Abstract
Background
Multiple treatment options at glioblastoma progression exist, including reintervention, reirradiation, additional systemic therapy, and novel strategies. No alternative has been proven to be superior in terms of postprogression survival (PPS). A second surgery has shown conflicting evidence in the literature regarding its prognostic impact, possibly affected by selection bias, and might benefit a sparse subset of patients with recurrent glioblastoma. The present study aims to determine the prognostic influence of salvage procedures in a cohort of patients treated in the same institution over 15 years.
Methods
Three hundred and fifty patients with confirmed primary glioblastoma diagnosed and treated between 2005 and 2019 were selected. To examine the role of reoperation, we intended to create comparable groups, previously excluding all diagnostic biopsies and patients who were not actively treated after the first surgery or at disease progression. Uni- and multivariate Cox proportional hazards regression models were employed, considering reintervention as a time-fixed or time-dependent covariate. The endpoints of the study were overall survival (OS) and PPS.
Results
At progression, 33 patients received a second surgery and 84 were treated with chemotherapy only. Clinical variables were similar among groups. OS, but not PPS, was superior in the reintervention group. Treatment modality had no impact in our multivariate Cox regression models considering OS or PPS as the endpoint.
Conclusions
The association of reoperation with improved prognosis in recurrent glioblastoma is unclear and may be influenced by selection bias. Regardless of our selective indications and high gross total resection rates in second procedures, we could not observe a survival advantage.
Similar content being viewed by others
Background
High-grade glioma remains one of the most frequent pathologies associated with poor prognosis, despite modest improvements in overall survival (OS) [1] and progression-free survival (PFS) after the introduction of the Stupp protocol [2] in recent years. This standard of care consists of maximal surgical resection whenever feasible, followed by radiotherapy and temozolomide (TMZ) concomitant and adjuvant schedules. Unfortunately, regardless of optimal treatment fulfillment, tumor regrowth is the rule in virtually all patients, with some options at this point that include different salvage chemotherapy schemes, reresection, additional radiotherapy, or tumor treating fields, alone or in combination [3,4,5,6].
As there is no established second-line chemotherapy regimen, patients are usually treated within investigational protocols. Bevacizumab is an agent commonly used in clinical practice for relapsed glioblastoma that has demonstrated high response rates [7, 8]. However, this short-lasting effect may be due to changes in vascular permeability. Nitrosurea-based therapeutic strategies (lomustine, fotemustine) have added limited survival effects, alone or in combination [9]. Newer strategies, such as immunotherapy, targeted agents, or novel radiation modalities, have yielded promising results in clinical trials, but further validation is needed [10].
A second surgery is a treatment option for a limited number of patients only due to poor clinical status or involvement of critical brain areas. The current data on the role of reoperation in recurrent glioblastoma are still lacking in high levels of clinical evidence, mainly owing to the retrospective nature of the majority of the studies, heterogeneity of the clinical scenario that always implies a strong selection bias, and lack of prospective data collection [11, 12]. This study aims to explore a prognostic role for reoperation in recurrent glioblastoma patients and to compare its benefits whether it is considered a standard, time-fixed covariate or a time-dependent covariate.
Methods
Patient selection
We retrospectively analyzed patients with new histopathological diagnoses of glioblastoma according to 2016 World Health Organization criteria [13] in our institution over a period between January 2005 and December 2019. The follow-up period ended on 12.31.2021. The study protocol was approved by the institutional ethics committee. Patients were divided based on the extent of the primary operation between resection and biopsy. Biopsies’ main indications were deep-seated or multicentric location, involvement of brain eloquent areas, and comorbidities that would preclude a debulking procedure. Our target study group included patients in whom surgical tumor resection was indicated, followed by ulterior complementary treatment; disease progression was detected and treated. Patients diagnosed only with biopsy, not treated within the Stupp protocol after the first surgery, or not actively treated after progression (best supportive care (BSC)) were excluded from the study group.
To determine the efficacy of a second surgery at glioblastoma progression, our group sample was stratified into two cohorts: (i) patients who underwent reresection generally followed by systemic treatment and (ii) patients treated with additional chemotherapy only. A flowchart diagram illustrates the patient selection process (Fig. 1).
