Abstract
Background
Analyses of extensive, nationally representative databases indicate a rising prevalence of venous thromboembolism (VTE) among critically ill children. However, the majority of studies on childhood VTE have primarily concentrated on Caucasian populations in the United States and European countries. There is a lack of epidemiological studies on VTE in Chinese children.
Methods
We conducted a retrospective cohort study of data from the Pediatric Intensive Care (PIC) database. Data were obtained and extracted by using Structured Query Language (SQL) and the administrative platform pgAdmin4 for PostgreSQL. Bivariate analyses were conducted in which categorical variables were analyzed by a chi-square test and continuous variables were analyzed by a Student’s t-test. Separate multivariable logistic regressions were employed to investigate the associations between VTE and sociodemographic factors as well as clinical factors.
Results
Our study included 12,881 pediatric patients from the PIC database, spanning the years 2010 to 2018. The incidence rate of pediatric VTE was 0.19% (24/12,881). The venous thrombotic locations were deep venous thrombosis extremities (n = 18), superior vena cava (n = 1), cerebral sinovenous (n = 1), and other deep venous thrombosis (n = 4). Univariate analysis showed that age, weight, shock, sepsis, cancer and vasopressor receipt were statistically significant risk factors for pediatric VTE (all p ≤ 0.05). After multivariable logistic regression analysis, only shock (aOR: 6.77, 95%CI: 1.33–34.73, p = 0.019) and admission for sepsis (aOR: 6.09, 95%CI: 1.76–21.09, p = 0.004) were statistically significant associated with pediatric VTE.
Conclusions
In conclusion, data obtained from the Pediatric Intensive Care (PIC) database revealed a prevalence of VTE in pediatric patients of 0.19%. The most common location for venous thrombi was deep venous thrombosis (DVT) in the extremities. We identified that shock and sepsis were statistically significant factors associated with pediatric VTE.
Similar content being viewed by others
Introduction
Venous thromboembolism (VTE), comprising deep venous thrombosis (DVT) and pulmonary embolism (PE), is becoming increasingly recognized among pediatric patients [1]. In the past, VTE was considered to occur mainly in adults, while VTE in childhood was considered a rare event. With the rising prevalence of utilizing diverse infusion catheters in clinical diagnoses and therapies, there has been a gradual increase in the incidence of VTE among critically ill pediatric patients. Meanwhile, with the continuous improvement of medical imaging, diagnostic equipment and technology, the diagnostic accuracy of VTE in children has been significantly improved. The first epidemiological study on VTE in children was conducted in the 1990s and showed an incidence of VTE of 0.7 per 10,000 children in Canada [2]. Subsequently, annual pediatric VTE rates of 0.14 per 10,000 were reported in the Netherlands and 0.07 per 10,000 in the United Kingdom [3, 4]. In 2000, pediatric VTE was reported to occur in about 20 per 10,000 admissions in North American hospitals, and a study conducted specifically in children’s hospitals revealed a progressive increase in pediatric VTE incidence over time [5, 6]. During the period of 2001 to 2007, the annual incidence of VTE in children in the United States increased by 70%, from 34 to 58 cases per 10,000 [7]. Nevertheless, the majority of studies on pediatric VTE have focused primarily on Caucasian populations in the United States and European countries, and although three decades have elapsed since these pioneering studies, the epidemiology of VTE in Chinese children is still poorly studied.
Thrombotic disease predominantly emerges in children when multiple concurrent risk factors are present. Epidemiological studies have identified several pediatric clinical conditions that may be significantly associated with VTE, including central venous catheter (CVC), congenital heart disease (CHD), cancers, infections, intensive care unit (ICU) stays, mechanical ventilation, surgery, sepsis, total parenteral nutrition (TPN), and vasopressor administration [2, 3, 8, 9]. Overall, our current understanding of VTE risk factors in children is limited to a few reviews originating from single institutions or multicenter national registries within a specific country and it is noteworthy that the incidence and risk factors of VTE in children may differ among different ethnic groups and nationalities [10, 11]. Various risk assessment scales, such as the Wells score, Caprini scale and Padua scale, are currently used to evaluate thrombosis risk in patients [12,13,14]. However, these scales take into account factors such as pregnancy, advanced age, and oral contraceptives and are not suitable for children. Therefore, there is a requirement for updated data and a comprehensive approach to examining risk factors in a larger patient population to facilitate the formulation of prevention protocols.
