Abstract
Background
According to several studies, ROS1 rearrangement is associated with thrombotic risk in non-small cell lung cancer (NSCLC). However, there is no clear understanding of the predictors and prognostic impact of thromboembolic events (TEEs) in patients with advanced ROS1 rearrangement NSCLC.
Methods
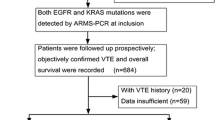
A total of 47 newly diagnosed advanced NSCLC patients with ROS1 rearrangement from four Chinese hospitals were retrospectively included and were evaluated for TEEs incidence, characteristics, predictors, as well as response to therapies and overall survival (OS).
Results
Of the 47 enrolled patients, 23.4% (n = 11) patients developed TEEs. Among them, 7 of 11 patients (64%) developed pulmonary embolism (PE), and 5 patients (45%) experienced recurrent TEEs. In multivariate analysis, D-dimer was associated with the occurrence of TEEs in ROS1 rearranged NSCLC (HR 1.16, 95% CI 1.08–1.23, P < 0.001). Median progression-free survival (PFS) after first-line ROS1 tyrosine kinase inhibitors (TKIs) therapy was significantly longer in patients without TEEs than in those developing TEEs (26 months vs. 12 months, P = 0.0383). Furthermore, patients with TEEs had a shorter OS period than those without TEEs (29.8 months vs. not estimable, P = 0.0647).
Conclusion
The results of this multicenter study indicated that advanced NSCLC patients with ROS1 rearrangement were more likely to experience PE and TEEs recurrence. And patients with TEEs tended to have a worse prognosis. Furthermore, an elevated D-dimer level suggested a hypercoagulable state in NSCLC patients with ROS1 rearrangement.
Similar content being viewed by others
Background
Thromboembolic events (TEEs) are common complications in patients with non-small cell lung cancer (NSCLC), with an incidence rate between 10 and 15% [1, 2]. Considerable evidence indicates that thrombotic complications are associated with a worse prognosis and are the second most frequent cause of death in cancer patients [3,4,5].
Molecular testing has become a standard procedure among patients with NSCLC. Previous research proved that specific mutations including epidermal growth factor receptor (EGFR) mutations and anaplastic lymphoma kinase (ALK) rearrangement played a role in thrombotic risk in NSCLC [6, 7].
Also, ROS1 rearrangement exhibited biological homology with ALK rearrangement [8], and a number of case-control and cohort studies demonstrated that ROS1 rearrangement was associated with TEEs in NSCLCs as well [9,10,11,12]. The prevalence of ROS1 rearrangement is reported to be less than 2% in NSCLC among Caucasian populations and is slightly higher in the East Asian populations with a prevalence of 2–3% [13]. Currently, the treatment status in China differs from that in developed countries. Since crizotinib was approved in China for ROS1-rearranged NSCLC in 2017 [14], chemotherapy was mainly adopted before 2017 among these patients. Meanwhile, little is known about the clinical relevance and characteristics of ROS1 rearrangement in Chinese NSCLC patients. The primary objective of the present multicenter study was to investigate the incidence and risk factors of TEEs in ROS1 rearrangement with newly diagnosed NSCLC in China. The secondary objective was to explore the treatment response and survival among ROS1 rearrangement NSCLC patients with TEEs and without TEEs.
Material and methods
Study populations
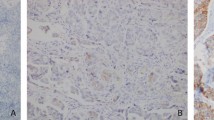
The ROS1-rearranged advanced NSCLC cohort included patients attending four Chinese hospitals from March 2015 to March 2021. The retrospective observational cohort included patients who met the following inclusion criteria: histological confirmation of the diagnosis; ROS1 rearrangement determined by fluorescence in situ hybridization (FISH), immunohistochemistry (IHC), reverse transcription-polymerase chain reaction (RT-PCR), or next generation sequencing (NGS). The exclusion criteria were as follows: any surgery, chemotherapy, or radiotherapy within 3 months before diagnosis; insufficient available clinical data and uncooperative follow-up. This study was approved by the central Ethics Committee of Beijing Chao-Yang Hospital, Capital Medical University, Beijing, China (No.2021-KE-443).
Outcome measurement
In this study, the primary outcome is the occurrence of TEEs, including arterial thromboembolism (ATE) and venous thromboembolism (VTE). The incidence of TEEs was estimated 3 months before diagnosis and 6 months after diagnosis, and the final follow-up date was September 2021.