All patients with recurrent disease were discussed in our multidisciplinary tumor board. Although a clear protocol in our institution is lacking, general considerations for reintervention include patients in good clinical condition with tumors that arise in the vicinity of the previous cavity and not involving eloquent cortical areas, basal ganglia, or diencephalic or brainstem structures, with a PFS generally superior to 9 months.
Clinical variables
Medical records were evaluated in terms of age, sex, comorbidities, clinical symptoms, tumor location, and estimated volume in cubic centimeter based on the abc/2 method. The extent of resection (EOR) was categorized as total (GTR) or partial (STR) if any contrast-enhanced image remained in an early postoperative MRI scan. The use of surgical assistants was divided between conventional neuronavigation or “advanced” if 5-ALA fluorescence guidance or intraoperative MRI were employed. Patients’ clinical status was defined based on the Eastern Cooperative Oncology Group (ECOG) scale and was measured after the first procedure, at the first progression, after the second surgery, and at the second progression. Patients were divided into symptomatic (ECOG 2–3–4) and asymptomatic or mild symptoms (ECOG 0–1) groups. Completion of maximal first-line treatment was assessed. All recorded complications were grouped according to the Landriel-Ibañez classification [14]. Finally, we divided our population depending on the year in which they were diagnosed.
The date, clinical characteristics, and choice of treatment at progression were noted. Continuous variables such as age and PFS were also dichotomized, taking into account the median of our study group as the cutoff value.
Outcomes
OS was defined as the time from initial diagnosis until death of any cause, considering censored patients who were still alive at the study endpoint or lost to follow-up. PFS was defined as the time from diagnosis to objective tumor recurrence in neuroimaging based on the RANO criteria [15]. MRIs with high suspicion of pseudoprogression [16] were monitored with follow-up images at 8–12 weeks. Postprogression survival (PPS), defined as the time from tumor recurrence to death of any cause, was also considered.
Statistical analysis
The statistical software used for the analyses was SPSS 22.0 (IBM, Armonk, NY). Categorical variables are presented as frequencies and percentages, and continuous variables are presented as medians and ranges. χ2 and Mann–Whitney U tests were conducted for intergroup comparisons. Survival analysis was performed using the log-rank test and illustrated by Kaplan–Meier survival curves. Univariate and multivariate Cox proportional hazards regression models were used to adjust for confounders in survival, obtaining hazard ratios (HR) and 95% confidence intervals (CI) [17]. p values less than or equal to 0.05 were considered significant.
The effect of a second surgery on OS and PPS in our multivariate models was evaluated in a classical manner first, considering reoperation as a time-fixed covariate (i.e., repeat resection status was known at initial diagnosis) and as a time-dependent covariate afterward (all patients belonged to the nonoperative group at the initial study, and it was only when they received a second operation that they crossed over to the reoperation group) [18].
Results
Descriptive statistics and intergroup comparison
Among the 350 patients with de novo glioblastoma diagnosis, total resection was attempted in 214 cases (61.1%). We excluded 136 patients who were diagnosed by open or stereotactic biopsies. Due to different clinical reasons, 48 patients did not receive further oncological treatment in our institution after surgical resection and were also excluded from the survival analysis. All patients were treated with 60 Gy of radiotherapy and completed a variable number of temozolomide adjuvant cycles. At progression, a combination of a second procedure followed by different chemotherapy schemes was elected in 33 cases (group i), 84 patients received chemotherapy (group ii), and exclusion was performed in the remaining 49 cases receiving BSC.
The main characteristics of the 117 patients (group i + ii) included in the study sample are summarized in Table 1. The mean age of the cohort was 58 years. There were significant differences between groups in terms of EOR, completeness of the Stupp protocol, clinical status at disease relapse, type, and radiological pattern of progression. We could not detect differences in age, sex, tumor volume or location, medical comorbidities, or complications after the first surgery. No differences were identified in molecular markers (p53, EGFR amplification, Ki67, IDH, and MGMT promoter methylation status). These facts demonstrate the homogeneity of the selected cohort.
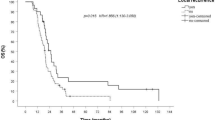
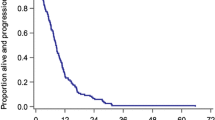
Among patients who underwent reintervention, the median OS was 25 months compared to 17 months in the nonsurgical group (log-rank test, p = 0.004). PFS differed significantly between cohorts (median 12 months vs. 9 months; p = 0.002). The median PPS was not significantly different between the surgical group (9 months) and the systemic treatment group (8 months) (p = 0.143). The Kaplan–Meier survival curves are illustrated in Figs. 2 and 3.