The main purpose of our study was to investigate the occurrence and risk factors of VTE in pediatric patients using a large database of children’s hospital in China, aiming to determine the current prevalence of VTE in children, and to explore the associations between socio-demographic and clinical factors with VTE in children.
Methods
Study design and data
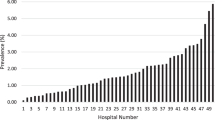
We conducted a retrospective cohort analysis of data from the Pediatric Intensive Care (PIC) database (http://pic.nbscn.org), which is a large, single-centered, bilingual database that contains information about children admitted to critical care units at the Children’s Hospital of Zhejiang University School of Medicine from 2010 to 2018 [15]. Data for the PIC database were extracted and downloaded from various information systems within the hospital, comprising the hospital’s electronic medical record system, laboratory information system, computerized physician order entry system, nursing information system, anesthesia information management system, and reporting system of various examination departments (such as radiology, ultrasound, ECG, pathology, and others). Following the schema of the MIMIC-III database, structured clinical data encompassing patient demographics, medications, fluid balances, comprehensive laboratory results, and microbiological information (including tests conducted and sensitivities) throughout the patients’ entire hospitalization were collated from various systems. Permission to use the data for this study was obtained from the data extraction and processing staff under the authentication number 12739887.
Study sample
The PIC database includes information on 13,499 intensive care unit admissions for 12,881 children aged 0 to 18 years. All pediatric patients in the PIC database were included, and for patients with multiple admissions, only the initial admission was taken into account given the difficulty in attributing results to events subsequent hospitalizations. VTE was identified using diagnosis codes based on ICD-10 Clinical Modification (ICD-10-CM) diagnosis codes. The specifics of the ICD-10 diagnosis codes employed for the identification of VTE are outlined in Supplementary Table 1.
Data extraction
We obtained and extracted all of the data using Structured Query Language (SQL) and the administrative platform pgAdmin4 for PostgreSQL. Demographic data such as ethnicity, age, gender, weight, length of hospital stay, and previously identified risk factors for thrombosis, such as shock, sepsis, cancer, surgical history, use of total parenteral nutrition (TPN), congenital heart disease, and use of vasoactive drugs were collected [2, 3, 8, 9].
Statistical analysis
The demographic information and potential risk factors of patients with thrombosis were compared with those without thrombosis using univariate and multivariate analyses. The variance inflation factor (VIF) method was employed to assess collinearity among variables. The result revealed no significant collinearity (VIF < 5) among the variables in our analysis. The distribution of the independent variables was examined through Shapiro–Wilk test. Bivariate analyses were then conducted utilizing a chi-square test for categorical variables and a Student’s t-tests for continuous variables. Separate multivariable logistic regressions were employed to investigate the associations between VTE and sociodemographic factors as well as clinical factors. The association between risk factors and thrombosis was assessed using the odds ratio (OR). Risk factors with a p-value < 0.1 were incorporated and adjusted for in the multiple logistic regression model. Statistical significance was defined at an alpha level of 5% (p-value < 0.05). All statistical analyses were performed using R, version 4.3.2.
Results
Participant characteristics
Our study included all pediatric patients from the PIC database. The population included 7,366 (57.2%) male and 5,515 (42.8%) female pediatric patients. The mean age of the included pediatric patients was 2.5 years (Q1–Q3: 0.1–3.4), and the mean hospital stay was 17.4 days (Q1–Q3: 7–20.1). The majority of the pediatric patients were Han ethnicity (98.8%).
Prevalence and location of VTE
The incidence rate of pediatric VTE was 0.19% (24/12,881 or 19 cases per 10,000 pediatric patients). Locations of thrombi included deep veins of an extremity (n = 18), the superior vena cava (n = 1), a cerebral venous sinus (n = 1), and other DVT that lacks site-specific information (labeled as “Embolism and thrombosis of other specified veins”) (n = 4).
