Abstract
Background
For patients with suspected pulmonary embolism (PE), age- or clinically-adjusted D-dimer threshold level can be used to define a negative test that safely excludes PE and reduces the use of imaging. However, the utility of this approach in patients hospitalized for chronic obstructive pulmonary disease (COPD) exacerbation is undefined.
Methods
We ran an analysis of the patients hospitalized for COPD exacerbation and randomized to the intervention in the SLICE trial. Using the conventional strategy as the reference, we compared the proportion of patients with a negative D-dimer result, and the negative predictive value and sensitivity of three D-dimer threshold strategies for initial PE or subsequent diagnosis of venous thromboembolism (VTE): the age-adjusted strategy, the Wells-adjusted strategy, and the YEARS-adjusted strategy.
Results
We included 368 patients. Using a conventional threshold, 182 (49.5%) patients had negative D-dimer values, of whom 1 (0.6%) had PE (sensitivity, 94.1%). The use of an age-adjusted threshold increased the number of patients in whom PE could be excluded from 182 to 233 patients (63.3%), and the proportion of false-negative findings increased from 0.5% to 1.7% (sensitivity, 76.5%). With the use of the Wells or YEARS strategies, 64.4% and 71.5% had negative values, and the proportion of false-negative findings was 2.5% (sensitivity, 64.7%) and 2.7% (sensitivity, 58.8%), respectively.
Conclusions
In patients hospitalized for COPD exacerbation, compared with the conventional strategy, age- or clinically-adjusted strategies of D-dimer interpretation were associated with a larger proportion of patients in whom PE was ruled out with a higher failure rate.
Trial Registration
ClinicalTrials.gov number: NCT02238639.
Similar content being viewed by others
Introduction
D-dimer is the initial diagnostic test for patients with suspected acute symptomatic pulmonary embolism (PE) [1, 2]. In patients with low or intermediate clinical pretest probability, a normal D-dimer test result safely excludes acute PE without the need for imaging testing [3]. In order to increase the clinical usefulness of D-dimer testing (i.e., to reduce the need for computed tomography pulmonary angiography [CTPA]) without missing relevant PE, several strategies for revising the conventional fixed D-dimer threshold have been proposed. These strategies include age-adjusted D-dimer interpretation and clinical probability-adjusted interpretation of D-dimer.
Studies have shown that these strategies can be effective and safe in the exclusion of PE and in the reduction of the risk of false positives when compared to the conventional D-Dimer cutoff strategy. The age-adjusted strategy for D-dimer interpretation uses a progressively higher D-dimer threshold to categorize results as positive in patients over 50 years of age (i.e., use of age multiplied by 10) [4]. A second strategy consists of ruling out PE in patients with a low clinical pretest probability (according to the Wells score) and a D-dimer level of less than 1000 ng/mL, and in those with a moderate clinical pretest probability and a D-dimer level of less than 500 ng/mL [5]. Finally, the YEARS diagnostic algorithm uses twice the D-dimer threshold (i.e., 1000 ng/mL) to exclude PE in patients with no YEARS criteria (clinical signs of deep vein thrombosis [DVT], hemoptysis, and PE as the most likely diagnosis), and a threshold of 500 ng/mL in patients with one or more criteria [6].
Though PE has been reported to be prevalent in patients with exacerbation of chronic obstructive pulmonary disease (COPD) [7,8,9,10], the Significance of Pulmonary Embolism in COPD Exacerbations (SLICE) showed that an active strategy for the diagnosis of PE (D-dimer testing and, if positive, CTPA) did not result in a lower percentage of patients experiencing the composite outcome of venous thromboembolism (VTE), readmission for COPD, or death within 90 days after randomization [11]. In daily practice, however, D-dimer testing is frequently ordered for the initial assessment of the patients presenting with chest symptoms (including those with COPD exacerbations). Such testing is, in many cases, unnecessary.
The objective of this study was to assess the clinical usefulness and diagnostic accuracy of the age-adjusted and clinical probability-adjusted strategies of D-dimer interpretation, compared with the conventional fixed threshold, in a large group of patients hospitalized for exacerbations of COPD.
Methods
We performed post hoc analyses of the recently completed SLICE trial. SLICE was a multicenter, open-label, randomized, clinical trial aimed at evaluating whether an active search for PE might improve clinical outcomes in patients with exacerbations of COPD who required hospital admission. The rationale, design and main results of the SLICE study were described previously [11, 12]. The trial was conducted in 18 academic hospitals across Spain. The institutional review board at each of the participating sites approved the protocol, and each patient provided written informed consent.