Classic univariate and multivariate models
Univariate Cox proportional hazards analysis was performed to identify the significant influencing variables in prognosis. The results revealed that receiving at least six cycles of temozolomide (p < 0.001), having a PFS equal to or higher than the median of our group (10 months, p < 0.001), having a low score on the ECOG scale at progression (p = 0.002), and belonging to the reintervention group (p = 0.006) were significantly associated with OS. Considering PPS as the endpoint, our results reveal that patients in good clinical condition at progression (p = 0.002) and cases diagnosed and treated in recent years (2012–2019, p = 0.021) are associated with longer PPS. Modality of treatment (p = 0.166) or higher PFS (p = 0.836) were no longer associated with survival benefits. The complete results are summarized in Tables 2 and 3.
The multivariate Cox proportional hazards regression model revealed that no differences were encountered regarding OS in the modality of treatment at progression (HR 0.75; CI 95% 0.46–1.21; p = 0.248), adjusting for the most significant covariates. A longer progression-free interval (HR 0.38; CI 95% 0.20–0.74; p = 0.004) seems to be the only variable statistically associated with superior OS in our group (Table 4). There is no longer such an association if we perform the multivariable model taking PPS as the endpoint (HR 1.12; CI 95% 0.80–1.82; p = 0.356). In this setting, a good clinical status at progression or being operated on in the recent years of the study (2012–2019) appears to favor PPS (Table 5).
Multivariate model with reoperation as a time-dependent covariate
An analog multivariate analysis was performed, considering reintervention as a time-dependent covariate and controlling it for known predictors of OS. In this setting, we conclude that a longer progression-free interval (HR, 0.43; CI 95% 0.22–0.83; p = 0.012) and low scores (0 or 1) on the ECOG scale at progression (HR, 0.57; CI 95% 0.37–0.88; p = 0.011) continue to influence OS independently, but once we incorporate the timing of resection, it seems that a second surgery may negatively affect survival (HR, 1.76; CI 95% 1.10–2.80; p = 0.017). The complete results are summarized in Table 6.
Discussion
The treatment of recurrent glioblastoma remains a challenging clinical decision. Different attempts have been made to guide whether to proceed with surgical management at progression. Scoring systems based on patients’ clinical status, tumor volume, and involvement of eloquent cortex or ependymal tissue were developed [19,20,21]. Literature reviews identify factors associated with better prognosis and generally correlate second procedures with a survival advantage in selected candidates but lack the determination of concrete indications [22,23,24].
The median values for OS and PFS in our series are in accordance with recent literature reviews [21]. Our rate for repeated surgery (15.4%) is slightly inferior when compared to the percentages reported in other studies [22, 25,26,27,28]. This may be influenced by different indications for a “redo” procedure among centers. We do not usually consider a second surgery for patients who have previously received a partial resection. However, some reports include patients who have had an incomplete first resection or even biopsies in the “surgical group” [26, 29]. Our group also does not consider reintervention in tumors that spread in a distal, contralateral, or multicentric manner [30]. Multiple reresections are seldom considered, even though some authors found improvements in OS with repetitive surgeries [31]. Some series report a high incidence of patients suffering from new neurological deficits before the second operation [26]; however, our main indication (24 patients, 73%) was radiological tumor progression with minimal symptoms. Differences in indications among institutions may over- or underestimate the clinical usefulness of multiple procedures. Our gross total resection rate (29 cases, 87.8%) in the second surgeries is much higher than that in other reports [25, 32,33,34,35] and may be due to our limited surgical indications and intraoperative MRI or 5-aminolevulinic acid fluorescence guidance. Although completeness of resection in recurrent tumors has been identified as an independent factor associated with improved survival [27, 32, 33, 35,36,37,38], our study failed to appreciate this. Our complication rate after the second procedure (4 of 33 patients; 12%) was within acceptable percentages and in accordance with other reports [28, 33]. Despite adequate clinical results in reoperated patients, we failed to demonstrate improvements in survival. In fact, when reintervention was examined as a time-dependent covariate, it seemed to counteract survival (HR 1.76; p = 0.017).
