Abstract
Background
Quality standards in postoperative outcomes have not yet been defined for gastric cancer surgery. Also, the effect of centralization of gastric cancer surgery on the improvement of postoperative outcomes continues to be debated. Short-term postoperative outcomes in gastric carcinoma patients in centers with low-volume of annual gastrectomies were assessed. The effect of age on major postoperative morbidity and mortality was also analyzed.
Methods
Patients with gastric or gastroesophageal junction Siewert III type carcinomas who underwent surgical treatment with curative intent between January 2013 and December 2016 were included. Data were obtained from the population-based surgical registry Esophagogastric Carcinoma Registry of the Comunitat Valenciana (RECEG-CV). The RECEG-CV gathers information on demographic characteristics and comorbidity, preoperative study and neoadjuvant treatment, surgical procedure, pathological study, postoperative outcomes, and follow-up. Seventeen hospitals belonging to the public network participated in this registry.
Results
Data from 591 patients were analyzed. Postoperative major morbidity occurred in 154 (26.1%) patients. Overall 30-day or in-hospital mortality, and 90-day postoperative mortality rates were 8.6% and 10.1% respectively. Failure-to-rescue was 39% and it was significantly higher in patients aged 75 years or older in comparison with younger patients (55.3% vs 23.1% p < 0.001).
In the multivariable analysis, age ≥ 75 years (p = 0.029), laparoscopic approach (p = 0.005), and total gastrectomy (p = 0.005) were associated with major postoperative morbidity. Age ≥ 75 years (p = 0.027), pulmonary complications (p = 0.001), cardiac complications (p = 0.001), leakage (p = 0.003), and hemorrhage (p = 0.013) were associated with postoperative mortality.
Conclusions
Centralization of gastric adenocarcinoma treatment in centers with higher annual caseload should be considered to improve the short-term postoperative outcomes in low-volume centers. Patients aged 75 or older had a significantly increased risk of major postoperative morbidity and mortality, and higher failure-to-rescue.
Similar content being viewed by others
Background
Incidence of gastric adenocarcinoma shows a progressive drop over the last decades in contrast with the increasing incidence of gastroesophageal junction (GEJ) adenocarcinomas in Western countries [1]. However, gastric adenocarcinoma is still the third leading cause of cancer-related death worldwide and long-term survival remains poor even in patients treated with curative intent [1, 2]. Surgery is the main treatment for locally advanced disease, usually combined with perioperative chemotherapy or adjuvant treatment [3, 4].
Likewise, postoperative morbidity and mortality after gastrectomy in patients with gastric and GEJ adenocarcinomas are even higher than those recorded after esophagectomy with noteworthy variations among Western countries [5, 6]. Standardization in reporting postoperative complications has been claimed to allow for comparison among different studies and for quality improvement [7].
There is a trend towards centralization of gastric cancer treatment in centers with a minimum of 20 gastrectomies annually to reduce morbidity and mortality rates, similarly to what has been done with the treatment of esophageal cancer [8,9,10]. However, the beneficial effect of centralization on postoperative outcomes is still controversial for gastric cancer surgery [11, 12].
Population-based cancer registries are useful for monitoring and improving clinical outcomes, permitting also comparison among centers or countries and for promoting epidemiological research [10,11,12]. Completeness, accuracy, and data verification are crucial to assure the quality of clinical registries [13, 14]. Control charts have been shown to be useful tools for monitoring and identifying deterioration of clinical outcomes and are increasingly used for quality control in surgical oncology [15].
The main aim of this study was to assess short-term postoperative outcomes in gastric adenocarcinoma patients surgically treated with curative intent in centers with low annual gastrectomies volume. The effect of age on major postoperative morbidity and mortality was also analyzed.
Methods
Patients
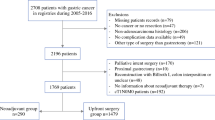
Data were obtained from the Esophagogastric Cancer Registry of the Comunitat Valenciana (RECEG-CV). The Comunitat Valenciana is an autonomous region in Eastern Spain with a population of more than 5 million inhabitants. All patients with gastric or GEJ Siewert III type (GEJ-SIII) adenocarcinomas treated with curative intent during a 4-year period (2013–2016) were included (Fig. 1). Seventeen of the 24 hospitals of the public network of the Comunitat Valenciana participated, even though 3 hospitals joined the RECEG-CV only for the last 2-year period (2015–2016). No center performed at least 20 gastrectomies annually, and for that reason all the hospitals were considered low-volume centers, although hospitals performing less than 10 gastrectomies per year were also considered as very low-volume hospitals.