Routine screening for TEEs was not conducted, and symptomatic or incidental TEEs were confirmed by objective imaging methods. VTE includes deep vein thrombosis (DVT) and pulmonary embolism (PE). Objective evidence for the diagnosis of DVT included venous ultrasound imaging or computed tomography (CT) angiography. And the objective evidence for the diagnosis of PE included CT pulmonary angiogram or ventilation-perfusion scan. ATE was defined as a composite of acute myocardial infarction, peripheral arterial occlusion, and stroke. To confirm the stroke diagnosis, CT or magnetic resonance imaging (MRI) was performed. The diagnosis of peripheral arterial occlusion was confirmed by the use of doppler-sonography, digital subtraction angiography, CT-angiography, and MRI-angiography. The diagnosis of myocardial infarction was confirmed by the use of echocardiography, angiography or cardiac biomarkers.
Data collection
Patient-related factors (age, sex, performance status, smoking history, and medical records), tumor-related factors (tumor histology, tumor stage, oncogenic status, occurrence time of TEEs, patients’ situation of TEEs and the location of TEEs), treatment-related factors (anti-tumor therapy and anticoagulant therapy) and baseline laboratory variables (complete blood count, serum carcinoembryonic antigen (CEA), lactate dehydrogenase (LDH), C-reactive protein (CRP) and D-dimer) were extracted from the patients’ electronic clinical records and collected from patients themselves via telephone follow-up.
In addition, we used the Charlson Comorbidity Index (CCI) to measure the burden of comorbidity. According to the calculated CCI scores, we categorized all patients into three groups: low (no comorbidity): CCI score of 0, medium: CCI score of 1–2, or high: CCI score of 3 or more.
Statistical analysis
Continuous variables were described by using median and range, and transformed into categorical variables by defining the best cut-offs using the maximum selection test method. Categorical variables were described as frequencies and percentages.
The cumulative incidence of TEEs was estimated using competing risk analysis, treating death as a competing event. And Grey’s test and Fine and Gray competing regression, with death as a competing risk, were conducted to identify the risk factors associated with TEEs. A value of P < 0.05 was considered statistically significant.
Progression-free survival (PFS) and overall survival (OS) were estimated by Kaplan-Meier (KM) method and were defined as NSCLC diagnosis to disease progression and death by any cause. The response was reported by the treating clinician according to the Response Evaluation Criteria In Solid Tumors version 1.1 (RECIST 1.1).
R statistical software version 4.1.0 was used to perform the maximum selection test and Fine and Gray competing regression analysis. Grey’s test analyses were performed using NCSS 12. Statistical analysis was performed using SPSS version 21.0. This study was reviewed by a professional epidemiologist.
Results
Patient characteristics
A total of 47 patients diagnosed with ROS1-rearranged NSCLC from four hospitals in Northern China were included in the study. The 47 patients had a mean age of 54.38 years (SD, 11.57) at diagnosis; 57% (27 of 47) of patients were female. A majority of the patients had a performance status (PS) of 0 to 1 (36 of 47, 77%), and 68% (32 of 47) of the patients were non-smokers. Our analysis of the medical records of the patients revealed that 25% (12 of 47) of the patients had a low CCI score, 53% (25 of 47) had a medium CCI score, and 21% (10 of 47) had a high CCI score.
And we also evaluated the tumor characteristics of the cohort. The population consisted of 47 patients with adenocarcinoma (46 of 47, 98%) and 1 patient with adenosquamous carcinoma (1 of 47, 2%). All patients had advanced disease stages at diagnosis, of which 70% (33 of 47) of patients had at least 2 sites of metastases, and 30% (14 of 47) of patients had 3 and more sites of metastases. Furthermore, 39 patients (39 of 47, 85%) had distant metastases; 6 had brain metastases, 22 had pleural metastases, and 13 had bone metastases (Table 1).
Development and recurrence of thromboembolic events
Of the NSCLC patients with ROS1 rearrangement, 11 (11 of 47, 23.4%) of 47 patients developed TEEs within 3 months prior to and 6 months after diagnosis. TEEs consisted of 9 VTE events (9 of 11, 72%) and 2 ATE combined VTE events (2 of 11, 28%). As for the VTE group, 4 patients had only DVT or only PE (4 of 9, 44%), while 5 had both DVT and PE (5 of 9, 56%). Meanwhile, among the entire TEEs group, 2 patients (2 of 11, 18%) developed both ATE and VTE. Overall, 7 patients (7 of 11, 64%) developed PE during follow-up. The majority of the patients developed TEEs symptomatically (10 of 11, 91%).