Due to the heterogeneity of clinical practice, it is difficult to achieve comparable groups. We ultimately created two cohorts according to the treatment received, having previously excluded from the analysis all patients diagnosed by biopsy, not treated with the Stupp protocol or candidates for BSC at disease relapse, making both groups more homogeneous. Minimal differences in age and comorbidities were found between cohorts. In addition, it is not uncommon to include patients who received biopsy as the first treatment [29] or BSC at progression [21, 39] in the nonoperative group, probably favoring selection bias and overestimating survival data [27].
We believe that studies that support reintervention are likely to introduce a strong selection bias that favors the best candidates for redo procedures [26,27,28, 31, 39, 40]. In several reports, greater OS in surgical cohorts may be more influenced by favorable clinical characteristics than the procedure itself. To better assess this question, a subgroup analysis was created by Tully et al., excluding patients in the control group who were very unlikely to be considered for reoperation, suggesting a much less significant effect of second procedures on prognosis [40]. However, the initial difference in OS was 10.9 months between the groups.
Furthermore, strategies to deal with temporal bias are well established in the literature and have been addressed in other medical areas. The time from the initial diagnosis to recurrence or reoperation is not predictable and, hence, reoperation is a time-dependent variable in nature. Time-dependent methodology has been used to determine prognosis in breast [41] or colon cancer [42]. The vast majority of studies consider reoperation as a fixed covariate, but as explained by Beyersmann et al. [43], ignoring timing in a time-dependent covariate, such as reintervention, will lead to erroneous findings, overestimating the survival benefit [44]. A few novel studies [45, 46] and even meta-analyses [47] account for the timing of repeat resection, reversing the relationship between OS and multiple surgical procedures when using the proper time-dependent methodology. We detected the same phenomenon in our time-dependent multivariate Cox regression, but the clinical interpretation for these results is yet to be determined and should be done judiciously. Nevertheless, we believe that treating reoperation as a time-dependent covariate is a basis for future work assessing multiple interventions in glioblastoma cases. One presumption for these dismal results may be related to the fact that a new surgical procedure does not counteract tumor progression distant to the contrast-enhanced lesion (i.e., T2WI changes) and might cause delays in the initiation of further systemic treatment. Moreover, this can be aggravated by any potential postoperative complication.
However, reports that do not give reintervention a survival advantage exist [34, 48,49,50,51,52]. De Bonis et al. reported similar PPS rates and found PPS to be higher in patients treated with chemotherapy alone than in those treated with surgery alone [34]. Michaelsen et al. compared patients who received only chemotherapy at progression with those receiving both treatments with no additional effect on survival [53]. Moreover, some studies did not measure the outcomes from the date of progression [27, 28]. For this reason, we employed PPS to determine if adding a second surgery benefits survival from the date of recurrence; having detected that, although initial differences in OS were found, treatment modality had little impact on this endpoint. Our study failed to perceive any relationship between longer PFS and PPS. This may reveal that patients with longer PFS, who usually complete the Stupp regime and receive active treatment at progression, may have longer OS. The choice of therapy at progression seems to have less impact on prognosis in our group.
Patients elected for second procedures may have significantly longer PFS, which seems to be the more influential variable that favors OS in our group. Other colleagues further validated this finding [23, 27, 28, 48, 54] and may reflect the usual practice of not offering salvage procedures to early progressions. Multivariate Cox regression methodology was performed to reduce the confounding effects of subrogated variables. The correlation between PFS and OS was maintained, treating reresection as a stationary or time-dependent covariate. Although some studies have determined that reoperation improves survival regardless of other prognostic factors [27, 40], we could not identify that outcome. Only longer PFS and good clinical status at progression proved to be protective effects for OS in our multivariable model.
Although reresection has yielded disappointing results in our group, it may still have a role in some patients to allow tumor mass effect reduction and achieve symptom relief, as stated in a recent EANO consensus review [55].
Our survival analysis presents several limitations: its retrospective design always implies selection bias because patients in better clinical condition and with surgically amenable lesions are considered for second procedures. Furthermore, the relatively small sample size compared to other works made in a multicenter fashion [32] diminishes the power of the statistical analysis and reduces the capacity of assessing the role of reoperation in recurrent glioblastoma. However, our time-dependent evaluation will add data for potential future meta-analyses. Another advantage of a single institutional data source diminishes possible confounding effects between different neurosurgical units and allows for more similar groups to be contrasted. Most studies are retrospective because it is difficult to consider a prospective and randomized study assessing this question mainly due to ethical reasons. Quality of life is another concern taken into account by other colleagues [34] and is lacking in our retrospective analysis.