RECEG-CV registry
The RECEG-CV is a population-based surgical online registry included into the NEOS platform that belongs to the Cancer Information System of the Comunitat Valenciana. It was fostered by the Valencian Surgical Society and the Epidemiological Studies and Health Statistics Service of the Comunitat Valenciana. The RECEG-CV gathers only clinical data from esophageal and gastric carcinoma patients following surgical treatment. Hospitals belonging to the public network feed data to this registry on a voluntary basis since 2013. Only one or 2 surgeons from each hospital are authorized to introduce data from their center into this online registry but are not allowed to check data from other centers. Only two investigators (F-JL and JE) had access to the entire data set in order to check the completeness and reliability of the data. Whenever some data seemed implausible or erroneous one of the two investigators contacted the authorized surgeons in the corresponding hospital for verification.
The study was approved by the Ethics Committee of the General University Hospital of Elche (PI 46/2022).
Data set
The RECEG-CV gathers information of 55 items allocated in 6 sections: demographic characteristics and comorbidity (6 items), preoperative study and neoadjuvant treatment (9 items), surgical procedure (9 items), pathological study (11 items), postoperative outcomes (11 items), and follow-up (8 items). This data set was designed as a reduced version of the online data set of the Spanish EURECCA Esophagogastric Cancer Registry (SEEGCR) [14].
Gastric and GJ-SIII tumors were staged according to the 7th edition of the UICC TNM classification [16] American Society of Anesthesiologists (ASA) score and Charlson index were collected in the comorbidity section. Pulmonary, cardiac, other medical complications, leakage, hemorrhage, reoperation, other surgical complications, Clavien-Dindo score [17], 30-day or in-hospital mortality, 90-day mortality and in-hospital stay were collected in the postoperative outcomes section. The item leakage included anastomotic or duodenal stump fistula and intra-abdominal abscess with a suspicion of an underlying fistula. Clavien-Dindo classification was also graded as no or minor postoperative morbidity (I and II) and major postoperative morbidity (III to V). Failure-to-rescue (FtR) was defined as the ratio between 90-day postoperative mortality and major postoperative morbidity.
Outcomes
Primary outcomes were major postoperative morbidity, 30-day or in-hospital mortality, and 90-day mortality. Secondary outcome was the effect of age on short-term postoperative outcomes.
Statistical analysis
Categorical variables were expressed as frequencies and percentages. Continuous variables were expressed as the median and the interquartile range. The chi-square test was used for the comparison of proportions and the Mann-Whitney test was used for the comparison of medians. The cumulative sum (CUSUM) chart was used to detect changes in postoperative mortality rates related to age. Funnel plot was used to detect variations of short-term postoperative outcomes among centers. Multivariable analysis was performed using a binary logistic regression. The statistical analysis was performed using the R version 4.0.3 (R Core Team, Vienna, Austria).
Results
Initially, 726 patients that fulfilled inclusion criteria underwent surgery. Sixty-two (8.5%) patients did not follow surgical resection due to abdominal metastasis found during laparotomy, and additional 73 (10%) underwent only a palliative R2 resection. Ultimately, data from 591 (81.4%) patients in whom a resection with curative intent was accomplished could be analyzed (Fig. 1).
Study population
Population characteristics are presented in Table 1. Five hundred and 48(92.7%) gastric carcinomas and 43 (7.3%) GEJ-SIII type carcinomas were analyzed. The antrum was the most frequent among gastric locations (49.4%) (Table 1). No center performed more than 15 gastrectomies annually and 10 of 17 hospitals participating in the study were very low-volume hospitals. Nevertheless, 366 (61.9%) patients were operated in hospitals performing 10 or more gastrectomies annually.
The median age of the whole study population was 71 (62–80), but significantly higher in patients with tumors located in the stomach compared to patients with GEJ-SIII tumors (72 vs 67 p = 0.019). Two age groups were established according to the cumulative sum plot depicted in Fig. 2. The risk of postoperative mortality increased steadily with age (p < 0.001), and after age 75, the observed probability exceeded the expected probability. The threshold established for 90-day postoperative mortality was 8.5% [18]. Patients aged 75 or older accounted for 42.3% of cases.