Briefly, consecutive patients with exacerbations of COPD who required hospital admission and had no initial clinical suspicion of PE were randomized to either the usual care plus an active search for PE (intervention group) or usual care alone (control group). Patients in the intervention group were investigated with a sequential diagnostic strategy based on D-dimer testing and CTPA. We used the Fibrinogen Equivalent Unit (FEU) to report D-dimer levels based on the molecular weight of fibrinogen. For patients with a negative conventional D-dimer (defined by the department of clinical chemistry at each participating site [Table 4 in the Appendix]), a diagnosis of PE was deemed as ruled out by the treating clinicians. For patients with a positive D-dimer according to the conventional criteria, a CTPA was performed. CTPA results were categorized as positive for PE if an intraluminal filling defect was seen in subsegmental or more proximal branches, and were considered negative if no filling defect was observed. For the present analysis, only patients who were randomized to the intervention were included.
D-dimer interpretation strategy definitions
Age-adjusted strategy
D-dimer results were categorized as negative if the D-dimer level was less than the conventional threshold used at each participating site in patients 50 years or younger or, in patients older than 50 years, if it was less than the patient’s age multiplied by 10 (e.g., less than 650 ng/mL if 65 years; less than 800 ng/mL if 80 years) [4].
Clinical probability-adjusted strategy
According to the seven-item Wells clinical prediction rule [5], D-dimer results were categorized as negative if the D-dimer level was less than 1000 ng/mL in patients with low clinical pretest probability and less than 500 ng/mL for patients with moderate clinical pretest probability.
The YEARS diagnostic algorithm consists of clinical signs of DVT, hemoptysis, and PE as the most likely diagnosis [6]. D-dimer results were categorized as negative if the D-dimer level was less than 1000 ng/mL in patients without any YEARS item and less than 500 ng/mL for patients with one or more of the YEARS items.
Outcome measures
The primary outcome for this analysis was the rate of adjudicated PE events at initial testing, or VTE events within a 3-month follow-up period in patients who did not receive anticoagulant therapy on the basis of negative results on the initial work-up.
A central independent adjudication committee whose members were unaware of management allocation adjudicated all suspected events during the study period.
Statistical analysis
A 2 x 2 table was constructed for each strategy according to whether the D-dimer result in individual patients was categorized as positive or negative, and whether the patient was categorized as VTE-positive or VTE-negative. Estimates of the proportion of all patients who had a negative D-dimer test, sensitivity, specificity, and negative predictive value (NPV) were calculated for all strategies, along with 95% confidence intervals (CI) using the Wilson score method. Using the conventional strategy as the reference, pairwise comparisons of the proportion of all patients with negative D-dimer results, sensitivity, and specificity were performed using exact binomial testing, and 95% CIs for the absolute differences were calculated using the Agresti and Min approach [13]. For the NPV, the method for paired data proposed by Leisenring, Alonzo and Pepe was used (generalized score statistic) [14]. Comparisons were considered significant if the two-sided P-values were less than 0.05. All statistical analyses were performed with the use of the SPSS/PC software package (version 26, SPSS) and the DTComPair package in R version 3.2.3.
Results
After excluding 1 patient who did not undergo D-dimer testing within 12 hours after randomization and 1 patient who had a high clinical pretest probability, a total of 368 patients were eligible for this analysis. The mean (SD) age was 70.2 (9.8) years, and 23.4% of the patients were women. A total of 44.3% of the patients had a low clinical pretest probability, and 55.7% had a moderate clinical pretest probability (Table 1). There were 2 PE-positive patients (1.2%) among those with low clinical pretest probability and 15 PE-positive patients (7.3%) among those with moderate clinical pretest probability.
Comparison of the strategies
The proportion of patients with a negative result was 49.5% with the conventional threshold strategy, 63.3% with the age-adjusted strategy (difference 13.8%; 95% CI, 6.5% to 21.0%; P <0.001), 64.4% with the Wells strategy (difference 14.9%; 95% CI, 7.6% to 22.1%; P <0.001), and 71.5% with the YEARS strategy (difference 22.0%; 95% CI, 14.8% to 28.9%; P <0.001).
Sensitivity of the conventional strategy was 94.1%, while it was 76.5% with the age-adjusted strategy (difference 17.6%; 95% CI, -11.8% to 44.9%; P =0.02), 64.7% with the Wells strategy (difference 29.4%; 95% CI, -2.5% to 56.1%; P <0.001), and 58.8% with the YEARS strategy (difference 35.3%; 95% CI, 2.3% to 61.3%; P <0.001). NPVs and negative likelihood ratios of the different strategies are shown in Table 2.