In the investigation of the TEEs occurrence, there were 5 ambulatory patients (5 of 11, 45%) and 6 hospitalized patients (6 of 11, 55%). Most of the TEEs (7 of 11, 64%) developed before treatment, and TEEs occurred at disease progression in 18% of cases. There were 4 patients (4 of 11, 36%) who developed TEEs during anti-tumor therapy. Almost half of the patients (5 of 11, 45%) suffered recurrent TEEs, and all the relapses happened under therapeutic anticoagulation, of which 4 patients took low molecular weight heparin (LMWH). Among the patients with TEEs recurrence, 4 patients (4 of 11, 36%) received chemotherapy while 6 patients (6 of 11, 55%) received ROS1 TKIs. More than half of the patients (3 of 4, 75%) in the chemotherapy group presented TEEs relapse and the recurrence rate in the ROS1 TKIs group was 33% (1 of 3), which showed a significant difference between these two therapies (Pearson Chi-Square 10.0, P = 0.005).
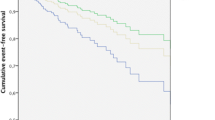
The clinical characteristics of TEEs were listed in Table 2, and the cumulative incidence of TEEs by Fine and Gray competing-risks regression with death as a competing risk was illustrated in Fig. 1.
Risk factors of TEEs in ROS1 rearranged NSCLC
For numeric variables in this cohort, laboratory parameters were categorized based on the best cut-offs determined by the maximum selection test. Prognostic factors and biomarkers were identified in univariate analysis. Additionally, the following variables were significantly associated with symptomatic or incidental TEEs occurrence in ROS1 rearranged NSCLC: (1) LDH > 312 U/L (P = 0.003); (2) D-dimer > 7.8μg/ml (P = 0.02) (Table 3).
In multivariate analysis, we selected the top three strongest predictors in univariate analysis (LDH, D-dimer, and CRP), and incorporated them into multivariate analysis. The results showed that a high level of D-dimer was of significant association with increased thrombotic risk in ROS1 rearranged NSCLC patients (HR 1.16, 95% CI 1.08–1.23, P < 0.001) (Table 3).
Response and survival
According to different treatments, 19 patients (19 of 72, 26%) received chemotherapy, 37 patients (37 of 72, 51%) were treated with ROS1 TKIs, and 16 patients (16 of 72, 22%) received other treatments (such as radiotherapy, palliative surgery, immune checkpoint therapy, and traditional Chinese medicine therapy). And among patients taking ROS1 TKIs at any line, 24 patients (24 of 37, 65%) adopted it as first-line therapy, while 13 patients (13 of 37, 35%) adopted it as second/third-line therapy (Table 1). Of 11 patients with TEEs, 6 patients (6 of 11, 55%) received ROS1 TKIs at any line therapy.
Moreover, at a median follow-up of 28.4 months, we evaluated the association between TEEs, PFS, and OS using KM analysis. In the 37 patients treated with ROS1 TKIs at first-line, patients with TEEs had significantly shorter PFS than patients without TEEs (12 vs. 26 months, P = 0.0383) (Fig. 2A). In the 47 ROS1 rearranged NSCLC patients, 5 of 11 (45%) and 8 of 36 (22%) died in the TE and non-TE cohorts. The median OS was 29.8 months with at least one TEE, whereas this was not reached in the group without TEEs (29.8 months vs. not estimable, P = 0.0647). According to the KM curve, the OS probability in patients with and without TEEs was 63% vs. 87% at 24 months, and was 42% vs. 69% at 48 months (Fig. 2B).
Additionally, we also evaluated the response to ROS1 TKIs in different lines of therapy among patients with ROS1 rearranged NSCLC. Patients treated with ROS1 TKIs at first-line (n = 24) showed a better response to TKIs than those at second/third-line (n = 13). The median PFS for the patients receiving ROS1 TKIs at first line treatment was 24 months whereas second/third line treatment was 12 months (24 vs. 12 months, P = 0.0446).
Discussion
Previous studies on ROS1-rearranged NSCLC mostly came from white patients.. Although the prevalence of ROS1-rearrangement was higher in East Asia and the therapy regimens were limited in China, the results of this Chinese multicentre observational study showed that the presence of ROS1 rearranged in NSCLC may increase the risk of TEEs. This study also investigated the risk factors for TEEs among ROS1-rearranged NSCLC, and analyzed the different responses to ROS1 TKIs and OS between TEEs and without TEEs group.