Conclusion
Treatment for glioblastoma recurrence may be beyond the scope of surgical means. To date, studies have provided conflicting results regarding second interventions in these cases. Moreover, the vast majority of the studies assessing this topic treat reoperation as a time-fixed covariate, which may overestimate survival data. A longer PFS with completion of the Stupp protocol seems to be the significant variable influencing OS, with little impact on PPS. Active treatment benefits survival after progression, while treatment choice is less relevant.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- TMZ:
-
Temozolomide
- OS:
-
Overall survival
- PFS:
-
Progression-free survival
- PPS:
-
Postprogression survival
- BSC:
-
Best supportive care
- ECOG:
-
Eastern Cooperative Oncology Group
- IDH-1:
-
Isocitrate dehydrogenase 1
- MRI:
-
Magnetic resonance imaging
- SPSS:
-
Statistical Package for the Social Sciences
- 5-ALA:
-
5-Aminolevulinic acid
- RANO:
-
Response assessment in neurooncology
- MGMT:
-
O6-Methylguanine-DNA-methyltransferase
- EGFR:
-
Endothelial growth factor receptor
- HR:
-
Hazard ratio
- CI:
-
Confidence interval
- T2WI:
-
T2-weighted image
- EANO:
-
European Society of Neuro-Oncology
References
deSouza RM, Shaweis H, Han C, et al. Has the survival of patients with glioblastoma changed over the years? Br J Cancer. 2016;114:146–50.
Stupp R, Mason WP, van den Bent MJ, et al. Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N Engl J Med. 2005;352:987–96.
Tosoni A, Franceschi E, Poggi R, et al. Relapsed glioblastoma: treatment strategies for initial and subsequent recurrences. Curr Treat Options Oncol. 2016;17:49.
Arvold ND, Shi DD, Aizer AA, et al. Salvage re-irradiation for recurrent high-grade glioma and comparison to bevacizumab alone. J Neurooncol. 2017;135:581–91.
Stupp R, Wong ET, Kanner AA, et al. NovoTTF-100A versus physician’s choice chemotherapy in recurrent glioblastoma: a randomised phase III trial of a novel treatment modality. Eur J Cancer. 2012;48:2192–202.
Weller M, Cloughesy T, Perry JR, et al. Standards of care for treatment of recurrent glioblastoma–are we there yet? Neuro Oncol. 2013;15:4–27.
Kreisl TN, Kim L, Moore K, et al. Phase II trial of single-agent bevacizumab followed by bevacizumab plus irinotecan at tumor progression in recurrent glioblastoma. J Clin Oncol. 2009;27:740–5.
Nagane M, Kobayashi K, Tanaka M, et al. Predictive significance of mean apparent diffusion coefficient value for responsiveness of temozolomide-refractory malignant glioma to bevacizumab: preliminary report. Int J Clin Oncol. 2014;19:16–23.
Lombardi G, Farina P, Della Puppa A, et al. An overview of fotemustine in high-grade gliomas: from single agent to association with bevacizumab. Biomed Res Int. 2014;2014:698542.
Liu EK, Sulman EP, Wen PY, et al. Novel therapies for glioblastoma. Curr Neurol Neurosci Rep. 2020;20:19.
Ryken TC, Kalkanis SN, Buatti JM, et al. The role of cytoreductive surgery in the management of progressive glioblastoma: a systematic review and evidence-based clinical practice guideline. J Neurooncol. 2014;118:479–88.
Patel M, Au K, Davis FG, et al. Clinical uncertainty and equipoise in the management of recurrent glioblastoma. Am J Clin Oncol. 2021;44:258–63.
Louis DN, Perry A, Reifenberger G, et al. The 2016 World Health Organization classification of tumors of the central nervous system: a summary. Acta Neuropathol. 2016;131:803–20.
Ibañez FAL, Hem S, Ajler P, et al. A new classification of complications in neurosurgery. World Neurosurg. 2011;75:709–15.
Wen PY, Macdonald DR, Reardon DA, et al. Updated response assessment criteria for high-grade gliomas: response assessment in neuro-oncology working group. J Clin Oncol. 2010;28:1963–72.
Brandsma D, Stalpers L, Taal W, et al. Clinical features, mechanisms, and management of pseudoprogression in malignant gliomas. Lancet Oncol. 2008;9:453–61.