Risk factors for VTE
Table 1 shows the parameters of univariate analysis comparing pediatric patients with or without thrombosis. Univariate analysis showed that age, weight, shock, sepsis, cancer and vasopressor receipt were statistically significant risk factors for pediatric VTE (all p ≤ 0.05). After multivariable logistic regression analysis, only shock (aOR: 6.77, 95%CI: 1.33–34.73, p = 0.019) and admission for sepsis (aOR: 6.09, 95%CI: 1.76–21.09, p = 0.004) were significantly associated with pediatric VTE. (Table 2)
Discussion
The present study systematically assessed the incidence and risk factors of pediatric VTE through the utilization of a large, pediatric-specific, single-center database. Twelve thousand, eight hundred eighty-one pediatric patients from the PIC database over 9 years were included and the VTE incidence rate was 19 cases per 10,000 pediatric patients. This is consistent with the reported incidence of pediatric VTE range from 0.07 to 21.9 per 10,000 hospital admissions, and with the rising prevalence of utilizing diverse infusion catheters and improvement of diagnostic modalities, the incidence of pediatric VTE increases year by year [2, 6, 11, 16]. Not surprisingly, the prevalence of pediatric VTE was much lower than that in adults [17, 18]. Pediatric VTE follows a bimodal distribution, with the most significant proportion of cases occurring in early infancy, which accounts for up to 20% of all instances [19]. A second peak is observed during adolescence, which represents around 50% of all VTE events in children aged 11 to 18 years old [19]. The reported overall incidence of neonatal thrombosis ranges from 20 to 380 cases per 10,000 neonatal intensive care unit (NICU) admissions [20,21,22,23]. In this study, a total of 24 children were diagnosed with VTE, of whom 8 were < 1 year old, accounting for 30%, a bit higher than the ∼20% reported in previous studies. However, because a relatively large proportion of the included population was < 1 year old, the overall incidence of VTE is lower than that of people aged 1–11 years (8/7041 vs. 11/5119). Moreover, the incidence of VTE in this age group in our study was significantly lower than the reported reference incidence of 1.35% [24]. This can be explained by differences in medical level, ethnic background, region and other factors. Our study observed a higher incidence of VTE in pediatric patients aged 11–18 years compared to those aged 0–1 and 1–11 years, aligning with previous reports.
VTE has been increasingly recognized in pediatric patients, especially in neonates in the ICU. In terms of the site of the thrombus, portal venous thrombosis exhibited the highest prevalence among neonatal thrombotic events, and umbilical venous catheterization was identified as a main risk factor [21, 25]. A multicenter, matched case-control study conducted in the United States showed that 85.5% of hospital-acquired VTE in critically ill children was limb deep venous thrombosis, which was often associated with central venous catheterization [26]. Consistently, in the present study, we found the most prevalent site of VTE in pediatric patients was DVT in the extremities.
As for risk factors for VTE, our results showed that age, weight, shock, sepsis, cancer and vasopressor receipt were statistically significant risk factors in univariate analysis, while shock and sepsis were statistically significant in multivariable logistic regression analysis. In a large prospective cohort study of 2,305,380 adults who underwent surgical procedures between 2005 and 2012 at 374 United States hospitals of all types, patients with sepsis were three times more likely to have postoperative arterial or venous thrombosis than other patients during all surgical procedures [27]. A 2023 meta-analysis similarly identified infection and sepsis as risk factors for thrombosis in pediatric patients [23]. Shock was also confirmed a risk factor for VTE by previous studies. Manohar et al. [28] reported circulatory shock as the predominant risk factor for catheter-related internal jugular vein thrombosis, and this could be attributed to the potential reduction in the bioavailability and efficacy of subcutaneously administered low molecular weight heparin during shock [29]. Multiple studies have explored the risk factors for VTE, and CVC has been proved the most important risk factor for pediatric VTE [16, 23]. The reported incidence of CVC-associated thrombosis in pediatric patients varied from 1.03 to 9.3% [30,31,32,33]. Furthermore, two meta-analyses yielded pooled odds ratios (ORs) for CVC-associated thrombosis: 3.66 (95% CI: 1.78–7.51) and 2.12 (95% CI: 2.00–2.25), respectively [23, 34]. However, as the PIC database does not provide relevant information regarding the use of CVC in pediatric patients, we were unable to assess the frequency of CVC-associated thrombosis in pediatric patients in our study.