The incidence of TEEs was relatively lower in this population than in patients from previous studies (Table 4). Since ROS1 rearrangement is a rare variation, the sample size of these studies was relatively small. Meanwhile, the observation periods were different in these studies. TEEs were estimated between 3 months prior to and 6 months after the NSCLC diagnosis since the TEEs during this period were more relevant to cancer.
Notably, more than half of the TEEs cohort experienced PE, many times the incidence (2–4%) in the general cohort [15, 16]. The high incidence of PE indicated that the patients with ROS1 rearranged NSCLC were in a hypercoagulable state, and whether or not to undertake thromboprophylaxis needs careful consideration. Meanwhile, TEEs occurred at time points across the patients’ disease course, including pre and post-treatment and throughout the disease course. In the TEEs cohort, most of the patients developed TEEs before treatment. As in previous studies, suspicion of underlying cancer is frequently raised in patients with TEEs [17].
Furthermore, half of the patients in the TEEs cohort experienced TEEs recurrence, which was 1.8-fold higher than the general cancer populations [18]. And all of them were during anticoagulant treatment. Meanwhile, these patients experienced TEEs relapse within 6 months of their first occurrence, which caused us to focus on anticoagulant treatment in the first 6 months after the first occurrence of TEEs in ROS1-rearranged NSCLC patients. Previous studies showed that chemotherapy was a clinical risk factor for TEEs occurrence [19], and our results showed that chemotherapy was a risk factor for TEEs recurrence as well.
In the univariate analysis, our study found that LDH and D-dimer may be relevant to TEEs occurrence in ROS1 rearranged NSCLC. And the Fine and Gray test showed that elevated D-dimer may be related to the risk of TEEs. The increased TEEs risk among these patients indicated that ROS1 rearranged patients were at a hypercoagulable state. And D-dimer can reflect the activation of the hemostatic system, which demonstrated that a high-level D-dimer might associate with thrombosis [10, 20]. Repeat assessment indicated that D-dimer has a considerable TEEs predictive capacity among cancer patients [20,21,22]. This study suggested that oncogenic status was closely associated with the hypercoagulable profile including ROS1 rearrangement.
Patients with ROS1 rearrangement were treated with ROS1 TKIs as preferred, such as crizotinib in the first-line, and ceritinib after progression. Kaplan-Meier survival analysis showed that among patients receiving ROS1 TKIs in the first-line therapy (23 of 46, 50%), patients without TEEs had better median PFS than those with TEEs patients, which was consistent with previous studies [23]. The OS among patients with TEEs tended to be shorter than those without TEEs. Nevertheless, there was no statistical significance.
Our study had some limitations. First, due to the retrospective nature of the cohort, there was recall bias in our study. Although we included multicenter data, the sample size was relatively small, because ROS1 rearrangement was a rare variation. And the regression analysis without correction for multiple comparisons could influence the stability of the results. These results must be further validated by a large-scale prospective study. Finally, the lack of TEEs screening in our study may result in the underestimation of the incidence of TEEs among the enrolled patients since asymptomatic TEEs may be missed.
Conclusion
Our study was a Chinese multicenter study that reported a high incidence rate of TEEs occurrence and TEEs recurrence in patients diagnosed with ROS1 rearranged advanced NSCLC. A high level D-dimer suggested that ROS1 rearranged NSCLC patients were at a hypercoagulable state, and chemotherapy tended to be the risk factor for TEEs recurrence. And the response to ROS1 TKIs was greater in patients without TEEs. Further large-scale prospective studies are needed to confirm these findings.