Wakkee M, Hollestein LM, Nijsten T. Multivariable analysis. J Invest Dermatol. 2014;134:1–5.
Fisher LD, Lin DY. Time-dependent covariates in the Cox proportional-hazards regression model. Annu Rev Public Health. 1999;20:145–57.
Park CK, Kim JH, Nam DH, et al. A practical scoring system to determine whether to proceed with surgical resection in recurrent glioblastoma. Neuro Oncol. 2013;15:1096–101.
Park JK, Hodges T, Arko L, et al. Scale to predict survival after surgery for recurrent glioblastoma multiforme. J Clin Oncol. 2010;28:3838–43.
Woernle CM, Péus D, Hofer S, et al. Efficacy of surgery and further treatment of progressive glioblastoma. World Neurosurg. 2015;84:301–7.
Montemurro N, Perrini P, Blanco MO, et al. Second surgery for recurrent glioblastoma: a concise overview of the current literature. Clin Neurol Neurosurg. 2016;142:60–4.
Hervey-Jumper SL, Berger MS. Reoperation for recurrent high-grade glioma: a current perspective of the literature. Neurosurg. 2014;75:491–9 (discussion 498–499).
Lu VM, Jue TR, McDonald KL, et al. The survival effect of repeat surgery at glioblastoma recurrence and its trend: a systematic review and meta-analysis. World Neurosurg. 2018;115:453-459.e3.
Barbagallo GM, Jenkinson MD, Brodbelt AR. ‘Recurrent’ glioblastoma multiforme, when should we reoperate? Br J Neurosurg. 2008;22:452–5.
Helseth R, Helseth E, Johannesen TB, et al. Overall survival, prognostic factors, and repeated surgery in a consecutive series of 516 patients with glioblastoma multiforme. Acta Neurol Scand. 2010;122:159–67.
Delgado-Fernandez J, Garcia-Pallero MÁ, Blasco G, et al. Usefulness of reintervention in recurrent glioblastoma: an indispensable weapon for increasing survival. World Neurosurg. 2017;108:610–7.
Ening G, Huynh MT, Schmieder K, et al. Repeat-surgery at glioblastoma recurrence, when and why to operate? Clin Neurol Neurosurg. 2015;136:89–94.
Wann A, Tully PA, Barnes EH, et al. Outcomes after second surgery for recurrent glioblastoma: a retrospective case-control study. J Neurooncol. 2018;137:409–15.
Azoulay M, Santos F, Shenouda G, et al. Benefit of re-operation and salvage therapies for recurrent glioblastoma multiforme: results from a single institution. J Neurooncol. 2017;132:419–26.
Chaichana KL, Zadnik P, Weingart JD, et al. Multiple resections for patients with glioblastoma: prolonging survival. J Neurosurg. 2013;118:812–20.
Quick J, Gessler F, Dützmann S, et al. Benefit of tumor resection for recurrent glioblastoma. J Neurooncol. 2014;117:365–72.
Ringel F, Pape H, Sabel M, et al. Clinical benefit from resection of recurrent glioblastomas: results of a multicenter study including 503 patients with recurrent glioblastomas undergoing surgical resection. Neuro Oncol. 2016;18:96–104.
De Bonis P, Fiorentino A, Anile C, et al. The impact of repeated surgery and adjuvant therapy on survival for patients with recurrent glioblastoma. Clin Neurol Neurosurg. 2013;115:883–6.
Mukherjee S, Wood J, Liaquat I, et al. Craniotomy for recurrent glioblastoma: is it justified? A comparative cohort study with outcomes over 10 years. Clin Neurol Neurosurg. 2020;188:105568.
Bloch O, Han SJ, Cha S, et al. Impact of extent of resection for recurrent glioblastoma on overall survival: clinical article. J Neurosurg. 2012;117:1032–8.
Suchorska B, Weller M, Tabatabai G, et al. Complete resection of contrast-enhancing tumor volume is associated with improved survival in recurrent glioblastoma-results from the DIRECTOR trial. Neuro Oncol. 2016;18:549–56.
Montemurro N, Fanelli GN, Scatena C, et al. Surgical outcome and molecular pattern characterization of recurrent glioblastoma multiforme: a single-center retrospective series. Clin Neurol Neurosurg. 2021;207:106735.