VTE in children significantly increases clinical morbidity and mortality [35, 36]. In our study, we analyzed the association between VTE and mortality in children and, probably due to the small sample size, no significant association was found (Table 1). Although the reported specific mortality of VTE in children may be low, the relatively high all-cause mortality highlights the severity of the underlying diseases in children with VTE, so it is important to identify risk factors for VTE in hospitalized children.
Limitation
The limitations of this study stem from the inherent characteristics of the administrative discharge database, which is dependent on coding and billing, occasionally resulting in limited granularity and missing data. With the presence of a CVC being the highest risk for thrombosis in children, as the PIC database does not provide relevant information regarding the use of CVC in pediatric patients, we were unable to assess the frequency of CVC-associated thrombosis in pediatric patients in our study. Employing BMI for evaluating the risk of thrombosis in children is considered more scientifically rigorous. However, due to missing height data for over 30% of pediatric patients in the PIC database, we were unable to calculate BMI and assess its association with VTE risk in this population. Variables such as the use of anticoagulants or antithrombotic agents, as well as the diagnosis of underlying disorders of hemostasis/thrombosis, are of significant interest to the pediatric critical care community. Nevertheless, obtaining these variables from the PIC database presents challenges. Consequently, we are unable to incorporate them into our analysis. The study is constrained by its dependence on ICD-10 codes for outcome identification. While we capture VTEs that are formally “diagnosed” through ICD-10 coding, the actual prevalence of VTEs, encompassing undiagnosed and uncoded cases, remains unknown and cannot be estimated. Additionally, this study is a single-center investigation, and there are limitations in extrapolating the findings to other hospitals.
Conclusions
In conclusion, this analysis of diagnosed VTE in a children’s hospital in China revealed a prevalence of 0.19% among pediatric patients. The most common location for venous thrombi was DVT in the extremities. We identified that shock and sepsis were statistically significant factors associated with pediatric VTE.
Data availability
Data available on request from the authors.
Abbreviations
- VTE:
-
venous thromboembolism
- PIC:
-
Pediatric Intensive Care
- SQL:
-
Structured Query Language
- DVT:
-
deep venous thrombosis
- PE:
-
pulmonary embolism
- CHD:
-
congenital heart disease
- TPN:
-
total parenteral nutrition
- OR:
-
odds ratio
- PHIS:
-
Pediatric Health Information System
- NICU:
-
neonatal intensive care unit
- CVCs:
-
central venous catheters
References
Chalmers E, Ganesen V, Liesner R, Maroo S, Nokes T, Saunders D, Williams M. British Committee for Standards in H: Guideline on the investigation, management and prevention of venous thrombosis in children. Br J Haematol. 2011;154:196–207.
Andrew M, David M, Adams M, Ali K, Anderson R, Barnard D, Bernstein M, Brisson L, Cairney B, DeSai D, et al. Venous thromboembolic complications (VTE) in children: first analyses of the Canadian Registry of VTE. Blood. 1994;83:1251–7.
van Ommen CH, Heijboer H, Buller HR, Hirasing RA, Heijmans HS, Peters M. Venous thromboembolism in childhood: a prospective two-year registry in the Netherlands. J Pediatr. 2001;139:676–81.
C BGE, B-M P, Henderson DLR. Thromboembolism in childhood: a prospective two-year BPSU study in the United Kingdom. Br J Haematol. 2004;125Suppl:1:1–72.
Setty BA, O’Brien SH, Kerlin BA. Pediatric venous thromboembolism in the United States: a tertiary care complication of chronic diseases. Pediatr Blood Cancer. 2012;59:258–64.