Availability of data and materials
Data were collected from all the patients. The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- NSCLC:
-
Non-small cell lung cancer
- TEE:
-
Thromboembolic event
- OS:
-
Overall survival
- PE:
-
Pulmonary embolism
- PFS:
-
Progression free survival
- TKI:
-
Tyrosine kinase inhibitor
- EGFR:
-
Epidermal growth factor receptor
- ALK:
-
Anaplastic lymphoma kinase
- FISH:
-
Fluorescence in situ hybridization
- IHC:
-
Immunohistochemistry
- RT-PCR:
-
Reverse transcription-polymerase chain reaction
- NGS:
-
Next generation sequencing
- ATE:
-
Arterial thromboembolism
- VTE:
-
Venous thromboembolism
- DVT:
-
Deep vein thrombosis
- CT:
-
Computed tomography
- MRI:
-
Magnetic resonance imaging
- CEA:
-
Carcinoembryonic antigen
- LDH:
-
Lactate dehydrogenase
- CRP:
-
C-reactive protein
- CCI:
-
Charlson Comorbidity Index
- KM:
-
Kaplan Meier
- RECIST 1.1:
-
Response Evaluation Criteria In Solid Tumors version 1.1
- PS:
-
Performance status
- LMWH:
-
Low molecular weight heparin
References
Tagalakis V, Levi D, Agulnik JS, Cohen V, Kasymjanova G, Small D. High risk of deep vein thrombosis in patients with non-small cell lung cancer: a cohort study of 493 patients. J Thorac Oncol. 2007;2(8):729–34. https://doi.org/10.1097/JTO.0b013e31811ea275.
Blom JW, Doggen CJ, Osanto S, Rosendaal FR. Malignancies, prothrombotic mutations, and the risk of venous thrombosis. JAMA. 2005;293(6):715–22. https://doi.org/10.1001/jama.293.6.715.
Zugazagoitia J, Biosca M, Oliveira J, Olmedo ME, Dómine M, Nadal E, et al. Incidence, predictors and prognostic significance of thromboembolic disease in patients with advanced ALK-rearranged non-small cell lung cancer. Eur Respir J. 2018;51(5). https://doi.org/10.1183/13993003.02431-2017.
Connolly GC, Dalal M, Lin J, Khorana AA. Incidence and predictors of venous thromboembolism (VTE) among ambulatory patients with lung cancer. Lung Cancer. 2012;78(3):253–8. https://doi.org/10.1016/j.lungcan.2012.09.007.
Chew HK, Wun T, Harvey D, Zhou H, White RH. Incidence of venous thromboembolism and its effect on survival among patients with common cancers. Arch Intern Med. 2006;166(4):458–64. https://doi.org/10.1001/archinte.166.4.458.
Dou F, Li H, Zhu M, Liang L, Zhang Y, Yi J, et al. Association between oncogenic status and risk of venous thromboembolism in patients with non-small cell lung cancer. Respir Res. 2018;19:88. https://doi.org/10.1186/s12931-018-0791-2.
Al-Samkari H, Leiva O, Dagogo-Jack I, Shaw A, Lennerz J, Iafrate AJ, et al. Impact of ALK rearrangement on venous and arterial thrombotic risk in NSCLC. J Thorac Oncol. 2020;15(9):1497–506. https://doi.org/10.1016/j.jtho.2020.04.033.
Barlesi F, Mazieres J, Merlio JP, Debieuvre D, Mosser J, Lena H, et al. Routine molecular profiling of patients with advanced non-small-cell lung cancer: results of a 1-year nationwide programme of the French cooperative thoracic intergroup (IFCT). Lancet. 2016;387(10026):1415–26. https://doi.org/10.1016/S0140-6736(16)00004-0.
Ng TL, Smith DE, Mushtaq R, Patil T, Dimou A, Yang S, et al. ROS1 gene rearrangements are associated with an elevated risk of Peridiagnosis thromboembolic events. J Thorac Oncol. 2019;14(4):596–605. https://doi.org/10.1016/j.jtho.2018.12.001.
Chiari R, Ricciuti B, Landi L, Morelli AM, Delmonte A, Spitaleri G, et al. ROS1-rearranged non-small-cell lung Cancer is associated with a high rate of venous thromboembolism: analysis from a phase II, prospective, multicenter, two-arms trial (METROS). Clin Lung Cancer. 2020;21(1):15–20. https://doi.org/10.1016/j.cllc.2019.06.012.
Alexander M, Pavlakis N, John T, O'Connell R, Kao S, Hughes B, et al. A multicenter study of thromboembolic events among patients diagnosed with ROS1-rearranged non-small cell lung cancer. Lung Cancer. 2020;142:34–40. https://doi.org/10.1016/j.lungcan.2020.01.017.
Muñoz-Unceta N, Zugazagoitia J, Manzano A, Jiménez-Aguilar E, Olmedo ME, Cacho JD, et al. High risk of thrombosis in patients with advanced lung cancer harboring rearrangements in ROS1. Eur J Cancer. 2020;141:193–8. https://doi.org/10.1016/j.ejca.2020.10.002.