Men were more prevalent than women (61.4% vs 38.6%) among gastric and GEJ-SIII adenocarcinoma patients. Most patients were classified with ASA II (40.9%) or ASA III (47.7%) scores. No comorbidity or low Charlson score were more prevalent in this series (56.4%), but the Charlson score was higher in patients aged 75 years or older (p = 0.003) (Table 1).
Surgical treatment and pathological features
A significantly higher proportion of patients younger than 75 years received neoadjuvant treatment (39.8%) in comparison with patients aged 75 or older (10.5%). Surgical and pathological data of the series are shown in Table 1. Overall, total and partial gastrectomy were performed in similar percentages, but total gastrectomy was more frequently performed in patients younger than 75 years (59.7% vs 33.1%). Only 60 (10.2%) patients were treated with a laparoscopic approach.
D1+ lymphadenectomy or a more extended lymph node resection was performed in 75.7% of the cases although it was carried out more frequently in patients younger than 75 years (83.5% vs 65.1%). The median number of retrieved lymph nodes was 17, and 15 or more lymph nodes were obtained in 60.7% of resections for pathological analysis. Positive lymph nodes were found in 55.7% of the lymphadenectomies, this percentage being higher in GEJ-SIII tumors (69%). Complete R0 resection was accomplished in 94.6% of the patients.
Postoperative morbidity and mortality. Failure to rescue
Postoperative morbidity and mortality are summarized in Table 2. Major postoperative morbidity occurred in 154 (26.1%) patients, and it did not differ between very low-volume hospitals and centers with an annual caseload of 10 or more gastrectomies (26.7% and 25.7%).
Patients aged 75 or older showed higher major postoperative morbidity in comparison with younger patients (30.4% vs 22.9% p = 0.039) (Table 2). Patients with GEJ-SIII tumors showed a trend towards a major postoperative morbidity rate compared to gastric tumors (37.2% vs 25.2% p = 0.084). Leakage occurred in 90 (15.3%) patients, somewhat higher but not statistically significant, in GEJ-SIII than in gastric tumors (23.8% and 14.6%). Sixty-seven (11.4%) patients were re-operated (GEJ-SIII 9.5% and gastric 11.5%) being in 43 (64.2%) of them associated with leakage. FtR occurred in 60 (39%) patients and it was higher in patients aged 75 or older in comparison with younger patients (55.3% vs 23.1%, p < 0.001). Variations among hospitals regarding leakage, major postoperative morbidity and failure-to-rescue rates are shown in Fig. 3a-c.
The univariable analysis showed that age 75 years or older (p = 0.039), ASA score (p = 0.034), neoadjuvant chemotherapy (p = 0.036), laparoscopic approach (p = 0.022), and type of gastrectomy (p = 0.015) were associated with major postoperative morbidity (Table 3). According to the results of the univariable analysis the following variables entered the multivariable analysis: age, sex, location, ASA score, neoadjuvant chemotherapy, laparoscopic approach, type of gastrectomy and type of lymphadenectomy. Age 75 years or older (OR 1.62, 95% CI 1.05–2.49), laparoscopic approach (OR 2.32, 95% CI 1.29–4.17), and total gastrectomy (OR 1.86, 95% CI 1.2–2.86), emerged as independent prognostic factors for major postoperative morbidity (Table 4).
Overall 30-day or in-hospital mortality, and 90-day postoperative mortality rates were 8.6% and 10.1% respectively. Postoperative mortality did not differ either between very low-volume hospitals and centers with an annual caseload of 10 or more gastrectomies (9.3% and 10.7%). The 90-day postoperative mortality did not differ depending on GEJ-SIII or gastric location but it was significantly higher in patients aged 75 years or older in comparison with younger patients (16.8% vs 5,3% p < 0.001) (Table 2). Pulmonary complications and cardiac complications occurred in 63% and 38% of patients who subsequently died. Multivariable analyses that included the variables age, ASA score, laparoscopic approach, type of gastrectomy, pulmonary complications, cardiac complications, leakage, hemorrhage and reoperation identified age 75 years or older (OR 2.42, 95%CI 1.15–5.29), pulmonary complications (OR 8.54, 95% CI 4.17–17.47), cardiac complications (OR 5.14, 95% CI 2.09–12.61), leakage (OR 3.56, 95% CI 1.56–8.12), and hemorrhage (OR 5.1, 95% CI 1.4–18.48) as independent risk factors of 90-day postoperative mortality (Table 4).