Wright JM, Watts RG. Venous thromboembolism in pediatric patients: epidemiologic data from a pediatric tertiary care center in Alabama. J Pediatr Hematol Oncol. 2011;33:261–4.
Raffini L, Huang YS, Witmer C, Feudtner C. Dramatic increase in venous thromboembolism in children’s hospitals in the United States from 2001 to 2007. Pediatrics. 2009;124:1001–8.
van Ommen CH, Nowak-Gottl U. Inherited Thrombophilia in Pediatric venous thromboembolic disease: why and who to test. Front Pediatr. 2017;5:50.
Panagopoulos D, Karydakis P, Noutsos G, Themistocleous M. Venous thromboembolism risk and Thromboprophylaxis in Pediatric Neurosurgery and spinal Injury: current trends and Literature Review. Semin Thromb Hemost. 2022;48:318–22.
Cheuk BL, Cheung GC, Cheng SW. Epidemiology of venous thromboembolism in a Chinese population. Br J Surg. 2004;91:424–8.
Stein PD, Kayali F, Olson RE, Milford CE. Pulmonary thromboembolism in Asians/Pacific Islanders in the United States: analysis of data from the National Hospital Discharge Survey and the United States Bureau of the Census. Am J Med. 2004;116:435–42.
Barbar S, Noventa F, Rossetto V, Ferrari A, Brandolin B, Perlati M, De Bon E, Tormene D, Pagnan A, Prandoni P. A risk assessment model for the identification of hospitalized medical patients at risk for venous thromboembolism: the Padua Prediction score. J Thromb Haemost. 2010;8:2450–7.
Wells PS, Hirsh J, Anderson DR, Lensing AW, Foster G, Kearon C, Weitz J, D’Ovidio R, Cogo A, Prandoni P, et al. A simple clinical model for the diagnosis of deep-vein thrombosis combined with impedance plethysmography: potential for an improvement in the diagnostic process. J Intern Med. 1998;243:15–23.
Caprini JA. Thrombosis risk assessment as a guide to quality patient care. Dis Mon. 2005;51:70–8.
Zeng X, Yu G, Lu Y, Tan L, Wu X, Shi S, Duan H, Shu Q, Li H. PIC, a paediatric-specific intensive care database. Sci Data. 2020;7:14.
Kim SJ, Sabharwal S. Risk factors for venous thromboembolism in hospitalized children and adolescents: a systemic review and pooled analysis. J Pediatr Orthop B. 2014;23:389–93.
Spentzouris G, Scriven RJ, Lee TK, Labropoulos N. Pediatric venous thromboembolism in relation to adults. J Vasc Surg. 2012;55:1785–93.
Meissner MH, Wakefield TW, Ascher E, Caprini JA, Comerota AJ, Eklof B, Gillespie DL, Greenfield LJ, He AR, Henke PK, et al. Acute venous disease: venous thrombosis and venous trauma. J Vasc Surg. 2007;46(Suppl S):S25–53.
Mahajerin A, Croteau SE. Epidemiology and Risk Assessment of Pediatric venous thromboembolism. Front Pediatr. 2017;5:68.
El-Naggar W, Yoon EW, McMillan D, Afifi J, Mitra S, Singh B, da Silva O, Lee SK, Shah PS. Canadian neonatal network I: epidemiology of thrombosis in Canadian neonatal intensive care units. J Perinatol. 2020;40:1083–90.
Bhatia K, Solanki S, Paes B, Chan AKC, Bhatt MD. Risk factors for neonatal thrombosis: a retrospective study conducted in a single Canadian intensive care unit. Pediatr Blood Cancer. 2022;69:e29668.
Robinson V, Achey MA, Nag UP, Reed CR, Pahl KS, Greenberg RG, Clark RH, Tracy ET. Thrombosis in infants in the neonatal intensive care unit: analysis of a large national database. J Thromb Haemost. 2021;19:400–7.
Song S, Li Z, Zhao G, Li X, Wang R, Li B, Liu Q. Epidemiology and risk factors for thrombosis in children and newborns: systematic evaluation and meta-analysis. BMC Pediatr. 2023;23:292.