Chen MW, Morsy AA, Liang S, et al. Re-do craniotomy for recurrent grade IV glioblastomas: impact and outcomes from the national neuroscience institute Singapore. World Neurosurg. 2016;87:439–45.
Tully PA, Gogos AJ, Love C, et al. Reoperation for recurrent glioblastoma and its association with survival benefit. Neurosurg. 2016;79:678–89.
Jatoi I, Anderson WF, Jeong JH, et al. Breast cancer adjuvant therapy: time to consider its time-dependent effects. J Clin Oncol. 2011;29:2301–4.
Bolard P, Quantin C, Esteve J, et al. Modelling time-dependent hazard ratios in relative survival: application to colon cancer. J Clin Epidemiol. 2001;54:986–96.
Beyersmann J, Gastmeier P, Wolkewitz M, et al. An easy mathematical proof showed that time-dependent bias inevitably leads to biased effect estimation. J Clin Epidemiol. 2008;61:1216–21.
van Walraven C, Davis D, Forster AJ, et al. Time-dependent bias was common in survival analyses published in leading clinical journals. J Clin Epidemiol. 2004;57:672–82.
Goldman DA, Hovinga K, Reiner AS, et al. The relationship between repeat resection and overall survival in patients with glioblastoma: a time-dependent analysis. J Neurosurg. 2018;129:1231–9.
Delgado-Fernández J, Frade-Porto N, Blasco G, et al. Does reintervention improve survival in recurrent glioblastoma? Facing a temporal bias in the literature. Acta Neurochir (Wien). 2020;162:1967–75.
Zhao YH, Wang ZF, Pan ZY, et al. A meta-analysis of survival outcomes following reoperation in recurrent glioblastoma: time to consider the timing of reoperation. Front Neurol. 2019;10:286.
van Linde ME, Brahm CG, de Witt Hamer PC, et al. Treatment outcome of patients with recurrent glioblastoma multiforme: a retrospective multicenter analysis. J Neurooncol. 2017;135:183–92.
Clarke JL, Ennis MM, Yung WK, et al. Is surgery at progression a prognostic marker for improved 6-month progression-free survival or overall survival for patients with recurrent glioblastoma? Neuro Oncol. 2011;13:1118–24.
Franceschi E, Bartolotti M, Tosoni A, et al. The effect of re-operation on survival in patients with recurrent glioblastoma. Anticancer Res. 2015;35:1743–8.
Filippini G, Falcone C, Boiardi A, et al. Prognostic factors for survival in 676 consecutive patients with newly diagnosed primary glioblastoma. Neuro Oncol. 2008;10:79–87.
Nava F, Tramacere I, Fittipaldo A, et al. Survival effect of first- and second-line treatments for patients with primary glioblastoma: a cohort study from a prospective registry, 1997–2010. Neuro Oncol. 2014;16:719–27.
Michaelsen SR, Christensen IJ, Grunnet K, et al. Clinical variables serve as prognostic factors in a model for survival from glioblastoma multiforme: an observational study of a cohort of consecutive non-selected patients from a single institution. BMC Cancer. 2013;13:402.
Ortega A, Sarmiento JM, Ly D, et al. Multiple resections and survival of recurrent glioblastoma patients in the temozolomide era. J Clin Neurosci. 2016;24:105–11.
Wen PY, Weller M, Lee EQ, et al. Glioblastoma in adults: a Society for Neuro-Oncology (SNO) and European Society of Neuro-Oncology (EANO) consensus review on current management and future directions. Neuro Oncol. 2020;22:1073–113.
Acknowledgements
Not applicable.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
• Conceptualization and design: VGJ, MBD, and JID.
• Methodology: VGJ, MBD, and JFS.
• Data acquisition: VGJ, MBD, JFS, LMF, DAR, and SLL.
• Analysis and interpretation of data: VGJ and MBD.
• Writing—original draft preparation: VGJ.
• Writing—review and editing: MBD and JID.
All authors have approved the submitted version.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study protocol was approved by the institutional ethics committee (Comité de Ética de la Investigación de las Islas Baleares (CEI-IB)).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
González, V., Brell, M., Fuster, J. et al. Analyzing the role of reoperation in recurrent glioblastoma: a 15-year retrospective study in a single institution. World J Surg Onc 20, 384 (2022). https://doi.org/10.1186/s12957-022-02852-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12957-022-02852-3