Discussion
The implementation of the RECEG-CV allowed to analyze overall short-term postoperative outcomes in gastric adenocarcinoma patients treated in 17 out of the 24 hospitals of the Public Health Service of the Comunitat Valenciana and to identify variations among hospitals as well. In this first assessment of the data registered during a 4-year period, 30-day and in-hospital mortality, and 90-day mortality rates were 8.6% and 10.1% respectively. The fact that all patients included in our registry were treated in low-volume centers might partly explain the higher mortality rate compared to that reported in other clinical registries that include patients treated in high-volume centers. In a study gathering data from 5 European countries the 30-day and in-hospital mortality after gastrectomy ranged from 2.2 to 7.2% [6]. However, 30-day and in-hospital mortality rates may underestimate the true postoperative mortality, and 90-day mortality is deemed more accurate in assessing surgery-related mortality [19, 20]. Thus, a recent report from the nationwide Swedish Gastric Cancer Surgery Study (SWEGASS) showed an outstanding 30-day mortality rate of 2.9% but 90-day mortality worsened remarkably to 7.1% [21]. This significant difference between 30- and 90-day postoperative mortality (4.6 and 8.6%) was also shown in a nationwide French study [18]. Altogether, data from European clinical registries show that postoperative mortality of gastric carcinoma patients remains high. Different variables related to patient and center characteristics have been associated with postoperative mortality.
The effect of age on postoperative mortality is controversial because different cutoffs have been used in the different studies. In our study, the CUSUM plot detected a significant increase of postoperative mortality from age of 75 on, and this age cutoff point emerged also as an independent factor associated with postoperative mortality in the multivariable analysis. In our cohort this age group constituted 42% of the patients, which might also explain to a certain extent the high postoperative mortality observed in our series. In another population-based study, 90-day postoperative mortality of gastric cancer patients aged 75 years and older was 16% [19], similar to the one observed in our cohort. A recent report of the Dutch Upper Gastrointestinal Cancer Audit (DUCA) nationwide registry showed that age 70 and older was on the verge of significant association with postoperative 30-day or in-hospital mortality (OR 1.56; CI 95% 0.99 to 2.46) [21]. A progressive increase in postoperative mortality above 70 years of age was also observed within the CUSUM plot in our cohort, but significance was only reached at a cutoff point of 75 years. In addition, older patients suffered higher comorbidity and often underwent less extended surgical procedures which are potential confounding factors for assessment the effect of age on postoperative mortality. However, ASA score and total gastrectomy were not associated with postoperative mortality in the multivariable analysis. Comorbidity has been associated to an increase of postoperative mortality in some studies [11, 22], but ASA score and Charlson index may depend on interobserver assignment variability. Our results suggest that other factors associated with age such as frailty might also explain the sharp increase of postoperative mortality observed in patients aged 75 or older. Unfortunately, a frailty score was not included as a variable in our registry. Probably, identifying frail older patients during the preoperative study would be helpful for assessing more carefully the risk of postoperative morbidity and mortality [23, 24].
Neoadjuvant chemotherapy was less frequently administered than reported by the DUCA registry during the same period [21], and it was seldom administered to patients aged 75 years and older. Also, patients following neoadjuvant chemotherapy showed a not statistically significant trend to a lower major postoperative morbidity rate, in line with that described in the previous study [21], suggesting that patients in better preoperative condition received more often chemotherapy. Pulmonary and cardiac complications, leakage, and hemorrhage were independent risk factors of postoperative mortality, as reported previously in other studies [25,26,27]. Anastomotic leakage rates from 4.9% to 9.8% have been reported in several European registries [25,26,27], but overall leakage rates may have been underestimated in them, because intra-abdominal abscess, or peritonitis were recorded separately. In our analysis, leakage rate was not higher in patients aged 75 or older or in hospitals with an annual caseload below 10 either, although marked variations were observed among hospitals. Quality standards in postoperative outcomes have been defined for some digestive neoplasias but not yet for gastric cancer surgery [28, 29]. Outstanding postoperative clinical outcomes after gastrectomy for gastric cancer have been reported by the Japanese nationwide registry [30] but this cannot be presumably taken as a benchmark in Western countries. Recently, the European Gastric Cancer Association created the Gastrectomy Complications Consensus Group, with 27 participating gastric cancer referral centers. It developed a list of postoperative complications and reported short-term postoperative outcomes that might be helpful as a benchmark for gastric cancer surgery [27]. However, it should be taken into account that only selected centers participated in this project.