Categorization of D-dimer results as positive or negative by the conventional and the age-adjusted strategies was in agreement for 317 (86%) patients and in disagreement for 51 (14%) patients (Table 3). Of the disagreements, 51 patients were categorized as positive by the conventional strategy and negative by the age-adjusted strategy. There were 3 PE-positive patients among those who were D-dimer positive by one strategy and negative by the other. Agreements between the conventional strategy and the Wells and YEARS strategies are shown in Table 3.
Findings according to clinical probability
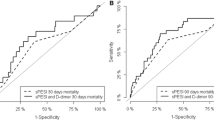
According to the Wells score, 163 (44.3%) patients had low clinical pretest probability. The conventional D-dimer strategy categorized 88 (54.0%) patients with low clinical pretest probability as negative, and had a NPV of 100% (95% CI, 95.9% to 100%). The age-adjusted D-dimer strategy categorized 113 (69.3%) patients with low clinical pretest probability as negative, and had a NPV of 99.1% (95% CI, 95.2% to 100%). The Wells-adjusted D-dimer strategy categorized 88 (54.0%) patients with low clinical pretest probability as negative, and had a NPV of 100% (95% CI, 95.9% to 100%). The YEARS-adjusted D-dimer strategy categorized 127 (77.9%) patients with low clinical pretest probability as negative, and had a NPV of 99.2% (95% CI, 95.7% to 100%) (Fig. 1).
Of the total, 205 (55.7%) patients had moderate clinical probability. The conventional D-dimer strategy categorized 94 (45.6%) patients with moderate clinical pretest probability as negative, and had a NPV of 98.9% (95% CI, 94.2% to 100%). The age-adjusted D-dimer strategy categorized 120 (58.5%) patients with moderate clinical pretest probability as negative, and had a NPV of 97.5% (95% CI, 92.9% to 99.5%). The Wells-adjusted D-dimer strategy categorized 149 (72.7%) patients with moderate clinical pretest probability as negative, and had a NPV of 96.0% (95% CI, 91.4% to 98.5%). The YEARS-adjusted D-dimer strategy categorized 136 (66.3%) patients with moderate clinical pretest probability as negative, and had a NPV of 95.6% (95% CI, 90.6% to 98.4%) (Fig. 1).
Overall, 311 (84.5%) patients had no YEARS items. The conventional D-dimer strategy categorized 164 (52.7%) patients with no YEARS items as negative, and had a NPV of 99.4% (95% CI, 96.7% to 100%). The age-adjusted D-dimer strategy categorized 212 (68.2%) patients with no YEARS items as negative, and had a NPV of 98.1% (95% CI, 95.2% to 99.5%). The Wells-adjusted D-dimer strategy categorized 206 (66.2%) patients with no YEARS items as negative, and had a NPV of 97.1% (95% CI, 93.8% to 98.9%). The YEARS-adjusted D-dimer strategy categorized 245 (78.8%) patients with no YEARS items as negative, and had a NPV of 97.1% (95% CI, 94.2% to 98.8%).
Among the 368 patients, 57 (15.5%) patients had one or more YEARS items. The conventional D-dimer strategy categorized 18 (31.6%) patients with one or more YEARS items as negative, and had a NPV of 100% (95% CI, 81.5% to 100%). The age-adjusted D-dimer strategy categorized 21 (36.8%) patients with one or more YEARS items as negative, and had a NPV of 100% (95% CI, 83.9% to 100%). The Wells-adjusted D-dimer strategy categorized 31 (54.4%) patients with one or more YEARS items as negative, and had a NPV of 100% (95% CI, 88.8% to 100%). The YEARS-adjusted D-dimer strategy categorized 18 (31.6%) patients with one or more YEARS items as negative, and had a NPV of 100% (95% CI, 81.5% to 100%).
Discussion
Our study provides external validation of different strategies of D-dimer interpretation in patients hospitalized for COPD exacerbation and no initial clinical suspicion of PE. While the conventional strategy was able to exclude PE in one half of the patients, the use of age- or clinically-adjusted D-dimer threshold strategies resulted in an even higher percentage of patients in whom PE could be considered ruled out without the need for imaging. Both the conventional and age-adjusted strategies were associated with a low risk of PE diagnosed at initial testing or VTE within a 3-month follow-up period [15], but only the conventional fixed D-dimer threshold strategy had a sensitivity high enough to rule out PE.
