveness of improving ventilation in commercial indoor spaces using standalone HEPA filtration units as a method of preventing the transmission of airborne SARS-CoV-2. We built our probabilistic model using a Monte Carlo simulation so that the average model outcomes account for uncertainties and represent different ranges of variability in model input parameters and assumptions. Our probabilistic analyses showed that under all scenarios—even when the mean year-round prevalence of actively infectious cases was as low as 0.1% and 90% of the restaurant’s patrons were fully vaccinated—improving the ventilation rate of the indoor spaces by standalone air-filtration units would result in cost savings and QALYs gained. Our model was robust to changes across a range of inputs and assumptions, suggesting that policy mandates for HEPA filtration system use would be prudent in most situations.
There is a growing body of research modeling airborne transmission of SARS CoV-2 via aerosolized particles in indoor spaces [18, 35,36,37,38,39]. A recent study suggested that inhalation of aerosolized SARS-COV-2 particles is deemed to be an important source of transmission of the virus among the general population [36] and provided a theoretical model to quantify a safety cap for the number of occupants and the amount of time they should spend in an indoor space to reduce the airborne transmission of the virus. Other studies support the transmission of Covid-19 by aerosols [37], and suggest that indoor ventilation can significantly reduce infection [39]. However, the cost-effectiveness of such airborne preventive measures in a poorly ventilated indoor space is not clear, and hinges upon multiple factors. These include the community prevalence of disease, number of occupants and their time spent in the room, size of the room, and the proportion of occupants that are fully vaccinated. Our model allows for adjustable model input parameters that can be customized by the user using the accompanying online application (https://openupuniversities.shinyapps.io/Airborne_Transmission_Covid19/).
The underpinning risk transmission model has been previously vetted [18]. However, the parameter representing the airborne transmissibility, or the probability of infection for exposure to one viral PFU, must be modified according to emerging data from the current, predominant strain of SARS-CoV-2 [24]. Moreover, room geometry, temperature differences, or the motion of occupants can produce large changes in concentrations of aerosolized virus [20, 21].
Our study was limited in several ways. First, we modeled the hospitalization rate and mortality rate only as a function of age in line with the previous studies [31, 40]. In theory, however, hospitalization and mortality rates are also functions of other patient characteristics, such as gender, race, comorbidity, and socioeconomic status. Because the intent of our analysis was improving ventilation, we only modeled infections through inhalation of airborne, aerosolized viruses that may accumulate indoors, and we did not model infections via other pathways such as fomite transmission or inhalation of small and large droplets shortly after they are exhaled. This would result in an underestimate of cost savings and QALYs gained. In addition, our model does not provide data across different variants of SARS-CoV-2. Users of our online model must input transmission rates of the currently circulating strain to estimate the impact of standalone HEPA filtration units. We also note that, irrespective of whether aerosol transmission, droplet transmission, or fomite transmission is dominant, our model outcomes are not impacted.
Conclusions
Even in the absence of SARS-CoV-2, poor ventilation systems in commercial spaces pose significant public health risks [41]. As the Covid-19 turns into an endemic disease, and as new pathogens emerge, it is critically important to set standards for ventilation of commercial spaces, even when they are in older buildings. In doing so, regulators must walk a fine line between setting standards that are too stringent to be economically viable for small business owners and the safety of the patrons of those establishments. We found that these systems are affordable from a governmental regulatory standpoint for most businesses. Moreover, as competition increases for novel air filtration systems, these systems are likely to fall in cost and increase in efficacy.
Availability of data and materials
We build an accompanying online dashboard for the model. Other data will be available upon request from the authors.
References
Coleman KK, Tay DJW, Sen Tan K, Ong SWX, Son TT, Koh MH, et al. Viral load of SARS-CoV-2 in respiratory aerosols emitted by COVID-19 patients while breathing, talking, and singing. Clin Infect Dis. 2021. https://doi.org/10.1093/cid/ciab691.
Lednicky JA, Lauzardo M, Fan ZH, Jutla A, Tilly TB, Gangwar M, et al. Viable SARS-CoV-2 in the air of a hospital room with COVID-19 patients. Int J Infect Dis. 2020;100:476–82.
Li Y, Leung GM, Tang JW, Yang X, Chao CYH, Lin JZ, et al. Role of ventilation in airborne transmission of infectious agents in the built environment - a multidisciplinary systematic review. Indoor Air. 2007;17(1):2–18.
Zhang R, Li Y, Zhang AL, Wang Y, Molina MJ. Identifying airborne transmission as the dominant route for the spread of COVID-19. Proc Natl Acad Sci. 2020;117(26):14857–63.