Patients with gastric carcinoma have a remarkable risk of death once postoperative major morbidity occurs and therefore, FtR has emerged as an important postoperative outcome in assessing the quality of surgical treatment. In our cohort, while major postoperative morbidity was only somewhat higher in patients aged 75 years or older (30% versus 23%), the FtR recorded was more than double for that group compared to younger patients (55% versus 23%). In addition, the FtR outcome detected remarkable differences among hospitals that might provide relevant information about the capacity to solve major postoperative complications in each center. These findings suggest that both age and center-related characteristics may have influence on this outcome. However, FtR should be analyzed with caution when the sample size of patients with major postoperative morbidity in a given hospital is relatively small. In a report from the DUCA registry where only 30-day and in-hospital mortality was considered, the FtR was initially 38% but this rate halved at the end of the 4-year study period [25]. Interestingly, a process of centralization was launched in The Netherlands during this period. Similarly, a report from the German nationwide registry showed a reduction of FtR associated with annual caseload [26].
Centralization policies for gastric cancer surgery have been launched in several European countries, and a minimum annual caseload of 20 gastrectomies has been proposed to achieve optimal short-term postoperative outcomes. We could not analyze the beneficial effect of annual hospital volume on short-term postoperative outcomes because only 7 centers performed 10 or more gastrectomies annually and none performed more than 15 during the study period. Thus, it might be proposed that poor rates in some short-term postoperative outcomes are related to this fact. In a report showing the short-term results after the implementation of the DUCA registry a decrease of 30-day mortality (7.1 to 4.3%) was observed at the end of the 8-year period [10]. During this period a progressive decrease of hospitals with an annual caseload below 20 gastrectomies occurred due to the centralization policy initiated in The Netherlands. Nevertheless, both, the implementation of the registry and the progressive centralization policy might have had an impact on the improvement of postoperative outcomes. In a study comparing short-term postoperative outcomes between the DUCA registry and the Swedish National Register for Oesophageal and Gastric Cancer (NREV) [12] postoperative morbidity and 30-day or in-hospital mortality was better in Sweden despite only 18% of the patients of the Swedish registry being surgically treated in hospitals performing over 20 gastrectomies per year. Nevertheless, a process of centralization of gastric cancer was formally recommended in Sweden afterwards [31]. Although centralization of gastric cancer patients is still a matter of debate, some nationwide population studies carried out in countries where centralization is not implemented suggest a beneficial effect on short-term postoperative outcomes in hospitals with a high annual volume of gastric resections [18, 26]. Moreover, minimally invasive surgical approach, increasingly introduced for the treatment gastric cancer, has a learning curve of around 40 procedures for laparoscopic distal gastrectomy and even more for laparoscopic total gastrectomy [32, 33]. In our cohort, all centers that performed laparoscopic gastrectomies were still within the learning curve which may explain that this procedure was associated with a higher postoperative major morbidity. It should also be considered that the progressive decrease of gastric carcinoma incidence in Western countries may add difficulties in completing the learning curve in low-volume centers.
Our study has some limitations. None of the hospitals performed more than 15 gastrectomies per year, and therefore the possible effect of centralization gastric cancer treatment in high-volume centers could not be analyzed. Also, participation in the RECEG-CV was optional and 7 of the 24 hospitals of the public network did not include patients in the RECEG-CV, but these 7 centers perform a low or very low volume of gastric resections annually. Finally, we did not perform a random sample verification. However, two investigators examined data carefully to detect those that were implausible or mistaken.
Conclusions
Our analysis shows that centralization of gastric cancer treatment in centers with higher annual caseload should be considered to improve the short-term postoperative outcomes in low-volume centers. Also, patients aged 75 or older had a significantly increased risk of major postoperative morbidity and mortality with a remarkably higher FtR, indicating that these patients should be more carefully studied before undergoing oncological gastrectomy. Finally, the implementation of the RECEG-CV was able to evaluate as a whole the studied short-term postoperative outcomes, also detecting noteworthy variations between the participating hospitals. Therefore, data supply to this registry should be required henceforth for all centers performing gastric cancer surgery in our autonomous region.