Our results are in line with those observed in studies using an age-adjusted D-dimer threshold [4, 16, 17]. Particularly, for patients with COPD and a PE-unlikely Wells score, a systematic review and individual-patient data meta-analysis showed that age-adjusted D-dimer testing was effective (i.e., increased the proportion of COPD patients managed without imaging from 21% to 32%) and safe (i.e., the false negative rate increased from 0.7% to 1.2%) [18]. SLICE showed that the application of the age adjusted D-dimer cut-off value would result in the exclusion of VTE in almost 2 out of 3 (63.3%) of the patients hospitalized with COPD exacerbation, while the negative predictive value stayed above 98%. Although the magnitude of false negative findings seemed small, some caution may be warranted in using the age-adjusted strategy in settings with a higher PE prevalence, since its sensitivity was low.
Previous studies have shown that the clinical-adjusted strategies (i.e., the Wells score and the YEARS algorithm) have the potential to safely reduce CTPA use [5, 6]. Our analysis suggests that the conventional strategy is a better way of interpreting D-dimer results than the clinical probability-adjusted strategy among patients hospitalized with COPD exacerbation and without initial clinical suspicion of PE. Study design, setting and patient selection might account for the difference between previous studies and this analysis. Moreover, some data suggest that the accuracy of clinical prediction rules might be compromised in patients with underlying cardiopulmonary disease [19].
This study might have practical implications. The SLICE trial showed that an active diagnostic strategy for PE is not beneficial among patients hospitalized for an exacerbation of COPD [11]. However, D-dimer is often used in daily practice as a screening test in patients admitted to the Emergency Departments with chest symptoms [20]. On the basis of this analysis, clinicians might consider the use of a conventional fixed threshold interpretation for patients with COPD exacerbations who have a D-dimer test result because it avoids imaging in half of the patients with great safety. The efficiency is most pronounced in patients with low clinical pretest probability. Since patients with COPD exacerbations tend to be older, the age-adjusted strategy might be employed to reduce unnecessary exposure to radiation and potentially harmful contrast medium, unacceptable diagnosis-related and treatment-related costs, and serious or life-threatening bleeding complications of unjustified anticoagulation therapy.
Limitations
This study has several limitations. First, this was a post hoc analysis of the intervention arm in a large randomized controlled trial with adjudicated outcomes. However, all the variables required to apply the Wells score and the YEARS algorithm were prospectively collected. Second, there was no a priori sample size calculation, and the modest number of patients in the analysis might not have provided estimates with reasonable precision. Third, the prevalence of PE was low. Therefore, the safety of the strategies might be lower in settings with a higher PE prevalence. Fourth, different D-dimer assays were used in the trial. However, we didn´t find any interaction between the D-dimer type or cutoff and the study results. Fifth, the findings in the study population might not apply to other patients with COPD. However, the inclusion and exclusion criteria were intended to be consistent with the pattern of patients admitted to the hospital with exacerbations of COPD. Finally, additional details about the body mass index, and baseline use of medications such as aspirin or statins would have been interesting. However, such data elements were not collected systematically in SLICE. This limitation is unlikely to undermine the findings of the current investigation.
Conclusions
Among patients hospitalized for an exacerbation of COPD, our study suggests that the age- and clinically-adjusted strategies of D-dimer interpretation were associated with a larger number of patients in whom PE could be considered ruled out with a higher likelihood of subsequent PE than the conventional strategy. Although the magnitude of false negative findings with the age-adjusted strategy was small, additional studies are warranted to ascertain the safety of this approach.
Availability of data and materials
Data will be available upon reasonable request by Dr Jiménez, djimenez.hrc@gmail.com
Abbreviations
- CI:
-
confidence interval
- COPD:
-
Chronic obstructive pulmonary disease
- CTPA:
-
Computed tomography pulmonary angiography
- DDU:
-
D-dimer Unit
- DVT:
-
Deep vein thrombosis
- FEU:
-
Fibrinogen Equivalent Unit
- NPV:
-
Negative predictive value
- PE:
-
Pulmonary embolism
- SLICE:
-
Significance of Pulmonary Embolism in COPD Exacerbations
- VTE:
-
Venous thromboembolism
References
Konstantinides SV, Meyer G, Becattini C, et al. ESC Scientific Document Group. 2019 ESC Guidelines for the diagnosis and management of acute pulmonary embolism developed in collaboration with the European Respiratory Society (ERS). Eur Heart J. 2020;41:543–603.