Fennelly KP. Particle sizes of infectious aerosols: implications for infection control. Lancet Respir Med. 2020;8(9):914–24.
Fisk WJ, Rosenfeld AH. Estimates of improved productivity and health from better indoor environments. Indoor Air. 1997;7(3):158–72.
Centers for Disease Control and Prevention. Ventilation in buildings. Atlanta: Centers for Disease Control and Prevention; 2020.
World Health Organization. Roadmap to improve and ensure good indoor ventilation in the context of COVID-19. Geneva: World Health Organization; 2021.
GOV.UK. Ventilation of indoor spaces to stop the spread of coronavirus (COVID-19). United Kingdom: GOV.UK; 2021.
Centers for Disease Control and Prevention. Guidelines for environmental infection control in health-care facilities. Atlanta: Centers for Disease Control and Prevention; 2019.
Environmental Protection Agency. Air cleaning devices that use bipolar ionization, including portable air cleaners and in-duct air cleaners used in HVAC systems. Washington, DC: Environmental Protection Agency; 2021.
Lerner AM, Folkers GK, Fauci AS. Preventing the spread of SARS-CoV-2 with masks and other “Low-tech” interventions. JAMA. 2020;324(19):1935–6.
Lewis D. Why indoor spaces are still prime COVID hotspots. Nature. 2021;592(7852):22–5.
Neumann PJ, Sanders GD, Russell LB, Siegel JE, Ganiats TG. Cost-effectiveness in health and medicine. 2nd ed. New York: Oxford University Press; 2016. p. 536.
Muennig PA, Bounthavong M. Cost-effectiveness analysis in health: a practical approach. Hoboken: Wiley; 2016.
Wonderling D, Sawyer L, Fenu E, Lovibond K, Laramée P. National clinical guideline centre cost-effectiveness assessment for the national institute for health and clinical excellence. Ann Intern Med. 2011;154(11):758–65.
Sanders GD, Neumann PJ, Basu A, Brock DW, Feeny D, Krahn M, et al. Recommendations for conduct, methodological practices, and reporting of cost-effectiveness analyses: second panel on cost-effectiveness in health and medicine. JAMA. 2016;316(10):1093–103.
de Oliveira PM, Mesquita LCC, Gkantonas S, Giusti A, Mastorakos E. Evolution of spray and aerosol from respiratory releases: theoretical estimates for insight on viral transmission. Proc R Soc Math Phys Eng Sci. 2021;477(2245):20200584.
Gkantonas S, Zabotti D, Mesquita L, Mastorakos E, de Oliveira P. Airborne.cam: a risk calculator of SARS-CoV-2 aerosol transmission under well-mixed ventilation conditions [Software]. 2021.https://doi.org/10.17863/CAM.72192. Accessed 20 Jul 2021.
Bhagat RK, Wykes MSD, Dalziel SB, Linden PF. Effects of ventilation on the indoor spread of COVID-19. J Fluid Mech. 2020. https://doi.org/10.1017/jfm.2020.720.
Mingotti N, Wood R, Noakes C, Woods AW. The mixing of airborne contaminants by the repeated passage of people along a corridor. J Fluid Mech. 2020. https://doi.org/10.1017/jfm.2020.671.
Castellini JE, Faulkner CA, Zuo W, Lorenzetti DM, Sohn MD. Assessing the use of portable air cleaners for reducing exposure to airborne diseases in a conference room with thermal stratification. Build Environ. 2022;1(207): 108441.
Wölfel R, Corman VM, Guggemos W, Seilmaier M, Zange S, Müller MA, et al. Virological assessment of hospitalized patients with COVID-2019. Nature. 2020;581(7809):465–9.
Li B, Deng A, Li K, Hu Y, Li Z, Xiong Q, et al. Viral infection and transmission in a large well-traced outbreak caused by the Delta SARS-CoV-2 variant. Nat Commun. 2021. https://doi.org/10.1101/2021.07.07.21260122v1.
van Doremalen N, Bushmaker T, Morris DH, Holbrook MG, Gamble A, Williamson BN, et al. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N Engl J Med. 2020;382(16):1564–7.
Gupta JK, Lin C-H, Chen Q. Characterizing exhaled airflow from breathing and talking. Indoor Air. 2010;20(1):31–9.
Watanabe T, Bartrand TA, Weir MH, Omura T, Haas CN. Development of a dose-response model for SARS coronavirus. Risk Anal. 2010;30(7):1129–38.
Bartsch SM, Ferguson MC, McKinnell JA, O’Shea KJ, Wedlock PT, Siegmund SS, et al. the potential health care costs and resource use associated with COVID-19 in the United States. Health Aff Proj Hope. 2020;39(6):927–35.