Availability of data and materials
The datasets generated are not publicly available because they are in the Esophagogastric Cancer Registry of the Comunitat Valenciana (RECEG-CV). The RECEG-CV is a population-based surgical online registry fostered by the Valencian Surgical Society and the Epidemiological Studies and Health Statistics Service of the Comunitat Valenciana (Spain). The RECEG-CV is included into the NEOS platform that belongs to the Cancer Information System of the Comunitat Valenciana which guarantees the compliance with the data protection law. The analyzed data of the current study could be available from the corresponding author on reasonable request.
Abbreviations
- GEJ:
-
Gastroesophageal junction
- GEJ-SIII:
-
GEJ Siewert III type
- RECEG-CV:
-
Esophagogastric Cancer Registry of the Comunitat Valenciana
- SEEGCR:
-
Spanish EURECCA Esophagogastric Cancer Registry
- FtR:
-
Failure to rescue
- CUSUM:
-
Cumulative sum chart
- ASA:
-
American Society of Anesthesiologists
- DUCA:
-
Dutch Upper Gastrointestinal Cancer Audit
References
Arnold M, Abnet CC, Neale RE, Vignat J, Giovannucci EL, McGlynn KA, et al. Global burden of 5 major types of gastrointestinal cancer. Gastroenterology. 2020;159(1):335–49.
Anderson LA, Tavilla A, Brenner H, Luttmann S, Navarro C, Gavin AT, et al. Survival for oesophageal, stomach and small intestine cancers in Europe 1999-2007: results from EUROCARE-5. Eur J Cancer. 2015;51:2155–7.
Al-Batran SE, Homann N, Pauligk C, Goetze TO, Meiler J, Kasper S, et al. Perioperative chemotherapy with fluorouracil plus leucovorin, oxaliplatin, and docetaxel versus fluorouracil or capecitabine plus cisplatin and epirubicin for locally advanced, resectable gastric or gastro-oesophageal junction adenocarcinoma (FLOT4): a randomised, phase 2/3 trial. Lancet. 2019;393(10184):1948–57.
Smyth EC, Nilsson M, Grabsch H, van Grieken NCT, Lordick F. Gastric cancer. Lancet. 2020;396(10251):635–48.
Dikken JL, van Sandick JW, Allum WH, Johansson J, Jensen LS, Putter H, et al. Differences in outcomes of oesophageal and gastric cancer surgery across Europe. Br J Surg. 2013;100:83–94.
Messaguer M, de Steur WO, van Sandick JW, Reynolds J, Pera M, Mariette C, et al. Variations among 5 European countries for curative treatment of resectable oesophageal and gastric cancer: a surrey from EURECCA Upper GI Group (European Registration of Cancer Care). Eur J Surg Oncol. 2016;42:116–22.
Low DE, Alderson D, Cecconello I, Chang AC, Darling GE, DʼJourno XB, et al. International Consensus on Standardization of Data Collection for Complications Associated With Esophagectomy: Esophagectomy Complications Consensus Group (ECCG). Ann Surg. 2015;262(2):286–94.
Coupland VH, Lagergren J, Lüchtenborg M, Jack RH, Allum W, Holmberg L, et al. Hospital volume, proportion resected and mortality fron oesophageal and gastric cancer: a population-based study in England, 2004-2008. Gut. 2013;62:961–6.
Jensen LS, Nielsen H, Mortensen PB, Pilegaard HK, Johnsen SP. Enforcing centralization for gastric cancer in Denmark. Eur J Surg Oncol. 2010;36:S50–4.
Voeten DM, Busweiler LAD, van der Werf LR, Wijnhoven BPL, Verhoeven RHA, van Sandick JW, et al. Outcomes of esophagogastric cancer surgery during eight years of surgical auditing by the Dutch Upper Gastrointestinal Cancer Audit (DUCA). Ann Surg. 2021;274:866–73.
Nelen SD, Heuthorst L, Verhoeven RHA, Polat F, Kruyt PM, Reijnders K, et al. Impact of centralizing gastric cancer surgery on treatment, morbidity, and mortality. J Gastrointest Surg. 2017;21:2000–8.