Lim W, Le Gal G, Bates S, et al. American Society of Hematology 2018 guidelines for management of venous thromboembolism: diagnosis of venous thromboembolism. Blood Adv. 2018;2:3226–56.
Wells PS, Anderson DR, Rodger M, et al. Excluding pulmonary embolism at the bedside without diagnostic imaging: management of patients with suspected pulmonary embolism presenting to the emergency department by using a simple clinical model and d-dimer. Ann Intern Med. 2001;135:98–107.
Righini M, Van Es J, Den Exter PL, et al. Age-adjusted D-dimer cutoff levels to rule out pulmonary embolism: the ADJUST-PE study. JAMA. 2014;311:1117–24.
Kearon C, de Wit K, Parpia S, et al. Diagnosis of pulmonary embolism with D-dimer adjusted to clinical probability. N Engl J Med. 2019;381:2125–34.
Van der Hulle T, Cheung WY, Kooij S, et al. Simplified diagnostic management of suspected pulmonary embolism (the YEARS study): a prospective, multicentre, cohort study. Lancet. 2017;390:289–97.
Winter JH, Buckler PW, Bautista AP, et al. Frequency of venous thrombosis in patients with an exacerbation of chronic obstructive lung disease. Thorax. 1983;38:605–8.
Tillie-Leblond I, Marquette CH, Perez T, et al. Pulmonary embolism in patients with unexplained exacerbations of chronic obstructive pulmonary disease: prevalence and risk factors. Ann Intern Med. 2006;144:390–6.
Rutschmann OT, Cornuz J, Poletti PA, et al. Should pulmonary embolism be suspected in exacerbation of chronic obstructive pulmonary disease? Thorax. 2007;62:121–5.
Rizkallah J, Man P, Sin D. Prevalence of pulmonary embolism in acute exacerbations of COPD. Chest. 2009;135:786–93.
Jiménez D, Agustí A, Tabernero E, et al. Effect of a pulmonary embolism diagnostic strategy on clinical outcomes in patients hospitalized for COPD exacerbation: a randomized clinical trial. JAMA. 2021;326:1277–85.
Jimenez D, Agusti A, Monreal M, et al. The rationale, design, and methods of a randomized, controlled trial to evaluate the efficacy and safety of an active strategy for the diagnosis and treatment of acute pulmonary embolism during exacerbations of chronic obstructive pulmonary disease. Clin Cardiol. 2019;42:346–51.
Agresti A, Min Y. Simple improved confidence intervals for comparing matched proportions. Stat Med. 2005;24:729–40.
Leisenring W, Alonzo T, Pepe MS. Comparisons of predictive values of binary medical diagnostic tests for paired designs. Biometrics. 2000;56:345–51.
Dronkers CEA, van der Hulle T, Le Gal G, et al. Towards a tailored diagnostic standard for future diagnostic studies in pulmonary embolism: communication from the SSC of the ISTH. J Thromb Haemost. 2017;15:1040–3.
Douma RA, Le Gal G, Sohne M, et al. Potential of an age adjusted D-dimer cut-off value to improve the exclusion of pulmonary embolism in older patients: a retrospective analysis of three large cohorts. BMJ. 2010;340:c1475.
Schouten HJ, Geersing GJ, Koek HL, et al. Diagnostic accuracy of conventional or age adjusted D-dimer cut-off values in older patients with suspected venous thromboembolism: systematic review and meta-analysis. BMJ. 2013;346:f2492.
Van Es N, van der Hulle T, van Es J, et al. Wells rule and D-dimer testing to rule out pulmonary embolism: a systematic review and individual-patient data meta-analysis. Ann Intern Med. 2016;165:253–61.
Monreal M, Sanchez Muñoz Torrero JF, Naraine VS, et al. Pulmonary embolism in patients with chronic obstructive pulmonary disease or congestive heart failure. Am J Med. 2006;119:851–8.
Kabrhel C, Matts C, McNamara M, et al. A highly sensitive ELISA D-dimer increases testing but not diagnosis of pulmonary embolism. Acad Emerg Med. 2006;13:519–24.
Acknowledgements
We express our gratitude to S&H Medical Science Service, for their quality control data, logistic and administrative support.
Role of the Funder/Sponsor
The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Group Information
A listing of the SLICE investigators appears in Appendix.