Kohno T, Nakaoku T, Tsuta K, Tsuchihara K, Matsumoto S, Yoh K, et al. Beyond ALK-RET, ROS1 and other oncogene fusions in lung cancer. Transl Lung Cancer Res. 2015;4:156–64. https://doi.org/10.3978/j.issn.2218-6751.2014.11.11.
Liu C, Yu H, Chang J, Chen H, Li Y, Zhao W, et al. Crizotinib in Chinese patients with ROS1-rearranged advanced non–Small-cell lung Cancer in routine clinical practice. Target Oncol. 2019;14:315–23. https://doi.org/10.1007/s11523-019-00636-6.
Sun JM, Kim TS, Lee J, Park YH, Ahn JS, Kim H, et al. Unsuspected pulmonary emboli in lung cancer patients: the impact on survival and the significance of anticoagulation therapy. Lung Cancer. 2010;69(3):330–6. https://doi.org/10.1016/j.lungcan.2009.11.015.
Malgor RD, Bilfinger TV, Labropoulos N. A systematic review of pulmonary embolism in patients with lung cancer. Ann Thorac Surg. 2012;94(1):311–6. https://doi.org/10.1016/j.athoracsur.2012.03.025.
van Es N, Ay C, Jara-Palomares L. Screening for occult Cancer in patients with venous thromboembolism: past, present, and future. Hamostaseologie. 2020;40(3):270–9. https://doi.org/10.1055/a-1150-2286.
Piran S, Schulman S. Management of recurrent venous thromboembolism in patients with cancer: a review. Thromb Res. 2018;164(Suppl 1):S172–172S177. https://doi.org/10.1016/j.thromres.2017.12.019.
Khorana AA, Connolly GC. Assessing risk of venous thromboembolism in the patient with cancer. J Clin Oncol. 2009;27(29):4839–47. https://doi.org/10.1200/JCO.2009.22.3271.
Ay C, Dunkler D, Marosi C, Chiriac AL, Vormittag R, Simanek R, et al. Prediction of venous thromboembolism in cancer patients. Blood. 2010;116(24):5377–82. https://doi.org/10.1182/blood-2010-02-270116.
Alexander M, Ball D, Solomon B, MacManus M, Manser R, Riedel B, et al. Dynamic thromboembolic risk modelling to target appropriate preventative strategies for patients with non-Small cell lung Cancer. Cancers (Basel). 2019;11(1). https://doi.org/10.3390/cancers11010050.
Pabinger I, van Es N, Heinze G, Posch F, Riedl J, Reitter EM, et al. A clinical prediction model for cancer-associated venous thromboembolism: a development and validation study in two independent prospective cohorts. Lancet Haematol. 2018;5(7):e289–289e298. https://doi.org/10.1016/S2352-3026(18)30063-2.
Liu Y, Wang W, Wu F, Gao G, Xu J, Li X, et al. High discrepancy in thrombotic events in non-small cell lung cancer patients with different genomic alterations. Transl Lung Cancer Res. 2021;10(3):1512–24. https://doi.org/10.21037/tlcr-20-1290.
Acknowledgements
We would like to thank Dr. Lin Hua for her technical assistance with the statistical analysis as well as her useful recommendations and discussions.
Funding
This study was supported by the National Natural Science Foundation of China (grant no. 31770961), Beijing Cancer Prevention and Treatment Research Association (no. CAPTRALung2019002), and CAMS Innovation Fund for Medical Sciences (CIFMS) (grant no. 2021–1-I2M-023).
Author information
Authors and Affiliations
Contributions
JWY was responsible for data collection, statistical analyses and manuscript writing. HC was responsible for data collection and manuscript writing. JL was responsible for statistical analyses. XRJ was responsible for data collection. YX was responsible for data collection. MZW was responsible for data collecting. ZW was responsible for data collection. ZGZ was responsible for manuscript correction. YHZ was responsible for study design, patient enrollment, statistical analyses, and manuscript correction. YHR was responsible for patient enrollment and manuscript correction. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This study was approved by the central Ethics Committee of Beijing Chao-Yang Hospital, Capital Medical University, Beijing, China (No.2021-KE-443).
Consent for publication
No applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Yi, J., Chen, H., Li, J. et al. The association between ROS1 rearrangement and risk of thromboembolic events in patients with advanced non-small cell lung cancer: a multicenter study in China. Thrombosis J 20, 56 (2022). https://doi.org/10.1186/s12959-022-00417-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12959-022-00417-8