Busweiler LAD, Jeremiasen M, Wijnhoven BPL, Lindblad M, Lundell L, van de Velde CJH, et al. International benchmarking in oesophageal and gastric cancer surgery. BJS Open. 2018;3(1):62–73.
van der Werf LR, Voeten SC, van Loe CMM, Karthaus EG, Wouters MWJM, Prins HA. Data verification of nationwide clinical quality registries. BJS Open. 2019;3(6):857–64.
Dal Cero MD, Rodríguez-Santiago J, Miró M, Castro S, Miranda C, Santamaría M, et al. Evaluation of data quality in the Spanish EURECCA Esophagogastric Cancer Registry. Eur J Surg Oncol. 2021;47(12):3081–7.
Collins GS, Ai J, McCulloch P. Control chart methods for monitoring surgical performance: a case study from gastro-oesophageal surgery. Eur J Surg Oncol. 2011;37(6):473–80.
Sobin LH, Gospodarowicz MK, Wittekind C. TNM classification of malignant tumours. 7th ed. New York: Wiley-Blackwell; 2009. p. 73–7.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications. A new proposal with evaluation in a cohorte of 6336 patients and results of a Surrey. Ann Surg. 2004;240:205–13.
Pasquer A, Renaud F, Hec F, Gandon A, Vanderbeken M, Drubay V, et al. Is centralization needed for esophageal and gastric cancer patients with low operative risk? A nationwide study. Ann Surg. 2016;264(5):823–30.
Van Gestel Y, Lemmens V, de Hingh I, Stevens J, Rutten H, Nieuwenhuijzen G, et al. Influence of comorbidity and age on 1-, 2-, and 3-month postoperative mortality rates in gastrointestinal cancer patients. Ann Surg Oncol. 2013;20:371–80.
Talsma AK, Lingsma HF, Steyerberg EW, Wijnhoven BP, Van Lanschot JJ. The 30-day versus in-hospital and 90-day mortality after esophagectomy as indicators for quality of care. Ann Surg. 2014;260(2):267–73.
Nelen SD, Bosscha K, Lemmens VEPP, Hartgrink HH, Verhoeven RHA, de Wilt JHW, et al. Morbidity and mortality according to age following gastrectomy for gastric cancer. Br J Surg. 2018;105(9):1163–70.
Asplund J, Gottlieb-Vedi E, Leijonmarck W, Mattsson F, Lagergren J. Prognosis after surgery for gastric adenocarcinoma in the Swedish Gastric Cancer Surgery Study (SWEGASS). Acta Oncol. 2021;60(4):513–20.
Tegels JJW, Maat MFG, Hulsewe KWE, Hoofwijk AGM, Stoot JHMB. Value of Geriatric Frailty and Nutritional Status Assessment in Predicting Postoperative Mortality in Gastric Cancer Surgery. J Gastrointest Surg. 2014;18:439–46.
Joharatnam-Hogan N, Shiu KK, Khan K. Challenges in the treatment of gastric cancer in the older patient. Cancer Treat Rev. 2020;85:101980.
Busweiler LA, Henneman D, Dikken JL, Fiocco M, van Berge Henegouwen MI, Wijnhoven BP, et al. Failure-to-rescue in patients undergoing surgery for esophageal or gastric cancer. Eur J Surg Oncol. 2017;43(10):1962–9.
Diers J, Baum P, Wagner JC, Matthes H, Pietryga S, Baumann N, et al. Hospital volume following major surgery for gastric cancer determines in-hospital mortality rate and failure to rescue: a nation-wide study based on German billing data (2009-2017). Gastric Cancer. 2021;24(4):959–69.
Baiocchi GL, Giacopuzzi S, Reim D, Piessen G, Matos da Costa P, Reynolds JV, et al. Incidence and Grading of Complications After Gastrectomy for Cancer Using the GASTRODATA Registry: A European Retrospective Observational Study. Ann Surg. 2020;272(5):807–13.
Low DE, Kuppusamy MK, Alderson D, Cecconello I, Chang AC, Darling G, et al. Benchmarking complications associated with esophagectomy. Ann Surg. 2019;269:291–8.