Funding
This work was supported by grants from the Instituto de Salud Carlos III (PI14/00400), Chest Foundation, Sociedad Española de Neumología y Cirugía Torácica (SEPAR), Neumosur, and Daiichi Sankyo.
Author information
Authors and Affiliations
Contributions
Concept and design: Rodríguez, Jiménez. Acquisition, analysis, or interpretation of data; statistical analysis: Rodríguez, Jara-Palomares, Tabernero, Tenes, González, Briceño, Lobo, Morillo, Bikdeli, Jiménez. Drafting of the manuscript: Rodríguez, Bikdeli, Jiménez. Critical revision of the manuscript for important intellectual content: Rodríguez, Jara-Palomares, Tabernero, Tenes, González, Briceño, Lobo, Morillo, Bikdeli, Jiménez. Obtained funding: Jiménez. Study supervision: Jimenez. Dr Jiménez had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. The author(s) read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The institutional review board at each of the participating sites approved the protocol, and each patient provided written informed consent.
Consent for publication
Not applicable.
Competing interests
C.R. has nothing to disclose.
L.J-P. has served as an advisor or consultant for Actelion Pharmaceuticals, Bayer HealthCare Pharmaceuticals, Leo Pharma, Menarini, Pfizer, and ROVI.
E.T. has nothing to disclose.
A.T. has nothing to disclose.
S.G. has nothing to disclose.
W.B. has nothing to disclose.
J.L.L. has nothing to disclose.
R.M. has nothing to disclose.
B.B. reports that he serves as a consulting expert (on behalf of the plaintiff) for litigation related to two specific brand models of inferior vena caval filters.
D.J. has served as an advisor or consultant for Bayer HealthCare Pharmaceuticals, Boehringer Ingelheim, Bristol-Myers Squibb, Daiichi Sankyo, Leo Pharma, Pfizer, ROVI and Sanofi; served as a speaker or a member of a speakers’ bureau for Bayer HealthCare Pharmaceuticals, Boehringer Ingelheim, Bristol-Myers Squibb, Daiichi Sankyo, Leo Pharma, ROVI and Sanofi; received grants for clinical research from Daiichi Sankyo, Sanofi and ROVI.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendices
Appendix 1
Investigators: Barcelona (20 patients) – S. Jiménez (16 patients), A. Vilas (3 patients), D. Aisa (1 patient); Bilbao (113 patients) – E. Tabernero/B. González-Quero (113 patients); Galdakao (21 patients) – A. Ballaz/L. Chasco (21 patients); Gran Canaria (35 patients) – G. Pérez-Peñate/F. León-Marrero (35 patients); La Coruña (25 patients) – P. Marcos-Rodríguez/S.J. Domínguez-Pazos (25 patients); Madrid (364 patients) – D. Jiménez/A. Quezada (171 patients), A. Hernando/J.I. de Granda-Orive (91 patients), P. Ruiz-Artacho/F. Beddar-Chaib (56 patients), M.J. Rodríguez-Nieto/Itziar Fernández-Ormaechea (28 patients), M. Calle/J.L. Rodríguez-Hermosa/J. Carriel (12 patients), A. Martínez-Verdasco (2 patients), J. de Miguel-Díez (2 patients), M.A. Quesada (2 patients); Santander (17 patients) – R. Agüero (17 patients); Sevilla (112 patients) – L. Jara-Palomares/R. Otero/E. Márquez-Martín (112 patients); Valencia (8 patients) – R. López-Reyes (8 patients); Vitoria (31 patients) – J.L. Lobo/A. Rivas-Guerrero (31 patients).
Appendix 2
Table 4 Methods for D-dimer analysis and cut-offs
Test | Criteria for positivity | Unit type |
|---|---|---|
D-dimer ELISA KIT | >500 ng/mL | FEU |
VIDAS D-dimer | >500 ng/mL | FEU |
IL Test D-dimer | >500 ng/mL | FEU |
HemosIL D-Dimer | >250 ng/mL | DDU |
HemosIL AcuStar | >491 ng/mL | FEU |
HemosIL D-dimer HS 500 | >500 ng/mL | FEU |
INNOVANCE D-dimer Assay | >500 ng/mL | FEU |
STA-Liatest D-Di | >500 ng/mL | FEU |
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Rodríguez, C., Jara-Palomares, L., Tabernero, E. et al. Adjusted D-dimer cutoff levels to rule out pulmonary embolism in patients hospitalized for COPD exacerbation: results from the SLICE trial. Thrombosis J 20, 10 (2022). https://doi.org/10.1186/s12959-022-00368-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12959-022-00368-0