Avalere. COVID-19 hospitalizations projected to cost up to $17B in US in 2020. Washington: Avalere; 2020.
May 2020 state occupational employment and wage estimates. https://www.bls.gov/oes/2020/may/oessrcst.htm. Accessed 23 Aug 2021.
Sandmann FG, Davies NG, Vassall A, Edmunds WJ, Jit M, Sun FY, et al. The potential health and economic value of SARS-CoV-2 vaccination alongside physical distancing in the UK: a transmission model-based future scenario analysis and economic evaluation. Lancet Infect Dis. 2021;21(7):962–74.
Briggs A. Moving beyond “lives saved” from COVID-19. https://avalonecon.com/moving-beyond-lives-saved-from-covid-19/. Accessed 20 Jul 2021.
CDC. Interim guidance on ending isolation and precautions for adults with COVID-19. Atlanta: Centers for Disease Control and Prevention; 2020.
Walsh KA, Spillane S, Comber L, Cardwell K, Harrington P, Connell J, et al. The duration of infectiousness of individuals infected with SARS-CoV-2. J Infect. 2020;81(6):847–56.
Pei G, Rim D, Taylor MI. Effects of indoor airflow and ventilation strategy on the airborne virus transmission. ASHRAE Trans. 2021;127(1):206–16.
Bazant MZ, Bush JWM. A guideline to limit indoor airborne transmission of COVID-19. Proc Natl Acad Sci. 2021. https://doi.org/10.1073/pnas.2018995118.
Greenhalgh T, Jimenez JL, Prather KA, Tufekci Z, Fisman D, Schooley R. Ten scientific reasons in support of airborne transmission of SARS-CoV-2. The Lancet. 2021;397(10285):1603–5.
National Academies of Sciences, Engineering, and Medicine. Airborne transmission of SARS-CoV-2: proceedings of a workshop—in brief. Natl Acad Sci. 2020. https://doi.org/10.17226/25958.
Allen JG, Ibrahim AM. Indoor air changes and potential implications for SARS-CoV-2 transmission. JAMA. 2021;325(20):2112–3.
Davies NG, Kucharski AJ, Eggo RM, Gimma A, Edmunds WJ, Jombart T, et al. Effects of non-pharmaceutical interventions on COVID-19 cases, deaths, and demand for hospital services in the UK: a modelling study. Lancet Public Health. 2020;5(7):e375–85.
Sundell J, Levin H, Nazaroff WW, Cain WS, Fisk WJ, Grimsrud DT, et al. Ventilation rates and health: multidisciplinary review of the scientific literature. Indoor Air. 2011;21(3):191–204.
Alene M, Yismaw L, Assemie MA, Ketema DB, Mengist B, Kassie B, et al. Magnitude of asymptomatic COVID-19 cases throughout the course of infection: a systematic review and meta-analysis. PLoS ONE. 2021;16(3): e0249090.
Sudre CH, Murray B, Varsavsky T, Graham MS, Penfold RS, Bowyer RC, et al. Attributes and predictors of long COVID. Nat Med. 2021;27(4):626–31.
Lopez Bernal J, Andrews N, Gower C, Gallagher E, Simmons R, Thelwall S, et al. Effectiveness of Covid-19 vaccines against the B.1.617.2 (Delta) variant. N Engl J Med. 2021;385(7):585–94.
Alen BreatheSmart 75i True HEPA Air Purifier. Alen. https://alen.com/products/alen-breathesmart-75i-air-purifier. Accessed 18 Aug 2021.
Acknowledgements
N/A.
Funding
This study did not have funding.
Author information
Authors and Affiliations
Contributions
ZZ developed the study idea, designed the study, performed the statistical analysis and programming, and wrote the first draft of the manuscript; PMDO and SG helped with the methodology, implementation, and interpretation of findings. PAM helped with the study design, implementation, and interpretation of findings. CE helped with data collection. All authors contributed to the writing. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was based upon modeling of previously published data and was exempt from ethics approval.
Consent for publication
N/A.
Competing interests
Authors declared no competing interests. The study was requested by officials advising the governor of New York and the mayor of New York City and the last author is advising Columbia University on Covid-19 transmission models. No authors have any financial or other stake in the outcomes of the analysis.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zafari, Z., de Oliveira, P.M., Gkantonas, S. et al. The cost-effectiveness of standalone HEPA filtration units for the prevention of airborne SARS CoV-2 transmission. Cost Eff Resour Alloc 20, 22 (2022). https://doi.org/10.1186/s12962-022-00356-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12962-022-00356-1