Sabater L, Garcia-Granero A, Escrig-Sos J, Gomez-Mateo MC, Sastre J, Ferrandez A, et al. Outcome quality standards in pancreatic oncologic surgery. Ann Surg Oncol. 2014;21:1138–46.
Kikuchi H, Miyata H, Konno H, Kamiya K, Tomotaki A, Gotoh M, et al. Development and external validation of preoperative risk models for operative morbidities after total gastrectomy using a Japanese web-based nationwide registry. Gastric Cancer. 2017;20:987–97.
Jeremiasen M, Linder G, Hedberg J, Lundell L, Björ O, Lindblad M, et al. Improvements in esophageal and gastric cancer care in Sweden-population-based results 2007-2016 from a national quality register. Dis Esophagus. 2020;33(3):1–9.
Hu W, Ma JJ, Zang L, Xue P, Xu H, Wang ML, et al. Learning curve and long-term outcomes of laparoscopy-assisted distal gastrectomy for gastric cancer. J Laparoendosc Adv Surg Tech A. 2014;24(7):487–92.
Jung DH, Son SY, Park YS, Shin DJ, Ahn HS, Ahn SH, et al. The learning curve associated with laparoscopic total gastrectomy. Gastric Cancer. 2016;19:264–72.
Acknowledgements
The authors thank Miguel Angel Cuesta and Jose Schneider for revising the manuscript.
Esophagogastric Cancer Registry of the Comunitat Valenciana (RECEG-CV) group: Consol Sabater (Servei d’Estudis Epidemiològics i Vigilància de Malalties no Transmissibles. Comunitat Valenciana), Vicente Espert (Hospital General Universitario de Elda, Alicante, Spain), Gonzalo Todoli (Hospital General La Plana, Spain), María-José Cases (Hospital Vega Baja de Orihuela, Spain), Mario Mella (Hospital Universitario San Juan, Spain), Fernando Lopez-Mozos (Hospital Clínico Universitario de Valencia, Spain), Silvia Carbonell (Hospital General Universitario de Alicante, Spain), Marcos Bruna (Hospital Universitario y Politécnico La Fe de Valencia, Spain), Claudia Mulas (Hospital General Universitario de Valencia, Spain), Ramon Trullenque (Hospital Doctor Peset de Valencia, Spain), José-Antonio Barreras (Hospital General Universitario de Elda, Spain), Luis Gomez (Hospital General Universitario de Castellón, Spain), Cristina Sancho (Hospital Universitario Arnau de Vilanova de Valencia, Spain), Javier Aguilo (Hospital Lluis Alcanyis de Xativa, Spain), Jose-Manuel Navarro (Hospital Vega Baja de Orihuela, Spain), Antonio Compañ (Hospital Universitario San Juan, Spain), Alicia Calero (Hospital General Universitario de Elche, Spain), Enrique Canelles (Hospital de Requena. Spain), Erick Montilla (Hospital de Denia, Spain), Rodolfo Rodriguez (Hospital de Sagunto, Spain), Yannko Gonzalez (Hospital de Torrevieja, Spain), Alejandro Moya (Universidad Miguel Hernández de Elche, Spain), Xavier Barber (Universidad Miguel Hernández de Elche, Spain), Jose Puche (Hospital General Universitario de Valencia, Spain), Francisco Asencio (Hospital Universitario Arnau de Vilanova de Valencia, Spain).
Funding
The authors declare no funding sources for that research.
Author information
Authors and Affiliations
Consortia
Contributions
Study design: F-J L, J E-S. Data acquisition: F-J L, J E-S, R M-O, C Z, F M, M O, N P, V E, J C, A R, and the RECEG-CV group. Data analysis and interpretation: F-J L, J E-S. Statistical analysis: J E-S, A M, X B. Manuscript writing: F-J L. Manuscript review: F-J L, R M-O, C Z, F M, M O, N P, V E, J C, A R. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Written informed consent previous to surgical resection was obtained from all patients. The study was approved by the Ethics Committee of the General University Hospital of Elche (Spain) (PI 46/2022).
Consent for publication
Not applicable
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Lacueva, FJ., Escrig-Sos, J., Marti-Obiol, R. et al. Short-term postoperative outcomes of gastric adenocarcinoma patients treated with curative intent in low-volume centers. World J Surg Onc 20, 344 (2022). https://doi.org/10.1186/s12957-022-02804-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12957-022-02804-x