Easterlin MC, Li Y, Yieh L, Gong CL, Jaffray J, Hall M, Friedlich PS, Lakshmanan A. Predictors of venous thromboembolism among infants in children’s hospitals in the United States: a retrospective Pediatric Health Information Study. J Perinatol. 2022;42:103–9.
Demirel N, Aydin M, Zenciroglu A, Bas AY, Yarali N, Okumus N, Cinar G, Ipek MS. Neonatal thrombo-embolism: risk factors, clinical features and outcome. Ann Trop Paediatr. 2009;29:271–9.
Sochet AA, Jaffray J, Branchford BR, Havlicek EE, Mosha M, Amankwah EK, Ignjatovic V, Faustino EVS, Goldenberg NA. Hospital-Acquired Venous Thromboembolism and Invasive Mechanical Ventilation: A Report From the Children’s Hospital Acquired Thrombosis Consortium. Pediatr Crit Care Med 2023.
Donze JD, Ridker PM, Finlayson SR, Bates DW. Impact of sepsis on risk of postoperative arterial and venous thromboses: large prospective cohort study. BMJ. 2014;349:g5334.
Nm Bhat M, Venkataraman R, Ramakrishnan N, B KA, Rajagopalan S. Value of Routine Sonographic Screening of Internal Jugular Vein to detect catheter related thrombosis in Intensive Care Unit. Indian J Crit Care Med. 2019;23:326–8.
Fries D. Thrombosis prophylaxis in critically ill patients. Wien Med Wochenschr. 2011;161:68–72.
Onyeama SN, Hanson SJ, Dasgupta M, Baker K, Simpson PM, Punzalan RC. Central venous catheter-associated venous thromboembolism in children with hematologic malignancy. J Pediatr Hematol Oncol. 2018;40:e519–24.
Steen EH, Lasa JJ, Nguyen TC, Keswani SG, Checchia PA, Anders MM. Central venous catheter-related deep vein thrombosis in the Pediatric Cardiac Intensive Care Unit. J Surg Res. 2019;241:149–59.
Dubois J, Rypens F, Garel L, David M, Lacroix J, Gauvin F. Incidence of deep vein thrombosis related to peripherally inserted central catheters in children and adolescents. CMAJ. 2007;177:1185–90.
Tran M, Shein SL, Ji X, Ahuja SP. Identification of a VTE-rich population in pediatrics - critically ill children with central venous catheters. Thromb Res. 2018;161:73–7.
Mahajerin A, Branchford BR, Amankwah EK, Raffini L, Chalmers E, van Ommen CH, Goldenberg NA. Hospital-associated venous thromboembolism in pediatrics: a systematic review and meta-analysis of risk factors and risk-assessment models. Haematologica. 2015;100:1045–50.
Sochet AA, Kiskaddon A, Betensky M, Goldenberg N. Venous thromboembolism among critically Ill children: a narrative review. Semin Thromb Hemost. 2021;47:631–42.
Hauser BM, Hoffman SE, Gupta S, Zaki MM, Xu E, Chua M, Bernstock JD, Khawaja A, Smith TR, Proctor MR, Zaidi HA. Association of venous thromboembolism following pediatric traumatic spinal injuries with injury severity and longer hospital stays. J Neurosurg Spine. 2022;36:153–9.
Acknowledgements
Not applicable
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
Conception and design of study: JTZ and JHZ; acquisition of data: YTZ, YL and PGN; analysis and interpretation of data: JTZ and YTZ; drafting the manuscript: JTZ, YTZ and PGN; revising the manuscript critically for important intellectual content: HJC and JHZ. All authors approved the version of the manuscript to be published.
Corresponding author
Ethics declarations
Ethical approval
Ethical approval has not been sought for this work. The present survey did not investigate and analyze human samples for pathophysiology, genetics, and other medical purposes.
Competing interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zhou, J., Zhu, Y., Liu, Y. et al. Risk factors for venous thromboembolism in a single pediatric intensive care unit in China. Thrombosis J 22, 26 (2024). https://doi.org/10.1186/s12959-024-00596-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12959-024-00596-6